Comparison of the Effect of Endurance, Strength and Endurance-Strength Training on Glucose and Insulin Homeostasis and the Lipid Profile of Overweight and Obese Subjects: A Systematic Review and Meta-Analysis †
Abstract
:1. Introduction
2. Methods
2.1. Protocol and Registration
2.2. Information Sources and Search Strategy
- Cochrane (1908–2021):
- PubMed (1966–2021):
- Scopus (1960–2021):
- Web of Science (1900–present):
2.3. Eligibility Criteria
2.4. Study Selection
2.5. Data Item and Data Collection Process
2.6. Data Analysis
2.7. Risk of Bias in Individual Studies
2.8. Statistical Analysis
3. Results
3.1. Search Results
3.2. Characteristics of Included Studies
3.3. Characteristics of Study Participants
3.4. Characteristics of Training Intervention
3.5. The Effect of Training Intervention on Glucose and Insulin Metabolism
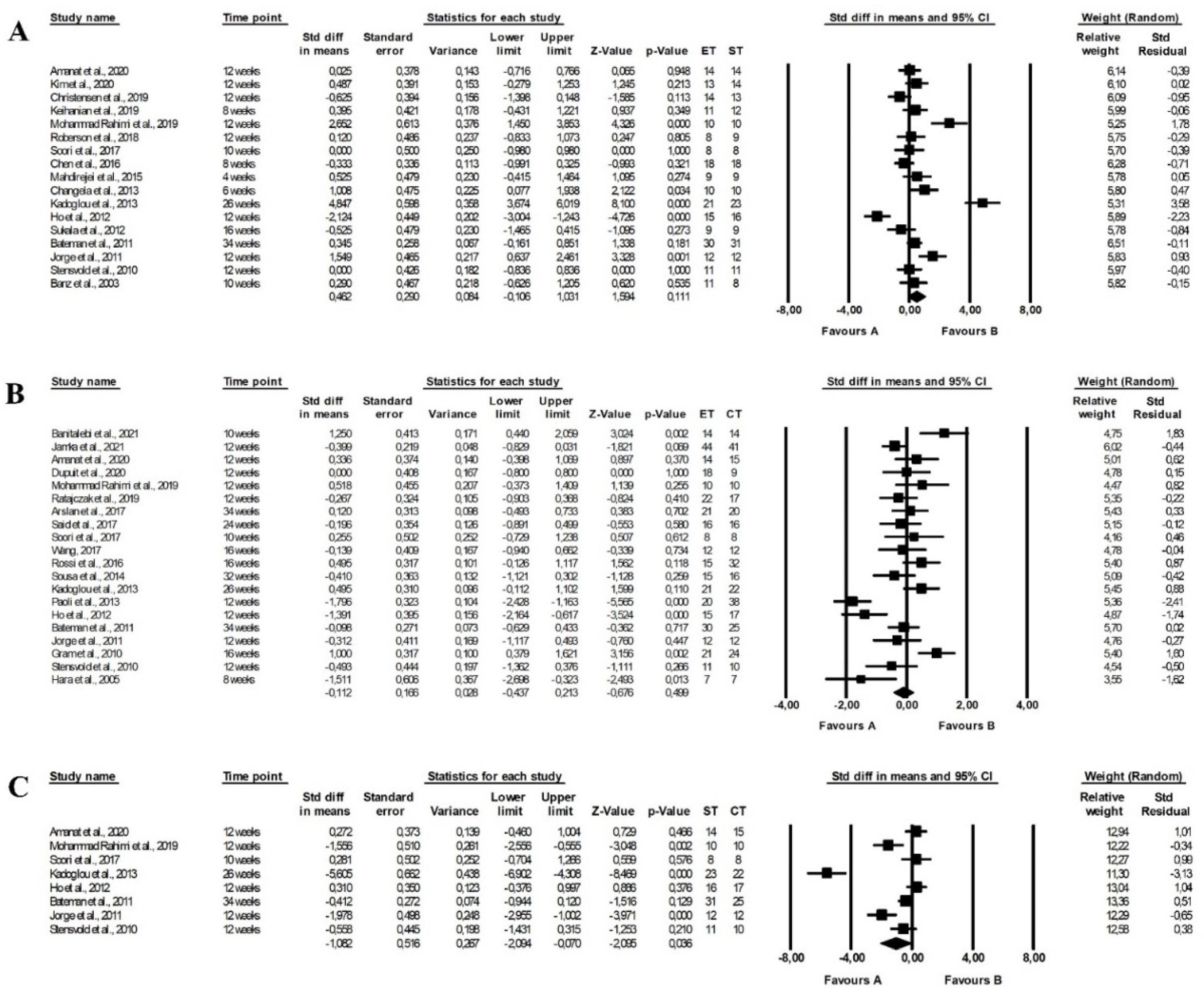
3.5.1. The Effect of Training Intervention on Fasting Glucose Levels
3.5.2. The Effect of Training Intervention on Fasting Insulin Levels
3.5.3. The Effect of Training Intervention on HbA1c Levels
3.5.4. The Effect of Training Intervention on the HOMA Index
3.5.5. The Effect of Training Intervention on 2 h Glucose Levels
3.5.6. The Effect of Training Intervention on 2 h Insulin Levels
3.5.7. The Effect of Training Intervention on C-Peptide Levels
3.6. The Effect of Training Intervention on Lipid Metabolism
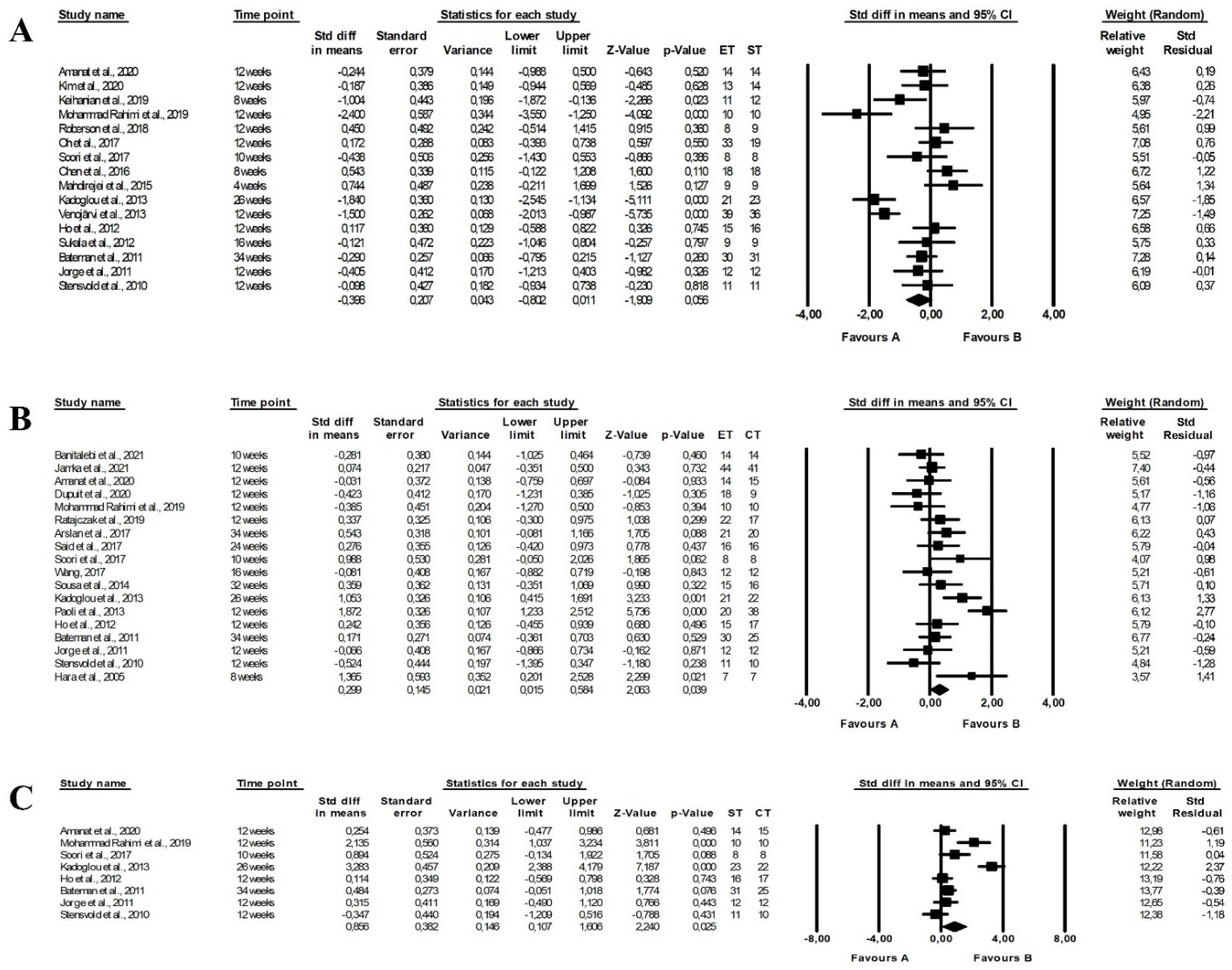
3.6.1. The Effect of Training Intervention on TC levels
3.6.2. The Effect of Training Intervention on LDL-C Levels
3.6.3. The Effect of Training Intervention on HDL-C Levels
3.6.4. The Effect of Training Intervention on TG Levels
3.7. Risk of Bias
3.8. Sensitivity and Cumulative Analyses
3.9. Subgroup Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 28 April 2021).
- Wondmkun, Y.T. Obesity, insulin resistance, and type 2 diabetes: Associations and therapeutic implications. Diabetes Metab. Syndr. Obes. 2020, 13, 3611–3616. [Google Scholar] [CrossRef]
- Mc Auley, M.T. Effects of obesity on cholesterol metabolism and its implications for healthy ageing. Nutr. Res. Rev. 2020, 33, 121–133. [Google Scholar] [CrossRef]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and cardiovascular disease: A scientific statement from the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef] [PubMed]
- Reyes, C.; Leyland, K.M.; Peat, G.; Cooper, C.; Arden, N.K.; Prieto-Alhambra, D. Association between overweight and obesity and risk of clinically diagnosed knee, hip, and hand osteoarthritis: A population-based cohort study. Arthritis Rheumatol. 2016, 68, 1869–1875. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scully, T.; Ettela, A.; LeRoith, D.; Gallagher, E.J. Obesity, type 2 diabetes, and cancer risk. Front. Oncol. 2021, 10, 615375. [Google Scholar] [CrossRef]
- Sarwar, R.; Pierce, N.; Koppe, S. Obesity and nonalcoholic fatty liver disease: Current perspectives. Diabetes Metab. Syndr. Obes. 2018, 11, 533–542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Afshin, A.; Forouzanfar, M.; Reitsma, M.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; Naghavi, M.; et al. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef]
- Galani, C.; Schneider, H. Prevention and treatment of obesity with lifestyle interventions: Review and meta-analysis. Int. J. Public Health 2007, 52, 348–359. [Google Scholar] [CrossRef] [PubMed]
- Liang, M.; Pan, Y.; Zhong, T.; Zeng, Y.; Cheng, A.S.K. Effects of aerobic, resistance, and combined exercise on metabolic syndrome parameters and cardiovascular risk factors: A systematic review and network meta-analysis. Rev. Cardiovasc. Med. 2021, 22, 1523–1533. [Google Scholar] [CrossRef]
- Busnatu, S.S.; Serbanoiu, L.I.; Lacraru, A.E.; Andrei, C.L.; Jercalau, C.E.; Stoian, M.; Stoian, A. Effects of exercise in improving cardiometabolic risk factors in overweight children: A systematic review and meta-analysis. Healthcare 2022, 10, 82. [Google Scholar] [CrossRef]
- Al Saif, A.; Alsenany, S. Aerobic and anaerobic exercise training in obese adults. J. Phys. Ther. Sci. 2015, 27, 1697–1700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bateman, L.A.; Slentz, C.A.; Willis, L.H.; Shields, A.T.; Piner, L.W.; Bales, C.W.; Houmard, J.A.; Kraus, W.E. Comparison of aerobic versus resistance exercise training effects on metabolic syndrome (from the studies of a targeted risk reduction intervention through defined exercise—STRRIDE-AT/ST). Am. J. Cardiol. 2011, 108, 838–844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mahdirejei, T.A.; Razi, M.; Barari, A.; Farzanegi, P.; Mahdirejei, H.A.; Shahrestani, Z.; Ahmadi, M. A comparative study of the effects of endurance and resistance exercise training on PON1 and lipid profile levels in obese men. Sport Sci. Health 2015, 11, 263–270. [Google Scholar] [CrossRef]
- Slentz, C.A.; Bateman, L.A.; Willis, L.H.; Shields, A.T.; Tanner, C.J.; Piner, L.W.; Hawk, V.H.; Muehlbauer, M.J.; Samsa, G.P.; Nelson, R.C.; et al. Effects of aerobic vs. resistance training on visceral and liver fat stores, liver enzymes, and insulin resistance by HOMA in overweight adults from STRRIDE AT/ST. Am. J. Physiol. Endocrinol. Metab. 2011, 301, e1033–e1039. [Google Scholar] [CrossRef] [Green Version]
- Nikseresht, M.; Agha-Alinejad, H.; Azarbayjani, M.A.; Ebrahim, K. Effects of nonlinear resistance and aerobic interval training on cytokines and insulin resistance in sedentary men who are obese. J. Strength Cond. Res. 2014, 28, 2560–2568. [Google Scholar] [CrossRef]
- El-Refaye, G.; Younis, H. The effect of 12 weeks of resistive exercises versus aerobic exercises in overweight hypertensive postmenopausal women. Bull. Fac. Phys. Ther. 2019, 24, 40–48. [Google Scholar] [CrossRef]
- Sawczyn, S.; Mishchenko, V.; Moska, W.; Sawczyn, M.; Jagiełło, M.; Kuehne, T.; Kostrzewa-Nowak, D.; Nowak, R.; Cięszczyk, P. Strength and aerobic training in overweight females in Gdansk, Poland. Open Med. 2015, 10, 152–162. [Google Scholar] [CrossRef] [Green Version]
- Said, M.A.; Abdelmoneim, M.A.; Alibrahim, M.S.; Kotb, A.A.H. Aerobic training, resistance training, or their combination as a means to fight against excess weight and metabolic syndrome in obese students—Which is the most effective modality? A randomized controlled trial. Appl. Physiol. Nutr. Metab. 2021, 46, 952–963. [Google Scholar] [CrossRef]
- Abouassi, H.; Slentz, C.A.; Mikus, C.R.; Tanner, C.J.; Bateman, L.A.; Willis, L.H.; Shields, A.T.; Piner, L.W.; Penry, L.E.; Kraus, E.A.; et al. The effects of aerobic, resistance, and combination training on insulin sensitivity and secretion in overweight adults from STRRIDE AT/ST: A randomized trial. J. Appl. Physiol. 2015, 118, 1474–1482. [Google Scholar] [CrossRef] [Green Version]
- Rossi, F.E.; Fortaleza, A.C.S.; Neves, L.M.; Buonani, C.; Picolo, M.R.; Diniz, T.A.; Kalva-Filho, C.A.; Papoti, M.; Lira, F.S.; Freitas Junior, I.F. Combined training (aerobic plus strength) potentiates a reduction in body fat but demonstrates no difference on the lipid profile in postmenopausal women when compared with aerobic training with a similar training load. J. Strength Cond. Res. 2016, 30, 226–234. [Google Scholar] [CrossRef]
- Stensvold, D.; Tjønna, A.E.; Skaug, E.A.; Aspenes, S.; Stølen, T.; Wisløff, U.; Slørdahl, S.A. Strength training versus aerobic interval training to modify risk factors of metabolic syndrome. J. Appl. Physiol. 2010, 108, 804–810. [Google Scholar] [CrossRef] [Green Version]
- Batrakoulis, A.; Jamurtas, A.Z.; Metsios, G.S.; Perivoliotis, K.; Liguori, G.; Feito, Y.; Riebe, D.; Thompson, W.R.; Angelopoulos, T.J.; Krustrup, P.; et al. Comparative efficacy of 5 exercise types on cardiometabolic health in overweight and obese adults: A systematic review and network meta-analysis of 81 randomized controlled trials. Circ. Cardiovasc. Qual. Outcomes 2022, 15, e008243. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane. 2022. Available online: https://training.cochrane.org/handbook (accessed on 16 August 2022).
- Jamka, M.; Makarewicz, A.; Śmidowicz, A.; Geltz, J.; Kokot, M.; Kaczmarek, N.; Mądry, E.; Walkowiak, J. Comparison of the Effect of Endurance, Strength and Endurance-Strength Training in Overweight and Obese Adults. PROSPERO: International Prospective Register of Systematic Reviews. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=183252 (accessed on 16 November 2020).
- World Health Organization. Body Mass Index—BMI. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 16 November 2020).
- Jih, J.; Mukherjea, A.; Vittinghoff, E.; Nguyen, T.T.; Tsoh, J.Y.; Fukuoka, Y.; Bender, M.S.; Tseng, W.; Kanaya, A.M. Using appropriate body mass index cut points for overweight and obesity among Asian Americans. Prev. Med. 2014, 65, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation; World Health Organization: Geneva, Switzerland, 2008; pp. 1–47.
- American Council on Exercise. Percent Body Fat Calculator. Available online: https://www.acefitness.org/education-and-resources/lifestyle/tools-calculators/percent-body-fat-calculator/ (accessed on 16 November 2020).
- American Diabetes Association. 2. Classification and diagnosis of diabetes: Standards of medical care in diabetes—2021. Diabetes Care 2021, 44, S15–S33. [Google Scholar] [CrossRef] [PubMed]
- Gayoso-Diz, P.; Otero-González, A.; Rodriguez-Alvarez, M.X.; Gude, F.; García, F.; De Francisco, A.; Quintela, A.G. Insulin resistance (HOMA-IR) cut-off values and the metabolic syndrome in a general adult population: Effect of gender and age: EPIRCE cross-sectional study. BMC Endocr. Disord. 2013, 13, 47. [Google Scholar] [CrossRef] [Green Version]
- Yosten, G.L.C.; Maric-Bilkan, C.; Luppi, P.; Wahren, J. Physiological effects and therapeutic potential of proinsulin C-peptide. Am. J. Physiol. Endocrinol. Metab. 2014, 307, 955–968. [Google Scholar] [CrossRef] [Green Version]
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Treatment E and T of HBC in A (Adult, Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef]
- Dupuit, M.; Rance, M.; Morel, C.; Bouillon, P.; Pereira, B.; Bonnet, A.; Maillard, F.; Duclos, M.; Boisseau, N. Moderate-intensity continuous training or high-intensity interval training with or without resistance training for altering body composition in postmenopausal women. Med. Sci. Sport. Exerc. 2020, 52, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Jamka, M.; Mądry, E.; Krzyżanowska-Jankowska, P.; Skrypnik, D.; Szulińska, M.; Mądry, R.; Lisowska, A.; Batyrova, G.; Duś-Żuchowska, M.; Gotz-Więckowska, A.; et al. The effect of endurance and endurance-strength training on body composition and cardiometabolic markers in abdominally obese women: A randomised trial. Sci. Rep. 2021, 11, 12339. [Google Scholar] [CrossRef] [PubMed]
- Banitalebi, E.; Ghahfarrokhi, M.M.; Faramarzi, M.; Earnest, C.P. Sprint interval training vs. combined aerobic + resistance training in overweight women with type 2 diabetes. J. Sport. Med. Phys. Fit. 2021, 61, 712–724. [Google Scholar] [CrossRef] [PubMed]
- Banitalebi, E.; Faramarzi, M.; Nasiri, S.; Mardaniyan, M.; Rabiee, V. Effects of different exercise modalities on novel hepatic steatosis indices in overweight women with type 2 diabetes. Clin. Mol. Hepatol. 2019, 25, 294–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amanat, S.; Sinaei, E.; Panji, M.; MohammadporHodki, R.; Bagheri-Hosseinabadi, Z.; Asadimehr, H.; Fararouei, M.; Dianatinasab, A. A randomized controlled trial on the effects of 12 weeks of aerobic, resistance, and combined exercises training on the serum levels of nesfatin-1, irisin-1 and HOMA-IR. Front. Physiol. 2020, 11, 562895. [Google Scholar] [CrossRef]
- Dianatinasab, A.; Koroni, R.; Bahramian, M.; Bagheri-Hosseinabadi, Z.; Vaismoradi, M.; Fararouei, M.; Amanat, S. The effects of aerobic, resistance, and combined exercises on the plasma irisin levels, HOMA-IR, and lipid profiles in women with metabolic syndrome: A randomized controlled trial. J. Exerc. Sci. Fit. 2020, 18, 168–176. [Google Scholar] [CrossRef]
- Kim, B.; Kim, S. Influences of resistance versus aerobic exercise on physiological and physical fitness changes in previously inactive men with obesity: A prospective, single-blinded randomized controlled trial. Diabetes Metab. Syndr. Obes. 2020, 13, 267–276. [Google Scholar] [CrossRef] [Green Version]
- Christensen, R.H.; Wedell-Neergaard, A.S.; Lehrskov, L.L.; Legaard, G.E.; Dorph, E.; Larsen, M.K.; Launbo, N.; Fagerlind, S.R.; Seide, S.K.; Nymand, S.; et al. Effect of aerobic and resistance exercise on cardiac adipose tissues: Secondary analyses from a randomized clinical trial. JAMA Cardiol. 2019, 4, 778–787. [Google Scholar] [CrossRef]
- Keihanian, A.; Arazi, H.; Kargarfard, M. Effects of aerobic versus resistance training on serum fetuin-A, fetuin-B, and fibroblast growth factor-21 levels in male diabetic patients. Physiol. Int. 2019, 106, 70–80. [Google Scholar] [CrossRef]
- Mohammad Rahimi, G.R.; Bijeh, N.; Rashidlamir, A. Effects of exercise training on serum preptin, undercarboxylated osteocalcin and high molecular weight adiponectin in adults with metabolic syndrome. Exp. Physiol. 2020, 105, 449–459. [Google Scholar] [CrossRef]
- Ratajczak, M.; Skrypnik, D.; Bogdański, P.; Madry, E.; Walkowiak, J.; Szulińska, M.; Maciaszek, J.; Kręgielska-Narożna, M.; Karolkiewicz, J. Effects of endurance and endurance–strength training on endothelial function in women with obesity: A randomized trial. Int. J. Environ. Res. Public Health 2019, 16, 4291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martins, F.M.; de Paula Souza, A.; Nunes, P.R.P.; Michelin, M.A.; Murta, E.F.C.; Resende, E.A.M.R.; de Oliveira, E.P.; Orsatti, F.L. High-intensity body weight training is comparable to combined training in changes in muscle mass, physical performance, inflammatory markers and metabolic health in postmenopausal women at high risk for type 2 diabetes mellitus: A randomized controlled trial. Exp. Gerontol. 2018, 107, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Roberson, K.B.; Potiaumpai, M.; Widdowson, K.; Jaghab, A.M.; Chowdhari, S.; Armitage, C.; Seeley, A.; Jacobs, K.A.; Signorile, J.F. Effects of high-velocity circuit resistance and treadmill training on cardiometabolic risk, blood markers, and quality of life in older adults. Appl. Physiol. Nutr. Metab. 2018, 43, 822–832. [Google Scholar] [CrossRef] [PubMed]
- Álvarez, C.; Ramírez-Campillo, R.; Ramírez-Vélez, R.; Izquierdo, M. Effects and prevalence of nonresponders after 12 weeks of high-intensity interval or resistance training in women with insulin resistance: A randomized trial. J. Appl. Physiol. 2017, 122, 985–996. [Google Scholar] [CrossRef]
- AminiLari, Z.; Fararouei, M.; Amanat, S.; Sinaei, E.; Dianatinasab, S.; AminiLari, M.; Daneshi, N.; Dianatinasab, M. The effect of 12 weeks aerobic, resistance, and combined exercises on omentin-1 levels and insulin resistance among type 2 diabetic middle-aged women. Diabetes Metab. J. 2017, 41, 205–212, Erratum in Diabetes Metab. J. 2017, 41, 422. [Google Scholar] [CrossRef]
- Arslan, E.; Can, S.; Demirkan, E. Effect of short-term aerobic and combined training program on body composition, lipids profile and psychological health in premenopausal women. Sci. Sport. 2017, 32, 106–113. [Google Scholar] [CrossRef]
- Oh, S.; So, R.; Shida, T.; Matsuo, T.; Kim, B.; Akiyama, K.; Isobe, T.; Okamoto, Y.; Tanaka, K.; Shoda, J. High-intensity aerobic exercise improves both hepatic fat content and stiffness in sedentary obese men with nonalcoholic fatty liver disease. Sci. Rep. 2017, 7, 43029. [Google Scholar] [CrossRef] [Green Version]
- Said, M.; Lamya, N.; Olfa, N.; Hamda, M. Effects of high-impact aerobics vs. low-impact aerobics and strength training in overweight and obese women. J. Sport. Med. Phys. Fit. 2017, 57, 278–288. [Google Scholar] [CrossRef]
- Soori, R.; Rezaeian, N.; Khosravi, N.; Ahmadizad, S.; Taleghani, H.M.; Jourkesh, M.; Stannard, S.R. Effects of water-based endurance training, resistance training, and combined water and resistance training programs on visfatin and ICAM-1 levels in sedentary obese women. Sci. Sport. 2017, 32, 144–151. [Google Scholar] [CrossRef]
- Wang, J. Impacts of combining aerobic exercises with resistance training on chemerin level in obese undergraduates. Biomed. Res. 2017, 2017, S654–S658. [Google Scholar]
- Chen, C.K.; Ismail, N.S.; Al-Safi, A.A. Effects of brisk walking and resistance training on cardiorespiratory fitness, body composition, and lipid profiles among overweight and obese individuals. J. Phys. Educ. Sport 2016, 16, 957–963. [Google Scholar] [CrossRef]
- Tayebi, S.M.; Saeidi, A.; Khosravi, M. Single and concurrent effects of endurance and resistance training on plasma visfatin, insulin, glucose and insulin resistance of non-athlete men with obesity. Ann. Appl. Sport Sci. 2016, 4, 21–31. [Google Scholar] [CrossRef] [Green Version]
- Huffman, K.M.; Koves, T.; Hubal, M.; Abouassi, H.; Beri, N.; Bateman, L.A.; Stevens, R.D.; Ilkayeva, O.R.; Hoffman, E.; Muoio, D.; et al. Metabolite signatures of exercise training in human skeletal muscle relate to mitochondrial remodelling and cardiometabolic fitness. Diabetologia 2014, 57, 2282–2295. [Google Scholar] [CrossRef] [Green Version]
- Sousa, N.; Mendes, R.; Abrantes, C.; Sampaio, J.; Oliveira, J. A randomized study on lipids response to different exercise programs in overweight older men. Int. J. Sport. Med. 2014, 35, 1106–1111. [Google Scholar] [CrossRef] [PubMed]
- Changela, P.K.; Sheth, K.K. A study to compare the effect of aerobic and resistance training on cardiovascular (CVS) fitness in young obese sedentary females. Int. J. Sci. Res. Publ. 2013, 3, 1–9. [Google Scholar]
- Donges, C.E.; Duffield, R.; Guelfi, K.J.; Smith, G.C.; Adams, D.R.; Edge, J.A. Comparative effects of single-mode vs. duration-matched concurrent exercise training on body composition, low-grade inflammation, and glucose regulation in sedentary, overweight, middle-aged men. Appl. Physiol. Nutr. Metab. 2013, 38, 779–788. [Google Scholar] [CrossRef]
- Kadoglou, N.P.E.; Fotiadis, G.; Kapelouzou, A.; Kostakis, A.; Liapis, C.D.; Vrabas, I.S. The differential anti-inflammatory effects of exercise modalities and their association with early carotid atherosclerosis progression in patients with type 2 diabetes. Diabet. Med. 2013, 30, e41. [Google Scholar] [CrossRef] [PubMed]
- Paoli, A.; Pacelli, Q.F.; Moro, T.; Marcolin, G.; Neri, M.; Battaglia, G.; Sergi, G.; Bolzetta, F.; Bianco, A. Effects of high-intensity circuit training, low-intensity circuit training and endurance training on blood pressure and lipoproteins in middle-aged overweight men. Lipids Health Dis. 2013, 12, 131. [Google Scholar] [CrossRef] [Green Version]
- Venojärvi, M.; Wasenius, N.; Manderoos, S.; Heinonen, O.J.; Hernelahti, M.; Lindholm, H.; Surakka, J.; Lindström, J.; Aunola, S.; Atalay, M.; et al. Nordic walking decreased circulating chemerin and leptin concentrations in middle-aged men with impaired glucose regulation. Ann. Med. 2013, 45, 162–170. [Google Scholar] [CrossRef]
- Ho, S.S.; Dhaliwal, S.S.; Hills, A.P.; Pal, S. The effect of 12 weeks of aerobic, resistance or combination exercise training on cardiovascular risk factors in the overweight and obese in a randomized trial. BMC Public Health 2012, 12, 704. [Google Scholar] [CrossRef] [Green Version]
- Stensvold, D.; Slørdahl, S.A.; Wisløff, U. Effect of exercise training on inflammation status among people with metabolic syndrome. Metab. Syndr. Relat. Disord. 2012, 10, 267–272. [Google Scholar] [CrossRef] [Green Version]
- Sukala, W.R.; Page, R.; Rowlands, D.S.; Krebs, J.; Lys, I.; Leikis, M.; Pearce, J.; Cheema, B.S. South Pacific Islanders resist type 2 diabetes: Comparison of aerobic and resistance training. Eur. J. Appl. Physiol. 2012, 112, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Jorge, M.L.M.P.; de Oliveira, V.N.; Resende, N.M.; Paraiso, L.F.; Calixto, A.; Diniz, A.L.D.; Resende, E.S.; Ropelle, E.R.; Carvalheira, J.B.; Espindola, F.S.; et al. The effects of aerobic, resistance, and combined exercise on metabolic control, inflammatory markers, adipocytokines, and muscle insulin signaling in patients with type 2 diabetes mellitus. Metabolism 2011, 60, 1244–1252. [Google Scholar] [CrossRef] [PubMed]
- Gram, B.; Christensen, R.; Christiansen, C.; Gram, J. Effects of nordic walking and exercise in type 2 diabetes mellitus: A randomized controlled trial. Clin. J. Sport Med. 2010, 20, 355–361. [Google Scholar]
- Ahmadizad, S.; Haghighi, A.H.; Hamedinia, M.R. Effects of resistance versus endurance training on serum adiponectin and insulin resistance index. Eur. J. Endocrinol. 2007, 157, 625–631. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hara, T.; Fujiwara, H.; Nakao, H.; Mimura, T.; Yoshikawa, T.; Fujimoto, S. Body composition is related to increase in plasma adiponectin levels rather than training in young obese men. Eur. J. Appl. Physiol. 2005, 94, 520–526. [Google Scholar] [CrossRef]
- Banz, W.J.; Maher, M.A.; Thompson, W.G.; Bassett, D.R.; Moore, W.; Ashraf, M.; Keefer, D.J.; Zemel, M.B. Effects of resistance versus aerobic training on coronary artery disease risk factors. Exp. Biol. Med. 2003, 228, 434–440. [Google Scholar] [CrossRef]
- Cuff, D.J.; Meneilly, G.S.; Martin, A.; Ignaszewski, A.; Tildesley, H.D.; Frohlich, J.J. Effective exercise modality to reduce insulin resistance in women with type 2 diabetes. Diabetes Care 2003, 26, 2977–2982. [Google Scholar] [CrossRef] [Green Version]
- Banitalebi, E.; Kazemi, A.R.; Faramarzi, M.; Nasiri, S.; Haghighi, M.M. Effects of sprint interval or combined aerobic and resistance training on myokines in overweight women with type 2 diabetes: A randomized controlled trial. Life Sci. 2019, 217, 101–109. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020; pp. 1–535.
- Oppert, J.; Bellicha, A.; van Baak, M.A.; Battista, F.; Beaulieu, K.; Blundell, J.E.; Carraça, E.V.; Encantado, J.; Ermolao, A.; Pramono, A.; et al. Exercise training in the management of overweight and obesity in adults: Synthesis of the evidence and recommendations from the European Association for the Study of Obesity Physical Activity Working Group. Obes. Rev. 2021, 22 (Suppl. 4), e13273. [Google Scholar] [CrossRef]
- American College of Sports Medicine; Liguori, G.; Feito, Y.; Fountaine, C.; Roy, B.A. ACSM’s Guidelines for Exercise Testing and Prescription, 11th ed.; Wolters Kluwer Health: Philadelphia, PA, USA, 2021; pp. 1–548. [Google Scholar]
- Snowling, N.J.; Hopkins, W.G. Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: A meta-analysis. Diabetes Care 2006, 29, 2518–2527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bays, H.E.; González-Campoy, J.M.; Bray, G.A.; Kitabchi, A.E.; Bergman, D.A.; Schorr, A.B.; Rodbard, H.W.; Henry, R.R. Pathogenic potential of adipose tissue and metabolic consequences of adipocyte hypertrophy and increased visceral adiposity. Expert Rev. Cardiovasc. Ther. 2008, 6, 343–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morze, J.; Rücker, G.; Danielewicz, A.; Przybyłowicz, K.; Neuenschwander, M.; Schlesinger, S.; Schwingshackl, S. Impact of different training modalities on anthropometric outcomes in patients with obesity: A systematic review and network meta-analysis. Obes. Rev. 2021, 22, e13218. [Google Scholar] [CrossRef] [PubMed]
- Yarizadeh, H.; Eftekhar, R.; Anjom-Shoae, J.; Speakman, J.R.; Djafarian, K. The effect of aerobic andr esistance training and combined exercise modalities on subcutaneous abdominal fat: A systematic review and meta-analysis of randomized clinical trials. Adv. Nutr. 2021, 12, 179–196. [Google Scholar] [CrossRef] [PubMed]
- Davidson, L.E.; Hudson, R.; Kilpatrick, K.; Kuk, J.L.; McMillan, K.; Janiszewski, P.M.; Lee, S.; Lam, M.; Ross, R. Effects of exercise modality on insulin resistance and functional limitation in older adults: A randomized controlled trial. Arch. Intern. Med. 2009, 169, 122–131. [Google Scholar] [CrossRef] [Green Version]
- Vilar Gomez, E.; Rodriguez De Miranda, A.; Gra Oramas, B.; Arus Soler, E.; Llanio Navarro, R.; Calzadilla Bertot, L.; Yasells Garcia, A.; Del Rosario Abreu Vazquez, M. Clinical trial: A nutritional supplement Viusid, in combination with diet and exercise, in patients with nonalcoholic fatty liver disease. Aliment. Pharmacol. Ther. 2009, 30, 999–1009. [Google Scholar] [CrossRef]
- Gleeson, M.; Bishop, N.C.; Stensel, D.J.; Lindley, M.R.; Mastana, S.S.; Nimmo, M.A. The anti-inflammatory effects of exercise: Mechanisms and implications for the prevention and treatment of disease. Nat. Rev. Immunol. 2011, 11, 607–610. [Google Scholar] [CrossRef]
- Ouchi, N.; Parker, J.L.; Lugus, J.J.; Walsh, K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol. 2011, 11, 85–97. [Google Scholar] [CrossRef]
- Bruunsgaard, H. Physical activity and modulation of systemic low-level inflammation. J. Leukoc. Biol. 2005, 78, 819–835. [Google Scholar] [CrossRef] [Green Version]
- Makarewicz, A.; Jamka, M.; Geltz, J.; Śmidowicz, A.; Kokot, M.; Kaczmarek, N.; Mądry, E.; Walkowiak, J. Comparison of the effect of endurance, strength, and endurance-strength training on inflammatory markers and adipokines levels in overweight and obese adults: Systematic review and meta-analysis of randomised trials. Healthcare 2022, 10, 1098. [Google Scholar] [CrossRef]
- Cadore, E.L.; Pinto, R.S.; Bottaro, M.; Izquierdo, M. Strength and endurance training prescription in healthy and frail elderly. Aging Dis. 2014, 5, 195. [Google Scholar] [CrossRef] [PubMed]
- Syed, I. Glycated haemoglobin; past, present, and future are we ready for the change. J. Pak. Med. Assoc. 2011, 61, 383–388. [Google Scholar] [PubMed]










| Author | Year | Country (Region) | Groups | n Included | n Completed | Studied Population | Obesity/Overweight Definition | Age [Years] | Sex [% of Women] |
|---|---|---|---|---|---|---|---|---|---|
| Jamka et al. [38] | 2021 | Poland (Europe) | ET CT | 52 49 | 44 41 | Abdominally obese women | BMI ≥ 30 kg/m2 WC > 80 cm %FM ≥ 32% | 55 ± 7 1 55 ± 7 1 | 100 |
| Banitalebi et al. [39] Banitalebi et al. [40,75] | 2021 2019 | Iran (Asia) | ET | 17 | 14 | Overweight or obese women with T2DM | BMI: 25–48 kg/m2 | 55.36 ± 5.94 1 | 100 |
| CT | 17 | 14 | 54.14 ± 5.43 1 | ||||||
| CG | 18 | 14 | 55.71 ± 6.40 1 | ||||||
| Amanat et al. a [41] | 2020 | Iran (Asia) | ET | 15 | 14 | Overweight or obese women with metabolic syndrome | WC > 88 cm | 54.5 ± 6.9 1 | 100 |
| ST | 15 | 14 | |||||||
| CT | 15 | 15 | |||||||
| CG | 15 | 14 | |||||||
| Dianatinasab et al. a [42] | 2020 | Iran (Asia) | ET | 15 | 13 | Overweight or obese women with metabolic syndrome | WC > 88 cm | 53.47 ± 6.53 1 | 100 |
| ST | 15 | 13 | |||||||
| CT | 15 | 13 | |||||||
| CG | 15 | 15 | |||||||
| Dupuit et al. [37] | 2020 | France (Europe) | ET 2 | 10 | 8 | Overweight or obese postmenopausal women | BMI > 25 and ≤40 kg/m2 | 67.1 ± 7.2 1 | 100 |
| ET 3 | 10 | 10 | 59.9 ± 5.9 1 | ||||||
| CT | 10 | 9 | 61.1 ± 5.4 1 | ||||||
| Kim et al. [43] | 2020 | South Korea (Asia) | ET | 19 | 13 | Previously inactive men with obesity | BMI ≥ 25 kg/m2 | 50.15 ± 5.84 1 | 0 |
| ST | 19 | 14 | 51.79 ± 8.22 1 | ||||||
| Christensen et al. [44] | 2019 | Denmark (Europe) | ET | 16 | 14 | Inactive subjects with abdominal obesity | WHR ≥ 0.5 and/or | 39 ± 14 1 | 79 |
| ST | 16 | 13 | WC ≥ 88 cm for women or | 38 ± 14 1 | 62 | ||||
| CG | 18 | 12 | WC ≥ 102 cm for men | 47 ± 12 1 | 83 | ||||
| Keihanian et al. [45] | 2019 | Iran (Asia) | ET | 39 | 11 | Obese men with T2DM | BMI > 30 kg/m2 | 52.4 ± 1.5 1 | 0 |
| ST | 12 | 52.4 ± 1.8 1 | |||||||
| CG | 11 | 53.0 ± 1.1 1 | |||||||
| Mohammad Rahimi et al. [46] | 2019 | Iran (Asia) | ET | 10 | 10 | Sedentary obese men with metabolic syndrome | BMI: 30–40 kg/m2 | 44.8 ± 4.8 1 | 0 |
| ST | 11 | 10 | 46.1 ± 5.1 1 | ||||||
| CT | 12 | 10 | 44.9 ± 4.2 1 | ||||||
| CG | 11 | 10 | 46.4 ± 5.1 1 | ||||||
| Ratajczak et al. [47] | 2019 | Poland (Europe) | ET | 22 | 22 | Women with simple obesity | BMI ≥ 30 kg/m2 and WC > 80 cm and %FM ≥ 33% | 51 ± 8 1 | 100 |
| CT | 22 | 17 | 49 ± 10 1 | ||||||
| Martins et al. [48] | 2018 | Brazil (South America) | ET | 14 | 8 | Overweight women with high risk for T2DM, not exercising for at least 6 months | BMI > 24.9 kg/m2 and %FM > 40% | 64.3 ± 6.7 1 | 100 |
| CT | 14 | 8 | 65.0 ± 6.3 1 | ||||||
| Roberson et al. [49] | 2018 | USA (North America) | ET | 10 | 8 | Older subjects with multiple cardiometabolic syndromes or cardiovascular disease risk factors | WC ≥ 88 cm for women or WC ≥ 102 cm for men | 68 ± 3 4 | 73 (included) 79 (completed) |
| ST | 10 | 9 | 72 ± 3 4 | ||||||
| CG | 10 | 7 | 70 ± 3 4 | ||||||
| Alvarez et al. [50] | 2017 | Chile (South America) | ET | 20 | 18 | Sedentary overweight or obese insulin-resistant women | BMI: 25–35 kg/m2 | 38.0 ± 8.0 1,5 | 100 |
| ST | 20 | 17 | 33.0 ± 7.0 1,5 | ||||||
| AminiLari et al. [51] | 2017 | Iran (Asia) | ET | 15 | 12 | Overweight middle-aged women with T2DM | NI | 45–60 6,7 | 100 |
| ST | 15 | 12 | |||||||
| CT | 15 | 13 | |||||||
| CG | 15 | 15 | |||||||
| Arslan et al. [52] | 2017 | Turkey (Asia) | ET | 78 | 21 | Middle-aged overweight premenopausal sedentary women | BMI > 25 kg/m2 | 39.0 ± 3.1 1 | 100 |
| CT | 20 | 38.7 ± 2.7 1 | |||||||
| CG | 23 | 38.9 ± 3.1 1 | |||||||
| Oh et al. [53] | 2017 | Japan (Asia) | ET 3 | 21 | 20 | Obese sedentary men with non-alcoholic fatty liver disease and no exercise habits | %FM > 25% for men | 48.6 ± 1.8 4 | 0 |
| ET 2 | 19 | 13 | 48.2 ± 2.3 4 | ||||||
| ST | 20 | 19 | 51.2 ± 1.9 4 | ||||||
| Said et al. [54] | 2017 | Tunisia (Africa) | ET | 16 | NI | Healthy overweight and obese women | BMI: 25–35 kg/m2 | 30.58 ± 3.8 1 | 100 |
| CT | 16 | 29.66 ± 4.2 1 | |||||||
| Soori et al. [55] | 2017 | Iran (Asia) | ET | 8 | NI | Postmenopausal sedentary obese women | BMI ≥ 30 kg/m2 | 45–60 6,7 | 100 |
| ST | 8 | ||||||||
| CT | 8 | ||||||||
| CG | 8 | ||||||||
| Wang [56] | 2017 | China (Asia) | ET | 12 | NI | Obese undergraduates | BMI ≥ 28 kg/m2 | NI | NI |
| CT | 12 | ||||||||
| CG | 12 | ||||||||
| Chen et al. [57] | 2016 | Malaysia (Asia) | ET | 20 | 18 | Overweight and obese subjects | BMI: 25–40 kg/m2 | 36.8 ± 8.1 1 | 65 |
| ST | 20 | 18 | 34.8 ± 10.6 1 | ||||||
| CG | 20 | 18 | 32.4 ± 9.9 1 | ||||||
| Rossi et al. [21] | 2016 | Brazil (South America) | ET | 35 | 15 | Obese postmenopausal Women | BMI > 25 kg/m2 | 60.5 6 ± 7.3 1 | 100 |
| CT | 35 | 32 | 60.3 ± 6.1 1 | ||||||
| CG | 34 | 18 | 62.6 ± 5.9 1 | ||||||
| Tayebi et al. [58] | 2016 | Iran (Asia) | ET | 12 | 11 | Non-athlete men with obesity | %FM > 25% | 21.48 ± 1.46 1,6 | 0 |
| ST | 12 | 9 | |||||||
| CT | 12 | 12 | |||||||
| AbouAssi et al. b [20] | 2015 | USA (North America) | ET | 196 | 27 | Sedentary overweight or obese subjects with mild to moderate dyslipidaemia | BMI: 26–35 kg/m2 | 51.4 ± 10 1 | 52 |
| ST | 38 | 51.1 ± 11 1 | 47 | ||||||
| CT | 23 | 46.9 ± 11 1 | 57 | ||||||
| Mahdirejei et al. [14] | 2015 | Iran (Asia) | ET | 9 | NI | Obese men with no exercise training history | NI | 21/4 ± 15/41 1,6 | 0 |
| ST | 9 | ||||||||
| CG | 8 | ||||||||
| Huffman et al. b [59] | 2014 | USA (North America) | ET 8 | 15 | 15 | Inactive overweight to mildly obese and dyslipidaemic subjects | BMI: 25–35 kg/m2 | 18–70 6,7 | 50 |
| ET 9 | 20 | 20 | |||||||
| ET 10 | 17 | 17 | |||||||
| ST | 20 | 20 | |||||||
| CT | 20 | 20 | |||||||
| CG | 20 | 20 | |||||||
| Nikseresht et al. [16] | 2014 | Iran (Asia) | ET | 12 | NI | Sedentary overweight or obese men with no regular exercise and with no history of any medical condition | BMI >25 kg/m2 | 39.6 ± 3.7 1 | 0 |
| ST | 12 | 40.4 ± 5.2 1 | |||||||
| CG | 10 | 38.9 ± 4.1 1 | |||||||
| Sousa et al. [60] | 2014 | Portugal (Europe) | ET | 19 | 15 | Overweight older men | BMI ≥ 25 and <35 kg/m2 | 69.1 ± 5.0 1,6 65–75 6,7 | 0 |
| CT | 20 | 16 | |||||||
| CG | 20 | 17 | |||||||
| Changela et al. [61] | 2013 | India (Asia) | ET | 10 | NI | Young obese sedentary women | BMI > 30 kg/m2 | 22.22 ± 1.98 1 | 100 |
| ST | 10 | 22.67 ± 1.50 1 | |||||||
| Donges et al. [62] | 2013 | Australia (Australia) | ET | 13 | 13 | Sedentary overweight middle-aged men | NI | 45.4 ± 1.7 4 | 0 |
| ST | 13 | 13 | 51.7 ± 2.1 4 | ||||||
| CT | 13 | 13 | 46.2 ± 1.4 4 | ||||||
| CG | 8 | 8 | 49.5 ± 2.6 4 | ||||||
| Kadoglou et al. [63] | 2013 | Greece (Europe) | ET | 25 | 21 | Overweight or obese subjects with T2DM | BMI ≥ 25 kg/m2 | 58.3 ± 5.4 1 | 71 |
| ST | 25 | 23 | 56.1 ± 5.3 1 | 70 | |||||
| CT | 25 | 22 | 57.9 ± 6.5 1 | 77 | |||||
| CG | 25 | 24 | 57.9 ± 7.2 1 | 71 | |||||
| Paoli et al. [64] | 2013 | Italy (Europe) | ET | 21 | 20 | Healthy untrained overweight middle-aged men | BMI > 25 kg/m2 | 61 ± 3.3 1,6 | 0 |
| CT 11 | 20 | 19 | |||||||
| CT 12 | 19 | 19 | |||||||
| Venojärvi et al. [65] | 2013 | Finland (Europe) | ET | 48 | 39 | Overweight and obese middle-aged men with impaired glucose tolerance | BMI: 25.1–34.9 kg/m2 | 55 ± 6.2 1 | 0 |
| ST | 49 | 36 | 54 ± 6.1 1 | ||||||
| CG | 47 | 40 | 54 ± 7.2 1 | ||||||
| Ho et al. [66] | 2012 | Australia (Australia) | ET | 25 | 15 | Overweight or obese men and women, sedentary or relatively inactive, participating in less than 1 h of moderate-intensity physical activity per week over the last 3 months | BMI >25 kg/m2 or WC > 80 cm for women and WC > 90 cm for men | 55 ± 1.2 13 | 80 |
| ST | 26 | 16 | 52 ± 1.1 13 | 81 | |||||
| CT | 25 | 17 | 53 ± 1.3 13 | 82 | |||||
| CG | 21 | 16 | 52 ± 1.8 13 | 94 | |||||
| Stensvold et al. c [67] | 2012 | Norway (Europe) | ET | 11 | 11 | Inactive subjects with metabolic syndrome | BMI ≥ 30 kg/m2 or WC ≥ 80 cm for women or WC ≥ 94 cm for men | 49.9 ± 10.1 1 | 23 |
| ST | 11 | 10 | 50.9 ± 7.6 1 | ||||||
| CG | 11 | 10 | 47.3 ± 10.2 1 | ||||||
| Sukala et al. [68] | 2012 | New Zealand (Australia) | ET | 13 | 9 | Subjects with T2DM and visceral obesity | WC ≥ 88 cm for women or WC ≥ 102 cm for men | 51 ± 4 1 48 ± 6 1 | 72 |
| ST | 13 | 9 | |||||||
| Bateman et al. b [13] | 2011 | USA (North America) | ET | 73 | 30 | Sedentary overweight dyslipidaemic subjects | BMI: 25–35 kg/m2 | 51.1 ± 9.49 1 | 47 |
| ST | 66 | 31 | 51.8 ± 11.0 1 | 48 | |||||
| CT | 57 | 25 | 45.8 ± 11.8 1 | 48 | |||||
| Jorge et al. [69] | 2011 | Brazil (South America) | ET | 12 | NI 14 | Overweight or obese subjects with T2DM | BMI: 25–40 kg/m2 | 52.09 ± 8.71 1 | 58 |
| ST | 12 | 54.1 ± 8.94 1 | 58 | ||||||
| CT | 12 | 57.90 ± 8.06 1 | 67 | ||||||
| CG | 12 | 53.42 ± 9.82 1 | 67 | ||||||
| Slentz et al. b [15] | 2011 | USA (North America) | ET | 196 | 48 | Sedentary overweight dyslipidaemic subjects | BMI: 26–35 kg/m2 | 49.5 ± 9.8 1 | 54 |
| ST | 52 | 49.7 ± 11.4 1 | 58 | ||||||
| CT | 44 | 46.9 ± 10.0 1 | 57 | ||||||
| Gram et al. [70] | 2010 | Denmark (Europe) | ET | 22 | 21 | Overweight or obese subjects with T2DM | BMI > 25 kg/m2 | 62 ± 10 1 | 54 |
| CT | 24 | 24 | 59 ± 10 1 | 42 | |||||
| CG | 22 | 22 15/20 16 | 61 ± 10 1 | 41 | |||||
| Stensvold et al. c [22] | 2010 | Norway (Europe) | ET | 11 | NI | Subjects with metabolic syndrome | BMI ≥ 30 kg/m2 or WC ≥ 80 cm for women or WC ≥ 94 cm for men | 49.9 ± 10.1 1 | 40 |
| ST | 11 | 50.9 ± 7.6 1 | |||||||
| CT | 10 | 52.9 ± 10.4 1 | |||||||
| CG | 11 | 47.3 ± 10.2 1 | |||||||
| Ahmadizad et al. [71] | 2007 | Iran (Asia) | ET | 8 | NI | Sedentary obese healthy men | NI | 41.3 ± 5.1 1 | 0 |
| ST | 8 | 40.9 ± 3.2 1 | |||||||
| CG | 8 | 38.6 ± 3.2 1 | |||||||
| Hara et al. [72] | 2005 | Japan (Asia) | ET | 7 | 7 | Young obese men | BMI > 25 kg/m2 | 19.7 ± 1.3 1 | 0 |
| CT | 7 | 7 | 18.4 ± 0.5 1 | ||||||
| CG | 7 | 7 | 19.4 ± 1.0 1 | ||||||
| Banz et al. [73] | 2003 | USA (North America) | ET | 14 | 11 | Men with android obesity and at least one risk factor for coronary artery disease | BMI > 27 kg/m2 and WHR > 0.95 | 47 ± 7 1 | 0 |
| ST | 12 | 8 | 48 ± 6 1 | ||||||
| Cuff et al. [74] | 2003 | Canada (North America) | ET | 9 | 9 | Postmenopausal women with T2DM, central obesity and an inactive lifestyle | WC > 90 cm | 59.4 ± 1.9 4 | 100 |
| CT | 10 | 10 | 63.4 ± 2.2 4 | ||||||
| CG | 9 | 9 | 60.0 ± 2.9 4 |
| Author | Year | Groups | Characteristic of Groups/Training (Including Volume) | Intensity of Training [%] | Duration of Training [min] | Frequency of Training [Days per Week] | Time of Intervention [Weeks] | Supervision |
|---|---|---|---|---|---|---|---|---|
| Jamka et al. [38] | 2021 | ET | Cycling on ergometer | 50–70% of HR max | 60 | 3 | 12 | Yes |
| CT | ET: Cycling on ergometer ST: Exercises with a barbell (16 repetitions per set) and a gymnastic ball (30 repetitions per set); between the series 10–15 s pauses were taken | ET: 50–70% of HR max ST: 50–60% of 1 RM | ||||||
| Banitalebi et al. [39] Banitalebi et al. [40,75] | 2021 2019 | ET | Sprint interval training on cycle ergometers at a pedalling rate of 20 rpm | 60–70% of HR max 1 | 20–50 1 | 3 | 10 | Yes |
| CT | ET: Treadmill or cycle ergometer ST: 1–3 set of 5 exercises of 10–15 repetitions with 10–15 RM 1 and 2–3 min rest between sets 1; training on weight stack machines: bilateral leg press, lateral pulldown, bench press, bilateral biceps curl, and bilateral triceps pushdown | ET: 60–70% of HR max 1 ST:NI | ||||||
| CG | Continued their usual medical care and received diabetes recommendations for self-management | N/A | N/A | N/A | ||||
| Amanat et al. a [41] Dianatinasab et al. a [42] | 2020 | ET | Running on the treadmill | 60–75% of HR max 1 | 30–60 1 | 3 | 12 (Amanat et al. [41]) 8 (Dianatinasab et al. [42]) | Yes |
| ST | 2 sets of 10 different exercises of 8–10 repetitions for each exercise and 5–10 min of rest between each set: bench press, seated row, shoulder press, chest press, lateral pulldown, abdominal crunches, leg press, leg extension, triceps pushdown, and seated bicep curls, for upper and lower parts of the body | 60–80% of 1 RM 1 | 60 | 2–3 1 | ||||
| CT | Walking on a treadmill, followed by 5 min rest and 1 set of strength training (different exercises similar to the ST group) | ET: 60–75% of HR max 1 ST: 60–80% of 1 RM 1 | 60 (including ET: 20) | 2–3 1 | ||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Dupuit et al. [37] | 2020 | ET 2 | Cycling program, energy expenditure: 180 ± 22 4 | 55–60% of peak power output 1 | 40 | 3 | 12 | Yes |
| ET 3 | Cycling programme (repeated cycles of sprinting/speeding for 8 s followed by slow pedalling (20–30 rpm) for 12 s), energy expenditure: 180 ± 22 4 | 80–90% of HR peak | 20 | |||||
| CT | ET: Cycling programme (repeated cycles of sprinting/speeding for 8 s followed by slow pedalling (20–30 rpm) for 12 s) ST: 2 different whole-body training programme each consisting of 1 set of 10 exercises of 8–12 repetitions with 1–1.5 min rest period between exercises: 1. Included leg press, bench press, knee extension, cable row, dumbbell calf raise, elbow flexion, abdominal muscle, triceps exercises with upper pulley, plank, and bum exercises 2. Included knees extension, pullover, leg press, side raise with dumbbells, dumbbell calf raise, triceps exercises with upper pulley, hip thrust, chin rowing, and plank to upright row | ET: 80–90% of HR peak ST: 80% of 1 RM | 40 (ET: 20 + ST: 20) | |||||
| Kim et al. [43] | 2020 | ET | Jogging and running outdoors or indoor exercise using stationary cycling | 65–85% of HR max | 30–60 1 | 3 | 12 | Yes |
| ST | 3 sets of 7 exercises of 10–15 repetitions with 1–2 min of rest between each set: crunch, high lat pulldown, seated row, chest press, leg press, leg extension and leg curl | ~50% of 1 RM | 60 | |||||
| Christensen et al. [44] | 2019 | ET | High-intensive interval exercise on an ergometer bicycle | NI | 45 | 3 | 12 | Yes |
| ST | 3–5 sets of 10 exercises | 60–80% of 1 RM 1 | ||||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Keihanian et al. [45] | 2019 | ET | Running | 65–75% of HR max (abstract) 75–85% of HR max (method) | 30–45 | 3 | 10 5 | Yes |
| ST | 3 sets of 10 RM of 7 exercises with 1.5 min rest between sets and 2 min rest between exercises: leg press, bench press, knee extension, seated cable row, knee flexion, military press, and calf rise | NI | 60 | |||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Mohammad Rahimi et al. [46] | 2019 | ET | 4 × 4 min intervals of walking/running on a treadmill, with 3 min exercise between each interval | 90% of HR peak (intervals) 70% of HR peak (between intervals) | 43 | 3 | 12 | Yes |
| ST | 2–3 sets of 7 weight machines exercises of 8–20 repetitions: lateral pulldown, chest press, seated row, triceps pushdown, knee flexion, knee extension, and leg press | 40–80% of 1 RM 1 | 45 | |||||
| CT | Exercises were similar to the practices of the other two groups | ET: 90% of HR peak (intervals) 70% of HR peak (between intervals) ST: 40–80% of 1 RM 1 | ET: 43 (performed in the week of 1, 3, 5, 7, 9 and 11 twice a week and ST once a week), ST: 45 (performed in the weeks of 2, 4, 6, 8, 10 and 12 twice a week and ET once a week) | |||||
| CG | The group was advised not to change their physical activity levels throughout the intervention | N/A | N/A | N/A | ||||
| Ratajczak et al. [47] | 2019 | ET | Training on cycle ergometers | 60–80% of HR max | 60 | 3 | 13 | Yes |
| CT | ET: Similar as described for ET ST: Exercises using a neck barbell and gymnastics ball: upper limb exercises with a neck barbell on Mondays; spine-stabilising exercises, deep muscle-forming exercises, and balance-adjusting exercises with a gymnastic ball on Wednesdays; lower limb exercises with a neck barbell on Fridays; the number of repetitions was systematically increased with the increase in subject’s muscle strength | ET: 60–80% of HR max ST: 50–60% of 1 RM | 60 (ET: 25 + ST: 20 + warm up: 5 + cool down: 10) | |||||
| Martins et al. [48] | 2018 | ET | High-intensity interval body weight training; 10 sets of vigorous exercises (30 s of stair climbing and 30 s of body weight squats) interspersed by 60 s of a light walk 6 | >85% of HR max + recovery at 60–70% of HR max | 36 | 3 | 12 | Yes |
| CT | ET: Moderate walking ST: 1–3 sets of 5 resistance exercises of 8–12 repetitions 1 with 1.5 min. rest intervals between the sets and exercises (half squat, bench press, leg curl, rowing machine, and unilateral leg extension) | ET: 70% of HR max ST: 70% of 1 RM 6 | 68 (including 30 min. of ET 6) | |||||
| Roberson et al. [49] | 2018 | ET | Moderate-intensity treadmill training | 55% of HR reserve (±2 bpm) | Prescription time: 35 Actual time: 33 ± 2 7 | 3 | 12 | Yes |
| ST | High-velocity circuit resistance training of 2–3 rotations 1 of 11 exercises of 12 repetitions at the specified optimal load (%1RM) in the following order: chest press (50%), leg press (60%), latissimus dorsi pulldown (40%), hip adduction (70%), overhead press (60%), leg curl (60%), seated row (50%), hip abduction (70%), elbow extension (50%), plantar flexion (60%), and elbow flexion (50%) | Börg scale: 6.0 ± 0.2 7 | Actual time: 30 ± 2 7 | |||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Alvarez et al. [50] | 2017 | ET | High-intensity interval training on cycle ergometers, energy expenditure: 45 kcal/kg/min, ~540 kcal/week | Börg scale: 8–10 70–100% of HR reserve | 38 | 3 | 12 | Yes |
| ST | 4 exercises per session: biceps curl, shoulder press, and upper row, which were performed using free weights and metal bars, and leg extension using the exercise machine; the programme consisted of an interval of working for 60 s; each interval of work was repeated 3 times and was interspersed by an inactive recovery period of 120 s; energy expenditure: 45 kcal/kg/min, ~540 kcal/week | Börg scale: 8–10 20–50% of 1 RM 1 | 36 | |||||
| AminiLari et al. [51] | 2017 | ET | Training on cycle ergometer | 50–55% of HR max 5.5–7.1 MET | 45 1,5 (25 ET + 20 warm-up) | 3 | 12 | NI |
| ST | 3 sets of 6 weight training exercises of 8 repetitions (leg extension, prone leg curl, abdominal crunch, biceps, triceps, and seated calf) | 50–55% of 1 RM 5.5–7.1 MET | NI 1 (20 warm-up) | |||||
| CT | Consisted of ET integrated with ST | ET: 50–55% of HR max ST: 50–55% of 1 RM Total: 5.5–7.1 MET | half the execution time of ET/ST | |||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Arslan et al. [52] | 2017 | ET | Major muscle group exercises using basic steps and a minimum of three rhythmic variations of popular dance styles and aerobics | 60–70% of HR max | 80 (60 ET + 10 warm-up and 10 cool-down) | 3 | 34 | Yes |
| CT | ET: Similar as described for ET ST: 3 sets of 9 exercises of 15–20 repetitions with 2–3 min between sets; the major muscle groups of the upper and lower limbs were exercised with the use of free weights (dumbbells); exercises used in the programme: biceps curl, triceps extension, sit up, squat, side elevation, shoulder press, side bends, pectoral fly and upright row | ET: 60–70% of HR max ST: 60–70% at 1 RM 1 | 60 (ET: 35 + ST: 25) | |||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Oh et al. [53] | 2017 | ET 3 | 3 sets of 3 min cycling with a 2 min active rest between sets, energy expenditure: 180 kcal | 80–85% of VO2 max (rest at 50% of VO2 max) | 13 | 3 | 12 | Yes |
| ET 2 | Cycling, energy expenditure: 360 kcal | 60–65% of VO2 max | 40 | |||||
| ST | Consisted of sit-ups, leg presses, leg extensions, leg curls, chest presses, seated rows, and pulldown, energy expenditure: 180 kcal | To 60% of 1 RM for lower body exercises 30–60% of 1 RM for upper body exercises | NI | |||||
| Said et al. [54] | 2017 | ET | High-impact training involves rhythmic exercises routine in which both feet leave the ground: side by side, step touch, side slot, v-step, grapevine, pivot, cha cha cha, mambo rock-line dance, diamond step, hamstring-curl, heel touch, sit-up and push up, fast walking, turn round, heel side, knee-up, scissors double, hop and jump, jumping jack, side kick, full turn, double kick | 70–85% of HR max 1 | 50–60 | 4 | 24 | Yes |
| CT | ET: Low-impact rhythmic exercises ST: 2 sets of muscle-strengthening exercises, with 15 s of rest between exercises and 3 min between sets, conducted on resistance machines: leg extension, leg flexion, bench press, shoulder press, triceps extension, and biceps curl; sit-ups for the abdominal muscles were also performed in all sessions; rhythmic exercises were performed without any jumping (side by side, step touch, side slot, v-step, grapevine, pivot, cha cha cha, mambo rock-line dance, diamond step, hamstring-curl, heel touch, sit-up and push up | ET: 50–65% of HR max ST: 60–80% of 1 RM | 60–70 (ET: 30 + ST: 20 + warm-up and cool down: 5–10) | |||||
| Soori et al. [55] | 2017 | ET | Water-based training: swimming or walking in the water | 40–60% of HR max 1 | 45 | 3 | 10 | Yes |
| ST | 3 sets of 6 dynamic exercises with free weights of 10–12 repetitions: bench press, lateral pulldown, rowing, leg press, hip flexion and extension | 40–60% of 1 RM 1 | ||||||
| CT | ET: Swimming ST: 2 sets of 10–12 repetitions of resistance exercises described in the ST group | ET: 40–60% of HR max ST: 40–60% of 1 RM 1 | 44 (ET: 22 + ST: 22) | |||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Wang [56] | 2017 | ET | Aerobics and jogging | 60–70% of HR max | 60 | 3 | 16 | NI |
| CT | ET: Similar as described for ET ST: 3 groups of 6 movement links repeated 6–8 times: flexion and extension of shoulder joints, elbow joints, hip joints, knee joints, and muscles of the trunk | ET: 60–70% of HR max ST: 60–70% of 1 RM | 60 (ET: 40 + ST: 20) | NI | ||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Chen et al. [57] | 2016 | ET | Brisk walking | 60–70% of HR max | NI | 3 | 8 | NI |
| ST | 3 sets of 8 exercise stations, 8–15 repetitions for each station of upper and lower body exercises by using dumbbells | NI | 45 | |||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Rossi et al. [21] | 2016 | ET | Traveling 3 distances (400, 800, and 1,200 m) in the shortest possible | 100% of critical velocity | 52 | 3 | 16 | NI |
| CT | ET: Similar as described for ET ST: 3–4 sets of 8–15 repetition exercises with 60–90 s between sets: leg press, leg extension, leg curl, bench press, seated row, arm curl, triceps extension, side elevation with dumbbells, and abdominal exercises | ET: 100% of critical velocity ST: 65–80% of maximum 1 | 57 (ET: 30 + ST: 27) | |||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Tayebi et al. [58] | 2016 | ET | Running program | 65–85% of HR max 1 | 25–40 1 | 3 | 8 | NI |
| ST | 6 sets of 5 exercises of 3–12 repetitions: leg press, knee extension, lat pulldown, biceps curls, dead lift | 50–80% of 1 RM | NI | |||||
| CT | ET: Similar as described for ET (one or a half-term ET) ST: 3 sets of 5 listed in the ST group exercises, 4–12 repetitions | ET: 65–85% of HR max 1 ST: 50–80% of 1 RM | ||||||
| AbouAssi et al. b [20] Bateman et al. b [13] Slentz et al. b [15] | 2015 2011 2011 | ET | Included treadmill, elliptical trainers, cycle ergometers, or any combination of this equivalent to roughly 19.2 km/wk (12 miles/wk), energy expenditure: 14 kcal/kg/week | 65–80% of VO2 peak 1 | Prescription time: 44 ± 8 4,8 Actual time: 40 ± 7 4,8 | 3 | 34 | Yes |
| ST | 3 sets of 8 exercises of 8–12 repetitions performed on 8 weight-lifting machines designed to target all major muscle groups | 70–85% of 1 RM | 60 | |||||
| CT | The full ET plus the full ST regimens | ET: 65–80% of VO2 peak 1 ST: 70–85% of 1 RM | ET: Prescription time: 45 ± 92 4,8 Actual time: 35 ± 11 4,8 ST: 60 | |||||
| Mahdirejei et al. [14] | 2015 | ET | Run interval training with active relaxation, at 2:1 ratio | 65–80% of HR max 1 | 45–60 | 3 | 4 | Yes |
| ST | 3 circuits of 8 isotonic exercises of 8–12 repetitions for each movement in a circuit; with 30–60 s intervals between each exercise and with 120–180 s intervals between each circuit: squat to press, arm curl, chest press, knee extension, seated rowing, heel raise, overhead press, and leg curl | 60–80% of 1 RM | ||||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Huffman et al. b [59] | 2014 | ET 9 | Low-amount moderate-intensity exercises, energy expenditure: 1200 kcal/week | 40–55% of VO2 peak | NI | NI | 26 | Yes |
| ET 10 | Low-amount vigorous-intensity exercises, energy expenditure: 1200 kcal/week | 65–80% of VO2 peak | 3 | |||||
| ET 11 | High-amount vigorous-intensity exercises, energy expenditure: 2000 kcal/week | |||||||
| ST | 3 sets, 8–12 repetitions of upper and lower body exercises | NI | ||||||
| CT | Linear combination of low-amount vigorous-intensity training and ST | ET: 65–80% of VO2 peak ST: NI | ||||||
| CG | No intervention | N/A | N/A | |||||
| Nikseresht et al. [16] | 2014 | ET | Running on a treadmill; 4 sets of 4 min with 3 min recovery intervals | 80–90% of HR max (recovery intervals at 55–65% of HR max) | 25 12 | 3 | 12 | Yes |
| ST | 1–4 sets of 12 exercises of 2–20 repetitions with 1–7 min of rest period: knee extension, bench press, incline bench press, seated row, dead lift, pulley crunches, lat pulldowns, calf raise, hamstring curl, press behind neck, upright row, arm curl | 40–95% of 1 RM | 40–65 | |||||
| CG | Continued their normal sedentary life | N/A | N/A | N/A | ||||
| Sousa et al. [60] | 2014 | ET | Trained in a land environment and in an aquatic environment; including walking and/or jogging and/or dancing patterns, and muscular endurance, which included 3 exercises (3 sets, 15–20 repetitions) using only bodyweight and gravity for strengthening the lower and upper limbs in a land environment, and water resistance in an aquatic environment; agility exercises in an informal game format (e. g. relay races, water volleyball and water polo) during the training sessions exclusively in the aquatic environment | Moderate-to-vigorous intensity | 60 | 3 | 32 | Yes |
| CT | ET: Similar as described for ET ST: 3 sets of 7 exercises of 8–12 repetitions with 30 s rest periods between sets and 1 min between exercises: bench press, leg press, lateral pulldown, leg extension, military press, leg curl and arm curl and floor exercises for the abdominals and erector spinae muscle groups | 65–75% of 1 RM 1 | ||||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Changela et al. [61] | 2013 | ET | Walking, jogging, aerobic dance with music | 60–70% of HR max | 40 | 3 | 6 | Yes |
| ST | 4 sets of 7 different types of exercises of 10 repetitions; training started with 10 lifts with 50% of 10 RM, then 75% of 10 RM and progressed to 100% of 10 RM; seven different types of exercises such as abdominal curl-ups, biceps curls, triceps extension, back extension, leg curls, side leg raises and knee extension were included | NI | NI | |||||
| Donges et al. [62] | 2013 | ET | Cycling with elliptical cross training | 75–80% of HR max | 40–60 1 | 3 | 12 | Yes |
| ST | Whole-body training program, including chest and shoulder press, seated rows, lat pulldown, leg press, leg curls, lunges, machine squats, and deadlifts; 3–4 sets × 8–10 of each exercise | 75–80% of 1 RM 1 | NI | |||||
| CT | ET: Similar as described for ET ST: 1.5–2 × 8–10 of each exercise described in the ST group | ET: 75–80% of HR max ST: 75–80% of 1 RM 1 | ET: 20–30 ST:NI | |||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Kadoglou et al. [63] | 2013 | ET | Walking or running on a treadmill, cycling or calisthenics | 60–75% of HR max | 60 | 4 | 26 | Yes |
| ST | 2–3 sets of 8 types of exercises of 8–10 repetitions: seated leg press, knee extension, knee flexion, chest press, lat pulldown, overhead press, biceps curl, and triceps extension | 60–80% of 1 RM | 60 1,5 | |||||
| CT | CT: combined training as in aerobic training group and resistance training group with the following pattern weekly: 1 session of ET programme; 1 session of ST; and 2 sessions combining the types of exercise of both ET and ST in the same session | ET: 60–75% of HR max ST: 60–80% of 1 RM | 55 1,5 | |||||
| CG | Patients were encouraged to perform self-controlled, leisure-time physical activity (e.g., walking briskly, cycling outdoor) | Low-to-moderate intensity | 150/week | N/A | ||||
| Paoli et al. [64] | 2013 | ET | Training on cycloergometer + 4 sets of 20 repetitions of abdominal crunches | 50% of HR reserve | 50 (ET: 8 + ST: 42) | 3 | 12 | Yes |
| CT 13 | ET: training on cycloergometer ST: 2 sets of the following exercises: back: underhand cable pulldowns; chest: pectoral machine; shoulders: lateral shoulder raise; lower limbs: horizontal press; abdomen: 1 set of 20 repetitions abdominal crunches performed with 3 sets of rest-pause; every set consists of 6 RM, 20 min recovery, 2 reps at exhaustion 20 min recovery | ET: 3 min at 50% of HR reserve and 1 min at 75% of HR reserve | ||||||
| CT 14 | ET: training on cycloergometer ST: 2 sets of the following exercises: back: underhand cable pulldowns; chest: pectoral machine; shoulders: lateral shoulder raise; lower limbs: horizontal press, the exercises were performed to reach 15 RM; abdomen: 1 set of 20 repetitions abdominal crunches | ET: 50% of HR reserve | ||||||
| Venojärvi et al. [65] | 2013 | ET | Nordic walking consisted of warmup exercises including walking for 5 min and stretching of main muscle groups in addition to walking with poles; after the pole walking, the main muscle groups were stretched for 5 min for cool-down | 55–75% of HR reserve 1 | 60 | 3 | 12 | Yes |
| ST | Started with warm-up exercises (cycling or rowing with ergometer for 5 min and stretching of main muscle groups). The main part of programme was performed by using regular resistance equipment, and the training focus was on strength and power exercises of the lower extremities and trunk but also muscles of the upper extremities were trained. Muscle contractions were performed with maximal or high velocity, and external loads were 50–85% from exercise-specific maximal strength, which was determined by the 5RM; At the end of every session, subjects cooled down by cycling or rowing with the ergometer for 5 min and by stretching the main muscle groups | 50–85% from exercise-specific maximal strength, which was determined by the 5 RM | ||||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Ho et al. [66] | 2012 | ET | Treadmill walking | 60% of HR reserve ± 10 beats/min | 30 | 5 | 12 | No |
| ST | 4 sets of 5 exercises of 8–12 repetitions at 10 RM of leg press, leg curl, leg extension, bench press, rear deltoid row | NI | ||||||
| CT | ET: Similar as described for ET ST: 2 sets of 8–12 repetitions at 10 RM of exercises described in the ST group | ET: 60% of HR reserve ± 10 beats/min ST: NI | 30 (ET: 15 + ST: 15) | |||||
| CG | No exercise, subjects were requested to continue their normal physical activity and received a placebo dietary supplement only | N/A | N/A | N/A | ||||
| Stensvold et al. c [67] Stensvold et al. c [22] | 2012 2010 | ET | Aerobic interval training: as treadmill walking or running (self-selected) consisted of 4 intervals of 4 min at and 3 min active recovery period | Intervals: 90–95% of HR peak Recovery period: 70% of HR peak | 43 | 3 | 12 | Yes |
| ST | 3 sets of 8–12 repetitions; consisted of two different programs including different muscle groups; the following exercises were performed twice weekly (programme 1): low row, bench press, and hack lift; the alternative programme was performed once each week (programme 2): deltoid exercise (lateral raise exercise), triceps pulldown, biceps curl, and low-row and core exercises (plank exercise) | 60–80% of 1 RM 1 | 40–50 15 | |||||
| CT | ET twice a week and ST once a week | ET: 90–95% of HR peak ST: 60–80% of 1 RM 1 | ET: 43 ST: 40–50 13 | |||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Sukala et al. [68] | 2012 | ET | Exercises on a cycle ergometer | 65–85% of HR reserve 1 | 40–60 1 | 3 | 16 | Yes |
| ST | 2–3 sets of 8 exercises of 6–8 repetitions with 1 min rest between sets and exercises; exercises with the use of machine weights targeting all the major muscle groups of the body: seated leg press, knee extension, knee flexion, chest press, lat pulldown, overhead press, biceps curl, and triceps extension | NI | ||||||
| Jorge et al. [69] | 2011 | ET | Cycling programme | HR corresponding to the lactate threshold | 60 | 3 | 12 | Yes |
| ST | Focused on the large muscle groups and consisted of a 7-exercise circuit as follows: leg press, bench press, lat pulldown, seated rowing, shoulder press, abdominal curls, and knee curls | NI | ||||||
| CT | Consisted of ST interchanged with ET performed at the same intensity and half the volume of the ET and ST groups | ET: HR corresponding to the lactate threshold ST:NI | ||||||
| CG | Light stretching exercises | N/A | N/A | |||||
| Gram et al. [70] | 2010 | ET | Nordic walking | At least 40% VO2 max | 45 | 1–2 | 16 (36 follow up) | Yes |
| CT | Training on ergometer cycles, rowing machines, step machines, and strength training machines (for chest and leg, upper back, and knee extension and flexion) | ET: At least 40% VO2 max CT: Börg scale 13–14 | ||||||
| CG | Written information about exercises and advice to be physically active | N/A | N/A | N/A | ||||
| Ahmadizad et al. [71] | 2007 | ET | Continuous running | 75–85% of HR max | 20–30 1 | 3 | 12 | Yes |
| ST | 4 sets of circuit weight training for 11 stations; the maximum number of repetitions in each station was 12; exercises involving the upper and lower body | 50–60% of 1 RM | 50–60 | |||||
| CG | No intervention | N/A | N/A | N/A | ||||
| Hara et al. [72] | 2005 | ET | Training on treadmills and cycle ergometers | 40.8–54.8% of VO2 max | 30–45 | 3 | 8 | NI |
| CT | ET: Similar as described for ET ST: Exercises: arm curl, triceps extension, and shoulder press for upper-limb training; squat, leg press, leg curl, leg extension, and calf raise for lower-limb training; and bench press, seated butterfly, lat pulldown, trunk curl, back extension, and dead lift for trunk training. Participants selected 2 types each from the upper and lower limb training options, and 3 from trunk training choices, and thus performed 7 exercises in each training session; 3 sets for each exercise consisting of 10 repetition | ET: 40.8–54.8% of VO2 max ST: 80% of 1 RM | 80–90 (ET: 30+ ST: 50–60) | ET: 3+ R: 2–3 | 22 | |||
| CG | No intervention | N/A | N/A | N/A | NI | |||
| Banz et al. [73] | 2003 | ET | Training with ski exercise equipment | 60–85% of HR max | 40 | 3 | 10 | Yes |
| ST | 3 sets of lifts using sub-maximal effort to complete each of 10 lifts/set; 8 different exercises during each workout: military press, leg extension, bench press, leg curl, lateral pulldown, triceps pushdown, biceps curl, and sit-ups | NI | N/A | |||||
| Cuff et al. [74] | 2003 | ET | Programme with using treadmills, stationary bicycles, recumbent steppers, elliptical trainers, and rowing machines | 60–75% of HR reserve | 75 | 3 | 16 | Yes |
| CT | ET: Similar as described for ET ST: 2 sets of 5 stack weight equipment exercises of 12 repetitions: leg press, leg curl, hip extension, chest press, and latissimus pulldown | ET: 60–75% of HR reserveST: NI | ||||||
| CG | No intervention | N/A | N/A | N/A |
| Author | Year | Group | Glucose [mmol/L] | Insulin [µU/mL] | HbA1c [%] | HOMA | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Changes | Pre | Post | Changes | Pre | Post | Changes | Pre | Post | Changes | |||
| Jamka et al. [38] | 2021 | ET CT | 5.49 ± 0.72 1 5.49 ± 0.83 1 | 5.67 ± 0.89 1 5.5 ± 0.67 1 | 0.17 ± 0.55 1,2 0 ± 0.44 1,2 | 14.7 ± 7.0 1 15.7 ± 8.4 1 | 15.5 ± 10.4 1 15.3 ± 9.2 1 | 0.5 ± 10.6 1,2 −1.4 ± 10.7 1,2 | 5.6 ± 0.4 1 5.6 ± 0.4 1 | 5.6 ± 0.4 1 5.7 ± 0.3 1 | 0.0 ± 0.5 1,2 0.1 ± 0.5 1,2 | 3.66 ± 1.99 1 3.88 ± 2.19 1 | 4.04 ± 3.27 1 3.75 ± 2.35 1 | −0.12 ± 2.36 1,2 −0.44 ± 2.44 1,2 |
| Banitalebi et al. [39] Banitalebi et al. [40,75] | 2021 2019 | ET | 11.67 ± 1.83 1,3 | 7.63 ± 1.83 1,3 | −4.04 3,5 | 10.08 ± 5.43 1 | 8.18 ± 5.75 1 | −1.9 5,6 | 9.64 ± 1.08 1 | 7.82 ± 0.93 1 | −1.82 (−2.5–−1.14) 4,7 | 1.63 ± 0.83 1 | 1.15 ± 0.74 1 | 0.21 5 |
| 8.21 ± 2.29 1,3,4 | 4.97 ± 1.3 1,4 | −5.11 (−7.76–−2.46) 4,7 | ||||||||||||
| CT | 11.92 ± 1.54 1,3 | 9.10 ± 3.97 1,3 | −2.82 3,5 | 10.37 ± 5.35 1 | 8.83 ± 7.60 1 | −1.54 5,6 | 9.49 ± 0.86 1 | 8.25 ± 1.22 1 | −1.24 (−2.19–−0.29) 4,7 | 1.13 ± 0.28 1 | 0.95 ± 0.24 1 | 1.38 5 | ||
| 11.99 ± 3.50 1,3,4 | 5.93 ± 2.24 1,4 | −4.44 (−7.20–−1.68) 4,7 | ||||||||||||
| CG | 11.16 ± 2.60 1,3 | 10.58 ± 3.32 1,3 | −0.58 3,5 | 9.55 ± 4.05 1 | 9.16 ± 3.75 1 | −0.39 5,6 | 9.10 ± 0.51 1 | 9.12 ± 1.41 1 | 0.02 (−0.67–0.71) 4,7 | 1.39 ± 0.63 1 | 1.42 ± 0.71 1 | 1.12 5 | ||
| 10.95 ± 2.61 1,3,4 | 11.28 ± 3.37 1,3,4 | 9.21 ± 2.06 1,4 | −0.33 (−2.49–1.83) 4,7 | |||||||||||
| p 8 | p = 0.0001 (group) p = 0.03 (time × group) ET: p = 0.001 (pre vs. post) 4 | p = 0.02 (group) ET, CT: p = 0.001 (pre vs. post) 4 0.036 (between groups) 4 | p = 0.0001 (group) p = 0.006 (time × group) ET: p = 0.0001 (pre vs. post) CT: 2021: p = 0.01, 2019: p = 0.002 (pre vs. post) | p = 0.007 (group) p = 0.02 (time × group) | ||||||||||
| Amanat et al. a [41] | 2020 | ET ST CT CG | 8.77 ± 1.74 1,3 8.83 ± 1.72 1,3 9.01 ± 1.51 1,3 9.08 ± 1.21 1,3 | 8.51 ± 1.76 1,3,9 8.65 ± 1.61 1,3,9 8.64 ± 1.51 1,3,9 9.13 ± 1.31 1,3,9 | −0.26 ± 0.27 1,2,3,10,11 −0.18 ± 0.29 1,2,3,10,11 −0.36 ± 0.27 1,2,3,10,11 0.05 ± 0.22 1,2,3,10,11 | 10.62 ± 1.03 9 10.66 ± 1.50 9 10.60 ± 1.35 9 10.34 ± 1.55 9 | 10.03 ± 0.91 9 9.91 ± 1.56 9 9.05 ± 1.27 9 10.46 ± 1.7 9 | −0,58 ± 0.63 2,10,11 −0.74 ± 0.66 2,10,11 −1.55 ± 1.16 2,10,11 0.12 ± 0.063 2,10,11 | NI | NI | NI | 4.11 ± 0.74 9 4.13 ± 0.67 9 4.24 ± 0.95 9 4.18 ± 0.85 9 | 3.69 ± 0.77 9 3.72 ± 0.68 9 3.48 ± 0.83 9 4.20 ± 0.99 9 | −0.41 ± 0.27 2,10,11 −0.4 ± 0.53 2,10,11 −0.76 ± 0.46 2,10,11 0.03 ± 0.29 2,10,11 |
| p8 | ET: p = 0.003, ST: p = 0.037, CT: p < 0.001 (pre vs. post) ET vs. CG, CT vs. CG: p < 0.05 (post) ET, CT vs. CG: p < 0.05 (changes) | ET: p = 0.004, ST: p = 0.001, CT: p < 0.001 (pre vs. post) ST vs. CG, CT vs. CG, CT vs. ET, CT vs. ST: p < 0.05 (post) ST vs. CG, CT vs. CG: p < 0.05 (changes) | ET: p < 0.001, ST: p = 0.012, CT: p < 0.001 (pre vs. post) ET vs. CG: p = 0.022 (post) ST vs. CG: p= 0.032 (post) CT vs. CG: p < 0.001 (post) ET vs. CG, ST vs. CG, CT vs. CG: p < 0.05 (changes) | |||||||||||
| Dianatinasab et al. a [42] | 2020 | ET ST CT CG | 7.16 ± 1.76 1,3 6.42 ± 0.71 1,3 7.26 ± 0.53 1,3 6.62 ± 0.50 1,3 | 5.84 ± 1.56 1 6.29 ± 0.72 1 6.17 ± 0.55 1 6.80 ± 0.50 1 | −1.35 3,5,10 −0.53 3,5,10 −1.08 3,5,10 0.07 3,5,10 | 11.57 ± 1.04 1 10.58 ± 1.55 1 10.72 ± 1.38 1 10.15 ± 1.60 1 | 10.50 ± 1.09 1 9.32 ± 1.52 1 8.45 ± 1.62 1 9.98 ± 1.61 1 | NI | NI | NI | NI | 3.37 ± 0.49 1 3.02 ± 0.65 1 3.46 ± 0.48 1 2.98 ± 0.35 1 | 2.72 ± 0.51 1 2.60 ± 0.64 1 2.31 ± 0.55 1 3.01 ± 0.54 1 | −0.63 5,10 −0.37 5,10 −1.07 5,10 0.04 5,10 |
| p8 | ET: p = 0.011, CT: p = 0.022 (pre vs. post) p = 0.01 (time × group) | ST: p = 0.042, CT: p = 0.011 (pre vs. post) p = 0.007 (time × group) | ET: p = 0.035, ST: p = 0.050, CT: p = 0.001 (pre vs. post) p = 0.001 (time × group) | |||||||||||
| Dupuit et al. [37] | 2020 | ET 12 ET 13 CT | 1.2 ± 0.7 1 1.2 ± 0.3 1 1.2 ± 0.6 1 | 1.2 ± 0.4 1 1.2 ± 0.3 1 1.2 ± 0.7 1 | NI | 11.2 ± 3.0 1 12.9 ± 14.8 1 11.5 ± 3.3 1 | 9.1 ± 3.3 1 12.5 ± 13.0 1 11.7 ± 4.4 1 | NI | 5.6 ± 0.5 1 6.1 ± 0.9 1 5.8 ± 0.2 1 | 5.5 ± 0.4 1 6.0 ± 0.7 1 5.7 ± 0.2 1 | NI | 3.0 ± 1.2 1 3.9 ± 4.7 1 2.8 ± 0.8 1 | 2.2 ± 0.8 1 3.8 ± 4.4 1 3.0 ± 1.4 1 | NI |
| Kim et al. [43] | 2020 | ET ST | 5.45 ± 0.76 1,3 5.52 ± 0.63 1,3 | 5.40 ± 0.63 1,3 5.56 ± 0.92 1,3 | −0.047 ± 0.46 1,3 0.059 ± 0.46 1,3 | NI | NI | NI | NI | NI | NI | 2.24 ± 1.16 1 2.15 ± 1.15 1 | 1.88 ± 0.81 1 2.07 ± 1.14 1 | −0.35 ± 0.84 1 −0.08 ± 0.63 1 |
| Christensen et al. [44] | 2019 | ET ST CG | 5.1 ± 0.5 1,3 4.7 ± 0.4 1,3 5.1 ± 0.5 1,3 | 5.1 (4.9–5.3) 14 5.1 (4.8–5.3) 14 5.0 (4.7–5.3) 14 | −0.2 (−0.4–0.0) 14 −0.2 (−0.4–0.1) 14 −0.1 (−0.3–0.2) 14 | NI | 12.38 (8.78–15.98) 3,14 12.96 (9.07–16.99) 3,14 16.99 (12.96–21.02) 3,14 | −1.23 (−5.47–1.87) 3,14 −1.15 (−5.18–2.74) 3,14 2.74 (−1.30–6.77) 3,14 | 5.8 ± 0.4 1 5.7 ± 0.5 1 6.2 ± 0.6 1 | 4.8 (4.6–4.8) 3,14 4.6 (4.5–4.8) 3,14 4.6 (4.5–4.8) 3,14 | 4 (1–6) 14 1 (−1–4) 14 3 (0–6) 14 | NI | NI | NI |
| Keihanian et al. [45] | 2019 | ET ST CG | 9.59 ± 0.49 1,3 9.68 ± 0.41 1,3 9.35 ± 0.39 1,3 | 7.59 ± 0.27 1,3 7.18 ± 0.42 1,3 8.91 ± 0.63 1,3 | −1.99 3,5 −2.50 3,5 −0.44 3,5 | 8.7 ± 0.2 1 8.6 ± 0.2 1 8.8 ± 0.2 1 | 8.3 ± 0.2 1 8.1 ± 0.2 1 8.7 ± 0.2 1 | −0.39 3,5 −0.50 3,5 −0.10 3,5 | 7.5 ± 1.2 1 7.8 ± 1.1 1 7.2 ± 1.6 1 | 7 ± 1.2 1 6.9 ± 0.8 1 7.2 ± 1.7 1 | −6.6 5 −11.5 5 0 5 | 3.7 ± 0.4 1 3.6 ± 0.3 1 3.5 ± 0.6 1 | 2.8 ± 0.3 1 2.6 ± 0.2 1 3.3 ± 0.6 1 | −0.9 3,5 −1.0 3,5 −0.2 3,5 |
| p8 | ET, ST: p < 0.05 (pre vs. post) ET vs. CG, ST vs. CG, ET vs. ST: p < 0.05 (post) | ET, ST: p < 0.05 (pre vs. post) ET vs. CG, ST vs. CG: p < 0.05 (post) | ET, ST: p < 0.05 (pre vs. post) ET vs. CG, ST vs. CG, ET vs. ST: p < 0.05 (post) | ET, ST: p < 0.05 (pre vs. post) ET vs. CG, ST vs. CG: p < 0.05 (post) | ||||||||||
| Mohammad Rahimi et al. [46] | 2019 | ET ST CT CG | 5.59 ± 0.27 1,3 5.62 ± 0.19 1,3 5.54 ± 0.32 1,3 5.57 ± 0.21 1,3 | 4.78 ± 0.54 1,3 5.43 ± 0.39 1,3 4.51 ± 0.41 1,3 5.53 ± 0.3 1,3 | NI | 23.7 ± 2.7 1 21.7 ± 3.5 1 21.8 ± 3.2 1 22.3 ± 4.2 1 | 13.9 ± 4.1 1 15.2 ± 3.3 1 10.2 ± 2.7 1 23.1 ± 2.7 1 | NI | 6.4 ± 0.8 1 6.5 ± 0.7 1 6.5 ± 0.7 1 6.4 ± 0.8 1 | 4.3 ± 0.7 1 6.0 ± 0.8 1 4.2 ± 0.8 1 6.2 ± 0.9 1 | NI | 5.9 ± 0.7 1 5.4 ± 0.9 1 5.4 ± 0.9 1 5.5 ± 1.1 1 | 3.0 ± 1.0 1 3.7 ± 0.9 1 2.0 ± 0.5 1 5.7 ± 0.8 1 | NI |
| p 8 | ET, CT: p < 0.001 (pre vs. post) ET vs. CG, CT vs. CG: p < 0.05 (post) | ET, ST, CT: p < 0.001 (pre vs. post) ET vs. CG, ST vs. CG, CT vs. CG: p < 0.05 (post) | ET, CT: p < 0.001 (pre vs. post) ET vs. CG, CT vs. CG, ET vs. ST, CT vs. ST: p < 0.05 (post) | ET, ST, CT: p < 0.001 (pre vs. post) ET vs. CG, ST vs. CG, CT vs. CG: p < 0.05 (post) | ||||||||||
| Martins et al. [48] | 2018 | ET CT | 6.09 ± 1.28 1,3 5.28 ± 0.83 1,3 | 5.64 ± 0.78 1,3 5.14 ± 0.95 1,3 | −0.46 3,5 −0.14 3,5 | 13.6 ± 6.11 3,15 9.9 ± 5.8 1,3,15 | 11.1 ± 4.2 1,3,15 8.6 ± 4.7 1,3,15 | −18.3 5,16 −13.1 5,16 | 6.2 ± 0.5 1,3 6.1 ± 0.4 1,3 | 5.9 ± 0.3 1,3 5.9 ± 0.2 1,3 | −4.8 5 −3.3 5 | 3.8 ± 2.2 1,3 2.4 ± 1.7 1,3 | 2.8 ± 1.1 1,3 2.1 ± 1.5 1,3 | −1.0 3,5 −0.3 3,5 |
| p 8 | ET, CT: p < 0.05 (pre vs. post) p = 0.045 (time × group) | ET, CT: p < 0.05 (pre vs. post) p = 0.022 (time × group) | ET, CT: p < 0.05 (pre vs. post) p = 0.021 (time × group) | ET, CT: p < 0.05 (pre vs. post) p = 0.025 (time × group) | ||||||||||
| Roberson et al. [49] | 2018 | ET ST CG | 5.44 ± 0.83 3,17 5.33 ± 0.41 3,17 4.94 ± 0.43 3,17 | 4.94 ± 0.55 3,17 4.83 ± 0.27 3,17 5.12 ± 0.37 3,17 | −0.5 ± 0.22 3,17 | NI | NI | NI | NI | NI | NI | NI | NI | NI |
| p8 | ST: p ≤ 0.05 (pre vs. post) | |||||||||||||
| Alvarez et al. [50] | 2017 | ET ST | 5.8 ± 0.3 1,3 5.7 ± 0.4 1,3 | 5.4 ± 0.5 1,3 5.4 ± 0.4 1,3 | −0.39 ± 0.39 1,3 −0.33 ± 0.39 1,3 | 16.5 ± 4.6 1,18 18.1 ± 4.9 1,18 | 8.7 ± 3.3 1,18 11.2 ± 3.9 1,18 | −7.8 ± 1.3 1,18 −6.9 ± 4.4 1,18 | NI | NI | NI | 4.2 ± 1.1 1 4.4 ± 1.0 1 | 2.1 ± 0.7 1 2.8 ± 1.0 1 | −2.1 ± 0.4 1 −1.6 ± 1.0 1 |
| p8 | p < 0.001 (pre vs. post) | p = 0.003 (pre) p < 0.0001 (pre vs. post) | p = 0.005 (pre) p < 0.0001 (pre vs. post) ET vs. ST: p = 0.026 (post) | |||||||||||
| AminiLari et al. [51] | 2017 | ET ST CT CG | 9.57 ± 1.01 1,3 9.43 ± 1.26 1,3 9.44 ± 1.18 1,3 10.10 ± 0.68 1,3 | 7.76 ± 1.21 1,3 7.18 ± 1.36 1,3 6.86 ± 0.52 1,3 9.26 ± 0.46 1,3 | −2.35 3,5 −2.09 3,5 −2.49 3,5 −0.81 3,5 | 13.25 ± 3.92 1 14.43 ± 3.09 1 12.16 ± 3.62 1 12.70 ± 3.39 1 | 14.90 ± 5.51 1 18.53 ± 5.65 1 13.01 ± 3.62 1 14.30 ± 3.36 1 | 1.73 3,5 4.23 3,5 1.22 3,5 1.83 3,5 | NI | NI | NI | 5.50 ± 1.2 1 5.94 ± 0.98 1 4.97 ± 0.98 1 5.66 ± 1.37 1 | 4.53 ± 0.88 1 18.53 ± 5.65 1,19 3.92 ± 1.11 1 5.90 ± 1.56 1 | −0.9 3,5 −0.3 3,5 −1.0 3,5 0.3 3,5 |
| p8 | ET, CT: p = 0.001 (pre vs. post) ST, CG: p = 0.005 (pre vs. post) ET vs. CG, ST vs. CG, CT vs. CG: p < 0.05 (post) CG: p = 0.02 (pre vs. post) p = 0.001 (group) | ST: p = 0.02 (pre vs. post) | ET: p = 0.004 (pre vs. post) ET vs. ST, ET vs. CG, CT vs. ST, CT vs. CG p < 0.05 (post) CT: p = 0.005 (pre vs. post) CG: p = 0.002 (group) | |||||||||||
| Oh et al. [53] | 2017 | ET 13 ET 12 ST | 2.009 ± 0.008 2,17,20 1.947 ± 0.021 2,17,20 1.991 ± 0.010 2,17,20 | 2.003 ± 0.013 2,17,20 1.962 ± 0.006 2,17,20 1.990 ± 0.015 2,17,20 | −0.006 2,5,17,20 0.015 2,5,17,20 −0.001 2,5,17,20 | NI | NI | NI | NI | NI | NI | 3.45 ± 0.50 17 2.24 ± 0.37 17 2.00 ± 0.24 17 | 3.25 ± 0.48 17 2.18 ± 0.29 17 1.88 ± 0.25 20 | −0.20 5 −0.06 5 −0.12 5 |
| p8 | ET 13 vs. ET 12 vs. ST: p < 0.01 (pre) | ET 13 vs. ET12 vs. ST: p < 0.05 (pre) | ||||||||||||
| Said et al. [54] | 2017 | ET CT | 5.69 ± 0.26 1,3 5.90 ± 0.57 1,3 | 5.62 ± 0.25 1,3 5.85 ± 0.57 1,3 | −0.091 ± 0.046 1,3 −0.060 ± 0.041 1,3 | NI | NI | NI | NI | NI | NI | NI | NI | NI |
| Soori et al. [55] | 2017 | ET ST CT CG | NI | NI | NI | NI | NI | NI | NI | NI | NI | 2.4 ± 0.6 1,3,10 1.8 ± 0.7 1,3,10 2.1 ± 0.9 1,3,10 1.96 ± 0.85 1,3,10 | 1.55 ± 0.55 1,3,10 2.0 ± 0.5 1,3,10 1.6 ± 0.8 1,3,10 2.05 ± 0.95 1,3,10 | −0.52 3,5 NI −0.66 3,5 NI |
| p8 | ET, CT: p < 0.05 (pre vs. post) ET vs. ST: p < 0.05 (post) ET: p = 0.027, CT: p = 0.002 (changes) ET, ST, CT vs. CG: p = 0.029 (post hoc) ET vs. ST: p = 0.03819 (post hoc) | |||||||||||||
| Tayebi et al. [58] | 2016 | ET ST CT | NI | 5.2 ± 0.05 2,3,10 4.9± 0.05 2,3,10 4.4 ± 0.05 2,3,10 | NI | NI | 14.1 ± 0.2 2,3,10 10.7 ± 0.15 2,3,10 15.0 ± 0.2 2,3,10 | NI | NI | NI | NI | NI | 63 ± 2 2,3,10,17 61 ± 2 2,3,10,17 56 ± 2 2,3,10,17 | NI |
| p8 | ET vs. ST, CT vs. ST, CT vs. ET: p = 0.001 | ET vs. ST, CT vs. ST, CT vs. ET: p = 0.001 | CT vs. ET: p = 0.016 | |||||||||||
| AbouAssi et al. b [20] | 2015 | ET ST CT | 5.4 ± 0.8 1,3 5.5 ± 0.6 1,3 5.1 ± 0.6 1,3 | NI | −0.111 ± 0.55 1,3 −0.017 ± 0.05 1,3 0.022 ± 0.48 1,3 | 9.66 ± 6.0 1 8.63 ± 4.0 1 9.93 ± 5.0 1 | NI | −2.03 ± 3.0 1 −0.22 ± 5.0 1 −2.06 ± 2.3 1 | NI | NI | NI | 2.43 ± 1.72 1 2.15 ± 1.12 1 2.21 ± 1.15 1 | NI | −0.59 ± 0.9 1 0.05 ± 1.3 1 −0.24 ± 1.16 1 |
| p8 | ET: p = 0.001 (pre vs. post) CT: p = 0.0005 (pre vs. post) | ET: p = 0.002 (pre vs. post) | ||||||||||||
| Nikseresht et al. [16] | 2014 | ET ST CG | 5.62 ± 0.04 1 6.21 ± 0.04 1 5.92 ± 0.05 1 | 5.36 ± 0.03 1 5.63 ± 0.07 1 5.81 ± 0.09 1 | NI | 5.52 ± 1.72 1 5.80 ± 1.58 1 6.60 ± 1.86 1 | 3.61 ± 1.48 1 3.66 ± 0.92 1 6.20 ± 2.64 1 | NI | NI | NI | NI | 1.39 ± 0.44 1 1.49 ± 0.47 1 1.72 ± 0.42 1 | 0.84 ± 0.34 1 0.84 ± 0.27 1 1.62 ± 0.56 1 | −0.57 3,5 −0.72 3,5 NI |
| p8 | ET, ST: p ≤ 0.05 (pre vs. post) ET, ST vs. CG: p ≤ 0.05 (post) p = 0.001 (time) p = 0.014 (group × time) p = 0.012 (group) | ET, ST: p ≤ 0.05 (pre vs. post) ET, ST vs. CG: p ≤ 0.05 (post) p = 0.001 (time) p = 0.006 (group × time) p = 0.003 (group) | ||||||||||||
| Donges et al. [62] | 2013 | ET ST CT CG | 5.62 ± 0.14 17 5.35 ± 0.13 17 5.53 ± 0.15 17 5.48 ± 0.19 17 | NI | NI | 12.8 ± 2.3 17 11.5 ± 1.8 17 13.1 ± 2.9 17 10.4 ± 2.5 17 | NI | NI | 5.4 ± 0.1 17 5.3 ± 0.1 17 5.3 ± 0.1 17 5.4 ± 0.1 17 | NI | NI | NI | NI | NI |
| Kadoglou et al. [63] | 2013 | ET ST CT CG | 11.59 ± 2.88 1 10.54 ± 1.55 1 11.15 ± 2.88 1 9.87 ± 1.99 1 | NI | −3.21 ± 1.49 1 −0.99 ± 0.38 1 −3.71 ± 1.60 1 −0.33 ± 0.61 1 | 6.96 ± 2.72 1 7.82 ± 1.84 1 7.46 ± 2.99 1 8.93 ± 2.12 1 | NI | −2.97 ± 0.84 1 −2.05 ± 0.75 1 −4.22 ± 1.57 1 −0.22 ± 0.59 1 | 8.3 ± 1.1 1 8 ± 0.7 1 8.2 ± 1 1 7.8 ± 0.8 1 | NI | −0.6 ± 0.1 1 −0.2 ± 0.05 1 −0.9 ± 0.4 1 −0.05 ± 0.01 1 | 3.59 ± 0.66 1 3.67 ± 0.78 1 3.7 ± 1.04 1 3.92 ± 0.43 1 | NI | −2.11 ± 0.87 1 −1.22 ± 0.34 1 −2.63 ± 0.43 1 −0.21 ± 0.05 1 |
| p8 | ET, ST, CT: p < 0.05 (pre vs. post) CT vs. CG: p < 0.001 (changes) CT vs. ST: p = 0.032 (changes) ET vs. CG: p = 0.008 (changes) ST vs. CG: p = 0.018 (changes) ET vs. ST: p < 0.05 (changes) | ET, ST, CT: p < 0.05 (pre vs. post) CT vs. CG: p < 0.001 (changes) CT vs. ST: p = 0.007 (changes) ET vs. CG: p < 0.001 (changes) ST vs. CG: p = 0.019 (changes) ET vs. ST: p < 0.05 (changes) | ET, ST, CT: p < 0.05 (pre vs. post) CT vs. CG: p < 0.001 (changes) CT vs. ST: p = 0.043 (changes) ET vs. CG: p = 0.002 (changes) ST vs. CG: p = 0.048 (changes) ET vs. ST: p < 0.05 (changes) | ET, ST, CT: p < 0.05 (pre vs. post) CT vs. CG: p < 0.001 (changes) CT vs. ST: p < 0.001 (changes) ET vs. CG: p < 0.001 (changes) ST vs. CG: p < 0.001 (changes) ET vs. ST: p < 0.05 (changes) | ||||||||||
| Venojärvi et al. [65] | 2013 | ET ST CG | 6.2 ± 0.1 17 6.1 ± 0.1 17 6.1 ± 0.1 17 | NI | −0.0 ± 0.1 17 −0.1 ± 0.1 17 −0.2 ± 0.1 17 | 12.6 ± 1.2 17 12.9 ± 0.7 17 7.7 ± 0.7 17 | NI | −1.7 ± 1.0 17 −0.8 ± 1.0 17 1.0 ± 0.9 17 | 5.5 ± 0.1 17 5.4 ± 0.1 17 5.4 ± 0.1 17 | NI | 0.0 ± 0.1 17 0.1 ± 0.1 17 0.2 ± 0.1 17 | 3.5 ± 0.4 17 3.6 ± 0.5 17 2.1 ± 0.2 17 | NI | −0.5 ± 0.3 17 −0.3 ± 0.3 17 0.3 ± 0.3 157 |
| p8 | CG vs. ET; CG vs. ST: p = 0.002 (0.006, 0.006) 28 (pre) | CG vs. ET; CG vs. ST: p = 0.004 (0.012, 0.015) 28 (pre) | ||||||||||||
| Ho et al. [66] | 2012 | ET | 5.68 ± 0.17 1 | 5.78 ± 0.18 1,9 | NI | 13.05 ± 1.01 22 | 16.67 ± 1.48 9,22 | NI | NI | NI | NI | 1.72 ± 0.52 22 | NI | NI |
| 5.73 ± 0.10 1,21 | 15.87 ± 1.86 21,22 | |||||||||||||
| ST | 5.81 ± 0.46 1 | 5.81 ± 0.17 1,9 | 13.98 ± 1.40 22 | 16.82 ± 1.33 9,22 | 1.86 ± 0.18 22 | |||||||||
| 5.77 ± 0.16 1,21 | 14.24 ± 1.03 22 | 13.48 ± 1.24 21,22 | ||||||||||||
| CT | 5.38 ± 0.13 1 | 5.31 ± 0.10 1,9 | 17.07 ± 1.33 9,22 | 1.86 ± 0.13 22 | ||||||||||
| 5.55 ± 0.13 1,21 | 14.89 ± 2.29 22 | 14.25 ± 1.25 21,22 | ||||||||||||
| CG | 5.35 ± 0.13 1 | 5.46 ± 0.10 1,9 | 14.82 ± 1.66 9,22 | 1.92 ± 0.28 22 | ||||||||||
| 5.26 ± 0.18 1,21 | 14.76 ± 1.69 21,22 | |||||||||||||
| p8 | ET, ST, CT: p < 0.05 (pre vs. post) | |||||||||||||
| Stensvold et al. c [6] | 2012 | ET ST CG | 6.0 ± 1.1 1 6.6 ± 2.0 1 6.2 ± 2.1 1 | NI | NI | NI | NI | −0.48 (2.11–1.81) 10,23 0.68 (7.45–2.49) 10,23 2.66 (7.03–1.96) 10,23 | NI | NI | NI | NI | NI | NI |
| Sukala et.al. [68] | 2012 | ET ST | 10.2 ± 3.3 1 9.5 ± 3.5 1 | 10.4 ± 2.9 1 11.4 ± 4 1 | 0.2 ± 1.6 1 1.9 ± 3.2 1 | 25.54 ± 11.88 1,3 20.26 ± 14.41 1,3 | 19.41 ± 9.23 1,3 19.31 ± 14.85 1,3 | −6.15 ± 9.47 1,3 −0.95 ± 3.46 1,3 | 8.9 ± 1.9 1 10.7 ± 2.11 | 8.8 ± 2.1 1 10.6 ± 2.4 1 | −0.1 ± 0.6 1 −0.1 ± 1.1 1 | 3.9 ± 1.9 1 2.9 ± 2 1 | 2.9 ± 1.3 1 2.9 ± 1.9 1 | −0.9 ± 1.6 1 0.0 ± 0.5 1 |
| p8 | ET: p = 0.09 (pre vs. post) | |||||||||||||
| Bateman et al. b [13] | 2011 | ET ST CT | 5.35 ± 0.74 1,3 5.54 ± 0.64 1,3 5.02 ± 0.51 1,3 | NI | −0.22 ± 9.54 1 −0.37 ± 9.22 1 1.86 ± 7.95 1 | NI | NI | NI | NI | NI | NI | NI | NI | NI |
| Jorge et al. [69] | 2011 | ET ST CT CG | 8.14 ± 2.33 1,3 10.79 ± 4.42 1,3 8.59 ± 2.35 1,3 8.27 ± 2.40 1,3 | 7.04 ± 2.00 1,3 9.23 ± 3.37 1,3 7.89± 2.04 1,3 6.94 ± 1.14 1,3 | NI | NI | NI | NI | 7.63 ± 1.70 1 8.51 ± 2.45 1 7.6 ± 1.12 1 6.94 ± 0.74 1 | 7.42 ± 1.48 1 8.24 ± 2.13 1 7.53 ± 1.05 1 7.07 ± 0.70 1 | NI | 2.45 ± 1.31 1 4.54 ± 3.94 1 3.14 ± 2.12 1 3.91 ± 4.42 1 | 2.24 ± 1.52 1 4.07 ± 2.90 1 2.59 ± 1.31 1 4.28 ± 5.74 1 | NI |
| p8 | ET, ST, CT, CG: p < 0.05 (pre vs. post) | |||||||||||||
| Slentz et al. b [15] | 2011 | ET ST CT | NI | NI | NI | NI | NI | NI | NI | NI | NI | 2.37 ± 1.6 1 2.08 ± 1.1 1 2.12 ± 1.2 1 | NI | −0.40 ± 0.8 1 −0.09 ± 1.3 1 −0.50 ± 0.9 1 |
| p8 | ET: p = 0.004 (pre vs. post) CT: p = 0.002 (pre vs. post) | |||||||||||||
| Gram et al. [70] | 2010 | ET | NI | NI | NI | NI | NI | NI | 7.2 ± 1.0 1 | 6.9 ± 0.214,24 | NI | NI | NI | NI |
| 7.0 ± 0.214,25 | ||||||||||||||
| CT | 7.2 ± 0.9 1 | 7.2 ± 0.214,24 | ||||||||||||
| 7.5 ± 0.314,25 | ||||||||||||||
| CT | 7.2 ± 0.9 1 | 7.9 ± 0.3 14,24 | ||||||||||||
| 7.6 ± 0.3 14,25 | ||||||||||||||
| Stensvold et al. c [22] | 2010 | ET ST CT CG | 6.0 ± 1.1 1 6.6 ± 2.0 1 6.0 ± 2.4 1 6.2 ± 2.1 1 | 5.9 ± 0.8 1 6.6 ± 1.5 1 5.6 ± 1.8 1 6.1 ± 2.3 1 | −0.2 (−0.71–0.35) 26 0.1 (−0.5–0.6) 26 −0.4 (−1.0–0.3) 26 −0.1 (−0.68–0.43) 26 | NI | NI | NI | 6.19 ± 0.80 1 6.44 ± 0.95 1 6.28 ± 0.78 1 6.12 ± 1.62 1 | 5.95 ± 0.66 1 6.47 ± 1.04 1 6.30 ± 0.76 1 6.24 ± 1.40 1 | −0.25 (−0.51–0.01) 26 0.03 (−0.21–0.33) 26 0.03 (−0.28–0.33) 26 0.10 (−0.17–0.37) 26 | 40.4 ± 8.3 1,16 38.1 ± 17.4 1,16 42.7 ± 24.8 1,16 41.0 ± 12.8 1,16 | 48.4 ± 17.1 1,16 46.5 ± 24.4 1,16 44.9 ± 17.6 1,16 44.3 ± 20.4 1,16 | 8.0 (−2.7–18.8) 16,26 7.5 (−3.8–18.8) 16,26 3.0 (−9.6–15.6) 16,26 3.5 (−7.8–14.7) 16,26 |
| Ahmadizad et al. [71] | 2007 | ET ST CG | 5.21 ± 0.77 1 5.09 ± 0.65 1 NI | 5.16 ± 1.0 1 5.09 ± 0.64 1 NI | NI | 8.54 ± 4.75 1 10.55 ± 3.57 1 NI | 5.73 ± 3.24 1 6.41 ± 3.07 1 NI | NI | NI | NI | NI | 2.0 ± 0.7 1,10 2.4 ± 0.7 1,10 2.25 ± 0.75 1,10 | 1.7 ± 0.3 1,10 1.5 ± 0.8 1,10 2.5 ± 0.7 1,10 | −0.7 3,5 −0.9 3,5 NI |
| p8 | p < 0.05 (pre vs. post) | ET vs. CG, ST vs. CG: p < 0.05 (post) p < 0.05 (pre vs. post) ET vs. CG, ST vs. CG: p < 0.05 (changes) | ||||||||||||
| Hara et al. [72] | 2005 | ET CT CG | 5.3 ± 0.3 1,3 5.6 ± 0.5 1,3 5.9 ± 0.8 1,3 | 5.2 ± 0.1 1,3 5.2 ± 0.3 1,3 5.6 ± 0.5 1,3 | NI | 16.0 ± 6.5 1 8.4 ± 2.9 1 15.0 ± 4.5 1 | 11.0 ± 4.1 1 8.0 ± 0.6 1 16.6 ± 5.9 1 | NI | NI | NI | NI | 3.78 ± 1.62 1 2.15 ± 0.89 1 3.78 ± 0.73 1 | 2.54 ± 0.93 1 1.85 ± 0.25 1 3.92 ± 1.43 1 | NI |
| p8 | CG vs. CT, ET vs. CT: p < 0.05 (pre) | CG vs. CT, ET vs. CT: p < 0.05 (pre) | ||||||||||||
| Banz et al. [73] | 2003 | ET ST | 6.23 ± 1.43 1,3 8.95 ± 2.9 1,3 | 6.48 ± 1.29 1,3 8.07 ± 2.93 1,3 | NI | 3.24 ± 0.98 3 2.92 ± 1.43 3 | 2.89 ± 1.27 3 2.97 ± 1.17 3 | NI | NI | NI | NI | NI | NI | NI |
| Cuff et al. [74] | 2003 | ET CT CG | NI | NI | NI | NI | NI | NI | 6.3 ± 0.2 17 6.9 ± 0.4 17 6.9 ± 0.4 17 | NI | −0.10 ± 0.11 22 −0.1 ± 0.22 22 −0.03 ± 0.20 22 | NI | NI | NI |
| Author | Year | Groups | 2 h Glucose [mmol/L] | 2 h Insulin [µU/mL] | C-Peptide [nmol/l] | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Changes | Pre | Post | Changes | Pre | Post | Changes | |||
| Donges et al. [62] | 2013 | ET | 4311 ± 410 1,2 | 3035 ± 384 1,2 | NI | 9167 ± 1222 1,2 | 5304 ± 560 1,2 | NI | 0.93 ± 0.11 2,3 | NI | NI |
| ST | 4812 ± 690 1,2 | 3765 ± 436 1,2 | 7857 ± 1425 1,2 | 6080 ± 1018 1,2 | 0.86 ± 0.07 2,3 | ||||||
| CT | 4594 ± 820 1,2 | 3958 ± 718 1,2 | 6342 ± 764 1,2 | 5075 ± 763 1,2 | 0.80 ± 0.06 2,3 | ||||||
| CG | 4607 ± 667 1,2 | 4714 ± 974 1,2 | 5591 ± 1019 1,2 | 6411 ± 1222 1,2 | 0.81 ± 0.14 2,3 | ||||||
| p 4 | ET: p < 0.05 (pre vs. post) | CG vs. ET: p < 0.05 (pre, post hoc) ET, CT: p < 0.05 (pre vs. post) | |||||||||
| Venojärvi et al. [65] | 2013 | ET | 6.8 ± 0.3 2 | NI | −0.5 ± 0.3 2 | 80.7 ± 10.1 2 | NI | −15.9 ± 6.4 2 | NI | NI | NI |
| ST | 6.6 ± 0.3 2 | −0.3 ± 0.3 2 | 63.0 ± 8.2 2 | −4.2 ± 4.8 2 | |||||||
| CG | 6.1 ± 0.2 2 | −0.3 ± 0.3 2 | 48.9 ± 6.7 2 | −9.1 ± 3.9 2 | |||||||
| p 4 | p = 0.036 (pre) CG vs. ET: p = 0.042 5 (pre, post hoc) | ||||||||||
| Sukala et al. [68] | 2012 | ET | NI | NI | NI | NI | NI | NI | 1.4 ± 0.3 6 | 1.5 ± 0.7 6 | 0.1 ± 0.5 6 |
| ST | 1.6 ± 1.1 6 | 1.6 ± 1 6 | 0.1 ± 0.5 6 | ||||||||
| Stensvold et al. [22] | 2010 | ET | NI | NI | NI | NI | NI | NI | 1.11 ± 0.24 6 | 1.00 ± 0.42 6 | −0.33 (−0.60–(−0.06)) 7 |
| ST | 1.88 ± 2.37 6 | 1.10 ± 0.46 6 | −0.29 (−0.58–0.1) 7 | ||||||||
| CT | 1.30 ± 0.68 6 | 1.08 ± 0.30 6 | −0.27 (−0.5–0.49) 7 | ||||||||
| CG | 1.12 ± 0.26 6 | 1.18 ± 0.58 6 | −0.15 (−0.44–(−0.14)) 7 | ||||||||
| p 4 | ET: p < 0.05 (pre vs. post) | ||||||||||
| Author | Year | Group | TC [mg/dL] | LDL-C [mg/dL] | HDL-C [mg/dL] | TG [mg/dL] | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Changes | Pre | Post | Changes | Pre | Post | Changes | Pre | Post | Changes | |||
| Jamka et al. [38] | 2021 | ET | 210 ± 48 1 | 209 ± 45 1 | −2 ± 46 1,2 | 124 ± 39 1 | 127 ± 37 1 | 0 ± 41 1,2 | 55 ± 14 1 | 55 ± 13 1 | 0 ± 17 1,2 | 148 ± 93 1 | 134 ± 57 1 | −5 ± 111 1,2 |
| CT | 210 ± 34 1 | 207 ± 34 1 | −4 ± 17 1,2 | 122 ± 30 1 | 121 ± 31 1 | −2 ± 49 1,2 | 61 ± 13 1 | 60 ± 12 1 | −1 ± 15 1,2 | 134 ± 66 1 | 130 ± 50 1 | −2 ± 118 1,2 | ||
| Banitalebi et al. [39] | 2021 | ET | NI | NI | NI | NI | NI | NI | 55.43 ± 8.55 1 | 58.50 ± 1.22 1 | NI | 179.14 ± 79.36 1 | 125.00 ± 21.75 1 | −54.14 (−93.26–−15.02) 3 |
| CT | 49.07 ± 8.26 1 | 50.79 ± 8.64 1 | 159.07 ± 28.64 1 | 135.07 ± 45.86 1 | −24.00 (−49.70–1.70) 3 | |||||||||
| CG | 54.50 ± 4.48 1 | 51.21 ± 6.27 1 | 149.21 ± 74.72 1 | 126.00 ± 40.23 1 | −23.21 (−63.55–17.13) 3 | |||||||||
| p4 | ET: p = 0.025 (pre vs. post) | |||||||||||||
| Amanat et al. a [41] | 2020 | ET | 189.85 ± 34.77 1 | 184.57 ± 34.521 | −5.29 ± 2.88 1,5 −2.79 ± 1.52% 1,6,7 | 93.64 ± 16.86 1 | 91.57 ± 16.35 1 | −1.95 ± 3.27 1,5 −2.08 ± 3.49% 1,6,7 | 52.35 ± 10.42 1 | 56.92 ± 10.11 1 | 4.56 ± 7.48 1,5 | 193.21 ± 50.12 1 | 190.42 ± 50.37 1 | −2.8 ± 3.78 1,5 −1.45 ± 1.96% 1,6,7 |
| ST | 197.28 ± 15.96 1 | 193.50 ± 16.441 | −3.84 ± 5.81 1,5 −1.95 ± 2.95% 1,6,7 | 97.14 ± 34.37 1 | 94.71 ± 34.95 1 | −2.32 ± 2.49 1,5 −2.39 ± 2.56% 1,6,7 | 54.28 ± 12.28 1 | 56.64 ± 12.41 1 | 2.27 ± 5.27 1,5 | 209.28 ± 54.95 1 | 202.64 ± 49.81 1 | −6.39 ± 6.39 1,5 −3.05 ± 3.05% 1,6,7 | ||
| CT | 166.92 ± 37.76 1 | 161.84 ± 37.561 | −5.12 ± 5.6 1,5 −3.07± 3.35% 1,6,7 | 109.69 ± 35.94 1 | 104.38 ± 38.04 1 | −5.18 ± 5.76 1,5 −4.72 ± 5.25% 1,6,7 | 49.61 ± 8.93 1 | 53.69 ± 9.14 1 | 3.99 ± 3.47 1,5 | 199.92 ± 34.17 1 | 191.76 ± 35.04 1 | −8,13 ± 5.04 1,5 −4.07 ± 2.52% 1,6,7 | ||
| CG | 184.85 ± 25.42 1 | 186.42 ± 27.021 | 1.59 ± 3.85 1,5 0.86 ± 2.08% 1,6,7 | 118.75 ± 32.25 1 | 120.59 ± 33.13 1 | 1.92 ± 2.88 1,5 1.61 ± 2.43% 1,6,7 | 50.92 ± 11.71 1 | 52.50 ± 13.24 1 | 1.53 ± 4.18 1,5 | 175.63 ± 27.01 1 | 177.13 ± 29.05 1 | 1.56 ± 3.78 1,5 0.89 ± 2.15% 1,6,7 | ||
| p4 | p = 0.037 (post) ET: p < 0.001, ST: p = 0.030, CT: p = 0.003 (pre vs. post) ET, ST, CT vs. CG: p < 0.05 (changes, post hoc) ET, CT vs. CG: p < 0.05 (post, post hoc) | ET: p = 0.034, ST, CT: p = 0.003 (pre vs. post) CT vs. CG: p < 0.05 (post, post hoc) CT, ST vs. CG: p < 0.05 (changes, post hoc) | ET: p = 0.041, CT: p < 0.001 (pre vs. post) | ET: p = 0.017, CT: p < 0.001 (pre vs. post) CT vs. GC: p < 0.05 (post, post hoc) ST, CT vs. CG: p < 0.05 (changes, post hoc) | ||||||||||
| Dianatinasab et al.a [42] | 2020 | ET | 161.25 ± 10.12 1 | 157.00 ± 9.12 1 | −4.4 5 | 131.58 ± 11.96 1 | 129.50 ± 12.74 1 | NI | 51.91 ± 9.26 1 | 51.08 ± 9.03 1 | NI | 154.41 ± 12.08 1 | 140.75 ± 12.67 1 | −14.34 5 |
| ST | 169.25 ± 14.55 1 | 167.33 ± 12.85 1 | −3.13 5 | 129.58 ± 11.98 1 | 126.33 ± 12.04 1 | 58.16 ± 13.24 1 | 58.83 ± 14.07 1 | 155.41 ± 11.27 1 | 148.66 ± 10.94 1 | −8.36 5 | ||||
| CT | 153.41 ± 13.05 1 | 147.83 ± 13.20 1 | −5.78 5 | 122.41 ± 11.03 1 | 117.25 ± 11.29 1 | 47.25 ± 8.40 1 | 50.08 ± 8.45 1 | 155.41 ± 12.68 1 | 142.75 ± 8.33 1 | −13.57 5 | ||||
| CG | 152.23 ± 8.47 1 | 151.11 ± 9.85 1 | −0.27 5 | 136.61 ± 12.37 1 | 137.30 ± 11.75 1 | 51.84 ± 9.59 1 | 52.00 ± 10.97 1 | 160.53 ± 11.70 1 | 160.00 ± 13.44 1 | −1.04 5 | ||||
| p4 | ET: p = 0.033, CT: p = 0.022 (pre vs. post) CT vs. CG: p < 0.05 (post, change, post hoc) | CT: p = 0.050 (pre vs. post) | p = 0.02 (time × group) ET: p = 0.011, ST: p = 0.022, CT: p = 0.011 (pre vs. post) ET, ST, CT vs. CG: p < 0.05 (post, post hoc) | |||||||||||
| Dupuit et al. [37] | 2020 | ET 8 | 244 ± 50 1,6 | 244 ± 50 1,6 | NI | 135 ± 62 1,6 | 139 ± 54 1,6 | NI | 65.7 ± 15.5 1,6 | 61.9 ± 3.9 1,6 | NI | 124 ± 97.4 1,6 | 97.4 ± 44.2 1,6 | NI |
| ET 9 | 217 ± 43 1,6 | 209 ± 46 1,6 | 128 ± 31 1,6 | 131 ± 31 1,6 | 65.7 ± 34.8 1,6 | 65.7 ± 19.3 1,6 | 106.3 ± 62 1,6 | 79.7 ± 35.4 1,6 | ||||||
| CT | 240 ± 39 1,6 | 240 ± 39 1,6 | 151 ± 39 1,6 | 151 ± 31 1,6 | 65.7 ± 19.3 1,6 | 65.7 ± 15.5 1,6 | 106.3 ± 44.2 1,6 | 106.3 ± 53.2 1,6 | ||||||
| p 4 | p < 0.05 (time) | |||||||||||||
| Kim et al. [43] | 2020 | ET | 199.85 ± 42.75 1 | 195.15 ± 37.83 1 | −4.69 ± 11.94 1 | 119.62 ± 50.81 1 −2.3 ± 6.0% 1,6,7 | 117.46 ± 41.22 1 | −2.15 ± 17.03 1 −1.80± 14.27% 1,6,7 | 56.85 ± 0.09 1 | 57.92 ± 13.48 1 | 1.08 ± 5.27 1 1.90 ± 9.27% 1,6,7 | 127.39 ± 89.30 1 | 120.31 ± 99.20 1 | −7.08 ± 66.47 1 −5.56 ± 52.20% 1,6,7 |
| ST | 205.21 ± 37.77 1 | 201.43 ± 44.88 1 | −3.79 ± 22.98 1 | 129.93 ± 32.40 1 −1.9 ± 11.2% 1,6,7 | 124.71 ± 39.58 1 | −5.21 ± 23.43 1 −4.01 ± 18.03% 1,6,7 | 52.00 ± 9.81 1 | 52.14 ± 10.17 1 | 0.14 ± 6.97 1 0.27 ± 13.40% 1,6,7 | 147.79 ± 112.30 1 | 136.93 ± 77.97 1 | −10.86 ± 50.14 1 −7.35 ± 33.93% 1,6,7 | ||
| Christensen et al. [44] | 2019 | ET | 185.6 ± 34.8 1 | 189 (178–201) 6,10 | −3.3 (−13.3–6.7) 6,8 −1.2 (−6.3–4.0)% 7,8 | 119.9 ± 23.2 1 | 100 (93.3–106.7) 6,8 | −3.33 (−10–3.33) 6,10 −3.6 (−10.9–3.70)% 7,10 | 54.1 ± 11.6 1 | 50.3 (46.4–54.1) 6,10 | 0.0 (−3.86–3.86) 6,10 −0.3 (−6.0–5.4)% 7,10 | NI | NI | NI |
| ST | 185.6 ± 30.9 1 | 189 (178–201) 6,10 | −3.3 (−13.3–6.7) 6,10 −2.3 (−7.6–3.1)% 7,10 | 119.9 ± 27.1 1 | 96.7 (90–106.7) 6,8 | −6.67 (−13.33–0.0) 6,10 −6.0 (−13.5–1.6) % 7,10 | 50.3 ± 7.7 10 | 50.3 (46.4–50.3) 6,10 | 0.0 (−3.86–0.0) 6,10 −3.2 (−9.1–2.7)% 7,10 | |||||
| CG | 197.2 ± 30.9 1 | 182 (4.4–193) 6,10 | 3.3 (−6.7–13.3) 6,10 1.1 (−4.7–7.0)% 7,10 | 127.6 ± 30.9 1 | 110 (100–116.7) 6,10 | 3.33 (−3.33–13.33) 6,10 5.0 (−3.2–13.2)% 7,10 | 46.4 ± 11.6 1 | 50.3 (46.4–54.1) 6,10 | 0.0 (−3.86–3.86) 6,10 2.3 (−4.0–8.7)% 7,10 | |||||
| Keihanian et al. [45] | 2019 | ET | 193.6 ± 12.9 1 | 158.2 ± 17.8 1 | −35.2 6 −18.2% 7 | 101.5 ± 6.7 1 | 89.8 ± 5.4 1 | −11.67 6 −11.5% 7 | 34.9 ± 6.3 1 | 42.8 ± 7.6 1 | 7.88 6 22.6% 7 | 199.2 ± 12.3 1 | 163.9 ± 17.5 1 | −35.26 6 −17.7% 7 |
| ST | 187.8 ± 20 1 | 161 ± 20.7 1 | −26.7 6 −14.2% 7 | 102.6 ± 10.1 1 | 91.5 ± 9.3 1 | −11.08 6 −10.8% 7 | 32.9 ± 6.9 1 | 39.9 ± 7.1 1 | 6.97 6 21.2% 7 | 216.6 ± 29.2 1 | 188.9 ± 30.1 1 | −27.51 6 −12.7% 7 | ||
| CG | 184.5 ± 18.9 1 | 180.8 ± 17 1 | −3.7 6 −2% 7 | 100 ± 8.1 1 | 98.5 ± 8.2 1 | −1.5 6 −1.5% 7 | 35.5 ± 7 1 | 35 ± 6.3 1 | −0.04 6 −0.1% 7 | 184.6 ± 37.5 1 | 183.5 ± 35.6 1 | −1.11 6 −0.6% 7 | ||
| p4 | ET, ST: p < 0.05 (pre vs. post) ET, ST vs. CG: p < 0.05, ET vs. ST: p < 0.05 (post, post hoc) | ET, ST: p < 0.05 (pre vs. post) ET, ST vs. CG: p < 0.05 (post, post hoc) | ET, ST: p < 0.05 (pre vs. post) ET, ST vs. CG: p < 0.05 (post, post hoc) | ET, ST: p < 0.05 (pre vs. post) ET, ST vs. CG: p < 0.05, ET vs. ST: p < 0.05 (post, post hoc) | ||||||||||
| Mohammad Rahimi et al. [46] | 2019 | ET | 221.0 ± 14.6 1 | 179.3 ± 14.9 1 | NI | 174.4 ± 14.6 1 | 120.1 ± 17.0 1 | NI | 32.6 ± 3.6 1 | 49.6 ± 3.7 1 | NI | 164.5 ± 16.8 1 | 121.2 ± 11.3 1 | NI |
| ST | 222.2 ± 15.6 1 | 211.1 ± 15.4 1 | 173.6 ± 12.7 1 | 169.6 ± 12.4 1 | 34.1 ± 5.3 1 | 36.7 ± 5.8 1 | 165.8 ± 15.4 1 | 152.8 ± 14.8 1 | ||||||
| CT | 225.5 ± 13.3 1 | 181.0 ± 16.4 1 | 175.2 ± 12.4 1 | 140.9 ± 10.6 1 | 33.9 ± 4.0 1 | 46.7 ± 7.0 1 | 167.3 ± 13.5 1 | 125.4 ± 10.5 1 | ||||||
| CG | 223.4 ± 17.6 1 | 225.3 ± 16.1 1 | 173.5 ± 11.1 1 | 174.2 ± 12.1 1 | 34.6 ± 4.3 1 | 34.8 ± 4.1 1 | 163.6 ± 14.8 1 | 162.6 ± 13.7 1 | ||||||
| p4 | ET, ST, CT: p < 0.05 (pre vs. post) ET, CT vs. CG: p < 0.05; ET, CT vs. ST: p < 0.05 (post, post hoc) | ET, ST, CT: p < 0.05 (pre vs. post) ET, CT vs. CG: p < 0.05; ET, CT vs. ST: p < 0.05 (post, post hoc) | ET, ST, CT: p < 0.05 (pre vs. post) ET, CT vs. CG: p < 0.05; ET vs. ST: p < 0.05 (post, post hoc) | ET, ST, CT: p < 0.05 (pre vs. post) ET, CT vs. CG: p < 0.05; ET vs. ST: p < 0.05 (post, post hoc) | ||||||||||
| Ratajczak et al. [47] | 2019 | ET | 217.3 ± 39.6 1,6 | 203.8 ± 37.7 1,6 | NI | 130.4 ± 30.8 1,6 | 121.5 ± 33.8 1,6 | NI | 51.2 ±13.8 1,6 | 55.8 ± 13.1 1,6 | NI | 133.74 ± 54.91 1,6 | 136.40 ± 66.43 1,6 | NI |
| CT | 225 ± 41.2 1,6 | 212.3 ± 41.9 1,6 | 138.1 ± 26.9 1,6 | 126.9 ± 29.6 1,6 | 55.4 ± 21.5 1,6 | 60 ± 18.8 1,6 | 117.80 ± 46.06 1,6 | 116.03 ± 51.37 1,6 | ||||||
| p4 | ET, CT: p < 0.05 (pre vs. post) | CT: p < 0.05 (pre vs. post) | ET: p < 0.01 (pre vs. post) | |||||||||||
| Roberson et al. [49] | 2018 | ET | NI | NI | NI | NI | NI | NI | 51.5 ± 5.4 11 | 55.9 ± 6.6 11 56.5 ± 2.6 2 | 4.38 ± 1.76 11 | 147.5 ± 19.8 11 | 138.4 ± 19.9 11 128.0 ± 14.2 2 | NI |
| ST | 50.2 ± 3.0 11 | 54.1 ± 3.6 11 56.1 ± 2.5 2 | NI | 127.9 ± 16.8 11 | 117.8 ± 11.3 11 125.8 ± 13.32 | |||||||||
| CG | 55.7 ± 5.2 11 | 61.2 ± 6.2 11 57.4 ± 3.0 2 | 134.5 ± 30.4 11 | 142.5 ± 42.1 11 144.3 ± 16.3 2 | ||||||||||
| p4 | ET: p = 0.04 (pre vs. post) | |||||||||||||
| Arslan et al. [52] | 2017 | ET | 195.7 ± 13.8 1 | 181.5 ± 13.6 1 | −15.2 6 −7.9% 7 | 119.6 ± 13.8 1 | 114.8 ± 13.5 1 | −4.8 6 −4.4% 7 | 54.2 ± 7.9 1 | 57.0 ± 8.0 1 | 2.80 6 4.8% 7 | 107.9 ± 12.3 1 | 102.0 ± 12.1 1 | −9 6 −5.8% 7 |
| CT | 207.1 ± 18.5 1 | 188.8 ± 15.2 1 | −18.3 6 −9.7% 7 | 110.2 ± 13.4 1 | 105.3 ± 13.8 1 | −4.9 6 −4.6% 7 | 53.1 ± 8.3 1 | 56.0 ± 8.7 1 | 2.9 6 5.3% 7 | 101.3 ± 14.6 1 | 94.8 ± 14.4 1 | −6.5 6 −6.9% 7 | ||
| CG | 200.3 ± 18.9 1 | 202.2 ± 19.1 1 | 1.9 0.9% 7 | 112.2 ± 12.9 1 | 115.6 ± 13.3 1 | 3.4 6 2.9% 7 | 51.6 ± 8.1 1 | 50.8 ± 7.5 1 | −0.8 6 −1.4% 7 | 103.4 ± 9.1 1 | 105.6 ± 8.6 1 | 2.2 6 2.0% 7 | ||
| p4 | ET, CT vs. CG: p = 0.022 (changes, post hoc) | ET, CT vs. CG: p = 0.012 (changes, post hoc) | ||||||||||||
| Oh et al. [53] | 2017 | ET 9 | NI | NI | NI | NI | NI | NI | NI | NI | NI | 130.62 ± 1.12 1,6,12 | 123.31 ± 1.10 1,6,12 | −0.025 12 |
| ET 8 | 151.01 ± 1.22 1,6,12 | 128.53 ± 1.17 1,6,12 | −0.070 12 | |||||||||||
| ST | 110.15 ± 1.15 1,6,12 | 114.29 ± 1.15 1,6,12 | 0.016 12 | |||||||||||
| Said et al. [54] | 2017 | ET | 207.5 ± 14.36 1 | 196.5 ± 17.88 1 | −14.0 ± 12. 1 1,6 −6.75 ± 5.84% 1,7 | 152.4 ± 15.3 1 | 143.6 ± 16.6 1 | −9.30 ± 6.49 1,6 −6.1 ± 4.26% 1,7 | 47.2 ± 2.7 1 | 51.4 ± 3.62 1 | 4.48 ± 2.55 1,6 9.5 ± 5.4% 1,7 | 133.8 ± 5.1 1 | 121.8 ± 8.3 1 | −15.30 ± 7.65 1,6 −11.57 ± 5.75% 1,7 |
| CT | 203.4 ± 21.40 1 | 195.0 ± 19.02 1 | −10.6 ± 9.2 1,6 −5.23 ± 4.51% 1,7 | 147.7 ± 18.13 1 | 140.9 ± 13.25 1 | −7.55 ± 6.20 1,6 −5.11 ± 4.2% 1,7 | 48.4 ± 6.7 1 | 52.2 ± 4.5 1 | 4.02 ± 6.3 1,6 8.3 ± 6.3% 1,7 | 130.7 ± 12.07 1 | 119.0 ± 11.68 1 | −13.16 ± 12.46 1,6 −10.07 ± 9.53% 1,7 | ||
| p4 | ET, CT: p < 0.05 (pre vs. post) | ET, CT: p < 0.05 (pre vs. post) | ET, CT: p < 0.01 (pre vs. post) | CT: p < 0.05; ET: p < 0.01 (pre vs. post) | ||||||||||
| Soori et al. [55] | 2017 | ET | 242 ± 23 1 | 215 ± 19 1 | NI | 169 ± 22 1 | 139 ± 22 1 | NI | 50.9 ± 8.7 1 | 58.6 ± 10.4 1 | NI | 120 ± 20 1 | 102 ± 19 1 | NI |
| ST | 253 ± 49 1 | 250 ± 48 1 | 170 ± 38 1 | 167 ± 43 1 | 59.5 ± 6.8 1 | 58.6 ± 6.9 1 | 116 ± 52 1 | 118 ± 48 1 | ||||||
| CT | 233 ± 40 1 | 198 ± 39 1 | 153 ± 45 1 | 160 ± 39 1 | 47.4 ± 11.7 1 | 55.3 ± 15.1 1 | 115 ± 27 1 | 87 ± 10 1 | ||||||
| CG | 217 ± 25 1 | 238 ± 39 1 | 145 ± 27 1 | 167 ± 34 1 | 50.9 ± 7.1 1 | 50.5 ± 6.6 1 | 107 ± 54 1 | 105 ± 25 1 | ||||||
| p4 | ET, CT: p < 0.05 (pre vs. post) ET, ST, CT vs. CG: p = 0.006 (post, post hoc) | ET, CT: p < 0.05 (pre vs. post) ET, ST, CT vs. CG: p = 0.008 (post, post hoc) | ET, CT: p < 0.05 (pre vs. post) | |||||||||||
| Wang [56] | 2017 | ET | 196 ± 51 1,6 | 121 ± 51 1,6 | NI | 51 ± 18 1,6 | 44 ± 24 1,6 | NI | 46.4 ± 21.7 1,6 | 52.2 ± 16.6 1,6 | NI | 271 ± 40.7 1,6 | 207.3 ± 96.5 1,6 | NI |
| CT | 197 ± 55 1,6 | 142 ± 60 1,6 | 60 ± 21 1,6 | 43 ± 23 1,6 | 45.6 ± 27.1 1,6 | 54.9 ± 22 1,6 | 286.1 ± 77.1 1,6 | 215.2 ± 100.1 1,6 | ||||||
| CG | 204 ± 48 1,6 | 205 ± 59 1,6 | 51 ± 18 1,6 | 54 ± 21 1,6 | 42.9 ± 21.7 1,6 | 45.2 ± 23.6 1,6 | 293.2 ± 54 1,6 | 290.5 ± 56.7 1,6 | ||||||
| p4 | ET, CT: p < 0.05 (pre vs. post) ET, CT vs. CG: p < 0.05 (post, post hoc) | ET, CT: p < 0.05 (pre vs. post) ET, CT vs. CG: p < 0.05 (post, post hoc) | ET, CT: p < 0.05 (pre vs. post) ET, CT vs. CG: p < 0.05 (post, post hoc) | ET, CT: p < 0.05 (pre vs. post) ET, CT vs. CG: p < 0.05 (post, post hoc) | ||||||||||
| Chen et al. [57] | 2016 | ET | 209 ± 54 1,5,6 | 205 ± 43 1,5,6,13 197 ± 54 1,5,6,14 | NI | 147 ± 27 1,5,6 | 135 ± 39 1,5,6,13 135 ± 39 1,5,6,14 | NI | 42.5 ± 11.6 1,5,6 | 39.8 ± 11.6 1,5,6,13 43.7 ± 12.4 1,5,6,14 | NI | 141.7 ± 101.9 1,5,6 | 141.7 ± 79.7 1,5,6,13 132.9 ± 44.3 1,5,6,14 | NI |
| ST | 193 ± 46 1,5,6 | 201 ± 31 1,5,6,13 193 ± 43 1,5,6,14 | 131 ± 35 1,5,6 | 131 ± 27 1,5,6,13 124 ± 46 1,5,6,14 | 42.2 ± 10.8 1,5,6 | 42.5 ± 17.4 1,5,6,13 46 ± 13.9 1,5,6,14 | 132.9 ± 88.6 1,5,6 | 106.3 ± 53.1 1,5,6,13 106.3 ± 44.3 1,5,6,14 | ||||||
| CG | 201 ± 46 1,5,6 | 209 ± 46 1,5,6,13 205 ± 46 1,5,6,14 | 135 ± 39 1,5,6 | 143 ± 39 1,5,6,13 143 ± 39 1,5,6,14 | 46.4 ± 11.6 1,5,6 | 48.3 ± 13.5 1,5,6,13 46.4 ± 14.7 1,5,6,14 | 106.3 ± 88.6 1,5,6 | 97.4 ± 53.1 1,5,6,13 106.3 ± 53.1 1,5,6,14 | ||||||
| p4 | ET: p < 0.05 (post vs. mild) ST: p < 0.05 (pre vs. post) ET vs. CG: p < 0.5 (mild, post hoc) | ST: p < 0.05 (pre vs. mild) | ||||||||||||
| Rossi et al. [21] | 2016 | ET | 202.5 ± 36.6 1 | 200.0 ± 37.2 1 | −2.5 ± 17.8 1 (−12.3–7.4) 15 −1.2 ± 8.8 1 (−5.9–3.6)% 6,7 | 124.5 ± 34.7 1 | 114.7 ± 29.9 1 | −9.9 ± 19.8 1 (−20.8–1.1) 15 −7.95 ± 15.90 1 (−16.70–0.88)% 6,7 | 57.9 ± 12.9 1 | 60.9 ± 13.0 1 | 3.0 ± 6.8 1 (−0.8–6.8) 15 5.18 ± 11.74 1 (−1.38–11.74)% 6,7 | NI | NI | NI |
| CT | 203.6 ± 30.4 1 | 209.8 ± 34.8 1 | 6.24 ± 30.8 (−4.0–16.5) 15 3.1 ± 15.1 (−2.0–8.2)% 6,7 | 122.5 ± 25.3 1 | 129.7 ± 27.6 1 | 7.1 ± 27.5 (−2.0–16.3) 15 5.80 ± 22.45 (−1.63–13.32)% 6,7 | 51.9 ± 10.7 1 | 54.8 ± 12.0 1 | 2.9 ± 6.7 (0.6–5.0) 5.59 ± 12.91 15 (1.16–9.64)% 6,7 | |||||
| CG | 195.8 ± 34.0 1 | 201.3 ± 34.9 1 | 5.5 ± 33.7 (−11.9–22.8) 15 2.8 ± 17.2 (−6.1–11.6)% 6,7 | 117.4 ± 26.7 1 | 123.3 ± 24.7 1 | 5.9 ± 24.8 (−6.8–18.7) 15 5.04 ± 21.20 (−8.46–15.97)% 6,7 | 49.1 ± 7.7 1 | 50.0 ± 8.4 1 | 0.9 ± 5.8 (−2.0–3.9) 15 1.83 ± 11.81 (−4.07–7.93)% 6,7 | |||||
| p4 | CT: p = 0.013 (pre vs. post) | |||||||||||||
| Mahdirejei et al. [14] | 2015 | ET | 211.88 ± 34.23 1 | 204.22 ± 30.31 1 | NI | 123.55 ± 20.15 1 | 111.33 ± 36.74 1 | −12.22 6 −9.89% 7 | 38.66 ± 4.24 1 | 41.66 ± 4.35 1 | NI | 236 ± 162 1 | 207.22 ± 90 1 | NI |
| ST | 185.3 ± 28.91 1 | 190.2 ± 29.84 1 | 108.44 ± 21.69 1 | 117.66 ± 24.78 1 | NI | 36.66 ± 3.84 1 | 39.11 ± 5.32 1 | 2.45 6 6.68% 7 | 166 ± 77.51 1 | 151.33 ± 56.46 1 | −14.66 6 −8.83% 7 | |||
| CG | 182.12 ± 43.69 1 | 190.12 ± 48.52 1 | 106.50 ± 22.77 1 | 113.62 ± 36.74 1 | 38.37 ± 3.24 1 | 37.87 ± 4.94 1 | NI | 150 ± 47.74 1 | 153.87 ± 63.55 1 | NI | ||||
| p4 | ET: p = 0.05 (pre vs. post) | |||||||||||||
| Huffman et al. b [59] | 2014 | ET 16 | NI | NI | NI | NI | NI | NI | NI | NI | NI | 147 ± 67.3 1,6 | 124 ± 39 1,6 | NI |
| ET 17 | 123.1 ± 48.7 1,6 | 124 ± 65.5 1,6 | ||||||||||||
| ET 18 | 139.1 ± 54.0 1,6 | 120.5 ± 45.2 1,6 | ||||||||||||
| ST | 132.9 ± 63.8 1,6 | 126.7 ± 57.6 1,6 | ||||||||||||
| CT | 130.2 ± 43.4 1,6 | 112.5 ± 50.5 1,6 | ||||||||||||
| CG | 163.9 ± 74.4 1,6 | 153.2 ± 83.3 1,6 | ||||||||||||
| p4 | ET: p < 0.05 (pre vs. post) | |||||||||||||
| Sousa et al. [60] | 2014 | ET | 194 ± 31.3 1 | 195 ± 28.7 1,14 200 ± 15.6 1,19 196 ± 21.2 1,20 193 ± 27.3 1,21 | −1.0 −0.5% 6,7 | 126 ± 24.4 1 | 120 ± 25.2 1,14 125 ± 11.9 1,19 122 ± 15.5 1,20 117 ± 19.0 1,21 | −8.9 −7.06% 6,7 | 52.5 ± 6.8 1 | 52.4 ± 7.2 1,14 50.7 ± 7.8 1,19 48.4 ± 6.0 1,20 48.7 ± 6.3 1,21 | −3.68 6 −7% 7 | 114 ± 56.6 1 | 86.5 ± 31.6 1,14 103 ± 31.7 1,19 101 ± 26.7 1,20 104 ± 59.7 1,21 | −10.1 −8.86% 6,7 |
| CT | 207 ± 30.7 1 | 205 ± 40.1 1,14 195 ± 32.8 1,19 196 ± 32.7 1,20 189 ± 26.9 1,21 | −17.6 −8.5% 6,7 | 137 ± 30.5 1 | 127 ± 31.8 1,14 125 ± 23.9 1,19 122 ± 23.3 1,20 120 ± 23.1 1,21 | −17.2 −12.56% 6,7 | 56.1 ± 13.0 1 | 52.6 ± 12.4 1,14 52.1 ± 10.4 1,19 52.4 ± 10.5 1,20 52.0 ± 9.4 1,21 | −4.49 6 −8% 7 | 112 ± 56.8 1 | 101 ± 43.4 1,14 91.8 ± 32.4 1,19 96.4 ± 35.7 1,20 86.5 ± 35.7 1,21 | −25.8 −20.04% 6,7 | ||
| CG | 191 ± 30.5 1 | 196 ± 27.0 1,15 210 ± 23.5 1,19 202 ± 25.6 1,20 200 ± 25.5 1,21 | 8.7 4.6% 6,7 | 128 ± 22.8 1 | 120 ± 20.6 1,15 133 ± 23.0 1,19 122 ± 22.2 1,20 125 ± 22.6 1,21 | NI | 52.5 ± 12.1 10 | 51.0 ± 10.5 1,14 51.9 ± 12.1 1,19 53.3 ± 12.5 1,20 52.1 ± 13.3 1,21 | NI | 93.5 ± 32.1 10 | 117 ± 48.8 1,14 122 ± 71.3 1,19 110 ± 66.1 1,20 107 ± 54.2 1,21 | 13.5 14.44% 6,7 | ||
| Changela et al. [61] | 2013 | ET | 242.70 ± 21.176 1 | 233.00 ± 19.539 1 | NI | NI | NI | NI | 45.40 ± 3.533 1 | 53.60 ± 3.134 1 | NI | NI | NI | NI |
| ST | 247.50 ± 13.360 1 | 242.60 ± 13.945 1 | 46.10 ± 5.724 1 | 49.40 ± 4.993 1 | ||||||||||
| p 4 | ET: p < 0.05 (pre vs. post) | |||||||||||||
| Donges et al. [62] | 2013 | ET | 204 ± 10 6,11 | NI | NI | 119 ± 9 6,11 | NI | NI | 43.33 ± 2.33 11 | NI | NI | 177.1 ± 34.5 11 | NI | NI |
| ST | 188 ± 7 6,11 | 113 ± 7 6,11 | 43.0 ± 2.33 11 | 128.4 ± 16.8 11 | ||||||||||
| CT | 223 ± 12 6,11 | 138 ± 10 b 6,11 | 46.33 ± 2.33 11 | 149.7 ± 13.3 11 | ||||||||||
| CG | 187 ± 17 6,11 | 111 ± 15 6,11 | 42.0 ± 4.67 11 | 138.2 ± 27.5 11 | ||||||||||
| p4 | CT vs. ST: p < 0.05 (pre, post hoc) | CT vs. ST: p < 0.05 (pre, post hoc) | ||||||||||||
| Kadoglou et al. [63] | 2013 | ET | 235 ± 52 1,6 | NI | −16 ± 5 1,6 −6.7 ± 2.06% 1,6,7 | 148 ± 51 1,6 | NI | −11 ± 4 1,6 −7.31 ± 2.61% 1,6,7 | 51 ± 12.8 1,6 | NI | 7 ± 2.7 1,6 13.73 ± 5.29% 1,6,7 | 154.1 ± 47.8 1,6 | NI | −34.5 ± 8.9 1,6 −22.39 ± 5.78% 1,6,7 |
| ST | 224 ± 34 1,6 | −11 ± 4 1,6 −4.8 ± 1.7% 1,6,7 | 142 ± 281,6 | −2 ± 0.8 1,6 −1.36 ± 0.55% 1,6,7 | 49.9 ± 17 1,6 | −2.7 ± 1 1,6 −5.41 ± 2.00% 1,6,7 | 144.4 ± 64.7 1,6 | −21.3 ± 5.3 1,6 −14.75 ± 3.67% 1,6,7 | ||||||
| CT | 2.33 ± 59 1,6 | −29 ± 5 1,6 −12.4 ± 2.0% 1,6,7 | 142 ± 431,6 | −18 ± 5 1,6 −12.53 ± 3.27% 1,6,7 | 48.7 ± 9.7 1,6 | 5.8 ± 1.9 1,6 11.91 ± 3.90% 1,6,7 | 157.7 ± 75.3 1,6 | −43.4 ± 8 1,6 −27.52 ± 5.07% 1,6,7 | ||||||
| CG | 227 ± 48 1,6 | −5 ± 2 1,6 −2.0 ± 0.9% 1,6,7 | 143 ± 451,6 | 0.8 ± 0.4 1,31,6 0.54 ± 0.27% 1,6,7 | 53 ± 10.8 1,6 | −3.9 ± 1.9 1,6 −7.36 ± 3.59% 1,6,7 | 147.9 ± 62.9 1,6 | −2.7 ± 0.9 1,6 −1.83 ± 0.61% 1,6,7 | ||||||
| p4 | p = 0.047 (changes) ET, CT: p < 0.05 (pre vs. post) CT vs. CG: p = 0.041 (changes, post hoc) | p = 0.044 (changes) ET, CT: p < 0.05 (pre vs. post) CT vs. CG: p = 0.039 (changes, post hoc) | p = 0.046 (changes) ET: p < 0.05 (pre vs. post) ET vs. CG: p = 0.029 (changes, post hoc) | p = 0.003 (changes) ET, ST, CT: p < 0.05 (pre vs. post) CT vs. CG: p < 0.001, ET vs. CG: p = 0.004, ST vs. CG: p = 0.011 (changes, post hoc) | ||||||||||
| Paoli et al. [64] | 2013 | ET | 216.3 ± 4 1 | 210.9 ± 4.3 1 | NI | 120.6 ± 4.2 1 | 116.9 ± 4.7 1 | NI | 49.3 ± 1.6 1 | 49.1 ± 1.8 1 | NI | 231.7 ± 2.9 1 | 224.2 ± 4.3 1 | NI |
| CT 22 | 213 ± 3.7 1 | 193 ± 2.4 1 | 115 ± 3.8 1 | 97 ± 3.2 1 | 51 ± 0.6 1 | 56 ± 1.2 1 | 235 ± 4 1 | 200 ± 1.7 1 | ||||||
| CT 23 | 227 ± 3.6 1 | 221 ± 3.6 1 | 117.6 ± 4.5 1 | 114.4 ± 4.8 1 | 50.2 ± 1.2 1 | 51.2 ± 1.4 1 | 235 ± 3.2 1 | 218.8 ± 3.4 1 | ||||||
| p4 | ET, CT 23: p < 0.05, CT 22: p < 0.005 (pre vs. post) CT 22 vs. CT 23, ET: p < 0.05 (post, post hoc) | ET, CT 22, CT 23: p < 0.05 (pre vs. post) CT 22 vs. CT 23, ET: p < 0.05 (post, post hoc) | CT 22: p < 0.001 (pre vs. post) CT 22 vs. CT 23, ET: p < 0.05 (post, post hoc) | CT22: p < 0.001, ET, CT23: p < 0.005 (pre vs. post) CT22 vs. CT23, ET: p < 0.05 (post, post hoc) | ||||||||||
| Venojärvi et al. [65] | 2013 | ET | 205 ± 8 1,6 | NI | −8 ± 4 1,6 −3.8 ± 1.9% 1,6,7 | 131 ± 4 1,6 | NI | −8 ± 4 1,6 −6.11 ± 3.05% 1,6,7 | 46.4 ± 3.9 1,6 | NI | 0.0 ± 0.0 1,6 0.0 ± 0.0% 1,6,7 | 168.3 ± 17.7 1,6 | NI | −26.6 ± 17.7 1,6 −15.81 ± 10.52% 1,6,7 |
| ST | 186 ± 8 1,6 | 8 ± 4 1,6 4.2 ± 2.1% 1,6,7 | 112 ± 4 1,6 | 8 ± 4 1,6 7.14 ± 3.57% 1,6,7 | 46.4 ± 3.9 1,6 | 3.9 ± 0.0 1,6 8.41 ± 0.0% 1,6,7 | 168.3 ± 26.6 1,6 | 0.0 ± 17.7 1,6 0.0 ± 17.7% 1,6 | ||||||
| CG | 201 ± 8 1,6 | 4 ± 4 1,6 1.9 ± 1.9% 1,6,7 | 128 ± 4 1,6 | 4 ± 4 1,6 3.13 ± 3.13% 1,6,7 | 46.4 ± 3.9 1,6 | 3.9 ± 0.0 1,6 8.41 ± 0.0% 1,6,7 | 141.7 ± 17.7 1,6 | −8.9 ± 17.7 1,6 −6.28 ± 12.49% 1,6,7 | ||||||
| p 4 | p = 0.005 (changes) ET vs. ST: p = 0.003 24 (changes, post hoc) | p = 0.035 (pre) p = 0.012 (changes) ET vs. ST: p = 0.048 24 (pre and changes, post hoc) | ||||||||||||
| Ho et al. [66] | 2012 | ET | 225 ± 12 6 | 221 ± 11 6,15 215 ± 14 6,25 | NI | 150 ± 12 6 | 148 ± 10 6,14 140.54 ± 13 6,25 | NI | 53.4 ± 3.5 6 | 50.7 ± 3.1 6,14 49.5 ± 10.4 6,25 | NI | 120.5 ± 16.8 6 | 114.3 ± 9.7 6,14 124 ± 14.2 6,25 | NI |
| ST | 212 ± 15 6 | 223 ± 14 6,15 238 ± 17 6,25 | 138 ± 13 6 | 145 ± 12 6,14 157.53 ± 14 6,256 | 51.8 ± 3.1 6 | 55.7 ± 3.1 6,14 55.7 ± 3.1 6,25 | 112.5 ± 10.6 6 | 107.2 ± 14.2 6,14 122.2 ± 15.9 6,25 | ||||||
| CT | 221 ± 12 6 | 222 ± 10 6,15 222 ± 10 6,25 | 146 ± 10 6 | 147 ± 9 6,14 143.24 ± 8.5 6,25 | 55.3 ± 4.3 6 | 55.7 ± 3.9 6,14 54.5 ± 4.3 6,25 | 97.4 ± 8.9 6 | 95.7 ± 8.9 6,14 120.5 ± 15.1 6,25 | ||||||
| CG | 213 ± 11 6 | 227 ± 12 6,15 212 ± 11 6,25 | 136 ± 10 6 | 147 ± 12 6,14 133.9 ± 9.6 6,25 | 1.42 ± 0.3 6 | 156.1 ± 4.3 6,14 52.2 ± 3.9 6,25 | 110.7 ± 15.16 | 121.3 ± 16.8 6,14 131.1 ± 20.4 6,25 | ||||||
| p4 | ST: p <0.05 (pre vs. post) ST vs. ET, CG: p <0.05 (post, post hoc) | ST: p <0.05 (pre vs. post) ST vs. ET, CT, CG: p <0.05 (post, post hoc) | ET, ST: p <0.05 (pre vs. post) ST vs. ET: p < 0.05 (mild and post, post hoc) ST vs. CG: p < 0.05 (post, post hoc) | CT: p <0.05 (pre vs. post) | ||||||||||
| Stensvold et al. c [67] | 2012 | ET | NI | NI | NI | NI | NI | NI | 45.2 ± 13.5 1,6 | NI | NI | 203.7 ± 88.6 1,6 | NI | NI |
| ST | 44.5 ± 7 1,6 | 159.4 ± 79.7 1,6 | ||||||||||||
| CG | 49.9 ± 13.5 1,6 | 150.6 ± 70.9 1,6 | ||||||||||||
| Sukala et al. [68] | 2012 | ET | 174 ± 15 1,6 | 182 ± 15 1,6 | 12 ± 23 1,6 6.7 ± 13.3% 1,6,7 | 101 ± 23 1,6 | 104 ± 15 1,6 | 4 ± 19 1,6 3.96 ± 18.81% 1,6,7 | 42.5 ± 7.7 1,6 | 42.5 ± 7.7 1,6 | 0.0 ± 3.9 1,6 | 141.7 ± 44.3 1,6 | 168.3 ± 53.2 1,6 | 26.6 ± 17.7 1,6 18.77 ± 12.49% 1,6,7 |
| ST | 189 ± 58 1,6 | 174 ± 39 1,6 | −15 ± 35 1,6 −8.2 ± 18.4% 1,6,7 | 104 ± 54 1,6 | 93 ± 27 1,6 | −12 ± 3 11,6 −11.54 ± 29.81% 1,6,7 | 50.3 ± 15.5 1,6 | 50.3 ± 19.3 1,6 | 0.0 ± 3.9 1,6 | 194.9 ± 106.3 1,6 | 177.1 ± 88.6 1,6 | −17.7 ± 53.1 1,6 −9.08 ± 27.24% 1,6,7 | ||
| p4 | ET vs. ST: p = 0.08 (changes, post hoc) | ET: p = 0.004 (pre vs. post) ET vs. ST: p = 0.03 (changes, post hoc) | ||||||||||||
| Bateman et al. b [13] | 2011 | ET | NI | NI | NI | NI | NI | NI | 41.5 ± 14.2 1 | NI | 1.03 ± 4.81 1 2.48 ± 11.59% 1,6,7 | 154 ± 81.3 1 | NI | −21 ± 56 1 −13.64 ± 36.36% 1,6,7 |
| ST | 46.8 ± 13.9 1 | −0.63 ± 4.81 1 −1.35 ± 10.28% 1,6,7 | 140 ± 81.0 1 | −5.25 ± 52.6 1 −3.75 ± 37.57% 1,6,7 | ||||||||||
| CT | 45.0 ± 11.0 1 | 1.55 ± 5.84 1 3.44 ± 12.98% 1,6,7 | 152 ± 93.9 1 | −30.1 ± 49.8 1 −19.80 ± 32.76% 1,6,7 | ||||||||||
| p4 | ET: p = 0.049, CT: p = 0.006 (pre vs. post) CT vs. ST: p < 0.10 (changes, post hoc) | |||||||||||||
| Jorge et al. [69] | 2011 | ET | 183.13 ± 23.09 1 | 165.75 ± 31.38 1 | NI | 103.2 ± 22.16 1 | NI | NI | 47.15 ± 9.54 1 | 44.11 ± 7.74 1 | NI | 141.88 ± 47.63 1 | 127.63 ± 55.22 1 | NI |
| ST | 164.38 ± 30.10 1 | 153.00 ± 25.56 1 | 88.5 ± 28.85 1 | 39.38 ± 7.78 1 | 34.75 ± 3.62 1 | 236.38 ± 231.37 1 | 154.63 ± 76.44 1 | |||||||
| CT | 181.13 ± 29.23 1 | 178.75 ± 30.27 1 | 99.11 ± 21.03 1 | 46.13 ± 7.97 1 | 46.50 ± 7.58 1 | 157.88 ± 86.62 1 | 131.75 ± 68.72 1 | |||||||
| CG | 179.45 ± 33.76 1 | 167.91 ± 35.76 1 | 93.58 ± 36.88 1 | 44 ± 8.20 1 | 41.89 ± 7.65 1 | 208.36 ± 76.63 1 | 157.09 ± 64.46 1 | |||||||
| p4 | p < 0.05 (changes) | ET, ST, CG: p < 0.05 (pre vs. post) | p < 0.05 (changes) | |||||||||||
| Gram et al. [70] | 2010 | ET | 166.5 ± 34.2 1,6 | 173.1 ± 7.7 6,19,26 153.8 ± 7.7 6,27,27 | NI | 98.5 ± 32.7 1,6 | 100 ± 7.7 6,19,26 69.2 ± 7.7 6,26,27 | NI | 44.2 ± 11.2 1,6 | 46.2 ± 3.9 6,20,27 42.3 ± 3.9 6,26,28 | NI | 170.1 ± 113.4 1,6 | NI | NI |
| CT | 168.8 ± 29.2 1,6 | 180.8 ± 7.7 6,19,26 176.9 ± 7.7 6,26,27 | 98.9 ± 23.5 1,6 | 115.4 ± 7.7 6,19,26 100 ± 15.4 6,26,27 | 44.6 ± 16.5 1,6 | 42.3 ± 3.9 6,20,27 103.9 ± 7.7 6,27,28 | 181.6 ± 134.6 1,6 | |||||||
| CG | 176.5 ± 53.5 1,6 | 173.1 ± 7.7 6,19,26 169.2 ± 7.7 6,26,27 | 98.5 ± 25.7 1,6 | 96.2 ± 3.9 6,19,26 100 ± 19.2 6,26,27 | 42.3 ± 14.2 1,6 | 42.3 ± 3.9 6,20,26 92.3 ± 7.7 6,26,27 | 236.5 ± 296.3 1,6 | |||||||
| Stensvold et al. c [22] | 2010 | ET | 236 ± 37 1,6 | 218 ± 24 1,6 | −13 (−27–1) 6,28 −5.6 (−11.5–0.3)% 6,7,28 | NI | NI | NI | 45.2 ± 13.5 1,6,19 | 47.6 ± 15.5 1,6,19 | 2.3 (−4.3–8.9) 6,28 5.09 (−9.51–19.70)% 6,7,28 | 203.7 ± 88.6 1,6 | 159.4 ± 70.9 1,6 | −35.4 (−79.7–17.7) 6,29 −17.38 (−39.12- 8.69)% 6,7,28 |
| ST | 212 ± 47 1,6 | 223 ± 39 1,6 | 5 (−10–20) 6,28 2.4 (−4.6–9.4)% 6,7,28 | 44.5 ± 7 1,6 | 47.6 ± 8.1 1,6 | 3.1 (−3.9–10.1) 6,28 6.97 (−8.76–22.71)% 6,7,28 | 159.4 ± 79.7 1,6 | 168.3 ± 106.3 1,6 | −8.9 (−53.1–44.3) 6,29 −5.58 (−33.31–27.77)% 6,7,28 | |||||
| CT | 244 ± 34 1,6 | 229 ± 26 1,6 | −13 (−29–3) 6,28 −5.2 (−11.9–1.4)% 6,7,28 | 53.8 ± 14.7 1,6 | 57.6 ± 24.7 1,6 | 4.6 (−3.5–12.4) 6,28 8.55 (−6.51–23.05)% 6,7,28 | 230.3 ± 124 1,6 | 203.7 ±97.4 1,6 | −8.9 (−70.9–44.3) 6,29 −3.87 (−30.79–19.26)% 6,7,28 | |||||
| CG | 221 ± 49 1,6 | 216 ± 37 1,6 | −7 (−21–8) 6,29 −3.1 (−9.6–3.4)% 6,7,28 | 49.9 ± 13.5 1,6 | 49.1 ± 24.4 1,6 | −0.8 (−7.3–6.2) 6,28 −1.60 (−14.63–12.4)% 6,7,28 | 150.6 ± 70.9 1,6 | 150.6 ± 88.6 1,6 | −8.9 (−53.1–44.3) 6,29 −5.91 (−35.26–29.42)% 6,7,28 | |||||
| Hara et al. [72] | 2005 | ET | 164.7 ± 31.5 1 | 172.9 ± 36.9 1 | NI | NI | NI | NI | 39.6 ± 6.6 1 | 42.0 ± 6.7 1 | NI | 136.7 ± 40.1 1 | 138.9 ± 43.7 1 | NI |
| CT | 153.4 ± 23.2 1 | 165.8 ± 14.7 1 | 39.9 ± 5.0 1 | 53.9 ± 8.9 1 | 99.6 ± 46.8 1 | 90.7 ± 24.2 1 | ||||||||
| CG | 170.0 ± 41.3 1 | 175.4 ± 37.7 1 | 38.9 ± 9.7 1 | 42.3 ± 8.6 1 | 119.9 ± 74.8 1 | 126.3 ± 59.7 1 | ||||||||
| p4 | CT: p < 0.05 (pre vs. post) | CT: p < 0.01 (pre vs. post) | ||||||||||||
| Banz et al. [73] | 2003 | ET | 205.0 ± 44.3 1 | 209.1 ± 42.3 1 | NI | 129.8 ± 56.7 1 | 133.2 ± 39.5 1 | NI | 29.8 ± 7.0 1 | 33.7 ± 4.0 1 | NI | NI | NI | NI |
| ST | 203.0 ± 41.6 1 | 205.6 ± 43.6 1 | 93.0 ± 70.4 1 | 114.3 ± 63.2 1 | 31.7 ± 8.4 1 | 32.0 ± 7.8 1 | ||||||||
| p4 | p < 0.05 (pre vs. post) | |||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jamka, M.; Makarewicz-Bukowska, A.; Bokayeva, K.; Śmidowicz, A.; Geltz, J.; Kokot, M.; Kaczmarek, N.; Żok, A.; Kononets, V.; Cielecka-Piontek, J.; et al. Comparison of the Effect of Endurance, Strength and Endurance-Strength Training on Glucose and Insulin Homeostasis and the Lipid Profile of Overweight and Obese Subjects: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 14928. https://doi.org/10.3390/ijerph192214928
Jamka M, Makarewicz-Bukowska A, Bokayeva K, Śmidowicz A, Geltz J, Kokot M, Kaczmarek N, Żok A, Kononets V, Cielecka-Piontek J, et al. Comparison of the Effect of Endurance, Strength and Endurance-Strength Training on Glucose and Insulin Homeostasis and the Lipid Profile of Overweight and Obese Subjects: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(22):14928. https://doi.org/10.3390/ijerph192214928
Chicago/Turabian StyleJamka, Małgorzata, Aleksandra Makarewicz-Bukowska, Kamila Bokayeva, Angelika Śmidowicz, Jakub Geltz, Marta Kokot, Nina Kaczmarek, Agnieszka Żok, Victoria Kononets, Judyta Cielecka-Piontek, and et al. 2022. "Comparison of the Effect of Endurance, Strength and Endurance-Strength Training on Glucose and Insulin Homeostasis and the Lipid Profile of Overweight and Obese Subjects: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 22: 14928. https://doi.org/10.3390/ijerph192214928






