Challenges and Advances in Interventional Cardiology for Coronary Artery Disease Management
Abstract
:1. Introduction
2. Acute Coronary Syndrome
3. STEMI Networks
4. Stable Coronary Artery Disease
5. Role of Invasive Imaging in CAD Revascularization
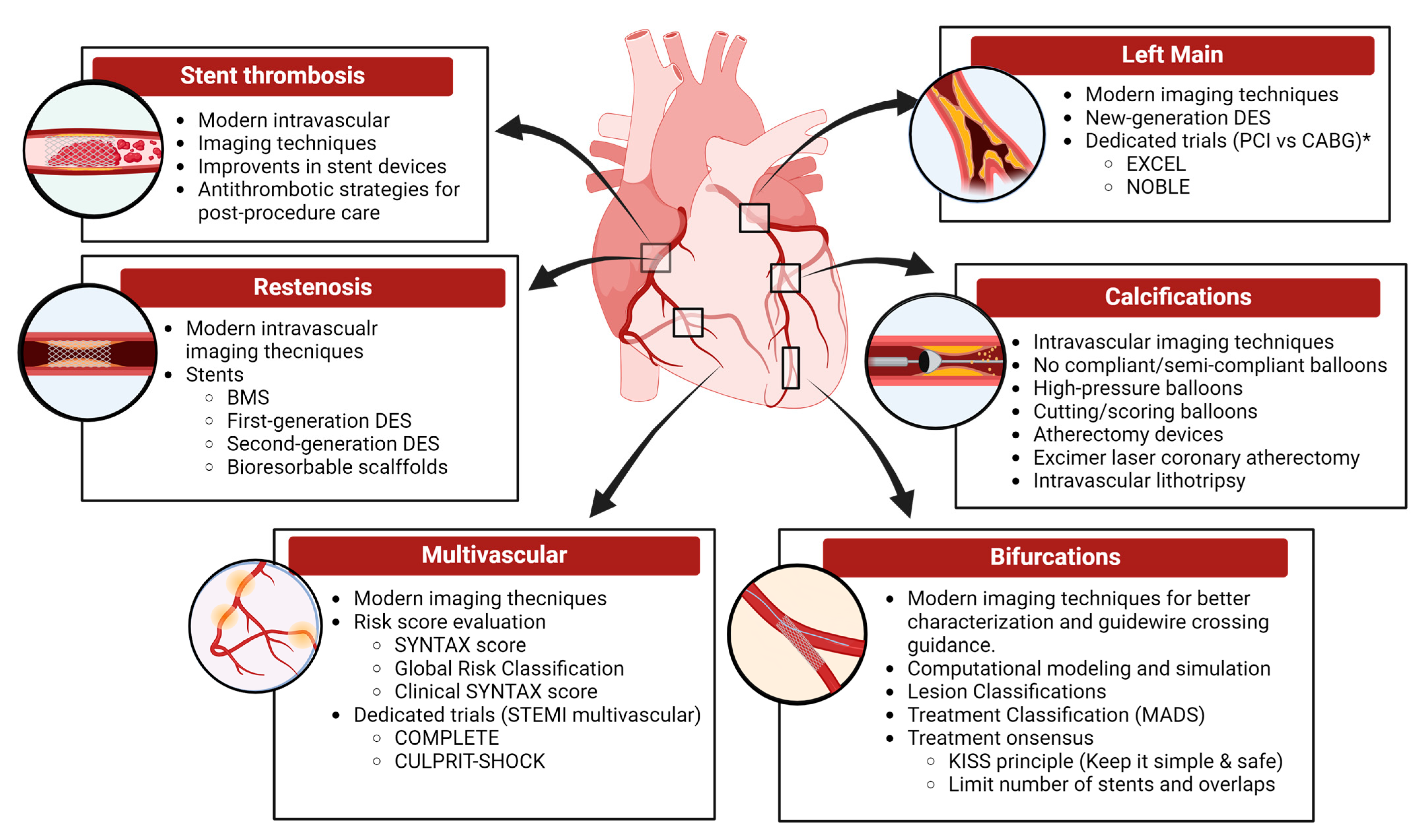
6. Restenosis
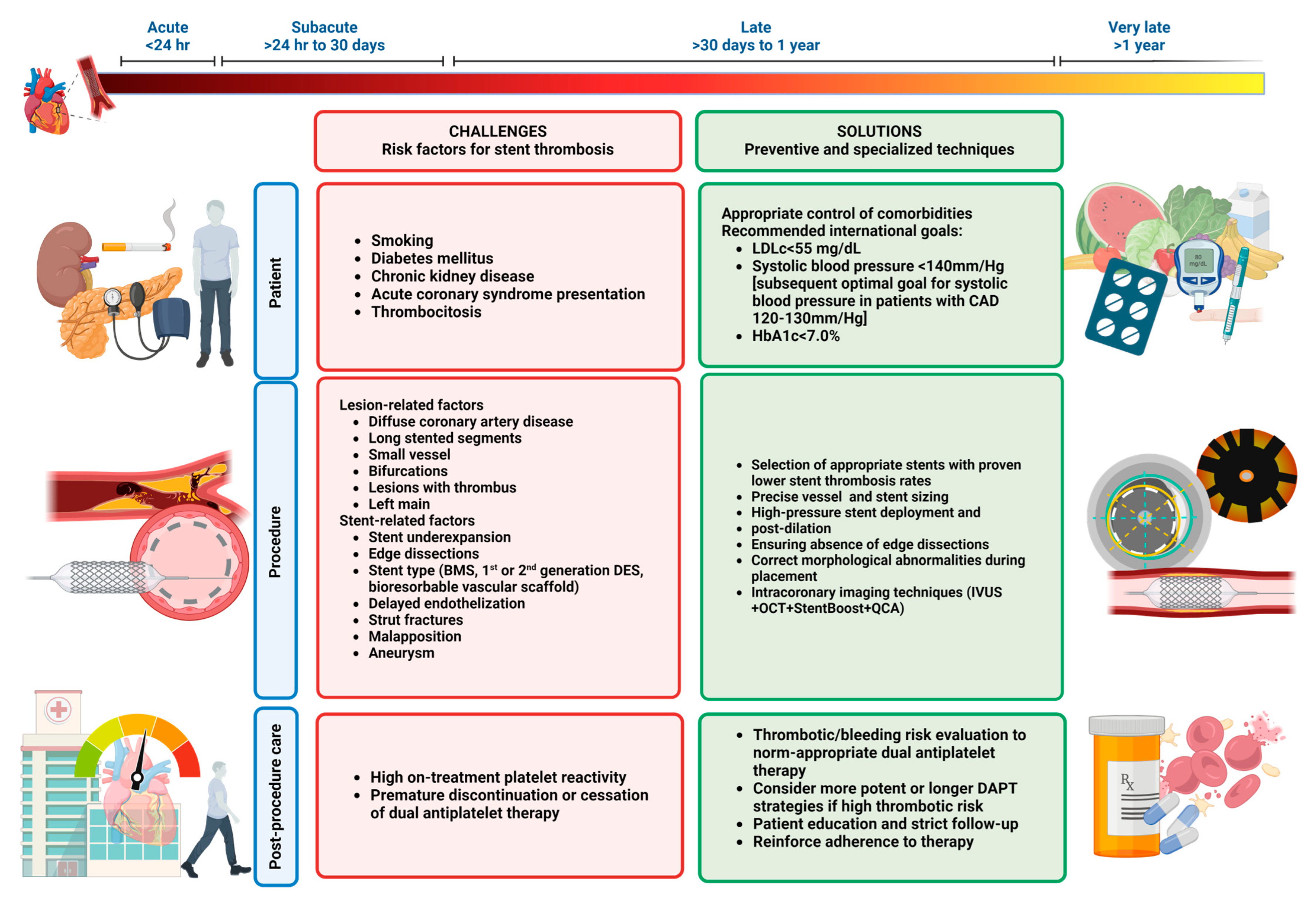
7. Stent Thrombosis
- Stent underexpansion: This is a common mechanism of ST; it can occur due to a stiff arterial segment or an undersized stent. It can be confirmed by IVUS or OCT and resolved with the use of a high-pressure balloon. If a high-calcium burden is detected, the use of rotational atherectomy can improve the stent deployment.
- Stent malposition: This occurs when there is a lack of contact between the struts and the intimal vascular wall of the vessel. It can be detected using imaging techniques (a space filled with blood is seen between the struts and vascular wall) and resolved with the stent post-dilatation.
- Stent edge dissections: This involves the mechanical disruption of the endothelium with blood extravasation into subendothelial planes [39]. Significant edge dissections (lumen narrowing < 4 mm2 or dissection angle > 60°) are associated with early ST. It can be detected with IVUS or OCT and treated with implantation of a second stent [14].
- Stent fracture: Tortuous or angled arteries, stent type, long stents, and/or overlapping stents are associated with the risk of stent fracture, which can promote ST. IVUS, OCT, StentBoost, and multislice CT scans can be used to diagnose. A thorough follow-up is required, and in some cases, re-stenting can be considered [40].
- Evaginations: Outward bulging of the luminal vessel contour between the stent struts. The use of intravascular imaging to ensure precise sizing can help prevent this issue.
8. PCI in Multivessel Disease
9. Coronary Bifurcation Lesions
10. Left Main Coronary Artery
11. Calcified Coronary Lesions
12. Research Opportunities and Future Perspectives
13. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Mariachiara Di Cesare, H.B.; Gaziano, T.; Hadeed, L.; Kabudula, C.; McGhie, D.V.; Mwangi, J.; Pervan, B.; Perel, P.; Piñeiro, D.; Taylor, S.; et al. World Heart Report 2023: Confronting the World’s Number One Killer; World Heart Federation: Geneva, Switzerland, 2023. [Google Scholar]
- Gu, D.; Qu, J.; Zhang, H.; Zheng, Z. Revascularization for Coronary Artery Disease: Principle and Challenges. Adv. Exp. Med. Biol. 2020, 1177, 75–100. [Google Scholar] [CrossRef] [PubMed]
- Borrayo-Sánchez, G.; Alcocer-Gamba, M.A.; Araiza-Garaygordobil, D.; Arias-Mendoza, A.; Aubanel-Riedel, P.; Cortés-Lawrenz, J.; González-Juanatey, J.R.; Gutiérrez-Fajardo, P.; Martín-Hernández, P.; Martínez-Ramírez, L.; et al. Interinstitutional clinical practice guidelines for the treatment of acute myocardial infarction. Gac. Med. Mex. 2020, 156, 559–569. [Google Scholar] [CrossRef] [PubMed]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.-A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes: Developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). Eur. Heart J. Acute Cardiovasc. Care 2024, 13, 55–161. [Google Scholar] [CrossRef] [PubMed]
- Candiello, A.; Alexander, T.; Delport, R.; Toth, G.G.; Ong, P.; Snyders, A.; Belardi, J.A.; Lee, M.K.Y.; Pereira, H.; Mohamed, A.; et al. How to set up regional STEMI networks: A “Stent—Save a life!” initiative. EuroIntervention 2022, 17, 1313–1317. [Google Scholar] [CrossRef] [PubMed]
- Kaifoszova, Z.; Kala, P.; Alexander, T.; Zhang, Y.; Huo, Y.; Snyders, A.; Delport, R.; Alcocer-Gamba, M.A.; Gavidia, L.M. Stent for Life Initiative: Leading example in building STEMI systems of care in emerging countries. EuroIntervention 2014, 10 (Suppl. T), T87–T95. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.; Grines, C.L.; Botelho, R.; Fernandez, F.; Cade, J.; Dusilek, C.; Prudente, M.; Cavalcanti, R.; Campos, C.; Alcocer Gamba, M. STEMI telemedicine for 100 million lives. Catheter. Cardiovasc. Interv. 2021, 98, 1066–1071. [Google Scholar] [CrossRef]
- Writing Committee Members; Virani Salim, S.; Newby, L.K.; Arnold Suzanne, V.; Bittner, V.; Brewer LaPrincess, C.; Demeter Susan, H.; Dixon Dave, L.; Fearon William, F.; Hess, B.; et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients with Chronic Coronary Disease. J. Am. Coll. Cardiol. 2023, 82, 833–955. [Google Scholar] [CrossRef]
- Bertolone, D.T.; Gallinoro, E.; Esposito, G.; Paolisso, P.; Bermpeis, K.; De Colle, C.; Fabbricatore, D.; Mileva, N.; Valeriano, C.; Munhoz, D.; et al. Contemporary Management of Stable Coronary Artery Disease. High Blood Press. Cardiovasc. Prev. 2022, 29, 207–219. [Google Scholar] [CrossRef]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2019, 41, 407–477. [Google Scholar] [CrossRef]
- Vidal-Perez, R.; Bouzas-Mosquera, A.; Peteiro, J.; Vazquez-Rodriguez, J.M. ISCHEMIA trial: How to apply the results to clinical practice. World J. Cardiol. 2021, 13, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Maron, D.J.; Hochman, J.S.; Reynolds, H.R.; Bangalore, S.; O’Brien, S.M.; Boden, W.E.; Chaitman, B.R.; Senior, R.; López-Sendón, J.; Alexander, K.P.; et al. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N. Engl. J. Med. 2020, 382, 1395–1407. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-J.; Ahn, J.-M. Intravascular Ultrasound for the Assessment of Coronary Lesion Severity and Optimization of Percutaneous Coronary Interventions. Interv. Cardiol. Clin. 2015, 4, 383–395. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Choi, K.H.; Song, Y.B.; Lee, J.Y.; Lee, S.J.; Lee, S.Y.; Kim, S.M.; Yun, K.H.; Cho, J.Y.; Kim, C.J.; et al. Intravascular Imaging-Guided or Angiography-Guided Complex PCI. N. Engl. J. Med. 2023, 388, 1668–1679. [Google Scholar] [CrossRef]
- Kume, T.; Okura, H.; Kawamoto, T.; Yamada, R.; Miyamoto, Y.; Hayashida, A.; Watanabe, N.; Neishi, Y.; Sadahira, Y.; Akasaka, T.; et al. Assessment of the coronary calcification by optical coherence tomography. EuroIntervention 2011, 6, 768–772. [Google Scholar] [CrossRef] [PubMed]
- Terashima, M.; Kaneda, H.; Suzuki, T. The role of optical coherence tomography in coronary intervention. Korean J. Intern. Med. 2012, 27, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.M.; Rochitte, C.E.; Dewey, M.; Arbab-Zadeh, A.; Niinuma, H.; Gottlieb, I.; Paul, N.; Clouse, M.E.; Shapiro, E.P.; Hoe, J.; et al. Diagnostic performance of coronary angiography by 64-row CT. N. Engl. J. Med. 2008, 359, 2324–2336. [Google Scholar] [CrossRef] [PubMed]
- Pijls, N.H.; Van Gelder, B.; Van der Voort, P.; Peels, K.; Bracke, F.A.; Bonnier, H.J.; el Gamal, M.I. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation 1995, 92, 3183–3193. [Google Scholar] [CrossRef] [PubMed]
- Hamilos, M.; Muller, O.; Cuisset, T.; Ntalianis, A.; Chlouverakis, G.; Sarno, G.; Nelis, O.; Bartunek, J.; Vanderheyden, M.; Wyffels, E.; et al. Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation 2009, 120, 1505–1512. [Google Scholar] [CrossRef]
- Eberhart, R.C.; Su, S.H.; Nguyen, K.T.; Zilberman, M.; Tang, L.; Nelson, K.D.; Frenkel, P. Bioresorbable polymeric stents: Current status and future promise. J. Biomater. Sci. Polym. Ed. 2003, 14, 299–312. [Google Scholar] [CrossRef]
- Stone, G.W.; Ellis, S.G.; Cox, D.A.; Hermiller, J.; O’Shaughnessy, C.; Mann, J.T.; Turco, M.; Caputo, R.; Bergin, P.; Greenberg, J.; et al. One-year clinical results with the slow-release, polymer-based, paclitaxel-eluting TAXUS stent: The TAXUS-IV trial. Circulation 2004, 109, 1942–1947. [Google Scholar] [CrossRef] [PubMed]
- Stone, G.W.; Ellis, S.G.; Cox, D.A.; Hermiller, J.; O’Shaughnessy, C.; Mann, J.T.; Turco, M.; Caputo, R.; Bergin, P.; Greenberg, J.; et al. A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease. N. Engl. J. Med. 2004, 350, 221–231. [Google Scholar] [CrossRef]
- Lüscher, T.F.; Steffel, J.; Eberli, F.R.; Joner, M.; Nakazawa, G.; Tanner, F.C.; Virmani, R. Drug-eluting stent and coronary thrombosis: Biological mechanisms and clinical implications. Circulation 2007, 115, 1051–1058. [Google Scholar] [CrossRef] [PubMed]
- The BASKET-LATE-Study. Basel stent cost-effectiveness trial-late thrombotic events trial. Herz 2006, 31, 259. [Google Scholar]
- Kandzari, D.E.; Leon, M.B.; Meredith, I.; Fajadet, J.; Wijns, W.; Mauri, L. Final 5-year outcomes from the Endeavor zotarolimus-eluting stent clinical trial program: Comparison of safety and efficacy with first-generation drug-eluting and bare-metal stents. JACC Cardiovasc. Interv. 2013, 6, 504–512. [Google Scholar] [CrossRef] [PubMed]
- Leon, M.B.; Mauri, L.; Popma, J.J.; Cutlip, D.E.; Nikolsky, E.; O’Shaughnessy, C.; Overlie, P.A.; McLaurin, B.T.; Solomon, S.L.; Douglas, J.S., Jr.; et al. A randomized comparison of the Endeavor zotarolimus-eluting stent versus the TAXUS paclitaxel-eluting stent in de novo native coronary lesions 12-month outcomes from the ENDEAVOR IV trial. J. Am. Coll. Cardiol. 2010, 55, 543–554. [Google Scholar] [CrossRef]
- Mauri, L.; Massaro, J.M.; Jiang, S.; Meredith, I.; Wijns, W.; Fajadet, J.; Kandzari, D.E.; Leon, M.B.; Cutlip, D.E.; Thompson, K.P. Long-term clinical outcomes with zotarolimus-eluting versus bare-metal coronary stents. JACC Cardiovasc. Interv. 2010, 3, 1240–1249. [Google Scholar] [CrossRef]
- Zong, J.; He, Q.; Liu, Y.; Qiu, M.; Wu, J.; Hu, B. Advances in the development of biodegradable coronary stents: A translational perspective. Mater. Today Bio 2022, 16, 100368. [Google Scholar] [CrossRef]
- Serruys, P.W.; Chevalier, B.; Dudek, D.; Cequier, A.; Carrié, D.; Iniguez, A.; Dominici, M.; van der Schaaf, R.J.; Haude, M.; Wasungu, L.; et al. A bioresorbable everolimus-eluting scaffold versus a metallic everolimus-eluting stent for ischaemic heart disease caused by de-novo native coronary artery lesions (ABSORB II): An interim 1-year analysis of clinical and procedural secondary outcomes from a randomised controlled trial. Lancet 2015, 385, 43–54. [Google Scholar] [CrossRef]
- Stone, G.W.; Kereiakes, D.J.; Gori, T.; Metzger, D.C.; Stein, B.; Erickson, M.; Torzewski, J.; Kabour, A.; Piegari, G.; Cavendish, J.; et al. 5-Year Outcomes After Bioresorbable Coronary Scaffolds Implanted With Improved Technique. J. Am. Coll. Cardiol. 2023, 82, 183–195. [Google Scholar] [CrossRef]
- Kereiakes, D.J.; Ellis, S.G.; Metzger, C.; Caputo, R.P.; Rizik, D.G.; Teirstein, P.S.; Litt, M.R.; Kini, A.; Kabour, A.; Marx, S.O.; et al. 3-Year Clinical Outcomes With Everolimus-Eluting Bioresorbable Coronary Scaffolds: The ABSORB III Trial. J. Am. Coll. Cardiol. 2017, 70, 2852–2862. [Google Scholar] [CrossRef] [PubMed]
- Haude, M.; Ince, H.; Kische, S.; Toelg, R.; Van Mieghem, N.M.; Verheye, S.; von Birgelen, C.; Christiansen, E.H.; Barbato, E.; Garcia-Garcia, H.M.; et al. Sustained Safety and Performance of the Second-Generation Sirolimus-Eluting Absorbable Metal Scaffold: Pooled Outcomes of the BIOSOLVE-II and -III Trials at 3 Years. Cardiovasc. Revasc Med. 2020, 21, 1150–1154. [Google Scholar] [CrossRef]
- Ortega-Paz, L.; Brugaletta, S.; Gomez-Lara, J.; Alfonso, F.; Cequier, A.; Romaní, S.; Bordes, P.; Serra, A.; Iñiguez, A.; Salinas, P.; et al. Magnesium-based resorbable scaffold vs permanent metallic sirolimus-eluting stent in patients with ST-segment elevation myocardial infarction: 3-year results of the MAGSTEMI randomised controlled trial. EuroIntervention 2022, 18, e389–e396. [Google Scholar] [CrossRef]
- Pradhan, A.; Vishwakarma, P.; Vankar, S.; Sethi, R. “The Unpredictable ABSORB”—Very Late Stent Thrombosis of Bioresorbable Vascular Scaffold. Heart Views 2019, 20, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Kirtane, A.J.; Stone, G.W. How to minimize stent thrombosis. Circulation 2011, 124, 1283–1287. [Google Scholar] [CrossRef] [PubMed]
- Reejhsinghani, R.; Lotfi, A.S. Prevention of stent thrombosis: Challenges and solutions. Vasc. Health Risk Manag. 2015, 11, 93–106. [Google Scholar] [CrossRef]
- Ullrich, H.; Münzel, T.; Gori, T. Coronary Stent Thrombosis- Predictors and Prevention. Dtsch. Arztebl. Int. 2020, 117, 320–326. [Google Scholar] [CrossRef]
- Fischman, D.L.; Vishnevsky, A. Management of Iatrogenic Coronary Artery Dissections: Failing to Prepare Is Preparing to Fail. JACC Case Rep. 2021, 3, 385–387. [Google Scholar] [CrossRef] [PubMed]
- Chinikar, M.; Sadeghipour, P. Coronary stent fracture: A recently appreciated phenomenon with clinical relevance. Curr. Cardiol. Rev. 2014, 10, 349–354. [Google Scholar] [CrossRef]
- Lugo, L.M.; Ferreiro, J.L. Dual antiplatelet therapy after coronary stent implantation: Individualizing the optimal duration. J. Cardiol. 2018, 72, 94–104. [Google Scholar] [CrossRef]
- Lugo, L.M.; Ferreiro, J.L. Ticagrelor in patients with myocardial infarction: Is the treatment strategy crystal clear? Eur. Heart J. Cardiovasc. Pharmacother. 2019, 5, 207–209. [Google Scholar] [CrossRef]
- Valgimigli, M.; Bueno, H.; Byrne, R.A.; Collet, J.-P.; Costa, F.; Jeppsson, A.; Jüni, P.; Kastrati, A.; Kolh, P.; Mauri, L.; et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2018, 39, 213–260. [Google Scholar] [CrossRef] [PubMed]
- Mehran, R.; Baber, U.; Sharma, S.K.; Cohen, D.J.; Angiolillo, D.J.; Briguori, C.; Cha, J.Y.; Collier, T.; Dangas, G.; Dudek, D.; et al. Ticagrelor with or without Aspirin in High-Risk Patients after PCI. N. Engl. J. Med. 2019, 381, 2032–2042. [Google Scholar] [CrossRef]
- Kim, B.K.; Hong, S.J.; Cho, Y.H.; Yun, K.H.; Kim, Y.H.; Suh, Y.; Cho, J.Y.; Her, A.Y.; Cho, S.; Jeon, D.W.; et al. Effect of Ticagrelor Monotherapy vs Ticagrelor with Aspirin on Major Bleeding and Cardiovascular Events in Patients with Acute Coronary Syndrome: The TICO Randomized Clinical Trial. JAMA 2020, 323, 2407–2416. [Google Scholar] [CrossRef]
- Sibbing, D.; Aradi, D.; Jacobshagen, C.; Gross, L.; Trenk, D.; Geisler, T.; Orban, M.; Hadamitzky, M.; Merkely, B.; Kiss, R.G.; et al. Guided de-escalation of antiplatelet treatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention (TROPICAL-ACS): A randomised, open-label, multicentre trial. Lancet 2017, 390, 1747–1757. [Google Scholar] [CrossRef] [PubMed]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Capodanno, D.; Caggegi, A.; Miano, M.; Cincotta, G.; Dipasqua, F.; Giacchi, G.; Capranzano, P.; Ussia, G.; Di Salvo, M.E.; La Manna, A.; et al. Global risk classification and clinical SYNTAX (synergy between percutaneous coronary intervention with TAXUS and cardiac surgery) score in patients undergoing percutaneous or surgical left main revascularization. JACC Cardiovasc. Interv. 2011, 4, 287–297. [Google Scholar] [CrossRef]
- Applegate, R.J. Toward better stratification of patients with left main disease: Value of clinical and angiographic-derived risk scores. JACC Cardiovasc. Interv. 2011, 4, 298–299. [Google Scholar] [CrossRef] [PubMed]
- Bajraktari, G.; Bytyçi, I.; Henein, M.Y.; Alfonso, F.; Ahmed, A.; Jashari, H.; Bhatt, D.L. Complete revascularization for patients with multivessel coronary artery disease and ST-segment elevation myocardial infarction after the COMPLETE trial: A meta-analysis of randomized controlled trials. Int. J. Cardiol. Heart Vasc. 2020, 29, 100549. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.R.; Wood, D.A.; Storey, R.F.; Mehran, R.; Bainey, K.R.; Nguyen, H.; Meeks, B.; Di Pasquale, G.; López-Sendón, J.; Faxon, D.P.; et al. Complete Revascularization with Multivessel PCI for Myocardial Infarction. N. Engl. J. Med. 2019, 381, 1411–1421. [Google Scholar] [CrossRef]
- Lunardi, M.; Louvard, Y.; Lefèvre, T.; Stankovic, G.; Burzotta, F.; Kassab, G.S.; Lassen, J.F.; Darremont, O.; Garg, S.; Koo, B.-K.; et al. Definitions and Standardized Endpoints for Treatment of Coronary Bifurcations. EuroIntervention 2023, 19, e807–e831. [Google Scholar] [CrossRef]
- Alfonso, F.; Pan, M. Do We Know How to Treat Bifurcation Coronary Lesions? Rev. Esp. Cardiol. 2014, 67, 790–793. [Google Scholar] [CrossRef]
- Louvard, Y.; Medina, A. Definitions and classifications of bifurcation lesions and treatment. EuroIntervention 2015, 11, V23–V26. [Google Scholar] [CrossRef] [PubMed]
- Louvard, Y.; Lefèvre, T.; Morice, M.-C. Percutaneous coronary intervention for bifurcation coronary disease. Heart 2004, 90, 713. [Google Scholar] [CrossRef]
- Burzotta, F.; Lassen, J.F.; Lefèvre, T.; Banning, A.P.; Chatzizisis, Y.S.; Johnson, T.W.; Ferenc, M.; Rathore, S.; Albiero, R.; Pan, M.; et al. Percutaneous coronary intervention for bifurcation coronary lesions: The 15(th) consensus document from the European Bifurcation Club. EuroIntervention 2021, 16, 1307–1317. [Google Scholar] [CrossRef]
- Manpoong, C.P.; Saikia, B.; Ram, M.K.; Sarma, A.; Malviya, A. Detailed Morphometric Analysis on Left Coronary Artery in the Population of North-East India. Cureus 2023, 15, e45023. [Google Scholar] [CrossRef] [PubMed]
- Lawton, J.S.; Tamis-Holland, J.E.; Bangalore, S.; Bates, E.R.; Beckie, T.M.; Bischoff, J.M.; Bittl, J.A.; Cohen, M.G.; DiMaio, J.M.; Don, C.W.; et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 145, e18–e114. [Google Scholar] [CrossRef] [PubMed]
- Neumann, F.-J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef]
- Hunter, G.W.; Sharma, V.; Varma, C.; Connolly, D. The EXCEL Trial: The Interventionalists’ Perspective. Eur. Cardiol. 2021, 16, e01. [Google Scholar] [CrossRef]
- Narayan, P. NOBLE trial-is it time to revise the guidelines? Indian. J. Thorac. Cardiovasc. Surg. 2020, 36, 541–543. [Google Scholar] [CrossRef]
- Ramadan, R.; Boden, W.E.; Kinlay, S. Management of Left Main Coronary Artery Disease. J. Am. Heart Assoc. 2018, 7, e008151. [Google Scholar] [CrossRef] [PubMed]
- Glagov, S.; Weisenberg, E.; Zarins, C.K.; Stankunavicius, R.; Kolettis, G.J. Compensatory enlargement of human atherosclerotic coronary arteries. N. Engl. J. Med. 1987, 316, 1371–1375. [Google Scholar] [CrossRef] [PubMed]
- Riley, R.F.; Patel, M.P.; Abbott, J.D.; Bangalore, S.; Brilakis, E.S.; Croce, K.J.; Doshi, D.; Kaul, P.; Kearney, K.E.; Kerrigan, J.L.; et al. SCAI Expert Consensus Statement on the Management of Calcified Coronary Lesions. J. Soc. Cardiovasc. Angiogr. Interv. 2024, 3, 101259. [Google Scholar] [CrossRef]
- Karimi Galougahi, K.; Shlofmitz, E.; Jeremias, A.; Gogia, S.; Kirtane, A.J.; Hill, J.M.; Karmpaliotis, D.; Mintz, G.S.; Maehara, A.; Stone, G.W.; et al. Therapeutic Approach to Calcified Coronary Lesions: Disruptive Technologies. Curr. Cardiol. Rep. 2021, 23, 33. [Google Scholar] [CrossRef] [PubMed]
- Sorini Dini, C.; Nardi, G.; Ristalli, F.; Mattesini, A.; Hamiti, B.; Di Mario, C. Contemporary Approach to Heavily Calcified Coronary Lesions. Interv. Cardiol. 2019, 14, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Lugo-Gavidia, L.M.; Nolde, J.M.; Carnagarin, R.; Burger, D.; Chan, J.; Robinson, S.; Bosio, E.; Matthews, V.B.; Schlaich, M.P. Association of Circulating Platelet Extracellular Vesicles and Pulse Wave Velocity with Cardiovascular Risk Estimation. Int. J. Mol. Sci. 2022, 23, 10524. [Google Scholar] [CrossRef] [PubMed]
- Vlachopoulos, C.; Aznaouridis, K.; Stefanadis, C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 55, 1318–1327. [Google Scholar] [CrossRef] [PubMed]
- Barter, P.J.; Rye, K.A. Homocysteine and cardiovascular disease: Is HDL the link? Circ. Res. 2006, 99, 565–566. [Google Scholar] [CrossRef]
- Carnagarin, R.; Nolde, J.M.; Ward, N.C.; Lugo-Gavidia, L.M.; Chan, J.; Robinson, S.; Jose, A.; Joyson, A.; Azzam, O.; Galindo Kiuchi, M.; et al. Homocysteine predicts vascular target organ damage in hypertension and may serve as guidance for first-line antihypertensive therapy. J. Clin. Hypertens. 2021, 23, 1380–1389. [Google Scholar] [CrossRef]
- Wang, J.; Tan, G.J.; Han, L.N.; Bai, Y.Y.; He, M.; Liu, H.B. Novel biomarkers for cardiovascular risk prediction. J. Geriatr. Cardiol. 2017, 14, 135–150. [Google Scholar] [CrossRef]
- Ferreiro, J.L.; Vivas, D.; De La Hera, J.M.; Marcano, A.L.; Lugo, L.M.; Gómez-Polo, J.C.; Silva, I.; Tello-Montoliu, A.; Marín, F.; Roldán, I. High and low on-treatment platelet reactivity to P2Y(12) inhibitors in a contemporary cohort of acute coronary syndrome patients undergoing percutaneous coronary intervention. Thromb. Res. 2019, 175, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Lugo-Gavidia, L.M.; Burger, D.; Matthews, V.B.; Nolde, J.M.; Galindo Kiuchi, M.; Carnagarin, R.; Kannenkeril, D.; Chan, J.; Joyson, A.; Herat, L.Y.; et al. Role of Microparticles in Cardiovascular Disease: Implications for Endothelial Dysfunction, Thrombosis, and Inflammation. Hypertension 2021, 77, 1825–1844. [Google Scholar] [CrossRef]
- Lugo-Gavidia, L.M.; Burger, D.; Nolde, J.M.; Carnagarin, R.; Chan, J.; Bosio, E.; Matthews, V.B.; Schlaich, M.P. Platelet-derived extracellular vesicles correlate with therapy-induced nocturnal blood pressure changes. J. Hypertens. 2022, 40, 2210–2218. [Google Scholar] [CrossRef]
- Lugo-Gavidia, L.M.; Burger, D.; Nolde, J.M.; Matthews, V.B.; Schlaich, M.P. Evaluation of Circulating Platelet Extracellular Vesicles and Hypertension Mediated Organ Damage. Int. J. Mol. Sci. 2022, 23, 5150. [Google Scholar] [CrossRef] [PubMed]
- Lugo-Gavidia, L.M.; Carnagarin, R.; Burger, D.; Nolde, J.M.; Chan, J.; Robinson, S.; Bosio, E.; Matthews, V.B.; Schlaich, M.P. Circulating platelet-derived extracellular vesicles correlate with night-time blood pressure and vascular organ damage and may represent an integrative biomarker of vascular health. J. Clin. Hypertens. 2022, 24, 738–749. [Google Scholar] [CrossRef]
- Marcano, A.L.; Lugo, L.M.; Besteiro, A.; Gomez-Lara, J.; Roura, G.; Fuentes, L.; Gracida, M.; Teruel, L.; Romaguera, R.; Sosa, S.G.; et al. Association of fractalkine with functional severity of heart failure and impact on clopidogrel efficacy in patients with ischemic heart disease. Thromb. Res. 2020, 196, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Christersson, C.; Thulin, A.; Siegbahn, A. Microparticles during long-term follow-up after acute myocardial infarction. Association to atherosclerotic burden and risk of cardiovascular events. Thromb. Haemost. 2017, 117, 1571–1581. [Google Scholar] [CrossRef]
- Bernal-Mizrachi, L.; Jy, W.; Fierro, C.; Macdonough, R.; Velazques, H.A.; Purow, J.; Jimenez, J.J.; Horstman, L.L.; Ferreira, A.; de Marchena, E.; et al. Endothelial microparticles correlate with high-risk angiographic lesions in acute coronary syndromes. Int. J. Cardiol. 2004, 97, 439–446. [Google Scholar] [CrossRef]
- Bernal-Mizrachi, L.; Jy, W.; Jimenez, J.J.; Pastor, J.; Mauro, L.M.; Horstman, L.L.; de Marchena, E.; Ahn, Y.S. High levels of circulating endothelial microparticles in patients with acute coronary syndromes. Am. Heart J. 2003, 145, 962–970. [Google Scholar] [CrossRef]
- Cui, Y.; Zheng, L.; Jiang, M.; Jia, R.; Zhang, X.; Quan, Q.; Du, G.; Shen, D.; Zhao, X.; Sun, W.; et al. Circulating microparticles in patients with coronary heart disease and its correlation with interleukin-6 and C-reactive protein. Mol. Biol. Rep. 2013, 40, 6437–6442. [Google Scholar] [CrossRef]
- Sinning, J.M.; Losch, J.; Walenta, K.; Bohm, M.; Nickenig, G.; Werner, N. Circulating CD31+/Annexin V+ microparticles correlate with cardiovascular outcomes. Eur. Heart J. 2011, 32, 2034–2041. [Google Scholar] [CrossRef] [PubMed]
- Stone, G.W.; Witzenbichler, B.; Weisz, G.; Rinaldi, M.J.; Neumann, F.J.; Metzger, D.C.; Henry, T.D.; Cox, D.A.; Duffy, P.L.; Mazzaferri, E.; et al. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): A prospective multicentre registry study. Lancet 2013, 382, 614–623. [Google Scholar] [CrossRef] [PubMed]
- Claassens, D.M.F.; Vos, G.J.A.; Bergmeijer, T.O.; Hermanides, R.S.; van ‘t Hof, A.W.J.; van der Harst, P.; Barbato, E.; Morisco, C.; Tjon Joe Gin, R.M.; Asselbergs, F.W.; et al. A Genotype-Guided Strategy for Oral P2Y(12) Inhibitors in Primary PCI. N. Engl. J. Med. 2019, 381, 1621–1631. [Google Scholar] [CrossRef] [PubMed]
- Kerkmeijer, L.S.M.; Chandrasekhar, J.; Kalkman, D.N.; Woudstra, P.; Menown, I.B.A.; Suryapranata, H.; den Heijer, P.; Iñiguez, A.; van ‘t Hof, A.W.J.; Erglis, A.; et al. Final five-year results of the REMEDEE Registry: Real-world experience with the dual-therapy COMBO stent. Catheter. Cardiovasc. Interv. 2021, 98, 503–510. [Google Scholar] [CrossRef]
- Lin, A.; Kolossváry, M.; Motwani, M.; Išgum, I.; Maurovich-Horvat, P.; Slomka, P.J.; Dey, D. Artificial Intelligence in Cardiovascular Imaging for Risk Stratification in Coronary Artery Disease. Radiol. Cardiothorac. Imaging 2021, 3, e200512. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lugo-Gavidia, L.M.; Alcocer-Gamba, M.A.; Martinez-Cervantes, A. Challenges and Advances in Interventional Cardiology for Coronary Artery Disease Management. Medicina 2024, 60, 1323. https://doi.org/10.3390/medicina60081323
Lugo-Gavidia LM, Alcocer-Gamba MA, Martinez-Cervantes A. Challenges and Advances in Interventional Cardiology for Coronary Artery Disease Management. Medicina. 2024; 60(8):1323. https://doi.org/10.3390/medicina60081323
Chicago/Turabian StyleLugo-Gavidia, Leslie Marisol, Marco Antonio Alcocer-Gamba, and Araceli Martinez-Cervantes. 2024. "Challenges and Advances in Interventional Cardiology for Coronary Artery Disease Management" Medicina 60, no. 8: 1323. https://doi.org/10.3390/medicina60081323




