Relationship between SLAP Lesions and Shoulder Joint Capsule Thickness: An MR Arthrographic Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Injection Technique, MR Arthrograms and Image Analysis
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Manoso-Hernando, D.; Bailón-Cerezo, J.; Angulo-Díaz-Parreño, S.; Reina-Varona, Á.; Elizagaray-García, I.; Gil-Martínez, A. Shoulder mobility and strength impairments in patients with rotator cuff related shoulder pain: A systematic review and meta analysis. PeerJ 2024, 12, e17604. [Google Scholar] [CrossRef] [PubMed]
- Dowe, J.N.; Bradley, M.W.; LeClere, L.E.; Dickens, J.F. Creating a Three-Dimensional Reconstruction of the Glenohumeral Joint From Magnetic Resonance Imaging to Assist in Surgical Decision-Making. Arthrosc. Tech. 2024, 13, 102972. [Google Scholar] [CrossRef] [PubMed]
- Wallace, A.L.; Calvo, E.; Ardèvol Cuesta, J.; Lanzetti, R.; Luengo-Alonso, G.; Rokito, A.S.; Spencer, E.E.; Jr Spoliti, M. Safety and efficacy of second-generation all-suture anchors in labral tear arthroscopic repairs: Prospective, multicenter, 1-year follow-up study. JSES Int. 2024, 8, 763–768. [Google Scholar] [CrossRef] [PubMed]
- Dakkak, M.; Saleem, A.; Patel, D.; Yeager, M.; Oliveira, L.; Gilot, G.; Spindler, K.P. A systematic review of randomized control trials looking at functional improvement of rotator cuff partial thickness tears following platelet-rich-plasma injection: A comparison of glenohumeral joint vs. subacromial bursa vs. intratendinous injection locations. JSES Int. 2024, 8, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.Y.; Kim, D.; Kim, H.; Ha, I.H.; Lee, Y.J. Health Care Utilization for Common Shoulder Disorders: Analysis of the 2010-2019 National Patient Sample Data from the Health Insurance Review and Assessment Service in Korea. Medicina 2024, 60, 744. [Google Scholar] [CrossRef] [PubMed]
- Baek, C.H.; Kim, B.T.; Kim, J.G.; Kim, S.J. Mid-Term Outcome of Superior Capsular Reconstruction Using Fascia Lata Autograft (At Least 6 mm in Thickness) Results in High Retear Rate and No Improvement in Muscle Strength. Arthroscopy 2024, 40, 1961–1971. [Google Scholar] [CrossRef] [PubMed]
- Guity, M.R.; Khan, F.; Gity, M.; Sheidaie, H.; Aghaghazvini, L. Prevalence and Correlation between MRI Findings and Outcome of Conservative Treatment in Primary Idiopathic Frozen Shoulder. Arch. Bone Jt. Surg. 2024, 12, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Antunes, M.; Quental, C.; Folgado, J.; Ângelo, A.C.; de Campos Azevedo, C. Influence of the rotator cuff tear pattern in shoulder stability after arthroscopic superior capsule reconstruction: A computational analysis. J. Isakos 2024, 9, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.S.; Han, J.Y.; Park, Y.J.; Kwak, J.W.; Lee, B.S. Comparative analysis of superior capsule reconstruction between long head of biceps tendon autograft and human dermis allograft. J. Shoulder Elbow Surg. 2023, 32, 820–831. [Google Scholar] [CrossRef] [PubMed]
- Alashkham, A.; Alraddadi, A.; Felts, P.; Soames, R. Histology, vascularity and innervation of the glenoid labrum. J. Orthop. Surg. 2018, 26, 2309499018770900. [Google Scholar] [CrossRef] [PubMed]
- Mohr, D.; Nammour, M.A.; Marcaccio, S.E.; Arner, J.W.; Bradley, J.P. Location of Shoulder Glenoid Labral Tears: A Study of 1763 Consecutive Patients. Am. J. Sports Med. 2024, 52, 2063–2070. [Google Scholar] [CrossRef] [PubMed]
- Dwivedi, A.; Sharma, R.; Sharma, A.; Gupta, P. Evaluation of Shoulder Injuries: A Comparative Study of Imaging by Magnetic Resonance Imaging (MRI) and Magnetic Resonance Arthrography (MRA). J. Pharm. Bioallied Sci. 2024, 16, S1494–S1497. [Google Scholar] [CrossRef] [PubMed]
- Shafiei, M.; Shomal Zadeh, F.; Shafiee, A.; Soltanolkotabi, M.; Gee, A.O.; Chalian, M. Diagnostic performance of MRA in abduction and external rotation position in the detection of glenoid labral lesions: A systematic review and meta-analysis. Skeletal Radiol. 2022, 51, 1611–1621. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.Y.; Chung, B.M.; Kim, W.T.; Lee, Y. MRI Findings Predictive of Shoulder Stiffness in Patients with Full-Thickness Rotator Cuff Tears. AJR Am. J. Roentgenol. 2022, 214, 1146–1151. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Choi, Y.H.; Chai, J.W.; Cha, S.W.; Lim, J.H.; Jo, C.H.; Kim, D.H. Anterior capsular abnormality: Another important MRI finding for the diagnosis of adhesive capsulitis of the shoulder. Skelet. Radiol. 2019, 48, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Dupont, T.; Idir, M.A.; Hossu, G.; Sirveaux, F.; Gillet, R.; Blum, A.; Teixeira, P.A.G. MR imaging signs of shoulder adhesive capsulitis: Analysis of potential differentials and improved diagnostic criteria. In Skeletal Radiology; Springer: Berlin/Heidelberg, Germany, 2024. [Google Scholar] [CrossRef]
- De Angelis Guerra Dotta, T.; Assunção, J.H.; Baptista, E.; e Silva, F.B.A.; Gracitelli, M.E.C.; Neto, A.A.F.; Malavolta, E.A. Diagnostic accuracy of non-contrast MRI in frozen shoulder. Arch. Orthop. Trauma Surg. 2024, 144, 1149–1159. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Chen, S.; Qiao, Y.; Ge, Y.; Li, H.; Chen, J.; Hua, Y.; Li, Y. A Long Preoperative Duration of Symptoms Is Associated with Worse Functional Outcomes After 1-Stage Arthroscopic Treatment of Rotator Cuff Tears with Shoulder Stiffness. Am. J. Sports Med. 2017, 45, 2336–2344. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.B.; Jung, D.W. A Rotator Cuff Tear Concomitant with Shoulder Stiffness Is Associated with a Lower Retear Rate After 1-Stage Arthroscopic Surgery. Am. J. Sports Med. 2018, 46, 1909–1918. [Google Scholar] [CrossRef] [PubMed]
- Thiagarajan, A.; Nagaraj, R.; Marathe, K. Correlation Between Clinical Diagnosis, MRI, and Arthroscopy in Diagnosing Shoulder Pathology. Cureus 2021, 13, e20654. [Google Scholar] [CrossRef] [PubMed]
- Saqib, R.; Harris, J.; Funk, L. Comparison of magnetic resonance arthrography with arthroscopy for imaging of shoulder injuries: Retrospective study. Ann. R. Coll. Surg. Engl. 2017, 99, 271–274. [Google Scholar] [CrossRef] [PubMed]
- Karasuyama, M.; Tsuruta, T.; Yamamoto, S.; Ariie, T.; Kawakami, J.; Minamikawa, T.; Ohzono, H.; Moriyama, H.; Gotoh, M. Comparative efficacy of treatments for a first-time traumatic anterior shoulder dislocation: A systematic review and network meta-analysis. J. Shoulder Elbow Surg. 2024. [CrossRef] [PubMed]
- Salas, M.; Zaldivar, B.; Fierro, G.; Gonzalez, J.C.; Lievano, J.R. Incidence and risk factors for shoulder stiffness after open and arthroscopic rotator cuff repair. Arch. Orthop. Trauma Surg. 2024, 144, 2047–2055. [Google Scholar] [CrossRef]
- Ni, M.; Gao, L.; Chen, W.; Zhao, Q.; Zhao, Y.; Jiang, C.; Yuan, H. Preliminary exploration of deep learning-assisted recognition of superior labrum anterior and posterior lesions in shoulder MR arthrography. Int. Orthop. 2024, 48, 183–191. [Google Scholar] [CrossRef]
- Rixey, A.; Rhodes, N.; Murthy, N.; Johnson, M.; Larson, N.; Ringler, M.D. Accuracy of MR arthrography in the detection of posterior glenoid labral injuries of the shoulder. Skeletal Radiol. 2023, 52, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Darbandi, A.; Credille, K.; Darbandi, A.; Hevesi, M.; Dandu, N.; Bodendorfer, B.M.; Wang, Z.; Garrigues, G.; Verma, N.; Yanke, A. Fatty Infiltration, Tear Size, and Retraction Size Are Significant Risk Factors for Retear following Arthroscopic Rotator Cuff Repair: A Systematic Review. Arthroscopy 2024, in press. [CrossRef]
- Rajalekshmi, R.; Agrawal, D.K. Understanding Fibrous Tissue in the Effective Healing of Rotator Cuff Injury. J. Surg. Res. 2024, 7, 215–228. [Google Scholar] [CrossRef]
- Matsunaga, K.; Miyake, S.; Izaki, T.; Shibata, T.; Yamamoto, T. Serial Magnetic Resonance Arthrography for a Midsubstance Capsular Tear in a Patient with Traumatic Anterior Shoulder Instability. Cureus 2024, 16, e59247. [Google Scholar] [CrossRef] [PubMed]
- Ogul, H.; Kantarci, M.; Topal, M.; Karaca, L.; Tuncer, K.; Pirimoglu, B.; Okur, A.; Yildirim, O.S.; Levent, A. Extra-articular contrast material leaks into locations unrelated to the injection path in shoulder MR arthrography. Eur. Radiol. 2014, 24, 2606–2613. [Google Scholar] [CrossRef]


| Characteristic. | Control Group (n = 46) | Patient Group (n = 32) | p Value |
|---|---|---|---|
| Age (Mean ± SD) | 38.76 ± 13 | 44.75 ± 14.18 | 0.058 * |
| Gender | 0.899 + | ||
| Male | 31 (67.39%) | 22 (68.75%) | |
| Female | 15 (32.61%) | 10 (31.25%) | |
| Side | 0.722 + | ||
| Right | 22 (47.83%) | 14 (43.75%) | |
| Left | 24 (52.17%) | 18 (56.25%) | |
| SLAP Lesion | 0.0001 + | ||
| None | 46 (100%) | 0 (0%) | |
| Present | 0 (0%) | 32 (100%) | |
| Cuff Pathology | 0.116 + | ||
| None | 35 (76.09%) | 19 (59.38%) | |
| Present | 11 (23.91%) | 13 (40.63%) | |
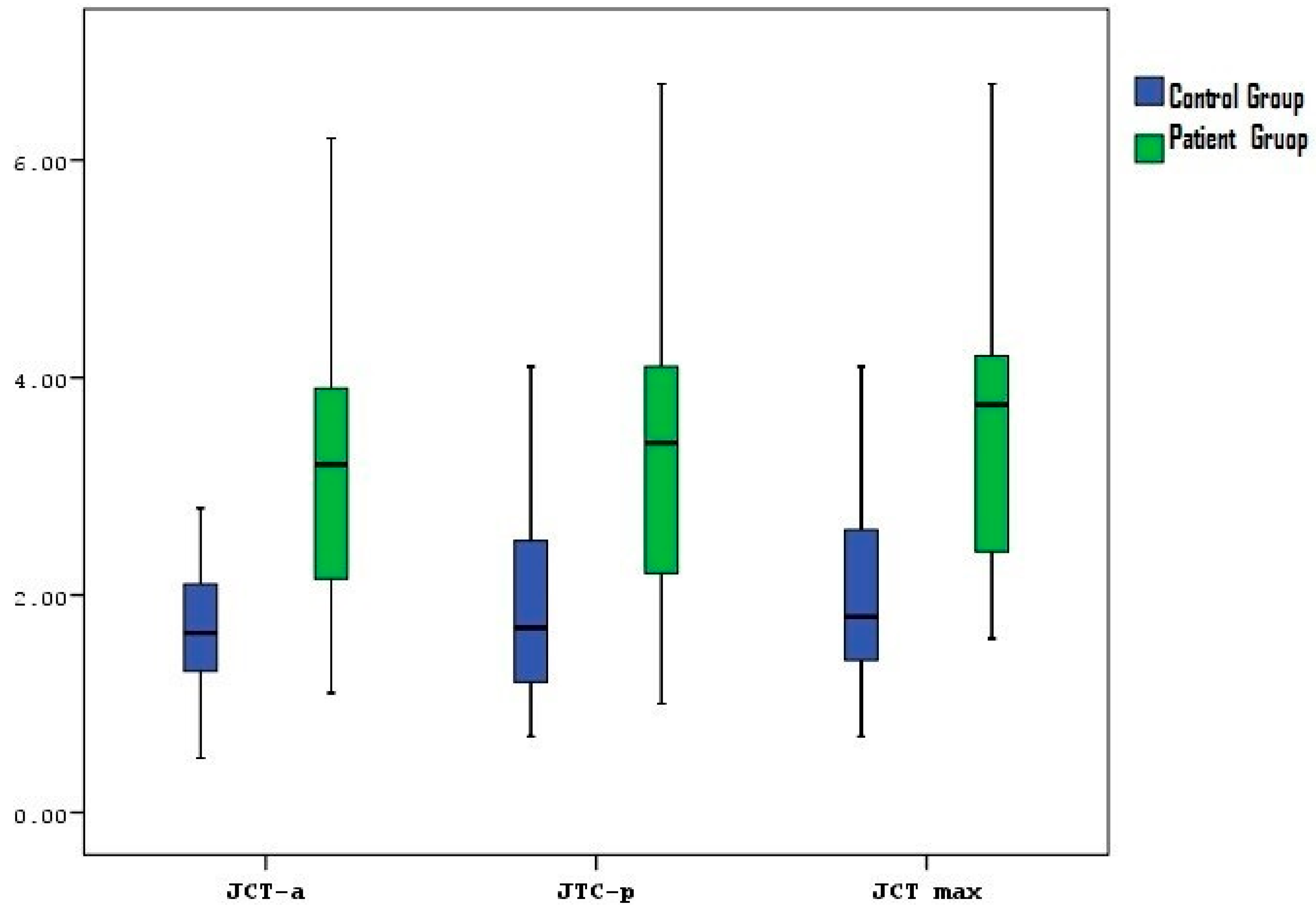
| Joint capsule thickness- Anterior (Mean ± SD) | 1.72 ± 0.7 | 3.13 ± 1.28 | 0.0001 † |
| Median (IQR) | 1.65 (1.28–2.10) | 3.20 (2.13–3.90) | |
| Joint capsule thickness- Posterior (Mean ± SD) | 1.95 ± 1.06 | 3.35 ± 1.32 | 0.0001 † |
| Median (IQR) | 1.70 (1.20–2.53) | 3.40 (2.20–4.10) | |
| Joint capsule thickness- Max (Mean ± SD) | 2.06 ± 1.01 | 3.6 ± 1.32 | 0.0001 † |
| Median (IQR) | 1.80 (1.40–2.60) | 3.75 (2.35–4.20) |
| SLAP Type | Patient Group (n = 32) |
|---|---|
| Type 1 | 7 (21.88%) |
| Type 2 | 14 (43.76%) |
| Type 4 | 3 (9.38%) |
| Type 5 | 3 (9.38%) |
| Type 8 | 3 (9.38%) |
| Type 9 | 1 (3.13%) |
| Type 10 | 1 (3.13%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Güçlü, D.; Uludağ, V.; Arıcan, M.; Ünlü, E.N.; Oğul, H. Relationship between SLAP Lesions and Shoulder Joint Capsule Thickness: An MR Arthrographic Study. Medicina 2024, 60, 1332. https://doi.org/10.3390/medicina60081332
Güçlü D, Uludağ V, Arıcan M, Ünlü EN, Oğul H. Relationship between SLAP Lesions and Shoulder Joint Capsule Thickness: An MR Arthrographic Study. Medicina. 2024; 60(8):1332. https://doi.org/10.3390/medicina60081332
Chicago/Turabian StyleGüçlü, Derya, Veysel Uludağ, Mehmet Arıcan, Elif Nisa Ünlü, and Hayri Oğul. 2024. "Relationship between SLAP Lesions and Shoulder Joint Capsule Thickness: An MR Arthrographic Study" Medicina 60, no. 8: 1332. https://doi.org/10.3390/medicina60081332
APA StyleGüçlü, D., Uludağ, V., Arıcan, M., Ünlü, E. N., & Oğul, H. (2024). Relationship between SLAP Lesions and Shoulder Joint Capsule Thickness: An MR Arthrographic Study. Medicina, 60(8), 1332. https://doi.org/10.3390/medicina60081332






