Deep Learning in Neovascular Age-Related Macular Degeneration
Abstract
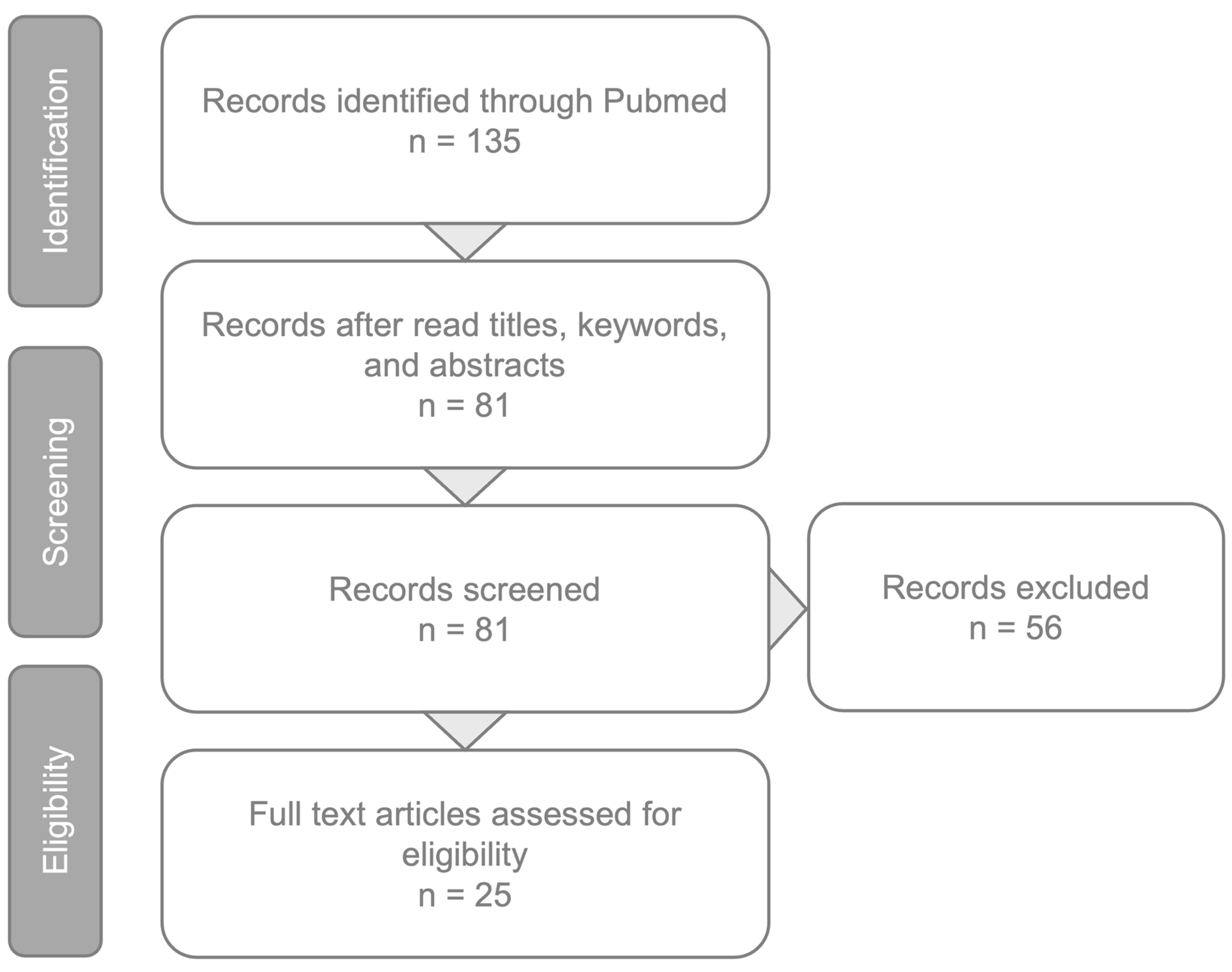
:1. Introduction
2. OCT Biomarkers in Neovascular AMD
- Intraretinal fluid (IRF) is characterized by the presence of round- or oval-shaped cysts within the inner retinal layers, appearing typically hyporeflective on OCT. IRF is more frequently associated with Type 2 and Type 3 MNV. Numerous studies suggest that IRF serves as a crucial negative prognostic biomarker, correlating not only with reduced visual acuity at baseline and less improvement after treatment, but also with a higher risk of fibrosis and atrophy development [32,33,34].
- Subretinal fluid (SRF) occurs when exudative fluid accumulates between the neuroretina and RPE. SRF is more frequently associated with Type 1 MNV. In contrast to IRF, SRF tends to indicate a more favorable prognosis. It is often associated with better visual acuity at baseline and after intravitreal therapy, as well as a reduced risk of atrophy [34,35]. However, it is important to note that the presence of SRF is considered as a negative biomarker in eyes with Type 3 MNV.
- Pigmented epithelium detachment (PED) occurs when there is a splitting between the RPE and Bruch’s membrane. The literature lacks consensus on the prognostic significance of PED. The latter aspect could be attributed to the existence of different types of PEDs, including fibrovascular, serous, drusenoid, and hemorrhagic, each potentially exerting distinct effects on visual acuity [34,35,36,37].
- Subretinal hyperreflective material (SHRM) refers to a hyperreflective material observed on structural OCT, situated beneath the neurosensory retina and above the RPE. SHRM could indicate various substances including fluid, blood, scar tissue, fibrin, vitelliform material, or neovascularization [38,39]. Previous studies have indicated that SHRM is a negative prognostic biomarker, correlating with a reduced response to anti-VEGF treatment and poorer visual outcomes [40,41,42].
- The disruption of the outer retinal layers refers to a notable OCT sign occurring when damage to the outer hyperreflective retinal layers is evident, including the ellipsoid zone (EZ) and external limiting membrane (ELM). Such disruptions in these hyperreflective bands have been associated with compromised visual acuity both at baseline and following anti-VEGF therapy [43,44,45].
- Retinal hyperreflective foci (HRF) are defined as hyperreflective spots on structural OCT, displaying a reflectivity akin to or higher than the retinal pigment epithelium (RPE), typically measuring between 20 to 40 microns and often exhibiting clear boundaries [46]. While intraretinal HRF may be the imaging surrogate of different cells/lesions, in AMD they are mostly associated with migrating RPE cells [47,48]. In a previous study, it was demonstrated that the number of HRF decreased after anti-VEGF therapy in responders, while they persisted in non-responders, and as a result their persistence despite treatment is considered a negative prognostic factor associated with poor VA [49]. Neuroretinal HRF were also suggested as an imaging indicator of inflammation in neovascular AMD, showing a decrease in number following effective anti-VEGF treatment [50]. Of note, HRF detection in neovascular AMD was considered a reliable predictor of poor visual prognosis after anti-VEGF treatment [51].
3. Artificial Intelligence in AMD
4. Deep Learning to Predict Progression from Intermediate to Neovascular AMD
5. Deep Learning to Segment OCT Features in Patients with Neovascular AMD
6. Deep Learning to Predict Anti-VEGF Treatment in Patients with Neovascular AMD
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Daien, V.; Finger, R.P.; Talks, J.S.; Mitchell, P.; Wong, T.Y.; Sakamoto, T.; Eldem, B.M.; Korobelnik, J.F. Evolution of treatment paradigms in neovascular age-related macular degeneration: A review of real-world evidence. Br. J. Ophthalmol. 2020, 105, 1475–1479. [Google Scholar] [CrossRef] [PubMed]
- Souied, E.H.; Benlian, P.; Amouyel, P.; Feingold, J.; Lagarde, J.P.; Munnich, A.; Kaplan, J.; Coscas, G.; Soubrane, G. The ε4 allele of the Apolipoprotein E gene as a potential protective factor for exudative age-related macular degeneration. Am. J. Ophthalmol. 1998, 125, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Reibaldi, M.; Barresi, C.; Berni, A.; Introini, U.; Bandello, F. Choroidal Hyper-Reflective Foci in Geographic Atrophy. Investig. Ophthalmol. Vis. Sci. 2023, 64, 5. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Borrelli, E.; Berni, A.; Mastropasqua, L.; Querques, G.; Sadda, S.R.; Sarraf, D.; Bandello, F. Pushing Retinal Imaging Forward: Innovations and Their Clinical Meaning—The 2022 Ophthalmologica Lecture. Ophthalmologica 2023, 246, 278–294. [Google Scholar] [CrossRef] [PubMed]
- Barresi, C.; Chhablani, J.; Dolz-Marco, R.; Gallego-Pinazo, R.; Berni, A.; Bandello, F.; Borrelli, E. Retinal neurodegeneration in age-related macular degeneration. Eur. J. Ophthalmol. 2023, 34, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Viggiano, P.; Grassi, M.O.; Pignataro, M.; Boscia, G.; Borrelli, E.; Molfetta, T.; Evangelista, F.; Alessio, G.; Boscia, F. Topographical Analysis of the Choriocapillaris Reperfusion after Loading Anti-VEGF Therapy in Neovascular AMD. Transl. Vis. Sci. Technol. 2022, 11, 18. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Borrelli, E.; Bandello, F.; Souied, E.H.; Barresi, C.; Miere, A.; Querques, L.; Sacconi, R.; Querques, G. Neovascular age-related macular degeneration: Advancement in retinal imaging builds a bridge between histopathology and clinical findings. Graefe’s Arch. Clin. Exp. Ophthalmol. 2022, 260, 2087–2093. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Sacconi, R.; Zuccaro, B.; Cavalleri, M.; Bordato, A.; Zucchiatti, I.; Querques, L.; Bandello, F.; Querques, G. Photoreceptor alteration in intermediate age-related macular degeneration. Sci. Rep. 2020, 10, 21036. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Borrelli, E.; Shi, Y.; Uji, A.; Balasubramanian, S.; Nassisi, M.; Sarraf, D.; Sadda, S.R. Topographic Analysis of the Choriocapillaris in Intermediate Age-related Macular Degeneration. Am. J. Ophthalmol. 2018, 196, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Sarraf, D.; Freund, K.B.; Sadda, S.R. OCT angiography and evaluation of the choroid and choroidal vascular disorders. Prog. Retin. Eye Res. 2018, 67, 30–55. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Mastropasqua, R.; Senatore, A.; Palmieri, M.; Toto, L.; Sadda, S.R.; Mastropasqua, L. Impact of Choriocapillaris Flow on Multifocal Electroretinography in Intermediate Age-Related Macular Degeneration Eyes. Investig. Ophthalmol. Vis. Sci. 2018, 59, AMD25–AMD30. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Souied, E.H.; Freund, K.B.; Querques, G.; Miere, A.; Gal-Or, O.; Sacconi, R.; Sadda, S.R.; Sarraf, D. Reduced choriocapillaris flow in eyes with type 3 neovascularization and age-related macular degeneration. Retina 2018, 38, 1968–1976. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Uji, A.; Sarraf, D.; Sadda, S.R. Alterations in the Choriocapillaris in Intermediate Age-Related Macular Degeneration. Investig. Ophthalmol. Vis. Sci. 2017, 58, 4792–4798. [Google Scholar] [CrossRef] [PubMed]
- Phadikar, P.; Saxena, S.; Ruia, S.; Lai, T.Y.; Meyer, C.H.; Eliott, D. The potential of spectral domain optical coherence tomography imaging based retinal biomarkers. Int. J. Retin. Vitr. 2017, 3, 1. [Google Scholar] [CrossRef] [PubMed]
- Spaide, R.F.; Jaffe, G.J.; Sarraf, D.; Freund, K.B.; Sadda, S.R.; Staurenghi, G.; Waheed, N.K.; Chakravarthy, U.; Rosenfeld, P.J.; Holz, F.G.; et al. Consensus Nomenclature for Reporting Neovascular Age-Related Macular Degeneration Data: Consensus on Neovascular Age-Related Macular Degeneration Nomenclature Study Group. Ophthalmology 2020, 127, 616–636. [Google Scholar] [CrossRef] [PubMed]
- Ferris, F.L., III; Wilkinson, C.P.; Bird, A.; Chakravarthy, U.; Chew, E.; Csaky, K.; Sadda, S.R.; Beckman Initiative for Macular Research Classification Committee. Clinical classification of age-related macular degeneration. Ophthalmology 2013, 120, 844–851. [Google Scholar] [CrossRef] [PubMed]
- Ricardi, F.; Borrelli, E.; Boscia, G.; Gelormini, F.; Marica, V.; Conte, F.; Viggiano, P.; Marolo, P.; Bandello, F.; Reibaldi, M. Relationship of Topographic Distribution of Macular Atrophy Secondary to Neovascular AMD and Reading Performance. Investig. Ophthalmol. Vis. Sci. 2024, 65, 44. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Boscia, G.; Ricardi, F.; Gelormini, F.; Marica, V.; Conte, F.; Ghilardi, A.; Viggiano, P.; Marolo, P.; Bandello, F.; Borrelli, E.; et al. Inter-session repeatability of reading performance measures in patients with neovascular AMD. Retina 2023, 44, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Barresi, C.; Lari, G.; Berni, A.; Battista, M.; Reibaldi, M.; Cascavilla, M.L.; Bandello, F. Capturing the Transition From Intermediate to Neovascular AMD: Longitudinal Inner Retinal Thinning and Factors Associated With Neuronal Loss. Investig. Ophthalmol. Vis. Sci. 2023, 6, 21. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barresi, C.; Borrelli, E.; Fantaguzzi, F.; Grosso, D.; Sacconi, R.; Bandello, F.; Querques, G. Complications Associated with Worse Visual Outcomes in Patients with Exudative Neovascular Age-Related Macular Degeneration. Ophthalmologica 2021, 244, 512–522. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Mastropasqua, L.; Souied, E.; Sadda, S.; Vella, G.; Toto, L.; Miere, A.; Corradetti, G.; Sacconi, R.; Ferro, G.; et al. Longitudinal assessment of type 3 macular neovascularization using 3D volume-rendering OCTA. Can. J. Ophthalmol. 2022, 57, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Grosso, D.; Vella, G.; Sacconi, R.; Battista, M.; Querques, L.; Zucchiatti, I.; Prascina, F.; Bandello, F.; Querques, G. Short-term outcomes of patients with neovascular exudative AMD: The effect of COVID-19 pandemic. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 2621–2628. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grossniklaus, H.E.; Green, W.R. Choroidal neovascularization. Am. J. Ophthalmol. 2004, 137, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Freund, K.B.; Yannuzzi, L.A.; Sorenson, J.A. Age-related macular degeneration and choroidal neovascularization. Am. J. Ophthalmol. 1993, 115, 786–791. [Google Scholar] [CrossRef] [PubMed]
- Nagiel, A.; Sarraf, D.; Sadda, S.R.; Spaide, R.F.; Jung, J.J.; Bhavsar, K.V.; Ameri, H.; Querques, G.; Freund, K.B. Type 3 neovascularization: Evolution, association with pigment epithelial detachment, and treatment response as revealed by spectral domain optical coherence tomography. Retina 2015, 35, 638–647. [Google Scholar] [CrossRef] [PubMed]
- Kuehlewein, L.; Dansingani, K.K.; De Carlo, T.E.; Bonini Filho, M.A.; Iafe, N.A.; Lenis, T.L.; Freund, K.B.; Waheed, N.K.; Duker, J.S.; Sadda, S.R.; et al. Optical Coherence Tomography Angiography of Type 3 Neovascularization Secondary To Age-Related Macular Degeneration. Retina 2015, 35, 2229–2235. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Barresi, C.; Ricardi, F.; Berni, A.; Grosso, D.; Viggiano, P.; Marolo, P.; Introini, U.; Reibaldi, M.; Bandello, F. Distinct Pathways of Macular Atrophy in Type 3 Macular Neovascularization Associated With AMD. Investig. Ophthalmol. Vis. Sci. 2024, 65, 18. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Zerbini, G.; Maestroni, S.; Sacconi, R.; Querques, L.; Zucchiatti, I.; Bandello, F.; Querques, G. Multimodal Imaging to Detect in vivo Responses to Aflibercept Therapy in a Mouse Model of Type 3 Neovascularization. Ophthalmologica 2021, 244, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Sacconi, R.; Battista, M.; Borrelli, E.; Miere, A.; Corbelli, E.; Capuano, V.; Querques, L.; Souied, E.H.; Bandello, F.; Querques, G. OCT-A characterisation of recurrent type 3 macular neovascularisation. Br. J. Ophthalmol. 2021, 105, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Sacconi, R.; Klose, G.; de Sisternes, L.; Bandello, F.; Querques, G. Rotational Three-dimensional OCTA: A Notable New Imaging Tool to Characterize Type 3 Macular Neovascularization. Sci. Rep. 2019, 9, 17053. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Metrangolo, C.; Donati, S.; Mazzola, M.; Fontanel, L.; Messina, W.; D’alterio, G.; Rubino, M.; Radice, P.; Premi, E.; Azzolini, C. OCT Biomarkers in Neovascular Age-Related Macular Degeneration: A Narrative Review. J. Ophthalmol. 2021, 2021, 9994098. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lai, T.T.; Hsieh, Y.T.; Yang, C.M.; Ho, T.C.; Yang, C.H. Biomarkers of optical coherence tomography in evaluating the treatment outcomes of neovascular agerelated macular degeneration: A real-world study. Sci. Rep. 2019, 9, 529. [Google Scholar] [CrossRef]
- Waldstein, S.M.; Simader, C.; Staurenghi, G.; Chong, N.V.; Mitchell, P.; Jaffe, G.J.; Lu, C.; Katz, T.A.; Schmidt-Erfurth, U. Morphology and visual acuity in aflibercept and ranibizumab therapy for neovascular age-related macular degeneration in the VIEW trials. Ophthalmology 2016, 123, 1521–1529. [Google Scholar] [CrossRef]
- Schmidt-Erfurth, U.; Waldstein, S.M.; Deak, G.G.; Kundi, M.; Simader, C. Pigment epithelial detachment followed by retinal cystoid degeneration leads to vision loss in treatment of neovascular age-related macular degeneration. Ophthalmology 2015, 122, 822–832. [Google Scholar] [CrossRef]
- Sadda, S.R.; Tuomi, L.L.; Ding, B.; Fung, A.E.; Hopkins, J.J. Macular atrophy in the HARBOR study for 12 Journal of Ophthalmology neovascular age-related macular degeneration. Ophthalmology 2018, 125, 878–886. [Google Scholar] [CrossRef]
- Ach, T.; Hoeh, A.E.; Ruppenstein, M.; Kretz, F.T.; Dithmar, S. Intravitreal bevacizumab in vascular pigment epithelium detachment as a result of subfoveal occult choroidal neovascularization in age-related macular degeneration. Retina 2010, 30, 1420–1425. [Google Scholar] [CrossRef]
- Borrelli, E.; Barresi, C.; Berni, A.; Viggiano, P.; Reibaldi, M.; Introini, U.; Bandello, F. OCT risk factors for 2-year foveal involvement in non-treated eyes with extrafoveal geographic atrophy and AMD. Graefe’s Arch. Clin. Exp. Ophthalmol. 2024. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Willoughby, A.S.; Ying, G.S.; Toth, C.A.; Maguire, M.G.; Burns, R.E.; Grunwald, J.E.; Ebenezer, D.; Jaffe, G.J. Subretinal hyperreflective material in the comparison of age-related macular degeneration treatments trials. Ophthalmology 2015, 122, 1846.e5–1853.e5. [Google Scholar] [CrossRef]
- Charafeddin, W.; Nittala, M.G.; Oregon, A.; Sadda, S.R. Relationship between subretinal hyperreflective material reflectivity and volume in patients with neovascular agerelated macular degeneration following anti-vascular endothelial growth factor treatment. Ophthalmic Surg. Lasers Imaging Retin. 2015, 46, 523–530. [Google Scholar] [CrossRef]
- Kawashima, Y.; Hata, M.; Oishi, A.; Ooto, S.; Yamashiro, K.; Tamura, H.; Miyata, M.; Uji, A.; Ueda-Arakawa, N. Association of vascular versus avascular subretinal hyperreflective material with aflibercept response in age-related macular degeneration. Am. J. Ophthalmol. 2017, 181, 61–70. [Google Scholar] [CrossRef]
- Kumar, J.B.; Stinnett, S.; Han, J.I.; Jaffe, G.J. Correlation of subretinal hyperreflective material morphology and visual acuity in neovascular age-related macular degeneration. Retina 2020, 40, 845–856. [Google Scholar] [CrossRef]
- Pokroy, R.; Mimouni, M.; Barayev, E.; Segev, F.; Geffen, N.; Nemet, A.Y.; Segal, O. Prognostic value of subretinal hyperreflective material in neovascular age-related macular degeneration treated with bevacizumab. Retina 2018, 38, 1485–1491. [Google Scholar] [CrossRef]
- Woronkowicz, M.; Lightman, S.; Tomkins-Netzer, O. The prognostic value of total macular external limiting membrane and ellipsoid zone damage for clinical outcome in treatment-resistant neovascular age-related macular degeneration. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 2373–2378. [Google Scholar] [CrossRef]
- FCoscas, F.; Coscas, G.; Lupidi, M.; Dirani, A.; Srour, M.; Semoun, O.; Français, C.; Souied, E.H. Restoration of outer retinal layers after aflibercept therapy in exudative AMD: Prognostic value. Investig. Opthalmology Vis. Sci. 2015, 56, 4129–4134. [Google Scholar] [CrossRef]
- Shin, H.J.; Chung, H.; Kim, H.C. Association between foveal microstructure and visual outcome in age-related macular degeneration. Retina 2011, 31, 1627–1636. [Google Scholar] [CrossRef]
- Kang, J.-W.; Lee, H.; Chung, H.; Kim, H.C. Correlation between optical coherence tomographic hyperreflective foci and visual outcomes after intravitreal bevacizumab for macular edema in branch retinal vein occlusion. Graefe’s Arch. Clin. Exp. Ophthalmol. 2014, 252, 1413–1421. [Google Scholar] [CrossRef]
- Omri, S.; Behar-Cohen, F.; De Kozak, Y.; Sennlaub, F.; Verissimo, L.M.; Jonet, L.; Savoldelli, M.; Omri, B.; Crisanti, P. Microglia/macrophages migrate through retinal epithelium barrier by a transcellular route in diabetic retinopathy: Role of PKCζ in the Goto Kakizaki rat model. Am. J. Pathol. 2011, 179, 942–953. [Google Scholar] [CrossRef]
- Bolz, M.; Schmidt-Erfurth, U.; Deak, G.; Mylonas, G.; Kriechbaum, K.; Scholda, C.; Diabetic Retinopathy Research Group Vienna. Optical coherence tomographic hyperreflective foci: A morphologic sign of lipid extravasation in diabetic macular edema. Ophthalmology 2009, 116, 914–920. [Google Scholar] [CrossRef]
- Coscas, G.; De Benedetto, U.; Coscas, F.; Li Calzi, C.I.; Vismara, S.; Roudot-Thoraval, F.; Bandello, F.; Souied, E. Hyperreflective dots: A new spectral-domain optical coherence tomography entity for follow-up and prognosis in exudative age-related macular degeneration. Ophthalmologica 2013, 229, 32–37. [Google Scholar] [CrossRef]
- Wu, J.; Zhang, C.; Yang, Q.; Xie, H.; Zhang, J.; Qiu, Q.; Liu, K.; Luo, D.; Liu, F.; Zhang, J. Imaging Hyperreflective Foci as an Inflammatory Biomarker after Anti-VEGF Treatment in Neovascular Age-Related Macular Degeneration Patients with Optical Coherence Tomography Angiography. BioMed Res. Int. 2021, 2021, 6648191. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, H.; Ji, B.; Chung, H.; Kim, H.C. Correlation between optical coherence tomographic hyperreflective foci and visual outcomes after anti-vegf treatment in neovascular age-related macular degeneration and polypoidal choroidal vasculopathy. Retina 2016, 36, 465–475. [Google Scholar] [CrossRef]
- Abràmoff, M.D.; Lou, Y.; Erginay, A.; Clarida, W.; Amelon, R.; Folk, J.C.; Niemeijer, M. Improved automated detection of diabetic retinopathy on a publicly available dataset through integration of deep learning. Investig. Ophthalmol. Vis. Sci. 2016, 57, 5200–5206. [Google Scholar] [CrossRef] [PubMed]
- Abbas, Q.; Fondon, I.; Sarmiento, A.; Jiménez, S.; Alemany, P. Automatic recognition of severity level for diagnosis of diabetic retinopathy using deep visual features. Med. Biol. Eng. Comput. 2017, 55, 1959–1974. [Google Scholar] [CrossRef]
- Takahashi, H.; Tampo, H.; Arai, Y.; Inoue, Y.; Kawashima, H. Applying artificial intelligence to disease staging: Deep learning for improved staging of diabetic retinopathy. PLoS ONE 2017, 12, e0179790. [Google Scholar] [CrossRef]
- Burlina, P.M.; Joshi, N.; Pekala, M.; Pacheco, K.D.; Freund, D.E.; Bressler, N.M. Automated grading of age- related macular degeneration from color fundus images using deep convolutional neural networks. JAMA Ophthalmol. 2017, 135, 1170–1176. [Google Scholar] [CrossRef]
- Schmidt-Erfurth, U.; Waldstein, S.M.; Klimscha, S.; Sadeghipour, A.; Hu, X.; Gerendas, B.S.; Osborne, A.; Bogunovic, H. Prediction of Individual Disease Conversion in Early AMD Using Artificial Intelligence. Investig. Ophthalmol. Vis. Sci. 2018, 59, 3199–3208. [Google Scholar] [CrossRef] [PubMed]
- Russakoff, D.B.; Lamin, A.; Oakley, J.D.; Dubis, A.M.; Sivaprasad, S. Deep Learning for Prediction of AMD Progression: A Pilot Study. Investig. Ophthalmol. Vis. Sci. 2019, 60, 712–722. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, I.; de Sisternes, L.; Hallak, J.A.; Leng, T.; Osborne, A.; Rosenfeld, P.J.; Gregori, G.; Durbin, M.; Rubin, D. Prediction of age-related macular degeneration disease using a sequential deep learning approach on longitudinal SD-OCT imaging biomarkers. Sci. Rep. 2020, 10, 15434. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yim, J.; Chopra, R.; Spitz, T.; Winkens, J.; Obika, A.; Kelly, C.; Askham, H.; Lukic, M.; Huemer, J.; Fasler, K.; et al. Predicting conversion to wet age-related macular degeneration using deep learning. Nat. Med. 2020, 2, 892–899. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Sahni, J.; Campa, C.; Stangos, A.N.; Raj, A.; Harding, S.P. Computerized assessment of intraretinal and subretinal fluid regions in spectral-domain optical coherence tomography images of the retina. Am. J. Ophthalmol. 2013, 155, 277–286.e1. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Erfurth, U.; Vogl, W.D.; Jampol, L.M.; Bogunović, H. Application of Automated Quantification of Fluid Volumes to Anti-VEGF Therapy of Neovascular Age-Related Macular Degeneration. Ophthalmology 2020, 127, 1211–1219. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.S.; Baughman, D.M.; Lee, A.Y. Deep learning is effective for the classification of OCT images of normal versus Age-related Macular Degeneration. Ophthalmol. Retin. 2017, 1, 322–327. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kermany, D.S.; Goldbaum, M.; Cai, W.; Valentim, C.C.; Liang, H.; Baxter, S.L.; McKeown, A.; Yang, G.; Wu, X.; Yan, F.; et al. Identifying medical diagnoses and treatable diseases by image-based deep learning. Cell 2018, 172, 1122–1131.e9. [Google Scholar] [CrossRef] [PubMed]
- Schlegl, T.; Waldstein, S.M.; Bogunovic, H.; Endstraßer, F.; Sadeghipour, A.; Philip, A.M.; Podkowinski, D.; Gerendas, B.S.; Langs, G.; Schmidt-Erfurth, U. Fully Automated Detection and Quantification of Macular Fluid in OCT Using Deep Learning. Ophthalmology 2018, 125, 549–558. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kang, K.E.; Chung, H.; Kim, H.C. Automated Segmentation of Lesions Including Subretinal Hyperreflective Material in Neovascular Age-related Macular Degeneration. Am. J. Ophthalmol. 2018, 191, 64–75. [Google Scholar] [CrossRef] [PubMed]
- Li, M.X.; Yu, S.Q.; Zhang, W.; Zhou, H.; Xu, X.; Qian, T.W.; Wan, Y.J. Segmentation of retinal fluid based on deep learning: Application of three-dimensional fully convolutional neural networks in optical coherence tomography images. Int. J. Ophthalmol. 2019, 12, 1012–1020. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moraes, G.; Fu, D.J.; Wilson, M.; Khalid, H.; Wagner, S.K.; Korot, E.; Ferraz, D.; Faes, L.; Kelly, C.J.; Spitz, T.; et al. Quantitative Analysis of OCT for Neovascular Age-Related Macular Degeneration Using Deep Learning. Ophthalmology 2021, 128, 693–705. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liefers, B.; Taylor, P.; Alsaedi, A.; Bailey, C.; Balaskas, K.; Dhingra, N.; Egan, C.A.; Rodrigues, F.G.; Gonzalo, C.G.; Heeren, T.F.C.; et al. Quantification of Key Retinal Features in Early and Late Age-Related Macular Degeneration Using Deep Learning. Am. J. Ophthalmol. 2021, 226, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Oakley, J.D.; Iaccarino, G.; Russakoff, D.B.; Battista, M.; Grosso, D.; Borghesan, F.; Barresi, C.; Sacconi, R.; Bandello, F.; et al. Deep-learning based automated quantification of critical optical coherence tomography features in neovascular age-related macular degeneration. Eye 2024, 38, 537–544. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ricardi, F.; Oakley, J.; Russakoff, D.; Boscia, G.; Caselgrandi, P.; Gelormini, F.; Ghilardi, A.; Pintore, G.; Tibaldi, T.; Marolo, P.; et al. Validation of a deep learning model for automatic detection and quantification of five OCT critical retinal features associated with neovascular age-related macular degeneration. Br. J. Ophthalmol. 2024, bjo-2023-324647. [Google Scholar] [CrossRef] [PubMed]
- Bogunovic, H.; Waldstein, S.M.; Schlegl, T.; Langs, G.; Sadeghipour, A.; Liu, X.; Gerendas, B.S.; Osborne, A.; Schmidt-Erfurth, U. Prediction of Anti-VEGF Treatment Requirements in Neovascular AMD Using a Machine Learning Approach. Investig. Ophthalmol. Vis. Sci. 2017, 58, 3240–3248. [Google Scholar] [CrossRef] [PubMed]
- Pfau, M.; Sahu, S.; Rupnow, R.A.; Romond, K.; Millet, D.; Holz, F.G.; Schmitz-Valckenberg, S.; Fleckenstein, M.; Lim, J.I.; de Sisternes, L.; et al. Probabilistic Forecasting of Anti-VEGF Treatment Frequency in Neovascular Age-Related Macular Degeneration. Transl. Vis. Sci. Technol. 2021, 10, 30. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Feng, D.; Chen, X.; Zhou, Z.; Liu, H.; Wang, Y.; Bai, L.; Zhang, S.; Mou, X. A Preliminary Study of Predicting Effectiveness of Anti-VEGF Injection Using OCT Images Based on Deep Learning. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2020, 2020, 5428–5431. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kim, S.; Kim, M.A.; Chung, H.; Kim, H.C. Post-treatment prediction of optical coherence tomography using a conditional generative adversarial network in age-related macular degeneration. Retina 2021, 41, 572–580. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Yang, J.; Zhou, Y.; Wang, W.; Zhao, J.; Yu, W.; Zhang, D.; Ding, D.; Li, X.; Chen, Y. Prediction of OCT images of short-term response to anti-VEGF treatment for neovascular age-related macular degeneration using generative adversarial network. Br. J. Ophthalmol. 2020, 104, 1735–1740. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.; Lee, Y.; Hwang, J.; Kim, C.G.; Kim, J.W.; Yoon, W.T.; Kim, J.H. Prediction of anti-vascular endothelial growth factor agent-specific treatment outcomes in neovascular age-related macular degeneration using a generative adversarial network. Sci. Rep. 2023, 13, 5639. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Erfurth, U.; Bogunovic, H.; Sadeghipour, A.; Schlegl, T.; Langs, G.; Gerendas, B.S.; Osborne, A.; Waldstein, S.M. Machine Learning to Analyze the Prognostic Value of Current Imaging Biomarkers in Neovascular Age-Related Macular Degeneration. Ophthalmol. Retin. 2018, 2, 24–30. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borrelli, E.; Serafino, S.; Ricardi, F.; Coletto, A.; Neri, G.; Olivieri, C.; Ulla, L.; Foti, C.; Marolo, P.; Toro, M.D.; et al. Deep Learning in Neovascular Age-Related Macular Degeneration. Medicina 2024, 60, 990. https://doi.org/10.3390/medicina60060990
Borrelli E, Serafino S, Ricardi F, Coletto A, Neri G, Olivieri C, Ulla L, Foti C, Marolo P, Toro MD, et al. Deep Learning in Neovascular Age-Related Macular Degeneration. Medicina. 2024; 60(6):990. https://doi.org/10.3390/medicina60060990
Chicago/Turabian StyleBorrelli, Enrico, Sonia Serafino, Federico Ricardi, Andrea Coletto, Giovanni Neri, Chiara Olivieri, Lorena Ulla, Claudio Foti, Paola Marolo, Mario Damiano Toro, and et al. 2024. "Deep Learning in Neovascular Age-Related Macular Degeneration" Medicina 60, no. 6: 990. https://doi.org/10.3390/medicina60060990





