Change of Use in Community Services among Disabled Older Adults during COVID-19 in Japan
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Subjects
2.3. Ethics Approval and Consent to Participate
2.4. Measures
2.5. Statistical Analysis
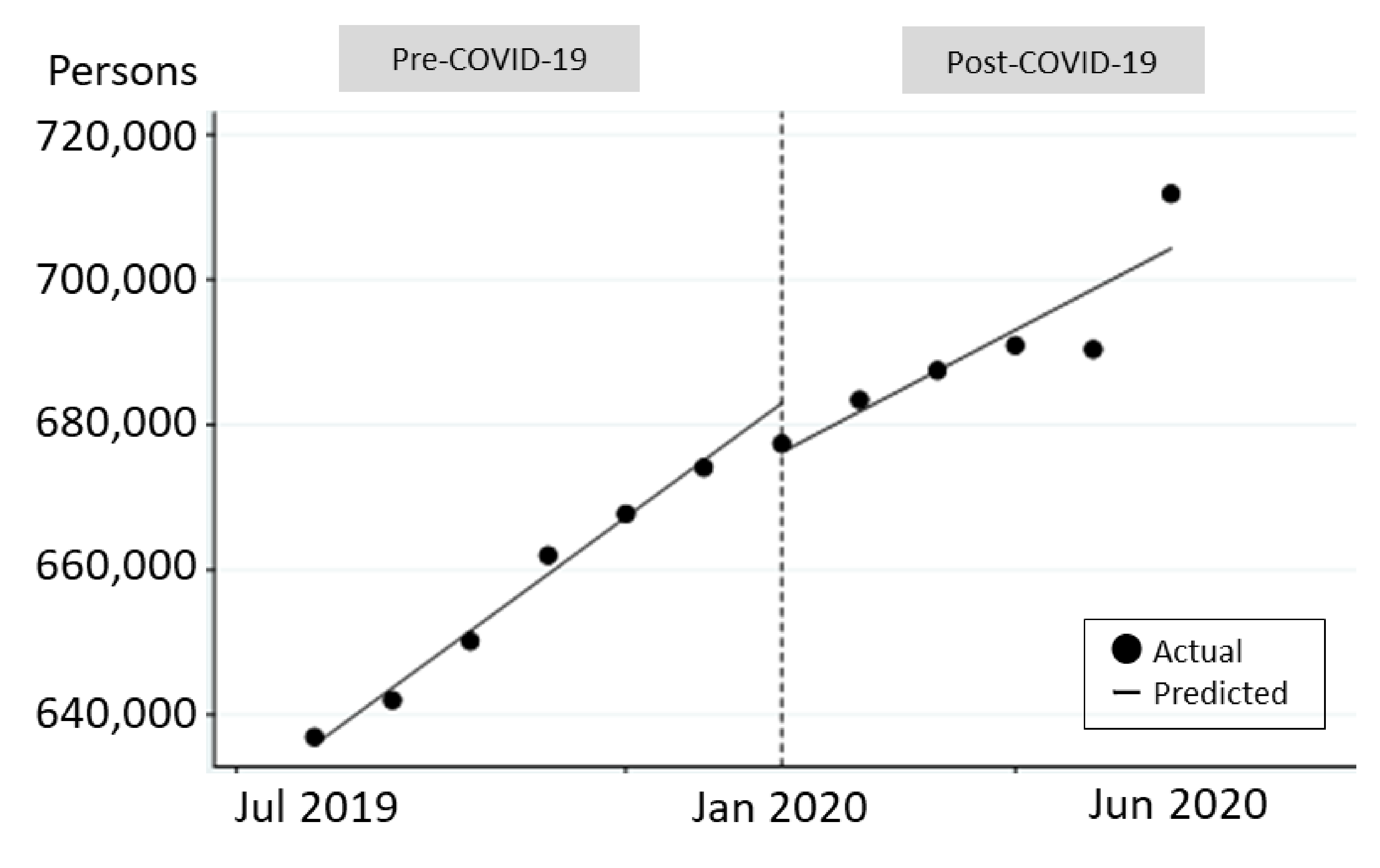
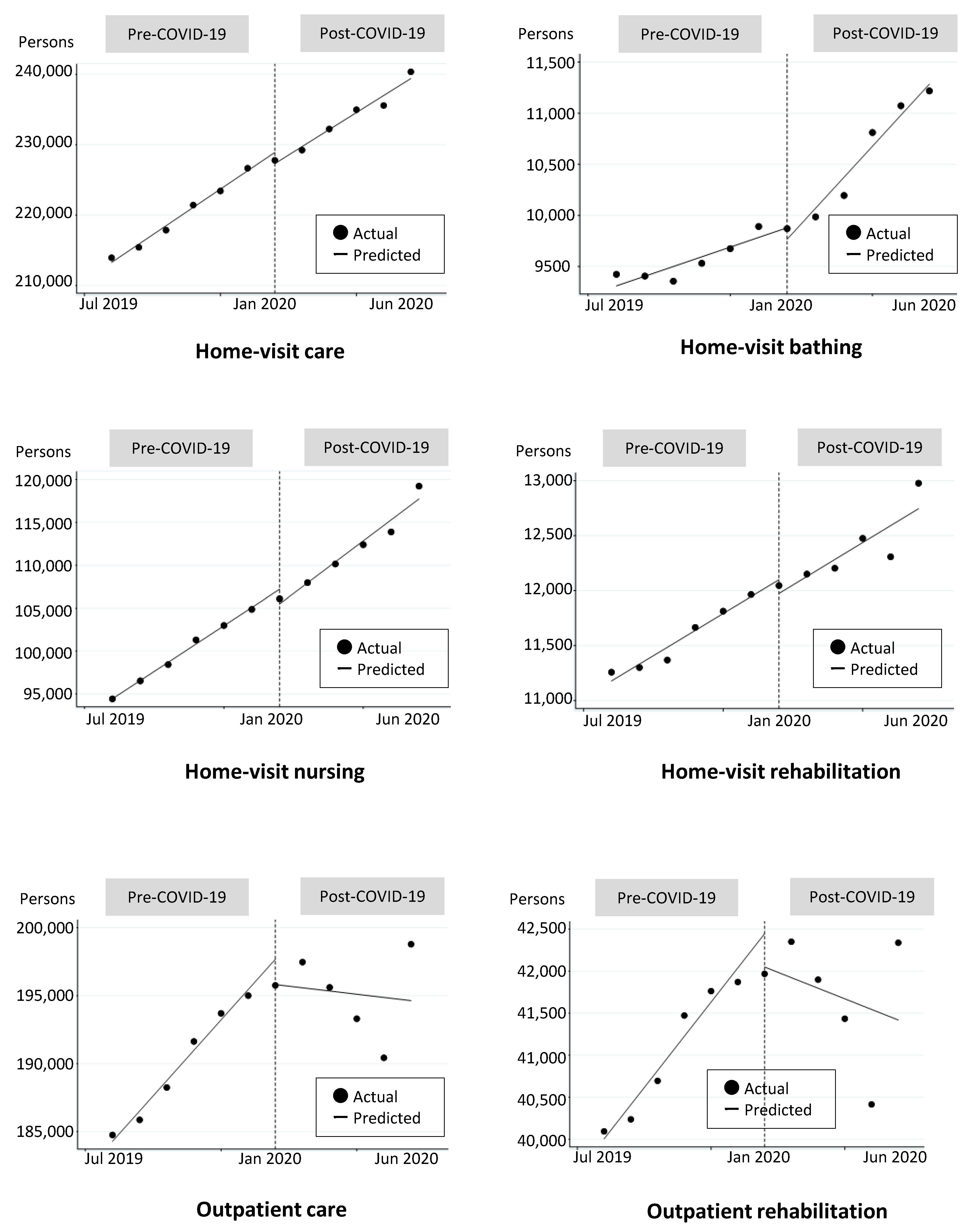
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Trend Pre-COVID-19 | Change in Level Post-COVID-19 | Change in Trend at the Post-COVID-19 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Est. | 95% CI | Est. | 95% CI | Est. | 95% CI | ||||
| All | 7845.0 | 7078.6 | 8611.4 | −6751.0 | −12,521.4 | −980.5 | −2229.3 | −6010.7 | 1552.2 |
| Home-visit care | 2605.1 | 2270.5 | 2939.7 | −1589.4 | −3055.9 | −122.9 | −187.4 | −841.9 | 467.1 |
| Home-visit bathing | 94.8 | 30.6 | 159.1 | −112.1 | −435.1 | 210.9 | 208.4 | 120.0 | 296.8 |
| Home-visit nursing | 2128.7 | 2031.2 | 2226.2 | −1713.4 | −3053.6 | −373.2 | 319.4 | −420.0 | 1058.7 |
| Home-visit rehabilitation | 153.3 | 117.8 | 188.8 | −125.0 | −325.9 | 75.9 | 1.1 | −123.9 | 126.1 |
| Outpatient care | 2232.2 | 1899.4 | 2564.9 | −1864.3 | −5232.1 | 1503.5 | −2468.7 | −4542.0 | −395.4 |
| Outpatient rehabilitation | 406.9 | 311.0 | 502.7 | −396.3 | −1219.8 | 427.2 | −533.1 | −1016.7 | −49.6 |
| Trend Pre-COVID-19 | Change in Level Post-COVID-19 | Change in Trend at the Post-COVID-19 | |||||
|---|---|---|---|---|---|---|---|
| βT | p-Value | βXt | p-Value | βTXt | p-Value | ||
| All | 0.0120 | <0.001 | 0.1002 | <0.001 | −0.0071 | <0.001 | |
| Sex | Male | 0.0121 | <0.001 | 0.0949 | <0.001 | −0.0066 | <0.001 |
| Female | 0.0119 | <0.001 | 0.1032 | <0.001 | −0.0073 | <0.001 | |
| Age | 65–74 | 0.0195 | <0.001 | −0.0234 | 0.248 | −0.0050 | <0.001 |
| 75–84 | 0.0180 | <0.001 | 0.0108 | 0.388 | −0.0084 | <0.001 | |
| 85+ | 0.0053 | <0.001 | 0.1841 | <0.001 | −0.0059 | <0.001 | |
| Care need level | CL1 | 0.0131 | <0.001 | 0.2096 | <0.001 | −0.0142 | <0.001 |
| CL2 | 0.0122 | <0.001 | 0.1140 | <0.001 | −0.0080 | <0.001 | |
| CL3 | 0.0111 | <0.001 | 0.0413 | 0.018 | −0.0033 | 0.005 | |
| CL4 | 0.0099 | <0.001 | −0.0421 | 0.043 | 0.0022 | 0.104 | |
| CL5 | 0.0120 | <0.001 | −0.0159 | 0.525 | 0.0004 | 0.819 | |
| Area | Seven prefectures | 0.0133 | <0.001 | 0.1536 | <0.001 | −0.0105 | <0.001 |
| Other prefectures | 0.0103 | <0.001 | 0.0345 | 0.002 | −0.0029 | <0.001 | |
| Service type | Home-visit care | 0.0119 | <0.001 | 0.0341 | 0.007 | −0.0027 | 0.001 |
| Home-visit bathing | 0.0099 | <0.001 | −0.3310 | <0.001 | 0.0212 | <0.001 | |
| Home-visit nursing | 0.0213 | <0.001 | 0.0354 | 0.056 | −0.0032 | 0.009 | |
| Home-visit rehabilitation | 0.0133 | <0.001 | 0.0914 | 0.098 | −0.0063 | 0.081 | |
| Outpatient care | 0.0118 | <0.001 | 0.2890 | <0.001 | −0.0194 | <0.001 | |
| Outpatient rehabilitation | 0.0099 | <0.001 | 0.2927 | <0.001 | −0.0196 | <0.001 | |
References
- Infectious Disease Surveillance Center, National Insitute of Infectous Disease. Information of New Coronavirus. Available online: https://www.niid.go.jp/niid/ja/from-idsc/2482-corona/9305-corona.html (accessed on 5 August 2020).
- Japan Cabinet Secretariat. Japan’s Response to the Novel Coronavirus Disease: Declaration of a State of Emergency. Available online: https://corona.go.jp/news/news_20200421_70.html (accessed on 5 August 2020).
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Kawana, A.; Mikasa, K.; Izumikawa, K. COVID-19. Nihon Naika Gakkai Zasshi 2020, 109, 392–395. [Google Scholar]
- McMichael, T.M.; Currie, D.W.; Clark, S.; Pogosjans, S.; Kay, M.; Schwartz, N.G.; Lewis, J.; Baer, A.; Kawakami, V.; Lukoff, M.D.; et al. Epidemiology of Covid-19 in a Long-Term Care Facility in King County, Washington. N. Engl. J. Med. 2020, 382, 2005–2011. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.C.; Ikegami, N. Long-term care insurance comes to Japan. Health Aff. 2000, 19, 26–39. [Google Scholar] [CrossRef]
- Ministry of Health, Labor and Welfare. Report for Provision of Long-Term Care Insurance (Kaigo Hoken Jigyo Jokyo Houkoku). 2018. Available online: https://www.mhlw.go.jp/topics/kaigo/osirase/jigyo/18/index.html (accessed on 12 January 2021).
- Hoogendijk, E.O.; Smit, A.P.; van Dam, C.; Schuster, N.A.; de Breij, S.; Holwerda, T.J.; Huisman, M.; Dent, E.; Andrew, M.K. Frailty Combined with Loneliness or Social Isolation: An Elevated Risk for Mortality in Later Life. J. Am. Geriatr. Soc. 2020, 68, 2587–2593. [Google Scholar] [CrossRef]
- Mehrabi, F.; Béland, F. Effects of social isolation, loneliness and frailty on health outcomes and their possible mediators and moderators in community-dwelling older adults: A scoping review. Arch. Gerontol. Geriatr. 2020, 90, 104119. [Google Scholar] [CrossRef]
- National Academies of Sciences. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System; The National Academies Press: Washington, DC, USA, 2020. [Google Scholar]
- Gale, C.R.; Westbury, L.; Cooper, C. Social isolation and loneliness as risk factors for the progression of frailty: The English Longitudinal Study of Ageing. Age Ageing 2018, 47, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Simard, J.; Volicer, L. Loneliness and Isolation in Long-term Care and the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2020, 21, 966–967. [Google Scholar] [CrossRef] [PubMed]
- Plagg, B.; Engl, A.; Piccoliori, G.; Eisendle, K. Prolonged social isolation of the elderly during COVID-19: Between benefit and damage. Arch. Gerontol. Geriatr. 2020, 89, 104086. [Google Scholar] [CrossRef]
- Eghtesadi, M. Breaking Social Isolation Amidst COVID-19: A Viewpoint on Improving Access to Technology in Long-Term Care Facilities. J. Am. Geriatr. Soc. 2020, 68, 949–950. [Google Scholar] [CrossRef]
- Jawaid, A. Protecting older adults during social distancing. Science 2020, 368, 145. [Google Scholar] [PubMed]
- Ministry of Health, Labor and Welfare. Ethical Guidelines for Medical and Health Research Involving Human Subjects. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hokabunya/kenkyujigyou/i-kenkyu/index.html (accessed on 12 January 2021).
- Ministry of Health, Labor and Welfare. How is the Certification of Need for Nursing Care Done? Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hukushi_kaigo/kaigo_koureisha/nintei/gaiyo2.html (accessed on 12 January 2021).
- Ministry of Health, Labor and Welfare. Overview of the 2015 Survey of Long-Term Care Service Facilities and Offices. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/kaigo/service15/dl/kekka-gaiyou_03.pdf (accessed on 12 January 2021).
- Lopez Bernal, J.; Cummins, S.; Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: A tutorial. Int. J. Epidemiol. 2017, 46, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Linden, A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J. 2015, 15, 480–500. [Google Scholar] [CrossRef]
- Prime Minister of Japan and His Cabinet. Information Related to COVID-19. Available online: https://www.kantei.go.jp/jp/headline/kansensho/coronavirus.html (accessed on 26 October 2020).
- Ministry of Health, Labor and Welfare. Social Security Council (Kaigo Kyuhu-hi Bunkakai) 188th (held on 15 October 2020) Document 1: Outpatient Care/Community-Based Outpatient Care/Reward for Outpatient Care for Dementia—About the Standard. Available online: https://www.mhlw.go.jp/content/12300000/000683014.pdf (accessed on 26 October 2020).
- Ministry of Health, Labor and Welfare. Home-Visit Care and Bathing. Available online: https://www.mhlw.go.jp/content/12300000/000660330.pdf (accessed on 12 January 2021).
- Meléndez, J.C.; Tomás, J.M.; Navarro, E. Everyday life activities and well-being: Their relationships with age and gender in the elderly. Ann. Psychol. 2011, 27, 164–169. [Google Scholar]
- Lim, W.; Liang, C.; Assantachai, P.; Auyeung, T.W.; Kang, L.; Lee, W.; Lim, J.; Sugimoto, K.; Akishita, M.; Chia, S.; et al. COVID-19 and older people in Asia: Asian Working Group for Sarcopenia calls to actions. Geriatr. Gerontol. Int. 2020, 20, 547–558. [Google Scholar] [CrossRef]
- Smith, B.J.; Lim, M.H. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res. Pract. 2020, 30, 3022008. [Google Scholar] [CrossRef]
- Goethals, L.; Barth, N.; Guyot, J.; Hupin, D.; Celarier, T.; Bongue, B. Impact of Home Quarantine on Physical Activity Among Older Adults Living at Home During the COVID-19 Pandemic: Qualitative Interview Study. JMIR Aging 2020, 3, e19007. [Google Scholar] [CrossRef]
- The Japan Geriatrics Society. COVID-10, Practice Caution for Older People. Available online: https://www.jpn-geriat-soc.or.jp/coronavirus/index.html (accessed on 12 January 2021).
- Ministry of Health, Labor and Welfare. Impact of the New Coronavirus Infection on the Medical Insurance System. Available online: https://www.mhlw.go.jp/content/12401000/000693625.pdf (accessed on 12 January 2021).
- KENPOREN National Federation of Health Insurance Societies. Statistical Data: Recent Trends in Health Insurance Association Medical Expenditures on September 2020. Available online: https://www.kenporen.com/toukei_data/pdf/chosa_r02_11_03.pdf (accessed on 12 January 2021).
- Tatematsu, M. On Problem of Respite Care Services Provision Appeared from Investigation to Cross Home Caregivers’ Daily-Care-Stresses and Use Effect of Respite Care Services—A Study on the Way Forward Nursing Home to Create a Sense of Community for Frail Elderly People (Part 2). J. Japan Soc. Home Econ. 2014, 65, 632–642. [Google Scholar]
- Etters, L.; Goodall, D.; Harrison, B.E. Caregiver burden among dementia patient caregivers: A review of the literature. J. Am. Acad. Nurse Pract. 2008, 20, 423–428. [Google Scholar] [CrossRef]
- Japan Federation of Kaigo Business Providers. Report of “Urgent Survey” on the Impact of the New Coronavirus Infection on Business. Available online: http://kaiziren.or.jp/wp/wp-content/uploads/2020/04/kinkyuutyousa20200422.pdf (accessed on 26 October 2020).
- Ministry of Health, Labor and Welfare. Merasurement to New Coronavirus Infections at Nursing Care Providers. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000121431_00089.html (accessed on 26 October 2020).
- Levitt, A.F.; Ling, S.M. COVID-19 in the Long-Term Care Setting: The CMS Perspective. J. Am. Geriatr. Soc. 2020, 68, 1366–1369. [Google Scholar] [CrossRef]
- Middleton, A.; Simpson, K.N.; Bettger, J.P.; Bowden, M.G. COVID-19 Pandemic and Beyond: Considerations and Costs of Telehealth Exercise Programs for Older Adults With Functional Impairments Living at Home-Lessons Learned From a Pilot Case Study. Phys. Ther. 2020, 100, 1278–1288. [Google Scholar] [CrossRef] [PubMed]
| Pre-COVID-19 | Post-COVID-19 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | |||||||||||
| Jul | Aug | Sep | Oct | Nov | Dec | Jan | Feb | Mar | Apr | May | Jun | |
| Users (persons) | ||||||||||||
| All services | 636,974 | 642,056 | 650,204 | 662,000 | 667,739 | 674,120 | 677,402 | 683,449 | 687,510 | 690,954 | 690,401 | 711,852 |
| Home-visit care | 213,939 | 215,423 | 217,854 | 221,429 | 223,429 | 226,656 | 227,786 | 229,238 | 232,232 | 234,976 | 235,575 | 240,359 |
| Home-visit bathing | 9424 | 9407 | 9357 | 9532 | 9675 | 9892 | 9871 | 9986 | 10,195 | 10,811 | 11,073 | 11,218 |
| Home-visit nursing | 94,425 | 96,528 | 98,430 | 101,313 | 102,993 | 104,870 | 106,091 | 107,968 | 110,139 | 112,393 | 113,882 | 119,228 |
| Home-visit rehabilitation | 11,258 | 11,301 | 11,369 | 11,666 | 11,814 | 11,964 | 12,045 | 12,150 | 12,203 | 12,475 | 12,307 | 12,977 |
| Outpatient care | 184,758 | 185,869 | 188,248 | 191,633 | 193,701 | 195,007 | 195,757 | 197,469 | 195,610 | 193,305 | 190,433 | 198,784 |
| Outpatient rehabilitation | 40,094 | 40,237 | 40,695 | 41,472 | 41,763 | 41,871 | 41,968 | 42,350 | 41,899 | 41,434 | 40,415 | 42,338 |
| Male (%) | 36.4 | 36.4 | 36.4 | 36.4 | 36.4 | 36.4 | 36.5 | 36.5 | 36.5 | 36.5 | 36.6 | 36.6 |
| Age (%) 65–74 | 13.5 | 13.6 | 13.7 | 13.8 | 13.9 | 14.1 | 12.9 | 13.0 | 13.2 | 13.3 | 13.4 | 13.5 |
| 75–84 | 36.5 | 36.7 | 36.9 | 37.1 | 37.4 | 37.6 | 33.9 | 34.1 | 34.3 | 34.4 | 34.5 | 34.8 |
| 85 + | 50.0 | 49.7 | 49.3 | 49.1 | 48.7 | 48.3 | 53.2 | 52.9 | 52.6 | 52.3 | 52.0 | 51.7 |
| Care need level (%) CL1 | 31.4 | 31.4 | 31.4 | 31.4 | 31.5 | 31.5 | 31.6 | 31.5 | 31.3 | 31.0 | 30.9 | 31.2 |
| CL2 | 29.7 | 29.7 | 29.8 | 29.7 | 29.7 | 29.8 | 29.8 | 29.8 | 29.8 | 29.7 | 29.7 | 29.7 |
| CL3 | 17.8 | 17.8 | 17.7 | 17.8 | 17.7 | 17.7 | 17.7 | 17.7 | 17.8 | 17.8 | 17.9 | 17.8 |
| CL4 | 12.5 | 12.5 | 12.5 | 12.5 | 12.4 | 12.4 | 12.4 | 12.4 | 12.5 | 12.6 | 12.7 | 12.6 |
| CL5 | 8.6 | 8.6 | 8.6 | 8.6 | 8.6 | 8.6 | 8.6 | 8.6 | 8.7 | 8.8 | 8.8 | 8.7 |
| Seven prefectures (%) | 54.8 | 54.9 | 55.0 | 55.1 | 55.1 | 55.2 | 55.3 | 55.4 | 55.3 | 55.0 | 54.9 | 55.2 |
| Trend Pre-COVID-19 | Change in Level Post-COVID-19 | Change in Trend at the Post-COVID-19 | |||||
|---|---|---|---|---|---|---|---|
| βT | p-Value | βXt | p-Value | βTXt | p-Value | ||
| All | 0.0120 | <0.001 | 0.0461 | <0.001 | −0.0038 | <0.001 | |
| Sex | Male | 0.0121 | <0.001 | 0.0413 | <0.001 | −0.0033 | <0.001 |
| Female | 0.0119 | <0.001 | 0.0503 | <0.001 | −0.0041 | <0.001 | |
| Age | 65–74 | 0.0195 | <0.001 | −0.0654 | <0.001 | −0.0024 | 0.031 |
| 75–84 | 0.0180 | <0.001 | −0.0500 | <0.001 | −0.0047 | <0.001 | |
| 85+ | 0.0053 | <0.001 | 0.1338 | <0.001 | −0.0028 | <0.001 | |
| Care need level | CL1 | 0.0131 | <0.001 | 0.1206 | <0.001 | −0.0088 | <0.001 |
| CL2 | 0.0122 | <0.001 | 0.0625 | <0.001 | −0.0048 | <0.001 | |
| CL3 | 0.0111 | <0.001 | 0.0100 | 0.490 | −0.0013 | 0.172 | |
| CL4 | 0.0099 | <0.001 | −0.0672 | <0.001 | 0.0038 | 0.001 | |
| CL5 | 0.0120 | <0.001 | −0.0305 | 0.143 | 0.0013 | 0.366 | |
| Area | Seven prefectures | 0.0133 | <0.001 | 0.0857 | <0.001 | −0.0064 | <0.001 |
| Other prefectures | 0.0103 | <0.001 | −0.0005 | 0.955 | −0.0007 | 0.241 | |
| Service type | Home-visit care | 0.0119 | <0.001 | 0.0148 | <0.001 | −0.0015 | <0.001 |
| Home-visit bathing | 0.0100 | <0.001 | −0.2924 | <0.001 | 0.0188 | <0.001 | |
| Home-visit nursing | 0.0213 | <0.001 | −0.0275 | <0.001 | 0.0007 | <0.001 | |
| Home-visit rehabilitation | 0.0133 | <0.001 | −0.0006 | <0.001 | −0.0007 | <0.001 | |
| Outpatient care | 0.0118 | <0.001 | 0.1827 | <0.001 | −0.0129 | <0.001 | |
| Outpatient rehabilitation | 0.0099 | <0.001 | 0.1826 | <0.001 | −0.0128 | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ito, T.; Hirata-Mogi, S.; Watanabe, T.; Sugiyama, T.; Jin, X.; Kobayashi, S.; Tamiya, N. Change of Use in Community Services among Disabled Older Adults during COVID-19 in Japan. Int. J. Environ. Res. Public Health 2021, 18, 1148. https://doi.org/10.3390/ijerph18031148
Ito T, Hirata-Mogi S, Watanabe T, Sugiyama T, Jin X, Kobayashi S, Tamiya N. Change of Use in Community Services among Disabled Older Adults during COVID-19 in Japan. International Journal of Environmental Research and Public Health. 2021; 18(3):1148. https://doi.org/10.3390/ijerph18031148
Chicago/Turabian StyleIto, Tomoko, Sachiko Hirata-Mogi, Taeko Watanabe, Takehiro Sugiyama, Xueying Jin, Shu Kobayashi, and Nanako Tamiya. 2021. "Change of Use in Community Services among Disabled Older Adults during COVID-19 in Japan" International Journal of Environmental Research and Public Health 18, no. 3: 1148. https://doi.org/10.3390/ijerph18031148
APA StyleIto, T., Hirata-Mogi, S., Watanabe, T., Sugiyama, T., Jin, X., Kobayashi, S., & Tamiya, N. (2021). Change of Use in Community Services among Disabled Older Adults during COVID-19 in Japan. International Journal of Environmental Research and Public Health, 18(3), 1148. https://doi.org/10.3390/ijerph18031148







