Oncologic Outcomes after Percutaneous Ablation for Colorectal Liver Metastases: An Updated Comprehensive Review
Abstract
Simple Summary
Abstract
1. Introduction
2. Percutaneous Ablation Modalities
2.1. Radiofrequency Ablation
2.2. Microwave Ablation
2.3. Cryoablation
2.4. Irreversible Electroporation
2.5. Histotripsy
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Siegel, R.L.; Wagle, N.S.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal cancer statistics, 2023. CA Cancer J. Clin. 2023, 73, 233–254. [Google Scholar] [CrossRef] [PubMed]
- Wolf, A.M.D.; Fontham, E.T.H.; Church, T.R.; Flowers, C.R.; Guerra, C.E.; LaMonte, S.J.; Etzioni, R.; McKenna, M.T.; Oeffinger, K.C.; Shih, Y.T.; et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J. Clin. 2018, 68, 250–281. [Google Scholar] [CrossRef] [PubMed]
- Helling, T.S.; Martin, M. Cause of Death from Liver Metastases in Colorectal Cancer. Ann. Surg. Oncol. 2014, 21, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Shady, W.; Petre, E.N.; Gonen, M.; Erinjeri, J.P.; Brown, K.T.; Covey, A.M.; Alago, W.; Durack, J.C.; Maybody, M.; Brody, L.A.; et al. Percutaneous Radiofrequency Ablation of Colorectal Cancer Liver Metastases: Factors Affecting Outcomes—A 10-year Experience at a Single Center. Radiology 2016, 278, 601–611. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. Colon Cancer Version 1.2024. 2024. Available online: https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf (accessed on 20 July 2024).
- Kurilova, I.; Bendet, A.; Petre, E.N.; Boas, F.E.; Kaye, E.; Gonen, M.; Covey, A.; Brody, L.A.; Brown, K.T.; Kemeny, N.E.; et al. Factors Associated With Local Tumor Control and Complications After Thermal Ablation of Colorectal Cancer Liver Metastases: A 15-year Retrospective Cohort Study. Clin. Color. Cancer. 2021, 20, e82–e95. [Google Scholar] [CrossRef]
- Meijerink, M.R.; Puijk, R.S.; van Tilborg, A.A.J.M.; Henningsen, K.H.; Fernandez, L.G.; Neyt, M.; Heymans, J.; Frankema, J.S.; de Jong, K.P.; Richel, D.J.; et al. Radiofrequency and Microwave Ablation Compared to Systemic Chemotherapy and to Partial Hepatectomy in the Treatment of Colorectal Liver Metastases: A Systematic Review and Meta-Analysis. Cardiovasc. Intervent. Radiol. 2018, 41, 1189–1204. [Google Scholar] [CrossRef]
- Glazer, D.I.; Tatli, S.; Shyn, P.B.; Vangel, M.G.; Tuncali, K.; Silverman, S.G. Percutaneous Image-Guided Cryoablation of Hepatic Tumors: Single-Center Experience With Intermediate to Long-Term Outcomes. Am. J. Roentgenol. 2017, 209, 1381–1389. [Google Scholar] [CrossRef]
- Ahmed, M.; Brace, C.L.; Lee, F.T.; Goldberg, S.N. Principles of and Advances in Percutaneous Ablation. Radiology 2011, 258, 351–369. [Google Scholar] [CrossRef]
- McGahan, J.P.; Gu, W.Z.; Brock, J.M.; Tesluk, H.; Darryl Jones, C. Hepatic ablation using bipolar radiofrequency electrocautery. Acad. Radiol. 1996, 3, 418–422. [Google Scholar] [CrossRef]
- Organ, L.W. Electrophysiologic Principles of Radiofrequency Lesion Making. Ster. Funct. Neurosurg. 1976, 39, 69–76. [Google Scholar] [CrossRef]
- Hong, K.; Georgiades, C. Radiofrequency Ablation: Mechanism of Action and Devices. J. Vasc. Interv. Radiol. 2010, 21, S179–S186. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, S.N.; Hahn, P.F.; Tanabe, K.K.; Mueller, P.R.; Schima, W.; Athanasoulis, C.A.; Compton, C.C.; Solbiati, L.; Gazelle, G.S. Percutaneous Radiofrequency Tissue Ablation: Does Perfusion-mediated Tissue Cooling Limit Coagulation Necrosis? J. Vasc. Interv. Radiol. 1998, 9, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Tatli, S.; Tapan, U.; Morrison, P.R.; Silverman, S.G. Radiofrequency ablation: Technique and clinical applications. Diagn. Interv. Radiol. 2012, 18, 508–516. [Google Scholar] [CrossRef] [PubMed]
- Sofocleous, C.T.; Petre, E.N.; Gonen, M.; Brown, K.T.; Solomon, S.B.; Covey, A.M.; Alago, W.; Brody, L.A.; Thornton, R.H.; D’Angelica, M.; et al. CT-guided Radiofrequency Ablation as a Salvage Treatment of Colorectal Cancer Hepatic Metastases Developing after Hepatectomy. J. Vasc. Interv. Radiol. 2011, 22, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Elias, D.; De Baere, T.; Smayra, T.; Ouellet, J.F.; Roche, A.; Lasser, P. Percutaneous radiofrequency thermoablation as an alternative to surgery for treatment of liver tumour recurrence after hepatectomy. Br. J. Surg. 2002, 89, 752–756. [Google Scholar] [CrossRef]
- Solbiati, L.; Livraghi, T.; Goldberg, S.N.; Ierace, T.; Meloni, F.; Dellanoce, M.; Cova, L.; Halpern, E.F.; Gazelle, G.S. Percutaneous Radio-frequency Ablation of Hepatic Metastases from Colorectal Cancer: Long-term Results in 117 Patients. Radiology 2001, 221, 159–166. [Google Scholar] [CrossRef]
- Solbiati, L.; Ahmed, M.; Cova, L.; Ierace, T.; Brioschi, M.; Goldberg, S.N. Small Liver Colorectal Metastases Treated with Percutaneous Radiofrequency Ablation: Local Response Rate and Long-term Survival with Up to 10-year Follow-up. Radiology 2012, 265, 958–968. [Google Scholar] [CrossRef]
- Pereira, P.L.; Siemou, P.; Rempp, H.J.; Hoffmann, R.; Hoffmann, R.T.; Kettenbach, J.; Clasen, S.; Helmberger, T. CT versus MR guidance for radiofrequency ablation in patients with colorectal liver metastases: A 10-year follow-up favors MR guidance. Eur. Radiol. 2023, 34, 4663–4671. [Google Scholar] [CrossRef]
- Ruers, T.; Van Coevorden, F.; Punt, C.J.A.; Pierie, J.P.E.N.; Borel-Rinkes, I.; Ledermann, J.A.; Poston, G.; Bechstein, W.; Lentz, M.A.; Mauer, M.; et al. Local Treatment of Unresectable Colorectal Liver Metastases: Results of a Randomized Phase II Trial. JNCI J. Natl. Cancer Inst. 2017, 109, djx015. [Google Scholar] [CrossRef]
- Yang, G.; Wang, G.; Sun, J.; Xiong, Y.; Li, W.; Tang, T.; Li, J. The prognosis of radiofrequency ablation versus hepatic resection for patients with colorectal liver metastases: A systematic review and meta-analysis based on 22 studies. Int. J. Surg. 2021, 87, 105896. [Google Scholar] [CrossRef]
- Leblanc, F.; Fonck, M.; Brunet, R.; Becouarn, Y.; Mathoulin-Pélissier, S.; Evrard, S. Comparison of hepatic recurrences after resection or intraoperative radiofrequency ablation indicated by size and topographical characteristics of the metastases. Eur. J. Surg. Oncol. 2008, 34, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.M.; Paolucci, I.; Brock, K.K.; Odisio, B.C. Image-Guided Ablation for Colorectal Liver Metastasis: Principles, Current Evidence, and the Path Forward. Cancers 2021, 13, 3926. [Google Scholar] [CrossRef] [PubMed]
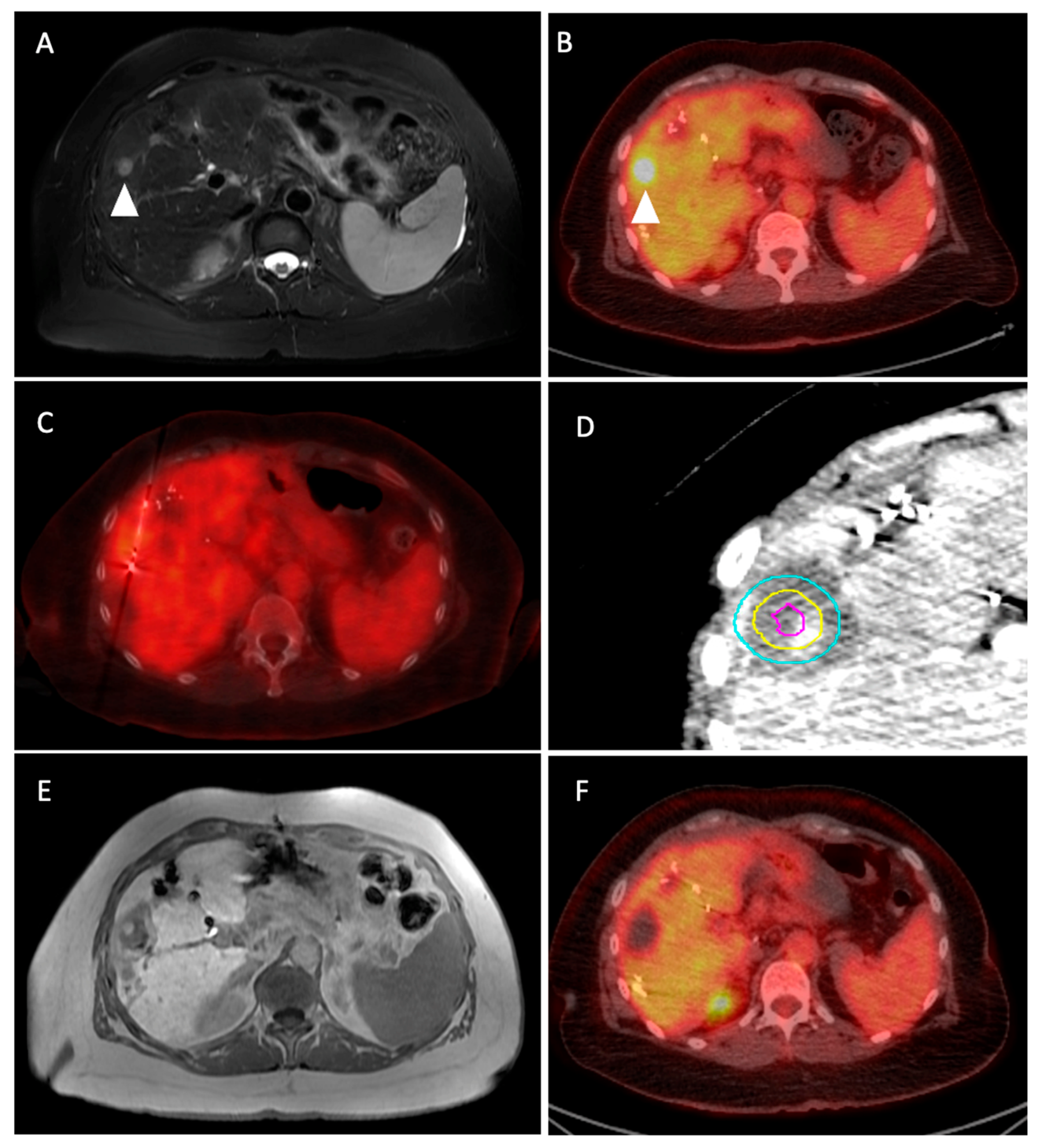
- Chlorogiannis, D.D.; Moussa, A.M.; Zhao, K.; Alexander, E.S.; Sofocleous, C.T.; Sotirchos, V.S. Imaging Considerations before and after Liver-Directed Locoregional Treatments for Metastatic Colorectal Cancer. Diagnostics 2024, 14, 772. [Google Scholar] [CrossRef] [PubMed]
- Calandri, M.; Yamashita, S.; Gazzera, C.; Fonio, P.; Veltri, A.; Bustreo, S.; Sheth, R.A.; Yevich, S.M.; Vauthey, J.N.; Odisio, B.C. Ablation of colorectal liver metastasis: Interaction of ablation margins and RAS mutation profiling on local tumour progression-free survival. Eur. Radiol. 2018, 28, 2727–2734. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Kim, J.H.; Yang, S.G.; Park, S.H.; Choi, H.K.; Chun, S.Y.; Kim, P.N.; Park, J.; Lee, M. A Single-Center Retrospective Analysis of Periprocedural Variables Affecting Local Tumor Progression after Radiofrequency Ablation of Colorectal Cancer Liver Metastases. Radiology 2021, 298, 212–218. [Google Scholar] [CrossRef]
- Yu, J.; Liang, P.; Yu, X.; Cheng, Z.; Han, Z.; Mu, M.; Li, Q.; Liu, Y. Local tumour progression after ultrasound-guided microwave ablation of liver malignancies: Risk factors analysis of 2529 tumours. Eur. Radiol. 2015, 25, 1119–1126. [Google Scholar] [CrossRef]
- Shady, W.; Petre, E.N.; Do, K.G.; Gonen, M.; Yarmohammadi, H.; Brown, K.T.; Kemeny, N.E.; D’Angelica, M.; Kingham, P.T.; Solomon, S.B.; et al. Percutaneous Microwave versus Radiofrequency Ablation of Colorectal Liver Metastases: Ablation with Clear Margins (A0) Provides the Best Local Tumor Control. J. Vasc. Interv. Radiol. 2018, 29, 268–275.e1. [Google Scholar] [CrossRef]
- Janne d’Othée, B.; Sofocleous, C.T.; Hanna, N.; Lewandowski, R.J.; Soulen, M.C.; Vauthey, J.N.; Cohen, S.J.; Venook, A.P.; Johnson, M.S.; Kennedy, A.S.; et al. Development of a Research Agenda for the Management of Metastatic Colorectal Cancer: Proceedings from a Multidisciplinary Research Consensus Panel. J. Vasc. Interv. Radiol. 2012, 23, 153–163. [Google Scholar] [CrossRef]
- Chlorogiannis, D.D.; Sotirchos, V.S.; Georgiades, C.; Filippiadis, D.; Arellano, R.S.; Gonen, M.; Makris, G.C.; Garg, T.; Sofocleous, C.T. The Importance of Optimal Thermal Ablation Margins in Colorectal Liver Metastases: A Systematic Review and Meta-Analysis of 21 Studies. Cancers 2023, 15, 5806. [Google Scholar] [CrossRef]
- Sotirchos, V.S.; Petrovic, L.M.; Gönen, M.; Klimstra, D.S.; Do, R.K.G.; Petre, E.N.; Garcia, A.R.; Barlas, A.; Erinjeri, J.P.; Brown, K.T.; et al. Colorectal Cancer Liver Metastases: Biopsy of the Ablation Zone and Margins Can Be Used to Predict Oncologic Outcome. Radiology 2016, 280, 949–959. [Google Scholar] [CrossRef]
- Vasiniotis Kamarinos, N.; Vakiani, E.; Gonen, M.; Kemeny, N.E.; Sigel, C.; Saltz, L.B.; Brown, K.T.; Covey, A.M.; Erinjeri, J.P.; Brody, L.A.; et al. Biopsy and Margins Optimize Outcomes after Thermal Ablation of Colorectal Liver Metastases. Cancers 2022, 14, 693. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, K.; van Tilborg, A.A.J.M.; Meijerink, M.R.; Macintosh, M.O.; Zonderhuis, B.M.; de Lange, E.S.M.; Comans, E.F.I.; Meijer, S.; van den Tol, M.P. Incidence and Treatment of Local Site Recurrences Following RFA of Colorectal Liver Metastases. World J. Surg. 2013, 37, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, M.; van der Lei, S.; Puijk, R.S.; Schulz, H.H.; Vos, D.J.W.; Timmer, F.E.F.; Scheffer, H.J.; Buffart, T.E.; van den Tol, M.P.; Lissenberg-Witte, B.I.; et al. Efficacy of Thermal Ablation for Small-Size (0–3 cm) versus Intermediate-Size (3–5 cm) Colorectal Liver Metastases: Results from the Amsterdam Colorectal Liver Met Registry (AmCORE). Cancers 2023, 15, 4346. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuizen, S.; Dijkstra, M.; Puijk, R.S.; Geboers, B.; Ruarus, A.H.; Schouten, E.A.; Nielsen, K.; de Vries, J.J.J.; Bruynzeel, A.M.E.; Scheffer, H.J.; et al. Microwave Ablation, Radiofrequency Ablation, Irreversible Electroporation, and Stereotactic Ablative Body Radiotherapy for Intermediate Size (3–5 cm) Unresectable Colorectal Liver Metastases: A Systematic Review and Meta-analysis. Curr. Oncol. Rep. 2022, 24, 793–808. [Google Scholar] [CrossRef] [PubMed]
- Simon, C.J.; Dupuy, D.E.; Mayo-Smith, W.W. Microwave Ablation: Principles and Applications. Radiographics 2005, 25, S69–S83. [Google Scholar] [CrossRef]
- Lubner, M.G.; Brace, C.L.; Hinshaw, J.L.; Lee, F.T. Microwave Tumor Ablation: Mechanism of Action, Clinical Results, and Devices. J. Vasc. Interv. Radiol. 2010, 21, S192–S203. [Google Scholar] [CrossRef]
- Gala, K.B.; Shetty, N.S.; Patel, P.; Kulkarni, S.S. Microwave ablation: How we do it? Indian J. Radiol. Imaging 2020, 30, 206–213. [Google Scholar] [CrossRef]
- Barrow, B.; Martin, R.C.G., II. Microwave ablation for hepatic malignancies: A systematic review of the technology and differences in devices. Surg. Endosc. 2023, 37, 817–834. [Google Scholar] [CrossRef]
- Dou, J.; Yu, J.; Yang, X.; Cheng, Z.; Han, Z.; Liu, F.; Yu, X.; Liang, P. Outcomes of microwave ablation for hepatocellular carcinoma adjacent to large vessels: A propensity score analysis. Oncotarget 2017, 8, 28758–28768. [Google Scholar] [CrossRef]
- Huang, S.; Yu, J.; Liang, P.; Yu, X.; Cheng, Z.; Han, Z.; Li, Q. Percutaneous microwave ablation for hepatocellular carcinoma adjacent to large vessels: A long-term follow-up. Eur. J. Radiol. 2014, 83, 552–558. [Google Scholar] [CrossRef]
- Vogl, T.J.; Jaraysa, Y.; Martin, S.S.; Gruber-Rouh, T.; Savage, R.H.; Nour-Eldin, N.E.A.; Mehmedovic, A. A prospective randomized trial comparing microwave and radiofrequency ablation for the treatment of liver metastases using a dual ablation system─The Mira study. Eur. J. Radiol. Open 2022, 9, 100399. [Google Scholar] [CrossRef] [PubMed]
- Di Martino, M.; Rompianesi, G.; Mora-Guzmán, I.; Martín-Pérez, E.; Montalti, R.; Troisi, R.I. Systematic review and meta-analysis of local ablative therapies for resectable colorectal liver metastases. Eur. J. Surg. Oncol. 2020, 46, 772–781. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Zhong, H.; Wang, Y.; Wu, J.; Zheng, J. Efficacy of microwave ablation versus radiofrequency ablation in the treatment of colorectal liver metastases: A systematic review and meta-analysis. Clin. Res. Hepatol. Gastroenterol. 2023, 47, 102182. [Google Scholar] [CrossRef] [PubMed]
- Georgiades, C.S.; Marx, J.K. Cryoablation: Mechanism of action and devices. In Percutaneous Tumor Ablation. Strategies and Techniques; Hong, K., Georgiades, C.S., Eds.; Thieme: Stuttgart, Germany, 2011; pp. 15–26. [Google Scholar]
- Erinjeri, J.P.; Clark, T.W.I. Cryoablation: Mechanism of Action and Devices. J. Vasc. Interv. Radiol. 2010, 21, S187–S191. [Google Scholar] [CrossRef] [PubMed]
- Werner, J.D.; Tregnago, A.C.; Netto, G.J.; Frangakis, C.; Georgiades, C.S. Single 15-Min Protocol Yields the Same Cryoablation Size and Margin as the Conventional 10–8–10-Min Protocol: Results of Kidney and Liver Swine Experiment. Cardiovasc. Interv. Radiol. 2018, 41, 1089–1094. [Google Scholar] [CrossRef]
- Young, S.; Abamyan, A.; Goldberg, D.; Hannallah, J.; Schaub, D.; Kalarn, S.; Fitzgerald, Z.; Woodhead, G. Cryoablation in the liver: How accurately does the iceball predict the ablation zone? Abdom. Radiol. 2023, 49, 625–630. [Google Scholar] [CrossRef]
- Adam, R. A Comparison of Percutaneous Cryosurgery and Percutaneous Radiofrequency for Unresectable Hepatic Malignancies. Arch. Surg. 2002, 137, 1332. [Google Scholar] [CrossRef]
- Xu, K.C.; Niu, L.Z.; He, W.B.; Hu, Y.Z.; Zuo, J.S. Percutaneous cryosurgery for the treatment of hepatic colorectal metastases. World J. Gastroenterol 2008, 14, 1430. [Google Scholar] [CrossRef]
- Dijkstra, M.; Nieuwenhuizen, S.; Puijk, R.S.; Timmer, F.E.F.; Geboers, B.; Schouten, E.A.C.; Opperman, J.; Scheffer, H.J.; Vries, J.J.J.; Swijnenburg, R.J.; et al. Thermal Ablation Compared to Partial Hepatectomy for Recurrent Colorectal Liver Metastases: An Amsterdam Colorectal Liver Met Registry (AmCORE) Based Study. Cancers 2021, 13, 2769. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Littrup, P.J.; Aoun, H.D.; Adam, B.; Krycia, M.; Prus, M.; Shields, A. Percutaneous cryoablation of hepatic tumors: Long-term experience of a large U.S. series. Abdom. Radiol. 2016, 41, 767–780. [Google Scholar] [CrossRef]
- Khanmohammadi, S.; Behnoush, A.H.; Akhlaghpoor, S. Survival outcomes and quality of life after percutaneous cryoablation for liver metastasis: A systematic review and meta-analysis. PLoS ONE 2023, 18, e0289975. [Google Scholar] [CrossRef]
- Narayanan, G. Irreversible Electroporation. Semin. Interv. Radiol. 2015, 32, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Ruarus, A.H.; Vroomen, L.G.P.H.; Puijk, R.S.; Scheffer, H.J.; Zonderhuis, B.M.; Kazemier, G.; van den Tol, M.P.; Berger, F.H.; Meijerink, M.R. Irreversible Electroporation in Hepatopancreaticobiliary Tumours. Can. Assoc. Radiol. J. 2018, 69, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.W.; Wong, D.; Prikhodko, S.V.; Perez, A.; Tran, C.; Loh, C.T.; Kee, S.T. Electron Microscopic Demonstration and Evaluation of Irreversible Electroporation-Induced Nanopores on Hepatocyte Membranes. J. Vasc. Interv. Radiol. 2012, 23, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Petre, E.N.; Sofocleous, C.T.; Solomon, S.B. Ablative and Catheter-Directed Therapies for Colorectal Liver and Lung Metastases. Hematol. Oncol. Clin. N. Am. 2015, 29, 117–133. [Google Scholar] [CrossRef] [PubMed]
- Yun, J.H.; Fang, A.; Khorshidi, F.; Habibollahi, P.; Kutsenko, O.; Etezadi, V.; Hunt, S.; Nezami, N. New Developments in Image-Guided Percutaneous Irreversible Electroporation of Solid Tumors. Curr. Oncol. Rep. 2023, 25, 1213–1226. [Google Scholar] [CrossRef] [PubMed]
- Silk, M.T.; Wimmer, T.; Lee, K.S.; Srimathveeravalli, G.; Brown, K.T.; Kingham, P.T.; Fong, Y.; Durack, J.C.; Sofocleous, C.T.; Solomon, S.B. Percutaneous Ablation of Peribiliary Tumors with Irreversible Electroporation. J. Vasc. Interv. Radiol. 2014, 25, 112–118. [Google Scholar] [CrossRef]
- O’Neill, C.H.; Martin, R.C.G. Cardiac synchronization and arrhythmia during irreversible electroporation. J. Surg. Oncol. 2020, 122, 407–411. [Google Scholar] [CrossRef]
- Scheffer, H.J.; Nielsen, K.; van Tilborg, A.A.J.M.; Vieveen, J.M.; Bouwman, R.A.; Kazemier, G.; Niessen, H.W.M.; Meijer, S.; van Kuijk, C.; van den Tol, M.P.; et al. Ablation of colorectal liver metastases by irreversible electroporation: Results of the COLDFIRE-I ablate-and-resect study. Eur. Radiol. 2014, 24, 2467–2475. [Google Scholar] [CrossRef]
- Scheffer, H.J.; Vroomen, L.G.P.H.; Nielsen, K.; van Tilborg, A.A.J.M.; Comans, E.F.I.; van Kuijk, C.; van der Meijs, B.B.; van den Bergh, J.; van den Tol, P.M.P.; Meijerink, M.R. Colorectal liver metastatic disease: Efficacy of irreversible electroporation—A single-arm phase II clinical trial (COLDFIRE-2 trial). BMC Cancer 2015, 15, 772. [Google Scholar] [CrossRef]
- Spiers, H.V.M.; Lancellotti, F.; de Liguori Carino, N.; Pandanaboyana, S.; Frampton, A.E.; Jegatheeswaran, S.; Nadarajah, V.; Siriwardena, A.K. Irreversible Electroporation for Liver Metastases from Colorectal Cancer: A Systematic Review. Cancers 2023, 15, 2428. [Google Scholar] [CrossRef] [PubMed]
- Frühling, P.; Stillström, D.; Holmquist, F.; Nilsson, A.; Freedman, J. Irreversible electroporation of hepatocellular carcinoma and colorectal cancer liver metastases: A nationwide multicenter study with short- and long-term follow-up. Eur. J. Surg. Oncol. 2023, 49, 107046. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, G.; Gentile, N.T.; Eyshi, J.; Schiro, B.J.; Gandhi, R.T.; Peña, C.S.; Ucar, A.; Aparo, S.; de Zarraga, F.I.; Joseph, S.N.; et al. Irreversible Electroporation in Treating Colorectal Liver Metastases in Proximity to Critical Structures. J. Vasc. Interv. Radiol. 2024, in press. [CrossRef] [PubMed]
- Pahk, K.J.; Gélat, P.; Kim, H.; Saffari, N. Bubble dynamics in boiling histotripsy. Ultrasound Med. Biol. 2018, 44, 2673–2696. [Google Scholar] [CrossRef] [PubMed]
- Bader, K.B.; Vlaisavljevich, E.; Maxwell, A.D. For Whom the Bubble Grows: Physical Principles of Bubble Nucleation and Dynamics in Histotripsy Ultrasound Therapy. Ultrasound Med. Biol. 2019, 45, 1056–1080. [Google Scholar] [CrossRef]
- Smolock, A.R.; Cristescu, M.M.; Vlaisavljevich, E.; Gendron-Fitzpatrick, A.; Green, C.; Cannata, J.; Ziemlewicz, T.J.; Lee, F.T. Robotically Assisted Sonic Therapy as a Noninvasive Nonthermal Ablation Modality: Proof of Concept in a Porcine Liver Model. Radiology 2018, 287, 485–493. [Google Scholar] [CrossRef]
- Xu, Z.; Hall, T.L.; Vlaisavljevich, E.; Lee, F.T. Histotripsy: The first noninvasive, non-ionizing, non-thermal ablation technique based on ultrasound. Int. J. Hyperth. 2021, 38, 561–575. [Google Scholar] [CrossRef]
- Vidal-Jove, J.; Serres, X.; Vlaisavljevich, E.; Cannata, J.; Duryea, A.; Miller, R.; Merino, X.; Velat, M.; Kam, Y.; Bolduan, R.; et al. First-in-man histotripsy of hepatic tumors: The THERESA trial, a feasibility study. Int. J. Hyperth. 2022, 39, 1115–1123. [Google Scholar] [CrossRef]
- Mendiratta-Lala, M.; Wiggermann, P.; Pech, M.; Serres-Créixams, X.; White, S.B.; Davis, C.; Ahmed, O.; Parikh, N.D.; Planert, M.; Thormann, M.; et al. The #HOPE4LIVER Single-Arm Pivotal Trial for Histotripsy of Primary and Metastatic Liver Tumors. Radiology 2024, 312, e233051. [Google Scholar]
- Wah, T.M.; Pech, M.; Thormann, M.; Serres, X.; Littler, P.; Stenberg, B.; Lenton, J.; Smith, J.; Wiggermann, P.; Planert, M.; et al. A Multi-centre, Single Arm, Non-randomized, Prospective European Trial to Evaluate the Safety and Efficacy of the HistoSonics System in the Treatment of Primary and Metastatic Liver Cancers (#HOPE4LIVER). Cardiovasc. Interv. Radiol 2023, 46, 259–267. [Google Scholar]
- Vulasala, S.S.R.; Sutphin, P.D.; Kethu, S.; Onteddu, N.K.; Kalva, S.P. Interventional radiological therapies in colorectal hepatic metastases. Front. Oncol. 2023, 13, 963966. [Google Scholar] [CrossRef] [PubMed]
- Zensen, S.; Bücker, A.; Meetschen, M.; Haubold, J.; Opitz, M.; Theysohn, J.M.; Schramm, S.; Jochheim, L.; Kasper, S.; Forsting, M.; et al. Current use of percutaneous image-guided tumor ablation for the therapy of liver tumors: Lessons learned from the registry of the German Society for Interventional Radiology and Minimally Invasive Therapy (DeGIR) 2018–2022. Eur. Radiol. 2023, 34, 3322–3330. [Google Scholar] [CrossRef] [PubMed]
- Dodd, G.D.; Dodd, N.A.; Lanctot, A.C.; Glueck, D.A. Effect of Variation of Portal Venous Blood Flow on Radiofrequency and Microwave Ablations in a Blood-perfused Bovine Liver Model. Radiology 2013, 267, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Ierardi, A.M.; Floridi, C.; Fontana, F.; Chini, C.; Giorlando, F.; Piacentino, F.; Brunese, L.; Pinotti, G.; Bacuzzi, A.; Carrafiello, G. Microwave ablation of liver metastases to overcome the limitations of radiofrequency ablation. Radiol. Med. 2013, 118, 949–961. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, N.; Strickland, A.D.; Ahmad, F.; Atanesyan, L.; West, K.; Lloyd, D.M. A comparative histological evaluation of the ablations produced by microwave, cryotherapy and radiofrequency in the liver. Pathology 2009, 41, 168–172. [Google Scholar] [CrossRef]
- Huang, J.; Silverman, S.G.; Shyn, P.B. Cryoablation of Liver Tumors. In Interventional Oncology; Springer International Publishing: Cham, Germany, 2024; pp. 1–19. [Google Scholar]
- Nair, R.T.; Silverman, S.G.; Tuncali, K.; Obuchowski, N.A.; vanSonnenberg, E.; Shankar, S. Biochemical and Hematologic Alterations Following Percutaneous Cryoablation of Liver Tumors: Experience in 48 Procedures. Radiology 2008, 248, 303–311. [Google Scholar] [CrossRef]
- Pearson, A.S.; Izzo, F.; Fleming, R.Y.D.; Ellis, L.M.; Delrio, P.; Roh, M.S.; Granchi, J.; Curley, S.A. Intraoperative radiofrequency ablation or cryoablation for hepatic malignancies. Am. J. Surg. 1999, 178, 592–598. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chlorogiannis, D.-D.; Sotirchos, V.S.; Sofocleous, C.T. Oncologic Outcomes after Percutaneous Ablation for Colorectal Liver Metastases: An Updated Comprehensive Review. Medicina 2024, 60, 1536. https://doi.org/10.3390/medicina60091536
Chlorogiannis D-D, Sotirchos VS, Sofocleous CT. Oncologic Outcomes after Percutaneous Ablation for Colorectal Liver Metastases: An Updated Comprehensive Review. Medicina. 2024; 60(9):1536. https://doi.org/10.3390/medicina60091536
Chicago/Turabian StyleChlorogiannis, David-Dimitris, Vlasios S. Sotirchos, and Constantinos T. Sofocleous. 2024. "Oncologic Outcomes after Percutaneous Ablation for Colorectal Liver Metastases: An Updated Comprehensive Review" Medicina 60, no. 9: 1536. https://doi.org/10.3390/medicina60091536
APA StyleChlorogiannis, D.-D., Sotirchos, V. S., & Sofocleous, C. T. (2024). Oncologic Outcomes after Percutaneous Ablation for Colorectal Liver Metastases: An Updated Comprehensive Review. Medicina, 60(9), 1536. https://doi.org/10.3390/medicina60091536







