The Influence of the COVID-19 Pandemic on Hospitalizations for Ambulatory Care-Sensitive Conditions in Split-Dalmatia County, Croatia
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. All Hospitalization’s General Descriptive Data and Age Distribution
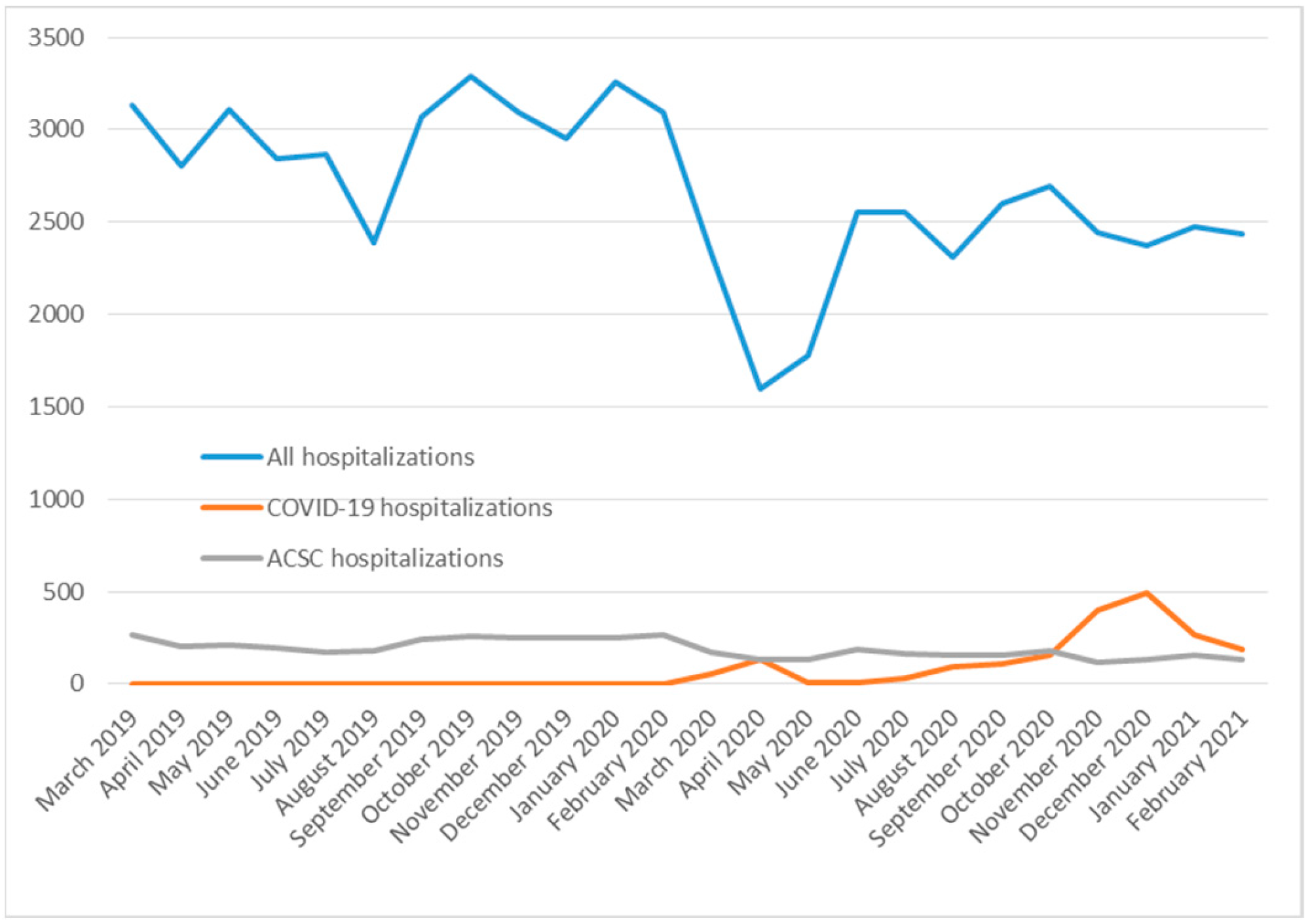
3.2. Timeline of All Hospitalizations, ACSC Hospitalizations, and COVID-19 Hospitalizations
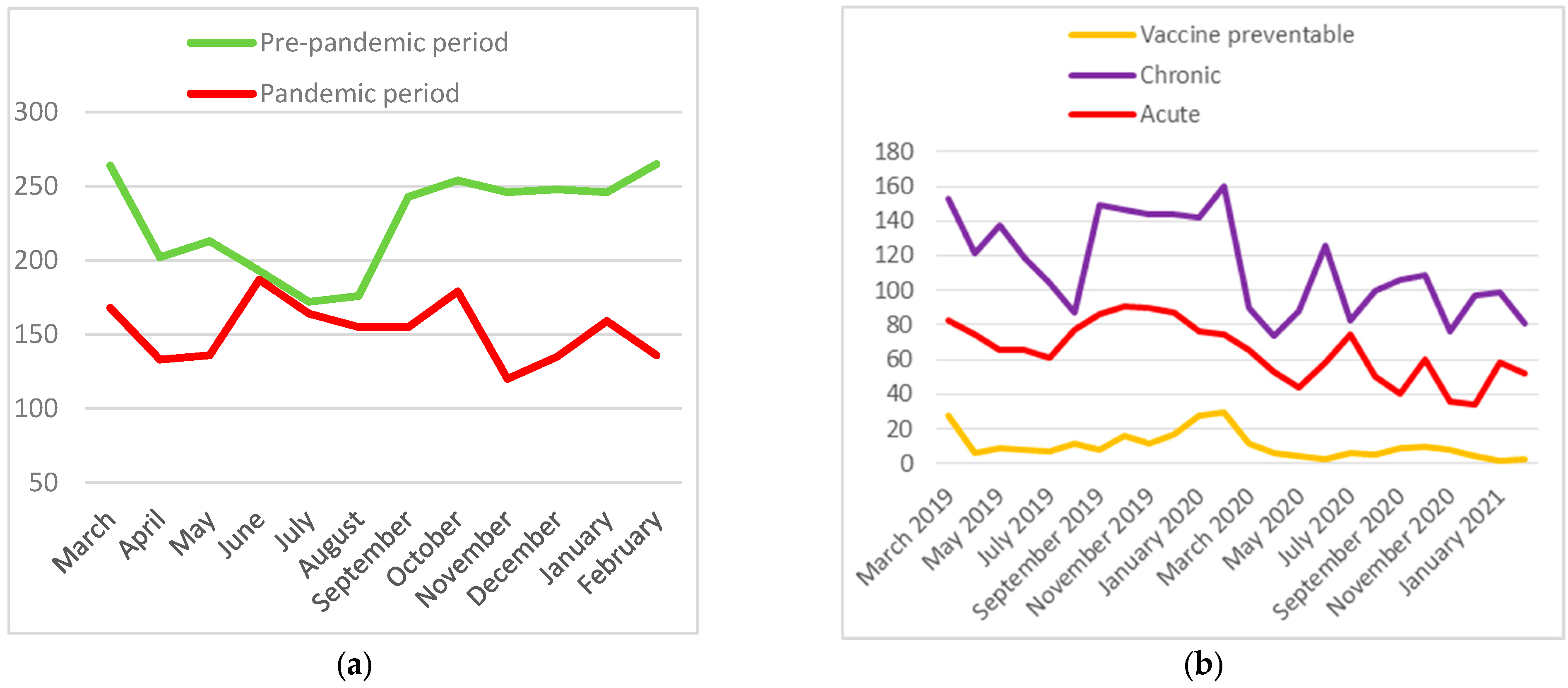
3.3. ACSC Hospitalizations
3.4. Vaccine-Preventable, Chronic and Acute ACSC Hospitalizations Distribution and Relative Risks
3.5. Vaccine-Preventable, Chronic and Acute ACSC Subcategories Hospitalizations
3.6. Type of Discharge Analyses
3.7. Inpatient Length of Stay Analyses
4. Discussion
4.1. Principal Findings
4.2. Comparisons with Other Studies
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 12 August 2023).
- Vrdoljak, E.; Balja, M.P.; Marušić, Z.; Avirović, M.; Blažičević, V.; Tomasović, Č.; Čerina, D.; Bajić, Ž.; Miše, B.P.; Lovasić, I.B.; et al. COVID-19 pandemic effects on breast cancer diagnosis in Croatia: A population- and registry-based study. Oncologist 2021, 26, e1156–e1160. [Google Scholar] [CrossRef] [PubMed]
- Toner, E.; Waldhorn, R. What US Hospitals Should Do Now to Prepare for a COVID-19 Pandemic; Johns Hopkins Center for Health Security: Baltimore, MD, USA, 2020. [Google Scholar]
- Rosenbaum, L. The untold toll—The pandemic’s effects on patients without COVID-19. N. Engl. J. Med. 2020, 382, 2368–2371. [Google Scholar] [CrossRef] [PubMed]
- Mayor, S. COVID-19: Impact on cancer workforce and delivery of care. Lancet Oncol. 2020, 21, 633. [Google Scholar] [CrossRef]
- DeJong, C.; Katz, M.H.; Covinsky, K. Deferral of care for serious non-COVID-19 conditions: A hidden harm of COVID-19. JAMA Intern. Med. 2021, 181, 274. [Google Scholar] [CrossRef] [PubMed]
- UK Coronavirus Cancer Monitoring Project Team. The UK Coronavirus Cancer Monitoring Project: Protecting patients with cancer in the era of COVID-19. Lancet. Oncol. 2020, 21, 622–624. [Google Scholar] [CrossRef] [PubMed]
- Eswaran, V.; Wang, R.C.; Vashi, A.A.; Kanzaria, H.K.; Fahimi, J.; Raven, M.C. Patient reported delays in obtaining emergency care during COVID19. Am. J. Emerg. Med. 2022, 56, 306–309. [Google Scholar] [CrossRef]
- Becker, N.V.; Karmakar, M.; Tipirneni, R.; Ayanian, J.Z. Trends in hospitalizations for ambulatory care-sensitive conditions during the COVID-19 pandemic. JAMA. Netw. Open. 2022, 5, e222933. [Google Scholar] [CrossRef]
- Whaley, C.M.; Pera, M.F.; Cantor, J.; Chang, J.; Velasco, J.; Hagg, H.K.; Sood, N.; Bravata, D.M. Changes in health services use among commercially insured US populations during the COVID-19 pandemic. JAMA Netw. Open. 2020, 3, e2024984. [Google Scholar] [CrossRef]
- Conway, R.; O’Riordan, D.; Byrne, D.; Cournane, S.; Coveney, S.; Silke, B. Deprivation influences the emergency admission rate of ambulatory care sensitive conditions. Clin. Med. 2016, 16, 119–123. [Google Scholar] [CrossRef]
- Billings, J.; Zeitel, L.; Lukomnik, J.; Carey, T.S.; Blank, A.E.; Newman, L. Impact of socioeconomic status on hospital use in New York City. Health Aff. 1993, 12, 162–173. [Google Scholar] [CrossRef]
- Purdy, S.; Griffin, T.; Salisbury, C.; Sharp, D. Ambulatory care sensitive conditions: Terminology and disease coding need to be more specific to aid policy makers and clinicians. Public Health 2009, 123, 169–173. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Regional Office for Europe. Assessing Health Services Delivery Performance with Hospitalizations for Ambulatory Care Sensitive Conditions Working Document; WHO Regional Office for Europe: Copenhagen, Denmark, 2016. [Google Scholar]
- Sarmento, J.; Rocha, J.V.M.; Santana, R. Defining ambulatory care sensitive conditions for adults in Portugal. BMC Health Serv. Res. 2020, 20, 75. [Google Scholar] [CrossRef] [PubMed]
- Nedel, F.B.; Facchini, L.A.; Bastos, J.L.; Martín, M. Conceptual and methodological aspects in the study of hospitalizations for ambulatory care sensitive conditions. Ciênc. Saúde Coletiva 2011, 16, 1145–1154. [Google Scholar] [CrossRef]
- Ham, C.; Imison, C.; Jennings, M. Avoiding Hospital Admissions: Lessons from Evidence and Experience; The King’s Fund: London, UK, 2010. [Google Scholar]
- Page, A.; Ambrose, S.; Glover, J.; Hetzel, D. Atlas of Avoidable Hospitalisations in Australia: Ambulatory Care-Sensitive Conditions; PHIDU, University of Adelaide: Adelaide, Australia, 2007. [Google Scholar]
- Lamberti-Castronuovo, A.; Valente, M.; Aleni, C.; Hubloue, I.; Ragazzoni, L.; Barone-Adesi, F. Using ambulatory care sensitive conditions to assess primary health care performance during disasters. A systematic review. Int. J. Environ. Res. Public Health 2022, 19, 9193. [Google Scholar] [CrossRef] [PubMed]
- Leuchter, R.K.; Villaflores, C.W.A.; Norris, K.C.; Sorensen, A.; Vangala, S.; Sarkisian, C.A. Racial disparities in potentially avoidable hospitalizations during the COVID-19 pandemic. Am. J. Prev. Med. 2021, 61, 235–239. [Google Scholar] [CrossRef] [PubMed]
- Wright, B.; Anderson, D.; Whitaker, R.; Shrader, P.; Bettger, J.P.; Wong, C.; Shafer, P. Comparing health care use and costs among new Medicaid enrollees before and during the COVID-19 pandemic. BMC Health Serv. Res. 2021, 21, 1152. [Google Scholar] [CrossRef] [PubMed]
- Rennert-May, E.; Leal, J.; Thanh, N.X.; Lang, E.; Dowling, S.; Manns, B.; Wasylak, T.; Ronksley, P.E. The impact of COVID-19 on hospital admissions and emergency department visits: A population-based study. PLoS ONE 2021, 16, e0252441. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative; The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 4, 344–349. [Google Scholar] [CrossRef]
- Smoljanović, A.; Smoljanović, M.; Marasović Šušnjara, I.; Sučić, K.K. Potentially preventable hospitalizations in Split-Dalmatia County (Croatia) from 2005 to 2014. Eur. J. Public Health 2018, 28, cky214.265. [Google Scholar] [CrossRef]
- Georgiev, G.Z. Chi-Square Calculator. Available online: https://www.gigacalculator.com/calculators/chi-square-calculator.php (accessed on 13 April 2023).
- Georgiev, G.Z. Relative Risk Calculator. Available online: https://www.gigacalculator.com/calculators/relative-risk-calculator.php (accessed on 6 April 2023).
- The Kolmogorov-Smirnov Test of Normality. Available online: https://www.socscistatistics.com/tests/kolmogorov/default.aspx (accessed on 12 April 2023).
- Chazard, E.; Ficheur, G.; Beuscart, J.B.; Preda, C. How to compare the length of stay of two samples of inpatients? A simulation study to compare type I and type II errors of 12 statistical tests. Value Health 2017, 20, 992–998. [Google Scholar] [CrossRef]
- Kaneko, M.; Shimizu, S.; Oishi, A.; Fushimi, K. Impact of COVID-19 infection rates on admissions for ambulatory care sensitive conditions: Nationwide difference-in-difference design in Japan. Fam. Med. Community Health 2022, 10, e001736. [Google Scholar] [CrossRef] [PubMed]
- IUS-INFO. Odluke Stožera Civilne Zaštite RH u 2020. Godini i Relevantni Propisi u Uvjetima Epidemije Koronavirusa. 2020. [IUS-INFO: Decisions of the Civil Protection Headquarters of the Republic of Croatia in 2020 and Relevant Regulations in the Conditions of The Coronavirus Epidemic. 2020]. 2020. Available online: https://www.iusinfo.hr/aktualno/u-sredistu/2020-odluke-stozera-civilne-zastite-rh-u-2020-godini-i-relevantni-propisi-u-uvjetima-epidemije-koronavirusa-41376 (accessed on 11 August 2023).
- Kalanj, K.; Marshall, R.; Karol, K.; Tiljak, M.K.; Orešković, S. The Impact of COVID-19 on Hospital Admissions in Croatia. Front. Public Health 2021, 9, 720948. [Google Scholar] [CrossRef] [PubMed]
- Džakula, A.; Banadinović, M.; Lukačević Lovrenčić, I.; Vajagić, M.; Dimova, A.; Rohova, M.; Minev, M.; Gabriela Scintee, S.; Vladescu, C.; Farcasanu, D.; et al. A comparison of health system responses to COVID-19 in Bulgaria, Croatia and Romania in 2020. Health Policy 2022, 126, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Bodilsen, J.; Nielsen, P.B.; Søgaard, M.; Dalager-Pedersen, M.; Speiser, L.O.Z.; Yndigegn, T.; Nielsen, H.; Larsen, T.B.; Skjøth, F. Hospital admission and mortality rates for non-covid diseases in Denmark during COVID-19 pandemic: Nationwide population based cohort study. BMJ 2021, 373, n1135. [Google Scholar] [CrossRef] [PubMed]
- European Observatory on Health Systems and Policies/European Commission/WHO Europe. COVID-19 Health System Response Monitor (HSRM). 2021. Available online: https://eurohealthobservatory.who.int/monitors/hsrm/ (accessed on 19 December 2023).
- Kaye, L.; Theye, B.; Smeenk, I.; Gondalia, R.; Barrett, M.A.; Stempel, D.A. Changes in medication adherence among patients with asthma and COPD during the COVID-19 pandemic. J. Allergy Clin. Immunol. Pract. 2020, 8, 2384–2385. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto, M.; Ishikawa, T.; Odawara, M. Behavioral changes in patients with diabetes during the COVID-19 pandemic. Diabetol. Int. 2021, 12, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulou, C.; Palmer, J.V.; Burls, A.; Ansuategi, E.; Ubeda-Carrillo, M.D.M.; Purdyet, S. What Conditions Could We Prioritise in the Primary Care Setting to Reduce Non-COVID-Related Admissions to Hospital? CEBM 2020, University of Oxford. Available online: https://www.cebm.net/covid-19/what-conditions-could-we-prioritise-in-the-primary-care-setting-to-reduce-non-covid-related-admissions-to-hospital (accessed on 6 April 2023).
- Abe, K.; Kawachi, I.; Iba, A.; Miyawaki, A. In-hospital deaths from ambulatory care–sensitive conditions before and during the COVID-19 pandemic in Japan. JAMA Netw. Open 2023, 6, e2319583. [Google Scholar] [CrossRef]
- De Filippo, O.; D’Ascenzo, F.; Angelini, F.; Bocchino, P.P.; Conrotto, F.; Saglietto, A.; Secco, G.G.; Campo, G.; Gallone, G.; Verardi, R.; et al. Reduced rate of hospital admissions for ACS during COVID-19 outbreak in Northern Italy. N. Engl. J. Med. 2020, 383, 88–89. [Google Scholar] [CrossRef]
- Tam, C.F.; Cheung, K.S.; Lam, S.; Wong, A.; Yung, A.; Sze, M.; Lam, Y.M.; Chan, C.; Tsang, T.C.; Tsui, M.; et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ. Cardiovasc. Qual. Outcomes 2020, 13, e006631. [Google Scholar] [CrossRef]
- Goddard, M.; Smith, P. Equity of access to health care services theory and evidence from the UK. Soc. Sci. Med. 2001, 53, 1149–1162. [Google Scholar] [CrossRef]
- Seherin, I.; Allen, G.; Henare, M.; Craig, K. Avoidable hospitalisations: Potential for primary and public health initiatives in Canterbury, New Zealand. N. Z. Med. J. 2006, 119, U2029. [Google Scholar]
- Rocha, J.V.M.; Santana, R.; Tell, J.E. Hospitalization for ambulatory care sensitive conditions: What conditions make inter-country comparisons possible? Health Policy Open 2021, 2, 100030. [Google Scholar] [CrossRef]
- Magan, P.; Otero, A.; Alberquilla, A.; Ribera, J.M. Geographic variations in avoidable hospitalizations in the elderly, in a health system with universal coverage. BMC Health Serv. Res. 2008, 8, 42. [Google Scholar] [CrossRef]
| Category | ICD-10 Code |
|---|---|
| Vaccine-preventable | |
| Influenza and pneumonia | J10, J11, J13, J14, J153, J154, J157, J159, J168, J181, J188 |
| Other vaccine preventable | A35, A36, A37, A80, B05, B06,B161, B169, B180, B181,B26,G000, M014 |
| Chronic | |
| Diabetes complications | E101–E108, E110–E118, E130–E138, E140–E148 |
| Nutritional deficiencies | E40–E43, E55.0, E643 |
| Iron deficiency anemia | D501-D509 |
| Hypertension | I10, I119 |
| Congestive heart failure | I110, I50, J81 |
| Angina | I20, I240, I248, I249 |
| Chronic obstructive pulmonary disease | J41–J44, J47, (J20) |
| Asthma | J45, J46 |
| Acute | |
| Dehydration and gastroenteritis | E86, K522, K528, K529 |
| Convulsions and epilepsy | G40, G41, O15, R56 |
| Ear, nose and throat infections | H66, H67, J02, J03, J06, J312 |
| Dental conditions | A690, K02–K06, K08, K098, K099, K12, K13 |
| Perforated/bleeding ulcer | K250–K252, K254–K256, K260–K262, K264–K266, K270–K272, K274–K276, K280–K282, K284–K286 |
| Ruptured appendix | K35 |
| Pyelonephritis | N10, N11, N12, N136 |
| Pelvic inflammatory disease | N70, N73, N74 |
| Cellulitis | L03, L04, L08.0, L08.8, L08.9, L88, L98.0, L98.3 |
| Gangrene | R02 |
| Age Group | Pre-Pandemic Period | Pandemic Period |
|---|---|---|
| 1–6 | 1072 (3.0%) | 718 (2.6%) |
| 7–14 | 1172 (3.3%) | 794 (2.8%) |
| 15–19 | 848 (2.4%) | 577 (2.1%) |
| 20–34 | 2825 (7.9%) | 2132 (7.6%) |
| 35–44 | 2482 (6.9%) | 1888 (6.7%) |
| 45–54 | 3620 (10.1%) | 2739 (9.7%) |
| 55–64 | 6081 (16.9%) | 4795 (17.0%) |
| 65–74 | 8054 (22.4%) | 6731 (23.9%) |
| 75 and more | 8571 (23.9%) | 7245 (25.7%) |
| Pre-Pandemic Period (March 20– February 2020) | Pandemic Period (March 2020– February 2021) | Pandemic vs. Pre-Pandemic Relative Risk (95% CI) | p-Value | |
|---|---|---|---|---|
| Hospitalization | ||||
| Total | 35,889 | 28,137 | 0.79 (0.775–0.798) | <0.01 |
| ACSC | 2772 | 1872 | 0.67 (0.635–0.714) | <0.01 |
| ACSC category | ||||
| Vaccine-preventable | 181 | 72 | 0.51 (0.386–0.666) | <0.01 |
| Chronic | 1608 | 1129 | 0.90 (0.831–0.965) | <0.01 |
| Acute | 933 | 626 | 0.86 (0.774–0.946) | <0.01 |
| ACSC—Type of discharge | ||||
| Death | 117 | 103 | 1.31 (1.013–1.698) | 0.05 |
| Other (home or transfer to another institution) | 2605 | 1724 | 0.986 (0.973–1.000) | 0.02 |
| ACSC Category | Relative Risk (95% CI) | p-Value |
| Chronic | ||
| Diabetes complications | 0.58 (0.49–0.68) | <0.001 |
| Hypertension | 0.63 (0.46–0.86) | 0.004 |
| Angina | 0.71 (0.61–0.82) | <0.001 |
| COPD | 0.37 (0.26–0.51) | <0.001 |
| Asthma | 0.22 (0.09–0.54) | <0.001 |
| Acute | ||
| Dehydration and gastroenteritis | 0.56 (0.36–0.88) | 0.006 |
| Convulsions and epilepsy | 0.76 (0.63–0.91) | 0.002 |
| Perforated/bleeding ulcer | 0.57 (0.44–0.74) | <0.001 |
| Pyelonephritis | 0.52 (0.40–0.67) | <0.001 |
| Pelvic inflammatory disease | 10.03 (2.35–42.92) | <0.001 |
| Cellulitis | 0.52 (0.38–0.72) | <0.001 |
| Vaccine-preventable | ||
| Influenza and pneumonia | 0.42 (0.32–0.55) | <0.001 |
| Other vaccine preventable | 0.09 (0.01–0.71) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marasović Šušnjara, I.; Mijaković, M.; Jurčev Savičević, A. The Influence of the COVID-19 Pandemic on Hospitalizations for Ambulatory Care-Sensitive Conditions in Split-Dalmatia County, Croatia. Medicina 2024, 60, 523. https://doi.org/10.3390/medicina60040523
Marasović Šušnjara I, Mijaković M, Jurčev Savičević A. The Influence of the COVID-19 Pandemic on Hospitalizations for Ambulatory Care-Sensitive Conditions in Split-Dalmatia County, Croatia. Medicina. 2024; 60(4):523. https://doi.org/10.3390/medicina60040523
Chicago/Turabian StyleMarasović Šušnjara, Ivana, Marijana Mijaković, and Anamarija Jurčev Savičević. 2024. "The Influence of the COVID-19 Pandemic on Hospitalizations for Ambulatory Care-Sensitive Conditions in Split-Dalmatia County, Croatia" Medicina 60, no. 4: 523. https://doi.org/10.3390/medicina60040523
APA StyleMarasović Šušnjara, I., Mijaković, M., & Jurčev Savičević, A. (2024). The Influence of the COVID-19 Pandemic on Hospitalizations for Ambulatory Care-Sensitive Conditions in Split-Dalmatia County, Croatia. Medicina, 60(4), 523. https://doi.org/10.3390/medicina60040523






