Aesthetic Rehabilitation Medicine: Enhancing Wellbeing beyond Functional Recovery
Abstract
1. Introduction
2. Materials and Methods
3. Multicomponent Role and Synergies in Aesthetic Rehabilitation
4. Injection Procedures in Aesthetic Rehabilitation
4.1. Botulinum Toxin Injections
4.2. Platelet-Rich Plasma (PRP) Therapy
4.3. Hyaluronic acid Therapy
4.4. Ozone Therapy and Carboxytherapy
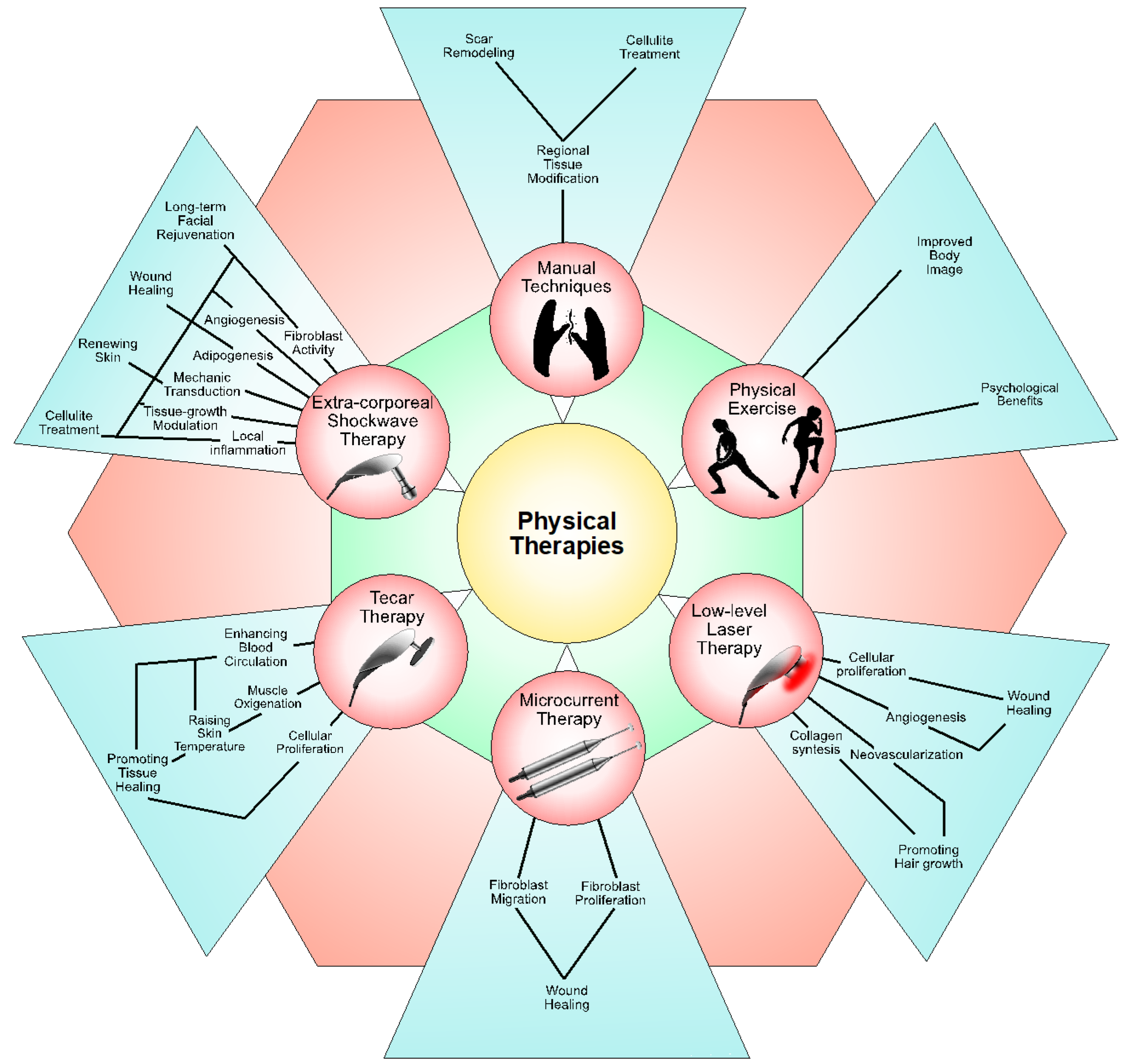
5. Physical Therapies in Aesthetic Rehabilitation
5.1. Extracorporeal Shock Wave Therapy (ESWT)
5.2. Laser Therapy
5.3. Microcurrent Therapy
5.4. Tecar Therapy
5.5. Physical Exercises
5.6. Manual Techniques
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leonardi, M.; Lee, H.; Kostanjsek, N.; Fornari, A.; Raggi, A.; Martinuzzi, A.; Yáñez, M.; Almborg, A.-H.; Fresk, M.; Besstrashnova, Y.; et al. 20 Years of ICF—International Classification of Functioning, Disability and Health: Uses and Applications around the World. Int. J. Environ. Res. Public Health 2022, 19, 11321. [Google Scholar] [CrossRef] [PubMed]
- Gimigliano, F.; de Sire, A.; Gastaldo, M.; Maghini, I.; Paoletta, M.; Pasquini, A.; Boldrini, P.; Selb, M.; Prodinger, B.; Group, S.R.S. Use of the International Classification of Functioning, Disability and Health Generic-30 Set for the characterization of outpatients: Italian Society of Physical and Rehabilitative Medicine Residents Section Project. Eur. J. Phys. Rehabil. Med. 2019, 55, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Dayan, S.; Rivkin, A.; Sykes, J.M.; Teller, C.F.; Weinkle, S.H.; Shumate, G.T.; Gallagher, C.J. Aesthetic Treatment Positively Impacts Social Perception: Analysis of Subjects From the HARMONY Study. Aesthetic Surg. J. 2019, 39, 1380–1389. [Google Scholar] [CrossRef]
- Papadopulos, N.A.; Kovacs, L.; Krammer, S.; Herschbach, P.; Henrich, G.; Biemer, E. Quality of life following aesthetic plastic surgery: A prospective study. J. Plast. Reconstr. Aesthetic Surg. 2007, 60, 915–921. [Google Scholar] [CrossRef] [PubMed]
- Papadopulos, N.A.; Kolassa, M.J.; Henrich, G.; Herschbach, P.; Kovacs, L.; Machens, H.G.; Klöppel, M. Quality of life following aesthetic liposuction: A prospective outcome study. J. Plast. Reconstr. Aesthetic Surg. 2019, 72, 1363–1372. [Google Scholar] [CrossRef] [PubMed]
- Pereira, I.N.; Hassan, H. Impact of botulinum toxin for facial aesthetics on psychological well-being and quality of life: Evidence-based review. J. Plast. Reconstr. Aesthetic Surg. 2022, 75, 4450–4463. [Google Scholar] [CrossRef] [PubMed]
- Oliveri, S.; Faccio, F.; Pizzoli, S.; Monzani, D.; Redaelli, C.; Indino, M.; Pravettoni, G. A pilot study on aesthetic treatments performed by qualified aesthetic practitioners: Efficacy on health-related quality of life in breast cancer patients. Qual. Life Res. 2019, 28, 1543–1553. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Liu, H.E. Effectiveness of cosmetic rehabilitation on the body image of oral cancer patients in Taiwan. Support. Care Cancer 2008, 16, 981–986. [Google Scholar] [CrossRef]
- Zwakman, M.; Tan, A.; Boersma, C.; Klinkenbijl, J.H.G.; Noorda, E.M.; de Jong, T.R.; Francken, A.B. Long-term quality of life and aesthetic outcomes after breast conserving surgery in patients with breast cancer. Eur. J. Surg. Oncol. 2022, 48, 1692–1698. [Google Scholar] [CrossRef]
- Kotzampasakis, D.; Piniara, A.; Themelis, S.; Kotzampasakis, S.; Gabriel, E.; Maroudias, N.; Nikolopoulos, T. Quality of life of patients who underwent aesthetic rhinoplasty: 100 cases assessed with the Glascow Benefit Inventory. Laryngoscope 2017, 127, 2017–2025. [Google Scholar] [CrossRef]
- Sarroca, N.; Valero, J.; Deus, J.; Casanova, J.; Luesma, M.J.; Lahoz, M. Quality of life, body image and self-esteem in patients with unilateral transtibial amputations. Sci. Rep. 2021, 11, 12559. [Google Scholar] [CrossRef]
- Leow, M.E.L.; Le, L.A.T.; Chan, Y.H.; Chong, A.K.S. Clinical intervention of a tighter-than-tolerated fit of aesthetic hand and finger prosthesis via controlled silicone swelling: A novel, speedier and versatile alternative method. Medicine 2022, 101, e30885. [Google Scholar] [CrossRef]
- Moss, H.; O’Neill, D. Aesthetic deprivation in clinical settings. Lancet 2014, 383, 1032–1033. [Google Scholar] [CrossRef]
- Beck, M.; Engelke, E.; Birkelund, R.; Martinsen, B. Aesthetics sets patients ‘free’ to recover during hospitalization with a neurological disease. A qualitative study. Int. J. Qual. Stud. Heal. Well-being 2021, 16, 1992843. [Google Scholar] [CrossRef]
- Silva, J.G.M.; Filoni, E.; Fitz, F.F. Physical therapy in the treatment of body aesthetics dysfunctions—Literature review. Man. Ther. Posturology Rehabil. J. 2014, 12, 194. [Google Scholar] [CrossRef]
- Borges, F.d.S.; Meyer, P.F.; Jahara, R.S.; de Morais Carreiro, E.; Antonuzzo, P.A.; Picariello, F.; Di Palma, C. Fundamentals of the use of ozone therapy in the treatment of aesthetic disorders: A review. J. Biosci. Med. 2021, 09, 40–70. [Google Scholar] [CrossRef]
- Lambrou, C.; Veale, D.; Wilson, G. The role of aesthetic sensitivity in body dysmorphic disorder. J. Abnorm. Psychol. 2011, 120, 443–453. [Google Scholar] [CrossRef]
- Van Borsel, J.; De Vos, M.C.; Bastiaansen, K.; Welvaert, J.; Lambert, J. The effectiveness of facial exercises for facial rejuvenation: A systematic review. Aesthetic Surg. J. 2014, 34, 22–27. [Google Scholar] [CrossRef]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 2019, 26, 5. [Google Scholar] [CrossRef] [PubMed]
- Losco, L.; Bolletta, A.; de Sire, A.; Chen, S.H.; Sert, G.; Aksoyler, D.; Velazquez-Mujica, J.; Invernizzi, M.; Cigna, E.; Chen, H.C. The Combination of Lymph Node Transfer and Excisional Procedures in Bilateral Lower Extremity Lymphedema: Clinical Outcomes and Quality of Life Assessment with Long-Term Follow-Up. J. Clin. Med. 2022, 11, 570. [Google Scholar] [CrossRef] [PubMed]
- Losco, L.; Bolletta, A.; Pierazzi, D.M.; Spadoni, D.; Cuomo, R.; Marcasciano, M.; Cavalieri, E.; Roxo, A.C.; Ciamarra, P.; Cantisani, C.; et al. Reconstruction of the Nose: Management of Nasal Cutaneous Defects According to Aesthetic Subunit and Defect Size. A Review. Medicina 2020, 56, 639. [Google Scholar] [CrossRef] [PubMed]
- Ciudad, P.; Kaciulyte, J.; Torto, F.L.; Vargas, M.I.; Bustamante, A.; Chen, H.C.; Maruccia, M.; Zulueta, J.; Trignano, E.; Bolletta, A. The profunda artery perforator free flap for lower extremity reconstruction. Microsurgery 2022, 42, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Ciudad, P.; Chen, H.C.; Bustos, S.S.; Manrique, O.J.; Bolletta, A.; Forte, A.J.; Huayllani, M.T.; Agko, M.; Urbina, J.A.; Date, S.; et al. The deep inferior epigastric lymphatic cable flap connected to gastroepiploic lymph node flap for treatment of refractory chylous ascites: Report of two cases. Microsurgery 2021, 41, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Edsander-Nord, A.; Brandberg, Y.; Wickman, M. Quality of life, patients’ satisfaction, and aesthetic outcome after pedicled or free TRAM flap breast surgery. Plast. Reconstr. Surg. 2001, 107, 1142–1153; discussion 1154–1155. [Google Scholar] [CrossRef] [PubMed]
- Mori, H.; Umeda, T.; Osanai, T.; Hata, Y. Esthetic evaluation of immediate breast reconstruction after nipple-sparing or skin-sparing mastectomy. Breast Cancer 2005, 12, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Bracaglia, R.; D’Ettorre, M.; Gniuli, D.; Gigliofiorito, P.; Gentileschi, S.; Mingrone, G. Morbidly obese patients undergoing bariatric and body contouring surgery: Psychological evaluation after treatments. J. Plast. Reconstr. Aesthetic Surg. 2011, 64, 1246–1248. [Google Scholar] [CrossRef]
- Losco, L.; Aksoyler, D.; Chen, S.-H.; Bolletta, A.; Velazquez-Mujica, J.; Di Taranto, G.; Lo Torto, F.; Marcasciano, M.; Cigna, E.; Chen, H.-C. Pharyngoesophageal reconstruction with free jejunum or radial forearm flap as diversionary conduit: Functional outcomes of patients with persistent dysphagia and aspiration. Microsurgery 2020, 40, 630–638. [Google Scholar] [CrossRef]
- Pravettoni, G.; Yoder, W.R.; Riva, S.; Mazzocco, K.; Arnaboldi, P.; Galimberti, V. Eliminating “ductal carcinoma in situ” and “lobular carcinoma in situ” (DCIS and LCIS) terminology in clinical breast practice: The cognitive psychology point of view. Breast 2016, 25, 82–85. [Google Scholar] [CrossRef]
- Kuhlefelt, C.; Repo, J.P.; Jahkola, T.; Kauhanen, S.; Homsy, P. Immediate versus delayed breast reconstruction: Long-term follow-up on health-related quality of life and satisfaction with breasts. J. Plast. Reconstr. Aesthetic Surg. 2024, 88, 478–486. [Google Scholar] [CrossRef]
- Losco, L.; Cigna, E. Aesthetic Refinements in C-V Flap: Raising a Perfect Cylinder. Aesthetic Surg. J. 2018, 38, Np26–Np28. [Google Scholar] [CrossRef]
- Eskenazi, L.B. New options for immediate reconstruction: Achieving optimal results with adjustable implants in a single stage. Plast. Reconstr. Surg. 2007, 119, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Caputo, G.G.; Marchetti, A.; Dalla Pozza, E.; Vigato, E.; Domenici, L.; Cigna, E.; Governa, M. Skin-Reduction Breast Reconstructions with Prepectoral Implant. Plast. Reconstr. Surg. 2016, 137, 1702–1705. [Google Scholar] [CrossRef]
- Domenici, L.; Caputo, G.G.; Losco, L.; Di Taranto, G.; Lo Torto, F.; Pierazzi, D.M.; Governa, M.; Benedetti Panici, P.; Ribuffo, D.; Cigna, E. Muscle-Sparing Skin-Reducing Breast Reconstruction with Pre-Pectoral Implants in Breast Cancer Patients: Long-Term Assessment of Patients’ Satisfaction and Quality of Life. J. Investig. Surg. 2022, 35, 841–847. [Google Scholar] [CrossRef]
- Poodt, I.G.; van Dijk, M.M.; Klein, S.; Hoogbergen, M.M. Complications of Lower Body Lift Surgery in Postbariatric Patients. Plast. Reconstr. Surg. Glob. Open 2016, 4, e1030. [Google Scholar] [CrossRef]
- Nemerofsky, R.B.; Oliak, D.A.; Capella, J.F. Body lift: An account of 200 consecutive cases in the massive weight loss patient. Plast. Reconstr. Surg. 2006, 117, 414–430. [Google Scholar] [CrossRef]
- Kitzinger, H.B.; Cakl, T.; Wenger, R.; Hacker, S.; Aszmann, O.C.; Karle, B. Prospective study on complications following a lower body lift after massive weight loss. J. Plast. Reconstr. Aesthetic Surg. 2013, 66, 231–238. [Google Scholar] [CrossRef]
- Bertheuil, N.; Chaput, B.; De Runz, A.; Girard, P.; Carloni, R.; Watier, E. The Lipo-Body Lift: A New Circumferential Body-Contouring Technique Useful after Bariatric Surgery. Plast. Reconstr. Surg. 2017, 139, 38e–49e. [Google Scholar] [CrossRef] [PubMed]
- Losco, L.; Roxo, A.C.; Roxo, C.W.; de Sire, A.; Bolletta, A.; Cuomo, R.; Grimaldi, L.; Cigna, E.; Roxo, C.D.P. Helix Thigh Lift. A Novel Approach to Severe Deformities in Massive Weight Loss Patients. J. Investig. Surg. 2022, 35, 620–626. [Google Scholar] [CrossRef] [PubMed]
- Koller, M.; Schubhart, S.; Hintringer, T. Quality of life and body image after circumferential body lifting of the lower trunk: A prospective clinical trial. Obes. Surg. 2013, 23, 561–566. [Google Scholar] [CrossRef]
- Klassen, A.F.; Cano, S.J.; Scott, A.; Johnson, J.; Pusic, A.L. Satisfaction and quality-of-life issues in body contouring surgery patients: A qualitative study. Obes. Surg. 2012, 22, 1527–1534. [Google Scholar] [CrossRef]
- Roh, D.S.; Panayi, A.C.; Bhasin, S.; Orgill, D.P.; Sinha, I. Implications of Aging in Plastic Surgery. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2085. [Google Scholar] [CrossRef] [PubMed]
- Lo Torto, F.; Redi, U.; Cigna, E.; Losco, L.; Marcasciano, M.; Casella, D.; Ciudad, P.; Ribuffo, D. Nasal Reconstruction With Two Stages Versus Three Stages Forehead Fap: What is Better for Patients With High Vascular Risk? J. Craniofacial Surg. 2020, 31, e57–e60. [Google Scholar] [CrossRef] [PubMed]
- Gohritz, A.; Osinga, R.; Haumer, A.; Schaefer, D.J. Microsurgical Reconstruction of the Lower Extremity in the Elderly. Clin. Plast. Surg. 2021, 48, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Reiter, M.; Baumeister, P.; Jacobi, C. Head and neck reconstruction in the elderly patient: A safe procedure? Eur. Arch. Oto-Rhino-Laryngology 2017, 274, 3169–3174. [Google Scholar] [CrossRef] [PubMed]
- Lo Torto, F.; Losco, L.; Bernardini, N.; Greco, M.; Scuderi, G.; Ribuffo, D. Surgical Treatment with Locoregional Flaps for the Eyelid: A Review. BioMed Res. Int. 2017, 2017, 6742537. [Google Scholar] [CrossRef]
- Paolino, G.; Cardone, M.; Didona, D.; Moliterni, E.; Losco, L.; Corsetti, P.; Schipani, G.; Lopez, T.; Calvieri, S.; Bottoni, U. Prognostic factors in head and neck melanoma according to facial aesthetic units. G. Ital. Di Dermatol. E Venereol. Organo Uff. Soc. Ital. Di Dermatol. E Sifilogr. 2020, 155, 41–45. [Google Scholar] [CrossRef]
- Cigna, E.; Pierazzi, D.M.; Sereni, S.; Marcasciano, M.; Losco, L.; Bolletta, A. Lymphatico-venous anastomosis in chronic ulcer with venous insufficiency: A case report. Microsurgery 2021, 41, 574–578. [Google Scholar] [CrossRef]
- Dressler, D.; Benecke, R. Pharmacology of therapeutic botulinum toxin preparations. Disabil. Rehabil. 2007, 29, 1761–1768. [Google Scholar] [CrossRef]
- Baricich, A.; Picelli, A.; Santamato, A.; Carda, S.; de Sire, A.; Smania, N.; Cisari, C.; Invernizzi, M. Safety Profile of High-Dose Botulinum Toxin Type A in Post-Stroke Spasticity Treatment. Clin. Drug Investig. 2018, 38, 991–1000. [Google Scholar] [CrossRef]
- Ascher, B.; Rzany, B.J.; Kestemont, P.; Redaelli, A.; Hendrickx, B.; Iozzo, I.; Martschin, C.; Milotich, A.; Molina, B.; Cartier, H.; et al. International Consensus Recommendations on the Aesthetic Usage of Ready-to-Use AbobotulinumtoxinA (Alluzience). Aesthetic Surg. J. 2024, 44, 192–202. [Google Scholar] [CrossRef]
- Kassir, M.; Babaei, M.; Hasanzadeh, S.; Rezaei Tavirani, M.; Razzaghi, Z.; Robati, R.M. Botulinium toxin applications in the lower face and neck: A comprehensive review. J. Cosmet. Dermatol. 2023, 23, 1205–1216. [Google Scholar] [CrossRef]
- Gadhia, K.; Walmsley, D. The therapeutic use of botulinum toxin in cervical and maxillofacial conditions. Evidence-Based Dent. 2009, 10, 53. [Google Scholar] [CrossRef][Green Version]
- Delcanho, R.; Val, M.; Guarda Nardini, L.; Manfredini, D. Botulinum Toxin for Treating Temporomandibular Disorders: What is the Evidence? J. Oral Facial Pain Headache 2022, 36, 6–20. [Google Scholar] [CrossRef]
- Ferrillo, M.; Ammendolia, A.; Paduano, S.; Calafiore, D.; Marotta, N.; Migliario, M.; Fortunato, L.; Giudice, A.; Michelotti, A.; de Sire, A. Efficacy of rehabilitation on reducing pain in muscle-related temporomandibular disorders: A systematic review and meta-analysis of randomized controlled trials. J. Back Musculoskelet. Rehabil. 2022, 35, 921–936. [Google Scholar] [CrossRef]
- Sipilä, K.; Ylöstalo, P.V.; Joukamaa, M.; Knuuttila, M.L. Comorbidity between facial pain, widespread pain, and depressive symptoms in young adults. J. Orofac. Pain 2006, 20, 24–30. [Google Scholar]
- Ernberg, M.; Hedenberg-Magnusson, B.; List, T.; Svensson, P. Efficacy of botulinum toxin type A for treatment of persistent myofascial TMD pain: A randomized, controlled, double-blind multicenter study. Pain 2011, 152, 1988–1996. [Google Scholar] [CrossRef]
- Guarda-Nardini, L.; Stecco, A.; Stecco, C.; Masiero, S.; Manfredini, D. Myofascial pain of the jaw muscles: Comparison of short-term effectiveness of botulinum toxin injections and fascial manipulation technique. Cranio 2012, 30, 95–102. [Google Scholar] [CrossRef]
- Kütük, S.G.; Özkan, Y.; Kütük, M.; Özdaş, T. Comparison of the Efficacies of Dry Needling and Botox Methods in the Treatment of Myofascial Pain Syndrome Affecting the Temporomandibular Joint. J. Craniofacial Surg. 2019, 30, 1556–1559. [Google Scholar] [CrossRef]
- De la Torre Canales, G.; Alvarez-Pinzon, N.; Muñoz-Lora, V.R.M.; Vieira Peroni, L.; Farias Gomes, A.; Sánchez-Ayala, A.; Haiter-Neto, F.; Manfredini, D.; Rizzatti-Barbosa, C.M. Efficacy and Safety of Botulinum Toxin Type A on Persistent Myofascial Pain: A Randomized Clinical Trial. Toxins 2020, 12, 395. [Google Scholar] [CrossRef]
- De Carli, B.M.; Magro, A.K.; Souza-Silva, B.N.; Matos Fde, S.; De Carli, J.P.; Paranhos, L.R.; Magro, E.D. The effect of laser and botulinum toxin in the treatment of myofascial pain and mouth opening: A randomized clinical trial. J. Photochem. Photobiol. B Biol. 2016, 159, 120–123. [Google Scholar] [CrossRef]
- Tan, E.K.; Jankovic, J. Botulinum toxin A in patients with oromandibular dystonia: Long-term follow-up. Neurology 1999, 53, 2102–2107. [Google Scholar] [CrossRef]
- Sinclair, C.F.; Gurey, L.E.; Blitzer, A. Oromandibular dystonia: Long-term management with botulinum toxin. Laryngoscope 2013, 123, 3078–3083. [Google Scholar] [CrossRef]
- Yoshida, K. Botulinum Toxin Therapy for Oromandibular Dystonia and Other Movement Disorders in the Stomatognathic System. Toxins 2022, 14, 282. [Google Scholar] [CrossRef]
- Jost, W.H.; Kohl, A. Botulinum toxin: Evidence-based medicine criteria in blepharospasm and hemifacial spasm. J. Neurol. 2001, 248 (Suppl. S1), I21–I24. [Google Scholar] [CrossRef]
- Hassell, T.J.W.; Charles, D. Treatment of Blepharospasm and Oromandibular Dystonia with Botulinum Toxins. Toxins 2020, 12, 269. [Google Scholar] [CrossRef]
- Bhidayasiri, R.; Cardoso, F.; Truong, D.D. Botulinum toxin in blepharospasm and oromandibular dystonia: Comparing different botulinum toxin preparations. Eur. J. Neurol. 2006, 13 (Suppl. S1), 21–29. [Google Scholar] [CrossRef]
- Balanta-Melo, J.; Toro-Ibacache, V.; Torres-Quintana, M.A.; Kupczik, K.; Vega, C.; Morales, C.; Hernández-Moya, N.; Arias-Calderón, M.; Beato, C.; Buvinic, S. Early molecular response and microanatomical changes in the masseter muscle and mandibular head after botulinum toxin intervention in adult mice. Ann. Anat. 2018, 216, 112–119. [Google Scholar] [CrossRef]
- Rafferty, K.L.; Liu, Z.J.; Ye, W.; Navarrete, A.L.; Nguyen, T.T.; Salamati, A.; Herring, S.W. Botulinum toxin in masticatory muscles: Short- and long-term effects on muscle, bone, and craniofacial function in adult rabbits. Bone 2012, 50, 651–662. [Google Scholar] [CrossRef]
- Ferrillo, M.; Giudice, A.; Marotta, N.; Fortunato, F.; Di Venere, D.; Ammendolia, A.; Fiore, P.; de Sire, A. Pain Management and Rehabilitation for Central Sensitization in Temporomandibular Disorders: A Comprehensive Review. Int. J. Mol. Sci. 2022, 23, 12164. [Google Scholar] [CrossRef]
- Bennardo, F.; Bennardo, L.; Del Duca, E.; Patruno, C.; Fortunato, L.; Giudice, A.; Nisticò, S.P. Autologous platelet-rich fibrin injections in the management of facial cutaneous sinus tracts secondary to medication-related osteonecrosis of the jaw. Dermatol. Ther. 2020, 33, e13334. [Google Scholar] [CrossRef]
- Bennardo, F.; Gallelli, L.; Palleria, C.; Colosimo, M.; Fortunato, L.; De Sarro, G.; Giudice, A. Can platelet-rich fibrin act as a natural carrier for antibiotics delivery? A proof-of-concept study for oral surgical procedures. BMC Oral Health 2023, 23, 134. [Google Scholar] [CrossRef]
- de Sire, A.; Lippi, L.; Mezian, K.; Calafiore, D.; Pellegrino, R.; Mascaro, G.; Cisari, C.; Invernizzi, M. Ultrasound-guided platelet-rich-plasma injections for reducing sacroiliac joint pain: A paradigmatic case report and literature review. J. Back Musculoskelet. Rehabil. 2022, 35, 977–982. [Google Scholar] [CrossRef]
- Cognasse, F.; Hamzeh-Cognasse, H.; Mismetti, P.; Thomas, T.; Eglin, D.; Marotte, H. The Non-Haemostatic Response of Platelets to Stress: An Actor of the Inflammatory Environment on Regenerative Medicine? Front. Immunol. 2021, 12, 741988. [Google Scholar] [CrossRef]
- Tey, R.V.; Haldankar, P.; Joshi, V.R.; Raj, R.; Maradi, R. Variability in Platelet-Rich Plasma Preparations Used in Regenerative Medicine: A Comparative Analysis. Stem Cells Int. 2022, 2022, 3852898. [Google Scholar] [CrossRef]
- Familiari, F.; Ammendolia, A.; Rupp, M.C.; Russo, R.; Pujia, A.; Montalcini, T.; Marotta, N.; Mercurio, M.; Galasso, O.; Millett, P.J.; et al. Efficacy of intra-articular injections of hyaluronic acid in patients with glenohumeral joint osteoarthritis: A systematic review and meta-analysis. J. Orthop. Res. 2023, 41, 2345–2358. [Google Scholar] [CrossRef]
- Kawase, T.; Mubarak, S.; Mourão, C.F. The Platelet Concentrates Therapy: From the Biased Past to the Anticipated Future. Bioengineering 2020, 7, 82. [Google Scholar] [CrossRef]
- Manole, C.G.; Soare, C.; Ceafalan, L.C.; Voiculescu, V.M. Platelet-Rich Plasma in Dermatology: New Insights on the Cellular Mechanism of Skin Repair and Regeneration. Life 2023, 14, 40. [Google Scholar] [CrossRef]
- Jain, N.K.; Gulati, M. Platelet-rich plasma: A healing virtuoso. Blood Res. 2016, 51, 3–5. [Google Scholar] [CrossRef]
- Sclafani, A.P.; Saman, M. Platelet-rich fibrin matrix for facial plastic surgery. Facial Plast. Surg. Clin. North Am. 2012, 20, 177–186, vi. [Google Scholar] [CrossRef]
- Sclafani, A.P. Safety, efficacy, and utility of platelet-rich fibrin matrix in facial plastic surgery. Arch. Facial Plast. Surg. 2011, 13, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.; Bassiri-Tehrani, M.; Abraham, M.T. The Effect of Platelet-Rich Fibrin Matrix on Skin Rejuvenation: A Split-Face Comparison. Aesthetic Surg. J. 2021, 41, 747–758. [Google Scholar] [CrossRef]
- Shin, M.K.; Lee, J.H.; Lee, S.J.; Kim, N.I. Platelet-rich plasma combined with fractional laser therapy for skin rejuvenation. Dermatol. Surg. 2012, 38, 623–630. [Google Scholar] [CrossRef]
- Singhal, P.; Agarwal, S.; Dhot, P.S.; Sayal, S.K. Efficacy of platelet-rich plasma in treatment of androgenic alopecia. Asian J. Transfus. Sci. 2015, 9, 159–162. [Google Scholar] [CrossRef]
- Khatu, S.S.; More, Y.E.; Gokhale, N.R.; Chavhan, D.C.; Bendsure, N. Platelet-rich plasma in androgenic alopecia: Myth or an effective tool. J. Cutan. Aesthetic Surg. 2014, 7, 107–110. [Google Scholar] [CrossRef]
- Garg, S. Outcome of Intra-operative Injected Platelet-rich Plasma Therapy During Follicular Unit Extraction Hair Transplant: A Prospective Randomised Study in Forty Patients. J. Cutan. Aesthetic Surg. 2016, 9, 157–164. [Google Scholar] [CrossRef]
- Balasundaram, M.; Kumari, R.; Ramassamy, S. Efficacy of autologous platelet-rich plasma therapy versus topical Minoxidil in men with moderate androgenetic alopecia: A randomized open-label trial. J. Dermatol. Treat. 2023, 34, 2182618. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Zhang, Y.; Long, B.; Zhang, Y.; Zhang, C.; Zhang, S. Injections of platelet-rich plasma prepared by automatic blood cell separator combined with topical 5% minoxidil in the treatment of male androgenetic alopecia. Ski. Res. Technol. 2023, 29, e13315. [Google Scholar] [CrossRef]
- Popescu, M.N.; Iliescu, M.G.; Beiu, C.; Popa, L.G.; Mihai, M.M.; Berteanu, M.; Ionescu, A.M. Autologous Platelet-Rich Plasma Efficacy in the Field of Regenerative Medicine: Product and Quality Control. BioMed Res. Int. 2021, 2021, 4672959. [Google Scholar] [CrossRef]
- Fraser, J.R.; Laurent, T.C.; Laurent, U.B. Hyaluronan: Its nature, distribution, functions and turnover. J. Intern. Med. 1997, 242, 27–33. [Google Scholar] [CrossRef]
- Lippi, L.; Ferrillo, M.; Turco, A.; Folli, A.; Moalli, S.; Refati, F.; Perrero, L.; Ammendolia, A.; de Sire, A.; Invernizzi, M. Multidisciplinary Rehabilitation after Hyaluronic Acid Injections for Elderly with Knee, Hip, Shoulder, and Temporomandibular Joint Osteoarthritis. Medicina 2023, 59, 2047. [Google Scholar] [CrossRef]
- Agostini, F.; Ferrillo, M.; Bernetti, A.; Finamore, N.; Mangone, M.; Giudice, A.; Paoloni, M.; de Sire, A. Hyaluronic acid injections for pain relief and functional improvement in patients with temporomandibular disorders: An umbrella review of systematic reviews. J. Oral Rehabil. 2023, 50, 1518–1534. [Google Scholar] [CrossRef]
- Castro-Calderón, A.; Roccuzzo, A.; Ferrillo, M.; Gada, S.; González-Serrano, J.; Fonseca, M.; Molinero-Mourelle, P. Hyaluronic acid injection to restore the lost interproximal papilla: A systematic review. Acta Odontol. Scand. 2022, 80, 295–307. [Google Scholar] [CrossRef]
- Bukhari, S.N.A.; Roswandi, N.L.; Waqas, M.; Habib, H.; Hussain, F.; Khan, S.; Sohail, M.; Ramli, N.A.; Thu, H.E.; Hussain, Z. Hyaluronic acid, a promising skin rejuvenating biomedicine: A review of recent updates and pre-clinical and clinical investigations on cosmetic and nutricosmetic effects. Int. J. Biol. Macromol. 2018, 120, 1682–1695. [Google Scholar] [CrossRef]
- de Maio, M. MD CodesTM: A Methodological Approach to Facial Aesthetic Treatment with Injectable Hyaluronic Acid Fillers. Aesthetic Plast. Surg. 2021, 45, 690–709. [Google Scholar] [CrossRef]
- Al-Khafaji, M.Q.M.; Althobaiti, N.S.A.; Alhassani, N.F.M.; Alnahwi, Z.A.H.; Aldawsari, W.A.; Alquraini, S.K.; Abdrabalameer, A.H.; Alharamlah, F.S.S.; Almalki, A.S.; Alotaibi, N.A.; et al. The Application and Efficacy of Hyaluronic Acid Fillers for Chin Enhancement and Retrusion Correction: A Systematic Review of Patient-Reported Outcomes. Cureus 2023, 15, e48807. [Google Scholar] [CrossRef]
- Kerscher, M.; Agsten, K.; Kravtsov, M.; Prager, W. Effectiveness evaluation of two volumizing hyaluronic acid dermal fillers in a controlled, randomized, double-blind, split-face clinical study. Clin. Cosmet. Investig. Dermatol. 2017, 10, 239–247. [Google Scholar] [CrossRef]
- Wiest, L.; Kerscher, M. Native hyaluronsäure in der ästhetischen medizin—Ergebnisse einer expertenkonferenz. JDDG J. Ger. Soc. Dermatol. 2008, 6, 176–180. [Google Scholar] [CrossRef]
- Paliwal, S.; Fagien, S.; Sun, X.; Holt, T.; Kim, T.; Hee, C.K.; Van Epps, D.; Messina, D.J. Skin extracellular matrix stimulation following injection of a hyaluronic acid-based dermal filler in a rat model. Plast. Reconstr. Surg. 2014, 134, 1224–1233. [Google Scholar] [CrossRef]
- Aubry, S.; Collart-Dutilleul, P.-Y.; Renaud, M.; Batifol, D.; Montal, S.; Pourreyron, L.; Carayon, D. Benefit of hyaluronic acid to treat facial aging in completely edentulous patients. J. Clin. Med. 2022, 11, 5874. [Google Scholar] [CrossRef]
- de Sire, A.; Baricich, A.; Ferrillo, M.; Migliario, M.; Cisari, C.; Invernizzi, M. Buccal hemineglect: Is it useful to evaluate the differences between the two halves of the oral cavity for the multidisciplinary rehabilitative management of right brain stroke survivors? A cross-sectional study. Top. Stroke Rehabil. 2020, 27, 208–214. [Google Scholar] [CrossRef]
- de Sire, A.; Invernizzi, M.; Ferrillo, M.; Gimigliano, F.; Baricich, A.; Cisari, C.; De Marchi, F.; Foglio Bonda, P.L.; Mazzini, L.; Migliario, M. Functional status and oral health in patients with amyotrophic lateral sclerosis: A cross-sectional study. NeuroRehabilitation 2021, 48, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Szczerkowska-Dobosz, A.; Olszewska, B.; Lemańska, M.; Purzycka-Bohdan, D.; Nowicki, R. Acquired facial lipoatrophy: Pathogenesis and therapeutic options. Postepy Dermatol. Alergol. 2015, 32, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Panettiere, P.; Marchetti, L.; Accorsi, D. Filler injection enhances the projection of the reconstructed nipple:An original easy technique. Aesthetic Plast. Surg. 2005, 29, 287–294. [Google Scholar] [CrossRef]
- Philipp-Dormston, W.G.; Eccleston, D.; De Boulle, K.; Hilton, S.; van den Elzen, H.; Nathan, M. A prospective, observational study of the volumizing effect of open-label aesthetic use of Juvéderm® VOLUMA® with Lidocaine in mid-face area. J. Cosmet. Laser Ther. 2014, 16, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Zeng, J.; Lu, J. Mechanisms of action involved in ozone-therapy in skin diseases. Int. Immunopharmacol. 2018, 56, 235–241. [Google Scholar] [CrossRef]
- Al-Saadi, H.; Potapova, I.; Rochford, E.T.; Moriarty, T.F.; Messmer, P. Ozonated saline shows activity against planktonic and biofilm growing Staphylococcus aureus in vitro: A potential irrigant for infected wounds. Int. Wound J. 2016, 13, 936–942. [Google Scholar] [CrossRef]
- Azarpazhooh, A.; Limeback, H. The application of ozone in dentistry: A systematic review of literature. J. Dent. 2008, 36, 104–116. [Google Scholar] [CrossRef]
- Martínez-Sánchez, G.; Al-Dalain, S.M.; Menéndez, S.; Re, L.; Giuliani, A.; Candelario-Jalil, E.; Alvarez, H.; Fernández-Montequín, J.I.; León, O.S. Therapeutic efficacy of ozone in patients with diabetic foot. Eur. J. Pharmacol. 2005, 523, 151–161. [Google Scholar] [CrossRef]
- Silva, R.A.; Garotti, J.E.; Silva, R.S.; Navarini, A.; Pacheco, A.M., Jr. Analysis of the bactericidal effect of ozone pneumoperitoneum. Acta Cir. Bras. 2009, 24, 124–127. [Google Scholar] [CrossRef]
- Lacerda, A.C.; Grillo, R.; de Barros, T.E.P.; Martins, C.B.; de Carvalho Luposeli, F. Efficacy of biostimulatory ozone therapy: Case report and literature review. J. Cosmet. Dermatol. 2022, 21, 130–133. [Google Scholar] [CrossRef]
- Jernberger, A. The neuropathic foot. Prosthet. Orthot. Int. 1993, 17, 189–195. [Google Scholar] [CrossRef][Green Version]
- Pianez, L.R.; Custódio, F.S.; Guidi, R.M.; de Freitas, J.N.; Sant’Ana, E. Effectiveness of carboxytherapy in the treatment of cellulite in healthy women: A pilot study. Clin. Cosmet. Investig. Dermatol. 2016, 9, 183–190. [Google Scholar] [CrossRef]
- Kroumpouzos, G.; Arora, G.; Kassir, M.; Galadari, H.; Wollina, U.; Lotti, T.; Grabbe, S.; Goldust, M. Carboxytherapy in dermatology. Clin. Dermatol. 2022, 40, 305–309. [Google Scholar] [CrossRef]
- Aksenenko, I.; Gerasimenko, M.; Aksenenko, A. Combined application of monopolar radiofrequency technology and injective carboxytherapy in the correction of involutive skin changes. J. Clin. Aesthet. Dermatol. 2022, 15, 44–47. [Google Scholar]
- Modena, D.A.O.; Soares, C.D.; Candido, E.C.; Chaim, F.D.M.; Cazzo, E.; Chaim, E.A. Effect of extracorporeal shock waves on inflammation and angiogenesis of integumentary tissue in obese individuals: Stimulating repair and regeneration. Lasers Med Sci. 2022, 37, 1289–1297. [Google Scholar] [CrossRef]
- Simplicio, C.L.; Purita, J.; Murrell, W.; Santos, G.S.; Dos Santos, R.G.; Lana, J. Extracorporeal shock wave therapy mechanisms in musculoskeletal regenerative medicine. J. Clin. Orthop. Trauma 2020, 11, S309–S318. [Google Scholar] [CrossRef]
- Kraemer, R.; Sorg, H.; Forstmeier, V.; Knobloch, K.; Liodaki, E.; Stang, F.H.; Mailaender, P.; Kisch, T. Immediate Dose-Response Effect of High-Energy Versus Low-Energy Extracorporeal Shock Wave Therapy on Cutaneous Microcirculation. Ultrasound Med. Biol. 2016, 42, 2975–2982. [Google Scholar] [CrossRef]
- Kisch, T.; Sorg, H.; Forstmeier, V.; Knobloch, K.; Liodaki, E.; Stang, F.; Mailänder, P.; Krämer, R. Remote effects of extracorporeal shock wave therapy on cutaneous microcirculation. J. Tissue Viability 2015, 24, 140–145. [Google Scholar] [CrossRef]
- Scarano, A.; Petrini, M.; Sbarbati, A.; Amore, R.; Iorio, E.L.; Marchetti, M.; Amuso, D. Pilot study of histology aspect of cellulite in seventy patients who differ in BMI and cellulite grading. J. Cosmet. Dermatol. 2021, 20, 4024–4031. [Google Scholar] [CrossRef]
- Knobloch, K.; Kraemer, R. Extracorporeal shock wave therapy (ESWT) for the treatment of cellulite--A current metaanalysis. Int. J. Surg. 2015, 24, 210–217. [Google Scholar] [CrossRef]
- Modena, D.A.O.; da Silva, C.N.; Grecco, C.; Guidi, R.M.; Moreira, R.G.; Coelho, A.A.; Sant’Ana, E.; de Souza, J.R. Extracorporeal shockwave: Mechanisms of action and physiological aspects for cellulite, body shaping, and localized fat-Systematic review. J. Cosmet. Laser Ther. 2017, 19, 314–319. [Google Scholar] [CrossRef]
- Michon, A. A Prospective Study Determining Patient Satisfaction with Combined Cryolipolysis and Shockwave Therapy Treatment for Noninvasive Body Contouring. Aesthetic Plast. Surg. 2021, 45, 2317–2325. [Google Scholar] [CrossRef]
- Allam, N.M.; Elshorbagy, R.T.; Eid, M.M.; Abdelbasset, W.K.; Elkholi, S.M.; Eladl, H.M. Comparison of Extracorporeal Shock Wave Therapy versus Manual Lymphatic Drainage on Cellulite after Liposuction: A Randomized Clinical Trial. Evidence-Based Complement. Altern. Med. 2021, 2021, 9956879. [Google Scholar] [CrossRef]
- Priglinger, E.; Sandhofer, M.; Peterbauer, A.; Wurzer, C.; Steffenhagen, C.; Maier, J.; Holnthoner, W.; Nuernberger, S.; Redl, H.; Wolbank, S. Extracorporeal shock wave therapy in situ—Novel approach to obtain an activated fat graft. J. Tissue Eng. Regen. Med. 2018, 12, 416–426. [Google Scholar] [CrossRef]
- Sorg, H.; Zwetzich, I.; Tilkorn, D.J.; Kolbenschlag, J.; Hauser, J.; Goertz, O.; Spindler, N.; Langer, S.; Ring, A. Effects of Extracorporeal Shock Waves on Microcirculation and Angiogenesis in the in vivo Wound Model of the Diver Box. Eur. Surg. Res. 2021, 62, 134–143. [Google Scholar] [CrossRef]
- Fioramonti, P.; Onesti, M.G.; Fino, P.; Fallico, N.; Scuderi, N. Extracorporeal shock wave therapy for the treatment of venous ulcers in the lower limbs. Ann. Ital. Chir. 2012, 83, 41–44. [Google Scholar]
- Djedovic, G.; Kamelger, F.S.; Jeschke, J.; Piza-Katzer, H. Effect of extracorporeal shock wave treatment on deep partial-thickness burn injury in rats: A pilot study. Plast. Surg. Int. 2014, 2014, 495967. [Google Scholar] [CrossRef]
- Arnó, A.; García, O.; Hernán, I.; Sancho, J.; Acosta, A.; Barret, J.P. Extracorporeal shock waves, a new non-surgical method to treat severe burns. Burns 2010, 36, 844–849. [Google Scholar] [CrossRef]
- Keil, H.; Mueller, W.; Herold-Mende, C.; Gebhard, M.M.; Germann, G.; Engel, H.; Reichenberger, M.A. Preoperative shock wave treatment enhances ischemic tissue survival, blood flow and angiogenesis in a rat skin flap model. Int. J. Surg. 2011, 9, 292–296. [Google Scholar] [CrossRef]
- Reichenberger, M.A.; Heimer, S.; Schaefer, A.; Lass, U.; Gebhard, M.M.; Germann, G.; Engel, H.; Köllensperger, E.; Leimer, U.; Mueller, W. Extracorporeal shock wave treatment protects skin flaps against ischemia-reperfusion injury. Injury 2012, 43, 374–380. [Google Scholar] [CrossRef]
- Nacak, U.; Calis, M.; Atilla, P.; Cetin, A.; Aksu, A.E. Extracorporal Shock Wave Therapy as a Delay Procedure to Improve Viability of Zone 4: An Experimental Study in a Rat TRAM Flap Model. Ann. Plast. Surg. 2016, 77, e15–e20. [Google Scholar] [CrossRef]
- Chuangsuwanich, A.; Kongkunnavat, N.; Kamanamool, M.; Maipeng, G.; Kamanamool, N.; Tonaree, W. Extracorporeal Shock Wave Therapy for Hypertrophic Scars. Arch. Plast. Surg. 2022, 49, 554–560. [Google Scholar] [CrossRef]
- Ostezan, L.; Peck, J. Radial Sound (Shockwave) Therapy Resolves Delayed-onset Nodules Following Injection of Hyaluronic Acid Dermal Filler: A Case Study. J. Clin. Aesthetic Dermatol. 2021, 14, S15–S17. [Google Scholar]
- Fischer, S.; Mueller, W.; Schulte, M.; Kiefer, J.; Hirche, C.; Heimer, S.; Köllensperger, E.; Germann, G.; Reichenberger, M.A. Multiple extracorporeal shock wave therapy degrades capsular fibrosis after insertion of silicone implants. Ultrasound Med. Biol. 2015, 41, 781–789. [Google Scholar] [CrossRef]
- Heine, N.; Prantl, L.; Eisenmann-Klein, M. Extracorporeal shock wave treatment of capsular fibrosis after mammary augmentation—Preliminary results. J. Cosmet. Laser Ther. 2013, 15, 330–333. [Google Scholar] [CrossRef]
- Cotler, H.B.; Chow, R.T.; Hamblin, M.R.; Carroll, J. The Use of Low Level Laser Therapy (LLLT) For Musculoskeletal Pain. MOJ Orthop. Rheumatol. 2015, 2, 62–65. [Google Scholar] [CrossRef]
- de Sire, A.; Lippi, L.; Marotta, N.; Ferrillo, M.; Folli, A.; Turco, A.; Ammendolia, A.; Invernizzi, M. Myths and truths on biophysics-based approach in rehabilitation of musculoskeletal disorders. Ther. Adv. Musculoskelet. Dis. 2023, 15, 1759720x231183867. [Google Scholar] [CrossRef]
- Rola, P.; Doroszko, A.; Derkacz, A. The Use of Low-Level Energy Laser Radiation in Basic and Clinical Research. Adv. Clin. Exp. Med. 2014, 23, 835–842. [Google Scholar] [CrossRef]
- Yu, S.; Lan, C.E.; Yu, H.S. Mechanisms of repigmentation induced by photobiomodulation therapy in vitiligo. Exp. Dermatol. 2019, 28 (Suppl. S1), 10–14. [Google Scholar] [CrossRef]
- Kuffler, D.P. Photobiomodulation in promoting wound healing: A review. Regen. Med. 2016, 11, 107–122. [Google Scholar] [CrossRef]
- Arjmand, B.; Khodadost, M.; Jahani Sherafat, S.; Rezaei Tavirani, M.; Ahmadi, N.; Hamzeloo Moghadam, M.; Okhovatian, F.; Rezaei Tavirani, S.; Rostami-Nejad, M. Low-Level Laser Therapy: Potential and Complications. J. Lasers Med Sci. 2021, 12, e42. [Google Scholar] [CrossRef]
- Firouz, B.; Faihs, L.; Slezak, P.; Ghaffari Tabrizi-Wizsy, N.; Schicho, K.; Winter, R.; Kamolz, L.P.; Dungel, P. Testing the effects of photobiomodulation on angiogenesis in a newly established CAM burn wound model. Sci. Rep. 2023, 13, 22985. [Google Scholar] [CrossRef]
- Ribeiro, M.; Santos, K.C.; Macedo, M.R.; de Souza, G.A.; Neto, F.I.A.; Araujo, G.H.M.; Cavalcante, D.R.; Costa, F.F.; de Sá Ferreira, G.; Peixoto, L.A.; et al. Use of adipose derived stem cells accelerates the healing process in third-degree burns. Burns 2024, 50, 132–145. [Google Scholar] [CrossRef]
- Lee, S.H.; Kim, Y.J.; Kim, Y.H.; Kim, H.Y.; Bhang, S.H. Enhancing therapeutic efficacy of human adipose-derived stem cells by modulating photoreceptor expression for advanced wound healing. Stem Cell Res. Ther. 2022, 13, 215. [Google Scholar] [CrossRef]
- Abbasnezhad, F.; Zare, S.; Razzaghi, M.; Karjou, R.; Karjou, Z.; Alavi Rad, E.; Zadehmodarres, S. Effective Combination Therapy with Human Amniotic Membrane Mesenchymal Stem Cells and Low-Level Laser Therapy in Wound Healing in Animal Models. J. Lasers Med Sci. 2022, 13, e72. [Google Scholar] [CrossRef]
- Nair, H.K.R.; Chong, S.S.Y.; Selvaraj, D.D.J. Photobiomodulation as an Adjunct Therapy in Wound Healing. Int. J. Low. Extremity Wounds 2023, 22, 278–282. [Google Scholar] [CrossRef]
- Kazemikhoo, N.; Vaghardoost, R.; Dahmardehei, M.; Mokmeli, S.; Momeni, M.; Nilforoushzadeh, M.A.; Ansari, F.; Razagi, M.R.; Razagi, Z.; Amirkhani, M.A.; et al. Evaluation of the Effects of Low Level Laser Therapy on the Healing Process After Skin Graft Surgery in Burned Patients (A Randomized Clinical Trial). J. Lasers Med Sci. 2018, 9, 139–143. [Google Scholar] [CrossRef]
- Zhang, Y.; Su, J.; Ma, K.; Li, H.; Fu, X.; Zhang, C. Photobiomodulation promotes hair regeneration in injured skin by enhancing migration and exosome secretion of dermal papilla cells. Wound Repair Regen. 2022, 30, 245–257. [Google Scholar] [CrossRef]
- Wikramanayake, T.C.; Villasante, A.C.; Mauro, L.M.; Nouri, K.; Schachner, L.A.; Perez, C.I.; Jimenez, J.J. Low-level laser treatment accelerated hair regrowth in a rat model of chemotherapy-induced alopecia (CIA). Lasers Med Sci. 2013, 28, 701–706. [Google Scholar] [CrossRef]
- Mansouri, V.; Arjmand, B.; Rezaei Tavirani, M.; Razzaghi, M.; Rostami-Nejad, M.; Hamdieh, M. Evaluation of Efficacy of Low-Level Laser Therapy. J. Lasers Med Sci. 2020, 11, 369–380. [Google Scholar] [CrossRef]
- Liu, D.; Xu, Q.; Meng, X.; Liu, X.; Liu, J. Status of research on the development and regeneration of hair follicles. Int. J. Med Sci. 2024, 21, 80–94. [Google Scholar] [CrossRef]
- Mosca, R.C.; Ong, A.A.; Albasha, O.; Bass, K.; Arany, P. Photobiomodulation Therapy for Wound Care: A Potent, Noninvasive, Photoceutical Approach. Adv. Ski. Wound Care 2019, 32, 157–167. [Google Scholar] [CrossRef]
- Iijima, H.; Takahashi, M. Microcurrent Therapy as a Therapeutic Modality for Musculoskeletal Pain: A Systematic Review Accelerating the Translation From Clinical Trials to Patient Care. Arch. Rehabil. Res. Clin. Transl. 2021, 3, 100145. [Google Scholar] [CrossRef]
- Yoshikawa, Y.; Hiramatsu, T.; Sugimoto, M.; Uemura, M.; Mori, Y.; Ichibori, R. Efficacy of Low-frequency Monophasic Pulsed Microcurrent Stimulation Therapy in Undermining Pressure Injury: A Double-blind Crossover-controlled Study. Prog. Rehabil. Med. 2022, 7, 20220045. [Google Scholar] [CrossRef]
- Park, G.Y.; Kwon, D.R.; Moon, Y.S. Low-intensity microcurrent therapy promotes regeneration of atrophied calf muscles in immobilized rabbits. J. Biomed. Res. 2018, 33, 30–37. [Google Scholar] [CrossRef]
- Zickri, M.B. Possible local stem cells activation by microcurrent application in experimentally injured soleus muscle. Int. J. Stem Cells 2014, 7, 79–86. [Google Scholar] [CrossRef][Green Version]
- Kwon, D.R.; Kim, K.L.; Moon, Y.S. Regeneration of Chronic Rotator Cuff Tear in a Rabbit Model: Synergetic Benefits of Human Umbilical Cord Blood-Derived Mesenchymal Stem Cells, Polydeoxyribonucleotides, and Microcurrent Therapy. BioMed Res. Int. 2022, 2022, 6496773. [Google Scholar] [CrossRef]
- Kwon, D.R.; Moon, Y.S.; Kwon, D.Y. Combination Therapy of Polydeoxyribonucleotide and Microcurrent in Muscle Regeneration on Cast-Induced Muscle Atrophy in Rabbit. BioMed Res. Int. 2022, 2022, 7469452. [Google Scholar] [CrossRef]
- Lennox, A.J.; Shafer, J.P.; Hatcher, M.; Beil, J.; Funder, S.J. Pilot study of impedance-controlled microcurrent therapy for managing radiation-induced fibrosis in head-and-neck cancer patients. Int. J. Radiat. Oncol. Biol. Phys. 2002, 54, 23–34. [Google Scholar] [CrossRef]
- Vahdatpour, B.; Haghighat, S.; Sadri, L.; Taghian, M.; Sadri, S. Effects of Transfer Energy Capacitive and Resistive On Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Galen Med J. 2022, 11, e2407. [Google Scholar] [CrossRef]
- Rodríguez-Sanz, J.; López-de-Celis, C.; Hidalgo-García, C.; González-Rueda, V.; Ragazzi, P.; Bueno-Gracia, E.; Llurda-Almuzara, L.; Pérez-Bellmunt, A. Is Tecar Therapy Effective on Biceps Femoris and Quadriceps Rehabilitation? A Cadaveric Study. J. Sport Rehabil. 2022, 31, 756–763. [Google Scholar] [CrossRef]
- Clijsen, R.; Leoni, D.; Schneebeli, A.; Cescon, C.; Soldini, E.; Li, L.; Barbero, M. Does the Application of Tecar Therapy Affect Temperature and Perfusion of Skin and Muscle Microcirculation? A Pilot Feasibility Study on Healthy Subjects. J. Altern. Complement. Med. 2020, 26, 147–153. [Google Scholar] [CrossRef]
- Hernández-Bule, M.L.; Toledano-Macías, E.; Pérez-González, L.A.; Martínez-Pascual, M.A.; Fernández-Guarino, M. Anti-Fibrotic Effects of RF Electric Currents. Int. J. Mol. Sci. 2023, 24, 10986. [Google Scholar] [CrossRef]
- Vale, A.L.; Pereira, A.S.; Morais, A.; de Carvalho, P.; Vilarinho, R.; Mendonça, A.; Noites, A. Effect of four sessions of aerobic exercise with abdominal radiofrequency in adipose tissue in healthy women: Randomized control trial. J. Cosmet. Dermatol. 2020, 19, 359–367. [Google Scholar] [CrossRef]
- Alizadeh, Z.; Halabchi, F.; Bodaghabadi, Z.; Zarandi, M.M.; Abolhasani, M.; Seifi, V.; Khazaei, R.; Ghanadi, S.; Mazaheri, R.; Tabesh, M.R. Non-invasive Body Contouring Technologies: An Updated Narrative Review. Aesthetic Plast. Surg. 2023. [Google Scholar] [CrossRef]
- Cau, N.; Cimolin, V.; Aspesi, V.; Galli, M.; Postiglione, F.; Todisco, A.; Tacchini, E.; Darno, D.; Capodaglio, P. Preliminary evidence of effectiveness of TECAR in lymphedema. Lymphology 2019, 52, 35–43. [Google Scholar] [CrossRef]
- Mihailescu, L.; Carmen, E.; Mihailescu, N.; Mihailescu, L. The Improvement of the Adult’s life Quality by the Body Autoplasty Effects of the Physical Exercises. Procedia Soc. Behav. Sci. 2012, 46, 3738–3741. [Google Scholar] [CrossRef]
- Hausenblas, H.A.; Fallon, E.A. Exercise and body image: A meta-analysis. Psychol. Health 2006, 21, 33–47. [Google Scholar] [CrossRef]
- Bąk-Sosnowska, M.; Gruszczyńska, M.; Skrypnik, D.; Grzegorczyn, S.; Karolkiewicz, J.; Ratajczak, M.; Mądry, E.; Walkowiak, J.; Bogdański, P. Type of Physical Training and Selected Aspects of Psychological Functioning of Women with Obesity: A Randomised Trial. Nutrients 2021, 13, 2555. [Google Scholar] [CrossRef]
- Kogure, G.S.; Lopes, I.P.; Ribeiro, V.B.; Mendes, M.C.; Kodato, S.; Furtado, C.L.M.; Silva de Sá, M.F.; Ferriani, R.A.; Lara, L.; Reis, R.M.D. The effects of aerobic physical exercises on body image among women with polycystic ovary syndrome. J. Affect. Disord. 2020, 262, 350–358. [Google Scholar] [CrossRef]
- Moraes, A.D.S.; Cipullo, M.A.T.; Poli, V.F.S.; Rebelo, R.A.; Ribeiro, E.B.; Oyama, L.M.; Silva, S.G.A.; Damaso, A.R.; Padovani, R.D.C.; Caranti, D.A. Neuroendocrine Control, Inflammation, and Psychological Aspects After Interdisciplinary Therapy in Obese Women. Horm. Metab. Res. 2019, 51, 375–380. [Google Scholar] [CrossRef]
- Herbst, K.L.; Ussery, C.; Eekema, A. Pilot study: Whole body manual subcutaneous adipose tissue (SAT) therapy improved pain and SAT structure in women with lipedema. Horm. Mol. Biol. Clin. Investig. 2017, 33. [Google Scholar] [CrossRef]
- Bayrakci Tunay, V.; Akbayrak, T.; Bakar, Y.; Kayihan, H.; Ergun, N. Effects of mechanical massage, manual lymphatic drainage and connective tissue manipulation techniques on fat mass in women with cellulite. J. Eur. Acad. Dermatol. Venereol. 2010, 24, 138–142. [Google Scholar] [CrossRef]
- Poddighe, D.; Ferriero, G.; Corna, S.; Bravini, E.; Sartorio, F.; Vercelli, S. Effects of soft tissue mobilisation on subacute adherent linear scars: A single-group intervention study. J. Wound Care 2024, 33, 43–50. [Google Scholar] [CrossRef]
- Olszewska, K.; Ptak, A.; Rusak, A.; Dębiec-Bąk, A.; Stefańska, M. Changes in the scar tissue structure after cesarean section as a result of manual therapy. Adv. Clin. Exp. Med. 2023, 33. [Google Scholar] [CrossRef]
- Lubczyńska, A.; Garncarczyk, A.; Wcisło-Dziadecka, D. Effectiveness of various methods of manual scar therapy. Ski. Res. Technol. 2023, 29, e13272. [Google Scholar] [CrossRef]
| S | PI | D | E | R |
|---|---|---|---|---|
| Sample | Phenomenon of Interest | Design | Evaluation | Research Type |
| Patient undergoing Aesthetic Rehabilitation Treatments | Physical Therapies | Any | Functional outcomes and Quality of Life | Qualitative |
| “Aesthetic Rehabilitation” “Physical Therapies” “Botulinum Toxin” “Laser Therapy” “Tecar Therapy” “ESWL” | “Function” “Quality of Life” |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lippi, L.; Ferrillo, M.; Losco, L.; Folli, A.; Marcasciano, M.; Curci, C.; Moalli, S.; Ammendolia, A.; de Sire, A.; Invernizzi, M. Aesthetic Rehabilitation Medicine: Enhancing Wellbeing beyond Functional Recovery. Medicina 2024, 60, 603. https://doi.org/10.3390/medicina60040603
Lippi L, Ferrillo M, Losco L, Folli A, Marcasciano M, Curci C, Moalli S, Ammendolia A, de Sire A, Invernizzi M. Aesthetic Rehabilitation Medicine: Enhancing Wellbeing beyond Functional Recovery. Medicina. 2024; 60(4):603. https://doi.org/10.3390/medicina60040603
Chicago/Turabian StyleLippi, Lorenzo, Martina Ferrillo, Luigi Losco, Arianna Folli, Marco Marcasciano, Claudio Curci, Stefano Moalli, Antonio Ammendolia, Alessandro de Sire, and Marco Invernizzi. 2024. "Aesthetic Rehabilitation Medicine: Enhancing Wellbeing beyond Functional Recovery" Medicina 60, no. 4: 603. https://doi.org/10.3390/medicina60040603
APA StyleLippi, L., Ferrillo, M., Losco, L., Folli, A., Marcasciano, M., Curci, C., Moalli, S., Ammendolia, A., de Sire, A., & Invernizzi, M. (2024). Aesthetic Rehabilitation Medicine: Enhancing Wellbeing beyond Functional Recovery. Medicina, 60(4), 603. https://doi.org/10.3390/medicina60040603












