Transforming Life: A Broad View of the Developmental Origins of Health and Disease Concept from an Ecological Justice Perspective
Abstract
:1. Introduction: Mere Survival Is Not Enough
“But the quality of the environment cannot be measured only in terms of gross defects such as air, water, or food pollution. Environmental conditions experienced early in life (including the formative months before birth) cause the most profound and lasting changes in man...the maintenance of biological and mental health requires that technological societies provide in some form the biological freedom enjoyed by our Paleolithic ancestors.”Rene Dubos, 1970 [1]
2. Roadmap to the Current Review
3. Ecological Justice as a Basic Human Right
4. Defining Grey Space and the Green Distinction
5. Broadening Developmental Origins of Disease Paradigms
6. Mental Health, Societal Health: Avoiding Mother Blame
7. The Prism of Socioeconomic Gradient
8. Lifestyle Factors: The Vicious Cycle of Ill-Health
9. Disadvantage and the Cognitive Tax
10. Lifestyle and Delay (Temporal) Discounting: Future Rewards?
11. Positive Emotions and States: Neglected Discussion
12. Natural Environments, Missing Exposures Exaggerate Disparity
“Urban dwellers never have the chance to see the Milky Way, or a night radiant with stars, or even a truly blue sky. They never experience the subtle fragrances peculiar to each season; they lose the exhilaration of early spring and the delightful melancholy of autumn. The loss of these experiences is more than an aesthetic affliction; it corresponds to a deprivation of needs which are essential to physical and mental sanity, because they were indelibly woven in man’s fabric during his evolutionary past.”[165]
13. Nature Relatedness
14. Humans, Microbes, Environment as an Ecological Unit
“Thus, life in the world of nature, implying as it does endless contact with all kinds of microbes, early brings forth in animals an adaptive response”.[234]
15. Encephalobiotics, Promissory Notes
16. Hygiene Hypothesis, Dysbiotic Drift
17. Grey Space, Inequity and the Environmental Push
18. Walking in Grey Space
“A more disturbing aspect of modern science is that the specialist himself commonly loses contact with the aspect of reality which was his primary concern, whether it was matter, life or man”.[299]
19. Behavioral Reinforcement
20. Ecological Justice and the Erosion of Health
“The tendency to disregard ecology in medical research may have far reaching consequences. For example, it facilitates the interpretation of the “environment” as “psychosocial environment”. The study of the environment is then implicitly relegated to psychology and social science. No wonder then that mental illness, in the orthodox view, gets a biological interpretation which skimps ecology.”van der Steen and Thung. In Faces of Medicine: A Philosophical Study, 1988 [349]
21. Preparedness: Training Clinicians for Ecological Medicine
“This is wonderfully entertaining, titillating kind of science fiction. We organize meetings about it in all sorts of pleasant places to talk about this, and that saves us the responsibility of walking across the street, where 100,000 children are being poisoned every day by lead in paint…something can be done immediately about this problem, but it is not being done because it is not of sufficient interest or as exciting intellectually”.[386]
22. Transforming Life: From Epigenetics to Advocacy
“The study of man as an integrated unit, and of the ecosystems in which he functions, is grossly neglected…a very different kind of knowledge is needed to understand the nature of the cohesive forces which maintain man in an integrated state, physically, psychologically, and socially, and enable him to relate successfully to his environment.”Rene Dubos, 1965 [299]
“Developing counter technologies to correct new kinds of damage constantly being created by technological innovations is a policy of despair...we must try to imagine the kind of surroundings and of life we want, lest we end up with a jumble of technologies that will eventually smother body and soul.”[404]
23. Green Gentrification
24. Conclusions
“I am eighty years old as I write these lines…I am still vigorous enough not only to resent many aspects of modern civilization but more importantly to enjoy the world and have faith in its future...I have become convinced that resiliency is a universal attribute of all living organisms—from natural ecosystems to individual human beings; it is also one of the most important. In living organisms, resiliency implies the ability both to recover from traumatic experiences and to create new values during the very process of recovery”.[436]
Author Contributions
Conflicts of Interest
References
- Dubos, R. Mere survival is not enough for man. Life 1970, 69, 2. [Google Scholar]
- Dubos, R.; Savage, D.; Schaedler, R. Biological freudianism: Lasting effects of early environmental influences. Int. J. Epidemiol. 2005, 34, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Dubos, R. Man Adapting; Yale University Press: New Haven, CT, USA, 1965. [Google Scholar]
- Boehm, J.K.; Trudel-Fitzgerald, C.; Kivimaki, M.; Kubzansky, L.D. The prospective association between positive psychological well-being and diabetes. Health Psychol. 2015, 34, 1013–1021. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, R.; Kershaw, K.N.; Siddique, J.; Boehm, J.K.; Kubzansky, L.D.; Diez-Roux, A.; Ning, H.; Lloyd-Jones, D.M. Optimism and cardiovascular health: Multi-ethnic study of atherosclerosis (MESA). Health Behav. Policy Rev. 2015, 2, 62–73. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, M.; Isowa, T.; Yamakawa, K.; Tsuboi, H.; Kawanishi, Y.; Kaneko, H.; Kasugai, K.; Yoneda, M.; Ohira, H. Association between perceived happiness levels and peripheral circulating pro-inflammatory cytokine levels in middle-aged adults in Japan. Neuro Endocrinol. Lett. 2011, 32, 458–463. [Google Scholar] [PubMed]
- Sarris, J.; Logan, A.C.; Akbaraly, T.N.; Amminger, G.P.; Balanza-Martinez, V.; Freeman, M.P.; Hibbeln, J.; Matsuoka, Y.; Mischoulon, D.; Mizoue, T.; et al. Nutritional medicine as mainstream in psychiatry. Lancet Psychiatry 2015, 2, 271–274. [Google Scholar] [CrossRef]
- United Nations General Assembly. Convention on the rights of the child. In United Nations Treaty Series; United Nations General Assembly: New York, NY, USA, 1989; Volume 1577, p. 3. [Google Scholar]
- Corburn, J. Confronting the challenges in reconnecting urban planning and public health. Am. J. Public Health 2004, 94, 541–546. [Google Scholar] [CrossRef] [PubMed]
- Heindel, J.J.; Balbus, J.; Birnbaum, L.; Brune-Drisse, M.N.; Grandjean, P.; Gray, K.; Landrigan, P.J.; Sly, P.D.; Suk, W.; Cory Slechta, D.; et al. Developmental origins of health and disease: Integrating environmental influences. Endocrinology 2015, 156, 3416–3421. [Google Scholar] [CrossRef] [PubMed]
- Chavatte-Palmer, P.; Tarrade, A.; Rousseau-Ralliard, D. Diet before and during pregnancy and offspring health: The importance of animal models and what can be learned from them. Int. J. Environ. Res. Public Health 2016, 13, 586. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, M.C.; Pallares, M.E.; Ceccatelli, S.; Spulber, S. Long-term consequences of prenatal stress and neurotoxicants exposure on neurodevelopment. Prog. Neurobiol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Short, A.K.; Fennell, K.A.; Perreau, V.M.; Fox, A.; O’Bryan, M.K.; Kim, J.H.; Bredy, T.W.; Pang, T.Y.; Hannan, A.J. Elevated paternal glucocorticoid exposure alters the small noncoding rna profile in sperm and modifies anxiety and depressive phenotypes in the offspring. Transl. Psychiatry 2016, 6, e837. [Google Scholar] [CrossRef] [PubMed]
- Babenko, O.; Kovalchuk, I.; Metz, G.A. Stress-induced perinatal and transgenerational epigenetic programming of brain development and mental health. Neurosci. Biobehav. Rev. 2015, 48, 70–91. [Google Scholar] [CrossRef] [PubMed]
- Metz, G.A.; Ng, J.W.; Kovalchuk, I.; Olson, D.M. Ancestral experience as a game changer in stress vulnerability and disease outcomes. BioEssays News Rev. Mol. Cell. Dev. Biol. 2015, 37, 602–611. [Google Scholar] [CrossRef] [PubMed]
- Baxter, A.J.; Scott, K.M.; Ferrari, A.J.; Norman, R.E.; Vos, T.; Whiteford, H.A. Challenging the myth of an “epidemic” of common mental disorders: Trends in the global prevalence of anxiety and depression between 1990 and 2010. Depress Anxiety 2014, 31, 506–516. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Janicki-Deverts, D. Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J. Appl. Soc. Psychol. 2012, 42, 1320–1334. [Google Scholar]
- Boak, A.; Hamilton, H.A.; Adlaf, E.M.; Henderson, J.L.; Mann, R.E. The Mental Well-Being of Ontario Students, 1991–2015; CAMH Research Document No. 43; The Centre for Addiction and Mental Health: Toronto, ON, Canada, 2015. [Google Scholar]
- Rowlands, I.J.; Dobson, A.J.; Mishra, G.D. Physical health of young, australian women: A comparison of two national cohorts surveyed 17 years apart. PLoS ONE 2015, 10, e0142088. [Google Scholar] [CrossRef] [PubMed]
- Twenge, J.M. Time period and birth cohort differences in depressive symptoms in the U.S., 1982–2013. Soc. Indic Res. 2015, 121, 437–454. [Google Scholar] [CrossRef]
- Nordstrom, A.; Bodlund, O. Every third patient in primary care suffers from depression, anxiety or alcohol problems. Nord. J. Psychiatry 2008, 62, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Safer, D.J.; Rajakannan, T.; Burcu, M.; Zito, J.M. Trends in subthreshold psychiatric diagnoses for youth in community treatment. JAMA Psychiatry 2015, 72, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Roberts, R.E.; Fisher, P.W.; Turner, J.B.; Tang, M. Estimating the burden of psychiatric disorders in adolescence: The impact of subthreshold disorders. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Kim, B.N.; Cho, S.C.; Kim, J.W.; Shin, M.S.; Yoo, H.J. Prevalence, correlates, and comorbidities of DSM-IV psychiatric disorders in children in Seoul, Korea. Asia Pac. J. Public Health 2015, 27, NP1942–NP1951. [Google Scholar] [CrossRef] [PubMed]
- Haller, H.; Cramer, H.; Lauche, R.; Gass, F.; Dobos, G.J. The prevalence and burden of subthreshold generalized anxiety disorder: A systematic review. BMC Psychiatry 2014, 14, 128. [Google Scholar] [CrossRef] [PubMed]
- Rucci, P.; Gherardi, S.; Tansella, M.; Piccinelli, M.; Berardi, D.; Bisoffi, G.; Corsino, M.A.; Pini, S. Subthreshold psychiatric disorders in primary care: Prevalence and associated characteristics. J. Affect. Disord. 2003, 76, 171–181. [Google Scholar] [CrossRef]
- Twenge, J.M. Overwhelming evidence for generation me. Emerg. Adulthood 2013, 1, 21–26. [Google Scholar] [CrossRef]
- Saeed, A.; Raana, T.; Saeed, A.M.; Humayun, A. Effect of antenatal depression on maternal dietary intake and neonatal outcome: A prospective cohort. Nutr. J. 2016, 15, 64. [Google Scholar] [CrossRef] [PubMed]
- Liou, S.R.; Wang, P.; Cheng, C.Y. Effects of prenatal maternal mental distress on birth outcomes. Women Birth 2016, 29, 376–380. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, K.K.; Riley, L.; Castro, V.M.; Perlis, R.H.; Kaimal, A.J. Association of antenatal depression symptoms and antidepressant treatment with preterm birth. Obstet. Gynecol. 2016, 127, 926–933. [Google Scholar] [CrossRef] [PubMed]
- Nosarti, C.; Reichenberg, A.; Murray, R.M.; Cnattingius, S.; Lambe, M.P.; Yin, L.; MacCabe, J.; Rifkin, L.; Hultman, C.M. Preterm birth and psychiatric disorders in young adult life. Arch. Gen. Psychiatry 2012, 69, E1–E8. [Google Scholar] [CrossRef] [PubMed]
- Lund, L.K.; Vik, T.; Lydersen, S.; Lohaugen, G.C.; Skranes, J.; Brubakk, A.M.; Indredavik, M.S. Mental health, quality of life and social relations in young adults born with low birth weight. Health Qual. Life Outcomes 2012, 10, 146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hack, M.; Youngstrom, E.A.; Cartar, L.; Schluchter, M.; Taylor, H.G.; Flannery, D.; Klein, N.; Borawski, E. Behavioral outcomes and evidence of psychopathology among very low birth weight infants at age 20 years. Pediatrics 2004, 114, 932–940. [Google Scholar] [CrossRef] [PubMed]
- Boyle, M.H.; Miskovic, V.; van Lieshout, R.; Duncan, L.; Schmidt, L.A.; Hoult, L.; Paneth, N.; Saigal, S. Psychopathology in young adults born at extremely low birth weight. Psychol. Med. 2011, 41, 1763–1774. [Google Scholar] [CrossRef] [PubMed]
- Lund, L.K.; Vik, T.; Skranes, J.; Lydersen, S.; Brubakk, A.M.; Indredavik, M.S. Low birth weight and psychiatric morbidity; stability and change between adolescence and young adulthood. Early Hum. Dev. 2012, 88, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Abel, K.M.; Wicks, S.; Susser, E.S.; Dalman, C.; Pedersen, M.G.; Mortensen, P.B.; Webb, R.T. Birth weight, schizophrenia, and adult mental disorder: Is risk confined to the smallest babies? Arch. Gen. Psychiatry 2010, 67, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Moster, D.; Lie, R.T.; Markestad, T. Long-term medical and social consequences of preterm birth. N. Engl. J. Med. 2008, 359, 262–273. [Google Scholar] [CrossRef] [PubMed]
- D’Onofrio, B.M.; Class, Q.A.; Rickert, M.E.; Larsson, H.; Langstrom, N.; Lichtenstein, P. Preterm birth and mortality and morbidity: A population-based quasi-experimental study. JAMA Psychiatry 2013, 70, 1231–1240. [Google Scholar] [CrossRef] [PubMed]
- Monfils Gustafsson, W.; Josefsson, A.; Ekholm Selling, K.; Sydsjo, G. Preterm birth or foetal growth impairment and psychiatric hospitalization in adolescence and early adulthood in a Swedish population-based birth cohort. Acta Psychiatr. Scand. 2009, 119, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Raikkonen, K.; Pesonen, A.K.; Heinonen, K.; Kajantie, E.; Hovi, P.; Jarvenpaa, A.L.; Eriksson, J.G.; Andersson, S. Depression in young adults with very low birth weight: The Helsinki study of very low-birth-weight adults. Arch. Gen. Psychiatry 2008, 65, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Heinonen, K.; Raikkonen, K.; Pesonen, A.K.; Andersson, S.; Kajantie, E.; Eriksson, J.G.; Wolke, D.; Lano, A. Behavioural symptoms of attention deficit/hyperactivity disorder in preterm and term children born small and appropriate for gestational age: A longitudinal study. BMC Pediatr. 2010, 10, 91. [Google Scholar] [CrossRef] [PubMed]
- Strang-Karlsson, S.; Raikkonen, K.; Pesonen, A.K.; Kajantie, E.; Paavonen, E.J.; Lahti, J.; Hovi, P.; Heinonen, K.; Jarvenpaa, A.L.; Eriksson, J.G.; et al. Very low birth weight and behavioral symptoms of attention deficit hyperactivity disorder in young adulthood: The Helsinki study of very-low-birth-weight adults. Am. J. Psychiatry 2008, 165, 1345–1353. [Google Scholar] [CrossRef] [PubMed]
- Luby, J.L.; Gaffrey, M.S.; Tillman, R.; April, L.M.; Belden, A.C. Trajectories of preschool disorders to full DSM depression at school age and early adolescence: Continuity of preschool depression. Am. J. Psychiatry 2014, 171, 768–776. [Google Scholar] [CrossRef] [PubMed]
- Hill, R.M.; Pettit, J.W.; Lewinsohn, P.M.; Seeley, J.R.; Klein, D.N. Escalation to major depressive disorder among adolescents with subthreshold depressive symptoms: Evidence of distinct subgroups at risk. J. Affect. Disord. 2014, 158, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Goldney, R.D.; Fisher, L.J.; Dal Grande, E.; Taylor, A.W. Subsyndromal depression: Prevalence, use of health services and quality of life in an Australian population. Soc. Psychiatry Psychiatr. Epidemiol. 2004, 39, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, M.R.; Nuevo, R.; Chatterji, S.; Ayuso-Mateos, J.L. Definitions and factors associated with subthreshold depressive conditions: A systematic review. BMC Psychiatry 2012, 12, 181. [Google Scholar] [CrossRef] [PubMed]
- Braungart-Rieker, J.M.; Lefever, J.B.; Planalp, E.M.; Moore, E.S. Body mass index at 3 years of age: Cascading effects of prenatal maternal depression and mother-infant dynamics. J. Pediatr. 2016, 177, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Barroso, N.E.; Hartley, C.M.; Bagner, D.M.; Pettit, J.W. The effect of preterm birth on infant negative affect and maternal postpartum depressive symptoms: A preliminary examination in an underrepresented minority sample. Infant Behav. Dev. 2015, 39, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Winett, L.B.; Wulf, A.B.; Wallack, L. Framing strategies to avoid mother-blame in communicating the origins of chronic disease. Am. J. Public Health 2016, 106, 1369–1373. [Google Scholar] [CrossRef] [PubMed]
- Winett, L.; Wallack, L.; Richardson, D.; Boone-Heinonen, J.; Messer, L. A framework to address challenges in communicating the developmental origins of health and disease. Curr. Environ. Health Rep. 2016, 3, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Caruso, E.M.; Vohs, K.D.; Baxter, B.; Waytz, A. Mere exposure to money increases endorsement of free-market systems and social inequality. J. Exp. Psychol. Gen. 2013, 142, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Wright, D. More equal societies have less mental illness: What should therapists do on monday morning? Int. J. Soc. Psychiatry 2014, 60, 436–441. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, S.; Schrecker, T. The double burden of neoliberalism? Noncommunicable disease policies and the global political economy of risk. Health Place 2016, 39, 204–211. [Google Scholar] [PubMed]
- Prescott, S.L.; Logan, A.C.; Millstein, R.A.; Katszman, M.A. Biodiversity, the human microbiome and mental health: Moving toward a new clinical ecology for the 21st century? Int. J. Biodivers. 2016, 2016, 2718275. [Google Scholar] [CrossRef]
- Penkalla, A.M.; Kohler, S. Urbanicity and mental health in europe: A systematic review. Eur. J. Ment. Health 2014, 9, 163–177. [Google Scholar] [CrossRef]
- Hyland, P.; Shevlin, M.; Elklit, A.; Christoffersen, M.; Murphy, J. Social, familial and psychological risk factors for mood and anxiety disorders in childhood and early adulthood: A birth cohort study using the danish registry system. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.; Balfour, R.; Bell, R.; Marmot, M. Social determinants of mental health. Int. Rev. Psychiatry 2014, 26, 392–407. [Google Scholar] [CrossRef] [PubMed]
- Delobel-Ayoub, M.; Ehlinger, V.; Klapouszczak, D.; Maffre, T.; Raynaud, J.P.; Delpierre, C.; Arnaud, C. Socioeconomic disparities and prevalence of autism spectrum disorders and intellectual disability. PLoS ONE 2015, 10, e0141964. [Google Scholar] [CrossRef] [PubMed]
- Robinson, R.L.; Stephenson, J.J.; Dennehy, E.B.; Grabner, M.; Faries, D.; Palli, S.R.; Swindle, R.W. The importance of unresolved fatigue in depression: Costs and comorbidities. Psychosomatics 2015, 56, 274–285. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.; Donkin, A.M.M. Opportunities for reducing socioeconomic inequalities in the mental health of children and young people—Reducing adversity and increasing resilience. J. Public Ment. Health 2016, 15, 4–17. [Google Scholar] [CrossRef]
- Pickett, K.E.; Wilkinson, R.G. Inequality: An underacknowledged source of mental illness and distress. Br. J. Psychiatry J. Ment. Sci. 2010, 197, 426–428. [Google Scholar] [CrossRef] [PubMed]
- Tiikkaja, S.; Sandin, S.; Hultman, C.M.; Modin, B.; Malki, N.; Sparen, P. Psychiatric disorder and work life: A longitudinal study of intra-generational social mobility. Int. J. Soc. Psychiatry 2016, 62, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Fuller-Thomson, E.; Agbeyaka, S.; LaFond, D.M.; Bern-Klug, M. Flourishing after depression: Factors associated with achieving complete mental health among those with a history of depression. Psychiatry Res. 2016, 242, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Bonet, M.; Smith, L.K.; Pilkington, H.; Draper, E.S.; Zeitlin, J. Neighbourhood deprivation and very preterm birth in an English and French cohort. BMC Pregnancy Childbirth 2013, 13, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glinianaia, S.V.; Ghosh, R.; Rankin, J.; Pearce, M.S.; Parker, L.; Pless-Mulloli, T. No improvement in socioeconomic inequalities in birthweight and preterm birth over four decades: A population-based cohort study. BMC Public Health 2013, 13, 345. [Google Scholar] [CrossRef] [PubMed]
- Potijk, M.R.; de Winter, A.F.; Bos, A.F.; Kerstjens, J.M.; Reijneveld, S.A. Behavioural and emotional problems in moderately preterm children with low socioeconomic status: A population-based study. Eur. Child Adolesc. Psychiatry 2015, 24, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Reeves, A.; McKee, M.; Mackenbach, J.; Whitehead, M.; Stuckler, D. Introduction of a national minimum wage reduced depressive symptoms in low-wage workers: A quasi-natural experiment in the UK. Health Econ. 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burmaster, K.B.; Landefeld, J.C.; Rehkopf, D.H.; Lahiff, M.; Sokal-Gutierrez, K.; Adler-Milstein, S.; Fernald, L.C. Impact of a private sector living wage intervention on depressive symptoms among apparel workers in the dominican republic: A quasi-experimental study. BMJ Open 2015, 5, e007336. [Google Scholar] [PubMed]
- Logan, A.C.; Katzman, M.A.; Balanza-Martinez, V. Natural environments, ancestral diets, and microbial ecology: Is there a modern “paleo-deficit disorder”? Part II. J. Physiol. Anthropol. 2015, 34, 9. [Google Scholar] [CrossRef] [PubMed]
- Logan, A.C.; Jacka, F.N. Nutritional psychiatry research: An emerging discipline and its intersection with global urbanization, environmental challenges and the evolutionary mismatch. J. Physiol. Anthropol. 2014, 33, 22. [Google Scholar] [CrossRef] [PubMed]
- Shivappa, N.; Schoenaker, D.A.; Hebert, J.R.; Mishra, G.D. Association between inflammatory potential of diet and risk of depression in middle-aged women: The Australian longitudinal study on women’s health. Br. J. Nutr. 2016, 116, 1077–1086. [Google Scholar] [CrossRef] [PubMed]
- Akbaraly, T.N.; Kerlau, C.; Wyart, M.; Chevallier, N.; Ndiaye, L.; Shivappa, N.; Hebert, J.R.; Kivimaki, M. Dietary inflammatory index and recurrence of depressive symptoms: Results from the whitehall II study. Clin. Psychol. Sci. 2016. [Google Scholar] [CrossRef]
- Jacka, F.N.; Ystrom, E.; Brantsaeter, A.L.; Karevold, E.; Roth, C.; Haugen, M.; Meltzer, H.M.; Schjolberg, S.; Berk, M. Maternal and early postnatal nutrition and mental health of offspring by age 5 years: A prospective cohort study. J. Am. Acad. Child Adolesc. Psychiatry 2013, 52, 1038–1047. [Google Scholar] [CrossRef] [PubMed]
- Pina-Camacho, L.; Jensen, S.K.; Gaysina, D.; Barker, E.D. Maternal depression symptoms, unhealthy diet and child emotional-behavioural dysregulation. Psychol. Med. 2015, 45, 1851–1860. [Google Scholar] [CrossRef] [PubMed]
- Purtell, K.M.; Gershoff, E.T. Fast food consumption and academic growth in late childhood. Clin. Pediatr. 2015, 54, 871–877. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.J.; Beilharz, J.E.; Maniam, J.; Reichelt, A.C.; Westbrook, R.F. Why is obesity such a problem in the 21st century? The intersection of palatable food, cues and reward pathways, stress, and cognition. Neurosci. Biobehav. Rev. 2015, 58, 36–45. [Google Scholar] [PubMed]
- Zeeni, N.; Bassil, M.; Fromentin, G.; Chaumontet, C.; Darcel, N.; Tome, D.; Daher, C.F. Environmental enrichment and cafeteria diet attenuate the response to chronic variable stress in rats. Physiol. Behav. 2015, 139, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Tryon, M.S.; Stanhope, K.L.; Epel, E.S.; Mason, A.E.; Brown, R.; Medici, V.; Havel, P.J.; Laugero, K.D. Excessive sugar consumption may be a difficult habit to break: A view from the brain and body. J. Clin. Endocrinol. Metab. 2015, 100, 2239–2247. [Google Scholar] [CrossRef] [PubMed]
- Van Oudenhove, L.; McKie, S.; Lassman, D.; Uddin, B.; Paine, P.; Coen, S.; Gregory, L.; Tack, J.; Aziz, Q. Fatty acid-induced gut-brain signaling attenuates neural and behavioral effects of sad emotion in humans. J. Clin. Investig. 2011, 121, 3094–3099. [Google Scholar] [CrossRef] [PubMed]
- Weltens, N.; Zhao, D.; van Oudenhove, L. Where is the comfort in comfort foods? Mechanisms linking fat signaling, reward, and emotion. Neurogastroenterol. Motil. 2014, 26, 303–315. [Google Scholar] [PubMed]
- St-Onge, M.P.; Roberts, A.; Shechter, A.; Choudhury, A.R. Fiber and saturated fat are associated with sleep arousals and slow wave sleep. J. Clin. Sleep Med. 2016, 12, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Zhang, J.; Zhou, R.; Liu, J.; Dai, Z.; Liu, D.; Wang, Y.; Zhang, H.; Li, Y.; Zeng, G. Sleep disturbances during pregnancy are associated with cesarean delivery and preterm birth. J. Matern. Fetal Neonatal Med. 2016, 16, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Krawczak, E.M.; Minuzzi, L.; Hidalgo, M.P.; Frey, B.N. Do changes in subjective sleep and biological rhythms predict worsening in postpartum depressive symptoms? A prospective study across the perinatal period. Arch. Womens Ment. Health 2016, 19, 591–598. [Google Scholar] [CrossRef] [PubMed]
- Okun, M.L. Disturbed sleep and postpartum depression. Curr. Psychiatry Rep. 2016, 18, 66. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, D.; Zelkowitz, P.; Dasgupta, K.; Sewitch, M.; Lowensteyn, I.; Cruz, R.; Hennegan, K.; Khalife, S. Dads get sad too: Depressive symptoms and associated factors in expectant first-time fathers. Am. J. Men’s Health 2015. [Google Scholar] [CrossRef] [PubMed]
- Armitage, R.; Flynn, H.; Hoffmann, R.; Vazquez, D.; Lopez, J.; Marcus, S. Early developmental changes in sleep in infants: The impact of maternal depression. Sleep 2009, 32, 693–696. [Google Scholar] [PubMed]
- Hairston, I.S.; Solnik-Menilo, T.; Deviri, D.; Handelzalts, J.E. Maternal depressed mood moderates the impact of infant sleep on mother-infant bonding. Arch. Womens Ment. Health 2016. [Google Scholar] [CrossRef] [PubMed]
- Hairston, I.S.; Waxler, E.; Seng, J.S.; Fezzey, A.G.; Rosenblum, K.L.; Muzik, M. The role of infant sleep in intergenerational transmission of trauma. Sleep 2011, 34, 1373–1383. [Google Scholar] [CrossRef] [PubMed]
- Goldfield, G.S.; Murray, M.; Maras, D.; Wilson, A.L.; Phillips, P.; Kenny, G.P.; Hadjiyannakis, S.; Alberga, A.; Cameron, J.D.; Tulluch, H.; et al. Screen time is associated with depressive symptomatology among obese adolescents: A hearty study. Eur. J. Pediatr. 2016, 175, 909–919. [Google Scholar] [CrossRef] [PubMed]
- Grontved, A.; Singhammer, J.; Froberg, K.; Moller, N.C.; Pan, A.; Pfeiffer, K.A.; Kristensen, P.L. A prospective study of screen time in adolescence and depression symptoms in young adulthood. Prev. Med. 2015, 81, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.L.; Wen, L.M.; Hardy, L.L.; Rissel, C. Associations of outdoor play and screen time with nocturnal sleep duration and pattern among young children. Acta Paediatr. 2016, 105, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Trinh, L.; Wong, B.; Faulkner, G.E. The independent and interactive associations of screen time and physical activity on mental health, school connectedness and academic achievement among a population-based sample of youth. J. Can. Acad. Child Adolesc. 2015, 24, 17–24. [Google Scholar]
- Ferraro, F.R.; Weatherly, J.N. Texting dependence, ipod dependence, and delay discounting. Am. J. Psychol. 2016, 129, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Costigan, S.A.; Barnett, L.; Plotnikoff, R.C.; Lubans, D.R. The health indicators associated with screen-based sedentary behavior among adolescent girls: A systematic review. J. Adolesc. Health 2013, 52, 382–392. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; Qian, Q.; Weng, T.; Yuan, C.; Sun, Y.; Wang, H.; Tao, F. Screen time, physical activity and mental health among urban adolescents in China. Prev. Med. 2011, 53, 316–320. [Google Scholar] [CrossRef] [PubMed]
- Feng, Q.; Zhang, Q.L.; Du, Y.; Ye, Y.L.; He, Q.Q. Associations of physical activity, screen time with depression, anxiety and sleep quality among chinese college freshmen. PLoS ONE 2014, 9, e100914. [Google Scholar] [CrossRef] [PubMed]
- Schule, S.A.; von Kries, R.; Fromme, H.; Bolte, G. Neighbourhood socioeconomic context, individual socioeconomic position, and overweight in young children: A multilevel study in a large german city. BMC Obes. 2016, 3, 25. [Google Scholar] [CrossRef] [PubMed]
- Ellaway, A.; Benzeval, M.; Green, M.; Leyland, A.; Macintyre, S. “Getting sicker quicker”: Does living in a more deprived neighbourhood mean your health deteriorates faster? Health Place 2012, 18, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Giurgescu, C.; Misra, D.P.; Sealy-Jefferson, S.; Caldwell, C.H.; Templin, T.N.; Slaughter-Acey, J.C.; Osypuk, T.L. The impact of neighborhood quality, perceived stress, and social support on depressive symptoms during pregnancy in African American women. Soc. Sci. Med. 2015, 130, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Chor, D.; Cardoso, L.O.; Nobre, A.A.; Griep, R.H.; Fonseca Mde, J.; Giatti, L.; Bensenor, I.; Del Carmen Bisi Molina, M.; Aquino, E.M.; Diez-Roux, A.; et al. Association between perceived neighbourhood characteristics, physical activity and diet quality: Results of the brazilian longitudinal study of adult health (Elsa-Brasil). BMC Public Health 2016, 16, 751. [Google Scholar] [CrossRef] [PubMed]
- Giese, H.; Konig, L.M.; Taut, D.; Ollila, H.; Baban, A.; Absetz, P.; Schupp, H.; Renner, B. Exploring the association between television advertising of healthy and unhealthy foods, self-control, and food intake in three European countries. Appl. Psychol. Health Well 2015, 7, 41–62. [Google Scholar] [CrossRef] [PubMed]
- Vohs, K.D. Psychology. The poor’s poor mental power. Science 2013, 341, 969–970. [Google Scholar] [PubMed]
- Mani, A.; Mullainathan, S.; Shafir, E.; Zhao, J. Poverty impedes cognitive function. Science 2013, 341, 976–980. [Google Scholar] [CrossRef] [PubMed]
- Bratanova, B.; Loughnan, S.; Klein, O.; Claassen, A.; Wood, R. Poverty, inequality, and increased consumption of high calorie food: Experimental evidence for a causal link. Appetite 2016, 100, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Cardel, M.I.; Johnson, S.L.; Beck, J.; Dhurandhar, E.; Keita, A.D.; Tomczik, A.C.; Pavela, G.; Huo, T.; Janicke, D.M.; Muller, K.; et al. The effects of experimentally manipulated social status on acute eating behavior: A randomized, crossover pilot study. Physiol. Behav. 2016, 162, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Searle, A.; Calnan, M.; Lewis, G.; Campbell, J.; Taylor, A.; Turner, K. Patients’ views of physical activity as treatment for depression: A qualitative study. Br. J. Gen. Pract. 2011, 61, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Marcora, S.M.; Staiano, W.; Manning, V. Mental fatigue impairs physical performance in humans. J. Appl. Physiol. (1985) 2009, 106, 857–864. [Google Scholar] [CrossRef] [PubMed]
- Blakely, M.J.; Kemp, S.; Helton, W.S. Volitional running and tone counting: The impact of cognitive load on running over natural terrain. Trans. Occup. Ergon. Hum. Factors 2016, 4, 104–114. [Google Scholar] [CrossRef]
- Thogersen-Ntoumani, C.; Shepherd, S.O.; Ntoumanis, N.; Wagenmakers, A.J.; Shaw, C.S. Intrinsic motivation in two exercise interventions: Associations with fitness and body composition. Health Psychol. 2016, 35, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, P.J.; Carraca, E.V.; Markland, D.; Silva, M.N.; Ryan, R.M. Exercise, physical activity, and self-determination theory: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 78. [Google Scholar] [CrossRef] [PubMed]
- Ben Cheikh, R.; Latiri, I.; Dogui, M.; Ben Saad, H. Effects of one night sleep deprivation on selective attention and isometric force in adolescent karate athletes. J. Sports Med. Phys. Fit. 2016, in press. [Google Scholar]
- Ekkekakis, P.; Parfitt, G.; Petruzzello, S.J. The pleasure and displeasure people feel when they exercise at different intensities decennial update and progress towards a tripartite rationale for exercise intensity prescription. Sports Med. 2011, 41, 641–671. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, A.A.; Deuster, P.A.; Francis, J.L.; Beadling, C.; Kop, W.J. The role of depression in short-term mood and fatigue responses to acute exercise. Int. J. Behav. Med. 2010, 17, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Huebschmann, A.G.; Kohrt, W.M.; Herlache, L.; Wolfe, P.; Daugherty, S.; Reusch, J.E.; Bauer, T.A.; Regensteiner, J.G. Type 2 diabetes exaggerates exercise effort and impairs exercise performance in older women. BMJ Open Diabetes Res. Care 2015, 3, e000124. [Google Scholar] [CrossRef] [PubMed]
- Annesi, J.J. Relations of self-motivation, perceived physical condition, and exercise-induced changes in revitalization and exhaustion with attendance in women initiating a moderate cardiovascular exercise regimen. Women Health 2005, 42, 77–93. [Google Scholar] [CrossRef] [PubMed]
- Kwan, B.M.; Bryan, A. In-task and post-task affective response to exercise: Translating exercise intentions into behaviour. Br. J. Health Psychol. 2010, 15, 115–131. [Google Scholar] [CrossRef] [PubMed]
- Sarmugam, R.; Worsley, A. Dietary behaviours, impulsivity and food involvement: Identification of three consumer segments. Nutrients 2015, 7, 8036–8057. [Google Scholar] [CrossRef] [PubMed]
- Lawyer, S.R.; Boomhower, S.R.; Rasmussen, E.B. Differential associations between obesity and behavioral measures of impulsivity. Appetite 2015, 95, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Joireman, J.; King, S. Individual differences in the consideration of future and (more) immediate consequences: A review and directions for future research. Soc. Personal. Psychol. 2016, 10, 313–326. [Google Scholar] [CrossRef]
- Ishii, K. Subjective socioeconomic status and cigarette smoking interact to delay discounting. Springerplus 2015, 4, 560. [Google Scholar] [CrossRef] [PubMed]
- Lovallo, W.R.; Farag, N.H.; Sorocco, K.H.; Acheson, A.; Cohoon, A.J.; Vincent, A.S. Early life adversity contributes to impaired cognition and impulsive behavior: Studies from the Oklahoma family health patterns project. Alcohol. Clin. Exp. Res. 2013, 37, 616–623. [Google Scholar] [CrossRef] [PubMed]
- Acheson, A.; Vincent, A.S.; Sorocco, K.H.; Lovallo, W.R. Greater discounting of delayed rewards in young adults with family histories of alcohol and drug use disorders: Studies from the Oklahoma family health patterns project. Alcohol. Clin. Exp. Res. 2011, 35, 1607–1613. [Google Scholar] [CrossRef] [PubMed]
- Fields, S.A.; Lange, K.; Ramos, A.; Thamotharan, S.; Rassu, F. The relationship between stress and delay discounting: A meta-analytic review. Behav. Pharmacol. 2014, 25, 434–444. [Google Scholar] [CrossRef] [PubMed]
- Worthy, D.A.; Byrne, K.A.; Fields, S. Effects of emotion on prospection during decision-making. Front. Psychol. 2014, 5, 591. [Google Scholar] [CrossRef] [PubMed]
- DeVoe, S.E.; House, J.; Zhong, C.B. Fast food and financial impatience: A socioecological approach. J. Personal. Soc. Psychol. 2013, 105, 476–494. [Google Scholar] [CrossRef] [PubMed]
- House, J.; DeVoe, S.E.; Zhong, C.B. Too impatient to smell the roses: Exposure to fast food impedes happiness. Soc. Psychol. Personal. Sci. 2014, 5, 534–541. [Google Scholar] [CrossRef]
- Van der Wal, A.J.; Schade, H.M.; Krabbendam, L.; van Vugt, M. Do natural landscapes reduce future discounting in humans? Proc. R. Soc. B Biol. Sci. 2013, 280, 20132295. [Google Scholar] [CrossRef] [PubMed]
- Berry, M.S.; Sweeney, M.M.; Morath, J.; Odum, A.L.; Jordan, K.E. The nature of impulsivity: Visual exposure to natural environments decreases impulsive decision-making in a delay discounting task. PLoS ONE 2014, 9, e97915. [Google Scholar] [CrossRef] [PubMed]
- Berry, M.S.; Repke, M.A.; Nickerson, N.P.; Conway, L.G.; Odum, A.L.; Jordan, K.E. Making time for nature: Visual exposure to natural environments lengthens subjective time perception and reduces impulsivity. PLoS ONE 2015, 10, e0141030. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.Y.; Shein, P.P.; Chiou, W.B. Escaping the impulse to immediate gratification: The prospect concept promotes a future-oriented mindset, prompting an inclination towards delayed gratification. Br. J. Psychol. 2012, 103, 129–141. [Google Scholar] [CrossRef] [PubMed]
- Dassen, F.C.M.; Jansen, A.; Nederkoorn, C.; Houben, K. Focus on the future: Episodic future thinking reduces discount rate and snacking. Appetite 2016, 96, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.E.; Pollack, L.; McCune, A.; Schulte, E.; Savage, C.R.; Lundgren, J.D. Comparison of obese adults with poor versus good sleep quality during a functional neuroimaging delay discounting task: A pilot study. Psychiatry Res. Imaging 2015, 234, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Engle-Friedman, M. The effects of sleep loss on capacity and effort. Sleep Sci. 2014, 7, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Libedinsky, C.; Massar, S.A.; Ling, A.; Chee, W.; Huettel, S.A.; Chee, M.W. Sleep deprivation alters effort discounting but not delay discounting of monetary rewards. Sleep 2013, 36, 899–904. [Google Scholar] [CrossRef] [PubMed]
- Chan, W.S. Delay discounting and response disinhibition moderate associations between actigraphically measured sleep parameters and body mass index. J. Sleep Res. 2016. [Google Scholar] [CrossRef] [PubMed]
- Park, N.; Peterson, C.; Szvarca, D.; Vander Molen, R.J.; Kim, E.S.; Collon, K. Positive psychology and physical health: Research and applications. Am. J. Lifestyle Med. 2016, 10, 200–206. [Google Scholar] [CrossRef]
- Steptoe, A.; O’Donnell, K.; Marmot, M.; Wardle, J. Positive affect, psychological well-being, and good sleep. J. Psychosom. Res. 2008, 64, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Voellmin, A.; Entringer, S.; Moog, N.; Wadhwa, P.D.; Buss, C. Maternal positive affect over the course of pregnancy is associated with the length of gestation and reduced risk of preterm delivery. J. Psychosom. Res. 2013, 75, 336–340. [Google Scholar] [CrossRef] [PubMed]
- Coffey, J.K.; Warren, M.T.; Gottfried, A.W. Does infant happiness forecast adult life satisfaction? Examining subjective well-being in the first quarter century of life. J. Happiness Stud. 2015, 16, 1401–1421. [Google Scholar]
- Kansky, J.; Allen, J.P.; Diener, E. Early adolescent affect predicts later life outcomes. Appl. Psychol. Health Well Being 2016, 8, 192–212. [Google Scholar] [CrossRef] [PubMed]
- Stellar, J.E.; John-Henderson, N.; Anderson, C.L.; Gordon, A.M.; McNeil, G.D.; Keltner, D. Positive affect and markers of inflammation: Discrete positive emotions predict lower levels of inflammatory cytokines. Emotion 2015, 15, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Kubzansky, L.D.; Baccarelli, A.; Sparrow, D.; Spiro, A., 3rd; Tarantini, L.; Cantone, L.; Vokonas, P.; Schwartz, J. Psychological factors and DNA methylation of genes related to immune/inflammatory system markers: The VA normative aging study. BMJ Open 2016, 6, e009790. [Google Scholar] [CrossRef] [PubMed]
- Reininghaus, E.Z.; Lackner, N.; Birner, A.; Bengesser, S.; Fellendorf, F.T.; Platzer, M.; Rieger, A.; Queissner, R.; Kainzbauer, N.; Reininghaus, B.; et al. Extracellular matrix proteins matrix metallopeptidase 9 (mmp9) and soluble intercellular adhesion molecule 1 (sicam-1) and correlations with clinical staging in euthymic bipolar disorder. Bipolar Disord. 2016, 18, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Wirtz, P.H.; Redwine, L.S.; Linke, S.; Hong, S.; Rutledge, T.; Greenberg, B.H.; Mills, P.J. Circulating levels of soluble intercellular adhesion molecule-1 (sicam-1) independently predict depressive symptom severity after 12 months in heart failure patients. Brain Behav. Immun. 2010, 24, 366–369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sin, N.L.; Graham-Engeland, J.E.; Almeida, D.M. Daily positive events and inflammation: Findings from the national study of daily experiences. Brain Behav. Immun. 2015, 43, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Sin, N.L.; Graham-Engeland, J.E.; Ong, A.D.; Almeida, D.M. Affective reactivity to daily stressors is associated with elevated inflammation. Health Psychol. 2015, 34, 1154–1165. [Google Scholar] [CrossRef] [PubMed]
- Roy, B.; Diez-Roux, A.V.; Seeman, T.; Ranjit, N.; Shea, S.; Cushman, M. Association of optimism and pessimism with inflammation and hemostasis in the multi-ethnic study of atherosclerosis (mesa). Psychosom. Med. 2010, 72, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Brydon, L.; Walker, C.; Wawrzyniak, A.J.; Chart, H.; Steptoe, A. Dispositional optimism and stress-induced changes in immunity and negative mood. Brain Behav. Immun. 2009, 23, 810–816. [Google Scholar] [CrossRef] [PubMed]
- Boehm, J.K.; Chen, Y.; Williams, D.R.; Ryff, C.; Kubzansky, L.D. Unequally distributed psychological assets: Are there social disparities in optimism, life satisfaction, and positive affect? PLoS ONE 2015, 10, e0118066. [Google Scholar] [CrossRef] [PubMed]
- Boehm, J.K.; Williams, D.R.; Rimm, E.B.; Ryff, C.; Kubzansky, L.D. Association between optimism and serum antioxidants in the midlife in the united states study. Psychosom. Med. 2013, 75, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Hingle, M.D.; Wertheim, B.C.; Tindle, H.A.; Tinker, L.; Seguin, R.A.; Rosal, M.C.; Thomson, C.A. Optimism and diet quality in the women’s health initiative. J. Acad. Nutr. Diet. 2014, 114, 1036–1045. [Google Scholar] [CrossRef] [PubMed]
- Lau, E.Y.; Harry Hui, C.; Cheung, S.F.; Lam, J. Bidirectional relationship between sleep and optimism with depressive mood as a mediator: A longitudinal study of chinese working adults. J. Psychosom. Res. 2015, 79, 428–434. [Google Scholar] [CrossRef] [PubMed]
- Cohen, R.; Bavishi, C.; Rozanski, A. Purpose in life and its relationship to all-cause mortality and cardiovascular events: A meta-analysis. Psychosom. Med. 2016, 78, 122–133. [Google Scholar] [CrossRef] [PubMed]
- Strecher, V.; Terry, P. Health and life purpose: What’s the connection? Am. J. Health Promot. 2014, 29, TAHP2–TAHP4. [Google Scholar] [PubMed]
- Burrow, A.L.; Spreng, R.N. Waiting with purpose: A reliable but small association between purpose in life and impulsivity. Pers. Individ. Differ. 2016, 90, 187–189. [Google Scholar] [CrossRef] [PubMed]
- Zilioli, S.; Slatcher, R.B.; Ong, A.D.; Gruenewald, T.L. Purpose in life predicts allostatic load ten years later. J. Psychosom. Res. 2015, 79, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S.; Strecher, V.J.; Ryff, C.D. Purpose in life and use of preventive health care services. Proc. Natl. Acad. Sci. USA 2014, 111, 16331–16336. [Google Scholar] [CrossRef] [PubMed]
- Lamis, D.A.; Wilson, C.K.; Tarantino, N.; Lansford, J.E.; Kaslow, N.J. Neighborhood disorder, spiritual well-being, and parenting stress in African American women. J. Fam. Psychol. 2014, 28, 769–778. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.; O’Driscoll, K.; Moore, C. The influence of empathic concern on prosocial behavior in children. Front. Psychol. 2014, 5, 425. [Google Scholar] [CrossRef] [PubMed]
- Bourgault, P.; Lavoie, S.; Paul-Savoie, E.; Gregoire, M.; Michaud, C.; Gosselin, E.; Johnston, C.C. Relationship between empathy and well-being among emergency nurses. J. Emerg. Nurs. 2015, 41, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Ma-Kellams, C.; Lerner, J. Trust your gut or think carefully? Examining whether an intuitive, versus a systematic, mode of thought produces greater empathic accuracy. J. Personal. Soc. Psychol. 2016, in press. [Google Scholar] [CrossRef] [PubMed]
- Allemand, M.; Steiger, A.E.; Fend, H.A. Empathy development in adolescence predicts social competencies in adulthood. J. Pers. 2015, 83, 229–241. [Google Scholar] [CrossRef] [PubMed]
- Di Fabio, A.; Bucci, O. Green positive guidance and green positive life counseling for decent work and decent lives: Some empirical results. Front. Psychol. 2016, 7, 261. [Google Scholar] [CrossRef] [PubMed]
- Schreier, H.M.; Schonert-Reichl, K.A.; Chen, E. Effect of volunteering on risk factors for cardiovascular disease in adolescents: A randomized controlled trial. JAMA Pediatr. 2013, 167, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Dubos, R. Adapting to pollution. Sci. Citiz. 1968, 10, 1–8. [Google Scholar] [CrossRef]
- Mantler, A.; Logan, A.C. Natural environments and mental health. Adv. Integr. Med. 2015, 2, 5–12. [Google Scholar] [CrossRef]
- Craig, J.M.; Logan, A.C.; Prescott, S.L. Natural environments, nature relatedness and the ecological theater: Connecting satellites and sequencing to Shinrin-Yoku. J. Physiol. Anthropol. 2016, 35, 1. [Google Scholar] [CrossRef] [PubMed]
- Song, C.; Ikei, H.; Miyazaki, Y. Physiological effects of nature therapy: A review of the research in Japan. Int. J. Environ. Res. Public Health 2016, 13, 781. [Google Scholar] [CrossRef] [PubMed]
- James, P.; Hart, J.E.; Banay, R.F.; Laden, F. Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ. Health Perspect. 2016. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.; Popham, F. Effect of exposure to natural environment on health inequalities: An observational population study. Lancet 2008, 372, 1655–1660. [Google Scholar] [CrossRef]
- Dadvand, P.; Wright, J.; Martinez, D.; Basagana, X.; McEachan, R.R.; Cirach, M.; Gidlow, C.J.; de Hoogh, K.; Grazuleviciene, R.; Nieuwenhuijsen, M.J. Inequality, green spaces, and pregnant women: Roles of ethnicity and individual and neighbourhood socioeconomic status. Environ. Int. 2014, 71, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Hystad, P.; Davies, H.W.; Frank, L.; van Loon, J.; Gehring, U.; Tamburic, L.; Brauer, M. Residential greenness and birth outcomes: Evaluating the influence of spatially correlated built-environment factors. Environ. Health Perspect. 2014, 122, 1095–1102. [Google Scholar] [CrossRef] [PubMed]
- Grazuleviciene, R.; Danileviciute, A.; Dedele, A.; Vencloviene, J.; Andrusaityte, S.; Uzdanaviciute, I.; Nieuwenhuijsen, M.J. Surrounding greenness, proximity to city parks and pregnancy outcomes in Kaunas cohort study. Int. J. Hyg. Environ. Health 2015, 218, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Ebisu, K.; Holford, T.R.; Bell, M.L. Association between greenness, urbanicity, and birth weight. Sci. Total Environ. 2016, 542, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Casey, J.A.; James, P.; Rudolph, K.E.; Wu, C.D.; Schwartz, B.S. Greenness and birth outcomes in a range of pennsylvania communities. Int. J. Environ. Res. Public Health 2016, 13, 311. [Google Scholar] [CrossRef] [PubMed]
- Laurent, O.; Wu, J.; Li, L.; Milesi, C. Green spaces and pregnancy outcomes in southern California. Health Place 2013, 24, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; de Nazelle, A.; Figueras, F.; Basagana, X.; Su, J.; Amoly, E.; Jerrett, M.; Vrijheid, M.; Sunyer, J.; Nieuwenhuijsen, M.J. Green space, health inequality and pregnancy. Environ. Int. 2012, 40, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; Sunyer, J.; Basagana, X.; Ballester, F.; Lertxundi, A.; Fernandez-Somoano, A.; Estarlich, M.; Garcia-Esteban, R.; Mendez, M.A.; Nieuwenhuijsen, M.J. Surrounding greenness and pregnancy outcomes in four Spanish birth cohorts. Environ. Health Perspect. 2012, 120, 1481–1487. [Google Scholar] [CrossRef] [PubMed]
- Kihal-Talantikite, W.; Padilla, C.M.; Lalloue, B.; Gelormini, M.; Zmirou-Navier, D.; Deguen, S. Green space, social inequalities and neonatal mortality in France. BMC Pregnancy Childbirth 2013, 13, 191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Markevych, I.; Fuertes, E.; Tiesler, C.M.; Birk, M.; Bauer, C.P.; Koletzko, S.; von Berg, A.; Berdel, D.; Heinrich, J. Surrounding greenness and birth weight: Results from the Giniplus and Lisaplus birth cohorts in Munich. Health Place 2014, 26, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Cusack, L.; Larkin, A.; Carozza, S.; Hystad, P. Associations between residential greenness and birth outcomes across texas. Environ. Res. 2016, 152, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Sbihi, H.; Tamburic, L.; Koehoorn, M.; Brauer, M. Greenness and incident childhood asthma: A 10-year follow-up in a population-based birth cohort. Am. J. Respir. Crit. Care Med. 2015, 192, 1131–1133. [Google Scholar] [CrossRef] [PubMed]
- McEachan, R.R.; Prady, S.L.; Smith, G.; Fairley, L.; Cabieses, B.; Gidlow, C.; Wright, J.; Dadvand, P.; van Gent, D.; Nieuwenhuijsen, M.J. The association between green space and depressive symptoms in pregnant women: Moderating roles of socioeconomic status and physical activity. J. Epidemiol. Community Health 2016, 70, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lee, C.; Sohn, W. Urban natural environments, obesity, and health-related quality of life among hispanic children living in inner-city neighborhoods. Int. J. Environ. Res. Public Health 2016, 13, 121. [Google Scholar] [CrossRef] [PubMed]
- Younan, D.; Tuvblad, C.; Li, L.F.; Wu, J.; Lurmann, F.; Franklin, M.; Berhane, K.; McConnell, R.; Wu, A.H.; Baker, L.A.; et al. Environmental determinants of aggression in adolescents: Role of urban neighborhood greenspace. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 591–601. [Google Scholar] [CrossRef] [PubMed]
- Gariepy, G.; Kaufman, J.S.; Blair, A.; Kestens, Y.; Schmitz, N. Place and health in diabetes: The neighbourhood environment and risk of depression in adults with type 2 diabetes. Diabet. Med. J. Br. Diabet. Assoc. 2015, 32, 944–950. [Google Scholar] [CrossRef] [PubMed]
- Maas, J.; Verheij, R.A.; de Vries, S.; Spreeuwenberg, P.; Schellevis, F.G.; Groenewegen, P.P. Morbidity is related to a green living environment. J. Epidemiol. Community Health 2009, 63, 967–973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beyer, K.M.M.; Kaltenbach, A.; Szabo, A.; Bogar, S.; Nieto, F.J.; Malecki, K.M. Exposure to neighborhood green space and mental health: Evidence from the survey of the health of Wisconsin. Int. J. Environ. Res. Public Health 2014, 11, 3453–3472. [Google Scholar] [CrossRef] [PubMed]
- Bodicoat, D.H.; O’Donovan, G.; Dalton, A.M.; Gray, L.J.; Yates, T.; Edwardson, C.; Hill, S.; Webb, D.R.; Khunti, K.; Davies, M.J.; et al. The association between neighbourhood greenspace and type 2 diabetes in a large cross-sectional study. BMJ Open 2014, 4, e006076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen-Cline, H.; Turkheimer, E.; Duncan, G.E. Access to green space, physical activity and mental health: A twin study. J. Epidemiol. Community Health 2015, 69, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Nutsford, D.; Pearson, A.L.; Kingham, S. An ecological study investigating the association between access to urban green space and mental health. Public Health 2013, 127, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Alcock, I.; White, M.P.; Wheeler, B.W.; Fleming, L.E.; Depledge, M.H. Longitudinal effects on mental health of moving to greener and less green urban areas. Environ. Sci. Technol. 2014, 48, 1247–1255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mills, J.R.; Cunningham, P.; Donovan, G.H. Urban forests and social inequality in the Pacific Northwest. Urban For. Urban Green. 2016, 16, 188–196. [Google Scholar] [CrossRef]
- Arroyo-Johnson, C.; Woodward, K.; Milam, L.; Ackermann, N.; Komaie, G.; Goodman, M.S.; Hipp, J.A. Still separate, still unequal: Social determinants of playground safety and proximity disparities in St. Louis. J. Urban Health Bull. N. Y. Acad. Med. 2016, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Leong, M.; Bertone, M.A.; Bayless, K.M.; Dunn, R.R.; Trautwein, M.D. Exoskeletons and economics: Indoor arthropod diversity increases in affluent neighbourhoods. Biol. Lett. 2016. [Google Scholar] [CrossRef] [PubMed]
- Zach, A.; Meyer, N.; Hendrowarsito, L.; Kolb, S.; Bolte, G.; Nennstiel-Ratzel, U.; Stilianakis, N.I.; Herr, C.; Grp, G.S. Association of sociodemographic and environmental factors with the mental health status among preschool children-results from a cross-sectional study in Bavaria, Germany. Int. J. Hyg. Environ. Health 2016, 219, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.A.; Han, B.; Nagel, C.J.; Harnik, P.; McKenzie, T.L.; Evenson, K.R.; Marsh, T.; Williamson, S.; Vaughan, C.; Katta, S. The first national study of neighborhood parks: Implications for physical activity. Am. J. Prev. Med. 2016, 51, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Salmon, J.; Veitch, J.; Abbott, G.; ChinAPaw, M.; Brug, J.J.; teVelde, S.J.; Cleland, V.; Hume, C.; Crawford, D.; Ball, K. Are associations between the perceived home and neighbourhood environment and children’s physical activity and sedentary behaviour moderated by urban/rural location? Health Place 2013, 24, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Tandon, P.S.; Zhou, C.; Sallis, J.F.; Cain, K.L.; Frank, L.D.; Saelens, B.E. Home environment relationships with children’s physical activity, sedentary time, and screen time by socioeconomic status. Int. J. Behav. Nutr. Phys. 2012, 9, 88. [Google Scholar] [CrossRef] [PubMed]
- McCormack, G.R.; Mardinger, C. Neighbourhood urban form and individual-level correlates of leisure-based screen time in Canadian adults. BMJ Open 2015, 5, e009418. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Sugiyama, T.; Winkler, E.; Cerin, E.; Wijndaele, K.; Owen, N. Correlates of change in adults’ television viewing time: A four-year follow-up study. Med. Sci. Sports Exerc. 2012, 44, 1287–1292. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, T.; Salmon, J.; Dunstan, D.W.; Bauman, A.E.; Owen, N. Neighborhood walkability and TV viewing time among Australian adults. Am. J. Prev. Med. 2007, 33, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Cote-Lussier, C.; Mathieu, M.E.; Barnett, T.A. Independent associations between child and parent perceived neighborhood safety, child screen time, physical activity and bmi: A structural equation modeling approach. Int. J. Obes. 2015, 39, 1475–1481. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.C.; Koleilat, M.; Hernandez, L.M.; Whaley, S.E.; Davis, J.N. Screen time associated to unhealthy diets in low-income children. J. Food Nutr. Res. 2016, 4, 94–99. [Google Scholar]
- Mitchell, R.J.; Richardson, E.A.; Shortt, N.K.; Pearce, J.R. Neighborhood environments and socioeconomic inequalities in mental well-being. Am. J. Prev. Med. 2015, 49, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Shanahan, D.F.; Bush, R.; Gaston, K.J.; Lin, B.B.; Dean, J.; Barber, E.; Fuller, R.A. Health benefits from nature experiences depend on dose. Sci. Rep. 2016, 6, 28551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Im, S.G.; Choi, H.; Jeon, Y.H.; Song, M.K.; Kim, W.; Woo, J.M. Comparison of effect of two-hour exposure to forest and urban environments on cytokine, anti-oxidant, and stress levels in young adults. Int. J. Environ. Res. Public Health 2016, 13, 625. [Google Scholar] [CrossRef] [PubMed]
- Seo, S.C.; Park, S.J.; Park, C.W.; Yoon, W.S.; Choung, J.T.; Yoo, Y. Clinical and immunological effects of a forest trip in children with asthma and atopic dermatitis. Iran. J. Allergy Asthma Immunol. 2015, 14, 28–36. [Google Scholar] [PubMed]
- Li, Q.; Kobayashi, M.; Kumeda, S.; Ochiai, T.; Miura, T.; Kagawa, T.; Imai, M.; Wang, Z.; Otsuka, T.; Kawada, T. Effects of forest bathing on cardiovascular and metabolic parameters in middle-aged males. Evid. Based Complement. Altern. Med. 2016, 2016, 2587381. [Google Scholar] [CrossRef] [PubMed]
- Grazuleviciene, R.; Vencloviene, J.; Kubilius, R.; Grizas, V.; Danileviciute, A.; Dedele, A.; Andrusaityte, S.; Vitkauskiene, A.; Steponaviciute, R.; Nieuwenhuijsen, M.J. Tracking restoration of park and urban street settings in coronary artery disease patients. Int. J. Environ. Res. Public Health 2016, 13, 550. [Google Scholar] [CrossRef] [PubMed]
- Gidlow, C.J.; Randall, J.; Gillman, J.; Smith, G.R.; Jones, M.V. Natural environments and chronic stress measured by hair cortisol. Landsc. Urban Plan. 2016, 148, 61–67. [Google Scholar] [CrossRef]
- Honold, J.; Lakes, T.; Beyer, R.; van der Meer, E. Restoration in urban spaces: Nature views from home, greenways, and public parks. Environ. Behav. 2016, 48, 796–825. [Google Scholar] [CrossRef]
- Ochiai, H.; Ikei, H.; Song, C.; Kobayashi, M.; Miura, T.; Kagawa, T.; Li, Q.; Kumeda, S.; Imai, M.; Miyazaki, Y. Physiological and psychological effects of a forest therapy program on middle-aged females. Int. J. Environ. Res. Public Health 2015, 12, 15222–15232. [Google Scholar] [CrossRef] [PubMed]
- Thompson, C.W.; Roe, J.; Aspinall, P.; Mitchell, R.; Clow, A.; Miller, D. More green space is linked to less stress in deprived communities: Evidence from salivary cortisol patterns. Landsc. Urban Plan. 2012, 105, 221–229. [Google Scholar] [CrossRef]
- Roe, J.J.; Thompson, C.W.; Aspinall, P.A.; Brewer, M.J.; Duff, E.I.; Miller, D.; Mitchell, R.; Clow, A. Green space and stress: Evidence from cortisol measures in deprived urban communities. Int. J. Environ. Res. Public Health 2013, 10, 4086–4103. [Google Scholar] [CrossRef] [PubMed]
- Grigsby-Toussaint, D.S.; Turi, K.N.; Krupa, M.; Williams, N.J.; Pandi-Perumal, S.R.; Jean-Louis, G. Sleep insufficiency and the natural environment: Results from the US behavioral risk factor surveillance system survey. Prev. Med. 2015, 78, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Astell-Burt, T.; Feng, X.Q.; Kolt, G.S. Does access to neighbourhood green space promote a healthy duration of sleep? Novel findings from a cross-sectional study of 259,319 Australians. BMJ Open 2013, 3, e003094. [Google Scholar] [CrossRef] [PubMed]
- Gladwell, V.F.; Kuoppa, P.; Tarvainen, M.P.; Rogerson, M. A lunchtime walk in nature enhances restoration of autonomic control during night-time sleep: Results from a preliminary study. Int. J. Environ. Res. Public Health 2016. [Google Scholar] [CrossRef] [PubMed]
- Seron-Ferre, M.; Richter, H.G.; Valenzuela, G.J.; Torres-Farfan, C. Circadian rhythms in the fetus and newborn: Significance of interactions with maternal physiology and the environment. Neuromethods 2016, 109, 147–165. [Google Scholar]
- Reiter, R.J.; Tan, D.X.; Korkmaz, A.; Rosales-Corral, S.A. Melatonin and stable circadian rhythms optimize maternal, placental and fetal physiology. Hum. Reprod. Update 2014, 20, 293–307. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.C.; Chen, M.H.; Hsieh, C.J.; Chen, P.C. Effect of rotating shift work on childbearing and birth weight: A study of women working in a semiconductor manufacturing factory. World J. Pediatr. 2011, 7, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Rybnikova, N.A.; Haim, A.; Portnov, B.A. Does artificial light-at-night exposure contribute to the worldwide obesity pandemic? Int. J. Obes. (Lond.) 2016, 40, 815–823. [Google Scholar] [CrossRef] [PubMed]
- Matsuoka, R.H. Student performance and high school landscapes: Examining the links. Landsc. Urban Plan. 2010, 97, 273–282. [Google Scholar] [CrossRef]
- Wu, C.D.; McNeely, E.; Cedeno-Laurent, J.G.; Pan, W.C.; Adamkiewicz, G.; Dominici, F.; Lung, S.C.C.; Su, H.J.; Spengler, J.D. Linking student performance in Massachusetts elementary schools with the “greenness” of school surroundings using remote sensing. PLoS ONE 2014. [Google Scholar] [CrossRef] [PubMed]
- Benfield, J.A.; Rainbolt, G.N.; Bell, P.A.; Donovan, G.H. Classrooms with nature views: Evidence of differing student perceptions and behaviors. Environ. Behav. 2015, 47, 140–157. [Google Scholar] [CrossRef]
- Dadvand, P.; Nieuwenhuijsen, M.J.; Esnaola, M.; Forns, J.; Basagana, X.; Alvarez-Pedrerol, M.; Rivas, I.; Lopez-Vicente, M.; de Castro Pascual, M.; Su, J.; et al. Green spaces and cognitive development in primary schoolchildren. Proc. Natl. Acad. Sci. USA 2015, 112, 7937–7942. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Sullivan, W.C. Impact of views to school landscapes on recovery from stress and mental fatigue. Landsc. Urban Plan. 2016, 148, 149–158. [Google Scholar] [CrossRef]
- Weinstein, N.; Przybylski, A.K.; Ryan, R.M. Can nature make us more caring? Effects of immersion in nature on intrinsic aspirations and generosity. Personal. Soc. Psychol. Bull. 2009, 35, 1315–1329. [Google Scholar] [CrossRef] [PubMed]
- Zelenski, J.M.; Dopko, R.L.; Capaldi, C.A. Cooperation is in our nature: Nature exposure may promote cooperative and environmentally sustainable behavior. J. Environ. Psychol. 2015, 42, 24–31. [Google Scholar] [CrossRef]
- Gueguen, N.; Stefan, J. “Green altruism”: Short immersion in natural green environments and helping behavior. Environ. Behav. 2016, 48, 324–342. [Google Scholar] [CrossRef]
- Zelenski, J.M.; Nisbet, E.K. Happiness and feeling connected: The distinct role of nature relatedness. Environ. Behav. 2014, 46, 3–23. [Google Scholar] [CrossRef]
- Capaldi, C.A.; Dopko, R.L.; Zelenski, J.M. The relationship between nature connectedness and happiness: A meta-analysis. Front. Psychol. 2014, 5, 976. [Google Scholar] [CrossRef] [PubMed]
- Flowers, E.P.; Freeman, P.; Gladwell, V.F. A cross-sectional study examining predictors of visit frequency to local green space and the impact this has on physical activity levels. BMC Public Health 2016, 16, 420. [Google Scholar] [CrossRef] [PubMed]
- Dubos, R. The Mirage of Health: Utopias, Progress and Biological Change; Rutgers University Press: New Brunswick, NJ, USA, 1959. [Google Scholar]
- Prescott, S.L. Disease prevention in the age of convergence—The need for a wider, long ranging and collaborative vision. Allergol. Int. 2014, 63, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Logan, A.C.; Jacka, F.N.; Prescott, S.L. Immune-microbiota interactions: Dysbiosis as a global health issue. Curr. Allergy Asthma Rep. 2016, 16, 13. [Google Scholar] [CrossRef] [PubMed]
- Petersen, C.; Round, J.L. Defining dysbiosis and its influence on host immunity and disease. Cell. Microbiol. 2014, 16, 1024–1033. [Google Scholar] [CrossRef] [PubMed]
- Szczesniak, O.; K, A.H.; Hanssen, J.F.; Rudi, K. Isovaleric acid in stool correlates with human depression. Nutr. Neurosci. 2015, 19, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Naseribafrouei, A.; Hestad, K.; Avershina, E.; Sekelja, M.; Linlokken, A.; Wilson, R.; Rudi, K. Correlation between the human fecal microbiota and depression. Neurogastroenterol. Motil. 2014, 26, 1155–1162. [Google Scholar] [CrossRef] [PubMed]
- Zheng, P.; Zeng, B.; Zhou, C.; Liu, M.; Fang, Z.; Xu, X.; Zeng, L.; Chen, J.; Fan, S.; Du, X.; et al. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host’s metabolism. Mol. Psychiatry 2016, 21, 786–796. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.R.; Borre, Y.; C, O.B.; Patterson, E.; El Aidy, S.; Deane, J.; Kennedy, P.J.; Beers, S.; Scott, K.; Moloney, G.; et al. Transferring the blues: Depression-associated gut microbiota induces neurobehavioural changes in the rat. J. Psychiatr. Res. 2016, 82, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Aizawa, E.; Tsuji, H.; Asahara, T.; Takahashi, T.; Teraishi, T.; Yoshida, S.; Ota, M.; Koga, N.; Hattori, K.; Kunugi, H. Possible association of bifidobacterium and lactobacillus in the gut microbiota of patients with major depressive disorder. J. Affect. Disord. 2016, 202, 254–257. [Google Scholar] [CrossRef] [PubMed]
- Tochitani, S.; Ikeno, T.; Ito, T.; Sakurai, A.; Yamauchi, T.; Matsuzaki, H. Administration of non-absorbable antibiotics to pregnant mice to perturb the maternal gut microbiota is associated with alterations in offspring behavior. PLoS ONE 2016, 11, e0138293. [Google Scholar] [CrossRef] [PubMed]
- Lurie, I.; Yang, Y.X.; Haynes, K.; Mamtani, R.; Boursi, B. Antibiotic exposure and the risk for depression, anxiety, or psychosis: A nested case-control study. J. Clin. Psychiatry 2015, 76, 1522–1528. [Google Scholar] [CrossRef] [PubMed]
- Logan, A.C.; Jacka, F.N.; Craig, J.M.; Prescott, S.L. The microbiome and mental health: Looking back, moving forward with lessons from allergic diseases. Clin. Psychopharmacol. Neurosci. 2016, 14, 131–147. [Google Scholar] [CrossRef] [PubMed]
- Pirbaglou, M.; Katz, J.; de Souza, R.J.; Stearns, J.C.; Motamed, M.; Ritvo, P. Probiotic supplementation can positively affect anxiety and depressive symptoms: A systematic review of randomized controlled trials. Nutr. Res. 2016, 36, 889–898. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Wang, K.; Hu, J. Effect of probiotics on depression: A systematic review and meta-analysis of randomized controlled trials. Nutrients 2016. [Google Scholar] [CrossRef] [PubMed]
- Dinan, T.G.; Stanton, C.; Cryan, J.F. Psychobiotics: A novel class of psychotropic. Biol. Psychiatry 2013, 74, 720–726. [Google Scholar] [CrossRef] [PubMed]
- Logan, A.C. Dysbiotic drift: Mental health, environmental grey space, and microbiota. J. Physiol. Anthropol. 2015, 34, 23. [Google Scholar] [CrossRef] [PubMed]
- Miller, G.E.; Engen, P.A.; Gillevet, P.M.; Shaikh, M.; Sikaroodi, M.; Forsyth, C.B.; Mutlu, E.; Keshavarzian, A. Lower neighborhood socioeconomic status associated with reduced diversity of the colonic microbiota in healthy adults. PLoS ONE 2016, 11, e0148952. [Google Scholar] [CrossRef] [PubMed]
- Strachan, D.P. Hay fever, hygiene, and household size. BMJ 1989, 299, 1259–1260. [Google Scholar] [CrossRef] [PubMed]
- Wold, A.E. The hygiene hypothesis revised: Is the rising frequency of allergy due to changes in the intestinal flora? Allergy 1998, 53, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Fox, M.; Knapp, L.A.; Andrews, P.W.; Fincher, C.L. Hygiene and the world distribution of alzheimer’s disease: Epidemiological evidence for a relationship between microbial environment and age-adjusted disease burden. Evol. Med. Public Health 2013, 2013, 173–186. [Google Scholar] [CrossRef] [PubMed]
- Selhub, E.M.; Logan, A.C.; Bested, A.C. Fermented foods, microbiota, and mental health: Ancient practice meets nutritional psychiatry. J. Physiol. Anthropol. 2014, 33, 2. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Bae, J.H. Fermented food intake is associated with a reduced likelihood of atopic dermatitis in an adult population (Korean national health and nutrition examination survey 2012–2013). Nutr. Res. 2016, 36, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Hesselmar, B.; Hicke-Roberts, A.; Wennergren, G. Allergy in children in hand versus machine dishwashing. Pediatrics 2015, 135, e590–e597. [Google Scholar] [CrossRef] [PubMed]
- Hilimire, M.R.; DeVylder, J.E.; Forestell, C.A. Fermented foods, neuroticism, and social anxiety: An interaction model. Psychiatry Res. 2015, 228, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Ozawa, N.; Shimojo, N.; Suzuki, Y.; Ochiai, S.; Nakano, T.; Morita, Y.; Inoue, Y.; Arima, T.; Suzuki, S.; Kohno, Y. Maternal intake of natto, a Japan’s traditional fermented soybean food, during pregnancy and the risk of eczema in Japanese babies. Allergol. Int. 2014, 63, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Cepeda, M.S.; Katz, E.G.; Blacketer, C. Microbiome-gut-brain axis: Probiotics and their association with depression. J. Neuropsychiatry Clin. Neurosci. 2016. [Google Scholar] [CrossRef] [PubMed]
- Covvey, J.R.; Johnson, B.F.; Elliott, V.; Malcolm, W.; Mullen, A.B. An association between socioeconomic deprivation and primary care antibiotic prescribing in Scotland. J. Antimicrob. Chemother. 2014, 69, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Hicks, L.A.; Bartoces, M.G.; Roberts, R.M.; Suda, K.J.; Hunkler, R.J.; Taylor, T.H., Jr.; Schrag, S.J. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clin. Infect. Dis. 2015, 60, 1308–1316. [Google Scholar] [CrossRef] [PubMed]
- Jensen, J.N.; Bjerrum, L.; Boel, J.; Jarlov, J.O.; Arpi, M. Parents’ socioeconomic factors related to high antibiotic prescribing in primary health care among children aged 0–6 years in the capital region of Denmark. Scand. J. Prim. Health Care 2016, 34, 274–281. [Google Scholar] [CrossRef] [PubMed]
- De Araujo, H.B.; Carmo-Rodrigues, M.S.; Mello, C.S.; Melli, L.C.F.L.; Tahan, S.; Pignatari, A.C.C.; de Morais, M.B. Children living near a sanitary landfill have increased breath methane and methanobrevibacter smithii in their intestinal microbiota. Archaea 2014, 2014, 576249. [Google Scholar]
- Seedorf, H.; Griffin, N.W.; Ridaura, V.K.; Reyes, A.; Cheng, J.Y.; Rey, F.E.; Smith, M.I.; Simon, G.M.; Scheffrahn, R.H.; Woebken, D.; et al. Bacteria from diverse habitats colonize and compete in the mouse gut. Cell 2014, 159, 253–266. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.D.; Compher, C.; Chen, E.Z.; Smith, S.A.; Shah, R.D.; Bittinger, K.; Chehoud, C.; Albenberg, L.G.; Nessel, L.; Gilroy, E.; et al. Comparative metabolomics in vegans and omnivores reveal constraints on diet-dependent gut microbiota metabolite production. Gut 2016, 65, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Escobar, J.S.; Klotz, B.; Valdes, B.E.; Agudelo, G.M. The gut microbiota of colombians differs from that of americans, europeans and asians. BMC Microbiol. 2014, 14, 311. [Google Scholar] [CrossRef] [PubMed]
- Locey, K.J.; Lennon, J.T. Scaling laws predict global microbial diversity. Proc. Natl. Acad. Sci. USA 2016, 113, 5970–5975. [Google Scholar] [CrossRef] [PubMed]
- Ruokolainen, L.; von Hertzen, L.; Fyhrquist, N.; Laatikainen, T.; Lehtomaki, J.; Auvinen, P.; Karvonen, A.M.; Hyvarinen, A.; Tillmann, V.; Niemela, O.; et al. Green areas around homes reduce atopic sensitization in children. Allergy 2015, 70, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Hanski, I.; von Hertzen, L.; Fyhrquist, N.; Koskinen, K.; Torppa, K.; Laatikainen, T.; Karisola, P.; Auvinen, P.; Paulin, L.; Makela, M.J.; et al. Environmental biodiversity, human microbiota, and allergy are interrelated. Proc. Natl. Acad. Sci. USA 2012, 109, 8334–8339. [Google Scholar] [CrossRef] [PubMed]
- Mhuireach, G.; Johnson, B.R.; Altrichter, A.E.; Ladau, J.; Meadow, J.F.; Pollard, K.S.; Green, J.L. Urban greenness influences airborne bacterial community composition. Sci. Total Environ. 2016, 571, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Lymperopoulou, D.S.; Adams, R.I.; Lindow, S.E. Contribution of vegetation to the microbial composition of nearby outdoor air. Appl. Environ. Microbiol. 2016, 82, 3822–3833. [Google Scholar] [CrossRef] [PubMed]
- Lowry, C.A.; Hollis, J.H.; de Vries, A.; Pan, B.; Brunet, L.R.; Hunt, J.R.; Paton, J.F.; van Kampen, E.; Knight, D.M.; Evans, A.K.; et al. Identification of an immune-responsive mesolimbocortical serotonergic system: Potential role in regulation of emotional behavior. Neuroscience 2007, 146, 756–772. [Google Scholar] [CrossRef] [PubMed]
- Matthews, D.M.; Jenks, S.M. Ingestion of mycobacterium vaccae decreases anxiety-related behavior and improves learning in mice. Behav. Process. 2013, 96, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Reber, S.O.; Siebler, P.H.; Donner, N.C.; Morton, J.T.; Smith, D.G.; Kopelman, J.M.; Lowe, K.R.; Wheeler, K.J.; Fox, J.H.; Hassell, J.E., Jr.; et al. Immunization with a heat-killed preparation of the environmental bacterium mycobacterium vaccae promotes stress resilience in mice. Proc. Natl. Acad. Sci. USA 2016, 113, E3130–E3139. [Google Scholar] [CrossRef] [PubMed]
- Knowles, S.R.; Nelson, E.A.; Palombo, E.A. Investigating the role of perceived stress on bacterial flora activity and salivary cortisol secretion: A possible mechanism underlying susceptibility to illness. Biol. Psychol. 2008, 77, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Sundin, J.; Rangel, I.; Fuentes, S.; Heikamp-de Jong, I.; Hultgren-Hornquist, E.; de Vos, W.M.; Brummer, R.J. Altered faecal and mucosal microbial composition in post-infectious irritable bowel syndrome patients correlates with mucosal lymphocyte phenotypes and psychological distress. Aliment. Pharmacol. Ther. 2015, 41, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Zijlmans, M.A.; Korpela, K.; Riksen-Walraven, J.M.; de Vos, W.M.; de Weerth, C. Maternal prenatal stress is associated with the infant intestinal microbiota. Psychoneuroendocrinology 2015, 53, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Lyte, M. The effect of stress on microbial growth. Anim. Health Res. Rev. 2014, 15, 172–174. [Google Scholar] [CrossRef] [PubMed]
- Tannock, G.W. The lactic microflora of pigs, mice and rats. Lactic Acid Bact. 1992, 1, 21–48. [Google Scholar]
- Timofeyev, I.; Loseva, E.; Alekseeva, T.; Perminova, N. Stability to sound stress and changeability in intestinal microflora. Eur. Psychiatr. 2002, 17, 200. [Google Scholar] [CrossRef]
- Suzuki, K.; Harasawa, R.; Yoshitake, Y.; Mitsuoka, T. Effects of crowding and heat-stress on intestinal flora, body-weight gain, and feed-efficiency of growing-rats and chicks. Jpn. J. Vet. Sci. 1983, 45, 331–338. [Google Scholar] [CrossRef]
- Wu, J.F.; Wen, X.W.; Faulk, C.; Boehnke, K.; Zhang, H.P.; Dolinoy, D.C.; Xi, C.W. Perinatal lead exposure alters gut microbiota composition and results in sex-specific bodyweight increases in adult mice. Toxicol. Sci. 2016, 151, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Ribiere, C.; Peyret, P.; Parisot, N.; Darcha, C.; Dechelotte, P.J.; Barnich, N.; Peyretaillade, E.; Boucher, D. Oral exposure to environmental pollutant benzo[a]pyrene impacts the intestinal epithelium and induces gut microbial shifts in murine model. Sci. Rep. 2016, 6, 31027. [Google Scholar] [CrossRef] [PubMed]
- Salim, S.Y.; Kaplan, G.G.; Madsen, K.L. Air pollution effects on the gut microbiota: A link between exposure and inflammatory disease. Gut Microbes 2014, 5, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Biedermann, L.; Brulisauer, K.; Zeitz, J.; Frei, P.; Scharl, M.; Vavricka, S.R.; Fried, M.; Loessner, M.J.; Rogler, G.; Schuppler, M. Smoking cessation alters intestinal microbiota: Insights from quantitative investigations on human fecal samples using fish. Inflamm. Bowel Dis. 2014, 20, 1496–1501. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zhao, J.X.; Hu, N.; Ren, J.; Du, M.; Zhu, M.J. Side-stream smoking reduces intestinal inflammation and increases expression of tight junction proteins. World J. Gastroenterol. 2012, 18, 2180–2187. [Google Scholar] [CrossRef] [PubMed]
- Allais, L.; Kerckhof, F.M.; Verschuere, S.; Bracke, K.R.; de Smet, R.; Laukens, D.; van den Abbeele, P.; de Vos, M.; Boon, N.; Brusselle, G.G.; et al. Chronic cigarette smoke exposure induces microbial and inflammatory shifts and mucin changes in the murine gut. Environ. Microbiol. 2016, 18, 1352–1363. [Google Scholar] [CrossRef] [PubMed]
- Dubinkina, V.B.; Tyakht, A.V.; Ilina, E.N.; Ischenko, D.S.; Kovarsky, B.A.; Yarygin, K.S.; Pavlenko, A.V.; Popenko, A.S.; Alexeev, D.G.; Taraskina, A.E.; et al. Metagenomic analysis of taxonomic and functional changes in gut microbiota of patients with alcoholic dependence syndrome. Biomed. Khimiia 2015, 61, 742–749. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.E.; Freel, N.; Findley, A.; Tomlin, K.; Howard, K.M.; Seran, C.C.; Cruz, P.; Kingsley, K. A molecular survey of S. mutans and P. gingivalis oral microbial burden in human saliva using Relative Endpoint Polymerase Chain Reaction (RE-PCR) within the population of a Nevada dental school revealed disparities among minorities. BMC Oral Health 2012, 12, 34. [Google Scholar] [CrossRef] [PubMed]
- Arimatsu, K.; Yamada, H.; Miyazawa, H.; Minagawa, T.; Nakajima, M.; Ryder, M.I.; Gotoh, K.; Motooka, D.; Nakamura, S.; Iida, T.; et al. Oral pathobiont induces systemic inflammation and metabolic changes associated with alteration of gut microbiota. Sci. Rep. 2014, 4, 4828. [Google Scholar] [CrossRef] [PubMed]
- Mason, M.; Zaganjor, H.; Bozlak, C.T.; Lammel-Harmon, C.; Gomez-Feliciano, L.; Becker, A.B. Working with community partners to implement and evaluate the chicago park district’s 100% healthier snack vending initiative. Prev. Chronic Dis. 2014, 11, E135. [Google Scholar] [CrossRef] [PubMed]
- Blanck, H.M.; Allen, D.; Bashir, Z.; Gordon, N.; Goodman, A.; Merriam, D.; Rutt, C. Let’s go to the park today: The role of parks in obesity prevention and improving the public’s health. Child. Obes. 2012, 8, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Mena, C.; Fuentes, E.; Ormazabal, Y.; Palomo-Velez, G.; Palomo, I. Role of access to parks and markets with anthropometric measurements, biological markers, and a healthy lifestyle. Int. J. Environ. Health Res. 2015, 25, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, S.; Klassen, A.C.; Curriero, F.C.; Caulfield, L.E.; Cheskin, L.J.; Davis, J.N.; Goran, M.I.; Weigensberg, M.J.; Spruijt-Metz, D. Fast-food restaurants, park access, and insulin resistance among Hispanic youth. Am. J. Prev. Med. 2014, 46, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Carroll-Scott, A.; Gilstad-Hayden, K.; Rosenthal, L.; Peters, S.M.; McCaslin, C.; Joyce, R.; Ickovics, J.R. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: The role of built, socioeconomic, and social environments. Soc. Sci. Med. 2013, 95, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Meyer, K.A.; Boone-Heinonen, J.; Duffey, K.J.; Rodriguez, D.A.; Kiefe, C.I.; Lewis, C.E.; Gordon-Larsen, P. Combined measure of neighborhood food and physical activity environments and weight-related outcomes: The cardia study. Health Place 2015, 33, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Chum, A.; O’Campo, P. Cross-sectional associations between residential environmental exposures and cardiovascular diseases. BMC Public Health 2015, 15, 438. [Google Scholar] [CrossRef] [PubMed]
- Coughenour, C.; Burns, M.S. Community design impacts on health habits in low-income southern Nevadans. Am. J. Health Behav. 2016, 40, 534–544. [Google Scholar] [CrossRef] [PubMed]
- Dubos, R. Science and man’s nature. J. Am. Acad. Art Sci. 1965, 94, 223–244. [Google Scholar]
- Basner, M.; Spaeth, A.M.; Dinges, D.F. Sociodemographic characteristics and waking activities and their role in the timing and duration of sleep. Sleep 2014, 37, 1889–1906. [Google Scholar] [CrossRef] [PubMed]
- Shiue, I. Correlations of indoor second-hand smoking, household smoking rules, regional deprivation and children mental health: Scottish health survey, 2013. Environ. Sci. Pollut. Res. Int. 2015, 22, 9858–9863. [Google Scholar] [CrossRef] [PubMed]
- Laxer, R.E.; Janssen, I. The proportion of excessive fast-food consumption attributable to the neighbourhood food environment among youth living within 1 km of their school. Appl. Physiol. Nutr. Metab. 2014, 39, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Coffee, N.T.; Kennedy, H.P.; Niyonsenga, T. Fast-food exposure around schools in urban Adelaide. Public Health Nutr. 2016, 14, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kestens, Y.; Daniel, M. Social inequalities in food exposure around schools in an urban area. Am. J. Prev. Med. 2010, 39, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Zenk, S.N.; Powell, L.M. US secondary schools and food outlets. Health Place 2008, 14, 336–346. [Google Scholar] [CrossRef] [PubMed]
- Simon, P.A.; Kwan, D.; Angelescu, A.; Shih, M.; Fielding, J.E. Proximity of fast food restaurants to schools: Do neighborhood income and type of school matter? Prev. Med. 2008, 47, 284–288. [Google Scholar] [CrossRef] [PubMed]
- Vandevijvere, S.; Sushil, Z.; Exeter, D.J.; Swinburn, B. Obesogenic retail food environments around New Zealand schools: A national study. Am. J. Prev. Med. 2016, 51, e57–e66. [Google Scholar] [CrossRef] [PubMed]
- D’Angelo, H.; Ammerman, A.; Gordon-Larsen, P.; Linnan, L.; Lytle, L.; Ribisl, K.M. Sociodemographic disparities in proximity of schools to tobacco outlets and fast-food restaurants. Am. J. Public Health 2016, 106, 1556–1562. [Google Scholar] [CrossRef] [PubMed]
- Arredondo, E.; Castaneda, D.; Elder, J.P.; Slymen, D.; Dozier, D. Brand name logo recognition of fast food and healthy food among children. J. Community Health 2009, 34, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Michimi, A.; Wimberly, M.C. The food environment and adult obesity in US metropolitan areas. Geospat. Health 2015, 10, 368. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.E.; Heinrich, K.M.; Reese-Smith, J.Y.; Regan, G.R.; Adamus-Leach, H.J. Obesogenic and youth oriented restaurant marketing in public housing neighborhoods. Am. J. Health Behav. 2014, 38, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.L.; Olive, N.C.; Waters, C.N.; Estabrooks, P.A.; You, W.; Zoellner, J.M. Lack of healthy food options on children’s menus of restaurants in the health-disparate dan river region of Virginia and North Carolina, 2013. Prev. Chronic Dis. 2015, 12, E40. [Google Scholar] [CrossRef] [PubMed]
- Zenk, S.N.; Powell, L.M.; Rimkus, L.; Isgor, Z.; Barker, D.C.; Ohri-Vachaspati, P.; Chaloupka, F. Relative and absolute availability of healthier food and beverage alternatives across communities in the United States. Am. J. Public Health 2014, 104, 2170–2178. [Google Scholar] [CrossRef] [PubMed]
- Isgor, Z.; Powell, L.; Rimkus, L.; Chaloupka, F. Associations between retail food store exterior advertisements and community demographic and socioeconomic composition. Health Place 2016, 39, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Kwate, N.O.; Lee, T.H. Ghettoizing outdoor advertising: Disadvantage and ad panel density in black neighborhoods. J. Urban Health Bull. N. Y. Acad. Med. 2007, 84, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Burgoine, T.; Forouhi, N.G.; Griffin, S.J.; Brage, S.; Wareham, N.J.; Monsivais, P. Does neighborhood fast-food outlet exposure amplify inequalities in diet and obesity? A cross-sectional study. Am. J. Clin. Nutr. 2016, 103, 1540–1547. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, L.; Schleicher, N.C.; Barker, D.C.; Liu, Y.; Chaloupka, F.J. Prices for Tobacco and Nontobacco Products in Pharmacies Versus Other Stores: Results from Retail Marketing Surveillance in California and in the United States. Am. J. Public Health 2016, 106, 1858–1864. [Google Scholar] [CrossRef] [PubMed]
- Cameron, A.J.; Thornton, L.E.; McNaughton, S.A.; Crawford, D. Variation in supermarket exposure to energy-dense snack foods by socio-economic position. Public Health Nutr. 2013, 16, 1178–1185. [Google Scholar] [CrossRef] [PubMed]
- Farley, T.A.; Rice, J.; Bodor, J.N.; Cohen, D.A.; Bluthenthal, R.N.; Rose, D. Measuring the food environment: Shelf space of fruits, vegetables, and snack foods in stores. J. Urban Health Bull. N. Y. Acad. Med. 2009, 86, 672–682. [Google Scholar] [CrossRef] [PubMed]
- Rose, D.; Hutchinson, P.L.; Bodor, J.N.; Swalm, C.M.; Farley, T.A.; Cohen, D.A.; Rice, J.C. Neighborhood food environments and body mass index: The importance of in-store contents. Am. J. Prev. Med. 2009, 37, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.; Diez Roux, A.V.; Glass, T.A.; Caballero, B.; Brancati, F.L. Neighborhood characteristics and availability of healthy foods in baltimore. Am. J. Prev. Med. 2008, 35, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Andreyeva, T.; Blumenthal, D.M.; Schwartz, M.B.; Long, M.W.; Brownell, K.D. Availability and prices of foods across stores and neighborhoods: The case of new haven, connecticut. Health Aff. 2008, 27, 1381–1388. [Google Scholar] [CrossRef] [PubMed]
- Adjoian, T.; Dannefer, R.; Sacks, R.; van Wye, G. Comparing sugary drinks in the food retail environment in six NYC neighborhoods. J. Community Health 2014, 39, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Rimkus, L.; Isgor, Z.; Ohri-Vachaspati, P.; Zenk, S.N.; Powell, L.M.; Barker, D.C.; Chaloupka, F.J. Disparities in the availability and price of low-fat and higher-fat milk in US food stores by community characteristics. J. Acad. Nutr. Diet. 2015, 115, 1975–1985. [Google Scholar] [CrossRef] [PubMed]
- Grigsby-Toussaint, D.S.; Moise, I.K.; Geiger, S.D. Observations of marketing on food packaging targeted to youth in retail food stores. Obesity (Silver Spring) 2011, 19, 1898–1900. [Google Scholar] [CrossRef] [PubMed]
- Bragg, M.A.; Miller, A.N.; Elizee, J.; Dighe, S.; Elbel, B.D. Popular music celebrity endorsements in food and nonalcoholic beverage marketing. Pediatrics 2016. [Google Scholar] [CrossRef] [PubMed]
- Howlett, E.; Davis, C.; Burton, S. From food desert to food oasis: The potential influence of food retailers on childhood obesity rates. J. Bus. Ethics 2015. [Google Scholar] [CrossRef]
- Kahr, M.K.; Suter, M.A.; Ballas, J.; Ramin, S.M.; Monga, M.; Lee, W.; Hu, M.; Shope, C.D.; Chesnokova, A.; Krannich, L.; et al. Geospatial analysis of food environment demonstrates associations with gestational diabetes. Am. J. Obstet. Gynecol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Russell, S.J.; Hughes, K.; Bellis, M.A. Impact of childhood experience and adult well-being on eating preferences and behaviours. BMJ Open 2016, 6, e007770. [Google Scholar] [CrossRef] [PubMed]
- Longacre, M.R.; Drake, K.M.; Titus, L.J.; Cleveland, L.P.; Langeloh, G.; Hendricks, K.; Dalton, M.A. A toy story: Association between young children’s knowledge of fast food toy premiums and their fast food consumption. Appetite 2016, 96, 473–480. [Google Scholar] [CrossRef] [PubMed]
- McGale, L.S.; Halford, J.C.; Harrold, J.A.; Boyland, E.J. The influence of brand equity characters on children’s food preferences and choices. J. Pediatr. 2016, 177, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Scourboutakos, M.J.; Semnani-Azad, Z.; L’Abbe, M.R. Added sugars in kids’ meals from chain restaurants. Prev. Med. Rep. 2016, 3, 391–393. [Google Scholar] [CrossRef] [PubMed]
- Norman, J.; Kelly, B.; Boyland, E.; McMahon, A.T. The impact of marketing and advertising on food behaviours: Evaluating the evidence for a causal relationship. Curr. Nutr. Rep. 2016, 5, 139. [Google Scholar] [CrossRef]
- Moodie, R.; Stuckler, D.; Monteiro, C.; Sheron, N.; Neal, B.; Thamarangsi, T.; Lincoln, P.; Casswell, S.; Lancet, N.C.D.A.G. Profits and pandemics: Prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet 2013, 381, 670–679. [Google Scholar] [CrossRef]
- Mialon, M.; Swinburn, B.; Wate, J.; Tukana, I.; Sacks, G. Analysis of the corporate political activity of major food industry actors in Fiji. Glob. Health 2016, 12, 18. [Google Scholar] [CrossRef] [PubMed]
- Mialon, M.; Swinburn, B.; Allender, S.; Sacks, G. Systematic examination of publicly-available information reveals the diverse and extensive corporate political activity of the food industry in Australia. BMC Public Health 2016, 16, 283. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, S.E.; Zimmerman, F.J.; Adler, G.J., Jr. Increasing public support for food-industry related, obesity prevention policies: The role of a taste-engineering frame and contextualized values. Soc. Sci. Med. 2016, 156, 142–153. [Google Scholar] [CrossRef] [PubMed]
- Goryakin, Y.; Rocco, L.; Suhrcke, M.; Roberts, B.; McKee, M. Fruit and vegetable consumption in the Former Soviet Union: The role of individual- and community-level factors. Public Health Nutr. 2015, 18, 2825–2835. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, F.J.; Shimoga, S.V. The effects of food advertising and cognitive load on food choices. BMC Public Health 2014, 14, 342. [Google Scholar] [CrossRef] [PubMed]
- Childs, E.; de Wit, H. Effects of acute psychosocial stress on cigarette craving and smoking. Nicotine Tob. Res. 2010, 12, 449–453. [Google Scholar] [CrossRef] [PubMed]
- Groth, S.W.; Simpson, A.H.; Fernandez, I.D. The dietary choices of women who are low-income, pregnant, and African American. J. Midwifery Womens Health 2016. [Google Scholar] [CrossRef] [PubMed]
- Gugusheff, J.R.; Ong, Z.Y.; Muhlhausler, B.S. The early origins of food preferences: Targeting the critical windows of development. FASEB J. 2015, 29, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Mercer, S.W.; Higgins, M.; Bikker, A.M.; Fitzpatrick, B.; McConnachie, A.; Lloyd, S.M.; Little, P.; Watt, G.C.M. General practitioners’ empathy and health outcomes: A prospective observational study of consultations in areas of high and low deprivation. Ann. Fam. Med. 2016, 14, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Jani, B.; Bikker, A.P.; Higgins, M.; Fitzpatrick, B.; Little, P.; Watt, G.C.M.; Mercer, S.W. Patient centredness and the outcome of primary care consultations with patients with depression in areas of high and low socioeconomic deprivation. Br. J. Gen. Pract. 2012, 62, e576–e581. [Google Scholar] [CrossRef] [PubMed]
- Mercer, S.W.; Jani, B.D.; Maxwell, M.; Wong, S.Y.S.; Watt, G.C.M. Patient enablement requires physician empathy: A cross-sectional study of general practice consultations in areas of high and low socioeconomic deprivation in scotland. BMC Fam. Pract. 2012, 13, 6. [Google Scholar] [CrossRef] [PubMed]
- Ruberton, P.M.; Huynh, H.P.; Miller, T.A.; Kruse, E.; Chancellor, J.; Lyubomirsky, S. The relationship between physician humility, physician-patient communication, and patient health. Patient Educ. Couns. 2016, 99, 1138–1145. [Google Scholar] [CrossRef] [PubMed]
- Fleming-Dutra, K.E.; Hersh, A.L.; Shapiro, D.J.; Bartoces, M.; Enns, E.A.; File, T.M.; Finkelstein, J.A.; Gerber, J.S.; Hyun, D.Y.; Linder, J.A.; et al. Prevalence of Inappropriate Antibiotic Prescriptions among US Ambulatory Care Visits, 2010–2011. JAMA J. Am. Med. Assoc. 2016, 315, 1864–1873. [Google Scholar] [CrossRef] [PubMed]
- Mercer, S.W.; Watt, G.C.M. The inverse care law: Clinical primary care encounters in deprived and affluent areas of Scotland. Ann. Fam. Med. 2007, 5, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Van der Steen, W.J.; Thung, P.J. Faces of Medicine: A Philosophical Study; Kluwer Academic Press: Dordrecht, The Netherlands, 1988; p. 50. [Google Scholar]
- Levy, B.S.; Patz, J.A. Climate change, human rights, and social justice. Ann. Glob. Health 2015, 81, 310–322. [Google Scholar] [CrossRef] [PubMed]
- Royal Botanic Gardens, Kew. The State of the World’s Plants Report 2016; Royal Botanic Gardens Publication: Kew, UK, 2016.
- Von Hertzen, L.; Beutler, B.; Bienenstock, J.; Blaser, M.; Cani, P.D.; Eriksson, J.; Farkkila, M.; Haahtela, T.; Hanski, I.; Jenmalm, M.C.; et al. Helsinki alert of biodiversity and health. Ann. Med. 2015, 47, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Soga, M.; Gaston, K.J. Extinction of experience: The loss of human-nature interactions. Front. Ecol. Environ. 2016, 14, 94–101. [Google Scholar] [CrossRef]
- Lancet, O. Climate change and non-communicable diseases. Lancet Oncol. 2016, 17, 1. [Google Scholar]
- Speldewinde, P.C.; Cook, A.; Davies, P.; Weinstein, P. A relationship between environmental degradation and mental health in Rural Western Australia. Health Place 2009, 15, 880–887. [Google Scholar] [CrossRef] [PubMed]
- Donovan, G.H.; Butry, D.T.; Michael, Y.L.; Prestemon, J.P.; Liebhold, A.M.; Gatziolis, D.; Mao, M.Y. The Relationship between Trees and Human Health Evidence from the Spread of the Emerald Ash Borer. Am. J. Prev. Med. 2013, 44, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Donovan, G.H.; Michael, Y.L.; Gatziolis, D.; Prestemon, J.P.; Whitsel, E.A. Is tree loss associated with cardiovascular-disease risk in the women’s health initiative? A natural experiment. Health Place 2015, 36, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Willox, A.C.; Harper, S.L.; Ford, J.D.; Edge, V.L.; Landman, K.; Houle, K.; Blake, S.; Wolfrey, C. Climate change and mental health: An exploratory case study from Rigolet, Nunatsiavut, Canada. Clim. Chang. 2013, 121, 255–270. [Google Scholar] [CrossRef]
- Hendrryx, M.; Innes-Wimsatt, K.A. Increased risk of depression for people living in coal mining areas of Central Appalachia. Ecopsychology 2013, 5, 179–187. [Google Scholar] [CrossRef]
- Jones, B.A. Work more and play less? Time use impacts of changing ecosystem services: The case of the invasive emerald ash borer. Ecol. Econ. 2016, 124, 49–58. [Google Scholar] [CrossRef]
- Gardiner, M.M.; Burkman, C.E.; Prajzner, S.P. The value of urban vacant land to support arthropod biodiversity and ecosystem services. Environ. Entomol. 2013, 42, 1123–1136. [Google Scholar] [CrossRef] [PubMed]
- Garvin, E.C.; Cannuscio, C.C.; Branas, C.C. Greening vacant lots to reduce violent crime: A randomised controlled trial. Inj. Prev. 2013, 19, 198–203. [Google Scholar] [CrossRef] [PubMed]
- South, E.C.; Kondo, M.C.; Cheney, R.A.; Branas, C.C. Neighborhood blight, stress, and health: A walking trial of urban greening and ambulatory heart rate. Am. J. Public Health 2015, 105, 909–913. [Google Scholar] [CrossRef] [PubMed]
- Branas, C.C.; Kondo, M.C.; Murphy, S.M.; South, E.C.; Polsky, D.; MacDonald, J.M. Urban blight remediation as a cost-beneficial solution to firearm violence. Am. J. Public Health 2016. [Google Scholar] [CrossRef] [PubMed]
- Cardinale, B.J.; Duffy, J.E.; Gonzalez, A.; Hooper, D.U.; Perrings, C.; Venail, P.; Narwani, A.; Mace, G.M.; Tilman, D.; Wardle, D.A.; et al. Biodiversity loss and its impact on humanity. Nature 2012, 486, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, A.S. Biodiversity and public health. Annu. Rev. Public Health 2014, 35, 153–167. [Google Scholar] [CrossRef] [PubMed]
- Soga, M.; Gaston, K.J.; Yamaura, Y.; Kurisu, K.; Hanaki, K. Both direct and vicarious experiences of nature affect children’s willingness to conserve biodiversity. Int. J. Environ. Res. Public Health 2016, 13, 529. [Google Scholar] [CrossRef] [PubMed]
- Lewis, M.; Townsend, M. 'Ecological embeddedness’ and its public health implications: Findings from an exploratory study. Ecohealth 2015, 12, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Lohr, V.I.; Pearson-Mims, C.H. The relative influence of childhood activities and demographics on adult appreciation for the role of trees in human well-being. Acta Hortic. 2004, 253–259. [Google Scholar] [CrossRef]
- Lohr, V.I.; Pearson-Mims, C.H. Children’s active and passive interactions with plants influence their attitudes and actions toward trees and gardening as adults. Horttechnology 2005, 15, 472–476. [Google Scholar]
- Ratcliffe, M.M.; Merrigan, K.A.; Rogers, B.L.; Goldberg, J.P. The effects of school garden experiences on middle school-aged students’ knowledge, attitudes, and behaviors associated with vegetable consumption. Health Promot. Pract. 2011, 12, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.N.; Martinez, L.C.; Spruijt-Metz, D.; Gatto, N.M. La sprouts: A 12-week gardening, nutrition, and cooking randomized control trial improves determinants of dietary behaviors. J. Nutr. Educ. Behav. 2016, 48, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Utter, J.; Denny, S.; Dyson, B. School gardens and adolescent nutrition and BMI: Results from a national, multilevel study. Prev. Med. 2016, 83, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Alaimo, K.; Beavers, A.W.; Crawford, C.; Snyder, E.H.; Litt, J.S. Amplifying health through community gardens: A framework for advancing multicomponent, behaviorally based neighborhood interventions. Curr. Environ. Health Rep. 2016, 3, 302–312. [Google Scholar] [CrossRef] [PubMed]
- Shay-Margalit, B.; Rubin, O.D. Effect of the israeli “green schools” reform on pupils’ environmental attitudes and behavior. Soc. Nat. Resour. 2016, 30, 112–128. [Google Scholar] [CrossRef]
- Rand, D.G.; Kraft-Todd, G.; Gruber, J. The collective benefits of feeling good and letting go: Positive emotion and (dis)inhibition interact to predict cooperative behavior. PLoS ONE 2015, 10, e0117426. [Google Scholar] [CrossRef] [PubMed]
- Prade, C.; Saroglou, V. Awe’s effects on generosity and helping. J. Posit. Psychol. 2016, 11, 522–530. [Google Scholar] [CrossRef]
- Wang, M.; Saudino, K.J. Positive affect: Phenotypic and etiologic associations with prosocial behaviors and internalizing problems in toddlers. Front. Psychol. 2015, 6, 416. [Google Scholar] [CrossRef] [PubMed]
- Tapia-Fonllem, C.; Corral-Verdugo, V.; Fraijo-Sing, B. Sustainable behavior and quality of life. In Handbook of Environmental Psychology and Quality of Life Research; Fleury-Bahi, G., Pol, E., Navarro, O., Eds.; Springer: New York, NY, USA, 2016. [Google Scholar]
- Aknin, L.B.; Broesch, T.; Hamlin, J.K.; van de Vondervoort, J.W. Prosocial behavior leads to happiness in a small-scale rural society. J. Exp. Psychol. Gen. 2015, 144, 788–795. [Google Scholar] [CrossRef] [PubMed]
- Tasimi, A.; Young, L. Memories of good deeds past: The reinforcing power of prosocial behavior in children. J. Exp. Child. Psychol. 2016, 147, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.K.; Layous, K.; Cole, S.W.; Lyubomirsky, S. Do unto others or treat yourself? The effects of prosocial and self-focused behavior on psychological flourishing. Emotion 2016, 16, 850–861. [Google Scholar] [PubMed]
- Flouri, E.; Sarmadi, Z. Prosocial behavior and childhood trajectories of internalizing and externalizing problems: The role of neighborhood and school contexts. Dev. Psychol. 2016, 52, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, K.M.; Wilcox, S.; Liu, J.; Blair, S.N.; Pate, R.R. Provider advice and women’s intentions to meet weight gain, physical activity, and nutrition guidelines during pregnancy. Matern. Child Health J. 2016. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Belski, R.; Radcliffe, J.; Newton, M. What do pregnant women know about the healthy eating guidelines for pregnancy? A web-based questionnaire. Matern. Child Health J. 2016, 20, 2179–2188. [Google Scholar] [CrossRef] [PubMed]
- Dubos, R. The genius of design. In Proceedings of the Rest of Our Lives, International Design Conference, Aspen, CO, USA, 15–20 June 1969; Chermayeff, I., Wolf, H., Eds.; 1969; pp. 57–63. [Google Scholar]
- Holtz, K.A.; Kokotilo, K.J.; Fitzgerald, B.E.; Frank, E. Exercise behaviour and attitudes among fourth-year medical students at the University of British Columbia. Can. Fam. Phys. 2013, 59, e26–e32. [Google Scholar]
- Cardinal, B.J.; Park, E.A.; Kim, M.; Cardinal, M.K. If exercise is medicine, where is exercise in medicine? Review of U.S. Medical education curricula for physical activity-related content. J. Phys. Act. Health 2015, 12, 1336–1343. [Google Scholar] [CrossRef] [PubMed]
- Adams, K.M.; Kohlmeier, M.; Zeisel, S.H. Nutrition education in U.S. Medical schools: Latest update of a national survey. Acad. Med. 2010, 85, 1537–1542. [Google Scholar] [CrossRef] [PubMed]
- Castillo, M.; Feinstein, R.; Tsang, J.; Fisher, M. Basic nutrition knowledge of recent medical graduates entering a pediatric residency program. Int. J. Adolesc. Med. Health 2015. [Google Scholar] [CrossRef] [PubMed]
- Attorp, A.; Scott, J.E.; Yew, A.C.; Rhodes, R.E.; Barr, S.I.; Naylor, P.J. Associations between socioeconomic, parental and home environment factors and fruit and vegetable consumption of children in grades five and six in British Columbia, Canada. BMC Public Health 2014, 14, 150. [Google Scholar] [CrossRef] [PubMed]
- Finger, J.D.; Varnaccia, G.; Tylleskar, T.; Lampert, T.; Mensink, G.B. Dietary behaviour and parental socioeconomic position among adolescents: The german health interview and examination survey for children and adolescents 2003–2006 (KIGGS). BMC Public Health 2015, 15, 498. [Google Scholar] [CrossRef] [PubMed]
- Fismen, A.S.; Smith, O.R.; Torsheim, T.; Samdal, O. A school based study of time trends in food habits and their relation to socio-economic status among norwegian adolescents, 2001–2009. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glen, K.E.; Thomas, H.M.; Loebach, J.E.; Gilliland, J.A.; Gobert, C.P. Fruit and vegetable consumption among children in a socioeconomically disadvantaged neighbourhood. Can. J. Diet. Pract. Res. 2013, 74, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.C.; Kirshenbaum, D.S.; Yan, J.; Kirshenbaum, E.; Aseltine, R.H. Characterizing changes in student empathy throughout medical school. Med. Teach. 2012, 34, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Neumann, M.; Edelhauser, F.; Tauschel, D.; Fischer, M.R.; Wirtz, M.; Woopen, C.; Haramati, A.; Scheffer, C. Empathy decline and its reasons: A systematic review of studies with medical students and residents. Acad. Med. 2011, 86, 996–1009. [Google Scholar] [CrossRef] [PubMed]
- Gomez, A.; Balsari, S.; Nusbaum, J.; Heerboth, A.; Lemery, J. Perspective: Environment, biodiversity, and the education of the physician of the future. Acad. Med. 2013, 88, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Sarfaty, M.; Kreslake, J.M.; Casale, T.B.; Maibach, E.W. Views of AAAAI members on climate change and health. J. Allergy Clin. Immunol. Pract. 2016, 4, 333–335. [Google Scholar] [CrossRef] [PubMed]
- Sarfaty, M.; Bloodhart, B.; Ewart, G.; Thurston, G.D.; Balmes, J.R.; Guidotti, T.L.; Maibach, E.W. American thoracic society member survey on climate change and health. Ann. Am. Thorac. Soc. 2015, 12, 274–278. [Google Scholar] [CrossRef] [PubMed]
- Sarfaty, M.; Kreslake, J.M.; Bloodhart, B.; Price, K.; Montoro, M.; Casale, T.B.; Folstein, S.; Maibach, E.W. George Mason University Centre for Climate Change Communication: Views of Allergy Specialists on Health Effects of Climate Change. Available online: https://www.aaaai.org/Aaaai/media/MediaLibrary/PDFDocuments/Libraries/Climate-Change-Survey.pdf (accessed on 29 August 2016).
- Huber, M.; Knutti, R. Anthropogenic and natural warming inferred from changes in earth’s energy balance. Nat. Geosci. 2012, 5, 31–36. [Google Scholar] [CrossRef]
- Aaron, D.G.; Siegel, M.B. Sponsorship of national health organizations by two major soda companies. Am. J. Prev. Med. 2016. [Google Scholar] [CrossRef] [PubMed]
- Dubos, R. Man and his environment: Scope, impact and nature. In Environmental Improvement; Marquis, R.W., Ed.; Graduate School Press: Washington, DC, USA, 1966; pp. 3–21. [Google Scholar]
- Dubos, R. The spaceship earth. J. Allergy 1969, 44, 1–9. [Google Scholar] [CrossRef]
- Rutt, R.L.; Gulsrud, N.M. Green justice in the city: A new agenda for urban green space research in Europe. Urban For. Urban Green. 2016, 19, 123–127. [Google Scholar] [CrossRef]
- Wolch, J.R.; Byrne, J.; Newell, J.P. Urban green space, public health, and environmental justice: The challenge of making cities ‘just green enough’. Landsc. Urban Plan. 2014, 125, 234–244. [Google Scholar] [CrossRef]
- Gatersleben, B.; Andrews, M. When walking in nature is not restorative-the role of prospect and refuge. Health Place 2013, 20, 91–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kabisch, N.; Qureshi, S.; Haase, D. Human-environment interactions in urban green spaces—A systematic review of contemporary issues and prospects for future research. Environ. Impact Assess. Rev. 2015, 50, 25–34. [Google Scholar] [CrossRef]
- Kabisch, N.; Haase, D. Green justice or just green? Provision of urban green spaces in Berlin, Germany. Landsc. Urban Plan. 2014, 122, 129–139. [Google Scholar] [CrossRef]
- Appleton, A.A.; Buka, S.L.; Loucks, E.B.; Rimm, E.B.; Martin, L.T.; Kubzansky, L.D. A prospective study of positive early-life psychosocial factors and favorable cardiovascular risk in adulthood. Circulation 2013, 127, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Demakakos, P.; Pillas, D.; Marmot, M.; Steptoe, A. Parenting style in childhood and mortality risk at older ages: A longitudinal cohort study. Br. J. Psychiatry J. Ment. Sci. 2016, 209, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Pulkki-Raback, L.; Elovainio, M.; Hakulinen, C.; Lipsanen, J.; Hintsanen, M.; Jokela, M.; Kubzansky, L.D.; Hintsa, T.; Serlachius, A.; Laitinen, T.T.; et al. Cumulative effect of psychosocial factors in youth on ideal cardiovascular health in adulthood: The cardiovascular risk in young finns study. Circulation 2015, 131, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Haworth, C.M.; Nelson, S.K.; Layous, K.; Carter, K.; Jacobs Bao, K.; Lyubomirsky, S.; Plomin, R. Stability and change in genetic and environmental influences on well-being in response to an intervention. PLoS ONE 2016, 11, e0155538. [Google Scholar] [CrossRef] [PubMed]
- Nikrahan, G.R.; Laferton, J.A.; Asgari, K.; Kalantari, M.; Abedi, M.R.; Etesampour, A.; Rezaei, A.; Suarez, L.; Huffman, J.C. Effects of positive psychology interventions on risk biomarkers in coronary patients: A randomized, wait-list controlled pilot trial. Psychosomatics 2016, 57, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Layous, K.; Chancellor, J.; Lyubomirsky, S. Positive activities as protective factors against mental health conditions. J. Abnorm. Psychol. 2014, 123, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Stahl, J.E.; Dossett, M.L.; LaJoie, A.S.; Denninger, J.W.; Mehta, D.H.; Goldman, R.; Fricchione, G.L.; Benson, H. Relaxation response and resiliency training and its effect on healthcare resource utilization. PLoS ONE 2015, 10, e0140212. [Google Scholar] [CrossRef] [PubMed]
- Hatcher, S.L.; Nadeau, M.S.; Walsh, L.K.; Reynolds, M.; Galea, J.; Marz, K. The teaching of empathy for high-school and college-students—Testing rogerian methods with the interpersonal reactivity index. Adolescence 1994, 29, 961–974. [Google Scholar] [PubMed]
- Barley, E.; Lawson, V. Using health psychology to help patients: Promoting wellbeing. Br. J. Nurs. 2016, 25, 852–855. [Google Scholar] [CrossRef] [PubMed]
- Capaldi, C.A.; Passmore, H.; Nisbet, E.K.; Zelenski, J.M.; Dopko, R.L. Flourishing in nature: A review of connecting with nature and its application as a well-being intervention. Int. J. Wellbeing 2015, 5, 1–6. [Google Scholar] [CrossRef]
- Richardson, M.; Cormack, A.; McRobert, L.; Underhill, R. 30 days wild: Development and evaluation of a large-scale nature engagement campaign to improve well-being. PLoS ONE 2016, 11, e0149777. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lowry, C.A.; Smith, D.G.; Siebler, P.H.; Schmidt, D.; Stamper, C.E.; Hassell, J.E., Jr.; Yamashita, P.S.; Fox, J.H.; Reber, S.O.; Brenner, L.A.; et al. The microbiota, immunoregulation, and mental health: Implications for public health. Curr. Environ. Health Rep. 2016, 3, 270–286. [Google Scholar] [CrossRef] [PubMed]
- Hoisington, A.J.; Brenner, L.A.; Kinney, K.A.; Postolache, T.T.; Lowry, C.A. The microbiome of the built environment and mental health. Microbiome 2015, 3, 60. [Google Scholar] [CrossRef] [PubMed]
- Dominguez-Bello, M.G.; de Jesus-Laboy, K.M.; Shen, N.; Cox, L.M.; Amir, A.; Gonzalez, A.; Bokulich, N.A.; Song, S.J.; Hoashi, M.; Rivera-Vinas, J.I.; et al. Partial restoration of the microbiota of cesarean-born infants via vaginal microbial transfer. Nat. Med. 2016, 22, 250–253. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.C.; Krizan, Z. Walking facilitates positive affect even when expecting the opposite. Emotion 2016, in press. [Google Scholar] [CrossRef] [PubMed]
- Paskett, E.; Thompson, B.; Ammerman, A.S.; Ortega, A.N.; Marsteller, J.; Richardson, D. Multilevel interventions to address health disparities show promise in improving population health. Health Aff. 2016, 35, 1429–1434. [Google Scholar] [CrossRef] [PubMed]
- Mah, C.L.; Cook, B.; Rideout, K.; Minaker, L.M. Policy options for healthier retail food environments in city-regions. Can. J. Public Health 2016, 107, 5343. [Google Scholar] [CrossRef] [PubMed]
- Bryan, C.J.; Yeager, D.S.; Hinojosa, C.P.; Chabot, A.; Bergen, H.; Kawamura, M.; Steubing, F. Harnessing adolescent values to motivate healthier eating. Proc. Natl. Acad. Sci. USA 2016, 113, 10830–10835. [Google Scholar] [CrossRef] [PubMed]
- Thompson, B.; Molina, Y.; Viswanath, K.; Warnecke, R.; Prelip, M.L. Strategies to empower communities to reduce health disparities. Health Aff. 2016, 35, 1424–1428. [Google Scholar] [CrossRef] [PubMed]
- Batis, C.; Rivera, J.A.; Popkin, B.M.; Taillie, L.S. First-year evaluation of Mexico’s tax on nonessential energy-dense foods: An observational study. PLoS Med. 2016, 13, e1002057. [Google Scholar] [CrossRef] [PubMed]
- Cradock, A.L.; Kenney, E.L.; McHugh, A.; Conley, L.; Mozaffarian, R.S.; Reiner, J.F.; Gortmaker, S.L. Evaluating the impact of the healthy beverage executive order for city agencies in Boston, Massachusetts, 2011–2013. Prev. Chronic Dis. 2015, 12, 140549. [Google Scholar] [CrossRef] [PubMed]
- Narain, K.; Mata, A.; Flores, J. Nutrition policy decreases sugar-sweetened beverages in municipal parks: Lessons learned from Carson, California. J. Public Health Manag. Pract. 2016, 22, 392–394. [Google Scholar] [CrossRef] [PubMed]
- Sobko, T.; Tse, M.; Kaplan, M. A randomized controlled trial for families with preschool children—Promoting healthy eating and active playtime by connecting to nature. BMC Public Health 2016, 16, 505. [Google Scholar] [CrossRef] [PubMed]
- Shelton, D.L. Problems in Environmental Protection and Human Rights: A Human Right to the Environment; Social Science Research Network: Rochester, NY, USA, 2001. [Google Scholar]
- Obama, B. Presidential Proclamation—20th Anniversary of Executive Order 12898 on Environmental Justice; The White House Office of the Press Secretary: Washington, DC, USA, 2014.
- Geltman, E.G.; Gill, G.; Jovanovic, M. Beyond baby steps: An empirical study of the impact of environmental justice executive order 12898. Fam. Community Health 2016, 39, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Dubos, R. Celebrations of Life; McGraw-Hill: New York, NY, USA, 1981. [Google Scholar]
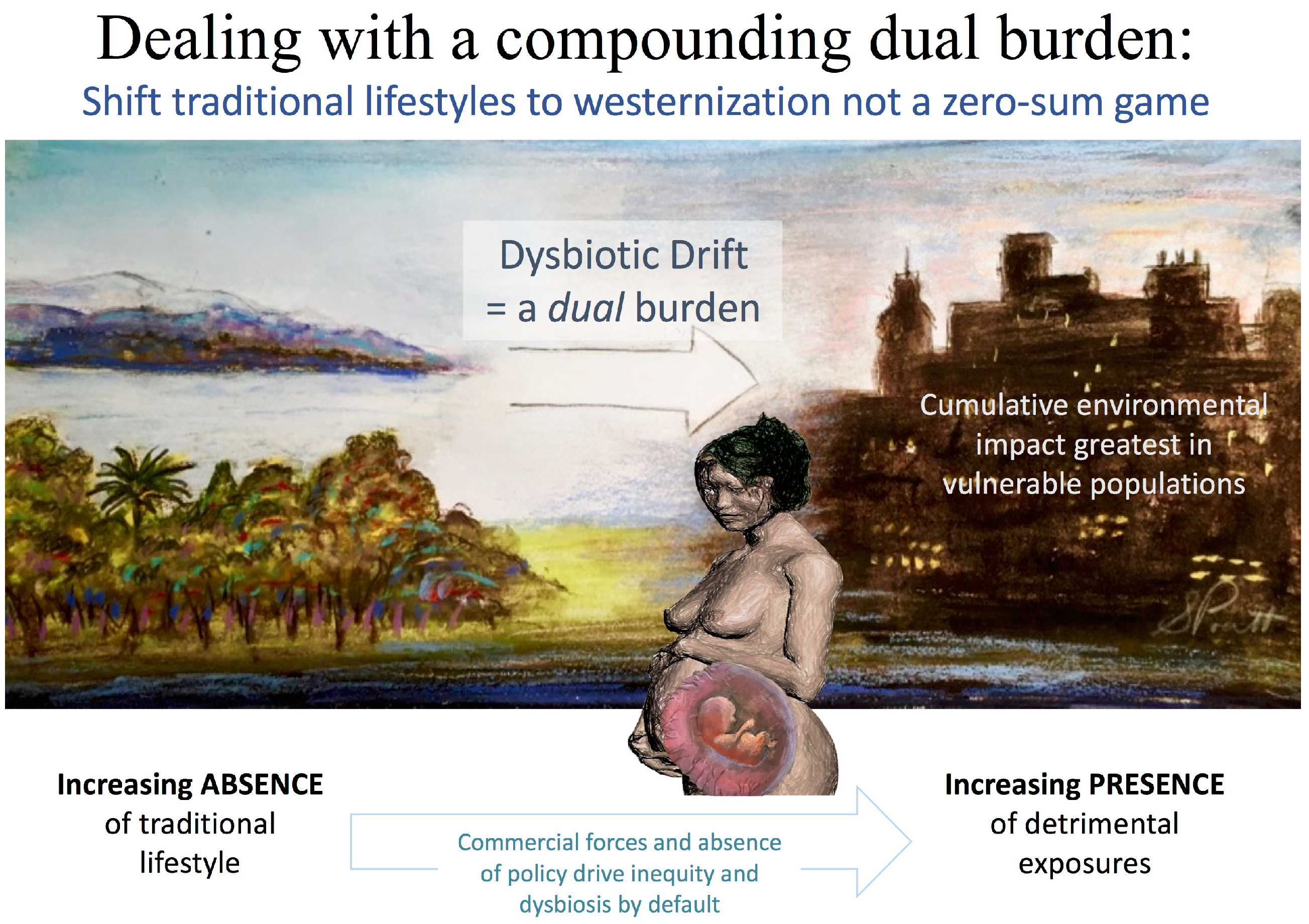

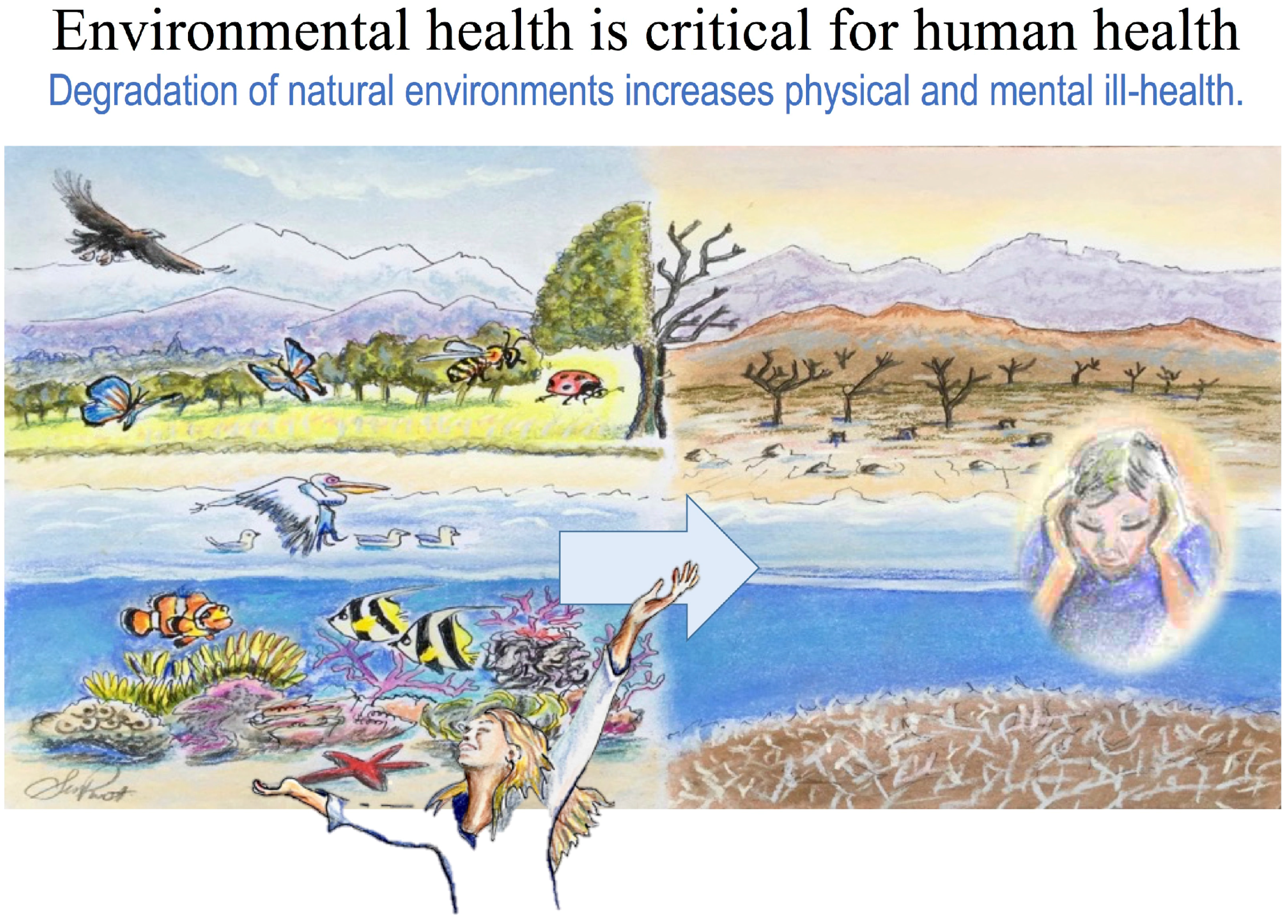



© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prescott, S.L.; Logan, A.C. Transforming Life: A Broad View of the Developmental Origins of Health and Disease Concept from an Ecological Justice Perspective. Int. J. Environ. Res. Public Health 2016, 13, 1075. https://doi.org/10.3390/ijerph13111075
Prescott SL, Logan AC. Transforming Life: A Broad View of the Developmental Origins of Health and Disease Concept from an Ecological Justice Perspective. International Journal of Environmental Research and Public Health. 2016; 13(11):1075. https://doi.org/10.3390/ijerph13111075
Chicago/Turabian StylePrescott, Susan L., and Alan C. Logan. 2016. "Transforming Life: A Broad View of the Developmental Origins of Health and Disease Concept from an Ecological Justice Perspective" International Journal of Environmental Research and Public Health 13, no. 11: 1075. https://doi.org/10.3390/ijerph13111075






