The Association between Red Blood Cell Distribution Width and Mortality Risk after Hip Fracture: A Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Study Identification
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Methodological Quality
2.4. Outcomes of Interest
2.5. Statistical Analysis, Data Synthesis, and Heterogeneity Assessment
3. Results
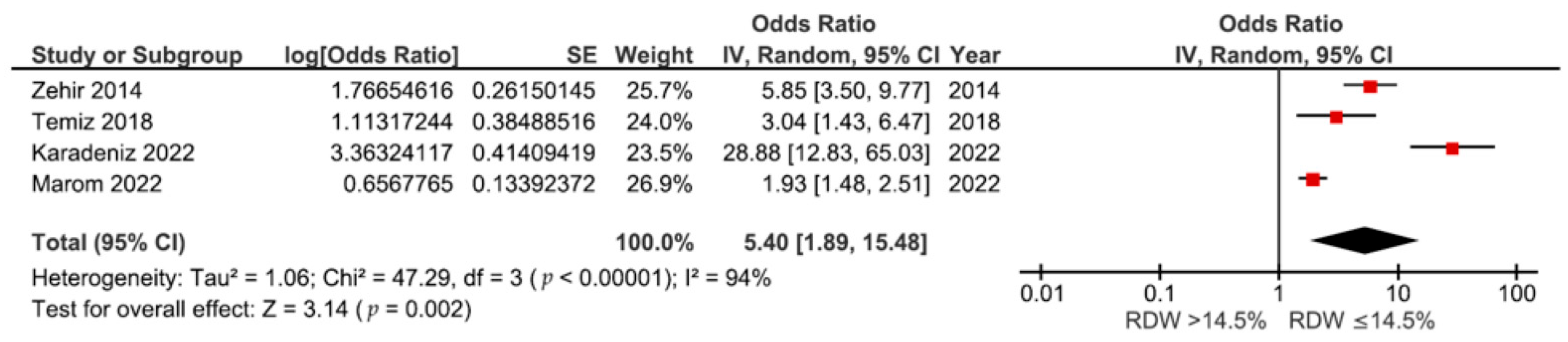
3.1. Association between RDW and 1-Year Mortality
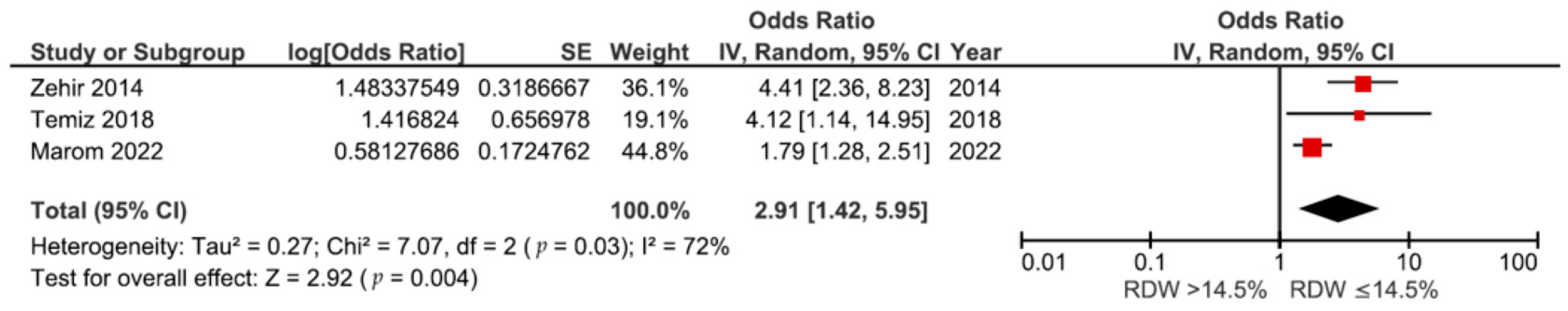
3.2. Association between RDW and 6-Month Mortality
3.3. Association between RDW and 3-Month Mortality
3.4. Association between RDW and 30-Day Mortality
3.5. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kanis, J.A.; Odén, A.; McCloskey, E.V.; Johansson, H.; Wahl, D.A.; Cooper, C.; on behalf of the IOF Working Group on Epidemiology and Quality of Life. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos. Int. 2012, 23, 2239–2256. [Google Scholar] [CrossRef]
- Mattisson, L.; Bojan, A.; Enocson, A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: Data from the Swedish fracture register. BMC Musculoskelet. Disord. 2018, 19, 369. [Google Scholar] [CrossRef] [PubMed]
- Adeyemi, A.; Delhougne, G. Incidence and Economic Burden of Intertrochanteric Fracture. JBJS Open Access 2019, 4, e0045. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-P.; Kuo, Y.-J.; Liu, C.-H.; Chien, P.-C.; Chang, W.-C.; Lin, C.-Y.; Pakpour, A.H. Prognostic factors for 1-year functional outcome, quality of life, care demands, and mortality after surgery in Taiwanese geriatric patients with a hip fracture: A prospective cohort study. Ther. Adv. Musculoskelet. Dis. 2021, 13, 1759720X211028360. [Google Scholar] [CrossRef] [PubMed]
- Lizaur-Utrilla, A.; Martinez-Mendez, D.; Collados-Maestre, I.; Miralles-Muñoz, F.A.; Marco-Gomez, L.; Lopez-Prats, F.A. Early surgery within 2 days for hip fracture is not reliable as healthcare quality indicator. Injury 2016, 47, 1530–1535. [Google Scholar] [CrossRef] [PubMed]
- Guzon-Illescas, O.; Fernandez, E.P.; Villarias, N.C.; Donate, F.J.Q.; Peña, M.; Alonso-Blas, C.; García-Vadillo, A.; Mazzucchelli, R. Mortality after osteoporotic hip fracture: Incidence, trends, and associated factors. J. Orthop. Surg. Res. 2019, 14, 203. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsen, B.; van Staa, T.; Ariely, R.; Olson, M.; Cooper, C. Excess mortality following hip fracture: A systematic epidemiological review. Osteoporos. Int. 2009, 20, 1633–1650. [Google Scholar] [CrossRef] [PubMed]
- Milman, R.; Zikrin, E.; Shacham, D.; Freud, T.; Press, Y. Handgrip Strength as a Predictor of Successful Rehabilitation after Hip Fracture in Patients 65 Years of Age and Above. Clin. Interv. Aging 2022, 17, 1307–1317. [Google Scholar] [CrossRef]
- Laulund, A.S.; Lauritzen, J.B.; Duus, B.R.; Mosfeldt, M.; Jørgensen, H.L. Routine blood tests as predictors of mortality in hip fracture patients. Injury 2012, 43, 1014–1020. [Google Scholar] [CrossRef]
- Chen, B.-K.; Liu, Y.-C.; Chen, C.-C.; Chen, Y.-P.; Kuo, Y.-J.; Huang, S.-W. Correlation between C-reactive protein and postoperative mortality in patients undergoing hip fracture surgery: A meta-analysis. J. Orthop. Surg. Res. 2023, 18, 182. [Google Scholar] [CrossRef]
- Garbharran, U.; Chinthapalli, S.; Hopper, I.; George, M.; Back, D.L.; Dockery, F. Red cell distribution width is an independent predictor of mortality in hip fracture. J. Am. Geriatr. Soc. 2012, 42, 258–261. [Google Scholar] [CrossRef] [PubMed]
- Lv, H.; Zhang, L.; Long, A.; Mao, Z.; Shen, J.; Yin, P.; Li, M.; Zeng, C.; Zhang, L.; Tang, P. Red Cell Distribution Width as an Independent Predictor of Long-Term Mortality in Hip Fracture Patients: A Prospective Cohort Study. J. Bone Miner. Res. 2015, 31, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Marom, O.; Paz, I.; Topaz, G.; Ohana, N.; Yaacobi, E. Red cell distribution width–A mortality predictor in older adults with proximal femoral fracture. Arch. Gerontol. Geriatr. 2022, 100, 104623. [Google Scholar] [CrossRef] [PubMed]
- De La Cruz-Vargas, J.A.; Vento Benel, F.C.; Perez, M.A.; Correa-Lopez, L.E. Red cell distribution width as mortality prognostic factor in patients 65 and older with hip fracture. Rev. Salud Uninorte 2019, 35, 13–28. [Google Scholar] [CrossRef]
- Salvagno, G.L.; Sanchis-Gomar, F.; Picanza, A.; Lippi, G. Red blood cell distribution width: A simple parameter with multiple clinical applications. Crit. Rev. Clin. Lab. Sci. 2014, 52, 86–105. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.C. Approach to Anemia in the Adult and Child. In Hematology—Basic Principles and Practice, 7th ed.; Hoffman, E.J.B.R., Silberstein, L.E., Heslop, H.E., Anastasi, J., Salama, M.E., Abutalib, S.A., Eds.; Elsevier: Philadelphia, PA, USA, 2018; pp. 458–467. [Google Scholar]
- Lippi, G.; Plebani, M. Red blood cell distribution width (RDW) and human pathology. One size fits all. CCLM 2014, 52, 1247–1249. [Google Scholar] [CrossRef]
- Fava, C.; Cattazzo, F.; Hu, Z.-D.; Lippi, G.; Montagnana, M. The role of red blood cell distribution width (RDW) in cardiovascular risk assessment: Useful or hype? Ann. Transl. Med. 2019, 7, 581. [Google Scholar] [CrossRef]
- Patel, K.V.; Semba, R.D.; Ferrucci, L.; Newman, A.B.; Fried, L.P.; Wallace, R.B.; Bandinelli, S.; Phillips, C.S.; Yu, B.; Connelly, S.; et al. Red Cell Distribution Width and Mortality in Older Adults: A Meta-analysis. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 65, 258–265. [Google Scholar] [CrossRef]
- Patel, K.V.; Ferrucci, L.; Ershler, W.B.; Longo, D.L.; Guralnik, J.M. Red Blood Cell Distribution Width and the Risk of Death in Middle-aged and Older Adults. JAMA Intern. Med. 2009, 169, 515–523. [Google Scholar] [CrossRef]
- Kinoshita, K.; Satake, S.; Murotani, K.; Takemura, M.; Matsui, Y.; Arai, H. Physical Frailty and Hemoglobin-to-Red Cell Distribution Width Ratio in Japanese Older Outpatients. J. Frailty Aging 2022, 11, 393–397. [Google Scholar] [CrossRef]
- Kim, K.M.; Lui, L.; A Cauley, J.; E Ensrud, K.; Orwoll, E.S.; Schousboe, J.T.; Cummings, S.R.; the Osteoporotic Fractures in Men (MrOS) Study Research Group. Red Cell Distribution Width Is a Risk Factor for Hip Fracture in Elderly Men without Anemia. J. Bone Miner. Res. 2020, 35, 869–874. [Google Scholar] [CrossRef]
- Cheng, X.; Fan, L.; Hao, J.; He, H.; Yan, J.; Zhu, Y. Red Cell Distribution Width-to-High-Density Lipoprotein Cholesterol Ratio (RHR): A Promising Novel Predictor for Preoperative Deep Vein Thrombosis in Geriatric Patients with Hip Fracture. Clin. Interv. Aging 2022, 17, 1319–1329. [Google Scholar] [CrossRef] [PubMed]
- Aali-Rezaie, A.; Alijanipour, P.; Shohat, N.; Vahedi, H.; Foltz, C.; Parvizi, J. Red Cell Distribution Width: An Unacknowledged Predictor of Mortality and Adverse Outcomes Following Revision Arthroplasty. J. Arthroplast. 2018, 33, 3514–3519. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews Systematic reviews and Meta-Analyses. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Wiley-Blackwell: Chichester, UK, 2023; Available online: www.training.cochrane.org/handbook (accessed on 1 June 2023).
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef]
- Thorlund, K.; Imberger, G.; Johnston, B.C.; Walsh, M.; Awad, T.; Thabane, L.; Gluud, C.; Devereaux, P.J.; Wetterslev, J. Evolution of Heterogeneity (I2) Estimates and Their 95% Confidence Intervals in Large Meta-Analyses. PLoS ONE 2012, 7, e39471. [Google Scholar] [CrossRef]
- Emektar, E.; Corbacioglu, S.K.; Dagar, S.; Uzunosmanoglu, H.; Safak, T.; Cevik, Y. Prognostic Value of the Neutrophil–Lymphocyte and Platelet–Lymphocyte Ratios in Predicting One-Year Mortality in Patients with Hip Fractures and Aged Over 60 Years. Eurasian J. Emerg. Med. 2017, 16, 165–170. [Google Scholar] [CrossRef]
- Hamdan, M.; Haddad, B.I.; Jabaiti, M.; Alryalat, S.A.; Abdulelah, A.A.; Alabed, S.H.; Alabdullah, T.F.; Aouant, A.N.; Shahein, H.E.; I Dweik, H.; et al. Does Red Cell Distribution Width Predict Hip Fracture Mortality Among the Arab Population? A Single-Center Retrospective Cohort Study. Int. J. Gen. Med. 2021, 14, 10195–10202. [Google Scholar] [CrossRef]
- Karadeniz, S.; Yurtbay, A. Predicting mortality rate in elderly patients operated for hip fracture using red blood cell distribution width, neutrophil-to-lymphocyte ratio, and Nottingham Hip Fracture Score. Jt. Dis. Relat. Surg. 2022, 33, 538–546. [Google Scholar] [CrossRef]
- Temiz, A. Association between admission red cell distribution width and mortality in elderly hip fracture patients: A Retrospective Case-Control Study. Eurasian J. Med. Investig. 2018, 2, 29–34. [Google Scholar] [CrossRef]
- Wei-Hsiang, H.; Zhu, Y.; Zhang, J.; Zhang, Y. Pretreatment red blood cell distribution width as an efficient predictor of survival in older patients undergoing hip fracture surgery. Int. J. Clin. Pract. 2021, 75, e14791. [Google Scholar] [CrossRef]
- Zehir, S. Red cell distribution width and mortality in patients with hip fracture treated with partial prosthesis. Acta Orthop. Traumatol. Turc. 2014, 48, 141–146. [Google Scholar] [CrossRef]
- Osawa, Y.; Tanaka, T.; Semba, R.D.; Fantoni, G.; Moaddel, R.; Candia, J.; Simonsick, E.M.; Bandinelli, S.; Ferrucci, L. Proteins in the pathway from high red blood cell width distribution to all-cause mortality. EBioMedicine 2022, 76, 103816. [Google Scholar] [CrossRef]
- Pepe, J.; Colangelo, L.; De Martino, V.; Occhiuto, M.; Iervolino, D.; Pasqualetti, P.; Minisola, S.; Cipriani, C. Study of the link between hemotopoietic and skeletal systems in patients attending a referral center for osteoporosis. J. Endocrinol. Investig. 2023, 46, 2391–2397. [Google Scholar] [CrossRef]
- Zurauskaite, G.; Meier, M.; Voegeli, A.; Koch, D.; Haubitz, S.; Kutz, A.; Bernasconi, L.; Huber, A.; Bargetzi, M.; Mueller, B.; et al. Biological pathways underlying the association of red cell distribution width and adverse clinical outcome: Results of a prospective cohort study. PLoS ONE 2018, 13, e0191280. [Google Scholar] [CrossRef]
- Atalay, H. Red Cell Distribution Width and Acute Complications of Diabetes. Acta Endocrinol. 2018, 14, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Ananthaseshan, S.; Bojakowski, K.; Sacharczuk, M.; Poznanski, P.; Skiba, D.S.; Wittberg, L.P.; McKenzie, J.; Szkulmowska, A.; Berg, N.; Andziak, P.; et al. Red blood cell distribution width is associated with increased interactions of blood cells with vascular wall. Sci. Rep. 2022, 12, 13676. [Google Scholar] [CrossRef] [PubMed]
- Malandrino, N.; Wu, W.C.; Taveira, T.H.; Whitlatch, H.B.; Smith, R.J. Association between red blood cell distribution width and macrovascular and microvascular complications in diabetes. Diabetologia 2011, 55, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Li, J.; Lin, Y.; Yang, H.; Cao, S. Association Between Red Blood Cell Distribution Width and All-cause Mortality in Chronic Kidney Disease Patients: A Systematic Review and Meta-analysis. Arch. Med Res. 2017, 48, 378–385. [Google Scholar] [CrossRef]
- Wu, H.; Liao, B.; Cao, T.; Ji, T.; Huang, J.; Ma, K. Diagnostic value of RDW for the prediction of mortality in adult sepsis patients: A systematic review and meta-analysis. Front. Immunol. 2022, 13, 997853. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Han, X.; Wang, Y.; Hou, T.; Cong, L.; Tang, S.; Han, X.; Ngandu, T.; Kivipelto, M.; Winblad, B.; et al. Red Cell Distribution Width and Dementia Among Rural-Dwelling Older Adults: The MIND-China Study. J. Alzheimer’s Dis. 2021, 83, 1187–1198. [Google Scholar] [CrossRef]
- Aslam, H.; Oza, F.; Ahmed, K.; Kopel, J.; Aloysius, M.M.; Ali, A.; Dahiya, D.S.; Aziz, M.; Perisetti, A.; Goyal, H. The Role of Red Cell Distribution Width as a Prognostic Marker in Chronic Liver Disease: A Literature Review. Int. J. Mol. Sci. 2023, 24, 3487. [Google Scholar] [CrossRef] [PubMed]
- Menzies, I.B.; Mendelson, D.A.; Kates, S.L.; Friedman, S.M. The Impact of Comorbidity on Perioperative Outcomes of Hip Fractures in a Geriatric Fracture Model. Geriatr. Orthop. Surg. Rehabilitation 2012, 3, 129–134. [Google Scholar] [CrossRef]
- Loecker, C.; Schmaderer, M.; Zimmerman, L. Frailty in Young and Middle-Aged Adults: An Integrative Review. J. Frailty Aging 2021, 10, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Thisayakorn, P.; Tangwongchai, S.; Tantavisut, S.; Thipakorn, Y.; Sukhanonsawat, S.; Wongwarawipat, T.; Sirivichayakul, S.; Maes, M. Immune, Blood Cell, and Blood Gas Biomarkers of Delirium in Elderly Individuals with Hip Fracture Surgery. Dement. Geriatr. Cogn. Disord. 2021, 50, 161–169. [Google Scholar] [CrossRef]
- Clark, D.; Nakamura, M.; Miclau, T.; Marcucio, R. Effects of Aging on Fracture Healing. Curr. Osteoporos. Rep. 2017, 15, 601–608. [Google Scholar] [CrossRef]
- Prasad, G.; Dhillon, M.S.; Khullar, M.; Nagi, O.N. Evaluation of oxidative stress after fractures. A preliminary study. Acta Orthop. Belg. 2003, 69, 546–551. [Google Scholar]
- Yin, P.; Lv, H.; Li, Y.; Meng, Y.; Zhang, L.; Tang, P. Hip fracture patients who experience a greater fluctuation in RDW during hospital course are at heightened risk for all-cause mortality: A prospective study with 2-year follow-up. Osteoporos. Int. 2018, 29, 1559–1567. [Google Scholar] [CrossRef]
- Akcal, M.; Eke, I. Post-Operative Red Cell Distribution Width Increase May Predict Mortality in Patients Operated for Hip Fracture. Clin. Lab. 2021, 67, 2568–2575. [Google Scholar] [CrossRef]
- Ryan, G.; Nowak, L.; Melo, L.; Ward, S.; Atrey, A.; Schemitsch, E.H.; Nauth, A.; Khoshbin, A. Anemia at Presentation Predicts Acute Mortality and Need for Readmission Following Geriatric Hip Fracture. JBJS Open Access 2020, 5, e20.00048. [Google Scholar] [CrossRef] [PubMed]
- Puckeridge, G.; Terblanche, M.; Wallis, M.; Fung, Y.L. Blood management in hip fractures; are we leaving it too late? A retrospective observational study. BMC Geriatr. 2019, 19, 79. [Google Scholar] [CrossRef] [PubMed]
- Vochteloo, A.J.; van der Burg, B.L.B.; Mertens, B.J.; Niggebrugge, A.H.; de Vries, M.R.; Tuinebreijer, W.E.; Bloem, R.M.; Nelissen, R.G.; Pilot, P. Outcome in hip fracture patients related to anemia at admission and allogeneic blood transfusion: An analysis of 1262 surgically treated patients. BMC Musculoskelet. Disord. 2011, 12, 262. [Google Scholar] [CrossRef] [PubMed]
- AAOS. Management of Hip Fractures in Older Adults—Evidence-Based Clinical Practice Guideline. 2021. Available online: https://www.aaos.org/hipfxcpg (accessed on 15 February 2024).
- NICE. Hip fracture: Management. In NICE Clinical Guidelines: National Institute for Health and Care Excellence; NICE: London, UK, 2023. [Google Scholar]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, B.T.T.; Tran, D.N.A.; Nguyen, T.T.; Kuo, Y.-J.; Chen, Y.-P. The Association between Red Blood Cell Distribution Width and Mortality Risk after Hip Fracture: A Meta-Analysis. Medicina 2024, 60, 485. https://doi.org/10.3390/medicina60030485
Nguyen BTT, Tran DNA, Nguyen TT, Kuo Y-J, Chen Y-P. The Association between Red Blood Cell Distribution Width and Mortality Risk after Hip Fracture: A Meta-Analysis. Medicina. 2024; 60(3):485. https://doi.org/10.3390/medicina60030485
Chicago/Turabian StyleNguyen, Bao Tu Thai, Duy Nguyen Anh Tran, Tan Thanh Nguyen, Yi-Jie Kuo, and Yu-Pin Chen. 2024. "The Association between Red Blood Cell Distribution Width and Mortality Risk after Hip Fracture: A Meta-Analysis" Medicina 60, no. 3: 485. https://doi.org/10.3390/medicina60030485
APA StyleNguyen, B. T. T., Tran, D. N. A., Nguyen, T. T., Kuo, Y.-J., & Chen, Y.-P. (2024). The Association between Red Blood Cell Distribution Width and Mortality Risk after Hip Fracture: A Meta-Analysis. Medicina, 60(3), 485. https://doi.org/10.3390/medicina60030485






