Anterior Sacroiliac Fracture Dislocation: A Comparative Radiologic analysis of Crescent Fractures in Pelvic Ring Injuries: A Retrospective Study
Abstract
1. Introduction
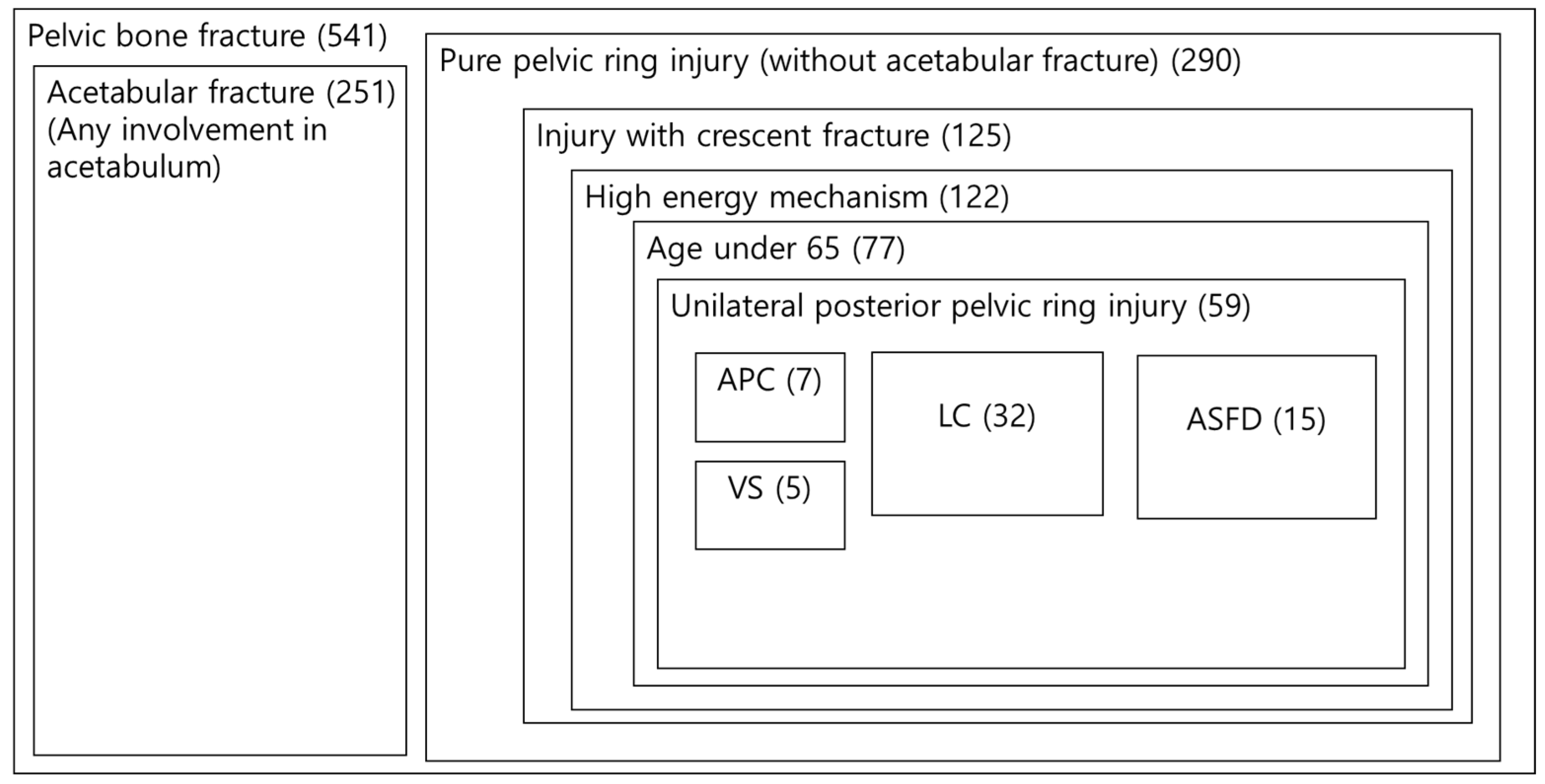
2. Methods
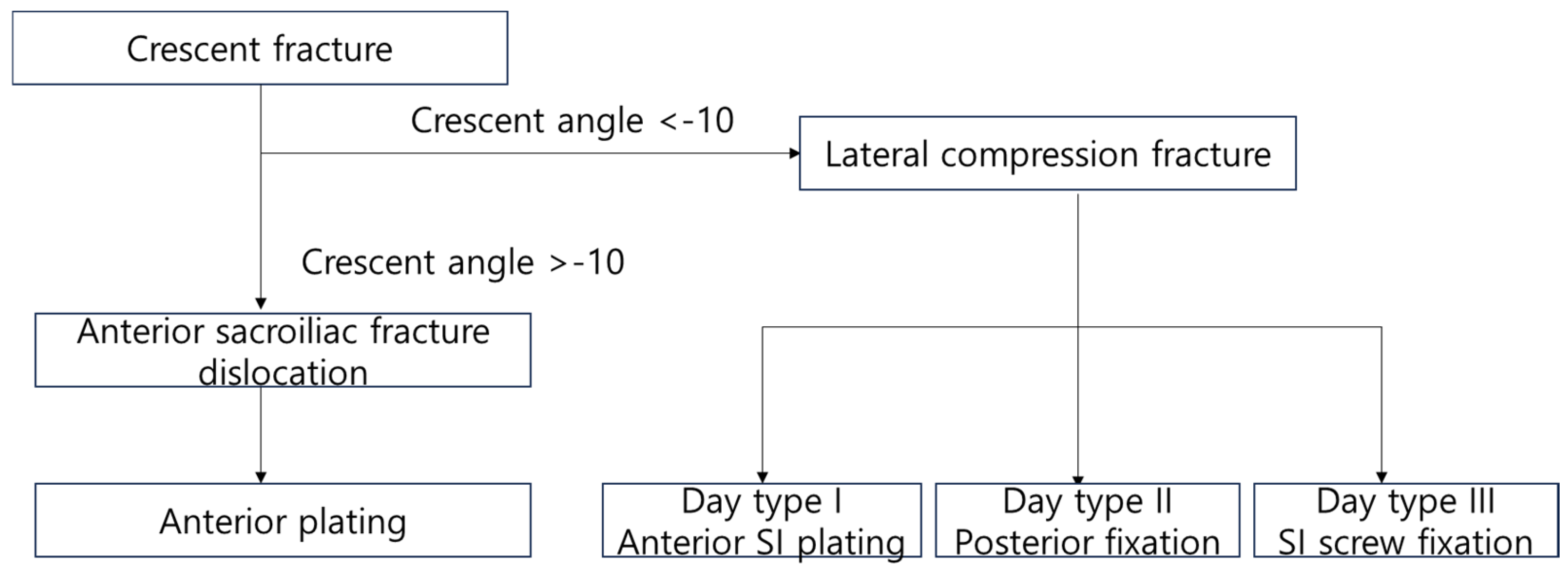
2.1. Classification of Fracture
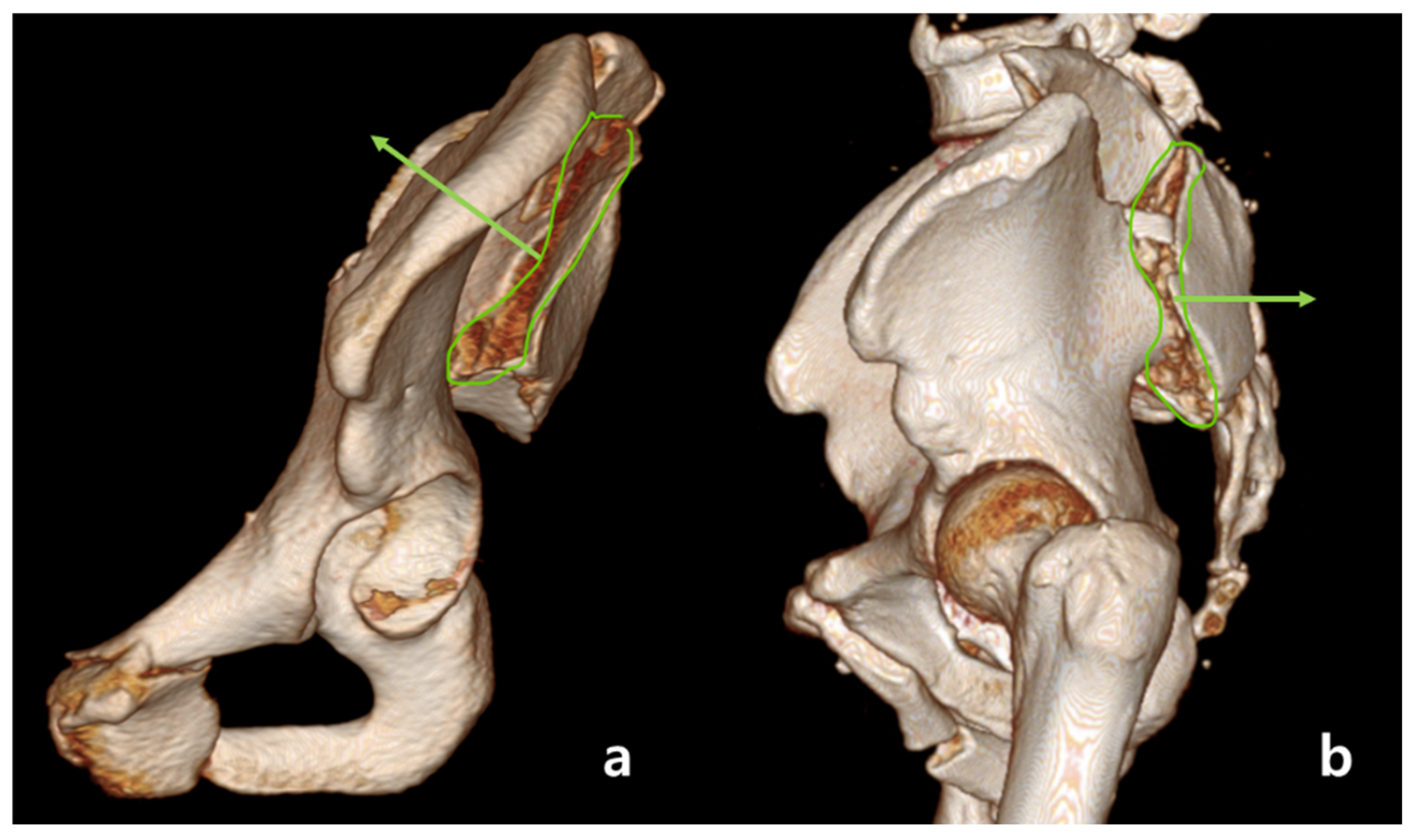
2.2. Definition of Anterior Sacroiliac Fracture Dislocation
2.3. Radiologic Assessment
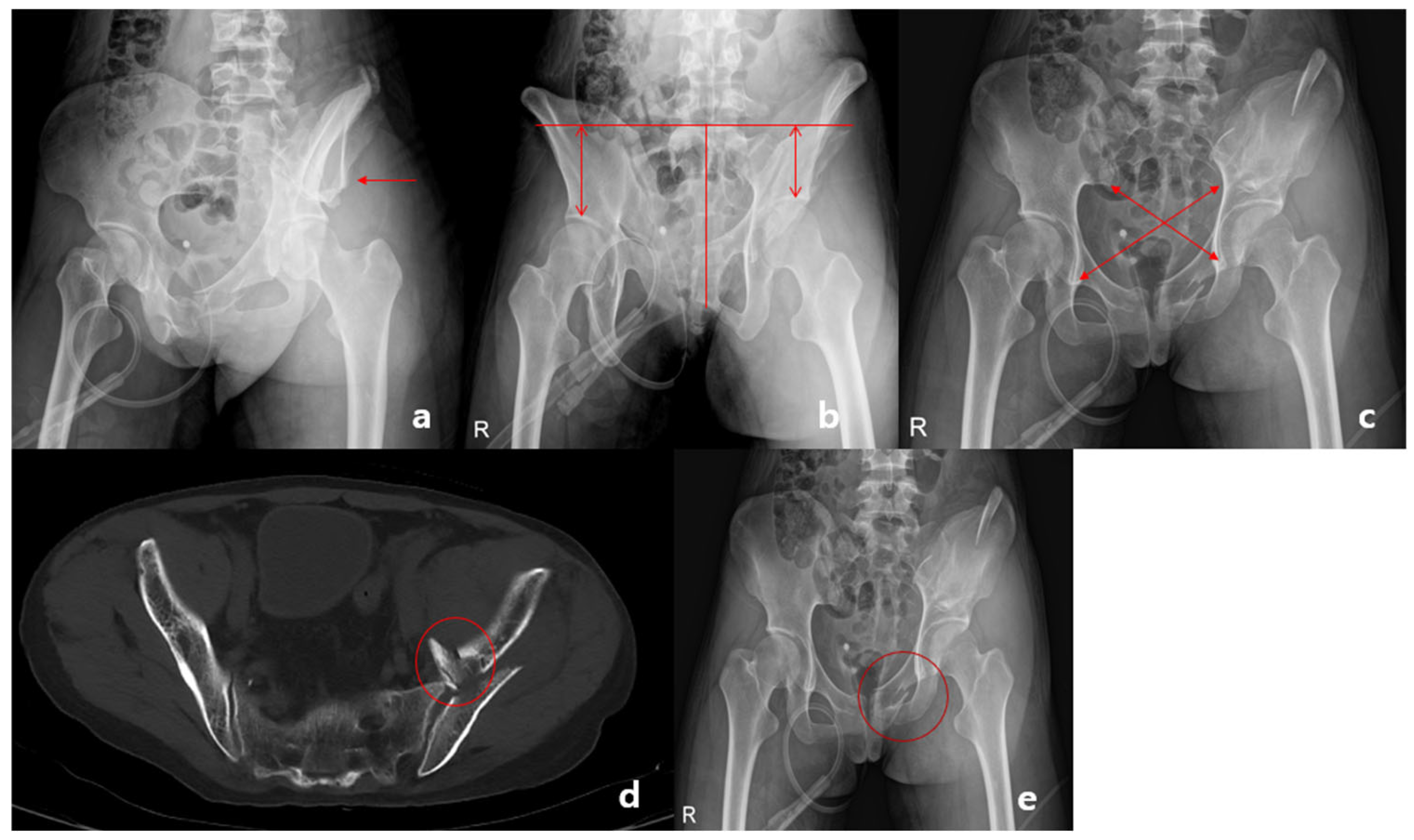
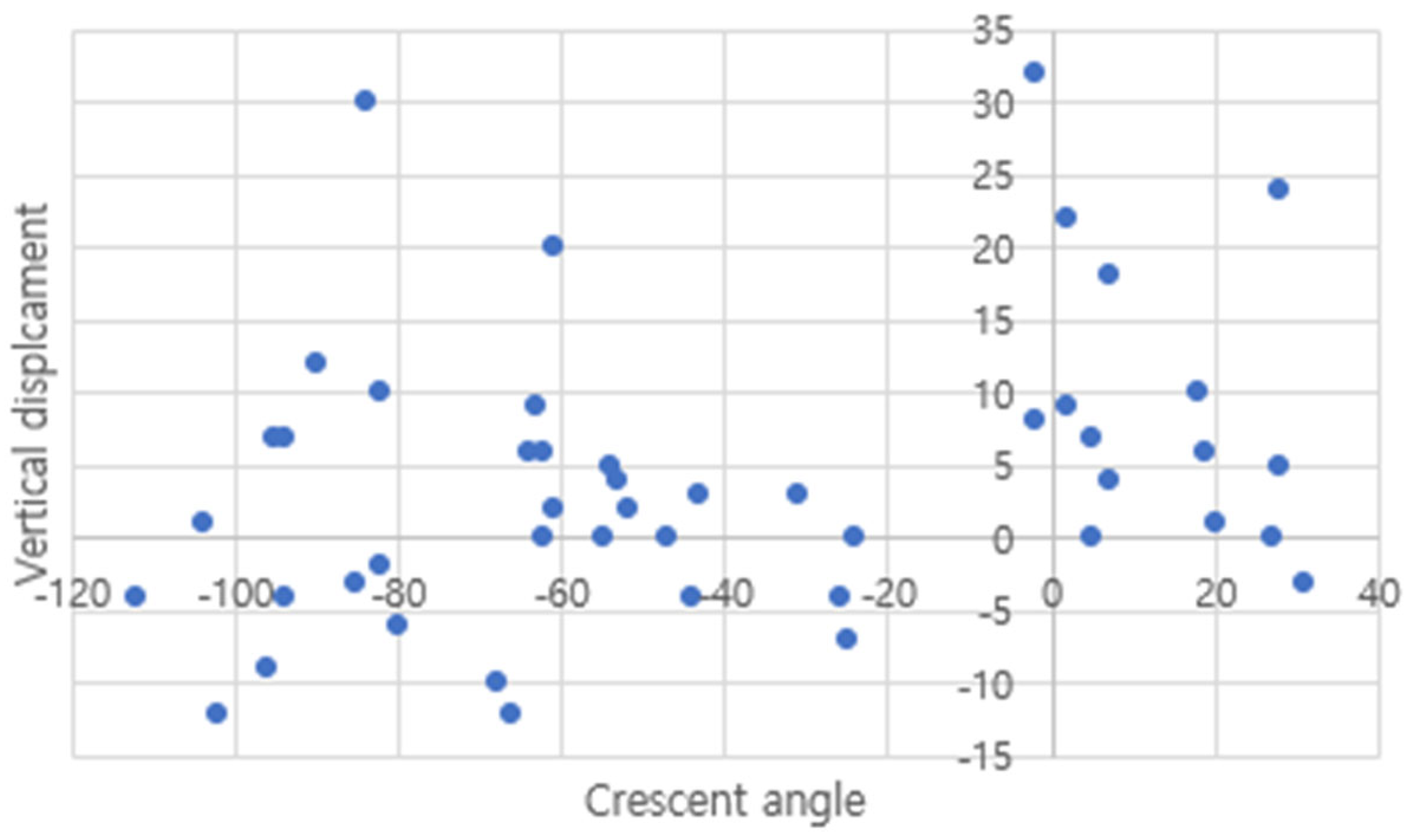
2.4. Assessment of Vertical Displacement
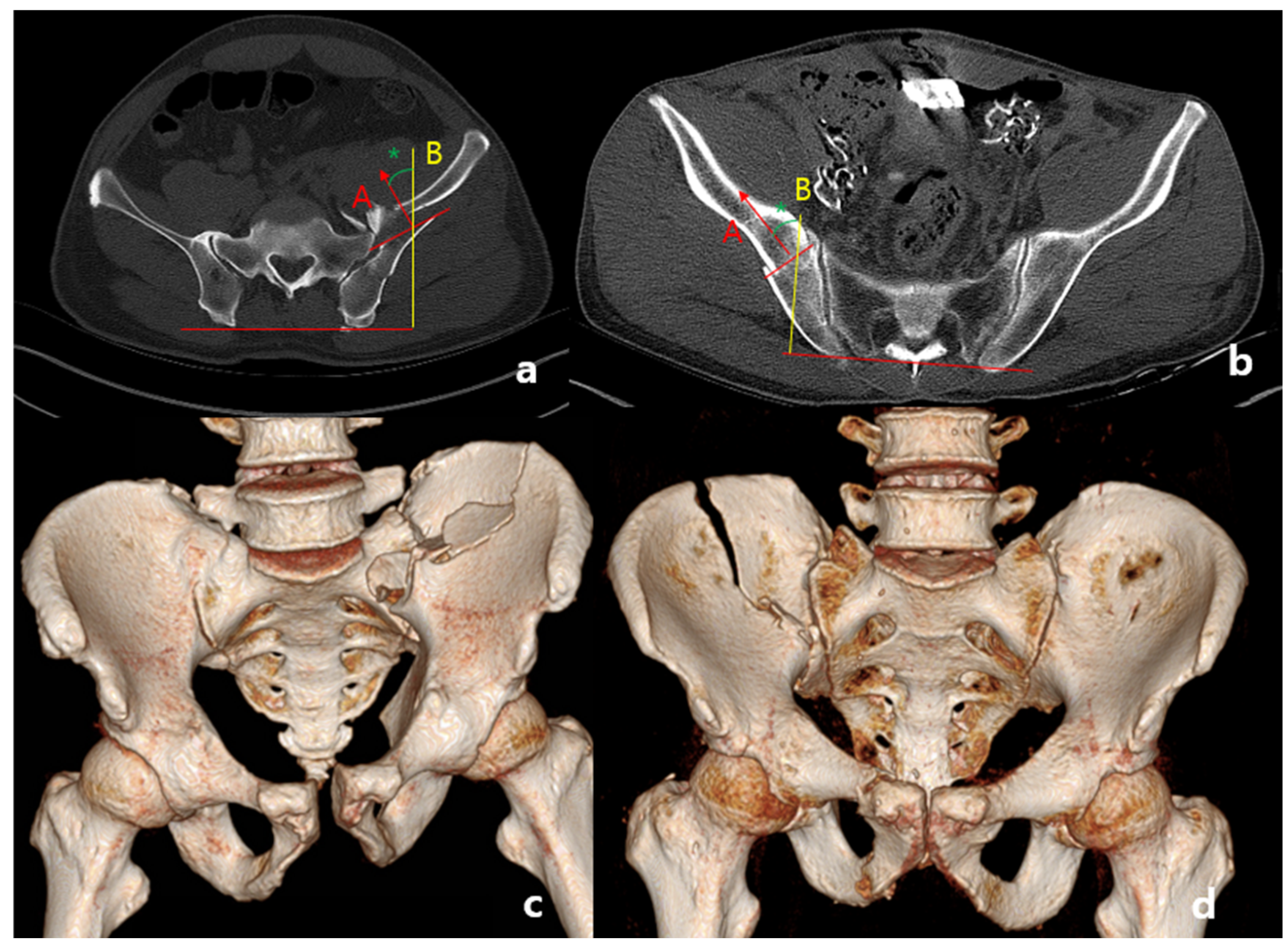
2.5. Assessment of Rotational Displacement
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Young, J.W.; Burgess, A.R.; Brumback, R.J.; Poka, A. Pelvic fractures: Value of plain radiography in early assessment and management. Radiology 1986, 160, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Tile, M. Pelvic ring fractures: Should they be fixed? J. Bone Jt. Surg. Br. 1988, 70, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Alton, T.B.; Gee, A.O. Classifications in brief: Young and burgess classification of pelvic ring injuries. Clin. Orthop. Relat. Res. 2014, 472, 2338–2342. [Google Scholar] [CrossRef] [PubMed]
- Day, A.C.; Kinmont, C.; Bircher, M.D.; Kumar, S. Crescent fracture-dislocation of the sacroiliac joint: A functional classification. J. Bone Jt. Surg. Br. 2007, 89, 651–658. [Google Scholar] [CrossRef]
- Trikha, V.; Singh, V.; Kumar, V.S. Anterior fracture dislocation of sacroiliac joint: A rare type of crescent fracture. Indian J. Orthop. 2015, 49, 255–259. [Google Scholar] [CrossRef]
- Xiao, J.; Wang, Y.; Zhang, M.; Jiang, R.; Zhu, T.; Liu, G.; Zuo, J. Anterior fracture dislocation of the sacroiliac joint: A case report and literature review. Technol. Health Care 2017, 25, 803–808. [Google Scholar] [CrossRef]
- Blum, L.; Hake, M.E.; Charles, R.; Conlan, T.; Rojas, D.; Martin, M.T.; Mauffrey, C. Vertical shear pelvic injury: Evaluation, management, and fixation strategies. Int. Orthop. 2018, 42, 2663–2674. [Google Scholar] [CrossRef]
- Lee, S.W.; Kim, W.Y.; Koh, S.J.; Kim, Y.Y. Posterior locked lateral compression injury of the pelvis in geriatric patients: An infrequent and specific variant of the fragility fracture of pelvis. Arch. Orthop. Trauma Surg. 2017, 137, 1207–1218. [Google Scholar] [CrossRef]
- Tornetta, P., 3rd; Matta, J.M. Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin. Orthop. Relat. Res. 1996, 329, 186–193. [Google Scholar] [CrossRef]
- Matta, J.M.; Tornetta, P., 3rd. Internal fixation of unstable pelvic ring injuries. Clin. Orthop. Relat. Res. 1996, 329, 129–140. [Google Scholar] [CrossRef]
- Keshishyan, R.A.; Rozinov, V.M.; Malakhov, O.A.; Kuznetsov, L.E.; Strunin, E.G.; Chogovadze, G.A.; Tsukanov, V.E. Pelvic polyfractures in children. Radiographic diagnosis and treatment. Clin. Orthop. Relat. Res. 1995, 320, 28–33. [Google Scholar]
- Bowerman, J.W.; Sena, J.M.; Chang, R. The teardrop shadow of the pelvis; anatomy and clinical significance. Radiology 1982, 143, 659–662. [Google Scholar] [CrossRef]
- Lefaivre, K.A.; Starr, A.J.; Barker, B.P.; Overturf, S.; Reinert, C.M. Early experience with reduction of displaced disruption of the pelvic ring using a pelvic reduction frame. J. Bone Jt. Surg. Br. 2009, 91, 1201–1207. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.R.; Eastridge, B.J.; Young, J.W.; Ellison, T.S.; Ellison, P.S., Jr.; Poka, A.; Bathon, G.H.; Brumback, R.J. Pelvic ring disruptions: Effective classification system and treatment protocols. J. Trauma Acute Care Surg. 1990, 30, 848–856. [Google Scholar] [CrossRef]
- Henderson, R.C. The long-term results of nonoperatively treated major pelvic disruptions. J. Orthop. Trauma 1989, 3, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Dickson, K.F.; Matta, J.M. Skeletal deformity after anterior external fixation of the pelvis. J. Orthop. Trauma 2009, 23, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Boontanapibul, K.; Harnroongroj, T.; Sudjai, N.; Harnroongroj, T. Vertical pelvic ring displacement in pelvic ring injury: Measurements in pelvic outlet radiograph and in cadavers. Indian J. Orthop. 2015, 49, 425–428. [Google Scholar] [CrossRef]
- Weaver, M.J.; Bruinsma, W.; Toney, E.; Dafford, E.; Vrahas, M.S. What Are the Patterns of Injury and Displacement Seen in Lateral Compression Pelvic Fractures? Clin. Orthop. Relat. Res. 2012, 470, 2104–2110. [Google Scholar] [CrossRef]
- Wu, Y.; Chen, H.; Zhou, X.; Tang, P. Lateral Compression Type 2 Pelvic Fractures-A Clinical Study of Fracture Displacement Measurement and Closed Reduction. Orthop. Surg. 2022, 14, 2545–2552. [Google Scholar] [CrossRef]
- Xiang, G.; Dong, X.; Jiang, X.; Cai, L.; Wang, J.; Guo, X.; Xiao, J.; Feng, Y. Comparison of percutaneous cross screw fixation versus open reduction and internal fixation for pelvic Day type II crescent fracture-dislocation: Case-control study. J. Orthop. Surg. Res. 2021, 16, 36. [Google Scholar] [CrossRef]
- Johnson, T.S. The spur sign. Radiology 2005, 235, 1023–1024. [Google Scholar] [CrossRef] [PubMed]
| Lateral Compression Fracture (n = 32) | Anterior Sacroiliac Fracture Dislocation (n = 15) | |
|---|---|---|
| Pseudo spur sign | 1 (3) | 14 (93) |
| Override of ilium on sacrum | 0 | 6 (40) |
| Keystone fragment | 3 (9) | 9 (60) |
| Wink sign | 2 (6) | 13 (87) |
| Vessel injury treated with embolization | 3 (9) | 1 (7) |
| Preperitoneal pelvic packing | 10 (31) | 4 (27) |
| Lateral Compression Fracture | Anterior Sacroiliac Fracture Dislocation | ||
|---|---|---|---|
| Mean ± SD | Mean ± SD | p-value | |
| Pre-operative vertical displacement | 1.9 ± 9.0 mm | 9.5 ± 10.1 mm | 0.013 † |
| Post-operative vertical displacement | −0.5 ± 5.9 mm | 4.7 ± 12.0 mm | 0.061 |
| Pre-operative asymmetry ratio (X − Y)/(X + Y) | 4.1 ± 3.2% | 7.8 ± 5.3% | 0.006 † |
| Post-operative asymmetry ratio | 3.8 ± 2.9% | 4.5 ± 3.1% | 0.462 |
| Lateral Compression 2 (n = 32) | Anterior Sacroiliac Fracture Dislocation (n = 15) | |
|---|---|---|
| Day 1 | 3 (9) | 12 (80) |
| Day 2 | 7 (21) | 2 (13) |
| Day 3 | 22 (68) | 1 (7) |
| ICC (95% CI) | p-Value | |
|---|---|---|
| Angle of crescent fracture line | 0.989 (0.980–0.994) | <0.001 |
| Pre-operative vertical displacement | 0.913 (0.847–0.951) | <0.001 |
| Post-operative vertical displacement | 0.842 (0.732–0.906) | <0.001 |
| Pre-operative asymmetry ratio | 0.917 (0.857–0.952) | <0.001 |
| Post-operative asymmetry ratio | 0.893 (0.815–0.939) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chun, Y.-S.; Kwon, K.-E.; Lee, S.-W. Anterior Sacroiliac Fracture Dislocation: A Comparative Radiologic analysis of Crescent Fractures in Pelvic Ring Injuries: A Retrospective Study. Medicina 2024, 60, 1375. https://doi.org/10.3390/medicina60081375
Chun Y-S, Kwon K-E, Lee S-W. Anterior Sacroiliac Fracture Dislocation: A Comparative Radiologic analysis of Crescent Fractures in Pelvic Ring Injuries: A Retrospective Study. Medicina. 2024; 60(8):1375. https://doi.org/10.3390/medicina60081375
Chicago/Turabian StyleChun, You-Seung, Kyeong-Eon Kwon, and Se-Won Lee. 2024. "Anterior Sacroiliac Fracture Dislocation: A Comparative Radiologic analysis of Crescent Fractures in Pelvic Ring Injuries: A Retrospective Study" Medicina 60, no. 8: 1375. https://doi.org/10.3390/medicina60081375
APA StyleChun, Y.-S., Kwon, K.-E., & Lee, S.-W. (2024). Anterior Sacroiliac Fracture Dislocation: A Comparative Radiologic analysis of Crescent Fractures in Pelvic Ring Injuries: A Retrospective Study. Medicina, 60(8), 1375. https://doi.org/10.3390/medicina60081375







