Scalable Screening and Treatment Response Monitoring for Perinatal Depression in Low- and Middle-Income Countries
Abstract
:1. Background
- (a)
- Propose a two-phased process for perinatal depression identification and screening, integrated into the primary health care system in rural Pakistan.
- (b)
- Propose a short tool for measuring the response to treatment for perinatal depression.
- (c)
- Report psychometric data on three short tools, including the model fit and accuracy: The Community Informant Detection Tool (CIDT) for identification of high-risk women, the 4-item Patient Health Questionnaire (PHQ-4) for screening for perinatal depression, and the 4-item Hamilton Depression Rating Scale (HAMD-4) for measuring responses to treatment.
2. Methods
2.1. Approach
2.2. Settings and Overall Study Design
2.2.1. Phase 1: Identification of Women at High Risk of Perinatal Depression
2.2.2. Phase 2: Screening of High-Risk Women for Perinatal Depression
2.2.3. Phase 3: Measuring Treatment-Response
3. Statistical Analyses
4. Results
4.1. Phase 1: Community Assessment with the Community Informant Detection Tool
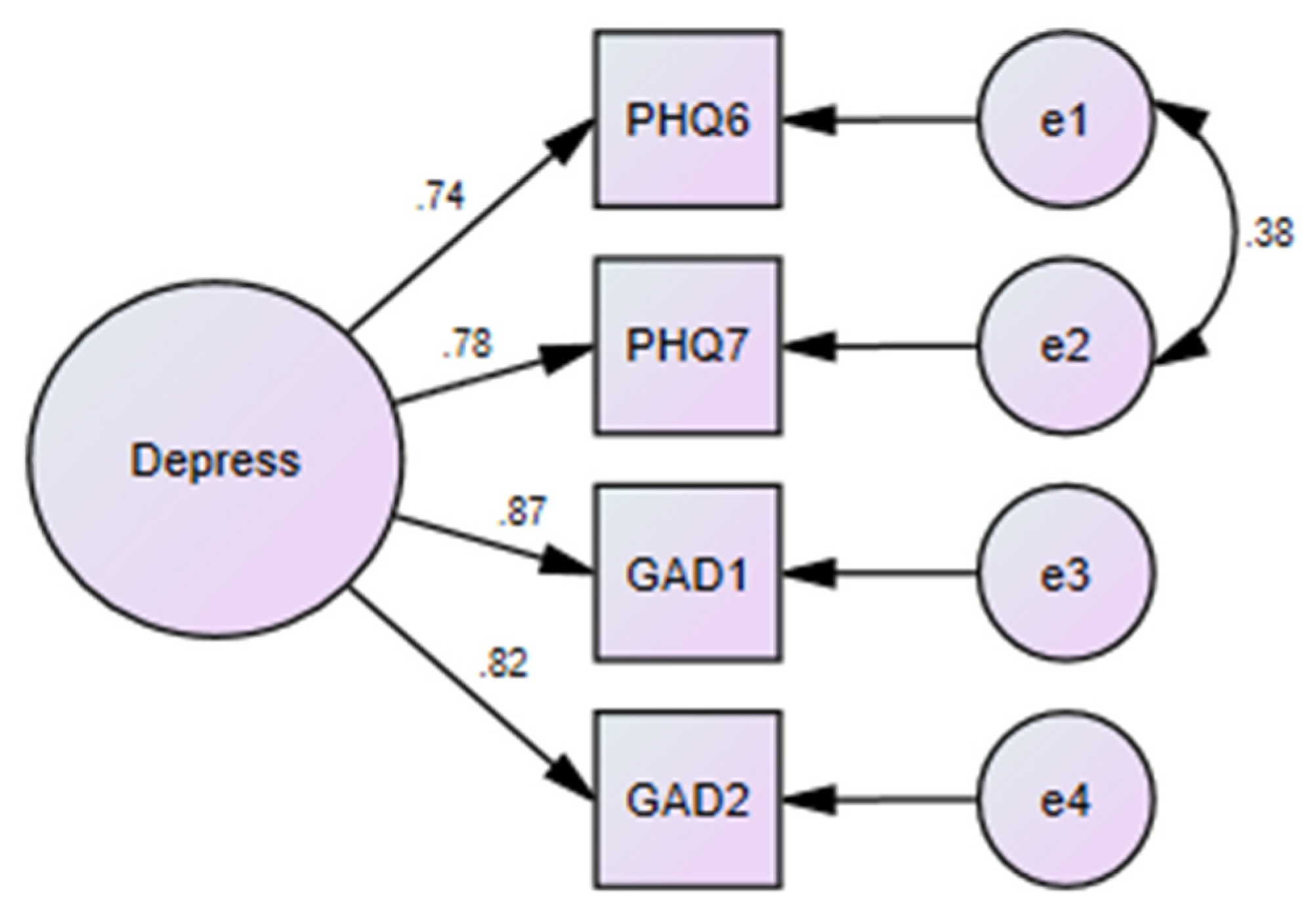
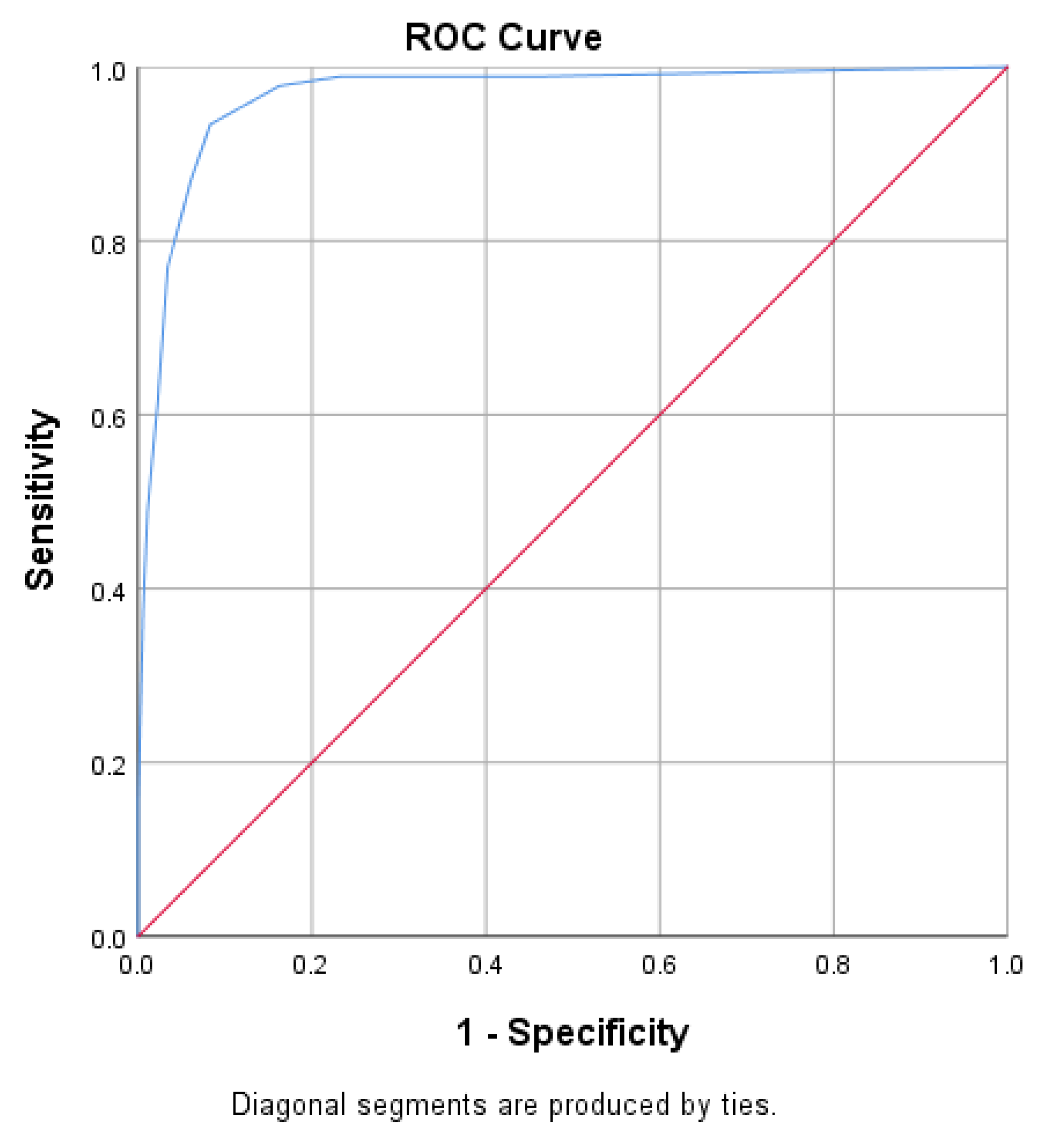
4.2. Phase 2: Formal Screening with the Patient Health Questionnaire-4 Items
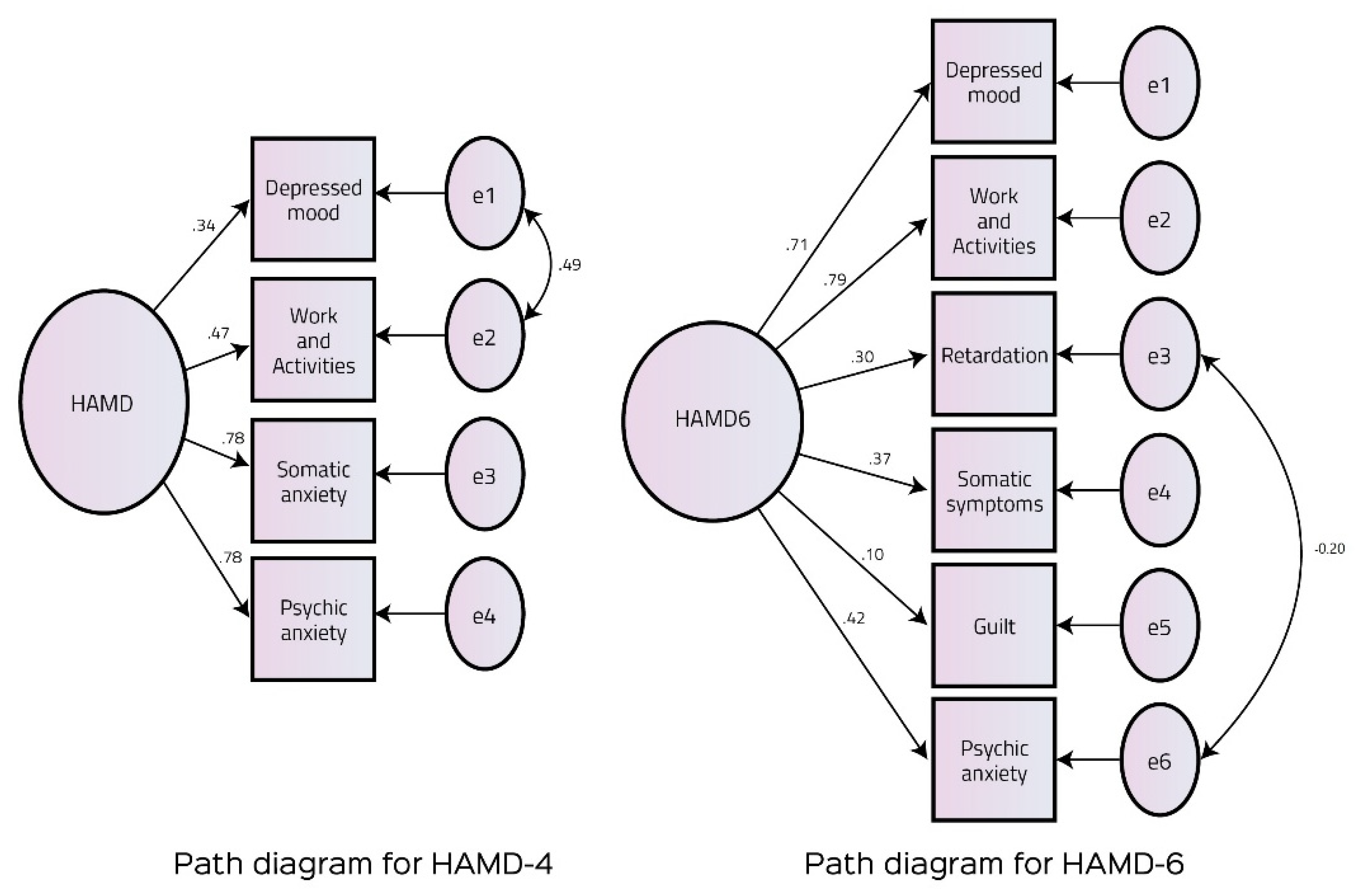
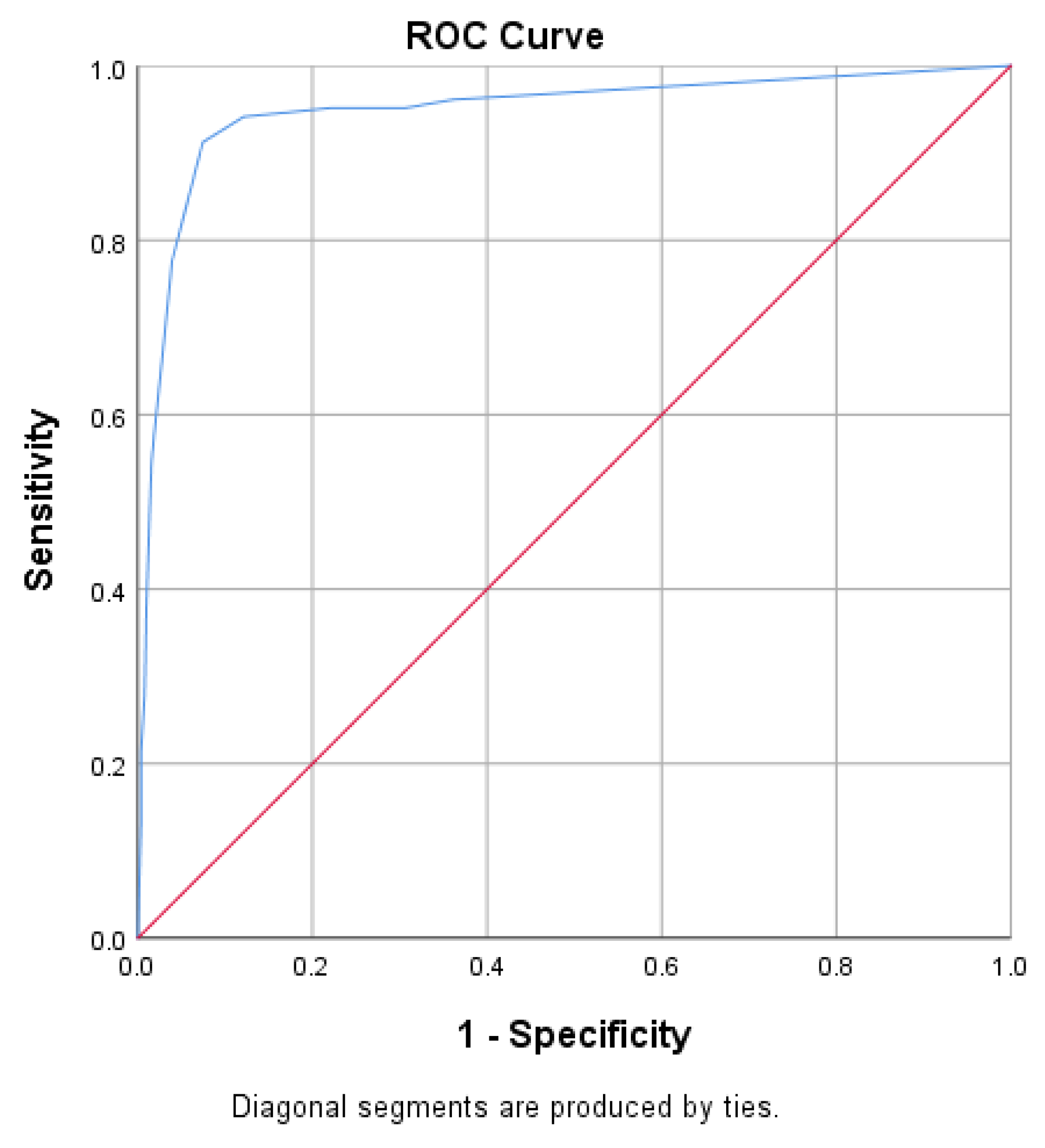
4.3. Phase 3: Measuring Intervention Response with the Hamilton Depression Rating Scale–4 Items
5. Discussion
5.1. Summary
5.2. The Need for Short Scales for Assessing Perinatal Depression
5.3. Comparisons with Previous Literature
5.4. Limitations of Our Work
6. Strengths and Implications for Future Research
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Atif, M.; Halaki, M.; Raynes-Greenow, C.; Chow, C.M. Perinatal depression in Pakistan: A systematic review and meta-analysis. Birth 2021, 48, 149–163. [Google Scholar]
- Slomian, J.; Honvo, G.; Emonts, P.; Reginster, J.Y.; Bruyère, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women’s Health 2019, 15. [Google Scholar] [CrossRef]
- Waqas, A.; Elhady, M.; Dila, K.S.; Kaboub, F.; Nhien, C.H.; Al-Husseini, M.J.; Kamel, M.G.; Elshafay, A.; Nhi, H.Y.; Hirayama, K.; et al. Association between maternal depression and risk of infant diarrhea: A systematic review and meta-analysis. Public Health 2018, 159, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Gelaye, B.; Rondon, M.B.; Araya, R.; Williams, M.A. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry 2016, 3, 973–982. [Google Scholar] [CrossRef]
- Spinhoven, P.; Kooiman, C.G. Defense Style in Depressed and Anxious Psychiatric Outpatients: An Explorative Study. J. Nerv. Ment. Dis. 1997, 185, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Bauer, A.; Parsonage, M.; Knapp, M.; Iemmi, V.; Adelaja, B.; Hogg, S. The Costs of Perinatal Mental Health Problems; London School of Economics and Political Science: London, UK, 2014. [Google Scholar]
- Rahman, A.; Lovel, H.; Bunn, J.; Iqbal, Z.; Harrington, R. Mothers’ mental health and infant growth: A case-control study from Rawalpindi, Pakistan. Child Care Health Dev. 2004, 30, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Iqbal, Z.; Bunn, J.; Lovel, H.; Harrington, R. Impact of maternal depression on infant nutritional status and illness: A cohort study. Arch. Gen. Psychiatry 2004, 61, 946–952. [Google Scholar] [CrossRef]
- Mirza, Z.; Rahman, A. Mental health care in Pakistan boosted by the highest office. The Lancet 2019, 394, 2239–2240. [Google Scholar] [CrossRef]
- Rahman, A.; Malik, A.; Sikander, S.; Roberts, C.; Creed, F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: A cluster-randomised controlled trial. The Lancet 2008, 372, 902–909. [Google Scholar] [CrossRef]
- Ishihara, M.; Harel, D.; Levis, B.; Levis, A.W.; Riehm, K.E.; Saadat, N.; Azar, M.; Rice, D.B.; Sanchez, T.A.; Chiovitti, M.J.; et al. Shortening self-report mental health symptom measures through optimal test assembly methods: Development and validation of the Patient Health Questionnaire-Depression-4. Depress. Anxiety 2019, 36, 82–92. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Mumford, D.B.; Tareen, I.A.K.; Bajwa, M.A.Z.; Bhatti, M.R.; Karim, R. The translation and evaluation of an Urdu version of the Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1991, 83, 81–85. [Google Scholar] [CrossRef]
- Waqas, A.; Raza, N.; Lodhi, H.W.; Muhammad, Z.; Jamal, M.; Rehman, A. Psychosocial factors of antenatal anxiety and depression in Pakistan: Is social support a mediator? PLoS ONE 2015, 10, e0116510. [Google Scholar] [CrossRef] [PubMed]
- Waqas, A.; Aedma, K.K.; Tariq, M.; Meraj, H.; Naveed, S. Validity and reliability of the Urdu version of the Hospital Anxiety & Depression Scale for assessing antenatal anxiety and depression in Pakistan. Asian J. Psychiatr. 2019, 45, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Thombs, B.D.; Levis, B.; Lyubenova, A.; Neupane, D.; Negeri, Z.; Wu, Y.; Sun, Y.; He, C.; Krishnan, A.; Vigod, S.N.; et al. Overestimation of Postpartum depression prevalence based on a 5-item version of the EPDS: Systematic review and individual particiapnt data meta-analysis. Can. J. Psychiatry 2020, 65, 835–844. [Google Scholar] [CrossRef]
- Morrell, C.J.; Warner, R.; Slade, P.; Dixon, S.; Walters, S.; Paley, G.; Brugha, T. Psychological interventions for postnatal depression: Cluster randomised trial and economic evaluation. The PoNDER trial. Health Technol. Assess 2009, 13. [Google Scholar] [CrossRef] [PubMed]
- Jordans, M.J.; Luitel, N.P.; Kohrt, B.A.; Rathod, S.D.; Garman, E.C.; De Silva, M.; Komproe, I.H.; Patel, V.; Lund, C. Community-, facility-, and individual-level outcomes of a district mental healthcare plan in a low-resource setting in Nepal: A population-based evaluation. PLoS Med. 2019, 16, 1–20. [Google Scholar] [CrossRef] [PubMed]
- National Collaborating Center for Mental Health. National Clinical Guideline Number 192: Antenatal and Postnatal Mental Health Clinical Management and Service Guidance Updated Edition. 2020. Available online: https://www.nice.org.uk/guidance/cg192/evidence/full-guideline-pdf-193396861 (accessed on 20 June 2021).
- Naveed, S.; Waqas, A.; Memon, A.R.; Jabeen, M.; Sheikh, M.H. Cross-cultural validation of the Urdu translation of the Patient Health Questionnaire for Adolescents among children and adolescents at a Pakistani school. Public Health 2019, 168, 59–66. [Google Scholar] [CrossRef]
- Sikander, S.; Ahmad, I.; Bates, L.M.; Gallis, J.; Hagaman, A.; O’Donnell, K.; Turner, E.L.; Zaidi, A.; Rahman, A.; Maselko, J. Cohort profile: Perinatal depression and child socioemotional development; The bachpan cohort study from rural Pakistan. BMJ Open 2019, 9, e025644. [Google Scholar] [CrossRef]
- Mohsin, S.; Atif, N.; Rabbani, W.; Tariq, A.; Khan, S.A.; Tariq, M.; Sikander, S. Cultural Adaptation of Community Informant Tool for Detection of Maternal Depression in Rural Pakistan. Front. Psychiatry 2021, 12, 181. [Google Scholar] [CrossRef]
- Keynejad, R.; Dua, T. CB-E Mental, Undefined. WHO Mental Health Gap Action Programme (mhGAP) Intervention Guide: A Systematic Review of Evidence from Low and Middle-Income Countries. ebmh.bmj.comSign in. 2018. Available online: https://ebmh.bmj.com/content/21/1/30.abstract (accessed on 27 July 2019).
- Mohsin, S.; Waqas, A.; Atif, N.; Rabbani, M.W.; Ali Khan, S.; Bilal, S.; Sharif, M.; Bibi, A.; Sikander, S. Accuracy of Community Informant Led Detection of Maternal Depression in Rural Pakistan. Int. J. Environ. Res. Public Health 2021, 18, 1075. [Google Scholar] [CrossRef] [PubMed]
- Jordans, M.J.D.; Kohrt, B.A.; Luitel, N.P.; Komproe, I.H.; Lund, C. Accuracy of proactive case finding for mental disorders by community informants in Nepal. Br. J. Psychiatry 2015, 207, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.; Gotman, N.; Lin, H.; Yonkers, K. Do the PHQ-8 and the PHQ-2 Accurately Screen for Depressive Disorders in a Sample of Pregnant Women? Megan. Gen. Hosp. Psychiatry 2010, 32, 544–548. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W.; Löwe, B. An Ultra-Brief Screening Scale for Anxiety and Depression: The PHQ–4. Psychosomatics 2009, 50, 613–621. [Google Scholar] [CrossRef]
- Zimmerman, M.; Martinez, J.H.; Young, D.; Chelminski, I.; Dalrymple, K. Severity classification on the Hamilton depression rating scale. J. Affect. Disord. 2013, 150, 384–388. [Google Scholar] [CrossRef]
- Hashmi, A.M.; Naz, S.; Asif, A.; Khawaja, I.S. Urdu translation of the hamilton rating scale for depression: Results of a validation study. Pak. J. Med. Sci. 2016, 32, 1479. [Google Scholar] [CrossRef]
- Williams, J.B.W. Standardizing the Hamilton Depression Rating Scale: Past, present, and future. Eur. Arch. Psychiatry Clin. Neurosci. 2001, 251, 6–12. [Google Scholar] [CrossRef]
- Gaskin, C.J.; Happell, B. On exploratory factor analysis: A review of recent evidence, an assessment of current practice, and recommendations for future use. Int. J. Nurs. Stud. 2014, 511–521. [Google Scholar] [CrossRef]
- Schulz, S.; Laessle, R.G. Associations of negative affect and eating behaviour in obese women with and without binge eating disorder. Eat Weight Disord. 2010, 15, e287–e293. [Google Scholar] [CrossRef]
- O’Connor, E.; Rossom, R.C.; Henninger, M.; Groom, H.C.; Burda, B.U. Primary care screening for and treatment of depression in pregnant and postpartumwomen evidence report and systematic review for the US preventive services task force. JAMA J. Am. Med. Assoc. 2016, 315, 388–406. [Google Scholar] [CrossRef]
- Yawn, B.P.; Dietrich, A.J.; Wollan, P.; Bertram, S.; Graham, D.; Huff, J.; Kurland, M.; Madison, S.; Pace, W.D. Trippd: A practice-based network effectiveness study of postpartum depression screening and management. Ann. Fam. Med. 2012, 10, 320–329. [Google Scholar] [CrossRef]
- Cronbach, L.; Meehl, P. Construct validity in psychological tests. Psychol. Bull. 1955, 52, 302. [Google Scholar] [CrossRef] [PubMed]
- Fava, M.; Rush, A.J.; Alpert, J.E.; Balasubramani, G.K.; Wisniewski, S.R.; Carmin, C.N.; Biggs, M.M.; Zisook, S.; Leuchter, A.; Howland, R.; et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: A STAR*D report. Am. J. Psychiatry 2008, 165, 342–351. [Google Scholar] [CrossRef]
- Judd, L.; Schettler, P.; Coryell, W.; Akiskal, H.; Fiedorowicz, J. Overt irritability/anger in unipolar major depressive episodes: Past and current characteristics and implications for long-term course. JAMA Psychiatry 2013, 70, 1171–1180. [Google Scholar] [CrossRef] [PubMed]
- Fried, E.I. Are more responsive depression scales really superior depression scales? J. Clin. Epidemiol. 2016, 77, 4–6. [Google Scholar] [CrossRef]
- Fried, E.I. Covert Heterogeneity of Major Depressive Disorder: Depression Is More Than the Sum-Score of its Symptoms. Psychol. Med. 2014, 44, 2067. [Google Scholar] [CrossRef]
- Fried, E.I.; Nesse, R.M. Depression sum-scores don’t add up: Why analyzing specific depression symptoms is essential. BMC Med. 2015, 13, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Fried, E.I.; Epskamp, S.; Nesse, R.M.; Tuerlinckx, F.; Borsboom, D. What are “good” depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J. Affect. Disord. 2016, 189, 314–320. [Google Scholar] [CrossRef]
- Fried, E.I. The 52 symptoms of major depression: Lack of content overlap among seven common depression scales. J. Affect. Disord. 2017, 208, 191–197. [Google Scholar] [CrossRef]

| Step | Scale | Items in the Scale | Delivery Agent |
|---|---|---|---|
| Phase 1: Identification of women at high risk of perinatal depression | Community informant detection tool |
| (1) Community health workers (2) Peers |
| Phase 2: Screening of high-risk women for perinatal depression | Patient Health Questionnaire-4 items |
| Lady Health Workers employed at Primary Care Centers |
| Phase 3: Measuring treatment responses | Hamilton Depression Rating Scale-4 items |
| Lady Health Workers employed at Primary Care Centers |
| Metric for Goodness of Fit | HAMD-6 | HAMD-4 |
|---|---|---|
| Chi-square (p-value) | 43.06 (<0.001) | 4.30 (0.04) |
| CMIN/df | 5.38 | 4.30 |
| GFI | 0.985 | 99.8 |
| AGFI | 0.960 | 97.6 |
| CFI | 94.9 | 99.6 |
| TLI | 90.4 | 97.9 |
| NFI | 93.8 | 99.5 |
| RMSEA | 0.07 | 0.06 |
| PCLOSE | 0.05 | 0.28 |
| AIC | 69.06 | 22.30 |
| BIC | 131.54 | 65.55 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Waqas, A.; Malik, A.; Atif, N.; Nisar, A.; Nazir, H.; Sikander, S.; Rahman, A. Scalable Screening and Treatment Response Monitoring for Perinatal Depression in Low- and Middle-Income Countries. Int. J. Environ. Res. Public Health 2021, 18, 6693. https://doi.org/10.3390/ijerph18136693
Waqas A, Malik A, Atif N, Nisar A, Nazir H, Sikander S, Rahman A. Scalable Screening and Treatment Response Monitoring for Perinatal Depression in Low- and Middle-Income Countries. International Journal of Environmental Research and Public Health. 2021; 18(13):6693. https://doi.org/10.3390/ijerph18136693
Chicago/Turabian StyleWaqas, Ahmed, Abid Malik, Najia Atif, Anum Nisar, Huma Nazir, Siham Sikander, and Atif Rahman. 2021. "Scalable Screening and Treatment Response Monitoring for Perinatal Depression in Low- and Middle-Income Countries" International Journal of Environmental Research and Public Health 18, no. 13: 6693. https://doi.org/10.3390/ijerph18136693
APA StyleWaqas, A., Malik, A., Atif, N., Nisar, A., Nazir, H., Sikander, S., & Rahman, A. (2021). Scalable Screening and Treatment Response Monitoring for Perinatal Depression in Low- and Middle-Income Countries. International Journal of Environmental Research and Public Health, 18(13), 6693. https://doi.org/10.3390/ijerph18136693





