1. Introduction
Worldwide, malnutrition is a public health, social, and economic problem, imposing high human capital costs directly and indirectly on individuals, families, and nations. Several studies have estimated that all forms of malnutrition may perhaps cost society up to 3.5 trillion USD per year, with overweight and obesity alone having an estimated cost of about 500 billion USD per year [
1,
2]. Thus, the public health concerns associated with growing prevalence of childhood deaths and impending adult disability, with diet-related noncommunicable diseases (NCDs), have imposed enormous economic and human capital costs [
3,
4]. Thus, the Sustainable Development Goals (SDGs), under the auspices of the World Health Organization and the 2030 Agenda for Sustainable Development, have committed to reducing one-third of the burden of NCDs through prevention and treatment (SDG target 3.4). Several studies have cited a major surge in nutrition transition cycle, resulting in a burden of all forms of malnutrition, especially in developing countries such as those in Africa [
5,
6].
Moreover, malnutrition (leading to underweight, overweight, and obesity) has posed serious health risks with adverse implications for population health. In 2014, about 462 million adults globally were underweight, and 1.9 billion were either overweight or obese [
7]. In 2016, approximately 41 million children under the age of 5 years were overweight or obese, whereas 155 million were persistently malnourished [
8]. Accordingly, being overweight or obese is one of the leading risk factors for several NCDs and other chronic medical conditions. Furthermore, women with non-normal body weights are prone to various adverse diseases that are associated with detrimental health conditions and increased risk of early mortality. Many studies have revealed that women are more susceptible to malnutrition and its health risks owing to the interplay between food consumed and their genetic makeup [
6,
9].
Although the prevalence of underweight is decreasing in high-income countries, the upsurge of underweight, overweight, and obesity across African countries such as Nigeria and South Africa has become a public health concern. In Nigeria, studies have reported epidemiological and demographical changes, as well as nutritional transitions, which are driven by urbanization and unhealthy lifestyles, as the leading contributors to underweight and overweight/obesity [
10,
11]. According to the Nigeria Demographic Health Survey (NDHS) [
11], there is an alarming increase in the prevalence of underweight (12%) and overweight/obesity (28%) among women of childbearing age (15−49 years). Moreover, the NDHS trend analysis has shown that the percentage of thin women aged 15–49 years has remained constant over the past 10 years at 12%, whereas the percentage of those who are overweight/obese has increased from 22% in 2008 to 28% in 2018 [
11].
In South Africa, malnutrition has become an emergent public health problem, as the country is going through an epidemiological health transition revealing prevailing chronic malnutrition [
12]. Factors such as increased adoption of more westernized diets and the rise in sedentary behavior, owing to modernization, improved transport systems, and easy convenient access to unhealthy fast foods, are associated with over-weight/obesity and its related-health problems in South Africa [
6,
13]. Studies have documented that the body mass index (BMI) cutoffs for women and men are 29.2 and 23.6 respectively, whereby 68% of women are overweight/obese while 3% are underweight, as two-thirds of women (59%) have a BMI in the standard range [
14]. According to the South Africa Demographic Health Survey (SADHS), the trend analysis indicated that the mean BMI among women aged 15 and older has increased from 27.3 in 1998 to 29.2 in 2016, and the prevalence of overweight/obesity among women of childbearing age rose from 56% to 68%, with a decreased prevalence of underweight from 6% to 3% [
12]. In Nigeria and South Africa, underweight prevalence is declining to an extent, in comparison to overweight/obesity, which has a higher prevalence [
11,
12,
15,
16]; yet, other countries are still observing an increased prevalence of underweight [
17,
18]. Hitherto, studies on malnutrition conducted in Nigeria and South Africa have shown that overweight or obese women of childbearing age were more likely to be older, educated, married, in the highest wealth quintile, and residing in urban areas [
11,
12]. By contrast, women who were never married, resided in poor households, and had lower education attainment were more likely to be underweight in both countries [
11,
12].
Although useful, these studies have a number of limitations. First, the earlier studies explored population-based subgroups (such as children, adolescents, the elderly, and males) using other national representative datasets and primary-based community surveys, which may not clearly give the true picture of the socioeconomic, demographic, and health status of both countries. Second, the previous studies did not consider the comparative analysis of both countries, as they have indispensable social and demographic dynamics. Moreover, earlier studies did not consider the most suitable method (comprising the categorized nature of data) in handling effectively larger datasets for Nigeria and smaller datasets for South Africa. In contrast, our study uses a multilevel model analysis (linear mixed-effect model) involving a level two regression equation and random intercepts model to weigh the intracluster correlation coefficient (ICC) and a binary logistic regression for bivariate analysis, an important statistical methodology that has not been employed in previous studies conducted in Nigeria and South Africa for comparative analysis according to urban–rural variations.
Understanding the factors associated with underweight and overweight/obesity among women of childbearing age in Nigeria and South Africa would be useful for relevant health and non-health experts to implement evidence-based and appropriate interventions to address all forms of malnutrition. This context-specific information is also important to national and international stakeholders, given the contemporary obligation to accomplish SDG 3 to end all forms of malnutrition, as well as the Global Action Plan for the Prevention and Control of NCDs target 9 to reduce the overweight/obesity burden in both countries [
19,
20,
21,
22]. However, there is a dearth of research on the influence of urban–rural residence on women’s body weight in Nigeria and South Africa. Moreover, nationally representative studies on the body weight of women of childbearing age (15–49 years) and associated factors, using a multi-level model and ICC involving a cross-sectional survey and comparative analysis stratified by urban–rural variations in Nigeria and South Africa, are lacking.
We undertook a cross-sectional and descriptive study to explore the prevalence of body weight (underweight, normal, overweight, and obese) and its associated factors among women of childbearing age in Nigeria and South Africa stratified by urban–rural variations. The specific objectives based on urban–rural differences in Nigeria and South Africa were to determine the prevalence of body weights by urban–rural variations, examine the predictive influence of the body weight on the associated factors, and appraise the mediating effects of the levels of body weight on the predictive influence of urban–rural variations on its associated factors among women of childbearing age in Nigeria and South Africa.
4. Discussion
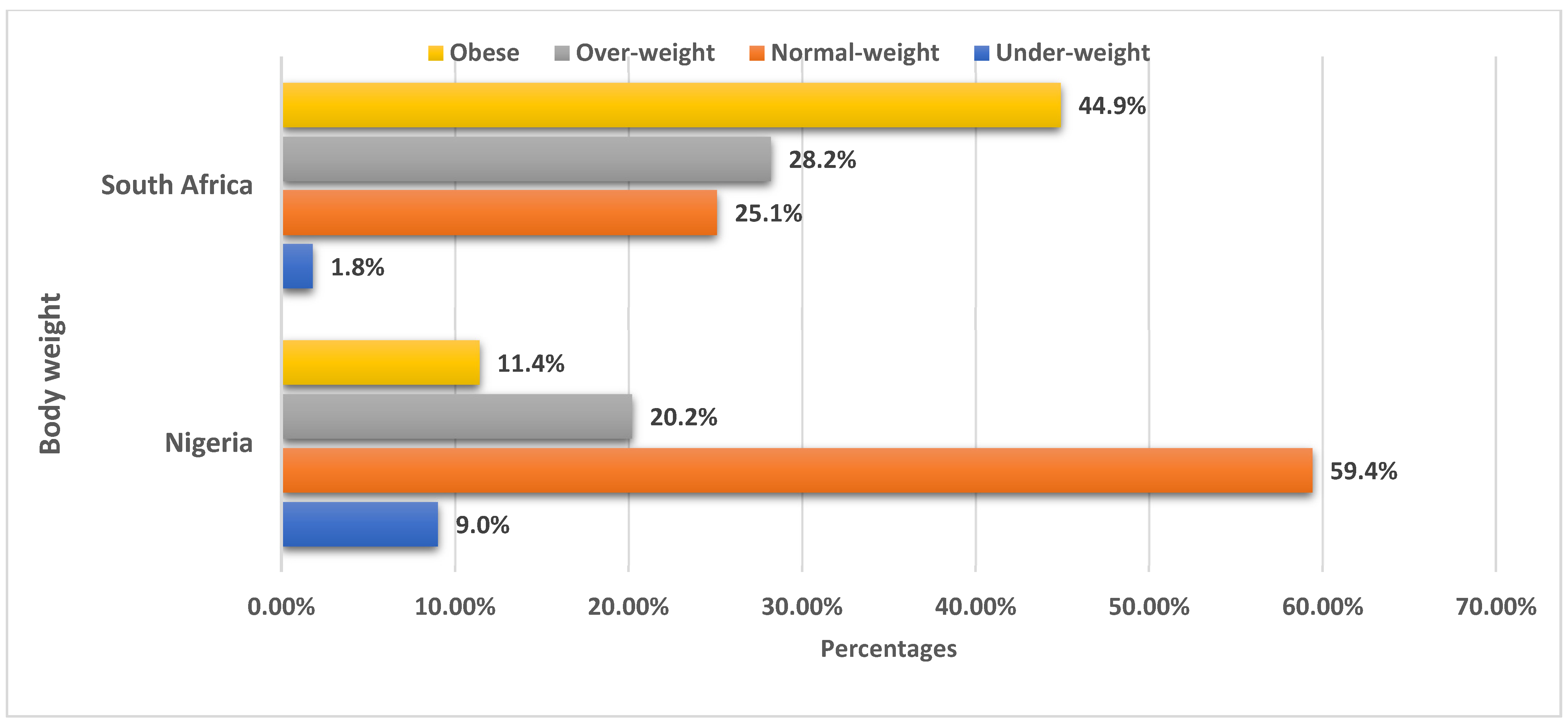
In this paper, we used data from two demographic health surveys (DHS), i.e., the 2018 NDHS and 2016 SADHS, to identify the urban–rural variations between women’s body weight and individual-level factors in Nigeria and South Africa. According to this study, the overall prevalence rates for overweight and obesity among women of childbearing age were 28.2% and 44.9% in South Africa. Similarly, the overall prevalence of overweight and obesity among women in South Africa in our study is comparable to evidence from the SADHS [
12] and existing studies conducted in South Africa among black men and women [
36,
37]. The findings showed that there is a higher prevalence of overweight and obesity among women aged between 30 and 59 years in South Africa, while the prevalence of overweight and obesity from other piloted studies conducted outside South Africa was lower [
38,
39,
40,
41,
42,
43]. The high prevalence of overweight and obesity obtained from previous South African studies piloted may in part be due to widespread sedentary lifestyles and a surge in processed food outlets, largely reflective of a trend across many African settings [
36,
37,
44].
On the other hand, a prevalence of overweight (20.2%) and obesity (11.4%) was obtained among women of childbearing age in Nigeria. This finding is not inconsistent with previous community surveys conducted in Nigeria, as well as a systematic review of Nigerian studies on overweight and obesity, where an increasing prevalence trend of overweight (25.5–45.3%) and obesity (19.8–40.2%) was obtained [
45,
46,
47]. A higher prevalence of overweight and obesity was marked among women of reproductive age obtained from previous Nigerian studies piloted [
9,
10,
11], which may be linked to cultural lifestyles, dietary choices, and sedentary lifestyles. However, a higher prevalence of underweight (9.0%) and normal weight (59.4%) was found among women in Nigeria compared to women who are underweight (1.8%) or have a normal weight (25.1%). This finding supports earlier research which showed the coexistence of both undernutrition and overnutrition in the same population, which over time has resulted in significant morbidity and mortality [
46,
47].
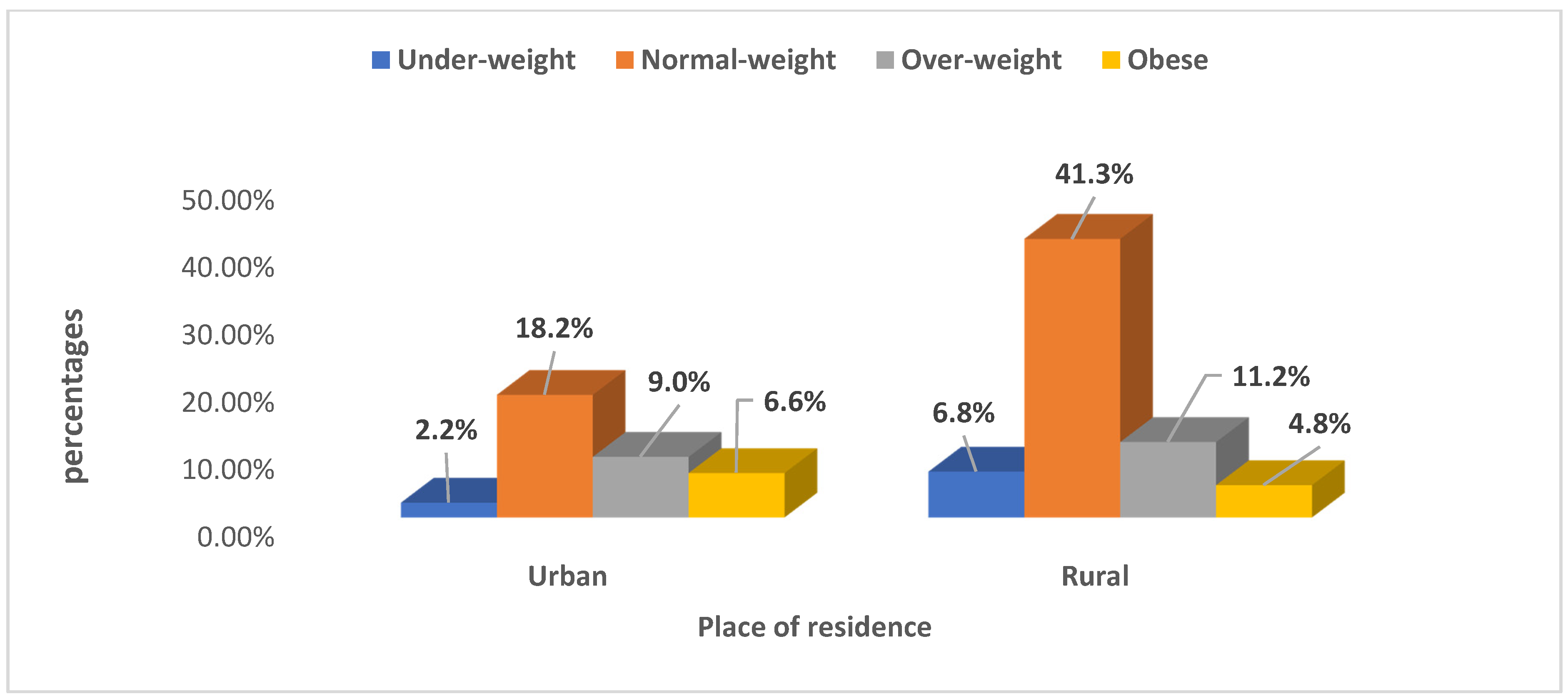
Research indicates that women from Nigeria residing in urban areas have a higher possibility of being overweight/obese, while rural women were found to be more likely to be either underweight or overweight. The findings of this study are consistent with previous studies from South Asian [
48,
49,
50,
51,
52,
53] and sub-Saharan Africa countries [
1,
2,
45,
54], which showed that women from rural households were at a higher risk of being underweight or overweight compared with their urban counterparts. The likely reason for the urban–rural differences in body weights of Nigerian women is due to a high level of financial constraints, shortage of job prospects, poor availability of healthcare services, and a sedentary and unhealthy dietary lifestyle (such as high intake of extremely caloric foods and poor consumption of fruits and vegetables) [
55,
56,
57]. Similarly, this finding is in line with studies in India and Nepal, which found that women in rural households were either underweight or overweight, as rural women are vulnerable to malnutrition [
48,
49]. This is also consistent with other study reports in low- and middle-income countries [
54]. This might be due to the fact that residing in rural areas is one of the determinant factors significantly associated with a high prevalence of underweight in this study and in other studies [
58,
59,
60,
61].
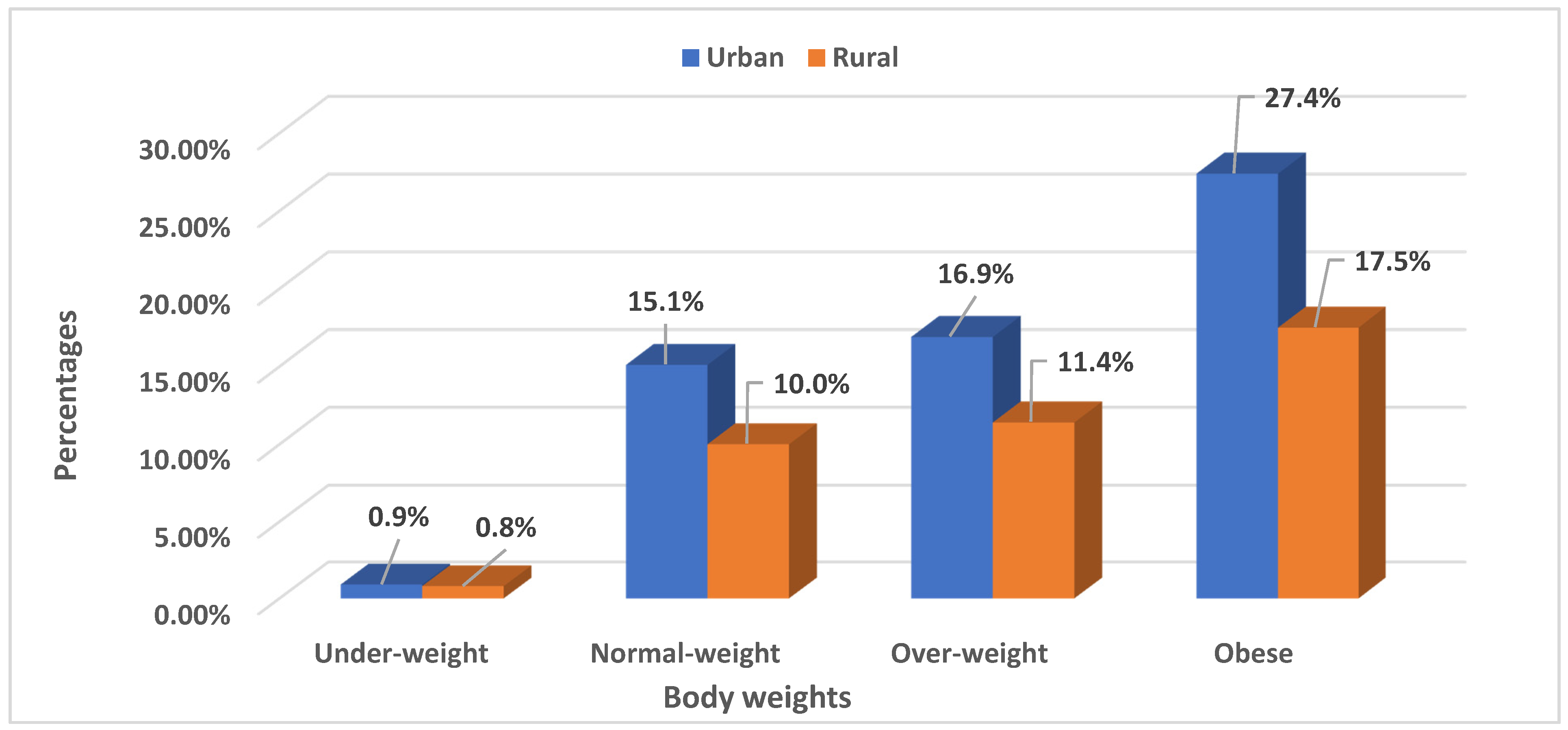
Furthermore, the findings of this study propose that long-term intervention to reduce the burden and health implications of being underweight/overweight among rural households should be aimed at women of low socio-economic class and who are from the poorest households. Moreover, in our study, which is consistent with other studies [
62,
63], there was a high prevalence of overweight and obesity among urban South African women. The prevalence of overweight/obesity was comparatively greater in urban than in rural settings [
12]. Thus, multiple factors are likely to contribute to the increased prevalence of overweight/obesity in urban populations, including the presence of modern communication facilities, increased availability of technology, easy access to energy-rich food, reduced levels of physical activity, and adoption of a sedentary lifestyle [
57,
58]. Studies revealed a higher prevalence of overweight and obesity among South African women of childbearing age compared with women from other African countries [
43,
59,
60]; this may be as a result of nutritional and epidemiological shifts, which are determined by factors such as demographic variations, rising earnings, suburbanization, unhealthy lifestyles, and consumption of highly processed diets, which appear to be strong drivers of a prevailing overweight and obesity epidemic among women of childbearing age in South Africa.
As expected, and consistent with other studies, our descriptive bivariate findings showed that there were significant differences in terms of body weight and socio-demographic factors in urban and rural populations in this study. The odds of being underweight among Nigerian women of childbearing age were increased by being self-employed, as well as being from the North east and North west geopolitical zones; breastfeeding was also significantly associated. This is consistent with other studies [
27,
28,
29,
59] and could be due to differences in educational status, food security, and access to information regarding nutrition education to address the prevalent underweight burden, especially among Nigerian women in rural grassroots communities. Moreover, in South Africa, our study findings showed that women of childbearing age who were underweight were more likely to belong to poorer wealth households, reside in the Northern Cape and Limpopo provinces, have height above average, be currently breastfeeding, and smoke cigarettes. These study findings are in line with other studies conducted in South Asian [
49,
51,
52] and other African countries [
39,
40,
59]. Studies have documented that the upturn in women’s employment is an important contributing factor to the direct causes of undernutrition such as feeding practices and ill health, and more distinct bases of undernutrition (such as income, food security, and education) have a greater prospect to improve women’s nutritional status [
64,
65,
66].
However, there were significant differences among overweight women and sociodemographic factors, such as increasing age (30–34 years; 35–39 years), secondary education, middle wealth index, divorced/separated, regional differences (South and South west zones), weight above average, contraceptive use (traditional and modern), and having more than four children. Similarly, significant differences were found among women who were obese, with socio-demographic factors, such as increasing age (40–44 years; 45–49 years), higher education, employed, higher wealth index, married/widowed, regional differences (South east, South south, and South west zones), height above average, weight above average, having more than four children, contraceptive use (traditional/modern), and cigarette smoking. Several studies (cross-sectional and longitudinal) have demonstrated the influence of socio-demographic factors with studies from sub-Saharan Africa [
1,
2,
67], and this is consistent with findings from studies conducted in Nigeria [
9,
13,
22].
In South Africa, the risk of being overweight and/or obese was also higher among women with increasing age (20–24; 25–29; 30–34; 35–39; 40–44; 45–49 years), higher education, employed, residing in higher wealth households, and presently married. For South African women, weight above average, having more than four children, and contraceptive use (modern method) were also significantly associated with obesity. Residing in urban settings (Eastern Cape, Free State, and Mpumalanga provinces) was associated with a higher risk of being overweight. Research indicates that women who are currently breastfeeding, are living with a partner, and have long working hours showed significant differences. Thus, women who are employed with long working hours were found to be obese. The results of this study are consistent with previous studies from Ghana [
58,
60], South Asian [
51,
52,
55], and sub-Saharan Africa countries [
2,
45].
In Nigeria and South Africa, overweight and obesity are often associated with affluence, and educational attainment is often used as a substitute indicator for socio-economic status. Therefore, it is not unexpected that the bivariate findings of this study showed that odds of overweight and obesity greatly increased as educational attainment increased among this study population. Women with tertiary education were two times more likely to be overweight or obese compared to those with no education. Similarly, women with higher education had progressively higher odds of being overweight/obese compared to those with no education. This finding is in agreement with the results from other studies conducted in Ethiopia [
6,
34,
40,
67] and in Asian countries [
48,
50,
51,
52,
53]. A likely explanation for this could be that, with higher education, women are more likely to earn a better income, and this makes it easier to adopt a more westernized way of life, which has been reported by several studies to be increasing the obesity epidemic in Nigeria [
21,
22] and South Africa [
15,
19].
From the multi-level findings of this study, older women were more associated with increased likelihood of overweight/obesity in Nigeria, and this supports previous studies showing that, as women get older, they face greater risks of being overweight/obese [
10,
16]. Women with secondary or higher education had higher odds of being overweight, while being employed was identified as a predictor of overweight/obesity in Nigeria and South Africa. Our findings also agree with these earlier studies, as socio-economic status is one of the major predictors of overweight/obesity in both countries [
51,
64,
68,
69]. In addition, research indications have revealed that higher education attainment is associated with the better health status of the community, owing to an improvement in socio-economic status [
68,
69], health literacy and health behaviors [
65,
66], and self-control and empowerment [
51,
64,
69]. This is not always the case in less developed and developing countries such as Nigeria and South Africa, where those with higher education are more likely to be overweight or obese [
37,
38,
41,
44].
Consistent with other studies conducted in other African countries, we found that South African women of childbearing age who attained secondary or higher education were more likely to be overweight/obese, similar to studies from Ghana [
58,
60], Bangladesh [
52,
53], and Ethiopia [
6,
40,
67]. The likely reasons for this study finding in Nigeria and South Africa are that women with higher education are more likely to have a higher socio-economic status and material resources and have ready access to energy-dense nutrition and sugary beverages, as well as a more sedentary paying job. Women from wealthier households, having weight above average, and presently living with partner had increased odds of being overweight or obese, among women from Nigeria [
9,
22] and South Africa [
14,
15]. Moreover, as the number of children increases, the odds of being overweight or obese were decreased, and smoking of cigarettes also increased the likelihood of being underweight among South African women. The results of this study are inconsistent with previous studies from Ghana [
58,
60], South Asian [
51,
61], and sub-Saharan Africa countries [
2,
45].
In Nigeria, women who are currently breastfeeding were found to have higher odds of being underweight compared to women in South Africa, who had lower odds of being overweight or obese when breastfeeding. Thus, weight loss or gain can be achieved during breastfeeding. Studies have shown that calories from fat cells stored in the body to produce milk are burned during breastfeeding [
27,
59,
70]. Furthermore, weight can be gained during breastfeeding if nursing mothers do not adopt healthy choices of dietary intake with increasing calories, rather than the necessary macro- and micronutrients [
63,
70]. This specific biochemical process depends on genetic factors, metabolism, and the hormone prolactin, which stimulates appetite, and breastfeeding predisposes nursing mothers to gain rapid weight during breastfeeding [
28,
29]. Furthermore, lack of sleep during breastfeeding may cause increased appetite and cravings for high-fat and high-calorie foods, stimulating weight gain among nursing mothers.
Our results showed variations in the way that regions of residence predict underweight and overweight in Nigeria. For instance, the North east region was consistently associated with increased odds of being underweight, whereas the South east and South south regions were consistently associated with increased odds of being overweight. These results are also in agreement with earlier studies which highlighted the influence of locational factors on body weight categories [
11,
16,
22]. In South Africa, women residing in Eastern Cape, Free State, KwaZulu-Natal, Northwest, Gauteng, and Mpumalanga were more associated with increased likelihood of obesity. This finding supports the higher odds of overweight and obesity by province reported by the 2016 South African Demographic Health Survey [
12,
15]. These results are also in agreement with earlier studies which highlighted the influence of locational factors on body weight categories [
58,
62]. The reason for this could also be due to dissimilarities in the socio-cultural and environmental practices and the dynamics prevailing in different provinces/geopolitical zones. These varying factors could lead to changes in the dimensions of culture and traditional beliefs, as well as the socio-economic status of the population, all of which usually have an intense influence on cultural interpretations and body weight [
36,
62,
71,
72].
However, the ICC for body weight and its associated factors among Nigerian and South African women of childbearing age varied substantially, from a minimum of underweight of 0.0102 in South Africa to a maximum of 0.0127 for Nigeria. Additionally, variances can be found in the overweight and obesity categories in Models 2 and 3 with respect to Nigeria and South Africa (
Table 4). These findings indicated that universal strategies to control overweight and obese body categories may not consistently show effective outcomes in both countries [
17,
34,
62]. For instance, some strategic interventions or preventive approaches regarding the problem of body weight in Nigeria may not be equally effective in South Africa. Therefore, each country should modify the World Health Organization’s (WHO) or other international strategies according to the country’s needs in terms of clustering in geographical areas (ICC). Countries with a low ICC, such as South Africa as found in this study, should consider giving more emphasis to an entire population approach [
34,
62]. Countries such as Nigeria with a high ICC should consider adding targeted population approaches to the aggregate population approach [
34,
62]. These approaches should be directed to identify those households with low socio-economic status that are eligible, and strict targeting should be a priority for any countries with variations in ICC.
Furthermore, these approaches to address high ICC variations for different countries have the potential for implementing public health interventions that are aimed at increasing healthy behavioral factors by targeting those geographic clusters with poor or unhealthy lifestyles. Similarly, to improve health behavioral factors, a targeted population approach should be implemented to curb unhealthy lifestyles such as low physical activity, unhealthy dietary intake and enactment of government policies to control advertisement and marketing of junk or fast food among populations in high-risk areas [
73,
74,
75]. Importantly, most developed countries across Europe, China and the United States of America have made efforts to place stringent advertisement controls, most especially directed at high-risk persons with overweight and obesity health concerns and the provision of supplemental nutrition assistance programs, to encourage adopting healthy lifestyle behaviors. In addition, determining the predictors of body weight and its associated factors using the intracluster correlation coefficient (ICC) may help to modify the public health interventions for body weight, socio-demographic, and behavioral factors according to geographic variations, targeting interventions in Nigeria and South Africa.
Strengths and Limitations
This study had several major strengths and limitations. Firstly, to the best of the authors’ knowledge, this is the first cross-sectional survey and nationally representative health demography and medical sociology study researching body weight and its individual-level factors among women of childbearing age by urban–rural variations in Nigeria and South Africa. Secondly, the data analysis was basically conducted to determine the association based on predictor likelihood and not a measure of causality; however, insight can be gained from comparing the 2018 DHS dataset from Nigeria and 2016 DHS dataset from South Africa to improve the study’s generalizability to other settings or populations. Thirdly, to the best of the authors’ knowledge, this is the first time that multi-level regression models were aimed at elucidating the predicting factors of the possibility of being underweight, overweight, or obese compared to normal weight in Nigeria and South Africa. A final strength is the practical application of employing the ICC of multilevel analytical methods in determining the magnitude of exposure of women of childbearing age in different countries to the characteristics associated with body weight.
There were some limitations, however, that need to be highlighted. Firstly, owing to the cross-sectional nature of the studies (2018 NDHS and 2016 SADHS), we cannot draw causal inferences from the findings. Secondly, possible bias in reporting body weights (underweight, normal, overweight, and obese) could have occurred related to individuals’ recall of behavioral factors, especially lifestyle factors. Thirdly, self-reported data on height and weight of the individuals were used in generating individual BMI, and possible errors might have occurred when recording the weight and height of the respondents.