Neighborhood Disadvantage and Poor Health: The Consequences of Race, Gender, and Age among Young Adults
Abstract
:1. Introduction
1.1. Background and Theory
1.2. Neighborhoods, Race, Gender and Health
1.3. Neighborhood Disadvantage and Health in Young Adulthood
1.4. Summary and Hypotheses
2. Materials and Methods
2.1. Sample
2.2. Measures
2.3. Analytic Strategy
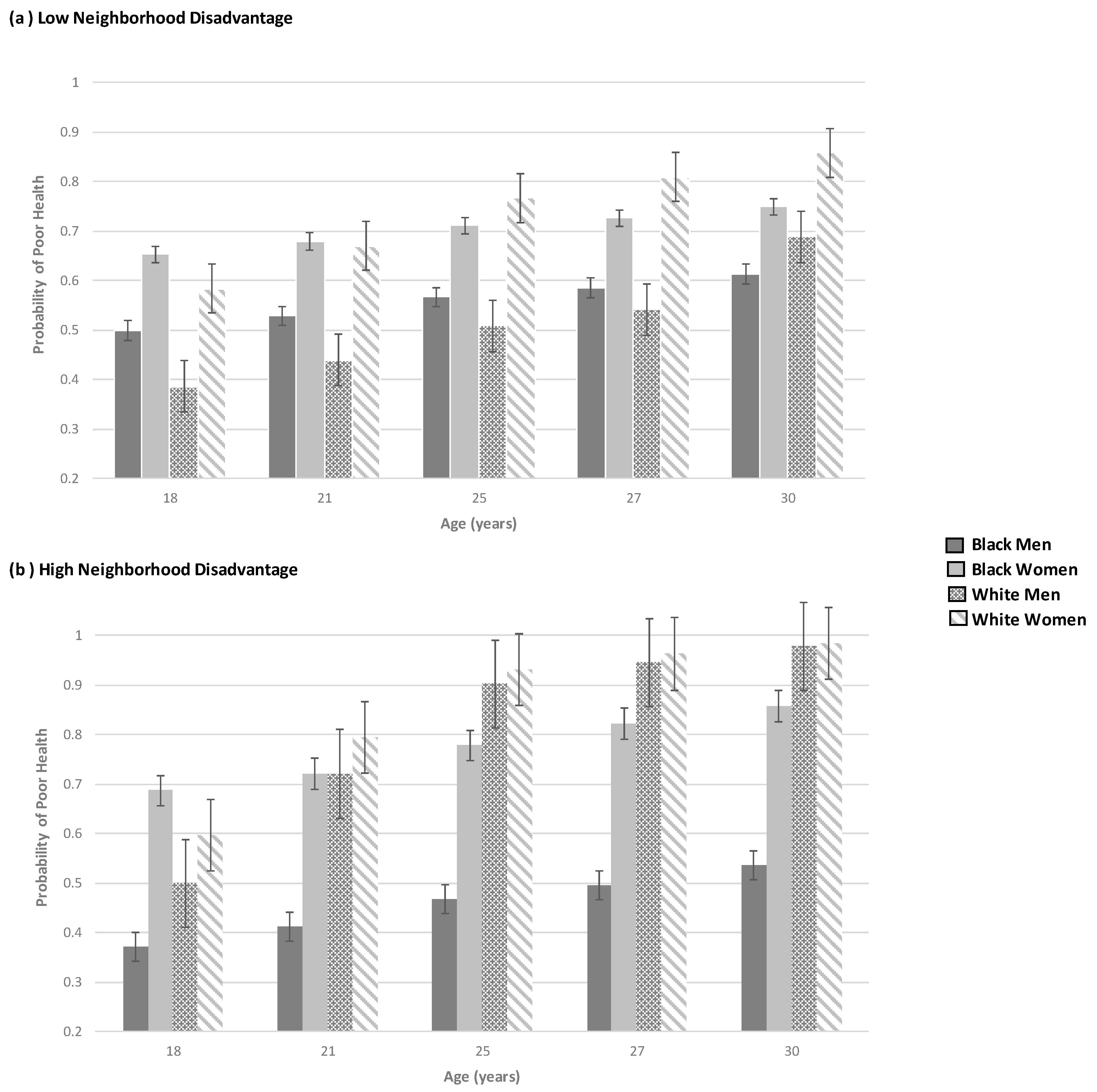
3. Results
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rodrigues, E.D.; César, C.C.; Xavier, C.C.; Caiaffa, T.W.; Proietti, A.F. Exploring neighborhood socioeconomic disparity in self-rated health: A multiple mediation analysis. Prev. Med. 2021, 45, 106443. [Google Scholar] [CrossRef] [PubMed]
- Ross, C.E.; Mirowsky, J. Neighborhood disadvantage, disorder, and health. J. Health Soc. Behav. 2001, 1, 258–276. [Google Scholar] [CrossRef] [Green Version]
- Tung, E.L.; Peek, M.E.; Rivas, M.A.; Yang, J.P.; Volerman, A. Association of neighborhood disadvantage with racial disparities in COVID-19 positivity in Chicago. Health Affairs. 2021, 40, 1784–1791. [Google Scholar] [CrossRef]
- Cohen, D.A.; Mason, K.; Bedimo, A.; Scribner, R.; Basolo, V.; Farley, T.A. Neighborhood physical conditions and health. Am. J. Public Health 2003, 93, 467–471. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.F.; Ang, A.; Pebley, A.R. The relationship between neighborhood characteristics and self-rated health for adults with chronic conditions. Am. J. Public Health 2007, 97, 926–932. [Google Scholar] [CrossRef] [PubMed]
- Green, K.M.; Matson, P.A.; Reboussin, B.A.; Milam, A.J.; Furr-Holden, C.D.M.; Rabinowitz, J.A.; Powell, T.W.; Ialongo, N.S. Individual and neighborhood factors associated with sexual behavior classes in an urban longitudinal sample. Sex. Transm. Dis. 2019, 46, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.D.; Lawrence, K.G.; Bodkin, M.R.; Kwok, R.K.; Engel, L.S.; Sandler, D.P. Neighborhood deprivation, obesity, and diabetes in residents of the U.S. gulf coast. Am. J. Epidemiol. 2021, 190, 295–304. [Google Scholar] [CrossRef]
- U.S. Census Bureau. American Community Survey 5-Year Data (2009–2020). 2022. Available online: https://www.census.gov/data/developers/data-sets/acs-5year.html (accessed on 1 February 2022).
- Firebaugh, G.; Acciai, F. For blacks in America, the gap in neighborhood poverty has declined faster than segregation. Proc. Natl. Acad. Sci. USA 2016, 113, 13372–13377. [Google Scholar] [CrossRef] [Green Version]
- National Equity Atlas. Neighborhood Poverty: All Neighborhoods Should be Communities of Opportunity. 2019. Available online: https://nationalequityatlas.org/indicators/Neighborhood_poverty# (accessed on 25 May 2022).
- Baker, R.S.; O’Connell, H.A. Structural racism, family structure, and Black–White inequality: The differential impact of the legacy of slavery on poverty among single mother and married parent households. J. Marriage Fam. 2022. [Google Scholar] [CrossRef]
- Bassett, E.; Moore, S. Gender differences in the social pathways linking neighborhood disadvantage to depressive symptoms in adults. PLoS ONE 2013, 8, e76554. [Google Scholar] [CrossRef] [Green Version]
- Stansfield, R.; Doherty, E. Neighborhood health, social structure and family violence. Soc. Sci. Res. 2019, 81, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, A.M.; St Sauver, J.L.; Finney Rutten, L.J.; Fan, C.; Jacobson, D.J.; Wilson, P.M.; Boyd, C.M.; Rocca, W.A. Associations of neighborhood socioeconomic disadvantage with chronic conditions by age, sex, race, and ethnicity in a population-based cohort. Mayo Clin. Proc. 2022, 97, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Riley, A.; Hawkley, L.C. Racial differences in the effects of neighborhood disadvantage on residential mobility in later life. J. Gerontol. B Psychol. Sci. Soc. Sci. 2016, 71, 1131–1140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simons, R.L.; Lei, M.K.; Klopack, E.; Beach, S.R.H.; Gibbons, F.X.; Philibert, R.A. The effects of social adversity, discrimination, and health risk behaviors on the accelerated aging of African Americans: Further support for the weathering hypothesis. Soc. Sci. Med. 2021, 282, 113169. [Google Scholar] [CrossRef]
- King, C.; Huang, X.; Dewan, N.A. Continuity and change in neighborhood disadvantage and adolescent depression and anxiety. Health Place 2022, 73, 102724. [Google Scholar] [CrossRef]
- Pinchak, N.P.; Swisher, R.R. Neighborhoods, schools, and adolescent violence: Ecological relative deprivation, disadvantage saturation, or cumulative disadvantage? J. Youth Adolesc. 2022, 51, 261–277. [Google Scholar] [CrossRef]
- Roubinov, D.S.; Hagan, M.J.; Boyce, W.T.; Adler, N.E.; Bush, N.R. Family Socioeconomic Status, Cortisol, and Physical Health in Early Childhood: The Role of Advantageous Neighborhood Characteristics. Psychosom. Med. 2018, 80, 492–501. [Google Scholar] [CrossRef]
- Saitadze, I. The effects of neighborhood factors, maternal depression and parental emotional support on social—Behavioral outcomes of children involved in the child welfare system. J. Public Child. Welf. 2022, 16, 249–271. [Google Scholar] [CrossRef]
- Christie-Mizell, C.A.; Leslie, E.T.A.; Hearne, B.N. Self-rated health, discrimination, and racial group identity: The consequences of ethnicity and nativity among black Americans. J. Afr. Am. Stud. 2017, 21, 643–664. [Google Scholar] [CrossRef]
- DeSalvo, K.B.; Bloser, N.; Reynolds, K.; He, J.; Muntner, P. Mortality prediction with a single general self-rated health question. J. Gen. Intern. Med. 2006, 21, 267. [Google Scholar] [CrossRef] [Green Version]
- Nakata, A.; Takahashi, M.; Otsuka, Y.; Swanson, N.G. Is self-rated health associated with blood immune markers in healthy individuals? Int. J. Behav. Med. 2010, 17, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Benjamins, M.R.; Hummer, R.A.; Eberstein, I.W.; Nam, C.B. Self-reported health and adult mortality risk: An analysis of cause-specific mortality. Soc. Sci. Med. 2004, 59, 1297–1306. [Google Scholar] [CrossRef]
- Benyamini, Y.; Blumstein, T.; Lusky, A.; Modan, B. Gender differences in the self-rated health–mortality association: Is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? Gerontologist 2003, 43, 396–405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Idler, E.; Leventhal, H.; Mclaughlin, J.; Leventhal, E. In sickness but not in health: Self-ratings, identity, and mortality. J. Health Soc. Behav. 2004, 45, 336–356. [Google Scholar] [CrossRef] [PubMed]
- Miller, T.R.; Wolinsky, F.D. Self-rated health trajectories and mortality among older adults. J. Gerontol. B Psychol. Sc.i Soc. Sci. 2007, 62, S22–S27. [Google Scholar] [CrossRef] [Green Version]
- Perlman, F.; Bobak, M. Determinants of self rated health and mortality in Russia—Are they the same? Int. J. Equity Health 2008, 7, 19. [Google Scholar] [CrossRef] [Green Version]
- Boynton-Jarrett, R.; Ryan, L.M.; Berkman, L.F.; Wright, R.J. Cumulative violence exposure and self-rated health: Longitudinal study of adolescents in the United States. Pediatrics 2008, 122, 961–970. [Google Scholar] [CrossRef]
- Pusch, S.; Mund, M.; Hagemeyer, B.; Finn, C. Personality development in emerging and young adulthood: A study of age differences. Eur. J. Pers. 2019, 33, 245–263. [Google Scholar] [CrossRef]
- Wood, D.; Crapnell, T.; Lau, L.; Bennett, A.; Lotstein, D.; Ferris, M.; Kuo, A. Emerging adulthood as a critical stage in the life course. In Handbook of Life Course Health Development; Halfon, N., Forrest, C.B., Lerner, R.M., Faustman, E.M., Eds.; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Britton, M.L. Race/ethnicity, attitudes, and living with parents during young adulthood. J. Marriage Fam. 2013, 75, 995–1013. [Google Scholar] [CrossRef]
- Cunningham, M.; Beutel, A.M.; Barber, J.S.; Thornton, A. Reciprocal relationships between attitudes about gender and social contexts during young adulthood. Soc. Sci. Res. 2005, 34, 862–892. [Google Scholar] [CrossRef]
- Tillman, K.H.; Brewster, K.L.; Holway, G.V. Sexual and romantic relationships in young adulthood. Ann. Rev. Soc. 2019, 45, 133–153. [Google Scholar] [CrossRef]
- Pearlin, L.I.; Menaghan, E.G.; Lieberman, M.A.; Mullan, J.T. The stress process. J. Health Soc. Behav. 1981, 22, 337. [Google Scholar] [CrossRef] [PubMed]
- Pearlin, L.I.; Schieman, S.; Fazio, E.M.; Meersman, S.C. Stress, health, and the life course: Some conceptual perspectives. J. Health Soc. Behav. 2005, 46, 205–219. [Google Scholar] [CrossRef] [PubMed]
- Christie-Mizell, C.A.; Erickson, R.J. Mothers and mastery: The consequences of perceived neighborhood disorder. Soc. Psychol. Q. 2007, 70, 340–365. [Google Scholar] [CrossRef]
- Christie-Mizell, C.A.; Steelman, L.C.; Stewart, J. Seeing their surroundings: The effects of neighborhood setting and race on maternal distress. Soc. Sci. Res. 2003, 32, 402–428. [Google Scholar] [CrossRef]
- López, N.; Gadsden, V.L. Health inequities, social determinants, and intersectionality. In NAM Perspectives; National Academy of Medicine: Washington, DC, USA, 2016. [Google Scholar] [CrossRef]
- Malcome, M.L.D.; Fedock, G.; Garthe, R.C.; Golder, S.; Higgins, G.; Logan, T.K. Weathering probation and parole: The protective role of social support on black women’s recent stressful events and depressive symptoms. J. Black Psychol. 2019, 45, 661–688. [Google Scholar] [CrossRef]
- Christie-Mizell, C.A.; Talbert, R.D.; Frazier, C.G.; Rainock, M.R.; Jurinsky, J. Race-gender variation in the relationship between arrest history and poor health from adolescence to adulthood. J. Nat. Med. Assoc. 2022. [Google Scholar] [CrossRef]
- Franks, P.; Gold, M.R.; Fiscella, K. Sociodemographics, self-rated health, and mortality in the US. Soc. Sci. Med. 2003, 56, 2505–2514. [Google Scholar] [CrossRef]
- Loh, V.H.Y.; Rachele, J.N.; Brown, W.J.; Ghani, F.; Turrell, G. Neighborhood disadvantage and physical function: The contributions of neighborhood-level perceptions of safety from crime and walking for recreation. J. Phys. Act. Health 2018, 15, 553–563. [Google Scholar] [CrossRef]
- Zimmerman, G.M.; Messner, S.F. Neighborhood context and the gender gap in adolescent violent crime. Am. Sociol. Rev. 2010, 75, 958–980. [Google Scholar] [CrossRef] [Green Version]
- Eliason, S.R.; Mortimer, J.T.; Vuolo, M. The Transition to Adulthood: Life Course Structures and Subjective Perceptions. Soc. Psychol. Q. 2015, 78, 205–227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, M.K.; Berg, J.A.; Sirotzki, T. Differentiation in self-perceived adulthood: Extending the confluence model of subjective age identity. Soc. Psychol. Q 2007, 70, 243–261. [Google Scholar] [CrossRef]
- Shanahan, M.J. Pathways to adulthood in changing societies: Variability and mechanisms in life course perspective. Ann. Rev. Soc. 2000, 26, 667–692. [Google Scholar] [CrossRef]
- Smith, D.A.; Akira, A.; Hudson, K.; Hudson, A.; Hudson, M.; Mitchell, M.; Crook, E. The effect of health insurance coverage and the doctor-patient relationship on health care utilization in high poverty neighborhoods. Prev. Med. Rep. 2017, 7, 158–161. [Google Scholar] [CrossRef] [PubMed]
- Tsui, J.; Hirsch, J.A.; Bayer, F.J.; Quinn, J.W.; Cahill, J.; Siscovick, D.; Lovasi, G.S. Patterns in Geographic Access to Health Care Facilities Across Neighborhoods in the United States Based on Data From the National Establishment Time-Series Between 2000 and 2014. JAMA Netw. Open 2020, 3, e205105. [Google Scholar] [CrossRef]
- Valdez, Z.; Golash-Boza, T. Towards an intersectionality of race and ethnicity. Ethn. Racial. Stud. 2017, 40, 2256–2261. [Google Scholar] [CrossRef]
- Klostermann, S.; Connell, A.; Stormshak, E.A. Gender differences in the developmental links between conduct problems and depression across early adolescence. J. Res. Adolesc. 2016, 26, 76–89. [Google Scholar] [CrossRef] [Green Version]
- Christie-Mizell, C.A.; Talbert, R.D.; Hope, A.R.; Frazier, C.G.; Hearne, B.N. Depression and African Americans in the first decade of midlife: The consequences of social roles and gender. J. Nat. Med. Assoc. 2019, 111, 285–295. [Google Scholar] [CrossRef]
- Hill, T.D.; Needham, B.L. Rethinking gender and mental health: A critical analysis of three propositions. Soc. Sci. Med. 2013, 92, 83–91. [Google Scholar] [CrossRef]
- Smith, D.T.; Mouzon, D.M.; Elliott, M. Reviewing the assumptions about men’s mental health: An exploration of the gender binary. Am. J. Mens Health 2018, 12, 78–89. [Google Scholar] [CrossRef] [Green Version]
- Moore, W.; Pedlow, S.; Krishnamurty, P.; Wolter, K. National Longitudinal Sample of Youth 1997 (NSLY97): Technical Sampling Report; National Opinion Research Center: Chicago, IL, USA, 2000. [Google Scholar]
- McLeod, J.D.; Uemura, R.; Rohrman, S. Adolescent mental health, behavior problems, and academic achievement. J. Health Soc. Behav. 2012, 53, 482–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas Tobin, C.S.; Erving, C.L.; Hargrove, T.W.; Satcher, L.A. Is the Black-White mental health paradox consistent across age, gender, and psychiatric disorders? Aging Ment. Health 2022, 26, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Omenka, O.I.; Watson, D.P.; Hendrie, H.C. Understanding the healthcare experiences and needs of African immigrants in the United States: A scoping review. BMC Public Health 2020, 20, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patterson, E.J. Incarcerating death: Mortality in U.S. state correctional facilities, 1985–1998. Demography 2010, 47, 587–607. [Google Scholar] [CrossRef] [PubMed]
- Jeffers, J.L. Justice is not blind: Disproportionate incarceration rate of people of color. Soc. Work Public Health 2019, 34, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Fryer, D. Race, reform, & progressive prosecution. J. Crim. Law Criminol. 2020, 110, 769–802. [Google Scholar] [CrossRef]
| Blacks | Whites | |||
|---|---|---|---|---|
| Variables b | Mean/% | Std. | Mean/% | Std. |
| Poor health | 9.96% | –– | 6.29% * | –– |
| Age (years) | 22.55 | 3.06 | 22.47 | 3.04 |
| Female (1 = yes) | 51.80% | –– | 48.77% * | –– |
| Neighborhood disadvantage | 0.36 | 0.68 | 0.17 * | 0.68 |
| Employed (1 = yes) | 59.96% | –– | 72.79% * | –– |
| Married (1 = yes) | 9.59% | –– | 19.04% | –– |
| Parenthood (1 = yes) | 41.67% | –– | 21.95% * | –– |
| College degree or more (1 = yes) | 6.76% | –– | 14.06% * | –– |
| Family income (1 = top fifth) | 9.43% | –– | 21.06% | –– |
| Urban (1 = yes) | 80.42% | –– | 69.02% * | –– |
| South (1 = yes) | 58.80% | –– | 29.67% * | –– |
| Arrest history (1 = yes) | 6.43% | –– | 4.79% * | –– |
| Respondent’s incarceration (1 = yes) | 12.28% | –– | 7.84% * | –– |
| N (person-years) | 20,191 | 38,710 | ||
| Blacks | Whites | |||||||
| Model 1A | Model 1B | Model 2A | Model 2B | |||||
| Variables a | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI |
| Age (centered at 18) | 1.04 *** | (1.02–1.05) | 1.31 | (0.87–1.98) | 1.08 *** | (1.06–1.09) | 0.85 | (0.68–1.06) |
| Female (1 = yes) | 1.83 *** | (1.70–1.97) | 4.56 *** | (2.11–9.85) | 1.46 *** | (1.34–1.57) | 1.61 * | (1.52–1.72) |
| Neighborhood disadvantage (ND) a | 1.13 *** | (1.04–1.23) | 1.40 ** | (1.12–1.75) | 1.04 * | (1.02–1.07) | 1.05 * | (1.03–1.07) |
| Control Variables | ||||||||
| Employed (1 = yes) | 0.87 * | (0.77–0.98) | 0.87 * | (0.77–0.98) | 0.85 ** | (0.77–0.94) | 0.86 ** | (0.77–0.95) |
| Married (1 = yes) | 0.95 | (0.84–1.07) | 0.95 | (0.84–1.07) | 0.74 *** | (0.68–0.80) | 0.74 *** | (0.68–0.80) |
| Parenthood (1 = yes) | 1.38 *** | (1.28–1.48) | 1.38 *** | (1.28–1.48) | 1.38 *** | (1.28–1.49) | 1.38 *** | (1.29–1.49) |
| College degree or more (1 = yes) | 0.37 *** | (0.30–0.45) | 0.37 *** | (0.30–0.45) | 0.28 *** | (0.24–0.32) | 0.28 *** | (0.24–0.32) |
| Family income (1 = top fifth) | 0.74 *** | (0.65–0.85) | 0.74 *** | (0.65–0.85) | 0.56 *** | (0.51–0.61) | 0.56 *** | (0.52–0.62) |
| Urban residence (1 = yes) | 0.92 | (0.84–1.01) | 0.92 | (0.84–1.01) | 1.09 ** | (1.02–1.16) | 1.09 ** | (1.02–1.16) |
| Southern residence (1 = yes) | 0.80 *** | (0.75–0.86) | 0.80 *** | (0.75–0.86) | 1.08 * | (1.01–1.15) | 1.08 * | (1.01–1.15) |
| Arrest history (1 = yes) | 1.29 *** | (1.13–1.48) | 1.29 *** | (1.13–1.48) | 1.53 *** | (1.36–1.71) | 1.54 *** | (1.37–1.72) |
| Respondent’s incarceration (1 = yes) | 1.24 *** | (1.11–1.38) | 1.24 *** | (1.11–1.38) | 1.80 *** | (1.64–1.97) | 1.80 *** | (1.64–1.97) |
| Interactions | ||||||||
| Age × female | –– | –– | 0.72 * | (0.53–0.98) | –– | –– | 1.27 ** | (1.16–1.40) |
| Age × ND | –– | –– | 0.92 | (0.81–1.06) | –– | –– | 1.12 * | (1.02–1.27) |
| Female × ND | –– | –– | 0.74 ** | (0.60–0.91) | –– | –– | 0.95 | (0.78–1.17) |
| Age × female × ND | –– | –– | 1.11 | (0.94–1.32) | –– | –– | 0.88 ** | (0.82–0.93) |
| AIC | 25,441.70 | 25,440.72 | 34,832.72 | 37,829.74 | ||||
| −2 Log likelihood | −12,707.85 | −12,704.36 | −17,403.63 | −17,397.73 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Christie-Mizell, C.A. Neighborhood Disadvantage and Poor Health: The Consequences of Race, Gender, and Age among Young Adults. Int. J. Environ. Res. Public Health 2022, 19, 8107. https://doi.org/10.3390/ijerph19138107
Christie-Mizell CA. Neighborhood Disadvantage and Poor Health: The Consequences of Race, Gender, and Age among Young Adults. International Journal of Environmental Research and Public Health. 2022; 19(13):8107. https://doi.org/10.3390/ijerph19138107
Chicago/Turabian StyleChristie-Mizell, C. André. 2022. "Neighborhood Disadvantage and Poor Health: The Consequences of Race, Gender, and Age among Young Adults" International Journal of Environmental Research and Public Health 19, no. 13: 8107. https://doi.org/10.3390/ijerph19138107
APA StyleChristie-Mizell, C. A. (2022). Neighborhood Disadvantage and Poor Health: The Consequences of Race, Gender, and Age among Young Adults. International Journal of Environmental Research and Public Health, 19(13), 8107. https://doi.org/10.3390/ijerph19138107






