Comparing a Sensor for Movement Assessment with Traditional Physiotherapeutic Assessment Methods in Patients after Knee Surgery—A Method Comparison and Reproducibility Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Definition of Assessment Procedures
2.2. Patient Recruitment and Conduct of Assessment
2.3. Statistical Analysis
2.4. Ethical Approval and Registration
3. Results
3.1. Population and Assessment Procedure Characteristics
3.2. Reproducibility of Raw Measurements
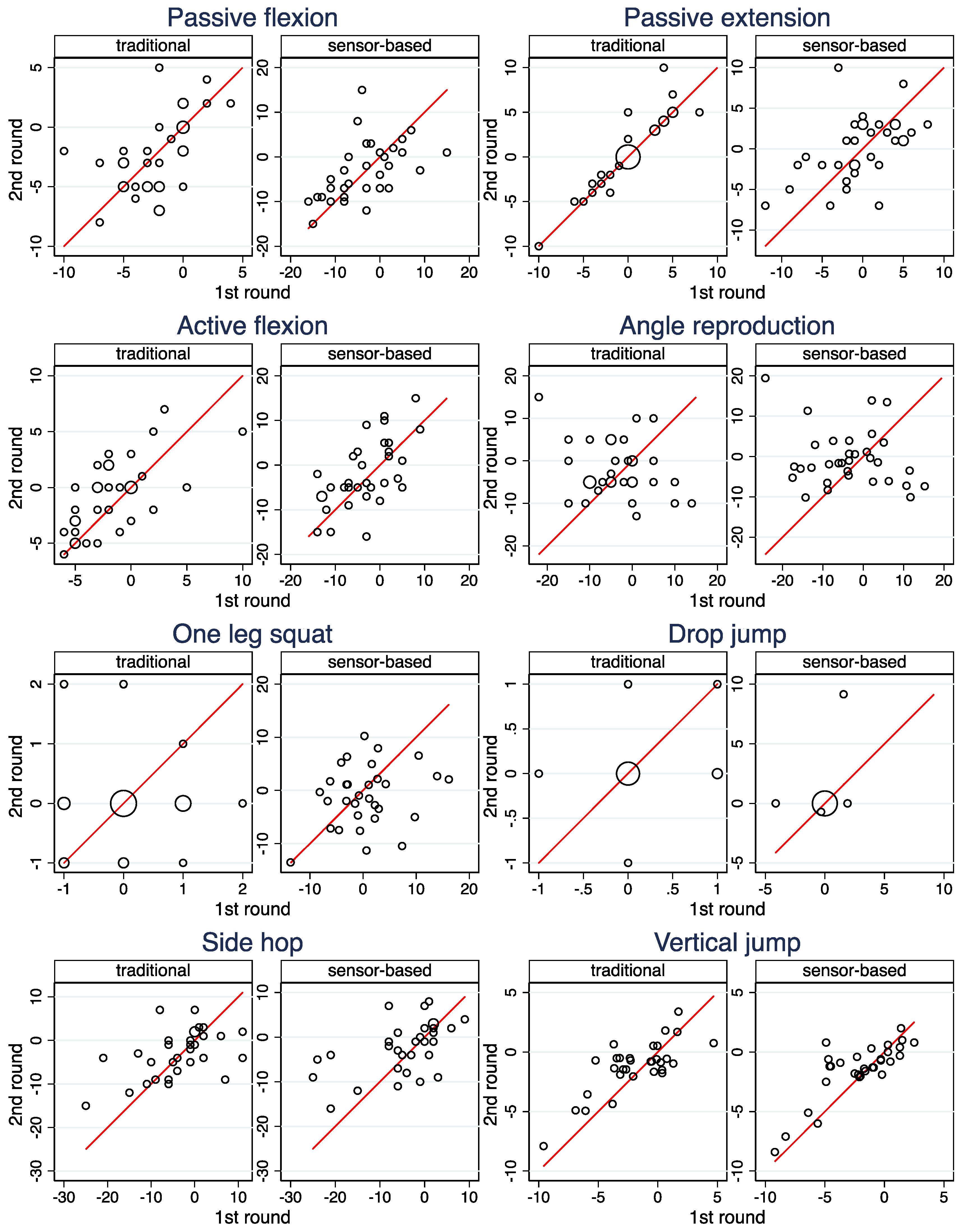
3.3. Reproducibility of Side Differences
3.4. Agreement of Raw Measurements between the Two Modalities
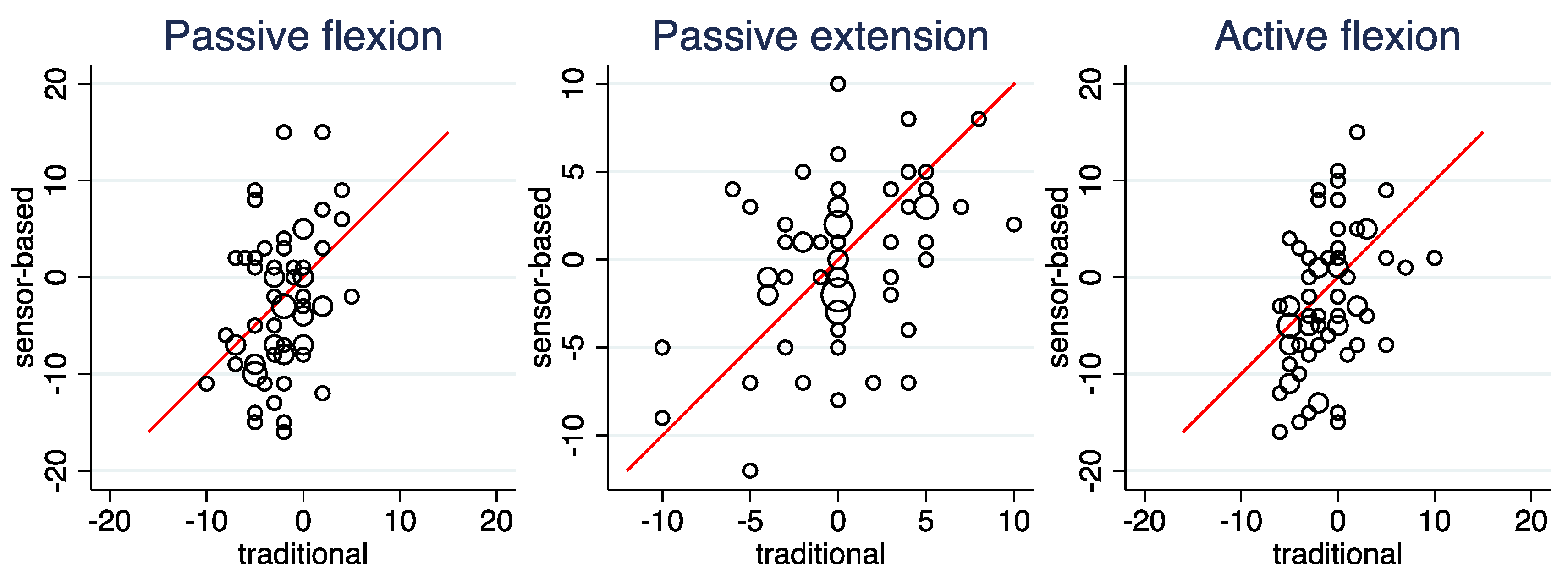
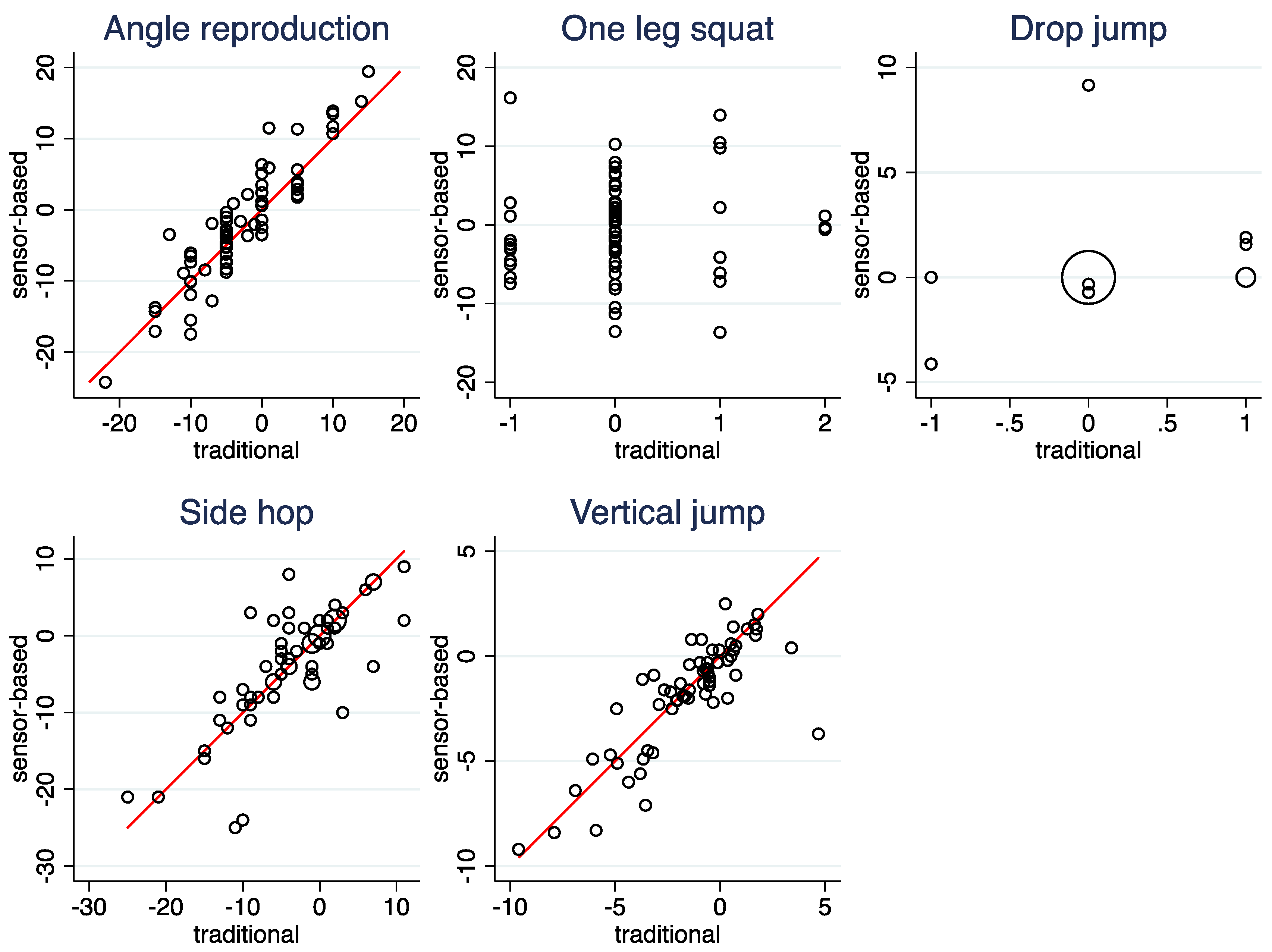
3.5. Agreement of Side Differences between the Two Modalities
4. Discussion
4.1. Summary of Results
4.2. Side Hops
4.3. Vertical Jump
4.4. Angle Reproduction
4.5. Mobility Assessments
4.6. Knee Instability
4.7. Implications for the Specific Sensor Investigated
4.8. Implications for the Use of Sensor-Based Assessments in General
4.9. Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Picerno, P.; Iosa, M.; D’Souza, C.; Benedetti, M.G.; Paolucci, S.; Morone, G. Wearable Inertial Sensors for Human Movement Analysis: A Five-Year Update. Expert Rev. Med. Devices 2021, 18, 79–94. [Google Scholar] [CrossRef] [PubMed]
- Porciuncula, F.; Roto, A.V.; Kumar, D.; Davis, I.; Roy, S.; Walsh, C.J.; Awad, L.N. Wearable Movement Sensors for Rehabilitation: A Focused Review of Technological and Clinical Advances. PM&R 2018, 10, S220–S232. [Google Scholar] [CrossRef]
- Rodgers, M.M.; Alon, G.; Pai, V.M.; Conroy, R.S. Wearable Technologies for Active Living and Rehabilitation: Current Research Challenges and Future Opportunities. J. Rehabil. Assist. Technol. Eng. 2019, 6, 2055668319839607. [Google Scholar] [CrossRef] [PubMed]
- Smuck, M.; Odonkor, C.A.; Wilt, J.K.; Schmidt, N.; Swiernik, M.A. The Emerging Clinical Role of Wearables: Factors for Successful Implementation in Healthcare. NPJ Digit. Med. 2021, 4, 1–8. [Google Scholar] [CrossRef]
- Lang, C.E.; Barth, J.; Holleran, C.L.; Konrad, J.D.; Bland, M.D. Implementation of Wearable Sensing Technology for Movement: Pushing Forward into the Routine Physical Rehabilitation Care Field. Sensors 2020, 20, E5744. [Google Scholar] [CrossRef]
- Lee, S.M.; Lee, D. Healthcare Wearable Devices: An Analysis of Key Factors for Continuous Use Intention. Serv. Bus. 2020, 14, 503–531. [Google Scholar] [CrossRef]
- Neves, A.L. The NHS Digital Clinical Safety Strategy. BMJ 2021, 375, n2981. [Google Scholar] [CrossRef]
- Díaz, S.; Stephenson, J.B.; Labrador, M.A. Use of Wearable Sensor Technology in Gait, Balance, and Range of Motion Analysis. Appl. Sci. 2020, 10, 234. [Google Scholar] [CrossRef]
- Poitras, I.; Bielmann, M.; Campeau-Lecours, A.; Mercier, C.; Bouyer, L.J.; Roy, J.-S. Validity of Wearable Sensors at the Shoulder Joint: Combining Wireless Electromyography Sensors and Inertial Measurement Units to Perform Physical Workplace Assessments. Sensors 2019, 19, E1885. [Google Scholar] [CrossRef]
- Small, S.R.; Bullock, G.S.; Khalid, S.; Barker, K.; Trivella, M.; Price, A.J. Current Clinical Utilisation of Wearable Motion Sensors for the Assessment of Outcome Following Knee Arthroplasty: A Scoping Review. BMJ Open 2019, 9, e033832. [Google Scholar] [CrossRef]
- Prill, R.; Walter, M.; Królikowska, A.; Becker, R. A Systematic Review of Diagnostic Accuracy and Clinical Applications of Wearable Movement Sensors for Knee Joint Rehabilitation. Sensors 2021, 21, 8221. [Google Scholar] [CrossRef] [PubMed]
- Mitternacht, J.; Hermann, A.; Carqueville, P. Acquisition of Lower-Limb Motion Characteristics with a Single Inertial Measurement Unit-Validation for Use in Physiotherapy. Diagnostics 2022, 12, 1640. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Statistical Methods for Assessing Agreement between Two Methods of Clinical Measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Kottner, J.; Audigé, L.; Brorson, S.; Donner, A.; Gajewski, B.J.; Hróbjartsson, A.; Roberts, C.; Shoukri, M.; Streiner, D.L. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) Were Proposed. J. Clin. Epidemiol. 2011, 64, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Petty, N.J.; Ryder, D. Musculoskeletal Examination and Assessment: A Handbook for Therapists, 5th ed.; Physiotherapy essentials; Elsevier: Edinburgh, UK, 2018; ISBN 978-0-7020-6717-4. [Google Scholar]
- Debrunner, H.U. Gelenkmessung: (Neutral-O-Methode), Längenmessung, Umfangmessung; Schweizerische Arbeitsgemeinschaft für Osteosynthesefragen: Biel, Switzerland, 1971. [Google Scholar]
- Ryf, C.; Weymann, A. Range of Motion—AO Neutral-0 Method: Measurement and Documentation; AO Publishing; Georg Thieme: Stuttgart, Germany, 1999; ISBN 978-3-13-116791-0. [Google Scholar]
- Löber, M.; Berg, F. Untersuchen und Behandeln nach Cyriax; Physiotherapie-basics; Springer: Heidelberg, Germany, 2007; ISBN 978-3-540-22550-8. [Google Scholar]
- Hüter-Becker, A.; Dölken, M. Physical Therapy Examination and Assessment, 2nd ed.; Thieme: Stuttgart, Germany, 2015; ISBN 978-3-13-174641-2. [Google Scholar]
- Suppé, B. FBL Klein-Vogelbach Functional Kinetics: Die Grundlagen: Bewegungsanalyse, Untersuchung, Behandlung, 7th ed.; Physiotherapie; Springer: Berlin, Germany, 2014; ISBN 978-3-642-41900-3. [Google Scholar]
- Reese, N.B.; Bandy, W.D.; Yates, C. Joint Range of Motion and Muscle Length Testing, 3rd ed.; Elsevier: St. Louis, MO, USA, 2016; ISBN 978-1-4557-5882-1. [Google Scholar]
- Gräfe, K. Bewegungs-, Längen- und Umfangmessungen: Neutral-Null-Durchgangsmethode, 5th ed.; Europa-Lehrmittel: Haan-Gruiten, Germany, 2014; ISBN 978-3-8085-6825-5. [Google Scholar]
- Salis-Soglio, G. Die Neutral-0-Methode: Mit Längen- und Umfangsmessung, 1st ed.; Springer: Berlin/Heidelberg, Germany, 2015; ISBN 978-3-662-47280-4. [Google Scholar]
- Ryf, C.; Weymann, A. The Neutral Zero Method—A Principle of Measuring Joint Function. Injury 1995, 26, S1–S11. [Google Scholar] [CrossRef]
- Arifin, W. Sample Size Calculator (Web). Available online: https://wnarifin.github.io/ssc/ssicc.html (accessed on 14 September 2022).
- Walter, S.D.; Eliasziw, M.; Donner, A. Sample Size and Optimal Designs for Reliability Studies. Stat. Med. 1998, 17, 101–110. [Google Scholar] [CrossRef]
- Bonett, D.G. Sample Size Requirements for Estimating Intraclass Correlations with Desired Precision. Stat. Med. 2002, 21, 1331–1335. [Google Scholar] [CrossRef]
- Gerke, O.; Pedersen, A.K.; Debrabant, B.; Halekoh, U.; Möller, S. Sample Size Determination in Method Comparison and Observer Variability Studies. J. Clin. Monit. Comput. 2022, 36, 1241–1243. [Google Scholar] [CrossRef]
- Scinicarelli, G.; Trofenik, M.; Froböse, I.; Wilke, C. The Reliability of Common Functional Performance Tests within an Experimental Test Battery for the Lower Extremities. Sports 2021, 9, 100. [Google Scholar] [CrossRef]
- Oh, D.-S.; Choi, Y.-H.; Shim, Y.-J.; Park, S.-H.; Lee, M.-M. Concurrent Validity, Inter-, and Intrarater Reliabilities of Smart Device Based Application for Measuring Vertical Jump Performance. BJHPA 2020, 12, 35–46. [Google Scholar] [CrossRef]
- Osama Al Saadawy, B.; Abdo, N.; Embaby, E.; Rehan Youssef, A. Validity and Reliability of Smartphones in Measuring Joint Position Sense among Asymptomatic Individuals and Patients with Knee Osteoarthritis: A Cross-Sectional Study. Knee 2021, 29, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Piriyaprasarth, P.; Morris, M.E. Psychometric Properties of Measurement Tools for Quantifying Knee Joint Position and Movement: A Systematic Review. Knee 2007, 14, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Ravi, B.; Kapoor, M.; Player, D. Feasibility and Reliability of a Web-Based Smartphone Application for Joint Position Measurement. J. Rehabil. Med. 2021, 53, jrm00188. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.; Sealey, R.; Crowe, M.; Gordon, S. Concurrent Validity and Reliability of the Simple Goniometer IPhone App Compared with the Universal Goniometer. Physiother. Theory Pract. 2014, 30, 512–516. [Google Scholar] [CrossRef]
- Milanese, S.; Gordon, S.; Buettner, P.; Flavell, C.; Ruston, S.; Coe, D.; O’Sullivan, W.; McCormack, S. Reliability and Concurrent Validity of Knee Angle Measurement: Smart Phone App versus Universal Goniometer Used by Experienced and Novice Clinicians. Man. Ther. 2014, 19, 569–574. [Google Scholar] [CrossRef]
- Van Trijffel, E.; van de Pol, R.J.; Oostendorp, R.A.; Lucas, C. Inter-Rater Reliability for Measurement of Passive Physiological Movements in Lower Extremity Joints Is Generally Low: A Systematic Review. J. Physiother. 2010, 56, 223–235. [Google Scholar] [CrossRef]
- Paterno, M.V.; Schmitt, L.C.; Ford, K.R.; Rauh, M.J.; Myer, G.D.; Huang, B.; Hewett, T.E. Biomechanical Measures during Landing and Postural Stability Predict Second Anterior Cruciate Ligament Injury after Anterior Cruciate Ligament Reconstruction and Return to Sport. Am. J. Sports Med. 2010, 38, 1968–1978. [Google Scholar] [CrossRef]
- Mehl, J.; Diermeier, T.; Herbst, E.; Imhoff, A.B.; Stoffels, T.; Zantop, T.; Petersen, W.; Achtnich, A. Evidence-Based Concepts for Prevention of Knee and ACL Injuries. 2017 Guidelines of the Ligament Committee of the German Knee Society (DKG). Arch. Orthop. Trauma Surg. 2018, 138, 51–61. [Google Scholar] [CrossRef]
- Bates, N.A.; Myer, G.D.; Hale, R.F.; Schilaty, N.D.; Hewett, T.E. Prospective Frontal Plane Angles Used to Predict ACL Strain and Identify Those at High Risk for Sports-Related ACL Injury. Orthop. J. Sport. Med. 2020, 8, 2325967120957646. [Google Scholar] [CrossRef]
- Ressman, J.; Grooten, W.J.A.; Rasmussen-Barr, E. Visual Assessment of Movement Quality: A Study on Intra- and Interrater Reliability of a Multi-Segmental Single Leg Squat Test. BMC Sports Sci. Med. Rehabil. 2021, 13, 66. [Google Scholar] [CrossRef]
- Whatman, C.; Hume, P.; Hing, W. The Reliability and Validity of Physiotherapist Visual Rating of Dynamic Pelvis and Knee Alignment in Young Athletes. Phys. Ther. Sport 2013, 14, 168–174. [Google Scholar] [CrossRef] [PubMed]


Passive flexion of the lower leg (knee joint) | |
| Sensor-based assessment | The subject sits on the floor with legs extended. The leg with the sensor is pulled into maximum knee flexion with the help of the hands (grip behind the back of the knee). The leg is then pushed back into the extended starting position. The movement is performed once. The heel remains in contact with the ground during the entire movement. The sensor measures the maximum flexion in degrees. |
| Traditional assessment * | The subject lies flat in a supine position on a mat on the floor. The therapist places one hand on the subject’s thigh and the other in the distal area of the lower leg. The therapist guides the knee joint into maximum knee flexion. Once the final position is reached, the extent of movement (180°—angle between the longitudinal axis of the femur and the tibia) is measured with the universal goniometer. |
Passive extension | |
| Sensor-based assessment | The subject sits with a straight back on an elevation of 10 cm. A roll (BLACKROLL STANDARD) with a diameter of 15 cm is placed centrally in the back of the knee of the leg to be tested. After the countdown, the knee is lifted slightly so that the roll can be pulled out. The subject should straighten the knee naturally without force. The heel remains in contact with the ground during the entire movement. The sensor measures the maximum passive extension in degrees. |
| Traditional assessment * | The extension test is performed as follows: The subject lies flat in the supine position on a mat on the floor. In the final position, the extent of movement (hypomobility: 0°—angle between the longitudinal axis of the thigh and lower leg or hypermobility: 0° + angle between the longitudinal axis of the thigh and lower leg) is measured with the universal goniometer. |
Active flexion of the lower leg (knee joint) | |
| Sensor-based assessment | The subject stands straight with legs extended. The knee is bent to the maximum and returned to the starting position (the end position does not have to be held). This is done slowly and without momentum, the knees remain together. Only the lower leg moves, without the whole leg shifting backward or forward. To ensure this, the subject leans the thighs against the back of a chair. The sensor measures the maximum flexion in degrees. |
| Traditional assessment * | The subject lies flat in a supine position on a mat on the floor. The subject brings the leg to be examined into knee flexion under his own strength as far as possible. The heel remains in contact with the floor. In the final position, the extent of movement (180°—angle between the longitudinal axis of the thigh and lower leg) is measured with the universal goniometer. |
Angle reproduction | |
| Sensor-based assessment | The app randomly specifies an angle that must be reached by the user. The randomly selected angle will not exceed the value of the angle measurement obtained for Active flexion. The test procedure itself is the same as for the Active flexion. The test procedure is used in a training phase, during which the subject can watch the actual angle achieved on the display. Then, the procedure is repeated 3 times without watching the display. Between each measurement, the subject should walk a few steps. The sensor measures the end angle in degrees for each reproduction attempt. Average deviation over the three trials is calculated by the sensor. |
| Traditional assessment | During the assessment run with the sensor, the angles are measured with the universal goniometer and rounded to the nearest 5 degrees, taking into account that the leg cannot be held completely still in the angled position. The average deviation over the three tests is noted. |
One leg squat | |
| Sensor-based assessment | An elevation of either 10 cm, 20 cm or 30 cm is used to perform the test. The subject stands on the elevation with an extended leg. After the countdown has elapsed, a one-legged squat is performed. The subject goes into a deep bend until the heel touches the floor. The upper body should remain upright. The height of the elevation must be chosen so that it is challenging for the patient. According to the manufacturer, 20 cm is a good starting value for averagely athletic subjects. The test must be performed exactly once within the time interval. The sensor measures the inward tilt of the lower leg in degrees. |
| Traditional assessment | The test performance with the sensor is recorded on video from the front with a tablet. Subsequently, knee valgus is assessed using an ordinal scale: 0 = no valgus (central patella always in line with hip joint and second toe) 1 = small valgus (small oscillatory movements around neutral position) 2 = moderate valgus (central patella over great toe) 3 = severe valgus (central patella medial from great toe) |
Drop jump | |
| Sensor-based assessment | A 30 cm elevation is used to perform the test. The subject stands upright on the elevation. The hands are placed on the hips. The subject jumps off with both legs simultaneously and lands about 30 cm in front of the box. After landing, the subject immediately jumps back up. The goal for the subject is to achieve a short ground contact time. The medial drift (the inward tilting) of the knee is measured from the sensor in a time range up to about 0.2 sec after the first landing impulse. |
| Traditional assessment | The test performance with the sensor is recorded on video from the front with a tablet. Subsequently, knee valgus is assessed using an ordinal scale: 0 = no valgus (central patella always in line with hip joint and second toe) 1 = moderate valgus (over great toe) 2 = severe valgus (medial from great toe) |
Side hops (30 s) | |
| Sensor-based assessment | Before the test, a distance (1 cm, 10 cm, 20 cm, 30 cm or 40 cm) is determined and marked with tape on the floor. The distance must be chosen so that it is challenging for the patient. According to the manufacturer, 20 cm is often a good starting value and optimal for averagely athletic patients. The subject has 30 s to jump as many times as possible with one leg over the given distance. The entire body should be involved in each jump. If the upper body always remains in the same place and only the foot jumps quickly from left to right, the distance is too short. During the measurement, the sensor automatically counts the ground contacts. The examiner counts the errors, such as touching the line or a correction jump. |
| Traditional assessment | The test performance with the sensor is recorded on video from the front with a tablet. Subsequently, the jumps are counted. The error count is not repeated. |
Vertical jump (on one leg) | |
| Sensor-based assessment | The subject takes up an upright position with the hands placed on the hips. After the countdown has elapsed, a single-leg jump is performed. The jump should be as high as possible. Momentum may be gained from the upper body. The jumping leg remains stretched in the air. The landing is also done with one leg. The movement of the center of gravity from the standing position to the maximum height is determined from the sensor. |
| Traditional assessment | The sensor-based assessment is already performed on a force plate (MLD Test Evo 2, SP-Sport, Innsbruck, Austria) to measure the ground reaction forces during the vertical jumps. The jump height (cm) is calculated from the recorded force-time history using the software provided by the plate manufacturer. |
| Exercise | Parameter to Be Measured | |
|---|---|---|
| Sensor-Based Assessment | Traditional Assessment | |
| Passive flexion of the lower leg (knee joint) | Tilt angle of the leg in degrees | |
| Passive extension | Tilt angle of the leg in degrees | |
| Active flexion of the lower leg (knee joint) | Tilt angle of the leg in degrees | |
| Angle reproduction | Deviation from prespecified angle in degrees | |
| One leg squat | Inward tilt of the lower leg in degrees | Ordinal assessment scale |
| Drop jump | Inward tilt of the lower leg in degrees | Ordinal assessment scale |
| Side hops (30 s) | Number of correct jumps | |
| Vertical jump (on one leg) | Jump height (in cm) | |
| Gender (n = 33) | |
| female | 17 (51.5%) |
| male | 16 (48.5%) |
| Injured side (n = 33) | |
| left | 14 (42.4%) |
| right | 19 (57.6%) |
| Type of arthroscopic surgery (n = 33) | |
| partial meniscectomy | 18 (54.5%) |
| ACL reconstruction cartilage smoothing others | 10 (30.3%) 3 (9.1%) 2 (6.1%) |
| Health problems at contralateral side (n = 33) | |
| no | 24 (72.7%) |
| yes | 9 (27.3%) |
| Age (n = 33) | |
| mean (sd) | 43.0 (15.4) |
| range | 20–70 |
| BMI (n = 33) | |
| mean (sd) | 24.7 (4.2) |
| range | 19.6–34.0 |
| Time since surgery (months) (n = 33) | |
| mean (sd) | 9.8 (2.8) |
| range | 5–16 |
| Traditional Assessment | Sensor-Based Assessment | ||||
|---|---|---|---|---|---|
| Injured Leg | Contralateral Leg | Injured Leg | Contralateral Leg | ||
| Passive flexion | n | 66 | 66 | 65 | 66 |
| mean | 134.42 | 136.74 | 119.22 | 121.71 | |
| range | 117–149 | 122–150 | 90–141 | 81–146 | |
| Passive extension | n | 66 | 66 | 66 | 66 |
| mean | 2.94 | 2.71 | −22.36 | −22.24 | |
| range | −10–15 | −10–15 | −31–−7 | −32–−10 | |
| Active flexion | n | 66 | 66 | 66 | 66 |
| mean | 126.95 | 128.17 | 101.56 | 104.24 | |
| range | 110–138 | 115–138 | 75–122 | 83–131 | |
| Angle reproduction | n | 66 | 66 | 66 | 66 |
| mean | 4.47 | 7.26 | 4.51 | 6.44 | |
| range | −15–25 | −10–20 | −16.82–29.72 | −13.47–23.98 | |
| One leg squat | n | 62 | 62 | 62 | 62 |
| mean | 1.50 | 1.45 | 8.83 | 9.14 | |
| range | 0–3 | 0–3 | 0.31–27.61 | 0.8–23.19 | |
| Drop jump | n | 34 | 34 | 34 | 34 |
| mean | 1.12 | 1.03 | 0.67 | 0.46 | |
| range | 0–3 | 0–3 | 0–10.48 | 0–7.76 | |
| Side hops | n | 63 | 63 | 63 | 63 |
| mean | 29.02 | 32.44 | 29.19 | 32.73 | |
| range | 4–68 | 10–66 | 4–69 | 10–65 | |
| Vertical jump | n | 63 | 64 | 64 | 64 |
| mean | 10.36 | 11.78 | 10.07 | 11.82 | |
| range | 3.85–21.33 | 5.57–20.6 | 4–21.3 | 4.9–20.9 | |
| Raw Measurements | Side Differences | |||
|---|---|---|---|---|
| Traditional Assessment | Sensor-Based Assessment | Traditional Assessment | Sensor-Based Assessment | |
| Passive flexion | 0.88 | 0.89 | 0.55 | 0.55 |
| Passive extension | 0.97 | 0.77 | 0.91 | 0.51 |
| Active flexion | 0.88 | 0.91 | 0.63 | 0.61 |
| Angle reproduction | 0.34 | 0.27 | 0.00 | 0.00 |
| One leg squat | 0.64 | 0.54 | 0.01 | 0.25 |
| Drop jump | 0.94 | 0.76 | 0.29 | 0.29 |
| Side hops | 0.88 | 0.90 | 0.48 | 0.49 |
| Vertical jump | 0.93 | 0.91 | 0.71 | 0.76 |
| ICC | ||
| Raw measurements | Side differences | |
| Passive flexion | 0.00 | 0.24 |
| Passive extension | 0.00 | 0.43 |
| Active flexion | 0.00 | 0.30 |
| Angle reproduction | 0.91 | 0.90 |
| Side hops | 0.96 | 0.78 |
| Vertical jump | 0.97 | 0.81 |
| Pearson correlation | ||
| Raw measurements | Side differences | |
| Passive flexion | 0.48 | 0.34 |
| Passive extension | 0.29 | 0.42 |
| Active flexion | 0.47 | 0.41 |
| Angle reproduction | 0.92 | 0.91 |
| One leg squat | 0.37 | 0.08 |
| Drop jump | 0.25 | 0.26 |
| Side hops | 0.96 | 0.78 |
| Vertical jump | 0.97 | 0.81 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eymann, J.; Vach, W.; Fischer, L.; Jakob, M.; Gösele, A. Comparing a Sensor for Movement Assessment with Traditional Physiotherapeutic Assessment Methods in Patients after Knee Surgery—A Method Comparison and Reproducibility Study. Int. J. Environ. Res. Public Health 2022, 19, 16581. https://doi.org/10.3390/ijerph192416581
Eymann J, Vach W, Fischer L, Jakob M, Gösele A. Comparing a Sensor for Movement Assessment with Traditional Physiotherapeutic Assessment Methods in Patients after Knee Surgery—A Method Comparison and Reproducibility Study. International Journal of Environmental Research and Public Health. 2022; 19(24):16581. https://doi.org/10.3390/ijerph192416581
Chicago/Turabian StyleEymann, Jennifer, Werner Vach, Luis Fischer, Marcel Jakob, and Andreas Gösele. 2022. "Comparing a Sensor for Movement Assessment with Traditional Physiotherapeutic Assessment Methods in Patients after Knee Surgery—A Method Comparison and Reproducibility Study" International Journal of Environmental Research and Public Health 19, no. 24: 16581. https://doi.org/10.3390/ijerph192416581
APA StyleEymann, J., Vach, W., Fischer, L., Jakob, M., & Gösele, A. (2022). Comparing a Sensor for Movement Assessment with Traditional Physiotherapeutic Assessment Methods in Patients after Knee Surgery—A Method Comparison and Reproducibility Study. International Journal of Environmental Research and Public Health, 19(24), 16581. https://doi.org/10.3390/ijerph192416581







