Clinical Use of Aligners Associated with Nuvola® OP System for Transverse Maxillary Deficiency: A Retrospective Study on 100 Patients
Abstract
:1. Introduction
2. Materials and Methods
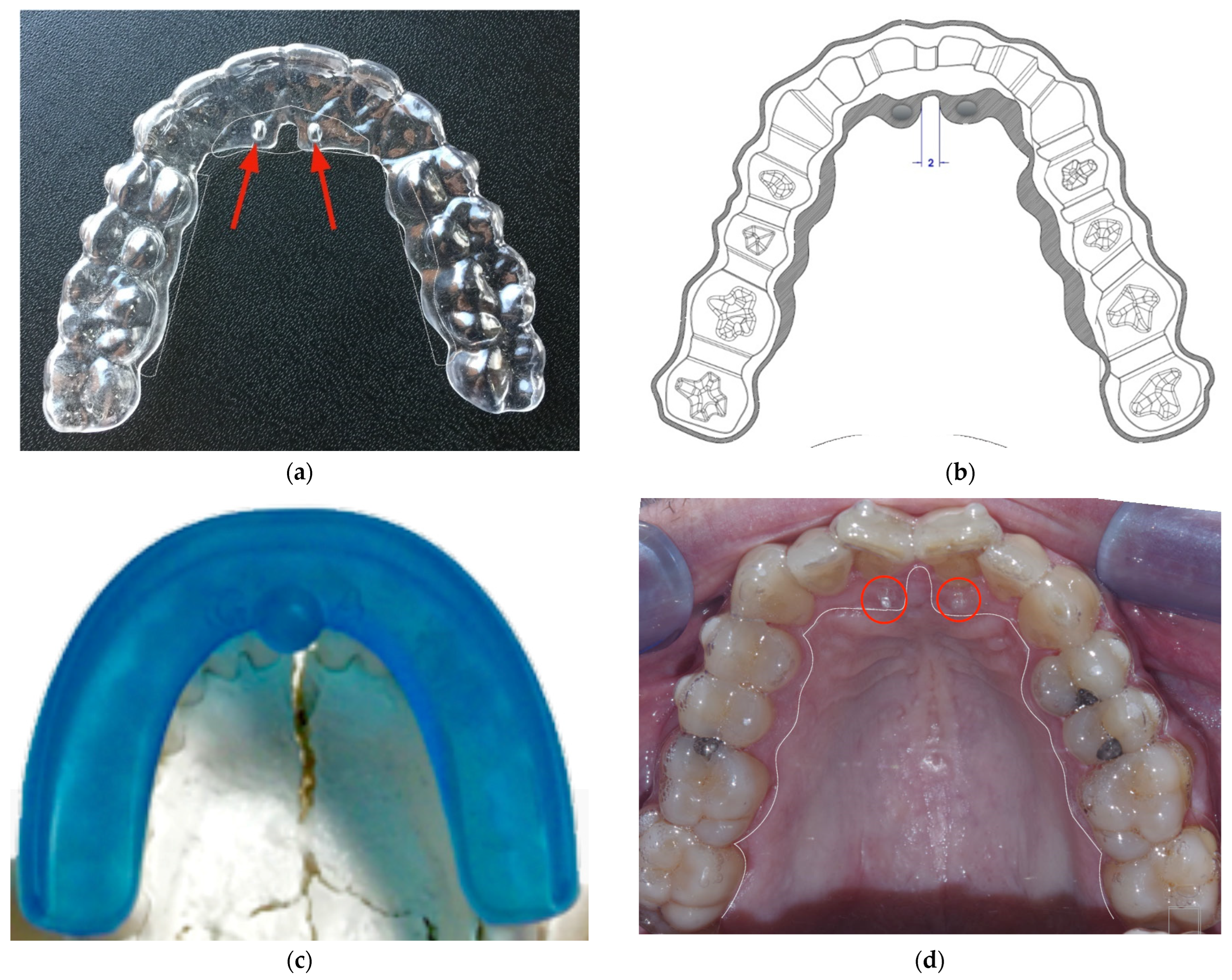
2.1. Nuvola® OP System
2.2. Linear Measurements
- D1 = distance between the palatine papilla and the mesial cusp of the sixth of the right hemi-arch;
- D2 = distance between the palatine papilla and the mesial cusp of the sixth of the left hemi-arch;
- D3 = distance between the canine-canine cusp;
- D4 = distance between the mesial cusp of the left and right first molar.
2.3. Superimposition Assessment
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- -
- The Nuvola® OP System is effective in obtaining dental expansion in the adult patient;
- -
- Further studies are needed to evaluate skeletal changes using radiological 3D techniques such as CBCT;
- -
- The system should be evaluated over the long term to assess the stability of changes;
- -
- The separate contribution of aligners and the myofunctional device to the achieved expansion should be investigated.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Melsen, B. Northcroft Lecture: How has the spectrum of orthodontics changed over the past decades? J. Orthod. 2011, 38, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Rosvall, M.D.; Fields, H.W.; Ziuchkovski, J.; Rosenstiel, S.F.; Johnston, W.M. Attractiveness, acceptability, and value of orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 276.e1–276.e12, discussion 276–277. [Google Scholar] [CrossRef]
- Ukra, A.; Bennani, F.; Farella, M. Psychological aspects of orthodontics in clinical practice. Part one: Treatment-specific variables. Prog. Orthod. 2011, 12, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Ukra, A.; Bennani, F.; Farella, M. Psychological aspects of orthodontics in clinical practice. Part two: General psychosocial wellbeing. Prog. Orthod. 2012, 13, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Kesling, H.D. Coordinating the predetermined pattern and tooth positioner with conventional treatment. Am. J. Orthod. Oral. Surg 1946, 32, 285–293. [Google Scholar] [CrossRef]
- Kuo, E.; Miller, R.J. Automated custom-manufacturing technology in orthodontics. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 578–581. [Google Scholar] [CrossRef]
- Baldwin, D.K.; King, G.; Ramsay, D.S.; Huang, G.; Bollen, A. Activation time and material stiffness of sequential removable orthodontic appliances. Part 3: Premolar extraction patients. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 837–845. [Google Scholar] [CrossRef]
- Lin, F.; Yao, L.; Bhikoo, C.; Guo, J. Impact of fixed orthodontic appliance or clear-aligner on daily performance, in adult patients with moderate need for treatment. Patient Prefer. Adhe.r 2016, 10, 1639–1645. [Google Scholar] [CrossRef] [Green Version]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Periodontal health during clear aligners treatment: A systematic review. Eur. J. Orthod. 2015, 37, 539–543. [Google Scholar] [CrossRef]
- Kravitz, N.D.; Kusnoto, B.; Agran, B.; Viana, G. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2009, 35, 27–35. [Google Scholar] [CrossRef]
- Krieger, E.; Seiferth, J.; Marinello, I.; Jung, B.A.; Wriedt, S.; Jacobs, C.; Wehrbein, H. Invisalign® treatment in the anterior region: Were the predicted tooth movements achieved? J. Orofac. Orthop. 2012, 73, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Lagravere, M.O.; Flores-Mir, C. The treatment effects of Invisalign orthodontic aligners: A systematic review. J. Am. Dent. Assoc. 2005, 136, 1724–1729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dasy, H.; Dasy, A.; Asatrian, G.; Ròzsa, N.; Lee, H.-F.; Kwak, J.H. Effects of variable attachment shapes and aligner material on aligner retention. Angle Orthod. 2015, 85, 934–940. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hahn, W.; Dathe, H.; Fialka-Fricke, J.; Fricke-Zech, S.; Zapf, A.; Kubein-Meesenburg, D.; Sadat-Khonsari, R. Influence of thermoplastic appliance thickness on the magnitude of force delivered to a maxillary central incisor during tipping. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 12.e1–12.e7. [Google Scholar] [CrossRef]
- Lombardo, L.; Martines, E.; Mazzanti, V.; Arreghini, A.; Mollica, F. Stress relaxation properties of four orthodontic aligner materials: A 24-hour in vitro study. Angle Orthod. 2017, 87, 11–18. [Google Scholar] [CrossRef] [Green Version]
- Martorelli, M.; Gerbino, S.; Giudice, M.; Ausiello, P. A comparison between customized clear and removable orthodontic appliances manufactured using RP and CNC techniques. Dent Mater. 2013, 29, e1–e10. [Google Scholar] [CrossRef]
- Lombardo, L.; Arreghini, A.; Ramina, F.; Huanca Ghislanzoni, L.T.; Siciliani, G. Predictability of orthodontic movement with orthodontic aligners: A retrospective study. Prog. Orthod. 2017, 18, 35. [Google Scholar] [CrossRef] [Green Version]
- Katchooi, M.; Cohanim, B.; Tai, S.; Bayirli, B.; Spiekerman, C.; Huang, G. Effect of supplemental vibration on orthodontic treatment with aligners: A randomized trial. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 336–346. [Google Scholar] [CrossRef]
- Bergersen, E. The eruption guidance myofunctional appliances: How it works, how to use it. Funct. Orthod. 1984, 1, 28–29, 31–35. [Google Scholar]
- Wishney, M.; Darendeliler, M.A.; Dalci, O. Myofunctional therapy and prefabricated functional appliances: An overview of the history and evidence. Aust. Dent. J. 2019, 64, 135–144. [Google Scholar] [CrossRef]
- Migliaccio, S.; Aprile, V.; Zicari, S.; Grenci, A. Eruption guidance appliance: A review. Eur. J. Paediatr. Dent. 2014, 15, 163–166. [Google Scholar] [PubMed]
- Idris, G.; Hajeer, M.Y.; Al-Jundi, A. Soft- and hard-tissue changes following treatment of Class II division 1 malocclusion with Activator versus Trainer: A randomized controlled trial. Eur. J. Orthod. 2019, 41, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Myrlund, R.; Dubland, M.; Keski-Nisula, K.; Kerosuo, H. One-year treatment effects of the eruption guidance appliance in 7-to 8-year-old children: A randomized clinical trial. Eur. J. Orthod. 2014, 37, 128–134. [Google Scholar] [CrossRef] [Green Version]
- Čirgić, E.; Kjellberg, H.; Hansen, K. Treatment of large overjet in Angle Class II: Division 1 malocclusion with Andresen activators versus prefabricated functional appliances—a multicenter, randomized, controlled trial. Eur. J. Orthod. 2016, 38, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Usumez, S.; Uysal, T.; Sari, Z.; Basciftci, F.A.; Karaman, A.I.; Guray, E. The effects of early preorthodontic trainer treatment on Class II, division 1 patients. Angle Orthod. 2004, 74, 605–609. [Google Scholar]
- Keski-Nisula, K.; Hernesniemi, R.; Heiskanen, M.; Keski-Nisula, L.; Varrela, J. Orthodontic intervention in the early mixed dentition: A prospective, controlled study on the effects of the eruption guidance appliance. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 254–260, quiz 328.e252. [Google Scholar] [CrossRef]
- Shu, X.; Magnusson, B.H.; Burt, I.A. Treatment of adolescent patients with class II division 1 malocclusion using Eruption guidance appliance: A comparative study with Twinblock and Activator-Headgear appliances. Swed. Dent. J. 2016, 40, 79–89. [Google Scholar]
- Janson, G.R.; da Silva, C.C.A.; Bergersen, E.O.; Henriques, J.F.C.; Pinzan, A. Eruption Guidance. Appliance effects in the treatment of Class II, Division 1 malocclusions. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 119–129. [Google Scholar] [CrossRef]
- Ramirez-Yañez, G.; Sidlauskas, A.; Junior, E.; Fluter, J. Dimensional changes in dental arches after treatment with a prefabricated functional appliance. J. Clin. Pediatr. Dent. 2007, 31, 279–283. [Google Scholar] [CrossRef]
- Martin, D.; Danforth, M.E. An analysis of secular change in the human mandible over the last century. Am. J. Hum. Biol. 2009, 1, 704–706. [Google Scholar] [CrossRef]
- Yang, X.; Li, C.; Bai, D.; Su, N.; Chen, T.; Xu, Y.; Han, X. Treatment effectiveness of Frankel function regulator on the Class III malocclusion: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Vidal-Bernárdez, M.-L.; Vilches-Arenas, A.; Sonnemberg, B.; Solano-Reina, E.; Solano-Mendoza, B. Efficacy and predictability of maxillary and mandibular expansion with the Invisalign® system. J. Clin. Exp. Dent. 2021, 13, e669–e677. [Google Scholar] [CrossRef] [PubMed]
- Lione, R.; Paoloni, V.; Bartolommei, L.; Gazzani, F.; MEuli, S.; Pavoni, C.; Cozza, P. Maxillary arch development with Invisalign system: Analysis of expansion dental movements on digital dental casts. Angle Orthod. 2021, 91, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Mai, D.D.; Stucki, S.; Gkantidis, N. Assessment of methods used for 3-dimensional superimposition of craniofacial skeletal structures: A systematic review. PeerJ 2020, 8, e9263. [Google Scholar] [CrossRef] [PubMed]
- Cuccia, A.M.; Caradonna, C. The natural head position. Different techniques of head positioning in the study of craniocervical posture. Minerva Stomatol. 2009, 58, 601–612. [Google Scholar] [PubMed]
- Perrotti, G.; Baccaglione, G.; Clauser, T.; Scaini, R.; Grassi, R.; Testarelli, L.; Reda, R.; Testori, T.; Del Fabbro, M. Total Face Approach (TFA) 3D Cephalometry and Superimposition in Orthognathic Surgery: Evaluation of the Vertical Dimensions in a Consecutive Series. Methods Protoc. 2021, 4, 36. [Google Scholar] [CrossRef] [PubMed]
- Cevidanes, L.H.S.; Bailey, L.J.; Tucker, G.R.; Styner, M.A.; Mol, A.; Phillips, C.L.; Proffit, W.R.; Turvey, T. Superimposition of 3D cone-beam CT models of orthognathic surgery patients. Dentomaxillofac. Radiol. 2005, 34, 369–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, D.S.; Jeong, Y.M.; Jang, I.; Jost-Brinkmann, P.G.; Cha, B.K. Accuracy and reliability of palatal superimposition of three-dimensional digital models. Angle Orthod. 2010, 80, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Baumrind, S.; Carlson, S.; Beers, A.; Curry, S.; Norris, K.; Boyd, R.L. Using three-dimensional imaging to assess treatment outcomes in orthodontics: A progress report from the University of the Pacific. Orthod. Craniofac. Res. 2003, 6, 132–142. [Google Scholar] [CrossRef]
- Joy, J.; Kumar, A. Methods of maxillary arch expansion in orthodontics: A literature review. Int. J. Appl. Dent. Sci. 2021, 7, 251–254. [Google Scholar] [CrossRef]
- Bi, W.G.; Li, K. Effectiveness of miniscrew-assisted rapid maxillary expansion: A systematic review and meta-analysis. Clin. Oral. Investig. 2022; in press. [Google Scholar] [CrossRef]
- McMullen, C.; Al Turkestani, N.N.; Ruellas, A.C.O.; Massaro, C.; Rego, M.V.N.N.; Yatabe, M.S.; Kim-Berman, H.; McNamara, J.A., Jr.; Angelieri, F.; Franchi, L.; et al. Three-dimensional evaluation of skeletal and dental effects of treatment with maxillary skeletal expansion. Am. J. Orthod. Dentofacial Orthop. 2022, 161, 666–678. [Google Scholar] [CrossRef] [PubMed]
- Vidalón, J.A.; Loú-Gómez, I.; Quiñe, A.; Diaz, K.T.; Liñan Duran, C.; Lagravère, M.O. Periodontal effects of maxillary expansion in adults using non-surgical expanders with skeletal anchorage vs. surgically assisted maxillary expansion: A systematic review. Head Face Med. 2021, 17, 47. [Google Scholar] [CrossRef] [PubMed]
- Coloccia, G.; Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Montenegro, V.; Patano, A.; Marinelli, G.; Laudadio, C.; Limongelli, L.; Di Venere, D.; et al. Effectiveness of Dental and Maxillary Transverse Changes in Tooth-Borne, Bone-Borne, and Hybrid Palatal Expansion through Cone-Beam Tomography: A Systematic Review of the Literature. Medicina (Kaunas) 2021, 57, 288. [Google Scholar] [CrossRef] [PubMed]
- Rutili, V.; Mrakic, G.; Nieri, M.; Franceschi, D.; Pierleoni, F.; Giuntini, V.; Franchi, L. Dento-skeletal effects produced by rapid versus slow maxillary expansion using fixed jackscrew expanders: A systematic review and meta-analysis. Eur. J. Orthod. 2021, 43, 301–312. [Google Scholar] [CrossRef]
- Grassia, V.; d’Apuzzo, F.; Jamilian, A.; Femiano, F.; Favero, L.; Perillo, L. Comparison between rapid and mixed maxillary expansion through an assessment of arch changes on dental casts. Prog. Orthod. 2015, 16, 20. [Google Scholar] [CrossRef] [Green Version]






| Parameters | Pre-Operative (Mean ± SD) | Post-Operative (Mean ± SD) | Expansion (mean ± SD) | p-Value | |
|---|---|---|---|---|---|
| TOTAL STL (n = 100) | D1-D1′(mm) | 34.63 ± 2.22 | 35.48 ± 2.02 | 0.82 ± 1.32 | * |
| D2-D2′(mm) | 34.69 ± 2.22 | 35.62 ± 2.09 | 0.93 ± 1.37 | * | |
| D3-D3′(mm) | 32.24 ± 2.60 | 33.59 ± 1.96 | 1.35 ± 1.74 | * | |
| D4-D4′(mm) | 48.19 ± 3.28 | 50.58 ± 2.91 | 2.35 ± 1.64 | * | |
| Trimmed dental cast STL (n = 33) | D1-D1′(mm) | 34.84 ± 2.41 | 35.73 ± 2.32 | 1.01 ± 0.10 | * |
| D2-D2′(mm) | 34.05 ± 2.42 | 35.90 ± 2.44 | 0.85 ± 1.14 | * | |
| D3-D3′(mm) | 32.36 ± 2.74 | 33.56 ± 1.90 | 1.20 ± 0.09 | * | |
| D4-D4′(mm) | 48.76 ± 3.30 | 50.76 ± 3.00 | 1.99 ± 0.09 | * | |
| Untrimmed dental cast STL (n = 67) | D1-D1′(mm) | 34.58 ± 2.12 | 35.33 ± 1.84 | 0.75 ± 0.10 | * |
| D2-D2′(mm) | 34.54 ± 2.08 | 35.49 ± 1.88 | 0.95 ± 0.11 | * | |
| D3-D3′(mm) | 32.13 ± 2.49 | 33.60 ± 1.99 | 1.47 ± 0.10 | * | |
| D4-D4′(mm) | 47.83 ± 3.21 | 50.84 ± 2.84 | 2.58 ± 0.08 | * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perrotti, G.; Carrafiello, A.; Rossi, O.; Karanxha, L.; Baccaglione, G.; Del Fabbro, M. Clinical Use of Aligners Associated with Nuvola® OP System for Transverse Maxillary Deficiency: A Retrospective Study on 100 Patients. Int. J. Environ. Res. Public Health 2022, 19, 5751. https://doi.org/10.3390/ijerph19095751
Perrotti G, Carrafiello A, Rossi O, Karanxha L, Baccaglione G, Del Fabbro M. Clinical Use of Aligners Associated with Nuvola® OP System for Transverse Maxillary Deficiency: A Retrospective Study on 100 Patients. International Journal of Environmental Research and Public Health. 2022; 19(9):5751. https://doi.org/10.3390/ijerph19095751
Chicago/Turabian StylePerrotti, Giovanna, Alessandro Carrafiello, Ornella Rossi, Lorena Karanxha, Giulia Baccaglione, and Massimo Del Fabbro. 2022. "Clinical Use of Aligners Associated with Nuvola® OP System for Transverse Maxillary Deficiency: A Retrospective Study on 100 Patients" International Journal of Environmental Research and Public Health 19, no. 9: 5751. https://doi.org/10.3390/ijerph19095751






