Factors Exacerbating Clinical Symptoms and CT Findings in Patients with Medication-Related Osteonecrosis of the Jaw Receiving Conservative Therapy: A Multicenter Retrospective Study of 53 Cases
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. Conservative Treatment
2.3. Variables
2.4. Outcome
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. The Outcome of Clinical and Imaging Findings and Comprehensive Treatment Outcome
3.3. Factors Related to Clinical Findings and Imaging Findings
3.4. Factors Related to Comprehensive Treatment Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ruggiero, S.L.; Dodson, T.B.; Fantasia, J.; Goodday, R.; Aghaloo, T.; Mehrotra, B.; O’Ryan, F.; American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons Position Paper on medication-related osteonecrosis of the jaw—2014 update. J. Oral Maxillofac. Surg. 2014, 72, 1938–1956. [Google Scholar] [CrossRef] [PubMed]
- Yoneda, T.; Hagino, H.; Sugimoto, T.; Ohta, H.; Takahashi, S.; Soen, S.; Taguchi, A.; Nagata, T.; Urade, M.; Shibahara, T.; et al. Antiresorptive agent-related osteonecrosis of the jaw: Position Paper 2017 of the Japanese Allied Committee on Osteonecrosis of the Jaw. J. Bone Miner. Metab. 2017, 35, 6–19. [Google Scholar] [CrossRef] [PubMed]
- Yarom, N.; Shapiro, C.L.; Peterson, D.E.; Van Poznak, C.H.; Bohlke, K.; Ruggiero, S.L.; Migliorati, C.A.; Khan, A.; Morrison, A.; Anderson, H.; et al. Medication-related osteonecrosis of the jaw: MASCC/ISOO/ASCO Clinical Practice Guideline. J. Clin. Oncol. 2019, 37, 2270–2290. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, S.L.; Dodson, T.B.; Aghaloo, T.; Carlson, E.R.; Ward, B.B.; Kademani, D. American Association of Oral and Maxillofacial Surgeons’ Position Paper on Medication-Related Osteonecrosis of the Jaws—2022 Update. J. Oral Maxillofac. Surg. 2022, 80, 920–943. [Google Scholar] [CrossRef] [PubMed]
- Rupel, K.; Ottaviani, G.; Gobbo, M.; Contardo, L.; Tirelli, G.; Vescovi, P.; Lenarda, R.D.; Biasotto, M. A systematic review of therapeutical approaches in bisphosphonate-related osteonecrosis of the jaw (BRONJ). Oral Oncol. 2014, 50, 1049–1057. [Google Scholar] [CrossRef]
- Fliefel, R.; Tröltzsch, M.; Kühnisch, J.; Ehrenfeld, M.; Otto, S. Treatment strategies and outcomes of bisphosphonate-related osteonecrosis of the jaw (BRONJ) with characterization of patients: A systematic review. Int. J. Oral Maxillofac. Surg. 2015, 44, 568–585. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, S.L.; Kohn, N. Disease stage and mode of therapy are important determinants of treatment outcomes for medication-related osteonecrosis of the jaw. J. Oral Maxillofac. Surg. 2015, 73, S94–S100. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.Y.; Lee, S.J.; Kim, S.M.; Myoung, H.; Hwang, S.J.; Choi, J.Y.; Lee, J.H.; Choung, P.H.; Kim, M.J.; Seo, B.M. Extensive surgical procedures result in better treatment outcomes for bisphosphonate-related osteonecrosis of the jaw in patients with osteoporosis. J. Oral Maxillofac. Surg. 2017, 75, 1404–1413. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayashida, S.; Soutome, S.; Yanamoto, S.; Fujita, S.; Hasegawa, T.; Komori, T.; Kojima, Y.; Miyamoto, H.; Shibuya, Y.; Ueda, N.; et al. Evaluation of the treatment strategies for medication-related osteonecrosis of the jaws (MRONJ) and the factors affecting treatment outcome: A multicenter retrospective study with propensity score matching analysis. J. Bone Min. Res. 2017, 32, 2022–2029. [Google Scholar] [CrossRef] [Green Version]
- Lerman, M.A.; Xie, W.; Treister, N.S.; Richardson, P.G.; Weller, E.A.; Woo, S.B. Conservative management of bisphosphonate-related osteonecrosis of the jaws: Staging and treatment outcomes. Oral Oncol. 2013, 49, 977–983. [Google Scholar] [CrossRef] [PubMed]
- Marx, R.E.; Sawatari, Y.; Fortin, M.; Broumand, V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: Risk factors, recognition, prevention, and treatment. J. Oral Maxillofac. Surg. 2005, 63, 1567–1575. [Google Scholar] [CrossRef] [PubMed]
- Lazarovici, T.S.; Yahalom, R.; Taicher, S.; Elad, S.; Hardan, I.; Yarom, N. Bisphosphonate-related osteonecrosis of the jaws: A single-center study of 101 patients. J. Oral Maxillofac. Surg. 2009, 67, 850–855. [Google Scholar] [CrossRef] [PubMed]
- Freiberger, J.J.; Padilla-Burgos, R.; Chhoeu, A.H.; Kraft, K.H.; Boneta, O.; Moon, R.E.; Piantadosi, C.A. Hyperbaric oxygen treatment and bisphosphonate-induced osteonecrosis of the jaw: A case series. J. Oral Maxillofac. Surg. 2007, 65, 1321–1327. [Google Scholar] [CrossRef] [PubMed]
- Freiberger, J.J.; Padilla-Burgos, R.; McGraw, T.; Suliman, H.B.; Kraft, K.H.; Stolp, B.W.; Moon, R.E.; Piantadosi, C.A. What is the role of hyperbaric oxygen in the management of bisphosphonate-related osteonecrosis of the jaw: A randomized controlled trial of hyperbaric oxygen as an adjunct to surgery and antibiotics. J. Oral Maxillofac. Surg. 2012, 70, 1573–1583. [Google Scholar] [CrossRef] [PubMed]
- Agrillo, A.; Ungari, C.; Filiaci, F.; Priore, P.; Iannetti, G. Ozone therapy in the treatment of avascular bisphosphonate-related jaw osteonecrosis. J. Craniofac Surg. 2007, 18, 1071–1075. [Google Scholar] [CrossRef]
- Petrucci, M.T.; Gallucci, C.; Agrillo, A.; Mustazza, M.C.; Foà, R. Role of ozone therapy in the treatment of osteonecrosis of the jaws in multiple myeloma patients. Haematologica 2007, 92, 1289–1290. [Google Scholar] [CrossRef] [Green Version]
- Agrillo, A.; Filiaci, F.; Ramieri, V.; Riccardi, E.; Quarato, D.; Rinna, C.; Gennaro, P.; Cascino, F.; Mitro, V.; Ungari, C. Bisphosphonate-related osteonecrosis of the jaw (BRONJ): 5 year experience in the treatment of 131 cases with ozone therapy. Eur. Rev. Med. Pharm. Sci. 2012, 16, 1741–1747. [Google Scholar]
- Favia, G.; Tempesta, A.; Limongelli, L.; Crincoli, V.; Maiorano, E. Medication-related osteonecrosis of the jaw: Surgical or non-surgical treatment? Oral Dis. 2018, 24, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Romeo, U.; Galanakis, A.; Marias, C.; Vecchio, A.D.; Tenore, G.; Palaia, G.; Vescovi, P.; Polimeni, A. Observation of pain control in patients with bisphosphonate-induced osteonecrosis using low level laser therapy: Preliminary results. Photomed. Laser Surg. 2011, 29, 447–452. [Google Scholar] [CrossRef]
- Scoletta, M.; Arduino, P.G.; Reggio, L.; Dalmasso, P.; Mozzati, M. Effect of low-level laser irradiation on bisphosphonate-induced osteonecrosis of the jaws: Preliminary results of a prospective study. Photomed. Laser Surg. 2010, 28, 179–184. [Google Scholar] [CrossRef] [Green Version]
- Vescovi, P.; Merigo, E.; Meleti, M.; Manfredi, M.; Guidotti, R.; Nammour, S. Bisphosphonates-related osteonecrosis of the jaws: A concise review of the literature and a report of a single-centre experience with 151 patients. J. Oral Pathol. Med. 2012, 41, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Atalay, B.; Yalcin, S.; Emes, Y.; Aktas, I.; Aybar, B.; Issever, H.; Mandel, N.M.; Cetin, O.; Oncu, B. Bisphosphonate-related osteonecrosis: Laser-assisted surgical treatment or conventional surgery? Lasers Med. Sci. 2011, 26, 815–823. [Google Scholar] [CrossRef] [PubMed]
- Angiero, F.; Sannino, C.; Borloni, R.; Crippa, R.; Benedicenti, S.; Romanos, G.E. Osteonecrosis of the jaws caused by bisphosphonates: Evaluation of a new therapeutic approach using the Er:YAG laser. Lasers Med. Sci. 2009, 24, 849–856. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.W.; Kim, S.J.; Kim, M.R. Leucocyte-rich and platelet-rich fibrin for the treatment of bisphosphonate-related osteonecrosis of the jaw: A prospective feasibility study. Br. J. Oral Maxillofac. Surg. 2014, 52, 854–859. [Google Scholar] [CrossRef]
- Giudice, A.; Barone, S.; Giudice, C.; Bennardo, F.; Fortunato, L. Can platelet-rich fibrin improve healing after surgical treatment of medication-related osteonecrosis of the jaw? A pilot study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 126, 390–403. [Google Scholar] [CrossRef] [PubMed]
- Longo, F.; Guida, A.; Aversa, C.; Pavone, E.; Di Costanzo, G.; Ramaglia, L.; Ionna, F. Platelet rich plasma in the treatment of bisphosphonate-related osteonecrosis of the jaw: Personal experience and review of the literature. Int. J. Dent. 2014, 2014, 298945. [Google Scholar] [CrossRef] [Green Version]
- Dincă, O.; Zurac, S.; Stăniceanu, F.; Bucur, M.B.; Bodnar, D.C.; Vlădan, C.; Bucur, A. Clinical and histopathological studies using fibrin-rich plasma in the treatment of bisphosphonate-related osteonecrosis of the jaw. Rom. J. Morphol. Embryol. 2014, 55, 961–964. [Google Scholar]
- Nørholt, S.E.; Hartlev, J. Surgical treatment of osteonecrosis of the jaw with the use of platelet-rich fibrin: A prospective study of 15 patients. Int. J. Oral Maxillofac. Surg. 2016, 45, 1256–1260. [Google Scholar] [CrossRef]
- Pelaz, A.; Junquera, L.; Gallego, L.; Garcia-Consuegra, L.; Junquera, S.; Gomez, C. Alternative treatments for oral bisphosphonate-related osteonecrosis of the jaws: A pilot study comparing fibrin rich in growth factors and teriparatide. Med. Oral Patol. Oral Cir. Bucal. 2014, 19, e320–e326. [Google Scholar] [CrossRef]
- Kim, K.M.; Park, W.; Oh, S.Y.; Kim, H.J.; Nam, W.; Lim, S.K.; Rhee, Y.; Cha, I.H. Distinctive role of 6-month teriparatide treatment on intractable bisphosphonate-related osteonecrosis of the jaw. Osteoporos. Int. 2014, 25, 1625–1632. [Google Scholar] [CrossRef]
- Mauceri, R.; Panzarella, V.; Maniscalco, L.; Bedogni, A.; Licata, M.E.; Albanese, A.; Toia, F.; Cumbo, E.M.G.; Mazzola, G.; Di Fede, O.; et al. Conservative surgical treatment of bisphosphonate-related osteonecrosis of the jaw with Er,Cr:YSGG laser and platelet-rich plasma: A longitudinal study. BioMed Res. Int. 2018, 2018, 3982540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merigo, E.; Cella, L.; Oppici, A.; Cristina Arbasi, M.; Clini, F.; Fontana, M.; Fornaini, C. Combined approach to treat medication-related osteonecrosis of the jaws. J. Lasers Med. Sci. 2018, 9, 92–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.H.; Kim, J.W.; Kim, S.J. Does the addition of bone morphogenetic protein 2 to platelet-rich fibrin improve healing after treatment for medication-related osteonecrosis of the jaw? J. Oral Maxillofac. Surg. 2017, 75, 1176–1184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayashida, S.; Yanamoto, S.; Fujita, S.; Hasegawa, T.; Komori, T.; Kojima, Y.; Miyamoto, H.; Shibuya, Y.; Ueda, N.; Kirita, T.; et al. Drug holiday clinical relevance verification for antiresorptive agents in medication-related osteonecrosis cases of the jaw. J. Bone Miner. Metab. 2020, 38, 126–134. [Google Scholar] [CrossRef]
- Ida, M.; Tetsumura, A.; Kurabayashi, T.; Sasaki, T. Periosteal new bone formation in the jaws. A computed tomographic study. DentoMaxillofac. Radiol. 1997, 6, 169–176. [Google Scholar] [CrossRef]
- Suei, Y. Radiographic findings of bisphosphonate-related osteomyelitis of the jaw: Investigation of the diagnostic points by comparison with radiation osteomyelitis, suppurative osteomyelitis, and diffuse sclerosing osteomyelitis. Oral Radiol. 2013, 29, 121–134. [Google Scholar] [CrossRef]
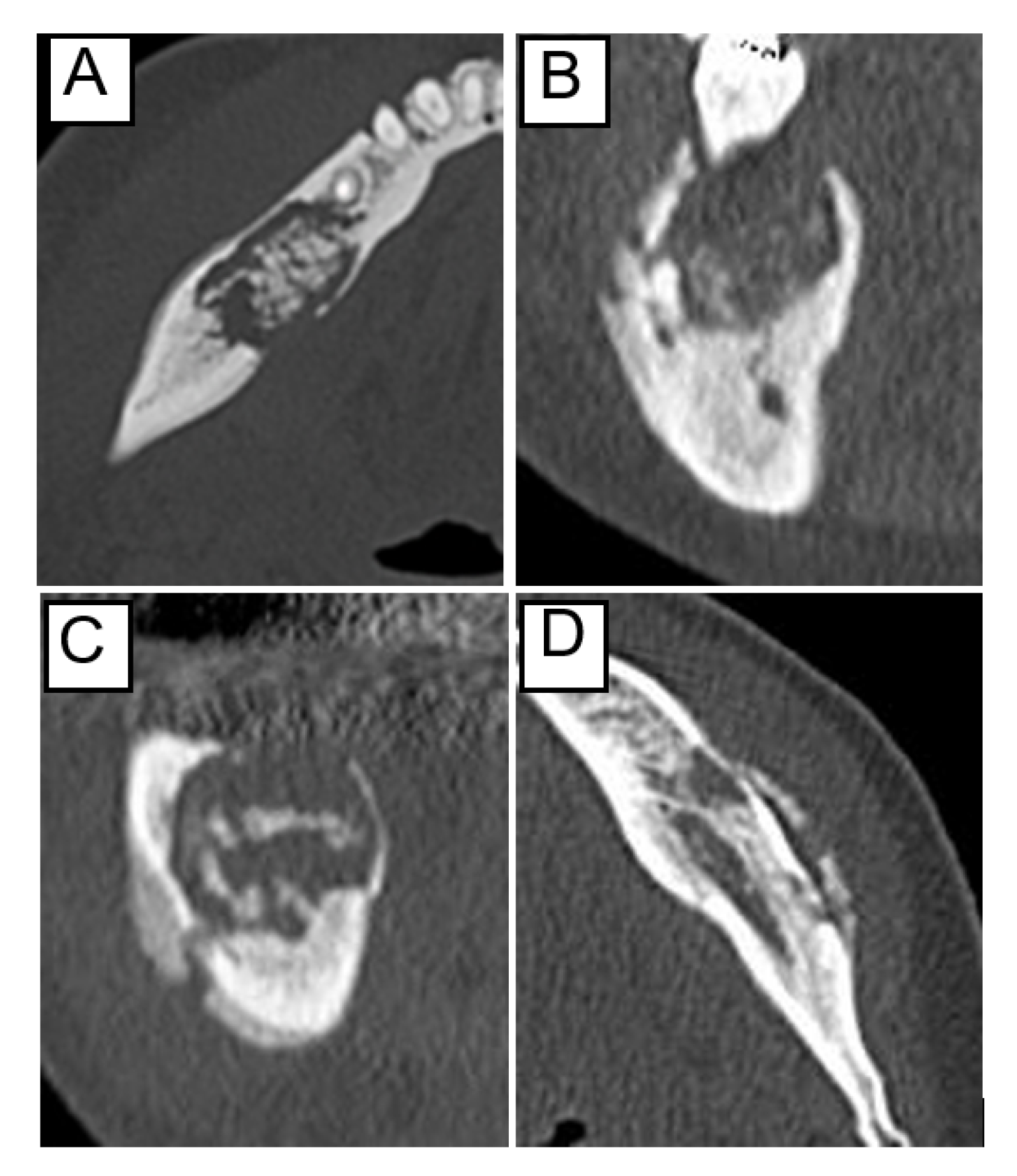
- Kojima, Y.; Kawaoka, Y.; Sawada, S.; Hayashida, S.; Okuyama, K.; Yutori, H.; Kawakita, A.; Ishida, S.; Soutome, S.; Yanamoto, S.; et al. Clinical significance of periosteal reaction as a predictive factor for treatment outcome of medication-related osteonecrosis of the jaw. J. Bone Miner. Metab. 2019, 37, 913–919. [Google Scholar] [CrossRef]
- Soutome, S.; Yanamoto, S.; Sumi, M.; Hayashida, S.; Kojima, Y.; Sawada, S.; Rokutanda, S.; Iwai, H.; Saito, T.; Umeda, M. Effect of periosteal reaction in medication-related osteonecrosis of the jaw on treatment outcome after surgery. J. Bone Miner. Metab. 2021, 39, 302–310. [Google Scholar] [CrossRef]
- Soutome, S.; Otsuru, M.; Hayashida, S.; Yanamoto, S.; Sasaki, M.; Takagi, Y.; Sumi, M.; Kojima, Y.; Sawada, S.; Iwai, H.; et al. Periosteal reaction of medication-related osteonecrosis of the jaw (MRONJ): Clinical significance and changes during conservative therapy. Support. Care Cancer 2021, 29, 6361–6368. [Google Scholar] [CrossRef]
- Soutome, S.; Otsuru, M.; Murata, M.; Morishita, K.; Omori, K.; Suyama, K.; Hayashida, S.; Umeda, M.; Saito, T. Risk factors for developing medication-related osteonecrosis of the jaw when preserving the tooth that can be a source of infection in cancer patients receiving high-dose antiresorptive agents: A retrospective study. Support. Care Cancer 2022. online ahead of print. [Google Scholar] [CrossRef]
- Soutome, S.; Otsuru, M.; Hayashida, S.; Murata, M.; Yanamoto, S.; Sawada, S.; Kojima, Y.; Funahara, M.; Iwai, H.; Umeda, M.; et al. Relationship between tooth extraction and development of medication-related osteonecrosis of the jaw in cancer patients. Sci. Rep. 2021, 11, 17226. [Google Scholar] [CrossRef] [PubMed]

| Variable | Number of Patient/Mean ± SD | |
|---|---|---|
| Sex | male | 18 |
| female | 35 | |
| Age | (years) | 74.9 ± 11.9 |
| Jaw | upper jaw | 10 |
| lower jaw | 43 | |
| Site | anterior | 5 |
| posterior | 34 | |
| anteroposterior | 14 | |
| Stage | stage 1 | 9 |
| stage 2 | 30 | |
| stage 3 | 14 | |
| Antiresorptive agent | bisphosphonate | 32 |
| alendronate | 11 | |
| zoledronate | 18 | |
| minodronate | 1 | |
| risedronate | 2 | |
| denosumab | 16 | |
| both | 5 | |
| alendronate + denosumab | 1 | |
| zoledronate + denosumab | 4 | |
| Primary disease | osteoporosis | 20 |
| malignant tumor | 33 | |
| Administration period of antiresorptive agent | (months) | 47.0 ± 33.9 |
| <4 years | 29 | |
| ≥4 years | 24 | |
| Drug holiday during treatment | (−) | 12 |
| (+) | 36 | |
| unknown | 5 | |
| Corticosteroid | (−) | 42 |
| (+) | 11 | |
| Diabetes | (−) | 43 |
| (+) | 10 | |
| Leukocytes | (/μ) | 6920 ± 2691 |
| Albumin | (g/dL) | 3.75 ± 0.567 |
| Creatinine | (mg/dL) | 1.06 ± 0.540 |
| Separation of sequestrum | (−) | 41 |
| (+) | 12 | |
| Osteolytic lesion | above the mandibular canal | 34 |
| including mandibular canal | 19 | |
| Periosteal reaction | (−) | 34 |
| (+) | 19 | |
| Observation period | days | 729 ± 494 |
| Total | 53 patients |
| Treatment Outcome | Number of Patients | Observation (Mean) | |
|---|---|---|---|
| Clinical symptoms | Healing | 8 | 249–1447 days (731) |
| Improvement | 7 | 149–1163 days (462) | |
| No change | 32 | 147–1955 days (759) | |
| Worsening | 6 | 111–1432 days (884) | |
| Osteolytic lesion on CT image | Disappearance | 0 | - |
| Reduction | 2 | 320–644 days (482) | |
| No change | 34 | 111–1819 days (650) | |
| Enlargement | 17 | 160–1955 days (917) | |
| Comprehensive treatment outcome | Success | 12 | 149–1447 days (592) |
| Failure | 41 | 111–1955 days (770) | |
| Total | 53 | 111–1955 days (729) | |
| Variable | Clinical Symptoms | Osteolytic Lesion of CT Image | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Number of Patient/Mean ± SD | Odd Ratio | p-Value | Number of Patient/Mean ± SD | Odd Ratio | p-Value | ||||
| Healing/Improvement | No Change/Worsening | Disappearance/Reduction/No Change | Enlargement | ||||||
| Sex | male | 7 | 11 | 1.000 | 0.334 | 10 | 8 | 1.000 | 0.218 |
| female | 8 | 27 | 0.296 | 26 | 9 | 2.311 | |||
| Age | (years) | 76.1 ± 11.8 | 74.4 ± 12.0 | 1.024 | 0.649 | 76.1 ± 11.5 | 72.2 ± 12.6 | 1.028 | 0.272 |
| Jaw | upper jaw | 2 | 8 | 1.000 | 0.706 | 8 | 2 | 1.000 | 0.471 |
| lower jaw | 13 | 30 | 2.143 | 28 | 15 | 0.467 | |||
| Site | anterior | 2 | 3 | 1.000 | 0.614 | 3 | 2 | 1.000 | 0.651 |
| posterior/anteroposterior | 13 | 35 | 0.557 | 33 | 15 | 1.457 | |||
| Stage | stage 1–2 | 5 | 4 | 1.000 | 0.096 | 27 | 12 | 1.000 | 0.776 |
| stage 3 | 2 | 12 | 0.487 | 9 | 5 | 0.800 | |||
| Antiresorptive agent | bisphosphonate | 9 | 23 | 1.000 | 1.000 | 21 | 11 | 1.000 | 0.768 |
| denosumab or both | 6 | 15 | 1.100 | 15 | 6 | 1.310 | |||
| Primary disease | osteoporosis | 6 | 14 | 1.000 | 1.000 | 16 | 4 | 1.000 | 0.225 |
| malignant tumor | 9 | 24 | 1.167 | 29 | 13 | 0.385 | |||
| Administration period | (months) | 40.9 ± 32.7 | 49.2 ± 34.4 | 0.990 | 0.454 | 51.1 ± 37.8 | 38.7 ± 22.5 | 1.013 | 0.234 |
| <4 years | 9 | 20 | 1.000 | 0.762 | 17 | 12 | 1.000 | 0.145 | |
| ≥4 years | 6 | 18 | 0.545 | 19 | 5 | 2.682 | |||
| Drug holiday during treatment | (−) | 4 | 8 | 1.000 | 0.331 | 24 | 12 | 1.000 | 0.800 |
| (+) | 11 | 25 | 1.000 | 9 | 3 | 1.500 | |||
| unknown | 0 | 5 | 3 | 2 | |||||
| Corticosteroid | (−) | 11 | 31 | 1.000 | 0.708 | 29 | 13 | 1.000 | 0.730 |
| (+) | 4 | 7 | 2.083 | 7 | 4 | 0.784 | |||
| Diabetes | (−) | 12 | 31 | 1.000 | 1.000 | 30 | 13 | 1.000 | 0.709 |
| (+) | 3 | 7 | 0.888 | 6 | 4 | 0.650 | |||
| Leukocytes | (/μ) | 7433 ± 2491 | 6728 ± 2775 | 1.000 | 0.446 | 7116 ± 3157 | 6500 ± 1202 | 1.000 | 0.486 |
| Albumin | (g/dL) | 3.76 ± 0.520 | 3.75 ± 0.591 | 0.696 | 0.995 | 3.74 ± 0.523 | 3.77 ± 0.664 | 0.917 | 0.887 |
| Creatinine | (mg/dL) | 0.947 ± 0.290 | 1.11 ± 0.606 | 1.237 | 0.383 | 1.05 ± 0.527 | 1.10 ± 0.587 | 0.837 | 0.769 |
| Separation of sequestrum | (−) | 9 | 32 | 1.000 | 0.076 | 25 | 16 | 1.000 | 0.077 |
| (+) | 6 | 6 | 2.727 | 11 | 1 | 7.040 | |||
| Osteolytic lesion | localized | 9 | 25 | 1.000 | 0.756 | 23 | 11 | 1.000 | 1.000 |
| extended | 6 | 13 | 1.400 | 13 | 6 | 1.036 | |||
| Periosteal reaction | (−) | 13 | 21 | 1.000 | 0.055 | 28 | 6 | 1.000 | 0.005 |
| (+) | 2 | 17 | 0.431 | 8 | 11 | 0.156 | |||
| Variable | Comprehensive Treatment Outcome | ||||
|---|---|---|---|---|---|
| Number of Patient/Mean ± SD | Odd Ratio | p-Value | |||
| Success | Failure | ||||
| Sex | male | 5 | 13 | 1.000 | 0.730 |
| female | 7 | 28 | 0.650 | ||
| Age | (years) | 75.2 ± 12.6 | 74.8 ± 11.8 | 1.003 | 0.922 |
| Jaw | upper jaw | 2 | 8 | 1.000 | 1.000 |
| lower jaw | 10 | 33 | 1.212 | ||
| Site | anterior | 2 | 3 | 1.000 | 0.315 |
| posterior/anteroposterior | 10 | 38 | 0.395 | ||
| Stage | stage 1–2 | 10 | 29 | 1.000 | 0.480 |
| stage 3 | 2 | 12 | 0.483 | ||
| Antiresorptive agent | bisphosphonate | 6 | 26 | 1.000 | 0.507 |
| denosumab or both | 6 | 15 | 1.733 | ||
| Primary disease | osteoporosis | 4 | 16 | 1.000 | 1.000 |
| malignant tumor | 8 | 25 | 1.280 | ||
| Administration period | (months) | 39.6 ± 35.3 | 49.2 ± 33.6 | 0.417 | |
| <4 years | 7 | 22 | 1.000 | 1.000 | |
| ≥4 years | 5 | 19 | 0.972 | ||
| Drug holiday during treatment | (−) | 8 | 28 | 1.000 | 0.434 |
| (+) | 4 | 8 | 2.063 | ||
| unknown | 0 | 5 | |||
| Corticosteroid | (−) | 9 | 33 | 1.000 | 0.697 |
| (+) | 3 | 8 | 1.375 | ||
| Diabetes | (−) | 11 | 32 | 1.000 | 0.423 |
| (+) | 1 | 9 | 0.323 | ||
| Leukocytes | (/μ) | 7459 ± 2648 | 6761 ± 2722 | 1.000 | 0.478 |
| Albumin | (g/dL) | 3.70 ± 0.480 | 3.77 ± 0.595 | 0.802 | 0.752 |
| Creatinine | (mg/dL) | 0.936 ± 0.302 | 1.10 ± 0.591 | 0.469 | 0.399 |
| Separation of sequestrum | (−) | 7 | 34 | 1.000 | 0.114 |
| (+) | 5 | 7 | 3.469 | ||
| Osteolytic lesion | localized | 7 | 27 | 1.000 | 0.735 |
| extended | 5 | 14 | 1.378 | ||
| Periosteal reaction | (−) | 11 | 23 | 1.000 | 0.038 |
| (+) | 1 | 18 | 0.116 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kojima, Y.; Soutome, S.; Otsuru, M.; Hayashida, S.; Sakamoto, Y.; Sawada, S.; Umeda, M. Factors Exacerbating Clinical Symptoms and CT Findings in Patients with Medication-Related Osteonecrosis of the Jaw Receiving Conservative Therapy: A Multicenter Retrospective Study of 53 Cases. Int. J. Environ. Res. Public Health 2022, 19, 7854. https://doi.org/10.3390/ijerph19137854
Kojima Y, Soutome S, Otsuru M, Hayashida S, Sakamoto Y, Sawada S, Umeda M. Factors Exacerbating Clinical Symptoms and CT Findings in Patients with Medication-Related Osteonecrosis of the Jaw Receiving Conservative Therapy: A Multicenter Retrospective Study of 53 Cases. International Journal of Environmental Research and Public Health. 2022; 19(13):7854. https://doi.org/10.3390/ijerph19137854
Chicago/Turabian StyleKojima, Yuka, Sakiko Soutome, Mitsunobu Otsuru, Saki Hayashida, Yuki Sakamoto, Shunsuke Sawada, and Masahiro Umeda. 2022. "Factors Exacerbating Clinical Symptoms and CT Findings in Patients with Medication-Related Osteonecrosis of the Jaw Receiving Conservative Therapy: A Multicenter Retrospective Study of 53 Cases" International Journal of Environmental Research and Public Health 19, no. 13: 7854. https://doi.org/10.3390/ijerph19137854
APA StyleKojima, Y., Soutome, S., Otsuru, M., Hayashida, S., Sakamoto, Y., Sawada, S., & Umeda, M. (2022). Factors Exacerbating Clinical Symptoms and CT Findings in Patients with Medication-Related Osteonecrosis of the Jaw Receiving Conservative Therapy: A Multicenter Retrospective Study of 53 Cases. International Journal of Environmental Research and Public Health, 19(13), 7854. https://doi.org/10.3390/ijerph19137854






