Unlocking the Potential: Angiotensin Receptor Neprilysin and Sodium Glucose Co-Transporter 2 Inhibitors for Right Ventricle Dysfunction in Heart Failure
Abstract
:1. Introduction
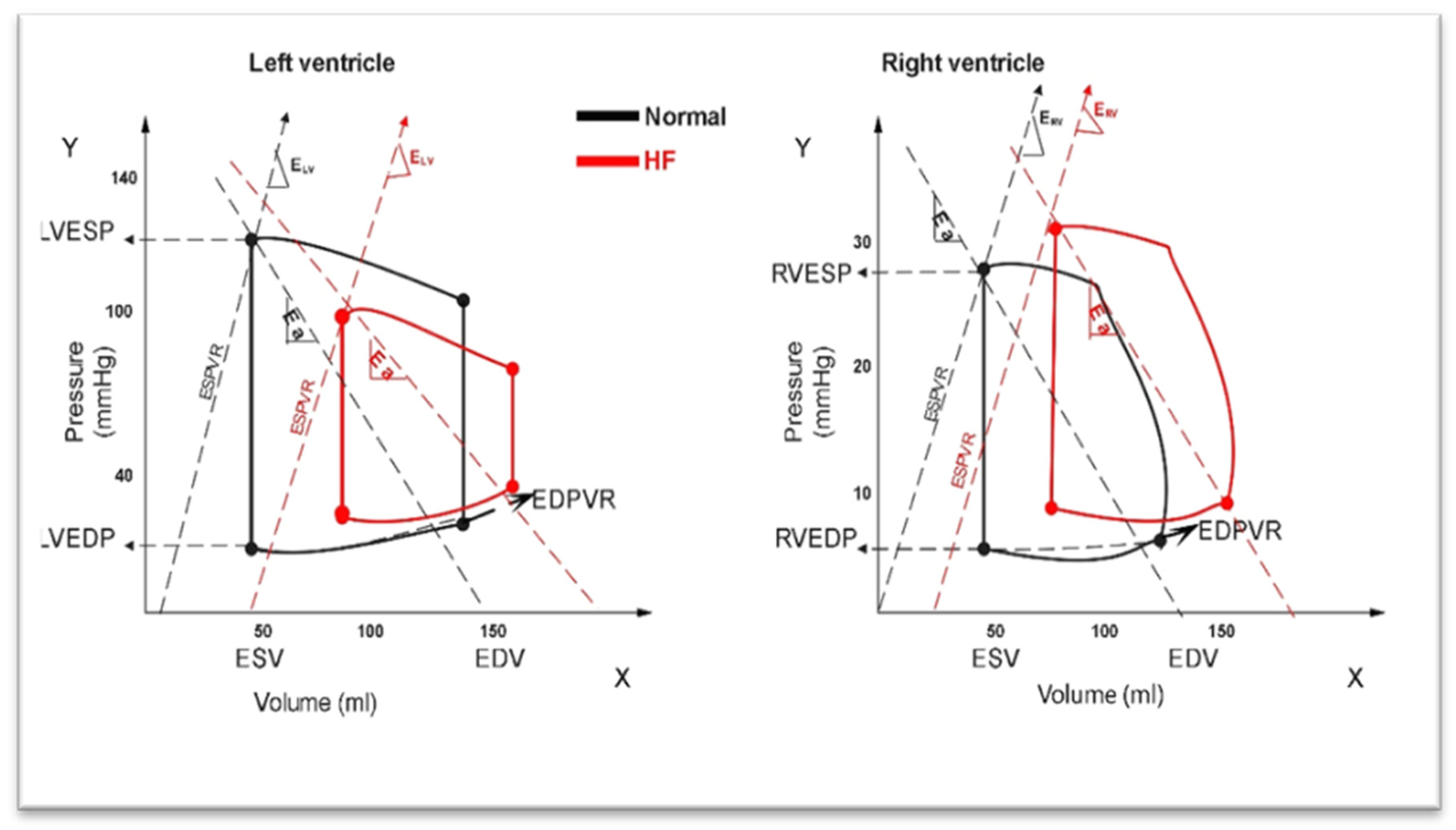
2. Differences between RV and LV in HF
3. Pressure–Volume (PV) Relationship between RV and LV in HF
4. RV Dysfunction with HF and Preserved Ejection Fraction (HFpEF)
5. RV Dysfunction with HF and Reduced Ejection Fraction (HFrEF)
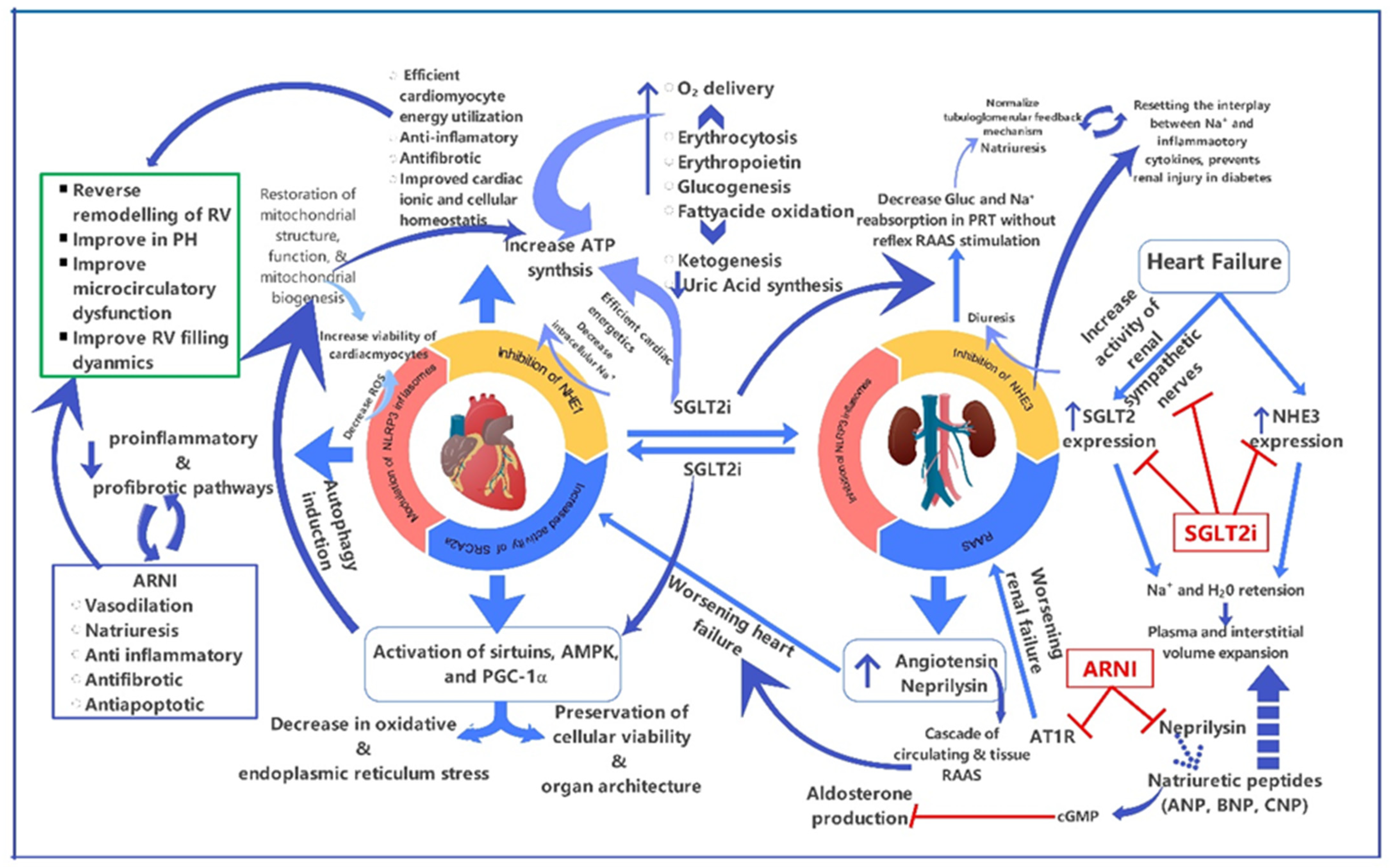
6. Mechanism of Action of ARNIs on RV Function
7. Mechanism of Action of SGLT2is on RV Function
8. Role of ARNIs or SGLT2is in Primary RV Dysfunction
9. Role of ARNIs or SGLT2is in RV Dysfunction Due to Volume Overload
10. Role of ARNIs or SGLT2is in RV Dysfunction Due to Pressure Overload
11. Role of ARNIs or SGLT2is in Systemic RV Dysfunction
12. Role of Combined ARNI and SGLT2i Therapy in RV Dysfunction
13. Conclusions
Funding
Conflicts of Interest
References
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 145, E895–E1032. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. J. Heart Fail. 2024, 26, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.S.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Barone Gibbs, B.; Beaton, A.Z.; Boehme, A.K.; et al. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation 2024, 149, e347–e913. [Google Scholar] [CrossRef]
- De Groote, P.; Millaire, A.; Foucher-Hossein, C.; Nugue, O.; Marchandise, X.; Ducloux, G.; Lablanche, J.-M. Right ventricular ejection fraction is an independent predictor of survival in patients with moderate heart failure. J. Am. Coll. Cardiol. 1998, 32, 948–954. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt, B.; Coats, A.J.S.; Tsutsui, H.; Abdelhamid, C.M.; Adamopoulos, S.; Albert, N.; Anker, S.D.; Atherton, J.; Böhm, M.; Butler, J.; et al. Universal definition and classification of heart failure: A report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. Eur. J. Heart Fail. 2021, 23, 352–380. [Google Scholar] [CrossRef] [PubMed]
- Houston, B.A.; Taichman, D.B.; Brittain, E.L.; Tedford, R.J. Right Ventricular Failure. N. Engl. J. Med. 2023, 388, 1111–1125. [Google Scholar] [CrossRef] [PubMed]
- Dini, F.L.; Carluccio, E.; Simioniuc, A.; Biagioli, P.; Reboldi, G.; Galeotti, G.G.; Raineri, C.; Gargani, L.; Scelsi, L.; Mandoli, G.E.; et al. Right ventricular recovery during follow-up is associated with improved survival in patients with chronic heart failure with reduced ejection fraction. Eur. J. Heart Fail. 2016, 18, 1462–1471. [Google Scholar] [CrossRef] [PubMed]
- Ghio, S.; Gavazzi, A.; Campana, C.; Inserra, C.; Klersy, C.; Sebastiani, R.; Arbustini, E.; Recusani, F.; Tavazzi, L. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J. Am. Coll. Cardiol. 2001, 37, 183–188. [Google Scholar] [CrossRef]
- Arora, S.; Patel, P.; Lahewala, S.; Patel, N.; Patel, N.J.; Thakore, K.; Amin, A.; Tripathi, B.; Kumar, V.; Shah, H.; et al. Etiologies, Trends, and Predictors of 30-Day Readmission in Patients With Heart Failure. Am. J. Cardiol. 2017, 119, 760–769. [Google Scholar] [CrossRef]
- Halliday, B.P.; Owen, R.; Gregson, J.; Vassiliou, V.S.; Chen, X.; Wage, R.; Lota, A.S.; Khalique, Z.; Tayal, U.; Hammersley, D.J.; et al. Myocardial remodelling after withdrawing therapy for heart failure in patients with recovered dilated cardiomyopathy: Insights from TRED-HF. Eur. J. Heart Fail. 2021, 23, 293–301. [Google Scholar] [CrossRef]
- Friedberg, M.K.; Redington, A.N. Right Versus Left Ventricular Failure. Circulation 2014, 129, 1033–1044. [Google Scholar] [CrossRef] [PubMed]
- Taverne, Y.J.H.J.; Sadeghi, A.; Bartelds, B.; Bogers, A.J.J.C.; Merkus, D. Right ventricular phenotype, function, and failure: A journey from evolution to clinics. Heart Fail. Rev. 2021, 26, 1447–1466. [Google Scholar] [CrossRef] [PubMed]
- Mittal, S. Genetic Variation and Outcomes in Right Ventricular Congenital Heart Disease. In Right Ventricular Physiology, Adaptation and Failure in Congenital and Acquired Heart Disease; Friedberg, M., Redington, A., Eds.; Springer: Cham, Switzerland, 2018. [Google Scholar] [CrossRef]
- Reddy, S.; Zhao, M.; Hu, D.Q.; Fajardo, G.; Hu, S.; Ghosh, Z.; Rajagopalan, V.; Wu, J.C.; Bernstein, D. Dynamic microRNA expression during the transition from right ventricular hypertrophy to failure. Physiol Genom. 2012, 44, 562–575. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.Y.; McCloskey, D.T.; Turcato, S.; Swigart, P.M.; Simpson, P.C.; Baker, A.J. Contrasting inotropic responses to alpha1-adrenergic receptor stimulation in left versus right ventricular myocardium. Am. J. Physiol. Heart Circ. Physiol. 2006, 291, H2013–H2017. [Google Scholar] [CrossRef] [PubMed]
- Nagendran, J.; Archer, S.L.; Soliman, D.; Gurtu, V.; Moudgil, R.; Haromy, A.; St. Aubin, C.; Webster, L.; Rebeyka, I.M.; Ross, D.B.; et al. Phosphodiesterase Type 5 Is Highly Expressed in the Hypertrophied Human Right Ventricle, and Acute Inhibition of Phosphodiesterase Type 5 Improves Contractility. Circulation 2007, 116, 238–248. [Google Scholar] [CrossRef]
- Modesti, P.A.; Vanni, S.; Bertolozzi, I.; Cecioni, I.; Lumachi, C.; Perna, A.M.; Boddi, M.; Gensini, G.F. Different Growth Factor Activation in the Right and Left Ventricles in Experimental Volume Overload. Hypertension 2004, 43, 101–108. [Google Scholar] [CrossRef]
- Havlenova, T.; Skaroupkova, P.; Miklovic, M.; Behounek, M.; Chmel, M.; Jarkovska, D.; Sviglerova, J.; Stengl, M.; Kolar, M.; Novotny, J.; et al. Right versus left ventricular remodeling in heart failure due to chronic volume overload. Sci. Rep. 2021, 11, 17136. [Google Scholar] [CrossRef] [PubMed]
- Bosch, L.; Lam, C.S.P.; Gong, L.; Chan, S.P.; Sim, D.; Yeo, D.; Jaufeerally, F.; Leong, K.T.G.; Ong, H.Y.; Ng, T.P.; et al. Right ventricular dysfunction in left-sided heart failure with preserved versus reduced ejection fraction. Eur. J. Heart Fail. 2017, 19, 1664–1671. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.L.; Koestenberger, M.; Rosenkranz, S.; Maron, B.A. Right ventricular dysfunction and long-term risk of death. Cardiovasc. Diagn. Ther. 2020, 10, 1646–1658. [Google Scholar] [CrossRef]
- Ghio, S.; Guazzi, M.; Scardovi, A.B.; Klersy, C.; Clemenza, F.; Carluccio, E.; Temporelli, P.L.; Rossi, A.; Faggiano, P.; Traversi, E.; et al. Different correlates but similar prognostic implications for right ventricular dysfunction in heart failure patients with reduced or preserved ejection fraction. Eur. J. Heart Fail. 2017, 19, 873–879. [Google Scholar] [CrossRef]
- Baandrup, J.D.; Markvardsen, L.H.; Peters, C.D.; Schou, U.K.; Jensen, J.L.; Magnusson, N.E.; Ørntoft, T.F.; Kruhøffer, M.; Simonsen, U. Pressure Load: The Main Factor for Altered Gene Expression in Right Ventricular Hypertrophy in Chronic Hypoxic Rats. PLoS ONE 2011, 6, e15859. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.D.; McMurray, J.J.V.; Anand, I.S.; Ge, J.; Lam, C.S.P.; Maggioni, A.P.; Martinez, F.; Packer, M.; Pfeffer, M.A.; Pieske, B.; et al. Angiotensin–Neprilysin Inhibition in Heart Failure with Preserved Ejection Fraction. N. Engl. J. Med. 2019, 381, 1609–1620. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Inciardi, R.M.; Abanda, M.; Shah, A.M.; Cikes, M.; Claggett, B.; Prasad, N.; Lam, C.S.; Redfield, M.M.; McMurray, J.J.; et al. Abstract 13706: Determinants of Right Ventricular Dysfunction in Patients With Heart Failure With Preserved Ejection Fraction: The PARAGON-HF Trial Experience. Circulation 2023, 148, A13706. [Google Scholar] [CrossRef]
- Frisk, C.; Das, S.; Eriksson, M.J.; Walentinsson, A.; Corbascio, M.; Hage, C.; Kumar, C.; Ekström, M.; Maret, E.; Persson, H.; et al. Cardiac biopsies reveal differences in transcriptomics between left and right ventricle in patients with or without diagnostic signs of heart failure. Sci. Rep. 2024, 14, 5811. [Google Scholar] [CrossRef] [PubMed]
- Anastasiou, V.; Papazoglou, A.S.; Moysidis, D.V.; Daios, S.; Barmpagiannos, K.; Gossios, T.; Efthimiadis, G.K.; Karamitsos, T.; Ziakas, A.; Kamperidis, V. The prognostic impact of right ventricular-pulmonary arterial coupling in heart failure: A systematic review and meta-analysis. Heart Fail. Rev. 2023, 29, 13–26. [Google Scholar] [CrossRef]
- Brockmöller, J.; Ivanoski, S.; Hundack, L.; Blohm, J.-H.; Januszewski, M.; Remppis, B.A.; Burgdorf, C. Clinical and Hemodynamic Improvement in Pulmonary Hypertension After Switching to Sacubitril/Valsartan in Patients With Heart Failure With Preserved Ejection Fraction. J. Cardiovasc. Pharmacol. 2023, 82, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Anker, S.D.; Butler, J.; Filippatos, G.; Ferreira, J.P.; Bocchi, E.; Böhm, M.; Brunner–La Rocca, H.-P.; Choi, D.-J.; Chopra, V.; Chuquiure-Valenzuela, E.; et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N. Engl. J. Med. 2021, 385, 1451–1461. [Google Scholar] [CrossRef] [PubMed]
- Packer, M.; Butler, J.; Zannad, F.; Filippatos, G.; Ferreira, J.P.; Pocock, S.J.; Carson, P.; Anand, I.; Doehner, W.; Haass, M.; et al. Effect of Empagliflozin on Worsening Heart Failure Events in Patients With Heart Failure and Preserved Ejection Fraction: EMPEROR-Preserved Trial. Circulation 2021, 144, 1284–1294. [Google Scholar] [CrossRef]
- Rodríguez, M.A.R.; Alonso, D.; Martín, J.M.; López-Benito, M.L.-B.; Garrote, C.; Olalla-Gómez, C.O.-G.; Iglesias-Garriz, I. Contribution of Right Ventricular Dysfunction to Heart Failure Mortality: A Meta-Analysis. Rev. Cardiovasc. Med. 2012, 13, 62–69. [Google Scholar] [CrossRef]
- Surkova, E.; Kovács, A.; Tokodi, M.; Lakatos, B.K.; Merkely, B.; Muraru, D.; Ruocco, A.; Parati, G.; Badano, L.P. Contraction Patterns of the Right Ventricle Associated with Different Degrees of Left Ventricular Systolic Dysfunction. Circ. Cardiovasc. Imaging 2021, 14, 982–994. [Google Scholar] [CrossRef]
- Tran, J.S.; Havakuk, O.; McLeod, J.M.; Hwang, J.; Kwong, H.Y.; Shavelle, D.; Zile, M.R.; Elkayam, U.; Fong, M.W.; Grazette, L.P. Acute pulmonary pressure change after transition to sacubitril/valsartan in patients with heart failure reduced ejection fraction. ESC Heart Fail. 2021, 8, 1706–1710. [Google Scholar] [CrossRef] [PubMed]
- Lampert, B.C.; Teuteberg, J.J. Right ventricular failure after left ventricular assist devices. J. Heart Lung Transplant. 2015, 34, 1123–1130. [Google Scholar] [CrossRef] [PubMed]
- Damy, T.; Kallvikbacka-Bennett, A.; Goode, K.; Khaleva, O.; Lewinter, C.; Hobkirk, J.; Nikitin, N.P.; Dubois-Randé, J.-L.; Hittinger, L.; Clark, A.L.; et al. Prevalence of, Associations With, and Prognostic Value of Tricuspid Annular Plane Systolic Excursion (TAPSE) Among Out-Patients Referred for the Evaluation of Heart Failure. J. Card. Fail. 2012, 18, 216–225. [Google Scholar] [CrossRef]
- Linde, C.; Ekström, M.; Eriksson, M.J.; Maret, E.; Wallén, H.; Lyngå, P.; Wedén, U.; Cabrera, C.; Löfström, U.; Stenudd, J.; et al. Baseline characteristics of 547 new onset heart failure patients in the PREFERS heart failure study. ESC Heart Fail. 2022, 9, 2125–2138. [Google Scholar] [CrossRef] [PubMed]
- Correale, M.; Mallardi, A.; Mazzeo, P.; Tricarico, L.; Diella, C.; Romano, V.; Ferraretti, A.; Leopizzi, A.; Merolla, G.; Di Biase, M.; et al. Sacubitril/valsartan improves right ventricular function in a real-life population of patients with chronic heart failure: The Daunia Heart Failure Registry. Int. J. Cardiol. Heart Vasc. 2020, 27, 100486. [Google Scholar] [CrossRef] [PubMed]
- Yenerçağ, M.; Arslan, U.; Dereli, S.; Çoksevim, M.; Doğduş, M.; Kaya, A. Effects of angiotensin receptor neprilysin inhibition on pulmonary arterial stiffness in heart failure with reduced ejection fraction. Int. J. Cardiovasc. Imaging 2021, 37, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Mustapic, I.; Bakovic, D.; Susilovic Grabovac, Z.; Borovac, J.A. Impact of SGLT2 Inhibitor Therapy on Right Ventricular Function in Patients with Heart Failure and Reduced Ejection Fraction. J. Clin. Med. 2022, 12, 42. [Google Scholar] [CrossRef]
- Axelsen, J.S.; Nielsen-Kudsk, A.H.; Schwab, J.; Ringgaard, S.; Nielsen-Kudsk, J.E.; De Man, F.S.; Andersen, A.; Andersen, S. Effects of empagliflozin on right ventricular adaptation to pressure overload. Front. Cardiovasc. Med. 2023, 10, 1302265. [Google Scholar] [CrossRef] [PubMed]
- Melenovsky, V.; Hwang, S.-J.; Lin, G.; Redfield, M.M.; Borlaug, B.A. Right heart dysfunction in heart failure with preserved ejection fraction. Eur. Heart J. 2014, 35, 3452–3462. [Google Scholar] [CrossRef]
- D’amato, A.; Prosperi, S.; Severino, P.; Myftari, V.; Francia, A.L.; Cestiè, C.; Pierucci, N.; Marek-Iannucci, S.; Mariani, M.V.; Germanò, R.; et al. Current Approaches to Worsening Heart Failure: Pathophysiological and Molecular Insights. Int. J. Mol. Sci. 2024, 25, 1574. [Google Scholar] [CrossRef]
- Vardeny, O.; Claggett, B.; Packer, M.; Zile, M.R.; Rouleau, J.; Swedberg, K.; Teerlink, J.R.; Desai, A.S.; Lefkowitz, M.; Shi, V.; et al. Efficacy of sacubitril/valsartan vs. enalapril at lower than target doses in heart failure with reduced ejection fraction: The PARADIGM-HF trial. Eur. J. Heart Fail. 2016, 18, 1228–1234. [Google Scholar] [CrossRef] [PubMed]
- Hechter, S.J.; Fredriksen, P.M.; Liu, P.; Veldtman, G.; Merchant, N.; Freeman, M.; Therrien, J.; Benson, L.; Siu, S.; Webb, G. Angiotensin-converting enzyme inhibitors in adults after the Mustard procedure. Am. J. Cardiol. 2001, 87, 660–663. [Google Scholar] [CrossRef] [PubMed]
- Tutarel, O.; Meyer, G.P.; Bertram, H.; Wessel, A.; Schieffer, B.; Westhoff-Bleck, M. Safety and efficiency of chronic ACE inhibition in symptomatic heart failure patients with a systemic right ventricle. Int. J. Cardiol. 2012, 154, 14–16. [Google Scholar] [CrossRef] [PubMed]
- Lester, S.J.; McElhinney, D.B.; Viloria, E.; Reddy, G.P.; Ryan, E.; Tworetzky, W.; Schiller, N.B.; Foster, E. Effects of losartan in patients with a systemically functioning morphologic right ventricle after atrial repair of transposition of the great arteries. Am. J. Cardiol. 2001, 88, 1314–1316. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.L.; Prescott, M.F.; Butler, J.; Felker, G.M.; Maisel, A.S.; McCague, K.; Camacho, A.; Piña, I.L.; Rocha, R.A.; Shah, A.M.; et al. Association of Change in N-Terminal Pro–B-Type Natriuretic Peptide Following Initiation of Sacubitril-Valsartan Treatment With Cardiac Structure and Function in Patients With Heart Failure With Reduced Ejection Fraction. JAMA 2019, 322, 1085–1095. [Google Scholar] [CrossRef] [PubMed]
- Packer, M.; McMurray, J.J.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; Rouleau, J.L.; Shi, V.C.; Solomon, S.D.; Swedberg, K.; et al. Angiotensin receptor neprilysin inhibition compared with enalapril on the risk of clinical progression in surviving patients with heart failure. Circulation 2015, 131, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.P.; Prescott, M.F.; Camacho, A.; Iyer, S.R.; Maisel, A.S.; Felker, G.M.; Butler, J.; Pina, I.L.; Ibrahim, N.E.; Abbas, C.; et al. Atrial Natriuretic Peptide and Treatment With Sacubitril/Valsartan in Heart Failure With Reduced Ejection Fraction. JACC Heart Fail 2021, 9, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Zile, M.R.; Claggett, B.L.; Prescott, M.F.; McMurray, J.J.; Packer, M.; Rouleau, J.L.; Swedberg, K.; Desai, A.S.; Gong, J.; Shi, V.C.; et al. Prognostic Implications of Changes in N-Terminal Pro-B-Type Natriuretic Peptide in Patients With Heart Failure. J. Am. Coll. Cardiol. 2016, 68, 2425–2436. [Google Scholar] [CrossRef] [PubMed]
- Myhre, P.L.; Vaduganathan, M.; Claggett, B.; Packer, M.; Desai, A.S.; Rouleau, J.L.; Zile, M.R.; Swedberg, K.; Lefkowitz, M.; Shi, V.; et al. B-Type Natriuretic Peptide During Treatment With Sacubitril/Valsartan: The PARADIGM-HF Trial. J. Am. Coll. Cardiol. 2019, 73, 1264–1272. [Google Scholar] [CrossRef]
- Pieske, B.; Wachter, R.; Shah, S.J.; Baldridge, A.; Szeczoedy, P.; Ibram, G.; Shi, V.; Zhao, Z.; Cowie, M.R.; Investigators, P.; et al. Effect of Sacubitril/Valsartan vs Standard Medical Therapies on Plasma NT-proBNP Concentration and Submaximal Exercise Capacity in Patients With Heart Failure and Preserved Ejection Fraction: The PARALLAX Randomized Clinical Trial. JAMA 2021, 326, 1919–1929. [Google Scholar] [CrossRef]
- Vives, D.; Farage, S.; Motta, R.; Lopes, A.G.; Caruso-Neves, C. Atrial natriuretic peptides and urodilatin modulate proximal tubule Na(+)-ATPase activity through activation of the NPR-A/cGMP/PKG pathway. Peptides 2010, 31, 903–908. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Du, L.; Qin, X.; Guo, X. Effect of Sacubitril/Valsartan on the Right Ventricular Function and Pulmonary Hypertension in Patients With Heart Failure With Reduced Ejection Fraction: A Systematic Review and Meta-Analysis of Observational Studies. J. Am. Heart Assoc. 2022, 11, e024449. [Google Scholar] [CrossRef]
- Alcidi, G.; Pugliese, R.; Ioannoni, S.; Romano, M.; Palmieri, G.; Tabella, E.; Correale, M.; Di Biase, M.; Brunetti, N.D.; Iacoviello, M. Improvement in Left and Right Ventricular Function after Introduction of SGLT2 Inhibitors in Heart Failure Outpatients with Reduced Ejection Fraction. Clin. Pract. 2023, 13, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- Imamura, T.; Hori, M.; Ueno, H.; Kinugawa, K. Impact of Sacubitril/Valsartan on Right Heart Failure. Int. Heart J. 2021, 62, 932–934. [Google Scholar] [CrossRef]
- Bazgir, F.; Nau, J.; Nakhaei-Rad, S.; Amin, E.; Wolf, M.J.; Saucerman, J.J.; Lorenz, K.; Ahmadian, M.R. The Microenvironment of the Pathogenesis of Cardiac Hypertrophy. Cells 2023, 12, 1780. [Google Scholar] [CrossRef]
- Winter, M.M.; Bouma, B.J.; Groenink, M.; Konings, T.C.; Tijssen, J.G.P.; Van Veldhuisen, D.J.; Mulder, B.J.M. Latest insights in therapeutic options for systemic right ventricular failure: A comparison with left ventricular failure. Heart 2009, 95, 960–963. [Google Scholar] [CrossRef] [PubMed]
- Llucià-Valldeperas, A.; van Wezenbeek, J.; Goumans, M.-J.; de Man, F.S. The battle of new biomarkers for right heart failure in pulmonary hypertension: Is the queen of hearts NT-proBNP defeated at last? Eur. Respir. J. 2021, 57, 2004277. [Google Scholar] [CrossRef]
- Sano, R.; Shinozaki, Y.; Ohta, T. Sodium–glucose cotransporters: Functional properties and pharmaceutical potential. J. Diabetes Investig. 2020, 11, 770–782. [Google Scholar] [CrossRef]
- Quagliariello, V.; De Laurentiis, M.; Rea, D.; Barbieri, A.; Monti, M.G.; Carbone, A.; Paccone, A.; Altucci, L.; Conte, M.; Canale, M.L.; et al. The SGLT-2 inhibitor empagliflozin improves myocardial strain, reduces cardiac fibrosis and pro-inflammatory cytokines in non-diabetic mice treated with doxorubicin. Cardiovasc. Diabetol. 2021, 20, 150. [Google Scholar] [CrossRef]
- Pawlos, A.; Broncel, M.; Woźniak, E.; Gorzelak-Pabiś, P. Neuroprotective Effect of SGLT2 Inhibitors. Molecules 2021, 26, 7213. [Google Scholar] [CrossRef]
- Packer, M. Critical Reanalysis of the Mechanisms Underlying the Cardiorenal Benefits of SGLT2 Inhibitors and Reaffirmation of the Nutrient Deprivation Signaling/Autophagy Hypothesis. Circulation 2022, 146, 1383–1405. [Google Scholar] [CrossRef] [PubMed]
- Zelniker, T.A.; Braunwald, E. Mechanisms of Cardiorenal Effects of Sodium-Glucose Cotransporter 2 Inhibitors. J. Am. Coll. Cardiol. 2020, 75, 422–434. [Google Scholar] [CrossRef]
- Wilcox, C.S. Antihypertensive and Renal Mechanisms of SGLT2 (Sodium-Glucose Linked Transporter 2) Inhibitors. Hypertension 2020, 75, 894–901. [Google Scholar] [CrossRef]
- Schiattarella, G.G.; Rodolico, D.; Hill, J.A. Metabolic inflammation in heart failure with preserved ejection fraction. Cardiovasc. Res. 2021, 117, 423–434. [Google Scholar] [CrossRef]
- Giannattasio, S.; Citarella, A.; Trocchianesi, S.; Filardi, T.; Morano, S.; Lenzi, A.; Ferretti, E.; Crescioli, C. Cell-Target-Specific Anti-Inflammatory Effect of Empagliflozin: In Vitro Evidence in Human Cardiomyocytes. Front. Mol. Biosci. 2022, 9, 879522. [Google Scholar] [CrossRef]
- Benes, J.; Kotrc, M.; Wohlfahrt, P.; Kroupova, K.; Tupy, M.; Kautzner, J.; Melenovsky, V. Right ventricular global dysfunction score: A new concept of right ventricular function assessment in patients with heart failure with reduced ejection fraction (HFrEF). Front. Cardiovasc. Med. 2023, 10, 1194174. [Google Scholar] [CrossRef] [PubMed]
- Iborra-Egea, O.; Santiago-Vacas, E.; Yurista, S.R.; Lupón, J.; Packer, M.; Heymans, S.; Zannad, F.; Butler, J.; Pascual-Figal, D.; Lax, A.; et al. Unraveling the Molecular Mechanism of Action of Empagliflozin in Heart Failure With Reduced Ejection Fraction With or Without Diabetes. JACC Basic Transl. Sci. 2019, 4, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Wei, Y.; Li, D.; Pu, J.; Ding, H.; Zhang, X. Mechanisms of SGLT2 Inhibitors in Heart Failure and Their Clinical Value. J. Cardiovasc. Pharmacol. 2023, 81, 4–14. [Google Scholar] [CrossRef] [PubMed]
- McMurray, J.J.V.; Solomon, S.D.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Anand, I.S.; Bělohlávek, J.; et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N. Engl. J. Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef]
- Nassif, M.E.; Qintar, M.; Windsor, S.L.; Jermyn, R.; Shavelle, D.M.; Tang, F.; Lamba, S.; Bhatt, K.; Brush, J.; Civitello, A.; et al. Empagliflozin Effects on Pulmonary Artery Pressure in Patients With Heart Failure. Circulation 2021, 143, 1673–1686. [Google Scholar] [CrossRef]
- Gorr, M.W.; Sriram, K.; Chinn, A.M.; Muthusamy, A.; Insel, P.A. Transcriptomic profile reveals differences etween the right and left ventricle in normoxia and hypoxia. Ohysiol. Rep. 2020, 8, e14344. [Google Scholar] [CrossRef]
- Alzaabi, M.A.; Abdelsalam, A.; Alhamaadi, M.; Hani, H.B.; Almheiri, A.; Matrooshi, N.A.; Al Zaman, K. Evaluating biomarkers as tools for early detection and prognosis of heart failure: A comprehensive review. Card. Fail. Rev. 2024, 10, e06. [Google Scholar] [CrossRef] [PubMed]
- Salam, M.F.; Gorgis, S.; Basir, M.B. Current and Emerging Strategies for RV Shock Management in the Setting of RV Infarct. JACC. Available online: https://www.acc.org/latest-in-cardiology/articles/2021/11/01/12/41/current-and-emerging-strategies-for-rv-shock-management (accessed on 26 June 2024).
- Mansoor, T.; Khalid, S.N.; Bilal, M.I.; Ijaz, S.H.; Fudim, M.; Greene, S.J.; Warraich, H.J.; Nambi, V.; Virani, S.S.; Fonarow, G.C.; et al. Ongoing and Future Clinical Trials of Pharmacotherapy for Heart Failure. Am. J. Cardiovasc. Drugs 2024. [Google Scholar] [CrossRef] [PubMed]
- Yuriditsky, E.; Chonde, M.; Friedman, O.; Horowitz, J.M. Medical and Mechanical Circulatory Support of the Failing Right Ventricle. Curr. Cardiol. Rep. 2024, 26, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Diaz, J.C.; Duque, M.; Aristizabal, J.; Marin, J.; Niño, C.; Bastidas, O.; Ruiz, L.M.; Matos, C.D.; Hoyos, C.; Hincapie, D.; et al. The Emerging Role of Left Bundle Branch Area Pacing for Cardiac Resynchronisation Therapy. Arrhythmia Electrophysiol. Rev. 2023, 12, e29. [Google Scholar] [CrossRef]
- Lippmann, M.R.; Maron, B.A. The Right Ventricle: From Embryologic Development to RV Failure. Curr. Heart Fail. Rep. 2022, 19, 325–333. [Google Scholar] [CrossRef]
- Chang, P.C.; Lin, S.F.; Chu, Y.; Wo, H.T.; Lee, H.L.; Huang, Y.C.; Wen, M.S.; Chou, C.C. LCZ696 Therapy Reduces Ventricular Tachyarrhythmia Inducibility in a Myocardial Infarction-Induced heart failure rat model. Cardiovasc Ther. 2019, 2019, 6032631. [Google Scholar] [CrossRef]
- Maitz, T.N.; Gupta, R.; Persin, K.; Sundlof, D.W. Utilization of sacubitril-valsartan for right ventricular failure in a patient with arrhythmogenic right ventricular cardiomyopathy. Future Cardiol. 2022, 18, 547–552. [Google Scholar] [CrossRef]
- Zhou, Y.; Rui, S.; Tang, S.; Ju, C. Exploration of Mechanisms of Sacubitril/Valsartan in the Treatment of Cardiac Arrhythmias Using a Network Pharmacology Approach. Front. Cardiovasc. Med. 2022, 9, 829484. [Google Scholar] [CrossRef]
- Yang, Z.; Li, T.; Xian, J.; Chen, J.; Huang, Y.; Zhang, Q.; Lin, X.; Lu, H.; Lin, Y. SGLT2 inhibitor dapagliflozin attenuates cardiac fibrosis and inflammation by reverting the HIF-2α signaling pathway in arrhythmogenic cardiomyopathy. FASEB J. 2022, 36, e22410. [Google Scholar] [CrossRef] [PubMed]
- Qin, T.; Kong, B.; Dai, C.; Xiao, Z.; Fang, J.; Shuai, W.; Huang, H. Protective effects of Dapagliflozin on the vulnerability of ventricular arrhythmia in rats with pulmonary artery hypertension induced by monocrotaline. Bioengineered 2022, 13, 2697–2709. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Liu, T.; Shi, S.; Fan, Z.; Hiram, R.; Xiong, F.; Cui, B.; Su, X.; Chang, R.; Zhang, W.; et al. Dapagliflozin reduces the vulnerability of rats with pulmonary arterial hypertension-induced right heart failure to ventricular arrhythmia by restoring calcium handling. Cardiovasc. Diabetol. 2022, 21, 197. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.; Ebrahimi, R.; Ling, Z.; Meyer, C.; Martinek, M.; Sommer, P.; Futyma, P.; Di Vece, D.; Schratter, A.; Acou, W.-J.; et al. Effect of SGLT-2 inhibitors on arrhythmia events: Insight from an updated secondary analysis of > 80,000 patients (the SGLT2i—Arrhythmias and Sudden Cardiac Death). Cardiovasc. Diabetol. 2024, 23, 78. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Montes, M.; Maccallini, M.; Barge-Caballero, G.; Enriquez-Vazquez, D.; Barge-Caballero, E.; Crespo-Leiro, M.G. Use of SGLT2i in patients with transthyretin amyloid cardiomyopathy: Prevalence and safety in a Spanish prospective cohort. Rev. Esp. Cardiol. 2024, 77, 349–352. [Google Scholar] [CrossRef] [PubMed]
- Lang, F.M.; Teruya, S.; Weinsaft, A.; Cuomo, M.; Santos, A.M.; Nalbandian, A.; Bampatsias, D.; Maurer, M.S. Sodium-glucose cotransporter 2 inhibitors for transthyretin amyloid cardiomyopathy: Analyses of short-term efficacy and safety. Eur. J. Heart Fail. 2024, 26, 938–947. [Google Scholar] [CrossRef]
- Li, N.; Zhou, H. SGLT2 Inhibitors: A Novel Player in the Treatment and Prevention of Diabetic Cardiomyopathy. Drug Des. Dev. Ther. 2020, 14, 4775–4788. [Google Scholar] [CrossRef] [PubMed]
- Patoulias, D.; Katsimardou, A.; Toumpourleka, M.; Papadopoulos, C.; Doumas, M. Time to assess the effects of sodium–glucose co-transporter-2 inhibitors on the ‘forgotten’ right ventricle? ESC Heart Fail. 2019, 7, 334–335. [Google Scholar] [CrossRef] [PubMed]
- Lopez, L.; Cohen, M.S.; Anderson, R.H.; Redington, A.N.; Nykanen, D.G.; Penny, D.J.; Deanfield, J.E.; Eidem, B.W. Unnatural history of the right ventricle in patients with congenitally malformed hearts. Cardiol. Young 2010, 20 (Suppl. 3), 107–112. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, M.; Chen, Y.; Chen, X.; Song, W.; Zhu, L.; Liu, L.; Gong, X.; Zhang, Y.; Xu, Z. Does sacubitril/valsartan work in children with heart failure?—A pilot study. Front. Cardiovasc. Med. 2023, 10, 1274990. [Google Scholar] [CrossRef]
- Stout, K.K.; Broberg, C.S.; Book, W.M.; Cecchin, F.; Chen, J.M.; Dimopoulos, K.; Everitt, M.D.; Gatzoulis, M.; Harris, L.; Hsu, D.T.; et al. Chronic Heart Failure in Congenital Heart Disease. Circulation 2016, 133, 770–801. [Google Scholar] [CrossRef] [PubMed]
- Thandavarayan, R.A.; Chitturi, K.R.; Guha, A. Pathophysiology of Acute and Chronic Right Heart Failure. Cardiol. Clin. 2020, 38, 149–160. [Google Scholar] [CrossRef]
- Ciepłucha, A.; Trojnarska, O.; Kociemba, A.; Łanocha, M.; Barczynski, M.; Rozmiarek, S.; Kramer, L.; Pyda, M. Clinical aspects of myocardial fibrosis in adults with Ebstein’s anomaly. Heart Vessels 2018, 33, 1076–1085. [Google Scholar] [CrossRef] [PubMed]
- Polito, M.V.; Silverio, A.; Rispoli, A.; Vitulano, G.; Auria, F.D.; De Angelis, E.; Loria, F.; Gigantino, A.; Bonadies, D.; Citro, R.; et al. Clinical and echocardiographic benefit of Sacubitril/Valsartan in a real-world population with HF with reduced ejection fraction. Sci. Rep. 2020, 10, 6665. [Google Scholar] [CrossRef] [PubMed]
- Fusco, F.; Scognamiglio, G.; Sorice, D.; Abbate, M.; Altobelli, I.; Sarubbi, B. Biventricular performance in adults with a systemic right ventricle: New insights from myocardial work analysis. Int. J. Cardiovasc. Imaging 2024, 40, 1067–1079. [Google Scholar] [CrossRef]
- Agasthi, P.; Van Houten, H.K.; Yao, X.; Jain, C.C.; Egbe, A.; Warnes, C.A.; Miranda, W.R.; Dunlay, S.M.; Stephens, E.H.; Johnson, J.N.; et al. Mortality and Morbidity of Heart Failure Hospitalization in Adult Patients With Congenital Heart Disease. J. Am. Heart Assoc. 2023, 12, e030649. [Google Scholar] [CrossRef]
- Fusco, F.; Scognamiglio, G.; Abbate, M.; Merola, A.; Grimaldi, N.; Ciriello, G.D.; Sarubbi, B. Dapagliflozin in Patients With a Failing Systemic Right Ventricle: Results From the DAPA-SERVE Trial. JACC Heart Fail. 2024, 12, 789–791. [Google Scholar] [CrossRef]
- Joki, Y.; Konishi, H.; Takasu, K.; Minamino, T. Tofogliflozin, a sodium-glucose cotransporter 2 inhibitor, improves pulmonary vascular remodeling due to left heart disease in mice. J. Cardiol. 2023, 81, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Konstam, M.A.; Kiernan, M.S.; Bernstein, D.; Bozkurt, B.; Jacob, M.; Kapur, N.K.; Kociol, R.D.; Lewis, E.F.; Mehra, M.R.; Pagani, F.D.; et al. Evaluation and Management of Right-Sided Heart Failure: A Scientific Statement From the American Heart Association. Circulation 2018, 137, e578–e622. [Google Scholar] [CrossRef]
- Clements, R.T.; Vang, A.; Fernandez-Nicolas, A.; Kue, N.R.; Mancini, T.J.; Morrison, A.R.; Mallem, K.; McCullough, D.J.; Choudhary, G. Treatment of Pulmonary Hypertension With Angiotensin II Receptor Blocker and Neprilysin Inhibitor Sacubitril/Valsartan. Circ. Heart Fail. 2019, 12, e005819. [Google Scholar] [CrossRef]
- Jariwala, P.; Pramod, G. Impact of SGLT2 Inhibitor Therapy, EMPAgliflozin on RIGHT Ventricular Function in Patients with Right Heart Failure and Severe Pulmonary Hypertension in Chronic Pulmonary Disorders (EMPA-RIGHT Study). Indian Heart J. 2023, 75, S11. [Google Scholar] [CrossRef]
- Sarak, B.; Verma, S.; David Mazer, C.; Teoh, H.; Quan, A.; Gilbert, R.E.; Goodman, S.G.; Bami, K.; Coelho-Filho, O.R.; Ahooja, V.; et al. Impact of empagliflozin on right ventricular parameters and function among patients with type 2 diabetes. Cardiovasc. Diabetol. 2021, 20, 200. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.H.; Chen, J.; Chen, F.D.; Ruan, H.Y.; Zhang, W.; Zhou, Y.L.; Wang, Q.Q.; Xu, X.L.; Feng, K.F.; Guo, J.Z.; et al. Evaluating the efficacy and safety of oral triple sequential combination therapy for treating patients with pulmonary arterial hypertension: A multicenter retrospective study. Pulm. Circ. 2024, 14, e12351. [Google Scholar] [CrossRef] [PubMed]
- Chaumais, M.-C.; Djessas, M.R.A.; Thuillet, R.; Cumont, A.; Tu, L.; Hebert, G.; Gaignard, P.; Huertas, A.; Savale, L.; Humbert, M.; et al. Additive protective effects of sacubitril/valsartan and bosentan on vascular remodelling in experimental pulmonary hypertension. Cardiovasc. Res. 2021, 117, 1391–1401. [Google Scholar] [CrossRef] [PubMed]
- Connelly, K.A.; Wu, E.; Visram, A.; Friedberg, M.K.; Batchu, S.N.; Yerra, V.G.; Thai, K.; Nghiem, L.; Zhang, Y.; Kabir, G.; et al. The SGLT2i Dapagliflozin Reduces RV Mass Independent of Changes in RV Pressure Induced by Pulmonary Artery Banding. Cardiovasc. Drugs Ther. 2022, 38, 57–68. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, B.; Luu, A.Z.; Luu, V.Z.; Kabir, M.G.; Pan, Y.; Teoh, H.; Quan, A.; Sabongui, S.; Al-Omran, M.; Bhatt, D.L.; et al. The SGLT2 inhibitor empagliflozin reduces mortality and prevents progression in experimental pulmonary hypertension. Biochem. Biophys. Res. Commun. 2020, 524, 50–56. [Google Scholar] [CrossRef]
- Andersen, S.; Axelsen, J.B.; Ringgaard, S.; Nyengaard, J.R.; Hyldebrandt, J.A.; Bogaard, H.J.; de Man, F.S.; Nielsen-Kudsk, J.E.; Andersen, A. Effects of combined angiotensin II receptor antagonism and neprilysin inhibition in experimental pulmonary hypertension and right ventricular failure. Int. J. Cardiol. 2019, 293, 203–210. [Google Scholar] [CrossRef]
- Liu, S.; Wang, Y.; Lu, S.; Hu, J.; Zeng, X.; Liu, W.; Wang, Y.; Wang, Z. Sacubitril/valsartan treatment relieved the progression of established pulmonary hypertension in rat model and its mechanism. Life Sci. 2021, 266, 118877. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Ma, Y.-R.; Chang, Y.-E.; Duo, D.-L.; Duan, K.-K.; Zhao, N.; Cui, W.-L.; Huan, Z.-L.; Wang, Y.-F. Preventive effect of LCZ696 on hypoxic pulmonary hypertension in rats via regulating the PI3K/AKT signaling pathway. Pulm. Pharmacol. Ther. 2023, 82, 102229. [Google Scholar] [CrossRef]
- Miranda, W.R.; Jain, C.C.; Egbe, A.C.; Reddy, Y.N.; Dearani, J.A.; Hagler, D.J.; Connolly, H.M. Hemodynamics in Adults with Systemic Right Ventricles: Differences Between Congenitally Corrected and Complete Transposition of the Great Arteries. Pediatr. Cardiol. 2024. [Google Scholar] [CrossRef]
- Ladouceur, M.; Segura de la Cal, T.; Gaye, B.; Valentin, E.; Ly, R.; Iserin, L.; Legendre, A.; Mousseaux, E.; Li, W.; Rafiq, I.; et al. Effect of medical treatment on heart failure incidence in patients with a systemic right ventricle. Heart 2021, 107, 1384–1389. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Candales, A.; Norgard, N.B. Right here and right now: Time to incorporate measuring right ventricular function when assessing left heart failure clinical outcomes. J. Card. Fail. 2022, 28, 1741–1742. [Google Scholar] [CrossRef] [PubMed]
- Chaix, M.-A.; Dore, A.; Mondésert, B.; Mongeon, F.-P.; Roy, V.; Guertin, M.-C.; White, M.; Ibrahim, R.; O’Meara, E.; Rouleau, J.-L.; et al. Design of the Prospective Comparison of Angiotensin Receptor-Neprilysin Inhibitor Versus Placebo in Patients With Congenital Systemic Right Ventricle Heart Failure (PARACYS-RV) Trial. CJC Open 2023, 5, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Andi, K.; Abozied, O.; Miranda, W.R.; Anderson, J.H.; Connolly, H.M.; Jain, C.C.; Burchill, L.J.; Egbe, A.C. Clinical benefits of angiotensin receptor-Neprilysin inhibitor in adults with congenital heart disease. Int. J. Cardiol. 2023, 387, 131152. [Google Scholar] [CrossRef] [PubMed]
- Appadurai, V.; Thoreau, J.; Malpas, T.; Nicolae, M. Sacubitril/Valsartan in Adult Congenital Heart Disease Patients With Chronic Heart Failure—A Single Centre Case Series and Call for an International Registry. Heart Lung Circ. 2020, 29, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Ephrem, G.; McCollum, J.C.; Green-Hess, D.; Guglin, M.E.; Sawada, S.G.; Rao, R.A. Subjective and Objective Impact of Angiotensin Receptor-Neprilysin Inhibitors on Systemic Right Ventricle Patients. Heart Lung Circ. 2022, 31, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Fusco, F.; Scognamiglio, G.; Merola, A.; Iannuzzi, A.; Palma, M.; Grimaldi, N.; Sarubbi, B. Safety and Efficacy of Sacubitril/Valsartan in Patients With a Failing Systemic Right Ventricle: A Prospective Single-Center Study. Circ. Heart Fail. 2023, 16, e009848. [Google Scholar] [CrossRef] [PubMed]
- Lluri, G.; Lin, J.; Reardon, L.; Miner, P.; Whalen, K.; Aboulhosn, J. Early Experience With Sacubitril/Valsartan in Adult Patients With Congenital Heart Disease. World J. Pediatr. Congenit. Heart Surg. 2019, 10, 292–295. [Google Scholar] [CrossRef]
- Maurer, S.J.; Pujol Salvador, C.; Schiele, S.; Hager, A.; Ewert, P.; Tutarel, O. Sacubitril/valsartan for heart failure in adults with complex congenital heart disease. Int. J. Cardiol. 2020, 300, 137–140. [Google Scholar] [CrossRef]
- Nederend, M.; Kies, P.; Regeer, M.V.; Vliegen, H.W.; Mertens, B.J.; Robbers-Visser, D.; Bouma, B.J.; Tops, L.F.; Schalij, M.J.; Jongbloed, M.R.M.; et al. Tolerability and beneficial effects of sacubitril/valsartan on systemic right ventricular failure. Heart 2023, 109, 1525–1532. [Google Scholar] [CrossRef]
- Yan, L.; Loh, J.K.; Tan, J.L. Sacubitril/valsartan for heart failure in patients with complex adult congenital heart disease—Experience from a tertiary centre in Singapore. Int. J. Cardiol. Congenit. Heart Dis. 2021, 6, 100268. [Google Scholar] [CrossRef]
- Zandstra, T.E.; Nederend, M.; Jongbloed, M.R.M.; Kies, P.; Vliegen, H.W.; Bouma, B.J.; Tops, L.F.; Schalij, M.J.; Egorova, A.D. Sacubitril/valsartan in the treatment of systemic right ventricular failure. Heart 2021, 107, 1725–1730. [Google Scholar] [CrossRef]
- Neijenhuis, R.M.L.; MacDonald, S.T.; Zemrak, F.; Mertens, B.J.A.; Dinsdale, A.; Hunter, A.; Walker, N.L.; Swan, L.; Reddy, S.; Rotmans, J.I.; et al. Effect of Sodium-Glucose Cotransporter 2 Inhibitors in Adults With Congenital Heart Disease. J. Am. Coll. Cardiol. 2024, 83, 1403–1414. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Maitz, T.; Egeler, D.; Mehta, A.; Nyaeme, M.; Hajra, A.; Goel, A.; Sreenivasan, J.; Patel, N.; Aronow, W.S. SGLT2 inhibitors in hypertension: Role beyond diabetes and heart failure. Trends Cardiovasc. Med. 2023, 33, 479–486. [Google Scholar] [CrossRef]
- Egorova, A.D.; Nederend, M.; Tops, L.F.; Vliegen, H.W.; Jongbloed, M.R.M.; Kies, P. The first experience with sodium-glucose cotransporter 2 inhibitor for the treatment of systemic right ventricular failure. ESC Heart Fail. 2022, 9, 2007–2012. [Google Scholar] [CrossRef]
- Muneuchi, J.; Sugitani, Y.; Kobayashi, M.; Ezaki, H.; Yamada, H.; Watanabe, M. Feasibility and Safety of Sodium Glucose Cotransporter-2 Inhibitors in Adults with Heart Failure after the Fontan Procedure. Case Rep. Cardiol. 2022, 2022, 5243594. [Google Scholar] [CrossRef] [PubMed]
- Kheiwa, A.; Ssembajjwe, B.; Chatta, P.; Nageotte, S.; Abramov, D. Safety of SGLT-2 inhibitors in the management of heart failure in the adult congenital heart disease patient population. Int. J. Cardiol. Congenit. Heart Dis. 2024, 15, 100495. [Google Scholar] [CrossRef]
- Saef, J.; Sundaravel, S.; Ortega-Legaspi, J.; Vaikunth, S. Safety and Treatment Experience With Sodium/glucose Cotransporter-2 Inhibitors in Adult Patients With Congenital Heart Disease. J. Card. Fail. 2023, 29, 974–975. [Google Scholar] [CrossRef] [PubMed]
- Karnakoti, S.; Andi, K.; Miranda, W.R.; Jain, C.C.; Burchill, L.J.; Jokhadar, M.; Connolly, H.M.; Egbe, A.C. Outcomes of Sodium-Glucose Cotransporter 2 Inhibitor Use in Adults With Congenital Heart Disease. CJC Pediatr. Congenit. Heart Dis. 2024, 3, 115–116. [Google Scholar] [CrossRef]
- Lin, Y.; Zhang, H.; Zhao, S.; Chen, L.; Li, J.; Wang, X.; Tian, W. The Efficacy and Safety of the Combined Therapy of Sodium-Glucose Co-Transporter-2 Inhibitors and Angiotensin Receptor-Neprilysin Inhibitor in Patients With Heart Failure With Reduced Ejection Fraction: A Meta-Analysis of the EMPEROR-Reduced and DAPA-HF Sub-Analysis. Front. Cardiovasc. Med. 2022, 9, 882089. [Google Scholar] [CrossRef]
- Mo, X.; Lu, P.; Yang, X. Efficacy of sacubitril-valsartan and SGLT2 inhibitors in heart failure with reduced ejection fraction: A systematic review and meta-analysis. Clin. Cardiol. 2023, 46, 1137–1145. [Google Scholar] [CrossRef] [PubMed]
- Tsai, M.-L.; Lin, Y.; Lin, M.-S.; Tsai, T.-H.; Yang, N.-I.; Wang, C.-Y.; Hsieh, I.C.; Hung, M.-J.; Chen, T.-H. Comparing angiotensin receptor–neprilysin inhibitors with sodium–glucose cotransporter 2 inhibitors for heart failure with diabetes mellitus. Diabetol. Metab. Syndr. 2023, 15, 110. [Google Scholar] [CrossRef] [PubMed]
- Diaz Acevedo, J.; Castro, A.; Moreno, P.M. Hierarchical ranking of novel therapies combinations in heart failure with reduced ejection fraction: Network meta-analysis. JACC Basic Transl. Sci. 2022, 79, 337. [Google Scholar] [CrossRef]
| Authors | Study | What the Study Entails |
|---|---|---|
| Salam et al. [75] | RV Shock Management | Strategies for managing RV shock, particularly in the setting of RV infarct |
| Mansoor et al. [76] | Pharmacotherapy for HF | Trials looking at novel medications, as well as currently approved drugs |
| Yuriditsky et al. [77] | Medical Optimization of Acute RV Failure | Tailored volume administration, ideal vasopressor selection, inotropes to restore contractility, and pulmonary vasodilators to improve afterload |
| Diaz JC et al. [78] | Left Bundle Branch Area Pacing (LBBAP) | Investigation of LBBAP in the context of RV depolarization provided by the right bundle branch |
| Lippman et al. [79] | Pathogenesis of RV Dysfunction | New insights into the role of fibrosis, inflammation, myocyte contraction, and mitochondrial dynamics in RV dysfunction |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Das, B.B. Unlocking the Potential: Angiotensin Receptor Neprilysin and Sodium Glucose Co-Transporter 2 Inhibitors for Right Ventricle Dysfunction in Heart Failure. Medicina 2024, 60, 1112. https://doi.org/10.3390/medicina60071112
Das BB. Unlocking the Potential: Angiotensin Receptor Neprilysin and Sodium Glucose Co-Transporter 2 Inhibitors for Right Ventricle Dysfunction in Heart Failure. Medicina. 2024; 60(7):1112. https://doi.org/10.3390/medicina60071112
Chicago/Turabian StyleDas, Bibhuti B. 2024. "Unlocking the Potential: Angiotensin Receptor Neprilysin and Sodium Glucose Co-Transporter 2 Inhibitors for Right Ventricle Dysfunction in Heart Failure" Medicina 60, no. 7: 1112. https://doi.org/10.3390/medicina60071112
APA StyleDas, B. B. (2024). Unlocking the Potential: Angiotensin Receptor Neprilysin and Sodium Glucose Co-Transporter 2 Inhibitors for Right Ventricle Dysfunction in Heart Failure. Medicina, 60(7), 1112. https://doi.org/10.3390/medicina60071112






