Beyond the Preventive Measures: A Delphi Method-Based Study of the Impact of the COVID-19 Pandemic on the Mental Health of Different Age Groups
Abstract
:1. Introduction
- RQ1:
- What measures to prevent and control COVID-19 have affected the lives of specific vulnerable demographic group (e.g., children and adolescents, emerging adults, the adult working population, the elderly), and in what ways have these measures impacted them during the COVID-19 pandemic?
- RQ2:
- What were the specific challenges of each vulnerable demographic group during the COVID-19 pandemic?
- RQ3:
- What protective factors contributed to maintaining the mental health and psychological well-being of each specific vulnerable demographic group during the COVID-19 pandemic?
2. Materials and Methods
2.1. Qualitative Study
2.1.1. Participants
2.1.2. Procedure
2.1.3. Instruments
- Which preventive measures have had the greatest impact on emerging adults and their lives during the COVID-19 pandemic? And why?
- What (psychological) needs of emerging adults have become particularly evident during the COVID-19 pandemic? And why?
- What particular challenges have emerging adults faced during the COVID-19 pandemic?
- What protective factors have helped to maintain psychological well-being and strengthen the mental health of emerging adults during this time? What are the most common internal and external factors? How can they be recognized?
2.2. Quantitative Study
2.2.1. Participants
2.2.2. Procedure
2.2.3. Instruments
3. Results
3.1. Qualitative Part
3.1.1. Children and Adolescents
“… all the knowledge; someone can catch up on it later. But the emotional aspect, the social aspect… These are aspects of development stages that kids miss out on, and it’s pretty hard to catch up on that.”(P10:9)
“And also, normally, when young people go out on their own, they start to feel a bit independent, and that gaining of independence is also an important part/…/of this adolescence stage. But now, when they were home all day and we had nowhere to go, it feels to me like we took a step back in that regard. They ended up feeling more and more dependent on their parents…”(P4:45)
3.1.2. Emerging Adults
“But humans are really social beings at our core. We need that genuine connection with others. And somehow this really caused a lot of distress among the young people because, on top of everything, that they somehow, I will say, they felt like they’d regressed five, ten steps, because just as they were getting independent, making progress, really somehow starting their adults’ lives, then they had to just somehow let go of all this and go back…”(P9:93)
3.1.3. The Adult Working Population
“… who were taking care of other adults, whether it was a partner, a parent, or some other older relatives. For them, I imagine this was a different dynamic. If you’re working from home and at the same time taking care of them.”(P6:62)
“… There was just no time, because of being so overloaded with work, home-schooling kids. So, all of that actually made the day so saturated, on top of keeping up with all the information, that I actually think that even this protective factor was somehow reduced because parents didn’t… there literally was no time, there was no chance for friends to either call each other or meet up…”(P9:9)
3.1.4. The Elderly
“… And then we have those elderly individuals who are just not good with technology./…/So, again we have this gap here, between the ones who could maintain their social interactions, at least with telephone calls or text messages and so on. And those who, because they are not familiar with technology, they had problems in this aspect or rather it was a case of even greater loneliness because of all this.”(P9:57)
3.1.5. Protective Factors
“… A close family as the first, but even if not a closer family, it seems to me that this contact with another human being is what is sincere. That genuine contact is present. It seems to me that this is also something that represents a safe harbor. When you have many problems, but you have the opportunity to talk about them or process these things in another way. This close social network is something that is a good protective factor for a person.”(P6:19)
3.2. Quantitative Study
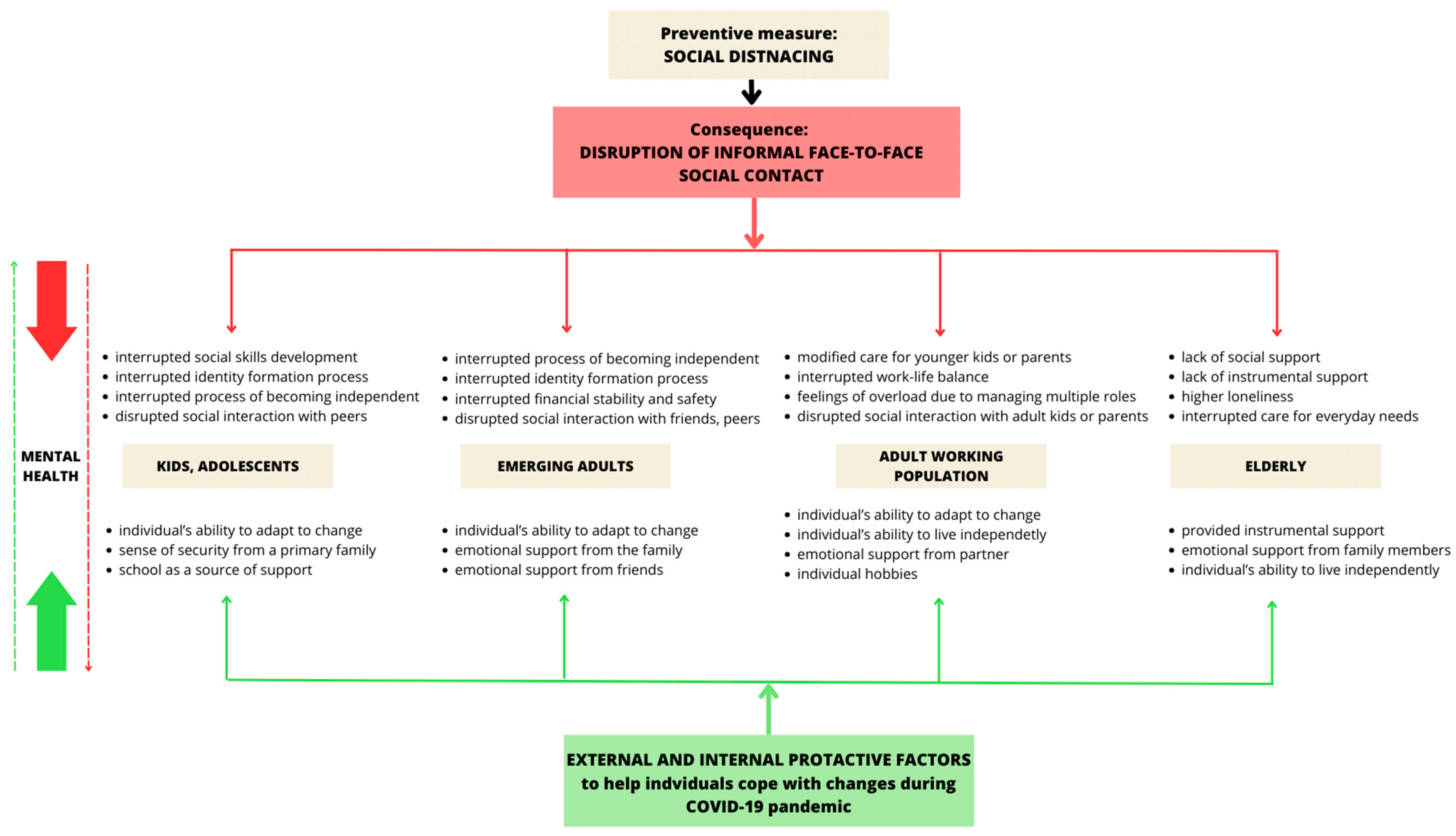
3.3. Integration of the Results
4. Discussion
4.1. Children and Adolescents
4.2. Emerging Adults
4.3. The Adult Working Population
4.4. The Elderly
4.5. Protective Factors
4.6. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, P.J.; Pusica, Y.; Sohaei, D.; Prassas, I.; Diamandis, E.P. An Overview of Mental Health during the COVID-19 Pandemic. Diagnosis 2021, 8, 403–412. [Google Scholar] [CrossRef] [PubMed]
- Talevi, D.; Socci, V.; Carai, M.; Carnaghi, G.; Faleri, S.; Trebbi, E.; Di Bernardo, A.; Capelli, F.; Pacitti, F. Mental Health Outcomes of the CoVID-19 Pandemic. Riv. Psichiatr 2020, 55, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.S.; Chee, C.Y.; Ho, R.C. Mental Health Strategies to Combat the Psychological Impact of Coronavirus Disease 2019 (COVID-19) Beyond Paranoia and Panic. Ann. Acad. Med. Singap. 2020, 49, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Lavrič, M.; Gomboc, V.; Krohne, N.; Podlogar, T.; Poštuvan, V.; Zadravec Šedivy, N.; De Leo, D. Concerns, Positive Changes, and Suggestions for Psychological Support during COVID-19: A Thematic Analysis. Sociol. Mind 2020, 10, 187–199. [Google Scholar] [CrossRef]
- Kavčič, T.; Avsec, A.; Zager Kocjan, G. Od začetka do konca uradne epidemije COVID-19 v Sloveniji: Stresorji, stres in blagostanje. In Psihologija Pandemije: Posamezniki in Družba v času Koronske Krize; Znanstvena založba Filozofske Fakultete Univerze v Ljubljani: Ljubljana, Slovenia, 2020; pp. 23–35. [Google Scholar]
- Horigian, V.E.; Schmidt, R.D.; Feaster, D.J. Loneliness, Mental Health, and Substance Use among US Young Adults during COVID-19. J. Psychoact. Drugs 2021, 53, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Zhang, E.; Wong, G.T.F.; Hyun, S.; Hahm, H. “Chris” Factors Associated with Depression, Anxiety, and PTSD Symptomatology during the COVID-19 Pandemic: Clinical Implications for U.S. Young Adult Mental Health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef] [PubMed]
- Mohler-Kuo, M.; Dzemaili, S.; Foster, S.; Werlen, L.; Walitza, S. Stress and Mental Health among Children/Adolescents, Their Parents, and Young Adults during the First COVID-19 Lockdown in Switzerland. Int. J. Environ. Res. Public Health 2021, 18, 4668. [Google Scholar] [CrossRef] [PubMed]
- Meyer, J.; McDowell, C.; Lansing, J.; Brower, C.; Smith, L.; Tully, M.; Herring, M. Changes in Physical Activity and Sedentary Behavior in Response to COVID-19 and Their Associations with Mental Health in 3052 Us Adults. Int. J. Environ. Res. Public Health 2020, 17, 6469. [Google Scholar] [CrossRef] [PubMed]
- Altena, E.; Baglioni, C.; Espie, C.A.; Ellis, J.; Gavriloff, D.; Holzinger, B.; Schlarb, A.; Frase, L.; Jernelöv, S.; Riemann, D. Dealing with Sleep Problems during Home Confinement Due to the COVID-19 Outbreak: Practical Recommendations from a Task Force of the European CBT-I Academy. J. Sleep Res. 2020, 29, e13052. [Google Scholar] [CrossRef] [PubMed]
- Pantell, M.S.; Shields-Zeeman, L. Maintaining Social Connections in the Setting of COVID-19 Social Distancing: A Call to Action. Am. J. Public Health 2020, 110, 1367–1368. [Google Scholar] [CrossRef]
- Lebow, J.L. Family in the Age of COVID-19. Fam. Process 2020, 59, 309–312. [Google Scholar] [CrossRef] [PubMed]
- Gomboc, V.; Krohne, N.; Lavrič, M.; Podlogar, T.; Poštuvan, V.; Zadravec Šedivy, N.; De Leo, D. Primerjava Osamljenosti in Subjektivnega Blagostanja v Normalnih in Izrednih Razmerah. In Psihologija Pandemije: Posamezniki in Družba v Času Koronske krize; Lep, Ž., Hacin Beyazoglu, K., Eds.; Znanstvena založba Filozofske fakultete Univerze v Ljubljani: Ljubljana, Slovenia, 2020; pp. 79–89. [Google Scholar]
- Einav, M.; Margalit, M. Loneliness before and after COVID-19: Sense of Coherence and Hope as Coping Mechanisms. Int. J. Environ. Res. Public Health 2023, 20, 5840. [Google Scholar] [CrossRef] [PubMed]
- De Jong Gierveld, J.; Van Tilburg, T. A 6-Item Scale for Overall, Emotional, and Social Loneliness: Confirmatory Tests on Survey Data. Res. Aging 2006, 28, 582–598. [Google Scholar] [CrossRef]
- Nazroo, J.; Murray, K.; Bécares, L.; Field, Y.; Kapadia, D.; Rolston, Y. Rapid Evidence Review: Inequalities in Relation to COVID-19 and Their Effects on London; University of Manchester: Manchester, UK, 2020. [Google Scholar]
- Lee, K.; Jeong, G.C.; Yim, J. Consideration of the Psychological and Mental Health of the Elderly during COVID-19: A Theoretical Review. Int. J. Environ. Res. Public Health 2020, 17, 8098. [Google Scholar] [CrossRef] [PubMed]
- Uršič, L.; Puklek Levpušček, M. Učenci Zadnje Triade OŠ in Dijaki o Učenju Na Daljavo Med Epidemijo COVID-19. In Psihologija Pandemije: Posamezniki in Družba v času Koronske krize; Lep, Ž., Hacin Beyazoglu, K., Eds.; Znanstvena založba Filozofske fakultete Univerze v Ljubljani: Ljubljana, Slovenia, 2020; pp. 191–203. [Google Scholar]
- Podlogar, N.; Žerak, U.; Lišić, A.; Lavrih, L.; Fricelj, N.; Juriševič, M. Pogledi in Izkušnje Študentov Pedagoških Smeri o Študiju Na Daljavo v Času Epidemije COVID-19. In Psihologija Pandemije: Posamezniki in Družba v času Koronske Krize; Lep, Ž., Hacin Beyazoglu, K., Eds.; Znanstvena založba Filozofske fakultete Univerze v Ljubljani: Ljubljana, Slovenia, 2020; pp. 205–216. [Google Scholar]
- Ghosh, R.; Dubey, M.J.; Chatterjee, S.; Dubey, S. Impact of COVID-19 on Children: Special Focus on the Psychosocial Aspect. Minerva Pediatr. 2020, 72, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Rupnik Vec, T.; Slivar, B.; Zupanc Grom, R.; Deutsch, T.; Ivanuš-Grmek, M.; Mithans, M.; Kregar, S.; Holcar Brunauer, A.; Preskar, S.; Bevc, V.; et al. Analiza Izobraževanja Na Daljavo v Času Prvega Vala Epidemije COVID-19 v Sloveniji; Zavod Republike Slovenije za šolstvo: Ljubljana, Slovenia, 2020; ISBN 978-961-03-0539-2. [Google Scholar]
- Lep, Ž.; Zupančič, M. Zdaj Pa Še Korona: Skrbi Mladih Na Prehodu v Odraslost v Času Tveganj, Povezanih z Epidemijo COVID-19. In Psihologija Pandemije: Posamezniki in Družba v Času Koronske krize; Lep, Ž., Hacin Beyazoglu, K., Eds.; Znanstvena Založba Filozofske Fakultete Univerze v Ljubljani: Ljubljana, Slovenia, 2020; pp. 67–78. [Google Scholar]
- Šraj Lebar, T.; Kerč, P.; Krohne, N.; Štirn, M. Students as a Vulnerable Group for Developing Psychological Distress during the Pandemic. Eur. J. Psychotraumatol. 2021, 12 (Suppl. S2), 11. [Google Scholar] [CrossRef] [PubMed]
- Hacin Beyazoglu, K.; Bertogna, T.; Hostnik, L.; Jakopič, T.; Škoda, K.; Zakelšek, M.; Fekonja, U. Težave in Izzivi Družin z Otroki v Zgodnjem in Srednjem Otroštvu Med Karanteno Zaradi Epidemije COVID-19. In Psihologija Pandemije: Posamezniki in Družba v času Koronske Kriz; Lep, Ž., Hacin Beyazoglu, K., Eds.; Znanstvena založba Filozofske fakultete Univerze v Ljubljani: Ljubljana, Slovenia, 2020; Volume 2020, pp. 53–65. [Google Scholar]
- Griffith, A.K. Parental Burnout and Child Maltreatment During the COVID-19 Pandemic. J. Fam. Violence 2022, 37, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Pišot, S.; Milovanović, I.; Šimunič, B.; Gentile, A.; Bosnar, K.; Prot, F.; Bianco, A.; Lo Coco, G.; Bartoluci, S.; Katović, D.; et al. Maintaining Everyday Life Praxis in the Time of COVID-19 Pandemic Measures (ELP-COVID-19 Survey). Eur. J. Public Health 2020, 11, 1181–1186. [Google Scholar] [CrossRef]
- Wilson, J.M.; Lee, J.; Fitzgerald, H.N.; Oosterhoff, B.; Sevi, B.; Shook, N.J. Job Insecurity and Financial Concern during the COVID-19 Pandemic Are Associated with Worse Mental Health. J. Occup. Environ. Med. 2020, 62, 686–691. [Google Scholar] [CrossRef]
- Krohne, N.; Kerč, P.; Šraj Lebar, T.; Štirn, M. Gendered Pandemic: Mental Health Differences in Men and Women during the COVID-19 Pandemic. In Proceedings of the Virtual Conference ESTSS 2021 Abstract Book Symposium Oral Present, Online, 4–7 October 2021; pp. 16–17. [Google Scholar]
- Armitage, R.; Nellums, L.B. COVID-19 and the Consequences of Isolating the Elderly. Lancet Public Health 2020, 5, e256. [Google Scholar] [CrossRef]
- Trabucchi, M.; De Leo, D. Nursing Homes or Besieged Castles: COVID-19 in Northern Italy. Lancet Psychiatry 2020, 7, 387–388. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of Mental Health Problems during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Lep, Ž.; Hacin Beyazoglu, K. (Eds.) Psihologija Pandemije: Posamezniki in Družba v Času Koronske Krize; Znanstvena Založba Filozofske Fakultete Univerze v Ljubljani: Ljubljana, Slovenia, 2020. [Google Scholar]
- Keeney, S.; Hasson, F.; McKenna, H. The Delphi Technique in Nursing and Health Research; Wiley Online Library: Chichester, UK, 2011; ISBN Online; ISBN 9781444392029. [Google Scholar]
- Powell, C. The Delphi Technique: Myths and Realities. J. Adv. Nurs. 2003, 41, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Matthews, T.; Danese, A.; Caspi, A.; Fisher, H.L.; Goldman-Mellor, S.; Kepa, A.; Moffitt, T.E.; Odgers, C.L.; Arseneault, L. Lonely Young Adults in Modern Britain: Findings from an Epidemiological Cohort Study. Psychol. Med. 2019, 49, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Orben, A.; Tomova, L.; Blakemore, S.J. The Effects of Social Deprivation on Adolescent Development and Mental Health. Lancet Child Adolesc. Health 2020, 4, 634–640. [Google Scholar] [CrossRef] [PubMed]
- Blakemore, S.J.; Mills, K.L. Is Adolescence a Sensitive Period for Sociocultural Processing? Annu. Rev. Psychol. 2014, 65, 187–207. [Google Scholar] [CrossRef] [PubMed]
- Marjanovič Umek, L.; Zupnačič, M. Razvojna Psihologija; Znanstvena Založba Filozofske Fakultete: Ljubljana, Slovenia, 2009. [Google Scholar]
- Deocadez, R.G.; Anna Gayoles, L.M. Emerging Adult Graduating Students Adapting to the COVID-19 Pandemic: A Phenomenological Study. Lond. J. Res. Humanit. Soc. Sci. 2022, 22, 29–60. [Google Scholar]
- Arnett, J.J. Emerging Adulthood: A Theory of Development From the Late Teens Through the Twenties. Am. Psychol. 2000, 55, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Cordingley, K.J. Emerging Adults and Identity Development in the Time of COVID-19. Master’s Thesis, University of Montana, Missoula, MT, USA, 2022. [Google Scholar]
- Modic, S.; Kobal Grum, D. Dejavniki Čustvovanja in Spoprijemanje s Stresom Med Pandemijo COVID-19. In Psihologija Pandemije Posamezniki in Družba v času Koronske Krize; Lep, Ž., Hacin Beyazoglu, K., Eds.; Znanstvena založba Filozofske fakultete Univerze v Ljubljani: Ljubljana, Slovenia, 2020; pp. 129–142. [Google Scholar]
- Lei, L.; Huang, X.; Zhang, S.; Yang, J.; Yang, L.; Xu, M. Comparison of Prevalence and Associated Factors of Anxiety and Depression among People Affected by versus People Unaffected by Quarantine during the COVID-19 Epidemic in Southwestern China. Med. Sci. Monit. 2020, 26, e924609. [Google Scholar] [CrossRef]
- Santini, Z.I.; Jose, P.E.; York Cornwell, E.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social Disconnectedness, Perceived Isolation, and Symptoms of Depression and Anxiety among Older Americans (NSHAP): A Longitudinal Mediation Analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef]
- Biggs, A.; Brough, P.; Drummond, S. Lazarus and Folkman’s Psychological Stress and Coping Theory. In The Handbook of Stress and Health: A Guide to Research and Practice, 1st ed.; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2017; pp. 351–363. [Google Scholar]
- PeConga, E.K.; Gauthier, G.M.; Holloway, A.; Walker, R.S.W.; Rosencrans, P.L.; Zoellner, L.A.; Bedard-Gilligan, M. Resilience Is Spreading: Mental Health within the COVID-19 Pandemic. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, S47–S48. [Google Scholar] [CrossRef] [PubMed]
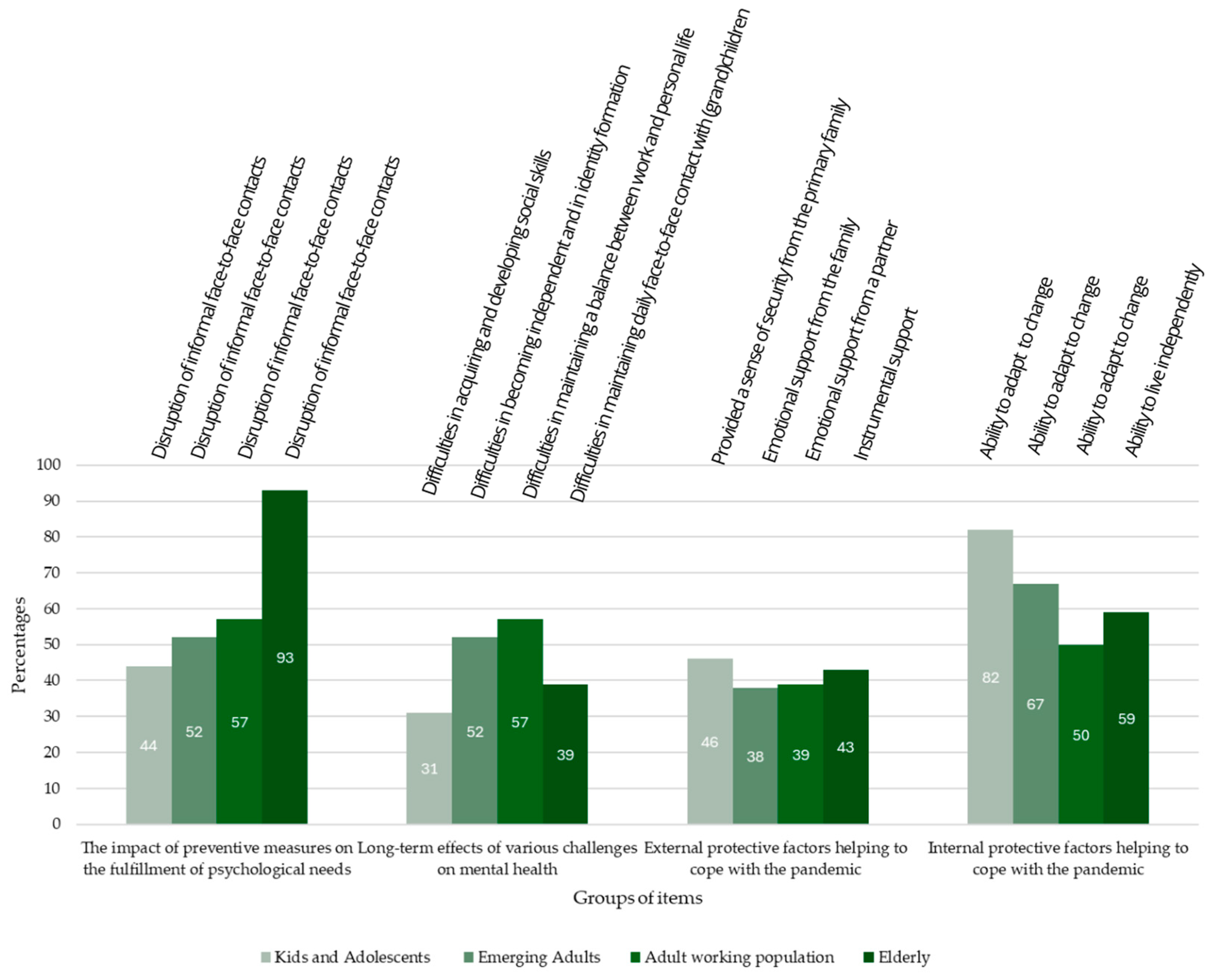
| Item | Percentage of Professionals 1 | M 2 (min–max) | SD | χ2 | df |
|---|---|---|---|---|---|
| CHILDREN AND ADOLESCENTS (N = 39) | |||||
| The impact of preventive measures on the fulfillment of psychological needs | 18.67 ** | 2 | |||
| Interruption of organized leisure activities | 13 | 2.56 (1–3) | 0.72 | ||
| Disruption of informal face-to-face contacts | 44 | 1.69 (1–3) | 0.70 | ||
| Closing of schools (interruption of face-to-face learning) | 44 | 1.74 (1–3) | 0.75 | ||
| Long-term effects of various challenges on mental health | 38.77 ** | 4 | |||
| Difficulties in maintaining daily face-to-face contact with peers | 23 | 2.67 (1–5) | 1.34 | ||
| Difficulties in becoming independent and in identity formation | 13 | 3.46 (1–5) | 1.25 | ||
| Difficulties in acquiring and developing social skills | 31 | 2.31 (1–5) | 1.20 | ||
| Difficulties in maintaining physical fitness | 5 | 4.15 (1–5) | 1.13 | ||
| Difficulties in following the school process | 28 | 2.41 (1–5) | 1.27 | ||
| External protective factors helping to cope with the pandemic | 68.52 ** | 5 | |||
| Emotional support from the family | 15 | 2.46 (1–6) | 1.14 | ||
| Provided a sense of security from the primary family | 46 | 2.13 (1–6) | 1.34 | ||
| Accepting attitudes of the primary family (pandemic, measures) | 26 | 3.10 (1–6) | 1.64 | ||
| Emotional support from friends and peers | 3 | 3.97 (1–6) | 1.27 | ||
| Emotional support from teachers and other school workers | 10 | 4.46 (1–6) | 1.75 | ||
| Individual hobbies | 0 | 4.87 (1–6) | 1.11 | ||
| Internal protective factors helping to cope with the pandemic | 16.03 ** | 1 | |||
| Ability to adapt to change | 82 | 1.18 (1–2) | 0.39 | ||
| Ability to perform tasks independently (e.g., homework) | 18 | 1.82 (1–2) | 0.39 | ||
| EMERGING ADULTS (N = 21) | |||||
| The impact of preventive measures on the fulfillment of psychological needs | 22.32 ** | 4 | |||
| Interruption of organized leisure activities | 5 | 3.14 (1–5) | 1.15 | ||
| Disruption of informal face-to-face contacts | 52 | 1.71 (1–5) | 1.01 | ||
| Closing of faculties (interruption of face-to-face courses) | 29 | 2.86 (1–5) | 1.49 | ||
| Introduction of remote working | 5 | 3.90 (1–5) | 1.18 | ||
| Changed market needs and opportunities | 9 | 3.38 (1–5) | 1.32 | ||
| Long-term effects of various challenges on mental health | 21.41 ** | 5 | |||
| Difficulties in maintaining daily face-to-face contact with peers | 19 | 2.71 (1–6) | 1.49 | ||
| Difficulties in maintaining daily face-to-face contact with parents | 10 | 4.57 (1–6) | 1.57 | ||
| Difficulties in maintaining daily face-to-face contact with a partner | 5 | 5.73 (1–6) | 1.29 | ||
| Difficulties in following the study process | 0 | 3.52 (1–6) | 1.37 | ||
| Difficulties in becoming independent and in identity formation | 52 | 2.38 (1–6) | 1.77 | ||
| Difficulties in maintaining a balance between work and personal life | 14 | 4.24 (1–6) | 1.81 | ||
| External protective factors helping to cope with the pandemic | 13.60 * | 5 | |||
| Emotional support from the family | 38 | 2.81 (1–6) | 1.75 | ||
| Financial support from the family | 5 | 3.86 (1–6) | 1.59 | ||
| Accepting attitudes of the primary family (pandemic, measures) | 10 | 4.52 (1–6) | 1.83 | ||
| Emotional support from peers | 24 | 2.90 (1–6) | 1.64 | ||
| Emotional support from a partner | 10 | 3.10 (1–6) | 1.22 | ||
| Individual hobbies | 14 | 3.81 (1–6) | 1.69 | ||
| Internal protective factors helping to cope with the pandemic | 29.80 ** | 3 | |||
| Ability to find meaning in the situation | 28 | 2.00 (1–4) | 0.84 | ||
| Ability to adapt to change | 67 | 1.52 (1–4) | 0.93 | ||
| Ability to perform tasks independently (e.g., cooking) | 5 | 3.05 (1–4) | 0.87 | ||
| Ability to provide financial security | 0 | 3.43 (1–4) | 0.68 | ||
| ADULT WORKING POPULATION (N = 36) | |||||
| The impact of preventive measures on the fulfillment of psychological needs | 21.07 ** | 3 | |||
| Disruption of informal face-to-face contacts | 57 | 1.73 (1–4) | 0.96 | ||
| Introduction of remote working | 21 | 2.59 (1–4) | 1.12 | ||
| Changed market needs and opportunities | 19 | 2.59 (1–4) | 1.11 | ||
| Mobility restrictions | 3 | 3.08 (1–4) | 0.92 | ||
| Long-term effects of various challenges on mental health | 12.34 * | 3 | |||
| Difficulties in maintaining daily face-to-face contact with parents | 19 | 2.51 (1–4) | 1.10 | ||
| Difficulties in maintaining daily face-to-face contact with adult children | 11 | 2.73 (1–4) | 0.93 | ||
| Difficulties in maintaining daily face-to-face contact with a partner | 13 | 2.86 (1–4) | 1.11 | ||
| Difficulties in maintaining a balance between work and personal life | 57 | 1.89 (1–4) | 1.15 | ||
| External protective factors helping to cope with the pandemic | 32.24 ** | 5 | |||
| Emotional support from a partner | 39 | 2.36 (1–6) | 1.55 | ||
| Financial support from close family members | 3 | 4.72 (1–6) | 1.39 | ||
| Accepting attitudes of close family members (pandemic, measures) | 11 | 3.81 (1–6) | 1.87 | ||
| Emotional support from friends | 0 | 3.72 (1–6) | 1.23 | ||
| Emotional support from an extended family | 22 | 3.28 (1–6) | 1.60 | ||
| Individual hobbies | 25 | 3.11 (1–6) | 1.70 | ||
| Internal protective factors helping to cope with the pandemic | 20.98 ** | 4 | |||
| Ability to adapt to change | 50 | 2.11 (1–5) | 1.37 | ||
| Ability to live independently | 23 | 3.67 (1–5) | 1.37 | ||
| Ability to organize effectively | 19 | 2.89 (1–5) | 1.39 | ||
| Ability to provide financial security | 11 | 3.44 (1–5) | 1.25 | ||
| Ability to think critically | 17 | 2.89 (1–5) | 1.28 | ||
| ELDERLY (N = 28) | |||||
| The impact of preventive measures on the fulfillment of psychological needs | 39.93 ** | 2 | |||
| Interruption of organized leisure activities | 0 | 2.11 (1–3) | 0.32 | ||
| Disruption of informal face-to-face contacts | 93 | 1.11 (1–3) | 0.45 | ||
| Mobility restrictions | 7 | 2.79 (1–3) | 0.57 | ||
| Long-term effects of various challenges on mental health | 1.14 | 2 | |||
| Difficulties in maintaining daily face-to-face contact with (grand)children | 39 | 1.86 (1–3) | 0.80 | ||
| Difficulties in protecting oneself from virus infection | 25 | 2.14 (1–3) | 0.80 | ||
| Difficulties in accessing medical care | 36 | 2.00 (1–3) | 0.86 | ||
| External protective factors helping to cope with the pandemic | 51.54 ** | 6 | |||
| Emotional support from a partner | 14 | 4.11 (1–7) | 2.10 | ||
| Emotional support from family members | 22 | 2.46 (1–7) | 1.07 | ||
| Emotional support from friends | 7 | 3.82 (1–7) | 1.77 | ||
| Financial support from family | 0 | 6.04 (1–7) | 1.29 | ||
| Own financial security | 7 | 4.54 (1–7) | 1.90 | ||
| Instrumental support | 43 | 2.71 (1–7) | 1.80 | ||
| Individual hobbies | 7 | 4.32 (1–7) | 1.72 | ||
| Internal protective factors helping to cope with the pandemic | 7.63 * | 2 | |||
| Ability to adapt to change | 30 | 2.07 (1–3) | 0.83 | ||
| Ability to live independently | 59 | 1.59 (1–3) | 0.80 | ||
| Ability to organize effectively | 11 | 2.33 (1–3) | 0.68 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sedlašek, E.; Krohne, N.; Borko, P.; Zemljarič, I.; Masten, R.; Vinko, M.; De Leo, D.; Poštuvan, V. Beyond the Preventive Measures: A Delphi Method-Based Study of the Impact of the COVID-19 Pandemic on the Mental Health of Different Age Groups. Medicina 2024, 60, 978. https://doi.org/10.3390/medicina60060978
Sedlašek E, Krohne N, Borko P, Zemljarič I, Masten R, Vinko M, De Leo D, Poštuvan V. Beyond the Preventive Measures: A Delphi Method-Based Study of the Impact of the COVID-19 Pandemic on the Mental Health of Different Age Groups. Medicina. 2024; 60(6):978. https://doi.org/10.3390/medicina60060978
Chicago/Turabian StyleSedlašek, Eva, Nina Krohne, Polonca Borko, Ives Zemljarič, Robert Masten, Matej Vinko, Diego De Leo, and Vita Poštuvan. 2024. "Beyond the Preventive Measures: A Delphi Method-Based Study of the Impact of the COVID-19 Pandemic on the Mental Health of Different Age Groups" Medicina 60, no. 6: 978. https://doi.org/10.3390/medicina60060978





