Abstract
Promoting patient safety culture (PSC) is a critical issue for healthcare providers. Quality control circles program (QCCP) can be used as an effective tool to foster long-lasting improvements on the quality of medical institution. The effect of QCCP on PSC is still unknown. This was a retrospective study conducted with matching data. A safety attitudes questionnaire (SAQ) was used for the evaluation of PSC. The association between all scores of six subscales of SAQ and the participation QCCP were analyzed with both the Mann–Whitney and Kruskal–Wallis tests. A total of 2718 valid questionnaires were collected. Most participants of QCCP were females (78.9%), nurses (52.6%), non-supervisors (92.2%), aged <40 years old (64.8%), degree of specialist or university graduates (78%), and with work experience of <10 years (61.6%). Of all participants, the highest scores were in the dimension of safety climate (74.11 ± 17.91) and the lowest scores in the dimension of working conditions (68.90 ± 18.84). The participation of QCCP was associated with higher scores in four dimensions, namely: teamwork climate (p = 0.006), safety climate (p = 0.037), perception of management (p = 0.009), and working conditions (p = 0.015). The participation or not of QCCP had similar results in the dimension of job satisfaction and stress recognition. QCCP was associated with SAQ in subjects with the following characteristics: female, nurse, non-supervisor, aged >50 years old, higher education degrees and with longer working experiences in the hospital. In this first study on the association between each dimension of SAQ and the implementation of QCCP, we found that QCCP interventions were associated with better PSC. QCCP had no benefits in the dimensions of job satisfaction and stress recognition.
1. Introduction
Promoting patient safety is a critical issue for healthcare providers. The World Health Organization has defined patient safety as “the prevention of errors and adverse effects to patients associated with healthcare” and “to do no harm to patients” [1]. Recently, patient safety is becoming a critical issue within healthcare organizations. The patient safety culture (PSC) of employees includes their shared beliefs, attitudes, values, norms, and behavioral characteristics. PSC influences attitudes and behaviors of staff in relation to patient safety performance [2]. It is well established that with a constant improvement in safety culture, medical errors could be reduced, leading to higher quality of healthcare [3,4]. Evidence showed that safety culture influences patient clinical outcomes, like rates of infection and readmission [5,6,7]. The safety attitudes questionnaire (SAQ) was developed by Sexton et al. [8] to evaluate PSCs widely. The three causal dimensions are teamwork climate, stress recognition, and perception of management. The three receiving dimensions are safety climate, job satisfaction, and working conditions [9]. The inter-relationships amongst these six dimensions were studied [9]. For example, teamwork climate and hospital management support for patient safety are two critical dimensions to improve PSCs, since these two dimensions have direct impacts on all six dimensions, with the exception of stress recognition [9]. However, it remains unclear as how to improve PSC in staff having different backgrounds.
Quality control circles program (QCCP) can be used as an effective tool to foster long-lasting improvement in the quality of medical institution. QCCP’s goal is to increase awareness of medical workers on spotting and solving medical problems, improving medical work environments, and eventually bettering safety, quality, and economic performance [10]. QCCP improves safety outcomes, such as facilitating incident reporting and reducing infections and other adverse events [5,11]. QCCPs have been the main focus of our institute, Taichung Veterans General Hospital (TCVGH), with the aim to improve service quality. From 2000 to 2019, our institute has conducted 30 QCCPs/year achieving good results [12,13,14]. Our QCCP activities included projects to reduce complications caused by venous indwelling needles, reducing internal errors from prescription dispensed for outpatients [10,15].
A variety of strategies have been used to improve PSC, like those in Taiwan from 2009 to 2016 [16]. Previous studies reported that three common types of interventions promote PSC: team training and team communication tools, executive walk rounds and interdisciplinary rounding, and comprehensive unit-based safety program [17]. The results showed that QCCP has prominent effects in long-lasting improvement in the quality of medical organizations [18]. However, the influence of QCCP on the PSC has been explored by only one study, in which the questionnaire of Hospital Survey on Patient Safety Culture (HSOPSC) was used as outcome after the establishment of QCCP [19]. In the present study, we aimed to determine if QCCP participation improves levels of PSC based on a larger case number and using another simpler evaluation tool on patient safety (safety attitude questionnaire (SAQ)).
2. Material and Methods
2.1. Characteristics of Taichung Veterans General Hospital (TCVGH)
This study was conducted in TCVGH, which is a 1500-bed medical center with around 5500 employees, located in Taichung City of Taiwan. As a public medical center, it aims to provide safe, high-quality medical services with advanced facilities and training programs as well as outstanding research and development programs. TCVGH is the referral hospital for the critically ill and difficult cases in central Taiwan. The case-mix index (levels of complexity/risk of disease and difficulty in treatment) of our patients is higher compared with other referral hospitals in Taiwan. In addition, it provides patient-centered holistic care with advanced equipment and technology. It involves multiple cross-department centers to provide integrated care services.
Center for Quality Management
Founded in July of 1986, TCVGH Quality of Medical Care Committee was chaired by the vice president of the institute and was responsible for the evaluation and management of issues concerning healthcare quality. Most departments and divisions formed their own Healthcare Quality Improvement Circles. They involved either a single unit or multidisciplinary team, to improve issues of healthcare quality including nursing care, environment safety, quality, and clinical process of patient care, and cross-department communications. The ultimate goal was to reduce medical costs, to improve patient satisfaction, and to better the public image of TCVGH.
2.2. Quality Control Circle program (QCCP)
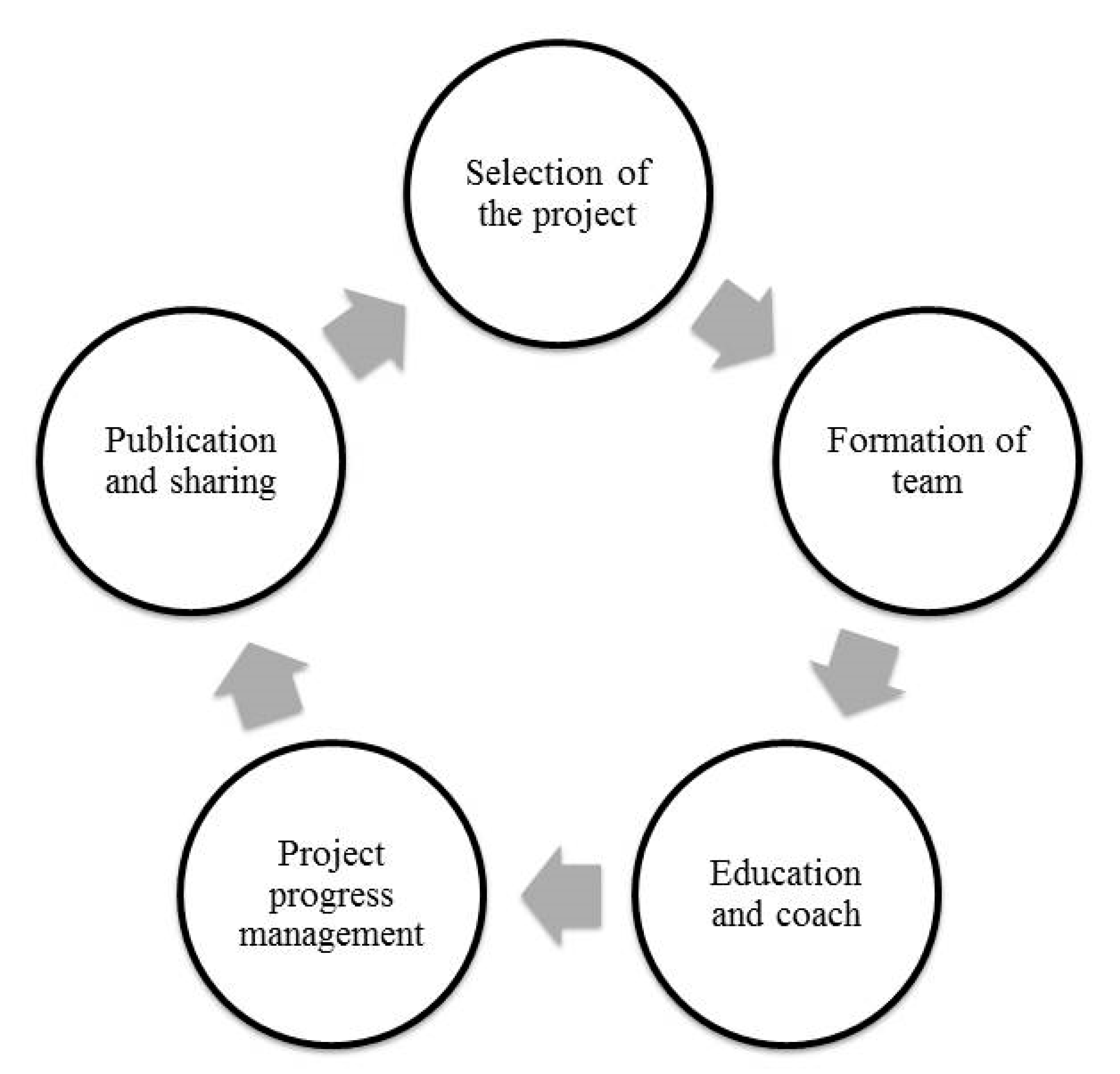
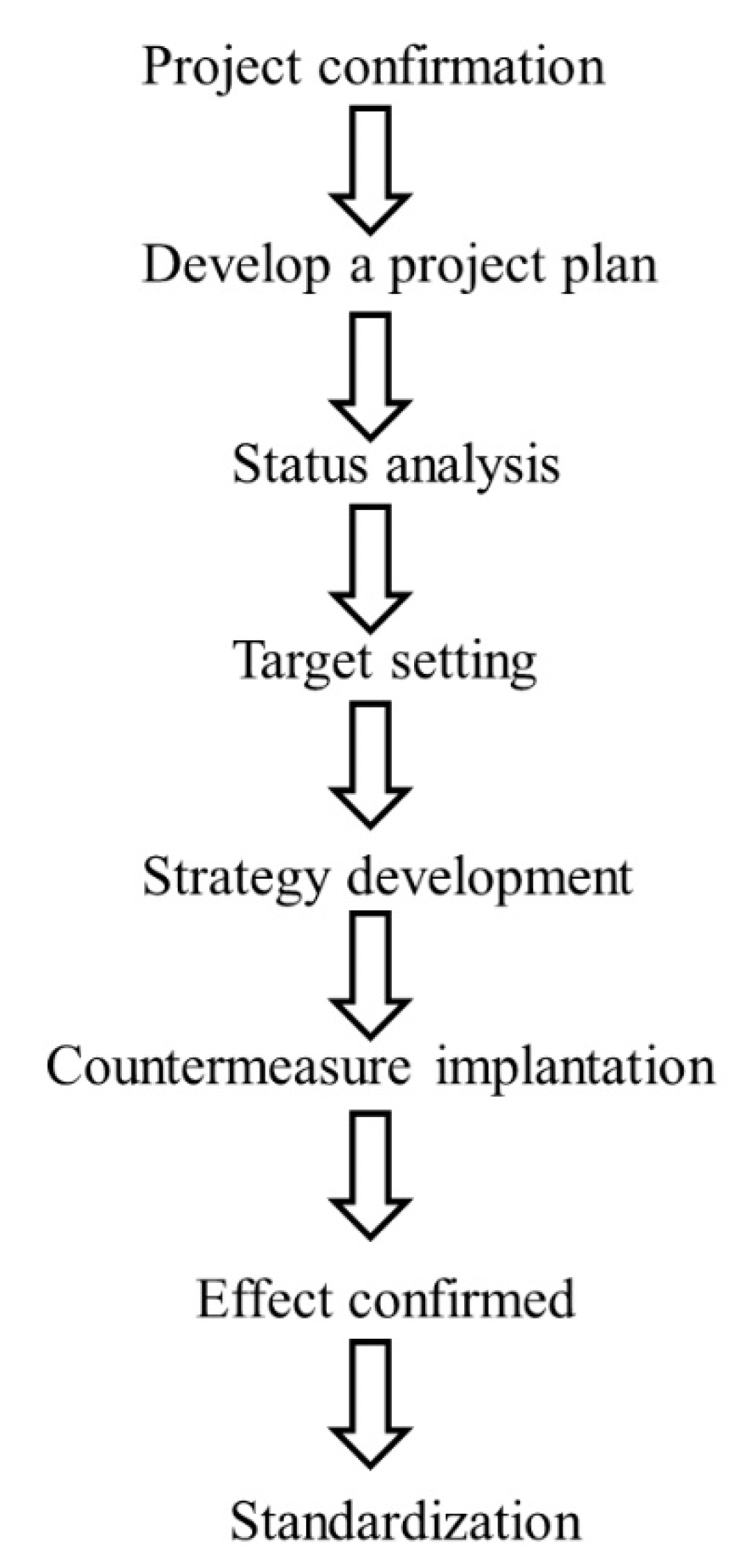
In 2000, our hospital started the comprehensive quality management, with the clinical department forming a QCCP to solve clinical problems to enhance the quality of healthcare. At the same time, the annual plan of QCCP was set up by the quality management center (Figure 1). This hospital arranged quality management-related education training for team members and provided expert guidance, and tracked the progress of each team based on the annual schedule of planning by the Quality Management Center (Figure 2). Each project was completed within a year, and results later published. T encouraged every project team translating results into the form of full papers to be published internationally at medical conferences.
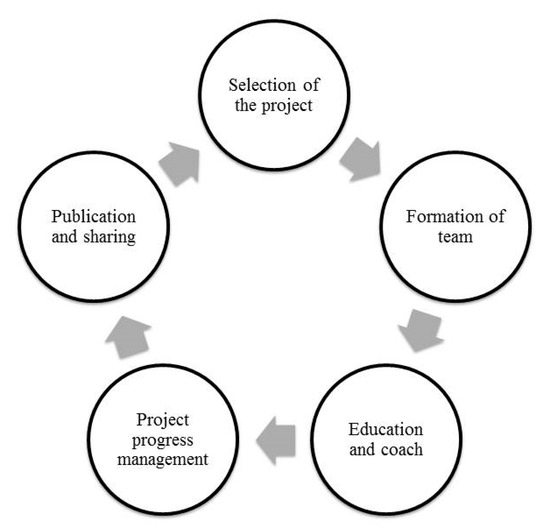
Figure 1.
Annual activity plan of quality control circles program (QCCP).
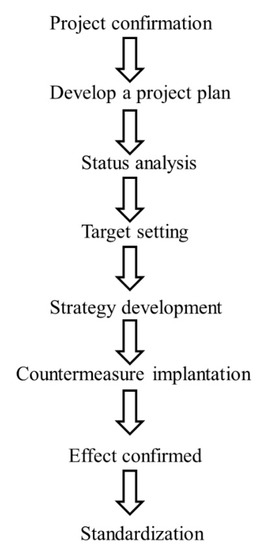
Figure 2.
Flow chart of the project.
2.3. Annula Survey of Safety Attitude Questionnaire (SAQ)
In 2009, our hospital implemented annual SAQ-based surveys regarding issues of patient safety. SAQ was first developed at the University of Texas. It is the one of the widely used instruments for PSC research in the healthcare industry [8,20,21]. SAQ contains 30 items to evaluate organizational staff’s opinions or attitudes toward PSC issues. It measures as already mentioned: namely teamwork climate, safety climate, job satisfaction, perception of management leadership, working conditions, and stress perception. Staff of the hospital (medical staff, and administrative personnel of all units, excluding short-term workers such as medical students and temporary workers) is typically asked to do the survey via an e-learning system. Each respondent rates 30 items according to a 5-point Likert scale ranging from strongly disagree to strongly agree, or a frequency such as “never, rarely, sometimes, most of the time and always”. The baseline data of subjects are collected for analysis, including job position (doctors, nurses, medical staff or administration staff), gender, supervisor or not, employment type (government employment or not), age, educational qualification, and years of experience in this hospital. Previous studies identified the above factors are associated with patient safety [21,22,23].
From 1 November 2018 to 30 November 2018, we conducted a cross-sectional survey using the SAQ questionnaire. At the time of completing the SAQ questionnaire, we also asked colleagues to indicate whether they had participated or not in the QCCP held in the hospital. Then, we analyzed possible effects from participating QCCP on their SAQ scores. All staff in this institute was encouraged to make response to this questionnaire. This survey had been performed from 2012 to 2020. This is voluntary only. The study protocol was approved by the Institutional Review Board of Taichung Veterans General Hospital in Taiwan (No: CW17045A). Informed consents of patients and family were waived, due to the pure data analysis nature of the study.
2.4. Statistical Methods
Frequency and descriptive statistics were generated for each variable in the questionnaire. Categorical data (i.e., profession, position, sex, educational level) were presented as frequency distribution and proportion. Numerical data (i.e., age, and years of work experience) were presented as mean ± standard deviation (SD). Initial data on variables of interest (i.e., job position, gender, supervisor, employment type, age, educational qualification and years of work experience in the hospital) between participating QCC or not were analyzed. The independent sample t-test was used to compare the means of continuous variables, and the Chi-square test was used to compare categorical variables between independent groups. After 1:1 data matching to reduce selection bias and to strengthen casual effects, we obtained a new database without any difference in the participation or not of QCCP across all variables of interest. After data matching, associations between scores of 6 subscales of SAQ and the participation of QCCP or not were determined using the Mann–Whitney and Kruskal–Wallis tests. The statistically significant difference was set at p < 0.05. The SPSS software (Statistical Package for the Social Science, version 20.0, Armonk, NY, USA) was used for all statistical analyses.
3. Results
3.1. Characteristics of Respondents
In this cross-sectional study, we collected 3939 questionnaires from staff. Initially, 2840 questionnaires were performed. After excluding invalid questionnaires (122 partially completed only), we finally analyzed a total of 2718 valid questionnaires. Of them, 502 employees had participated in the QCCP. All baseline demographic characteristics of participants are shown in Table 1. Most participants of QCCP were female (78.9%), nurses (52.6%), non-supervisors (92.2%), aged <40 years old (64.8%), holding degrees of specialist or university (78%), and with working experience <10 years (61.6%). All these baseline variables were associated with the participation of QCCP or not (p values all <0.05). However, after data matching, all baseline variables were not different between participation of QCCP or not.

Table 1.
Demographic characteristics of participants (before and after 1:1 matching).
3.2. Associations between QCC Implementation and Scores of SAQ
Table 2 shows mean difference of SAQ subscale between those with or without QCCP participation. Of them, total participants had the highest score in the dimension of safety climate (74.11 ± 17.91) and the lowest score in the dimension of working conditions (68.90 ± 18.84). After participation in QCCP, staff showed higher scores in the following four dimensions: teamwork climate (75.5 ± 18 vs. 72.4 ± 18.4, p = 0.006), safety climate (75.3 ± 17.9 vs. 73.0 ± 17.9, p = 0.037), perception of management (72.9 ± 19.5 vs. 70.1 ± 18.7, p = 0.009), and working conditions (70.4 ± 19.5 vs. 67.5 ± 18.1, p = 0.015). Participation of QCCP or not however, had no effect on the dimension of job satisfaction and stress recognition.

Table 2.
Scores of safety attitudes questionnaire (SAQ) subscales between participants with or without QCC.
3.3. Associations between QCC Implementation and All Background Variables in the 6 Dimensions of SAQ
Associations between scores of the 6 dimensions of SAQ (with QCCP participation or not) and different baseline conditions are shown in Table 3. For the dimension of teamwork climate, staff showing higher scores were doctors, males, supervisors, public service workers, aged >50 years old, higher education degrees, and longer working experience in our hospital. In contrast, staff showing the lowest scores were administration staff, females, non-supervisors, non-public service workers, aged 31 to 40 years old, with lower education degree and shorter working experiences (5 to 10 years in our hospital). The participation of QCCP was associated with better teamwork climate in nurses (p = 0.016), females (p = 0.009), non-supervisors (p = 0.017), public service workers (p = 0.032), aged >40 years old (p = 0.042 for 41–50 years old and p = 0.036 for >50 years old), with higher education degrees (p = 0.001), and longer (>20 years) working experiences in our hospital (p = 0.012).

Table 3.
Scores of six subscales shown according to participants with or without QCC.
For the dimension of safety climate, staff having higher scores were doctors, males, supervisors, public service workers, aged >50 years old, with higher education degrees, and longer (>20 years) work experience. On the contrary, staff with the lowest scores was administration staff, females, non-supervisors, non-public service workers, aged 31 to 40 years old, with lower education degrees, and shorter work experience (5 to 10 years) in our hospital. The participation of QCCP was associated with better safety climate for administration staff (p = 0.018), non-supervisor (p = 0.032), aged 41 to 50 years old (p = 0.03), with higher education degrees (p = 0.009), and longer (>20 years) of work experience in our hospital (p = 0.018).
For the dimension of perception of management, staff with higher scores were doctors, males, supervisors, public service workers, aged >50 years old, with higher education degrees, and longer work experience (>20 years). On the contrary, staff with the lowest scores was administration staff, females, non-supervisors, non-public service workers, aged 31 to 40 years old, with lower education degrees, and shorter work experience (5 to 10 years) in our hospital. The participation of QCCP was associated with better perception of management in administration staff (p = 0.002), males (p = 0.049), non-supervisors (p = 0.019), public service workers (p = 0.031), aged >50 years old (p = 0.006), with higher education degrees (p = 0.002), and longer (>20 years) of work experience in our hospital (p = 0.014).
For the dimension of working conditions, staff with higher scores were doctors, males, supervisors, public service workers, aged >50 years old, with higher education degrees, and longer work experience (>20 years). On the contrary, staff with lowest scores was administration staff, females, non-supervisors, non-public service workers, aged 31 to 40 years old, with lower education degrees, and shorter work experience (5 to 10 years) in our hospital. The participation of QCCP was associated with better working conditions in males (p = 0.005), non-supervisors (p = 0.036), aged >50 years old (p = 0.004), with higher education degrees (p = 0.012), and longer work experience (>20 years) in our hospital (p = 0.001).
For the dimension of job satisfaction, staff with higher scores were doctors, males, supervisors, public service workers, aged >50 years old, with higher education degrees, and work experience of >20 years. On the contrary, staff with the lowest scores was administration staff females, non-supervisors, non-public service workers, aged <40 years old, with lower education degrees, and shorter work experience (1 to 10 years) in our hospital. The participation of QCCP did not affect job satisfaction under all conditions.
For the dimension of stress recognition, staff with higher scores were nurses, females, and aged 41 to 50 years old. On the contrary, staff with the lowest scores was administration staff (for QCC-) and doctors (QCC+), males, and those aged >50 years old. The participation of QCCP only improved stress recognition for those worked for 11 to 20 years in our hospital (p = 0.024).
4. Discussion
This study is the first one to investigate the association between SAQ and QCCP. The introduction of QCCP had not been integrated to improve patient care safety until 2018 [24]. Noviyanti et al. reported that implementation of quality control circle has a significant effect on patient safety and recommended implementing QCCP as a problem-solving approach to optimize patient safety [24]. In 2019, another study was also published to show a positive association between QCCP and HSOPSC [19]. Many safety culture surveys exist, but only two of them have been used extensively: HSOPSC [25] and SAQ [8]. SAQ and HSOPSC are similar in terms of reliability and predictive validity [26]. The implementation of QCCP produced higher HSOPSC scores (3.73 ± 0.61 vs. 3.57 ± 0.41, p < 0.05) based on a study with limited sample size [19]. The multiple linear regression of data in that study was only 0.407, indicating that the evidence is not compelling. There could be more independent variables. Thirdly, that study did not analyze the associations between each dimension of HSOPSC and QCCP. On the other hand, our present study had much more cases (2718 instead of their 685) for evaluating associations between each dimensions of PSC and the implementation of QCCP for quality improvement. Even their HSOPSC measures included more dimensions than the SAQ, that study failed to analyze each of the dimensions [19]. In addition, HSOPSC is more complicated than SAQ. SAQ is shorter, and one can evaluate PSC efficiently over a shorter time [26]. Our present study is the first one to elucidate the association between each dimension of SAQ and the implementation of QCCP.
Different characteristics of participants were associated with different results of SAQ. Of all scores of SAQ (Table 2), the result revealed that the highest score in the dimension of safety climate (74.11 ± 17.91) and the lowest score in the dimension of working conditions (68.90 ± 18.84). These results are associated with different background characteristics of participants in this study (Table 1): mostly females (78.9%), nurses (52.6%), non-supervisor (92.2%), younger than 40 years old (64.8%), with lower education degree (78%), and working period less than 10 years (61.6%). Those types of staff were younger and apt to obey orders. In the pre-employment training, we were enthusiastic on promoting PSC. The concept of safety climate was likely consolidated in their minds. In addition, in the past 10 years, we have been constantly promoting PSC. Therefore, most participants experienced the dimension of safety climate strongly. The lowest score was in the dimension of working conditions. That result is associated with more newly graduated nurses. For them, they had lower confidence in coping with patients, unfriendly senior staff, more sense of isolation and more pressure of burnout according to previous studies [27,28]. Kramer et al described the beginning work experience of new nurses as “reality shock” [28]. Therefore, they felt weaker support in working conditions, which was associated with lower scores in this dimension.
Different characteristics of participants were associated with different results of the implementation of QCCP. For all participants after the implementation of QCCP (Table 2), they made progress in four out of six dimensions of PSC (namely teamwork climate, safety climate, perception of management and working conditions). However, the participation of QCCP or not had no effect on the dimension of job satisfaction and stress recognition. There was still no effect on these two dimensions after the implementation of QCCP in all variables, including job position, gender, supervisor or not, employment type, age groups, education level, and working experience (Table 3). Some reasons can explain this result. The implementation of QCCP was requested by management unit and the topic should be associated with patient safety. Team members should include young staff in order to train them and adequately supervise them. All processes of QCCP were associated with four dimensions of SAQ (i.e., teamwork climate, safety climate, perception of management, and working conditions). The spirit of QCCP was not associated with job satisfaction and stress recognition. In addition, other more important factors (such as higher pay and salary, and psychological empowerment) are found to associate with job satisfaction [29]. QCCP alone therefore cannot improve this dimension significantly. As for stress recognition, it recognition influences job satisfaction but it is not associated with other dimensions, according to a study using causal relationship analysis [9].
For a variety of participants (i.e., doctor, male, supervisor, public service, older than 40 years of age, higher education degree, and longer than 20-year work experience in this hospital), they had significantly higher scores in nearly all dimensions (i.e., teamwork climate, safety climate, perception of management, working conditions, and job satisfaction) (Table 3). Even with such high scores, some characteristics (older than 50 years old, higher education degree and more experienced in this hospital) were still found to associate with improved scores after the implementation of QCCP
In the four former dimensions, the above characteristics (i.e., >50 years old, higher education degree, and more experienced in this hospital) indicated their greater dedication or faith to the institute. They were also more open-minded and more willing to join quality improvement. On the contrary, for those characteristics (non-doctor, female, and non-supervisor) associated with lower scores, they still showed improvements after the implementation of QCCP.
There are some limitations to this study. First, we did not record topics of QCCP. That could have affected the results of SAQ. Second, we did not analyze the association between all 29 items of SAQ and the implementation of QCCP. Thirdly, this is a retrospective study. We will perform another “before and after” study in the future, to investigate where a causal effect relationship between QCCP participation and improvement of SAQ. Finally, the performance of QCCP may also have affected the results. Despite of these limitations, the strength of our study is being the first one to demonstrate the association of all six dimensions of SAQ and the implementation of QCCP. The findings may help improving QCCP in terms of efficiency and feasibility.
5. Conclusions
Our study is the first one to elucidate the association between each dimension of SAQ and the implementation of QCCP. QCCP can be an intervention to improve PSC. To obtain greater benefits, one could focus on the special group of staff: female, nurses, non-supervisor, those older than 50 years of age, with higher education degrees, and more work experience in the hospital. However, the implementation of QCCP had no benefits on the dimension of job satisfaction and stress recognition.
Author Contributions
Conceptualization, N.-H.T., J.-H.L., W.H.-H.S, and C.L.W.; methodology, N.-H.T., J.-H.L., and C.L.W.; software, N.-H.T., and J.-H.L.; validation, N.-H.T., S.-F.T., J.-H.L., W.H.-H.S., and C.L.W.; formal analysis, N.-H.T., and J.-H.L., Y.-H.L.; investigation, N.-H.T., S.-F.T., and J.-H.L.; resources, S.-A.L., W.H.-H.S., and C.L.W.; data curation, N.-H.T. and J.-H.L.; writing—original draft preparation, N.-H.T., S.-F.T., and J.-H.L.; writing—review and editing, S.-F.T., and C.L.W.; supervision, S.-F.T., S.-A.L., W.H.-H.S., and C.L.W.; project administration, S.-A.L., W.H.-H.S., and C.L.W.; funding acquisition, C.L.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Guldenmund, F.W. The nature of safety culture: A review of theory and research. Safety Sci. 2000, 34, 215–257. [Google Scholar] [CrossRef]
- Morello, R.T.; Lowthian, J.A.; Barker, A.L.; McGinnes, R.; Dunt, D.; Brand, C. Strategies for improving patient safety culture in hospitals: A systematic review. BMJ Qual. Saf. 2013, 22, 11–18. [Google Scholar] [CrossRef] [PubMed]
- DiCuccio, M.H. The Relationship Between Patient Safety Culture and Patient Outcomes: A Systematic Review. J. Patient Saf. 2015, 11, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Fan, C.J.; Pawlik, T.M.; Daniels, T.; Vernon, N.; Banks, K.; Westby, P.; Wick, E.C.; Sexton, J.B.; Makary, M.A. Association of Safety Culture with Surgical Site Infection Outcomes. J. Am. Coll. Surg. 2016, 222, 122–128. [Google Scholar] [CrossRef]
- Mardon, R.E.; Khanna, K.; Sorra, J.; Dyer, N.; Famolaro, T. Exploring relationships between hospital patient safety culture and adverse events. J. Patient Saf. 2010, 6, 226–232. [Google Scholar] [CrossRef]
- Huang, D.T.; Clermont, G.; Kong, L.; Weissfeld, L.A.; Sexton, J.B.; Rowan, K.M.; Angus, D.C. Intensive care unit safety culture and outcomes: A US multicenter study. Int. J. Qual. Health Care 2010, 22, 151–161. [Google Scholar] [CrossRef]
- Hansen, L.O.; Williams, M.V.; Singer, S.J. Perceptions of hospital safety climate and incidence of readmission. Health Serv. Res. 2011, 46, 596–616. [Google Scholar] [CrossRef]
- Sexton, J.B.; Helmreich, R.L.; Neilands, T.B.; Rowan, K.; Vella, K.; Boyden, J.; Roberts, P.R.; Thomas, E.J. The Safety Attitudes Questionnaire: Psychometric properties, benchmarking data, and emerging research. BMC Health Serv. Res. 2006, 6, 44. [Google Scholar] [CrossRef]
- Lee, Y.C.; Zeng, P.S.; Huang, C.H.; Wu, H.H. Causal Relationship Analysis of the Patient Safety Culture Based on Safety Attitudes Questionnaire in Taiwan. J. Healthc. Eng. 2018, 2018, 4268781. [Google Scholar] [CrossRef]
- Chang, L.Y.; Yu, H.H.; Chao, Y.C. The Relationship Between Nursing Workload, Quality of Care, and Nursing Payment in Intensive Care Units. J. Nurs. Res. 2019, 27, 1–9. [Google Scholar] [CrossRef]
- Clancy, C.M. New research highlights the role of patient safety culture and safer care. J. Nurs. Care Qual. 2011, 26, 193–196. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.S.; Leu, F.Y.; Yang, C.W.; Lai, L.S. Healthcare-based on Cloud Electrocardiogram System: A Medical Center Experience in Middle Taiwan. J. Med Syst. 2018, 42, 39. [Google Scholar] [CrossRef] [PubMed]
- Liao, C.Y.; Wu, M.F.; Poon, S.K.; Liu, Y.M.; Chen, H.C.; Wu, C.L.; Sheu, W.H.; Liou, W.S. Improving medication safety by cloud technology: Progression and value-added applications in Taiwan. Int. J. Med Inform. 2019, 126, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.W.; Wang, C.Y.; Lai, Y.H.; Liao, Y.C.; Wen, Y.K.; Chang, S.T.; Huang, J.L.; Wu, T.J. Home-based cardiac rehabilitation improves quality of life, aerobic capacity, and readmission rates in patients with chronic heart failure. Medicine 2018, 97, e9629. [Google Scholar] [CrossRef]
- Chang, Y.Y.; Yu, H.H.; Loh el, W.; Chang, L.Y. The Efficacy of an In-Service Education Program Designed to Enhance the Effectiveness of Physical Restraints. J. Nurs. Res 2016, 24, 79–86. [Google Scholar] [CrossRef]
- Yu, B.; Wen, C.F.; Lo, H.L.; Liao, H.H.; Wang, P.C. Improvements in patient safety culture: A national Taiwanese survey, 2009–2016. Int. J. Qual. Health Care 2020. [Google Scholar] [CrossRef]
- Weaver, S.J.; Lubomksi, L.H.; Wilson, R.F.; Pfoh, E.R.; Martinez, K.A.; Dy, S.M. Promoting a culture of safety as a patient safety strategy: A systematic review. Ann. Intern. Med. 2013, 158 Pt 2, 369–374. [Google Scholar] [CrossRef]
- Wang, L.R.; Wang, Y.; Lou, Y.; Li, Y.; Zhang, X.G. The role of quality control circles in sustained improvement of medical quality. Springerplus 2013, 2, 141. [Google Scholar] [CrossRef][Green Version]
- Zhang, D.; Liao, M.; Zhou, Y.; Liu, T. Quality control circle: A tool for enhancing perceptions of patient safety culture among hospital staff in Chinese hospitals. Int. J. Qual. Health Care 2019. [Google Scholar] [CrossRef]
- Fujita, S.; Seto, K.; Ito, S.; Wu, Y.; Huang, C.C.; Hasegawa, T. The characteristics of patient safety culture in Japan, Taiwan and the United States. BMC Health Serv. Res. 2013, 13, 20. [Google Scholar] [CrossRef]
- Wagner, C.; Smits, M.; Sorra, J.; Huang, C.C. Assessing patient safety culture in hospitals across countries. Int. J. Qual. Health Care 2013, 25, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.C.; Li, H.H. Measuring patient safety culture in Taiwan using the Hospital Survey on Patient Safety Culture (HSOPSC). BMC Health Serv. Res. 2010, 10, 152. [Google Scholar] [CrossRef] [PubMed]
- Nie, Y.; Mao, X.; Cui, H.; He, S.; Li, J.; Zhang, M. Hospital survey on patient safety culture in China. BMC Health Serv. Res. 2013, 13, 228. [Google Scholar] [CrossRef] [PubMed]
- Noviyanti, L.W.; Handiyani, H.; Gayatri, D. Improving the implementation of patient safety by nursing students using nursing instructors trained in the use of quality circles. BMC Nurs. 2018, 17 (Suppl. 2), 53. [Google Scholar] [CrossRef]
- Leigh, B. Re: The use and impact of national confidential enquiries in high-income countries. BMJ Qual. Saf. 2011, 20, 38–45. [Google Scholar]
- Etchegaray, J.M.; Thomas, E.J. Comparing two safety culture surveys: Safety attitudes questionnaire and hospital survey on patient safety. BMJ Qual. Saf. 2012, 21, 490–498. [Google Scholar] [CrossRef]
- Zhang, Y.; Wu, J.; Fang, Z.; Zhang, Y.; Wong, F.K. Newly graduated nurses’ intention to leave in their first year of practice in Shanghai: A longitudinal study. Nurs. Outlook 2017, 65, 202–211. [Google Scholar] [CrossRef]
- Cheng, C.Y.; Tsai, H.M.; Chang, C.H.; Liou, S.R. New graduate nurses’ clinical competence, clinical stress, and intention to leave: A longitudinal study in Taiwan. Sci. World J. 2014, 2014, 748389. [Google Scholar] [CrossRef]
- Arian, M.; Soleimani, M.; Oghazian, M.B. Job satisfaction and the factors affecting satisfaction in nurse educators: A systematic review. J. Prof. Nurs. Off. J. Am. Assoc. Coll. Nurs. 2018, 34, 389–399. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).