Experience of Bangladeshi Dental Students towards Online Learning during the COVID-19 Pandemic: A Web-Based Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Procedure
2.3. Measures
2.4. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chang, T.; Hsu, M.; Kwon, J.; Kusdhany, M.L.S.; Hong, G. Effect of online learning for dental education in asia during the pandemic of COVID-19. J. Dent. Sci. 2021, 16, 1095–1101. [Google Scholar] [CrossRef] [PubMed]
- Binshehab, S.M.; An, N. Perception for online learning among undergraduate and postgraduate dental students during COVID-19 pandemic. Ann. Med. Health Sci. Res. 2021, 11, 1334–1339. [Google Scholar]
- Selvaraj, A.; Radhin, V.; Nithin, K.A.; Benson, N.; Mathew, A.J. Effect of pandemic based online education on teaching and learning system. Int. J. Educ. Dev. 2021, 85, 102444. [Google Scholar] [CrossRef] [PubMed]
- Купер, И.P.; Rosenberg, M.J. e-learning: Strategies for delivering knowledge in the digital age. New York: McGrow-Hill, 2001. Coцuoлoгuчecкuй жypнaл 2002, 2, 169–174. [Google Scholar]
- Rossett, A.; Kendra, S. Beyond the Podium: Delivering Training and Performance to a Digital World; Academy of Management: Briar Cliff Manor, NY, USA, 2001. [Google Scholar]
- Palvia, S.; Aeron, P.; Gupta, P.; Mahapatra, D.; Parida, R.; Rosner, R.; Sindhi, S. Online education: Worldwide status, challenges, trends, and implications. J. Glob. Inf. Technol. Manag. 2018, 21, 233–241. [Google Scholar] [CrossRef] [Green Version]
- Islam, M.I.; Biswas, R.K.; Khanam, R. Effect of internet use and electronic game-play on academic performance of Australian children. Sci. Rep. 2020, 10, 21727. [Google Scholar] [CrossRef]
- Hillenburg, K.L.; Cederberg, R.A.; Gray, S.A.; Hurst, C.L.; Johnson, G.K.; Potter, B.J. E-learning and the future of dental education: Opinions of administrators and information technology specialists. Eur. J. Dent. Educ. 2006, 10, 169–177. [Google Scholar] [CrossRef]
- Reynolds, P.A.; Rice, S.; Uddin, M. Online learning in dentistry: The changes in undergraduate perceptions and attitudes over a four year period. Br. Dent. J. 2007, 203, 419–423. [Google Scholar] [CrossRef]
- Miller, C.J.; Metz, M.J. Can clinical scenario videos improve dental students’ perceptions of the basic sciences and ability to apply content knowledge? J. Dent. Educ. 2015, 79, 1452–1460. [Google Scholar] [CrossRef]
- Hempel, G.; Neef, M.; Rotzoll, D.; Heinke, W. Study of medicine 2.0 due to Web 2.0?!-risks and opportunities for the curriculum in Leipzig. GMS Z. Für Med. Ausbild. 2013, 30, Doc11. [Google Scholar] [CrossRef]
- Sucha, M.; Engelhardt, S.; Sarikas, A. Internet discussion forums as part of a student-centred teaching concept of pharmacology. GMS Z. Für Med. Ausbild. 2013, 30, Doc2. [Google Scholar] [CrossRef]
- UNESCO. UNICEF and the World Bank Survey on National Education Responses to COVID-19 School Closures; UNESCO: Paris, France, 2020. [Google Scholar]
- O’Doherty, D.; Dromey, M.; Lougheed, J.; Hannigan, A.; Last, J.; McGrath, D. Barriers and solutions to online learning in medical education–an integrative review. BMC Med. Educ. 2018, 18, 130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, J.Y.; Wang, L.; Lin, T.; Cheng, F.; Chiang, C. Comparison of learning effectiveness between physical classroom and online learning for dental education during the COVID-19 pandemic. J. Dent. Sci. 2021, 16, 1281–1289. [Google Scholar] [CrossRef]
- Badovinac, A.; Par, M.; Plančak, L.; Balić, M.D.; Vražić, D.; Božić, D.; Musić, L. The impact of the COVID-19 pandemic on dental education: An online survey of students’ perceptions and attitudes. Dent. J. 2021, 9, 116. [Google Scholar] [CrossRef]
- Li, W.; Gillies, R.; He, M.; Wu, C.; Liu, S.; Gong, Z.; Sun, H. Barriers and facilitators to online medical and nursing education during the COVID-19 pandemic: Perspectives from international students from low-and middle-income countries and their teaching staff. Hum. Resour. Health 2021, 19, 64. [Google Scholar] [CrossRef] [PubMed]
- Quinn, B.; Field, J.; Gorter, R.; Akota, I.; Manzanares, M.; Paganelli, C.; Davies, J.; Dixon, J.; Gabor, G.; Amaral Mendes, R. COVID-19: The immediate response of european academic dental institutions and future implications for dental education. Eur. J. Dent. Educ. 2020, 24, 811–814. [Google Scholar] [CrossRef]
- Pei, L.; Wu, H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med. Educ. Online 2019, 24, 1666538. [Google Scholar] [CrossRef] [Green Version]
- Barteit, S.; Guzek, D.; Jahn, A.; Bärnighausen, T.; Jorge, M.M.; Neuhann, F. Evaluation of e-learning for medical education in low-and middle-income countries: A systematic review. Comput. Educ. 2020, 145, 103726. [Google Scholar] [CrossRef]
- Akhter, H.; Abdul Rahman, A.A.; Jafrin, N.; Mohammad Saif, A.N.; Esha, B.H.; Mostafa, R. Investigating the barriers that intensify undergraduates’ unwillingness to online learning during COVID-19: A study on public universities in a developing country. Cogent Educ. 2022, 9, 2028342. [Google Scholar] [CrossRef]
- Karim, M.A. Digital Bangladesh for good governance. In Proceedings of the Bangladesh Development Forum, Dhaka, Bangladesh, 15–16 February 2010; pp. 15–16. [Google Scholar]
- Kabir, R.; Mahmud, I.; Chowdhury, M.T.H.; Vinnakota, D.; Jahan, S.S.; Siddika, N.; Isha, S.N.; Nath, S.K.; Hoque Apu, E. COVID-19 vaccination intent and willingness to pay in Bangladesh: A cross-sectional study. Vaccines 2021, 9, 416. [Google Scholar] [CrossRef]
- Pahinis, K.; Stokes, C.W.; Walsh, T.F.; Cannavina, G. Evaluating a blended-learning course taught to different groups of learners in a dental school. J. Dent. Educ. 2007, 71, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Baticulon, R.E.; Sy, J.J.; Alberto, N.R.I.; Baron, M.B.C.; Mabulay, R.E.C.; Rizada, L.G.T.; Tiu, C.J.S.; Clarion, C.A.; Reyes, J.C.B. Barriers to online learning in the time of COVID-19: A national survey of medical students in the Philippines. Med. Sci. Educ. 2021, 31, 615–626. [Google Scholar] [CrossRef] [PubMed]
- Alrashdi, M.; Hameed, A.; Aljabr, A. COVID-19 and a Call to Adapt Dental Education. Front. Dent. Med. 2021, 2, 664460. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Rahiotis, C.; Tseroni, M.; Madianos, P.; Tzoutzas, I. Attitudes toward Vaccinations and Vaccination Coverage Rates among Dental Students in Greece. Int. J. Environ. Res. Public Health 2022, 19, 2879. [Google Scholar] [CrossRef]
- Saqlain, M.; Munir, M.M.; Rehman, S.U.; Gulzar, A.; Naz, S.; Ahmed, Z.; Tahir, A.H.; Mashhood, M. Knowledge, attitude, practice and perceived barriers among healthcare workers regarding COVID-19: A cross-sectional survey from Pakistan. J. Hosp. Infect. 2020, 105, 419–423. [Google Scholar] [CrossRef]
- Isha, S.N.; Ahmad, A.; Kabir, R.; Apu, E.H. Dental clinic architecture prevents COVID-19-like infectious diseases. HERD Health Environ. Res. Des. J. 2020, 13, 240–241. [Google Scholar] [CrossRef]
- Hassan, R.; Khalifa, A.; ElSewefy, T.; Hassan, M.G. Perceptions of clinical dental students towards online education during the COVID-19 crisis: An Egyptian multicenter cross-sectional survey. Front. Psychol. 2022, 12, 704179. [Google Scholar] [CrossRef]
- Ilić, J.; Radović, K.; Savić-Stanković, T.; Popovac, A.; Miletić, V.; Milić Lemić, A. The effect of COVID-19 pandemic on final year dental students’ self-confidence level in performing clinical procedures. PLoS ONE 2021, 16, e0257359. [Google Scholar] [CrossRef]
- Sarwar, H.; Akhtar, H.; Naeem, M.M.; Khan, J.A.; Waraich, K.; Shabbir, S.; Hasan, A.; Khurshid, Z. Self-reported effectiveness of e-Learning classes during COVID-19 pandemic: A nation-wide survey of Pakistani undergraduate dentistry students. Eur. J. Dent. 2020, 14, S34–S43. [Google Scholar] [CrossRef]
- Hossain, M.J.; Ahmmed, F.; Rahman, S.A.; Sanam, S.; Emran, T.B.; Mitra, S. Impact of online education on fear of academic delay and psychological distress among university students following one year of COVID-19 outbreak in Bangladesh. Heliyon 2021, 7, e07388. [Google Scholar] [CrossRef]
- Young, T.K. Minds Matter: Resources. 2022. Available online: https://youngmindsmatter.telethonkids.org.au/for-researchers/ (accessed on 21 June 2022).
- Veall, M.R.; Zimmermann, K.F. Pseudo-R2 measures for some common limited dependent variable models. J. Econ. Surv. 1996, 10, 241–259. [Google Scholar] [CrossRef] [Green Version]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons: Hoboken, NJ, USA, 2013; Volume 398. [Google Scholar]
- Jones, A.M. Models for Health Care; University of York, Centre for Health Economics: York, UK, 2010. [Google Scholar]
- Seshan, V.E.; Gönen, M.; Begg, C.B. Comparing ROC curves derived from regression models. Stat. Med. 2013, 32, 1483–1493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herr, L.; Jih, M.K.; Shin, J.; Chae, Y.K.; Lee, H.; Choi, S.C.; Nam, O.H. The perspective of undergraduate dental students on web-based learning in pediatric dentistry during the COVID-19 pandemic: A Korean multicenter cross-sectional survey. BMC Med. Educ. 2021, 21, 505. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Bhusal, C.K.; Subedi, S.; Kasarla, R.R. Perception towards Online Classes during COVID-19 among MBBS and BDS Students in a Medical College of Nepal: A Descriptive Crosssectional Study. JNMA J. Nepal Med. Assoc. 2021, 59, 276. [Google Scholar] [CrossRef]
- Haroon, Z.; Azad, A.A.; Sharif, M.; Aslam, A.; Arshad, K.; Rafiq, S. COVID-19 era: Challenges and solutions in dental education. J. Coll. Physicians Surg. Pak. 2020, 30, 129–131. [Google Scholar]
- Cheng, H.; Lu, S.; Yen, Y.; Siewchaisakul, P.; Yen, A.M.; Chen, S.L. Dental education changed by COVID-19: Student’s perceptions and attitudes. BMC Med. Educ. 2021, 21, 364. [Google Scholar] [CrossRef]
- Jiang, Z.; Zhu, D.; Li, J.; Ren, L.; Pu, R.; Yang, G. Online dental teaching practices during the COVID-19 pandemic: A cross-sectional online survey from China. BMC Oral Health 2021, 21, 189. [Google Scholar] [CrossRef]
- Wang, K.; Zhang, L.; Ye, L. A nationwide survey of online teaching strategies in dental education in China. J. Dent. Educ. 2021, 85, 128–134. [Google Scholar] [CrossRef]
- Abbasi, S.; Ayoob, T.; Malik, A.; Memon, S.I. Perceptions of students regarding E-learning during COVID-19 at a private medical college. Pak. J. Med. Sci. 2020, 36, S57. [Google Scholar] [CrossRef]
- Ardies, J.; De Maeyer, S.; Gijbels, D.; van Keulen, H. Students attitudes towards technology. Int. J. Technol. Des. Educ. 2015, 25, 43–65. [Google Scholar] [CrossRef]
- Avunduk, A.T.E.; Delikan, E. Satisfaction and stress levels of dentistry students relating to distance education. Dent. Med. Probl. 2021, 58, 291–298. [Google Scholar]
- Dost, S.; Hossain, A.; Shehab, M.; Abdelwahed, A.; Al-Nusair, L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: A national cross-sectional survey of 2721 UK medical students. BMJ Open 2020, 10, e042378. [Google Scholar] [CrossRef] [PubMed]
- Iurcov, R.; Pop, L.; Iorga, M. Impact of COVID-19 pandemic on academic activity and health status among romanian medical dentistry students; A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 6041. [Google Scholar] [CrossRef]
- Schlenz, M.A.; Schmidt, A.; Wöstmann, B.; Krämer, N.; Schulz-Weidner, N. Students’ and lecturers’ perspective on the implementation of online learning in dental education due to SARS-CoV-2 (COVID-19): A cross-sectional study. BMC Med. Educ. 2020, 20, 354. [Google Scholar] [CrossRef] [PubMed]
- Deery, C. The COVID-19 pandemic: Implications for dental education. Evid.-Based Dent. 2020, 21, 46–47. [Google Scholar] [CrossRef]
- Silva, P.G.D.B.; de Oliveira, C.A.L.; Borges, M.M.F.; Moreira, D.M.; Alencar, P.N.B.; Avelar, R.L.; Bitu Sousa, R.M.R.; Sousa, F.B. Distance learning during social seclusion by COVID-19: Improving the quality of life of undergraduate dentistry students. Eur. J. Dent. Educ. 2021, 25, 124–134. [Google Scholar] [CrossRef]
- Varvara, G.; Bernardi, S.; Bianchi, S.; Sinjari, B.; Piattelli, M. Dental education challenges during the COVID-19 pandemic period in Italy: Undergraduate student feedback, future perspectives, and the needs of teaching strategies for professional development. Healthcare 2021, 9, 454. [Google Scholar] [CrossRef]
- Kabir, R.; Isha, S.N.; Chowdhury, M.T.H.; Siddika, N.; Jahan, S.S.; Saha, A.K.; Nath, S.K.; Jahan, M.S.; Sivasubramanian, M.; Mahmud, I. Depression among the non-native international undergraduate students studying Dentistry in Bangladesh. Int. J. Environ. Res. Public Health 2021, 18, 5802. [Google Scholar] [CrossRef]
| Characteristics | n (%) |
|---|---|
| Total | 952 (100) |
| Age (Mean ± SD) | 21.7 (1.66) |
| Gender | |
| Male | 246 (25.8) |
| Female | 706 (74.2) |
| Type of institute | |
| Private | 728 (76.5) |
| Public | 224 (23.5) |
| Year of dental school | |
| 1st | 304 (31.9) |
| 2nd | 203 (21.3) |
| 3rd | 241 (25.3) |
| 4th | 204 (21.4) |
| Access to internet | |
| Easy | 758 (79.6) |
| Difficult | 194 (20.4) |
| Supply of electricity | |
| Interrupted | 511 (53.7) |
| Uninterrupted | 441 (46.3) |
| Type of electronic device used | |
| Smartphone | 910 (95.6) |
| Laptop/desktop/tablet | 39 (4.1) |
| Combination | 3 (0.3) |
| Device owned | |
| Student | 828 (86.9) |
| Others | 125 (13.1) |
| Level of satisfaction | |
| Satisfied | 119 (12.5) |
| Dissatisfied | 833 (87.5) |
| Variables | Satisfied n (%) | Dissatisfied n (%) | χ2 | p-Value |
|---|---|---|---|---|
| Gender | ||||
| Male | 43 (17.48) | 203 (82.52) | 7.52 | 0.006 |
| Female | 76 (10.76) | 630 (89.24) | ||
| Type of Institute | ||||
| Private | 94 (12.91) | 634 (87.09) | 0.48 | 0.488 |
| Public | 25 (11.16) | 199 (88.84) | ||
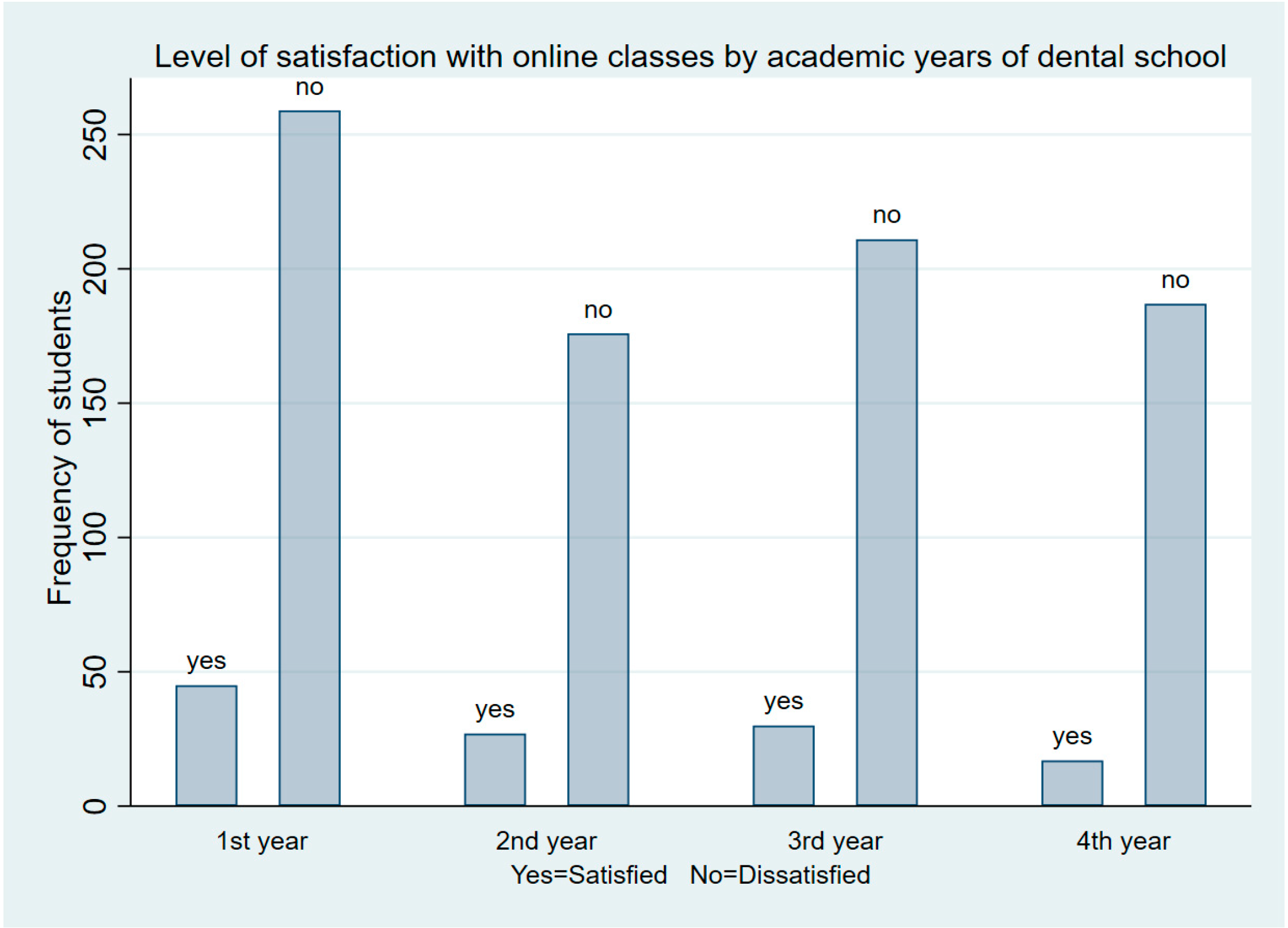
| Year of dental school | ||||
| 1st | 45 (14.80) | 259 (85.20) | 4.83 | 0.185 |
| 2nd | 27 (13.30) | 176 (86.70) | ||
| 3rd | 30 (12.45) | 211 (87.55) | ||
| 4th | 17 (8.33) | 187 (91.67) | ||
| Access to internet | ||||
| Easy | 92 (12.14) | 666 (87.86) | 0.44 | 0.503 |
| Difficult | 27 (13.92) | 167 (86.08) | ||
| Supply of electricity | ||||
| Interrupted | 57 (11.15) | 454 (88.85) | 1.83 | 0.177 |
| Uninterrupted | 62 (14.06) | 379 (85.94) | ||
| Type of electronic device used | ||||
| Smartphone | 111 (12.20) | 799 (87.80) | 2.79 | 0.247 |
| Laptop/desktop/tab | 8 (20.51) | 31 (79.49) | ||
| Combination | 0 (0.00) | 3 (100.00) | ||
| Monthly Internet cost (in BDT) | ||||
| Less than 500 | 31 (13.14) | 205 (86.86) | 0.30 | 0.860 |
| 500–1000 | 67 (12.01) | 491 (87.99) | ||
| More than 1000 | 21 (13.29) | 137 (86.71) | ||
| Notification of online class schedule received | ||||
| On the same day | 35 (14.40) | 208 (85.60) | 1.99 | 0.370 |
| 1 day before | 67 (12.52) | 468 (87.48) | ||
| 2 or more days before | 17 (9.77) | 157 (90.23) | ||
| Being assessed at the end of each class | ||||
| Yes | 79 (14.82) | 454 (85.18) | 5.97 | 0.015 |
| No | 40 (9.55) | 379 (90.45) | ||
| Availability of online LMS or Institutional Website | ||||
| Available | 68 (20.00) | 272 (80.00) | 27.20 | 0.000 |
| Unavailable | 51 (8.33) | 561 (91.67) | ||
| All key information about the course is available on learning management system | ||||
| Available | 59 (19.87) | 238 (80.13) | 21.41 | 0.000 |
| Unavailable | 60 (9.16) | 595(90.84) | ||
| Students are assisted in overcoming obstacles in accessing the classes or materials? | ||||
| Yes | 76 (20.32) | 298 (79.68) | 34.45 | 0.000 |
| No | 43 (7.44) | 535 (92.56) | ||
| Time allotted for online classes is sufficient? | ||||
| Yes | 93 (17.78) | 430 (82.22) | 29.61 | 0.000 |
| No | 26 (6.06) | 403 (93.94) | ||
| Student–teacher interaction during or after classes | ||||
| Interactive | 85 (17.75) | 394 (82.25) | 24.25 | 0.000 |
| Not interactive | 34 (7.19) | 439 (92.81) | ||
| Factors | Crude OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Gender | ||
| Male | Ref. | Ref. |
| Female | 1.76 (1.17, 2.64) | 1.82 (1.19, 2.80) |
| Assessment at the end of each class | ||
| Yes | Ref. | Ref. |
| No | 1.65 (1.10, 2.47) | 1.08 (0.69, 1.67) |
| OLMS (availability of online LMS or institutional website) | ||
| Yes | Ref. | Ref. |
| No | 2.75 (1.86, 4.07) | 1.97 (1.14, 3.41) |
| All key information about the course is available in OLMS | ||
| Yes | Ref. | Ref. |
| No | 2.46 (1.67, 3.63) | 0.94 (0.53, 1.65) |
| Assistance with overcoming obstacles to accessing classes or materials | ||
| Yes | Ref. | Ref. |
| No | 3.17 (2.13, 4.73) | 1.78 (1.12, 2.80) |
| Time allotted for online classes sufficient? | ||
| Yes | Ref. | Ref. |
| No | 3.35 (2.13, 5.29) | 2.11 (1.28, 3.46) |
| Interaction with teacher (during + after class) | ||
| Yes | Ref. | Ref. |
| No | 2.79 (1.83, 4.24) | 1.62 (1.02, 2.59) |
| Model performance test | ||
| McFadden’s R2: 0.074 | ||
| Goodness-of-fit test statistic (p-value): 139.31 (0.97) | ||
| Link test: 1.94 *** | ||
| Area under the ROC curve: 0.7241 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Islam, M.I.; Jahan, S.S.; Chowdhury, M.T.H.; Isha, S.N.; Saha, A.K.; Nath, S.K.; Jahan, M.S.; Kabir, M.H.; Hoque Apu, E.; Kabir, R.; et al. Experience of Bangladeshi Dental Students towards Online Learning during the COVID-19 Pandemic: A Web-Based Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 7786. https://doi.org/10.3390/ijerph19137786
Islam MI, Jahan SS, Chowdhury MTH, Isha SN, Saha AK, Nath SK, Jahan MS, Kabir MH, Hoque Apu E, Kabir R, et al. Experience of Bangladeshi Dental Students towards Online Learning during the COVID-19 Pandemic: A Web-Based Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(13):7786. https://doi.org/10.3390/ijerph19137786
Chicago/Turabian StyleIslam, Md Irteja, Shah Saif Jahan, Mohammad Tawfique Hossain Chowdhury, Samia Naz Isha, Arup Kumar Saha, Sujan Kanti Nath, Mohammed Shahed Jahan, Md. Humayun Kabir, Ehsanul Hoque Apu, Russell Kabir, and et al. 2022. "Experience of Bangladeshi Dental Students towards Online Learning during the COVID-19 Pandemic: A Web-Based Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 13: 7786. https://doi.org/10.3390/ijerph19137786







