How Could Peers in Online Health Community Help Improve Health Behavior
Abstract
1. Introduction
2. Theoretical Foundations
2.1. Theoretical Background
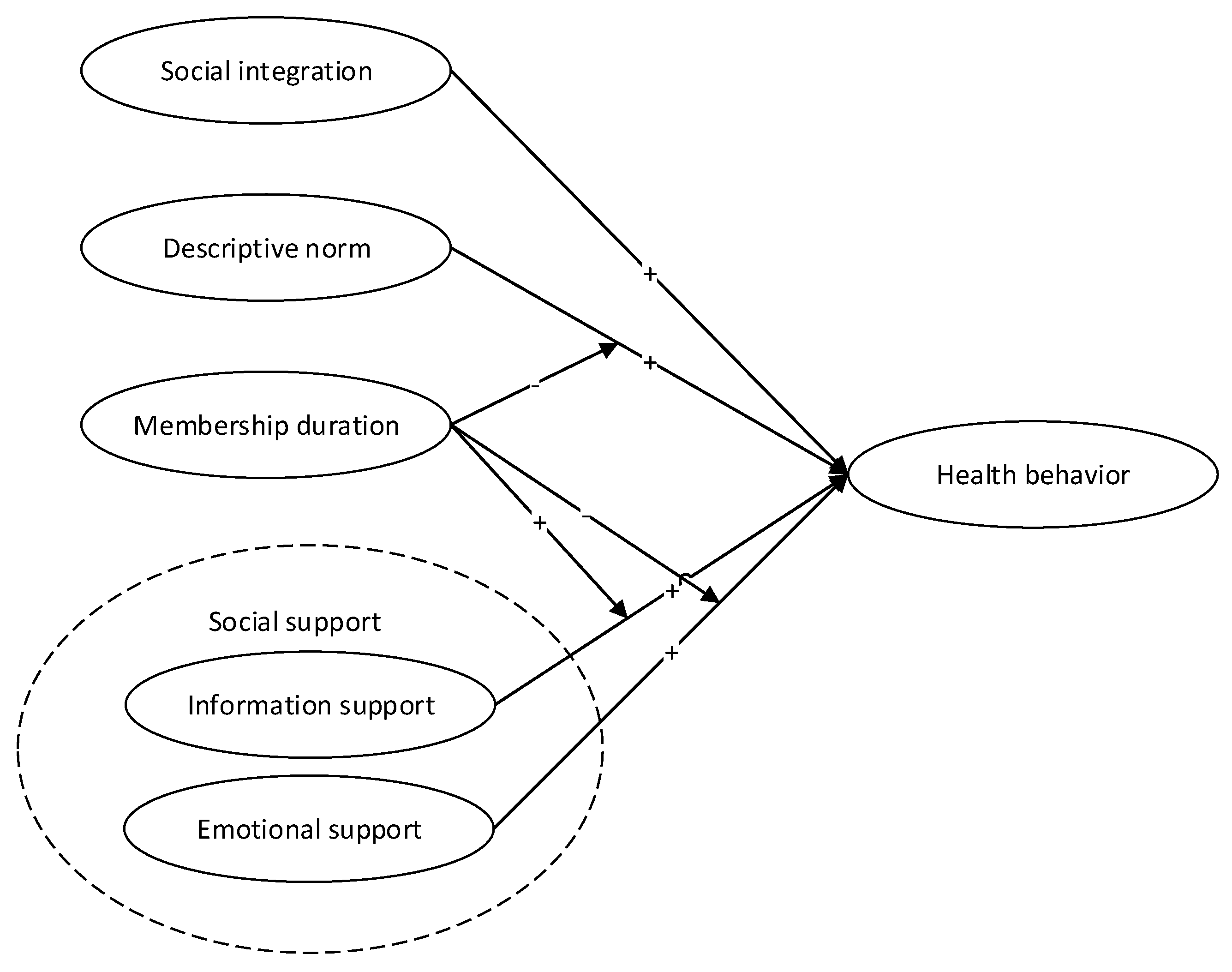
2.2. Hypotheses Development
3. Materials and Methods
3.1. Study Context
3.2. Dependent Variables
3.3. Independent Variables
3.4. Research Method
4. Results
4.1. Main Result
4.2. Online Social Relationships’ Effect on Health Behavior over Time
4.2.1. The Effect of Online Social Relationship Duration
4.2.2. Comparing the Importance of Online Social Relationships
4.2.3. The Effect of OHC Membership Duration
5. Discussion
5.1. Interpretation of Findings
5.2. Contribution and Implications
5.3. Limitations
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Informational support (a1) | Emotional support (a2) | Companionship (a3) | |
| seeking support (b1) | a1b1 | a2b1 | |
| providing support (b2) | a1b2 | a2b2 |
References
- Schroeder, S.A. We can do better—improving the health of the American people. N. Engl. J. Med. 2007, 357, 1221–1228. [Google Scholar] [CrossRef]
- Conner, M.; Norman, P. Predicting Health Behaviour: A Social Cognition Approach. In Predicting Health Behaviour; McGraw-Hill Education: New York, NY, USA, 2005; pp. 1–27. [Google Scholar]
- Chronic Diseases and Health Promotion. Available online: https://www.cdc.gov/chronicdisease/about/ (accessed on 26 August 2019).
- Heaney, C.A.; Israel, B.A. Social networks and social support. In Health Behavior and Health Education: Theory, Research, and Practice, 4th ed.; Jossey-Bass: San Francisco, CA, USA, 2008; pp. 189–209. [Google Scholar]
- Sallis, J.F.; Owen, N.; Fisher, E.B. Ecological models of health behavior. In Health Behavior and Health Education: Theory, Research, and Practice; John Wiley & Sons: Hoboken, NJ, USA, 2008; Volume 4, pp. 465–486. [Google Scholar]
- Emmons, K.M. Health behaviors in a social context. Soc. Epidemiol. 2000, 242–266. [Google Scholar]
- Jordan, B. Blurring boundaries: The “real” and the “virtual” in hybrid spaces. Hum. Organ. 2009, 68, 181–193. [Google Scholar] [CrossRef]
- Bos, L.; Marsh, A.; Carroll, D.; Gupta, S.; Rees, M. Patient 2.0 Empowerment. In Proceedings of the International Conference on Semantic Web & Web Services, Las Vegas, NV, USA, 14–17 July 2008; CSREA Press: Las Vegas, NV, USA, 2008; pp. 164–168. [Google Scholar]
- Mattila, E.; Korhonen, I.; Salminen, J.H.; Ahtinen, A.; Koskinen, E.; Sarela, A.; Parkka, J.; Lappalainen, R. Empowering citizens for well-being and chronic disease management with wellness diary. Inf. Technol. Biomed. IEEE Trans. 2010, 14, 456–463. [Google Scholar] [CrossRef] [PubMed]
- Swan, M. Emerging patient-driven health care models: An examination of health social networks, consumer personalized medicine and quantified self-tracking. Int. J. Environ. Res. Public Health 2009, 6, 492–525. [Google Scholar] [CrossRef] [PubMed]
- Gimpel, H.; Nißen, M.; Görlitz, R. Quantifying the Quantified Self: A Study on the Motivations of Patients to Track Their Own Health. In Proceedings of the 34th International Conference on Information Systems (ICIS), Milan, Italy, 17 December 2013. [Google Scholar]
- Overberg, R.; Otten, W.; de Man, A.; Toussaint, P.; Westenbrink, J.; Zwetsloot-Schonk, B. How breast cancer patients want to search for and retrieve information from stories of other patients on the internet: An online randomized controlled experiment. J. Med. Internet Res. 2010, 12. [Google Scholar] [CrossRef] [PubMed]
- Shiue, Y.-C.; Chiu, C.-M.; Chang, C.-C. Exploring and mitigating social loafing in online communities. Comput. Hum. Behav. 2010, 26, 768–777. [Google Scholar] [CrossRef]
- Berge, J.M.; MacLehose, R.F.; Meyer, C.; Didericksen, K.; Loth, K.A.; Neumark-Sztainer, D. He Said, She Said: Examining Parental Concordance on Home Environment Factors and Adolescent Health Behaviors and Weight Status. J. Acad. Nutr. Diet. 2016, 116, 46–60. [Google Scholar] [CrossRef]
- Watt, R.G.; Heilmann, A.; Sabbah, W.; Newton, T.; Chandola, T.; Aida, J.; Sheiham, A.; Marmot, M.; Kawachi, I.; Tsakos, G. Social relationships and health related behaviors among older US adults. BMC Public Health 2014, 14, 533. [Google Scholar] [CrossRef]
- Ball, L.; Leveritt, M.; Cass, S.; Chaboyer, W. Effect of nutrition care provided by primary health professionals on adults’ dietary behaviours: A systematic review. Fam. Pract. 2015, 32, 605. [Google Scholar] [CrossRef]
- Brewer, G.; Robinson, S.; Sumra, A.; Tatsi, E.; Gire, N. The Influence of Religious Coping and Religious Social Support on Health Behaviour, Health Status and Health Attitudes in a British Christian Sample. J. Relig. Health 2014, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.W.; Lu, C.C.; Yang, Y.H.; Huang, C.L. Smoking behaviours of adolescents, influenced by smoking of teachers, family and friends. Int. Nurs. Rev. 2014, 61, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Aliyas, Z. Social Capital and Physical Activity Level in an Urban Adult Population. Am. J. Health Educ. 2020, 51, 40–49. [Google Scholar] [CrossRef]
- Yun, L.R.; Vanderloo, L.; Berry, T.R.; Latimer-Cheung, A.E.; O’Reilly, N.; Rhodes, R.E.; Spence, J.C.; Tremblay, M.S.; Faulkner, G. Assessing the social climate of physical (in)activity in Canada. BMC Public Health 2018, 18. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.A.; Lewis, L.K.; Ferrar, K.; Marshall, S.; De Bourdeaudhuij, I.; Vandelanotte, C. Are health behavior change interventions that use online social networks effective? A systematic review. J. Med. Internet Res. 2014, 16. [Google Scholar] [CrossRef]
- De la Pena, A.; Quintanilla, C. Share, like and achieve: The power of Facebook to reach health-related goals. Int. J. Consum. Stud. 2015, 39, 495–505. [Google Scholar] [CrossRef]
- Walker, M.; Thornton, L.; De Choudhury, M.; Teevan, J.; Bulik, C.M.; Levinson, C.A.; Zerwas, S. Facebook use and disordered eating in college-aged women. J. Adolesc. Health 2015, 57, 157–163. [Google Scholar] [CrossRef]
- Mhasawade, V.; Elghafari, A.; Duncan, D.T.; Chunara, R. Role of the Built and Online Social Environments on Expression of Dining on Instagram. Int. J. Environ. Res. Public Health 2020, 17, 735. [Google Scholar] [CrossRef]
- Merchant, G.; Weibel, N.; Patrick, K.; Fowler, J.H.; Norman, G.J.; Gupta, A.; Servetas, C.; Calfas, K.; Raste, K.; Pina, L. Click “like” to change your behavior: A mixed methods study of college students’ exposure to and engagement with Facebook content designed for weight loss. J. Med. Internet Res. 2014, 16. [Google Scholar] [CrossRef]
- Wang, C.K.J.; Leng, H.K.; Kee, Y.H. Use of Facebook in physical activity intervention programme A test of self-determination theory. Int. J. Sport Psychol. 2015, 46, 210–224. [Google Scholar]
- Bambina, A. Online Social Support: The Interplay of Social Networks and Computer-Mediated Communication; Cambria Press: Amherst, NY, USA, 2007. [Google Scholar]
- Deci, E.L.; Ryan, R.M. The “what” and “why” of goal pursuits: Human needs and the self-determination of behavior. Psychol. Inq. 2000, 11, 227–268. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68. [Google Scholar] [CrossRef] [PubMed]
- Shumaker, S.A.; Brownell, A. Toward a theory of social support: Closing conceptual gaps. J. Soc. Issues 1984, 40, 11–36. [Google Scholar] [CrossRef]
- Yan, L.; Tan, Y. Feel blue so go online: An empirical study of online social support among patients. Inf. Syst. Res. 2014, 25, 690–709. [Google Scholar] [CrossRef]
- Umberson, D.; Montez, J.K. Social relationships and health a flashpoint for health policy. J. Health Soc. Behav. 2010, 51 (Suppl. 1), S54–S66. [Google Scholar] [CrossRef]
- Michael, Y.L.; Colditz, G.A.; Coakley, E.; Kawachi, I. Health behaviors, social networks, and healthy aging: Cross-sectional evidence from the Nurses’ Health Study. Qual. Life Res. 1999, 8, 711–722. [Google Scholar] [CrossRef]
- Cowan, N. Working Memory Capacity; Psychology Press: London, UK, 2012. [Google Scholar]
- Dunbar, R. How Many Friends Does One Person Need?: Dunbar’S Number and Other Evolutionary Quirks; Faber & Faber: London, UK, 2010. [Google Scholar]
- Staunton, M.; Louis, W.R.; Smith, J.R.; Terry, D.J.; McDonald, R.I. How negative descriptive norms for healthy eating undermine the effects of positive injunctive norms. J. Appl. Soc. Psychol. 2014, 44, 319–330. [Google Scholar] [CrossRef]
- Rivis, A.; Sheeran, P. Descriptive norms as an additional predictor in the theory of planned behaviour: A meta-analysis. Curr. Psychol. 2003, 22, 218–233. [Google Scholar] [CrossRef]
- Banerjee, A.V. A simple model of herd behavior. Q. J. Econ. 1992, 797–817. [Google Scholar] [CrossRef]
- Bandura, A. Social cognitive theory. In Handbook of Social Psychological Theories; Sage: London, UK, 2011; pp. 349–373. [Google Scholar]
- Berkman, L.F.; Glass, T.; Brissette, I.; Seeman, T.E. From social integration to health: Durkheim in the new millennium. Soc. Sci. Med. 2000, 51, 843–857. [Google Scholar]
- Cobb, N.K.; Graham, A.L.; Abrams, D.B. Social network structure of a large online community for smoking cessation. Am. J. Public Health 2010, 100, 1282–1289. [Google Scholar] [CrossRef] [PubMed]
- Thompson, H.S.; Littles, M.; Jacob, S.; Coker, C. Posttreatment breast cancer surveillance and follow-up care experiences of breast cancer survivors of African descent: An exploratory qualitative study. Cancer Nurs. 2006, 29, 478–487. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Health promotion by social cognitive means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar]
- Reblin, M.; Uchino, B.N. Social and emotional support and its implication for health. Curr. Opin. Psychiatry 2008, 21, 201. [Google Scholar] [CrossRef] [PubMed]
- Wellman, B.; Wortley, S. Different strokes from different folks: Community ties and social support. Am. J. Sociol. 1990, 96, 558. [Google Scholar] [CrossRef]
- Powell, G.B.; Almond, G. Comparative Politics: A Developmental Approach; Little, Brown and Co.: Boston, MA, USA, 1966. [Google Scholar]
- Sjöström, L.; Narbro, K.; Sjöström, C.D.; Karason, K.; Larsson, B.; Wedel, H.; Lystig, T.; Sullivan, M.; Bouchard, C.; Carlsson, B. Effects of bariatric surgery on mortality in Swedish obese subjects. N. Engl. J. Med. 2007, 357, 741–752. [Google Scholar] [CrossRef]
- Group, L.A.R. Long term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes: Four year results of the Look AHEAD trial. Arch. Intern. Med. 2010, 170, 1566. [Google Scholar]
- Hall, K.D.; Sacks, G.; Chandramohan, D.; Chow, C.C.; Wang, Y.C.; Gortmaker, S.L.; Swinburn, B.A. Quantification of the effect of energy imbalance on bodyweight. Lancet 2011, 378, 826–837. [Google Scholar] [CrossRef]
- Burke, L.E.; Wang, J.; Sevick, M.A. Self-monitoring in weight loss: A systematic review of the literature. J. Am. Diet. Assoc. 2011, 111, 92–102. [Google Scholar] [CrossRef]
- Carels, R.A.; Darby, L.A.; Rydin, S.; Douglass, O.M.; Cacciapaglia, H.M.; O’Brien, W.H. The relationship between self-monitoring, outcome expectancies, difficulties with eating and exercise, and physical activity and weight loss treatment outcomes. Ann. Behav. Med. 2005, 30, 182–190. [Google Scholar] [CrossRef]
- Kanfer, F.H.; Gaelick-Buys, L. Self-management methods. In Helping People Change: A Textbook of Methods (4th ed.); Goldstein, F.H.K.A.P., Ed.; Pergamon Press: Elmsford, NY, USA, 1991; pp. 305–360. [Google Scholar]
- Welsh, E.M.; Sherwood, N.E.; VanWormer, J.J.; Hotop, A.M.; Jeffery, R.W. Is frequent self-weighing associated with poorer body satisfaction? Findings from a phone-based weight loss trial. J. Nutr. Educ. Behav. 2009, 41, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Foster, G.D.; Makris, A.P.; Bailer, B.A. Behavioral treatment of obesity. Am. J. Clin. Nutr. 2005, 82, 230S–235S. [Google Scholar] [CrossRef] [PubMed]
- Pang, B.; Lee, L. Seeing stars: Exploiting class relationships for sentiment categorization with respect to rating scales. In Proceedings of the 43rd Annual Meeting on Association for Computational Linguistics, Ann Arbor, MI, USA, 25–30 June 2005; Association for Computational Linguistics: Stroudsburg, PA, USA, 2005; pp. 115–124. [Google Scholar]
- Lee, Y.J.; Hosanagar, K.; Tan, Y. Do I Follow My Friends or the Crowd? Information Cascades in Online Movie Ratings. Manag. Sci. 2015, 61, 2241–2258. [Google Scholar] [CrossRef]
- Tutz, G.; Hennevogl, W. Random effects in ordinal regression models. Comput. Stat. Data Anal. 1996, 22, 537–557. [Google Scholar]
- Jabr, W.; Mookerjee, R.; Tan, Y.; Mookerjee, V.S. Leveraging philanthropic behavior for customer support: The case of user support forums. MIS Q. 2014, 38, 187–208. [Google Scholar] [CrossRef]
- Cheung, R.; Vogel, D. Predicting user acceptance of collaborative technologies: An extension of the technology acceptance model for e-learning. Comput. Educ. 2013, 63, 160–175. [Google Scholar]
| Frequency | Diet Behavior | Exercise Behavior | ||
|---|---|---|---|---|
| Number | Percentage | Number | Percentage | |
| 0 | 165,534 | 84.14% | 179,097 | 91.04% |
| 1 | 7348 | 3.74% | 4562 | 2.32% |
| 2 | 3833 | 1.95% | 2322 | 1.18% |
| 3 | 2969 | 1.51% | 1762 | 0.90% |
| 4 | 2799 | 1.42% | 1640 | 0.83% |
| 5 | 2904 | 1.48% | 1418 | 0.72% |
| 6 | 2443 | 1.24% | 1138 | 0.58% |
| 7 | 8898 | 4.52% | 4789 | 2.43% |
| Total | 196,728 | 100% | 196,728 | 100% |
| Model Variable | Measurement | Description | Mean | Min | Max | Std. Dev. |
|---|---|---|---|---|---|---|
| Behavior | DietNum | Number of diet diaries at week t | 0.643 | 0 | 7 | 1.760 |
| ExerNum | Number of exercise diaries at week t | 0.348 | 0 | 7 | 1.321 | |
| Social integration | FNum | Number of friends at week t-1 | 1.690 | 0 | 437 | 6.223 |
| Fnum3M | Number of friendships established for no more than three months at week t-1 | 1.586 | 0 | 136 | 5.651 | |
| SpNum | Number of support groups at week t-1 | 0.827 | 0 | 21 | 1.528 | |
| SpNum3M | Number of support groups, no more than three months at week t-1 | 0.126 | 0 | 17 | 0.550 | |
| ChalNum | Number of challenges group at week t-1 | 0.122 | 0 | 35 | 0.522 | |
| Social norm | FDietNum | Average diet diary number of friends at week t-1 | 1.008 | 0 | 190 | 5.372 |
| FDietNum3M | Average diet diary number of no more than three months friends at week t-1 | 0.994 | 0 | 145 | 3.409 | |
| FExerNum | Average exercise diary number of no more than three months friends at week t-1 | 0.563 | 0 | 117 | 3.362 | |
| FExerNum3M | Average exercise diary number of friends at week t-1 | 0.725 | 0 | 92 | 2.775 | |
| SpDietNum | Average diet diary number of group at week t-1 | 283.742 | 0 | 8429 | 529.665 | |
| SpDietNum3M | Average diet diary number of group participating for no more than three months at week t-1 | 44.825 | 0 | 5392 | 205.432 | |
| SpExerNum | Average exercise diary number of support group at week t-1 | 160.721 | 0 | 5197 | 305.888 | |
| SpExerNum3M | Average exercise diary number of support group participating for no more than three months at week t-1 | 25.505 | 0 | 3443 | 118.537 | |
| ChalDietNum | Diet diary number of challenge members at week t-1 | 18.153 | 0 | 3392 | 90.630 | |
| ChalExerNum | Average exercise diary number of challenge members at week t-1 | 11.430 | 0 | 2238 | 57.849 | |
| Social support | CompSp | Companionship support at week t-1 | 0.002 | 0 | 11.54 | 0.059 |
| EmotSp | Emotional Support at week t-1 | 0.009 | 0 | 34.847 | 0.172 | |
| InfoSp | Informational Support at week t-1 | 0.012 | 0 | 50.217 | 0.297 | |
| Member | InitWeight | The last weight input before 2011.1.2 | 90.578 | 100 | 244.9 | 23.507 |
| ExpLossRatio | Expectation loss ratio a | 19.164 | 0.088 | 67 | 11.287 | |
| Membership | Months since participated OHC until week t | 12.545 | 0.267 | 62.233 | 9.769 | |
| DietChangeTs | Number of diet changes until week t | 1.159 | 1 | 7 | 0.466 |
| Variables | Diet | Exercise | ||
|---|---|---|---|---|
| Estimate | Standard Error | Estimate | Standard Error | |
| γ1 FNum | −0.0207 ** | (0.0072) | −0.0248 *** | (0.0076) |
| γ2 SpNum | 0.0489 | (0.0352) | −0.0231 | (0.0404) |
| γ3 ChalNum | 0.2490 *** | (0.0258) | 0.1517 *** | (0.0305) |
| γ4 Fnum2 | 0.0001 * | (0.0000) | 0.0001 ** | (0.0000) |
| γ5 SpNum2 | −0.0098 *** | (0.0027) | −0.0063 * | (0.0031) |
| γ6 ChalNum2 | −0.0090 *** | (0.0011) | −0.0062 *** | (0.0011) |
| δ1 FDietNum(FExerNum) | 0.0520 *** | (0.0029) | 0.0571 *** | (0.0042) |
| δ2 SpDietNum(SpExerNum) | 0.0000 | (0.0001) | 0.0003 *** | (0.0001) |
| δ3 ChalDietNum(ChalExerNum) | 0.0014 *** | (0.0001) | 0.0027 *** | (0.0002) |
| β1 InfoSp | 0.2113 *** | (0.0442) | 0.1390 *** | (0.0402) |
| β2 EmotSp | 0.5968 *** | (0.0589) | 0.4627 *** | (0.0557) |
| β3 CompSp | 0.2637 | (0.1465) | −0.0428 | (0.1425) |
| α1 InitWeight | 0.0088 *** | (0.0020) | 0.0042 *** | (0.0022) |
| α2 ExpLossRatio | −0.0052 *** | (0.0001) | −0.0052 *** | (0.0001) |
| α3 Membership | −0.1564 *** | (0.0027) | −0.1573 *** | (0.0034) |
| α4 DietChangeTs | 0.8366 *** | (0.0515) | 0.7360 *** | (0.0635) |
| Number of obs | 196,728 | 196,728 | ||
| VIF | 2.56 | 2.46 | ||
| Log likelihood | −104906.87 | −65733.06 | ||
| Variables | Diet | Exercise | ||||||
|---|---|---|---|---|---|---|---|---|
| Model 2 | Model 3 | Model 2 | Model 3 | |||||
| Estimate | Standard Error | Estimate | Standard Error | Estimate | Standard Error | Estimate | Standard Error | |
| γ1 FNum3M | 0.0694 *** | (0.0161) | 0.0547 *** | (0.0169) | 0.0461 ** | (0.0166) | 0.0465 * | (0.0190) |
| γ2 SpNum3M | 0.2012 *** | (0.034) | 0.1662 *** | (0.0398) | 0.1563 *** | (0.0424) | 0.0757 | (0.0463) |
| γ3 ChalNum | 0.2154 *** | (0.0258) | 0.1415 *** | (0.0359) | 0.1129 *** | (0.0305) | 0.0788 | (0.0411) |
| γ4 Fnum2 | −0.0007 ** | (0.0002) | −0.0006 *** | (0.0002) | −0.0006 ** | (0.0002) | −0.0005* | (0.0002) |
| γ5 SpNum2 | −0.0283 *** | (0.0038) | −0.0251 *** | (0.0037) | −0.0354 *** | (0.0057) | −0.0345 *** | (0.0061) |
| γ6 ChalNum2 | −0.0091 *** | (0.0011) | −0.0086 *** | (0.0012) | −0.0059 *** | (0.0011) | −0.0058 *** | (0.0012) |
| δ1 FdietNum3M(FexerNum3M) | 0.0719 *** | (0.0145) | 0.1503 *** | (0.017) | 0.1120 *** | (0.0209) | 0.1660 *** | (0.0253) |
| δ2SpDietNum3M(SpExerNum3M) | 0.0006 *** | (0.0001) | 0.0009 *** | (0.0001) | 0.0013 *** | (0.0001) | 0.0019 *** | (0.0002) |
| δ3 ChalDietNum (ChalExerNum) | 0.0014 *** | (0.0001) | 0.0018 *** | (0.0001) | 0.0027 *** | (0.0002) | 0.0031 *** | (0.0003) |
| β1 InfoSp | 0.2013 *** | (0.0431) | 0.1287 * | (0.0537) | 0.1277 *** | (0.0391) | 0.0626 | (0.0461) |
| β2 EmotSp | 0.6515 *** | (0.0577) | 0.6921 *** | (0.0772) | 0.5141 *** | (0.0537) | 0.7390 *** | (0.0750) |
| β3 CompSp | 0.3533 *** | (0.1374) | 0.1177 | (0.2022) | −0.0147 *** | (0.1405) | −0.2047 | (0.1927) |
| γ7 FNum*Membership | 0.0010 ** | (0.0004) | −0.0001 | (0.0006) | ||||
| γ8 SpNum*Membership | 0.0067 * | (0.0032) | 0.0157 *** | (0.0037) | ||||
| γ9 ChalNum*Membership | 0.0103 *** | (0.003) | 0.0057 | (0.0035) | ||||
| δ4 FDietNum(FExerNum) * Membership | −0.0069 *** | (0.0007) | −0.0048 *** | (0.0011) | ||||
| δ5 SpDietNum(SpExerNum) * Membership | −0.0001 *** | (0) | −0.0001 *** | (0) | ||||
| δ6 ChalDietNum(ChalExerNum) * Membership | −0.0001 *** | (0) | −0.0001 ** | (0) | ||||
| β4 InfoSp*Membership | 0.0101 * | (0.0048) | 0.0098 * | (0.0047) | ||||
| β5 EmotSp*Membership | −0.0082 | (0.0068) | −0.0342 *** | (0.0072) | ||||
| β6 CompSp*Membership | 0.0275 | (0.0176) | 0.0304 | (0.017) | ||||
| α1 InitWeight | 0.0090 *** | (0.0020) | 0.0090 *** | (0.0020) | 0.0042 | (0.0022) | 0.0042 | (0.0022) |
| α2 ExpLossRatio | −0.0052 *** | (0.0001) | −0.0049 *** | (0.0001) | −0.0053 *** | (0.0001) | −0.0051 *** | (0.0001) |
| α3 Membership | −0.1557 *** | (0.0001) | −0.1481 *** | (0.0027) | −0.1597 *** | (0.0032) | −0.1533 *** | (0.0034) |
| α4 DietChangeTs | 0.7942 *** | (0.0510) | 0.8147 *** | (0.0511) | 0.6758 *** | (0.0630) | 0.6932 *** | (0.0633) |
| Number of obs | 196,728 | 196,728 | 196,728 | 196,728 | ||||
| VIF | 2.63 | 4.13 | 2.54 | 4.10 | ||||
| Log likelihood | −104852.52 | −104761.22 | −65675.016 | −65620.46 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Yan, X. How Could Peers in Online Health Community Help Improve Health Behavior. Int. J. Environ. Res. Public Health 2020, 17, 2995. https://doi.org/10.3390/ijerph17092995
Li Y, Yan X. How Could Peers in Online Health Community Help Improve Health Behavior. International Journal of Environmental Research and Public Health. 2020; 17(9):2995. https://doi.org/10.3390/ijerph17092995
Chicago/Turabian StyleLi, Yumei, and Xiangbin Yan. 2020. "How Could Peers in Online Health Community Help Improve Health Behavior" International Journal of Environmental Research and Public Health 17, no. 9: 2995. https://doi.org/10.3390/ijerph17092995
APA StyleLi, Y., & Yan, X. (2020). How Could Peers in Online Health Community Help Improve Health Behavior. International Journal of Environmental Research and Public Health, 17(9), 2995. https://doi.org/10.3390/ijerph17092995




