A New Full Digital Workflow for Fixed Prosthetic Rehabilitation of Full-Arch Edentulism Using the All-on-4 Concept
Abstract
1. Introduction
2. Materials and Methods
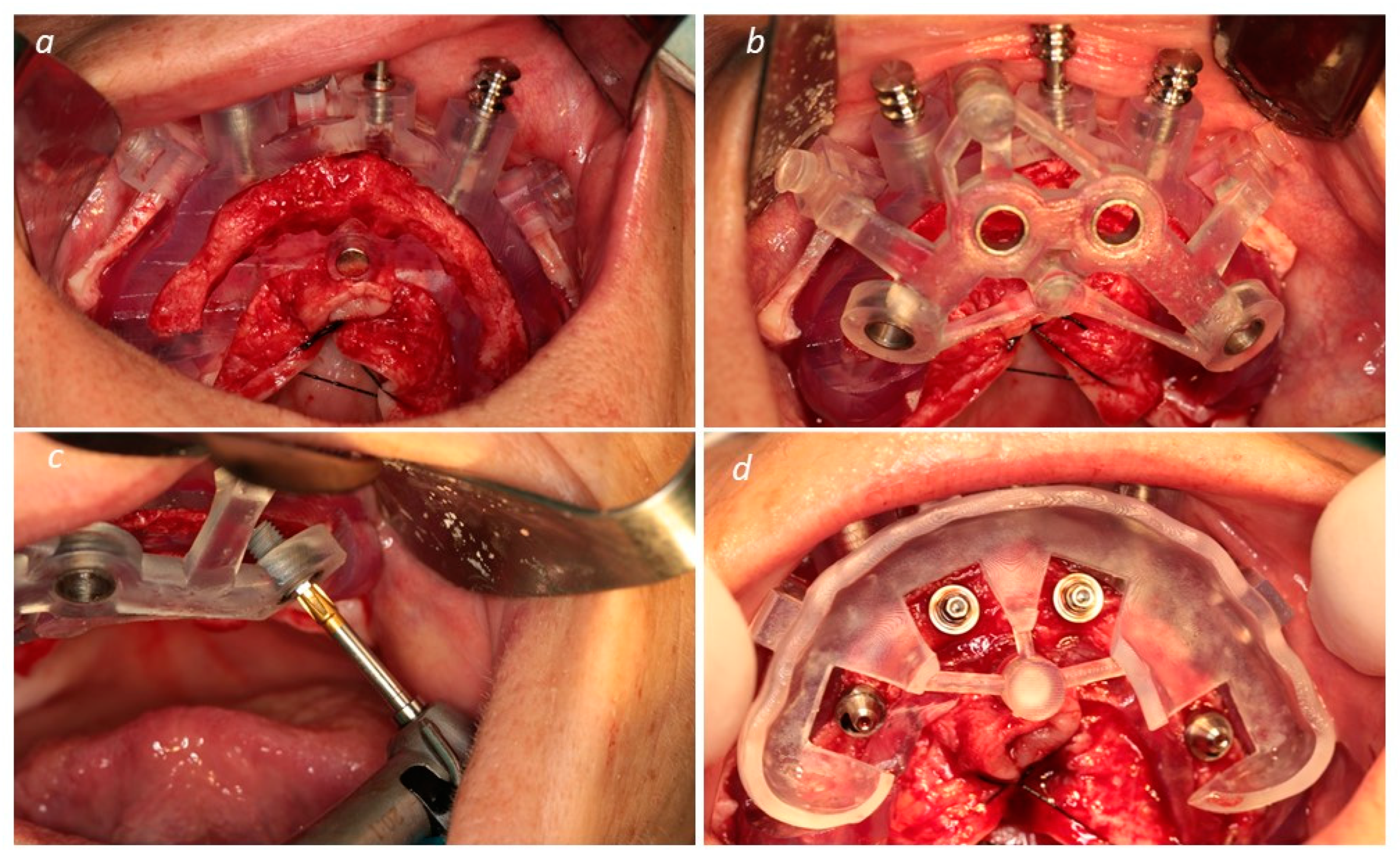
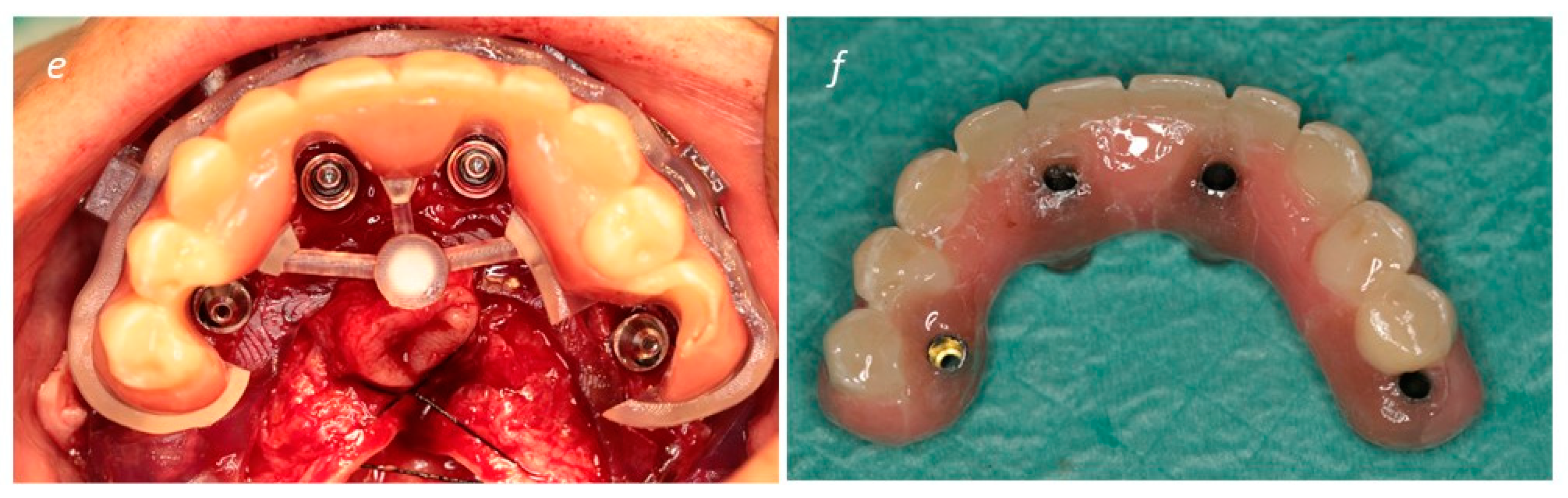
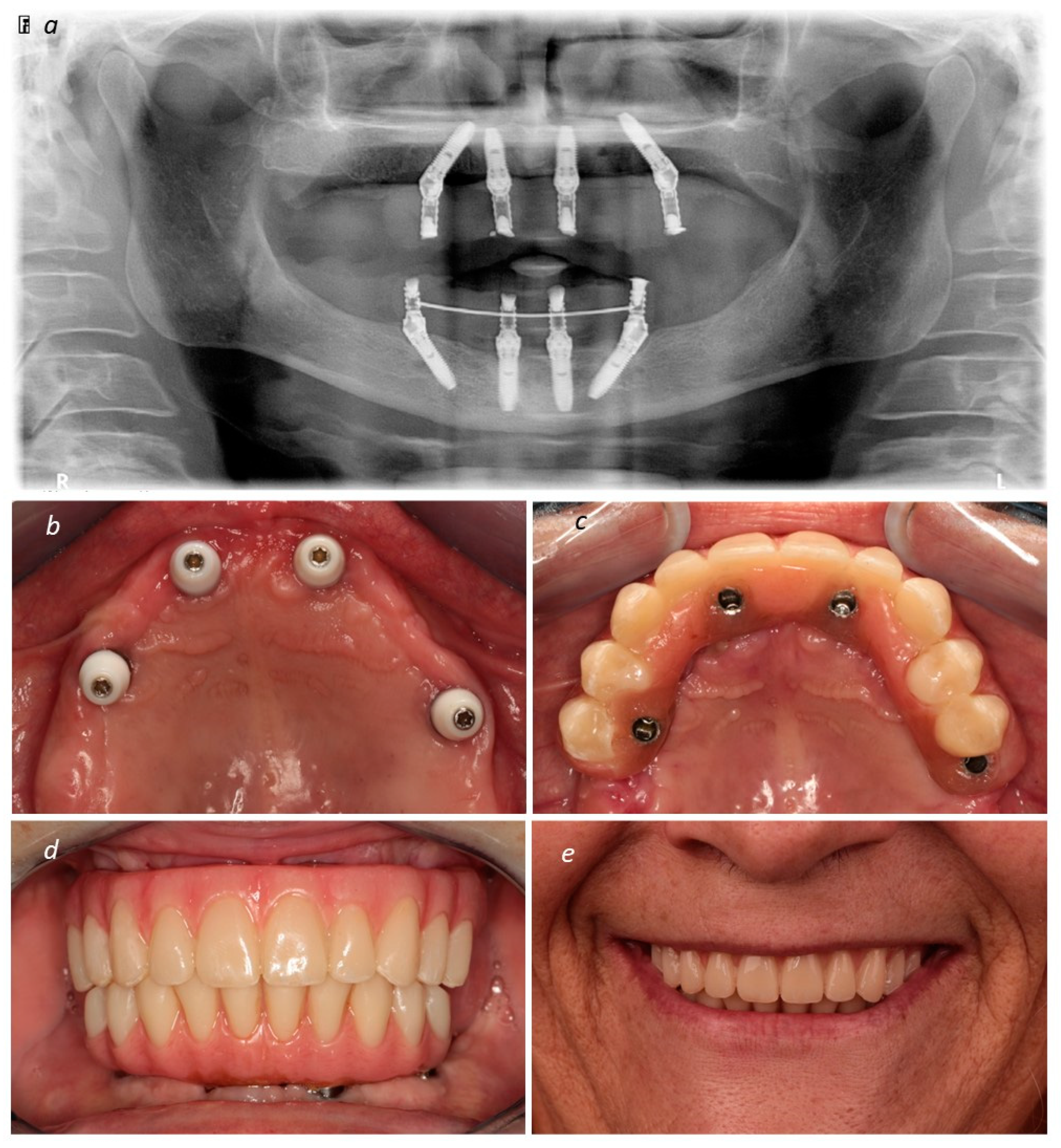
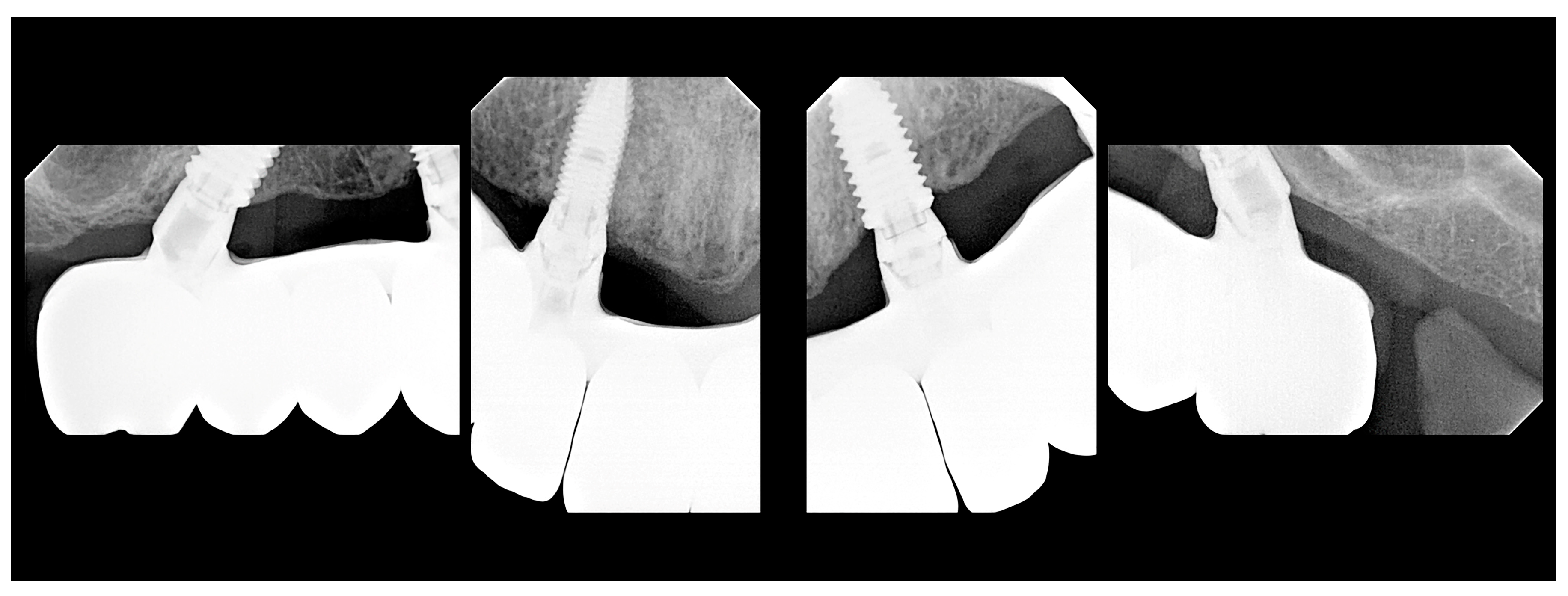
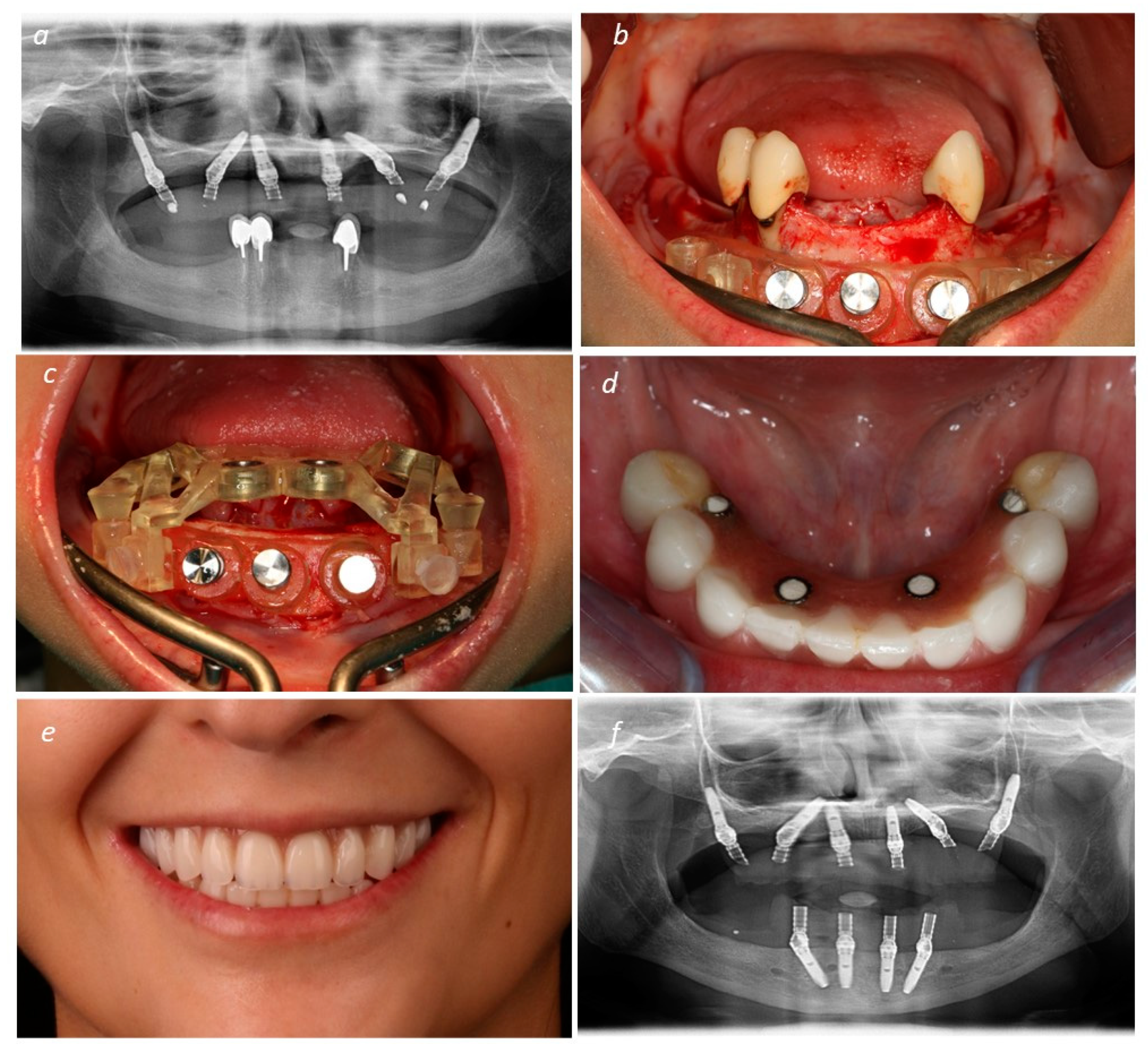
Description of the Technique
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Ferro, A.; Nunes, M. The All-on-4 concept for full-arch rehabilitation of the edentulous maxillae: A longitudinal study with 5-13 years of follow-up. Clin. Implant. Dent. Relat. Res. 2019, 21, 538–549. [Google Scholar] [CrossRef]
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Ferro, A.; Botto, J. The All-on-4 treatment concept for the rehabilitation of the completely edentulous mandible: A longitudinal study with 10 to 18 years of follow-up. Clin. Implant. Dent. Relat. Res. 2019, 21, 565–577. [Google Scholar] [CrossRef]
- Ferro, A.; de Araújo Nobre, M. All-on-4 concept using TiUltra surface implants and Multi-unit Xeal abutments: Report on the outcomes between 6 to 36 months. Clin. Oral Implant. Res. 2023, 34, S137–S138. [Google Scholar] [CrossRef]
- Gama, L.T.; Bezerra, A.P.; Schimmel, M.; Rodrigues Garcia, R.C.M.; de Luca Canto, G.; Gonçalves, T.M.S.V. Clinical performance of polymer frameworks in dental prostheses: A systematic review. J. Prosthet. Dent. 2024, 131, 579–590. [Google Scholar] [CrossRef]
- de Araújo Nobre, M.; Melo, F.; Almeida, R.; Moura Guedes, C.; Lopes, J. Workflow of All-on-4 with full-arch prostheses integrating Hi-Fiber technopolymer reinforced bars. Clin. Oral Implant. Res. 2022, 33, S178–S179. [Google Scholar]
- Mishra, S.K.; Bhasmey, S.R.; Chowdhary, R. Complete-arch implant-supported fixed dental prostheses fabricated with PEEK and PEKK framework: A systematic review. Evid. Based Dent. 2023, 24, 193. [Google Scholar] [CrossRef]
- Pozzi, A.; Hansson, L.; Carosi, P.; Arcuri, L. Dynamic navigation guided surgery and prosthetics for immediate loading of complete-arch restoration. J. Esthet. Restor. Dent. 2021, 33, 224–236. [Google Scholar] [CrossRef]
- Walker-Finch, K.; Ucer, C. Five-year survival rates for implants placed using digitally-designed static surgical guides: A systematic review. Br. J. Oral Maxillofac. Surg. 2020, 58, 268–276. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Chochlidakis, K.; Kang, K.; Chen, Y.; Alghfeli, A.; Kudara, Y.; Weber, H. Digital Workflow for Implant Rehabilitation with Double Full-Arch Monolithic Zirconia Prostheses. J. Prosthodont. 2020, 29, 460–465. [Google Scholar] [CrossRef]
- Chochlidakis, K.; Papaspyridakos, P.; Tsigarida, A.; Romeo, D.; Chen, Y.; Natto, Z.; Ercoli, C. Digital Versus Conventional Full-Arch Implant Impressions: A Prospective Study on 16 Edentulous Maxillae. J. Prosthodont. 2020, 29, 281–286. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Vazouras, K.; Chen, Y.; Kotina, E.; Natto, Z.; Kang, K.; Chochlidakis, K. Digital vs Conventional Implant Impressions: A Systematic Review and Meta-Analysis. J. Prosthodont. 2020, 29, 660–678. [Google Scholar] [CrossRef] [PubMed]
- Papaspyridakos, P.; Chen, Y.; Gonzalez-Gusmao, I.; Att, W. Complete digital workflow in prosthesis prototype fabrication for complete-arch implant rehabilitation: A technique. J. Prosthet. Dent. 2019, 122, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, R. Simplifying Full-Arch Treatment With In-House 3D-Printed Surgical Guides and Immediate Fixed Provisional Prostheses Using Only CBCT Data. Compend. Contin. Educ. Dent. 2020, 41, 521–526. [Google Scholar] [PubMed]
- García-Sala Bonmati, F.; Pérez-Barquero, J.A.; Ilzarbe Ripoll, L.M.; Labaig Rueda, C.; Fernandez-Estevan, L.; Revilla-León, M. An additively manufactured, magnetically retained, and stackable implant surgical guide: A dental technique. J. Prosthet. Dent. 2023, 130, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Amin, S.A.; Hann, S.; Elsheikh, A.K.; Boltchi, F.; Zandinejad, A. A complete digital approach for facially generated full arch diagnostic wax up, guided surgery, and implant-supported interim prosthesis by integrating 3D facial scanning, intraoral scan and CBCT. J. Prosthodont. 2023, 32, 90–93. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; De Souza, A.; Bathija, A.; Kang, K.; Chochlidakis, K. Complete Digital Workflow for Mandibular Full-Arch Implant Rehabilitation in 3 Appointments. J. Prosthodont. 2021, 30, 548–552. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.W.; Liu, Q.; Yue, Z.G.; Hou, J.X.; Afrashtehfar, K.I. Digital Workflow for Full-Arch Immediate Implant Placement Using a Stackable Surgical Guide Fabricated Using SLM Technology. J. Prosthodont. 2021, 30, 645–650. [Google Scholar] [CrossRef]
- Costa, A.J.M.; Teixeira Neto, A.D.; Burgoa, S.; Gutierrez, V.; Cortes, A.R.G. Fully Digital Workflow with Magnetically Connected Guides for Full-Arch Implant Rehabilitation Following Guided Alveolar Ridge Reduction. J. Prosthodont. 2020, 29, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Pommer, B.; Mailath-Pokorny, G.; Haas, R.; Busenlechner, D.; Rudolf, F.; Watzek, G. Patients’ preferences towards minimally invasive treatment alternatives for implant rehabilitation of edentulous jaws. Eur. J. Oral Implant. 2014, 7, S91–S109. [Google Scholar]
- Maló, P.; Rangert, B.; Nobre, M. All-on-four” immediate-function concept with brånemark system® implants for completely edentulous mandibles: A retrospective clinical study. Clin. Implant. Dent. Relat. Res. 2003, 5, S2–S9. [Google Scholar] [CrossRef]
- Lopes, L.F.; da Silva, V.F.; Santiago, J.F., Jr.; Panzarini, S.R.; Pellizzer, E.P. Placement of dental implants in the maxillary tuberosity: A systematic review. Int. J. Oral Maxillofac. Surg. 2015, 44, 229–238. [Google Scholar] [CrossRef]
- Bidra, A.S.; Peña-Cardelles, J.F.; Iverson, M. Implants in the pterygoid region: An updated systematic review of modern roughened surface implants. J. Prosthodont. 2023, 32, 285–291. [Google Scholar] [CrossRef]
- Del Fabbro, M.; Pozzi, A.; Romeo, D.; de Araújo Nobre, M.; Agliardi, E. Outcomes of Fixed Full-Arch Rehabilitations Supported by Tilted and Axially Placed Implants: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implants. 2022, 37, 1003–1025. [Google Scholar] [CrossRef]
- Varga, E.; Antal, M.; Major, L.; Kiscsatári, R.; Braunitzer, G.; Piffkó, J. Guidance means accuracy: A randomized clinical trial on freehand versus guided dental implantation. Clin. Oral Implants Res. 2020, 31, 417–430. [Google Scholar] [CrossRef]
- Bover-Ramos, F.; Viña-Almunia, J.; Cervera-Ballester, J.; Peñarrocha-Diago, M.; García-Mira, B. Accuracy of Implant Placement with Computer-Guided Surgery: A Systematic Review and Meta-Analysis Comparing Cadaver, Clinical, and In Vitro Studies. Int. J. Oral Maxillofac. Implants 2018, 33, 101–115. [Google Scholar] [CrossRef]
- Choi, W.; Nguyen, B.C.; Doan, A.; Girod, S.; Gaudilliere, B.; Gaudilliere, D. Freehand Versus Guided Surgery: Factors Influencing Accuracy of Dental Implant Placement. Implant. Dent. 2017, 26, 500–509. [Google Scholar] [CrossRef]
- Oh, J.H.; An, X.; Jeong, S.M.; Choi, B.H. A digital technique for fabricating an interim implant-supported fixed prosthesis immediately after implant placement in patients with complete edentulism. J. Prosthet. Dent. 2019, 121, 26–31. [Google Scholar] [CrossRef]
- Colombo, M.; Mangano, C.; Mijiritsky, E.; Krebs, M.; Hauschild, U.; Fortin, T. Clinical applications and effectiveness of guided implant surgery: A critical review based on randomized controlled trials. BMC Oral Health 2017, 17, 150. [Google Scholar] [CrossRef]
- Abdelhay, N.; Prasad, S.; Gibson, M.P. Failure rates associated with guided versus non-guided dental implant placement: A systematic review and meta-analysis. BDJ Open 2021, 7, 31. [Google Scholar] [CrossRef]
- Liu, X.Q.; Liu, J.Z.; Feng, H.L.; Heng, M.D.; Wang, B.; Pan, S.X. Time Efficiency of Immediate Loading of Full-arch Implant Reconstructions Using Prefabricated Prostheses Located by an Anchor Pin: A Pilot Study. Chin. J. Dent. Res. 2021, 24, 257–265. [Google Scholar] [CrossRef]
- Block, M.S.; Emery, R.W. Static or Dynamic Navigation for Implant Placement-Choosing the Method of Guidance. J. Oral Maxillofac. Surg. 2016, 74, 269–277. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martins, J.; Rangel, J.; de Araújo Nobre, M.; Ferro, A.; Nunes, M.; Almeida, R.; Moura Guedes, C. A New Full Digital Workflow for Fixed Prosthetic Rehabilitation of Full-Arch Edentulism Using the All-on-4 Concept. Medicina 2024, 60, 720. https://doi.org/10.3390/medicina60050720
Martins J, Rangel J, de Araújo Nobre M, Ferro A, Nunes M, Almeida R, Moura Guedes C. A New Full Digital Workflow for Fixed Prosthetic Rehabilitation of Full-Arch Edentulism Using the All-on-4 Concept. Medicina. 2024; 60(5):720. https://doi.org/10.3390/medicina60050720
Chicago/Turabian StyleMartins, João, João Rangel, Miguel de Araújo Nobre, Ana Ferro, Mariana Nunes, Ricardo Almeida, and Carlos Moura Guedes. 2024. "A New Full Digital Workflow for Fixed Prosthetic Rehabilitation of Full-Arch Edentulism Using the All-on-4 Concept" Medicina 60, no. 5: 720. https://doi.org/10.3390/medicina60050720
APA StyleMartins, J., Rangel, J., de Araújo Nobre, M., Ferro, A., Nunes, M., Almeida, R., & Moura Guedes, C. (2024). A New Full Digital Workflow for Fixed Prosthetic Rehabilitation of Full-Arch Edentulism Using the All-on-4 Concept. Medicina, 60(5), 720. https://doi.org/10.3390/medicina60050720






