Understanding Fear after an Anterior Cruciate Ligament Injury: A Qualitative Thematic Analysis Using the Common-Sense Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
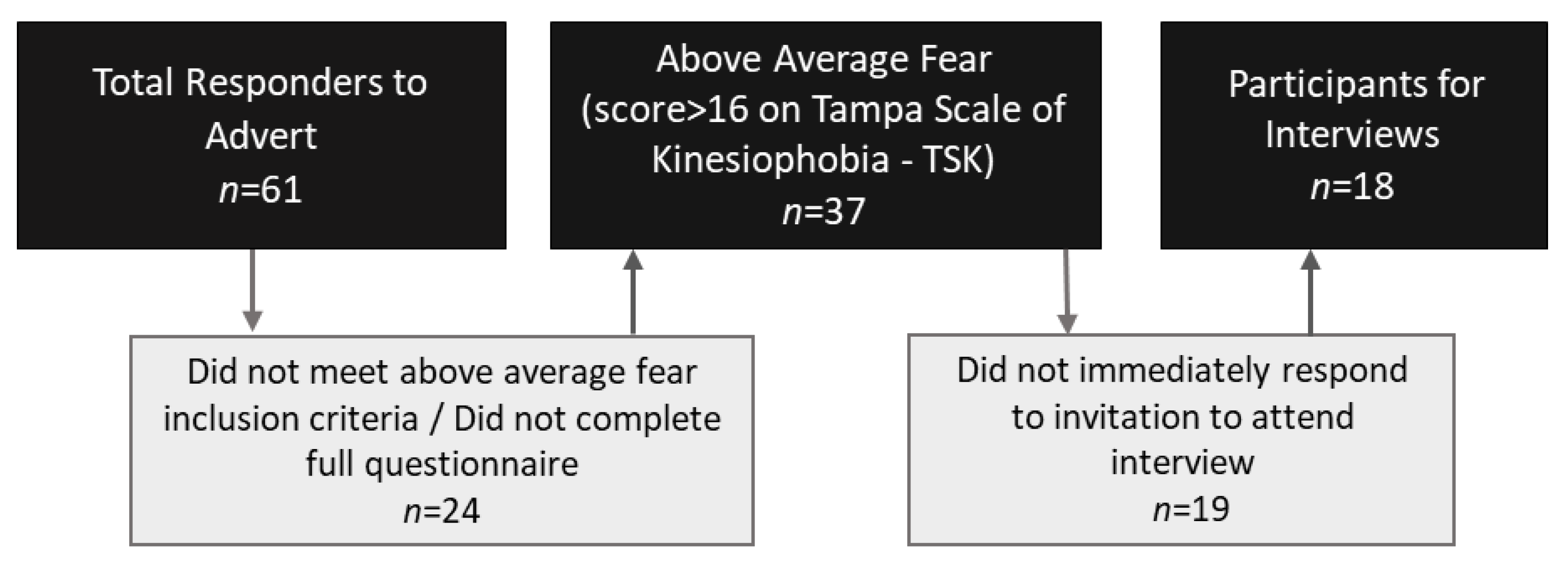
2.2. Participants
2.3. Participant Measures
2.4. Sample Size
2.5. Qualitative Data Analysis
2.6. Community Engagement
3. Results
3.1. Participant Characteristics
3.2. Themes
3.2.1. Theme 1: External Messages Driving Fear
3.2.2. Theme 2: Difficulty of the ACL Rehabilitation Journey Driving Fear
3.2.3. Theme 3: Threat to Identity and Independence Driving Fear
3.2.4. Theme 4: Socio-Economic Factors Driving Fear
3.2.5. Theme 5: Ongoing Psychological Barriers Driving Fear
3.2.6. Theme 6: Positive Coping Strategies Reducing Fear
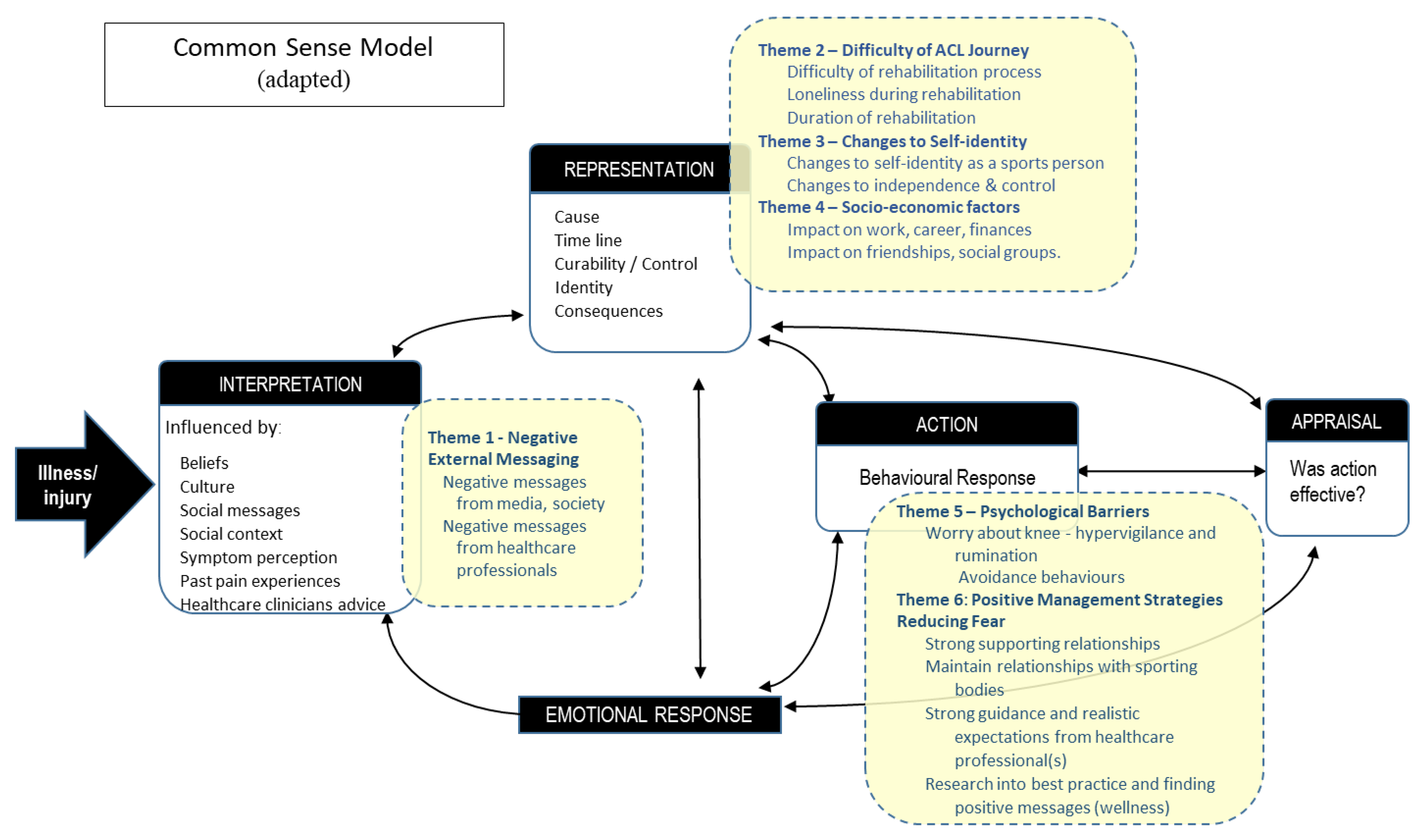
3.3. Common-Sense Model
3.4. Consumer Group Review of Results
4. Discussion
4.1. External Messages
4.2. Changes to Identity
4.3. Pain
4.4. Common-Sense Model and Fear
5. Clinical Implications
6. Strengths, Limitations, and Future Research Considerations
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Filbay, S.R.; Grindem, H. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract. Res. Clin. Rheumatol. 2019, 33, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fear of re-injury in people who have returned to sport following anterior cruciate ligament reconstruction surgery. J. Sci. Med. Sport 2012, 15, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Zbrojkiewicz, D.; Vertullo, C.; Grayson, J. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000–2015. Med. J. Aust. 2018, 208, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Maniar, N.; Verhagen, E.; Bryant, A.L.; Opar, D.A. Trends in Australian knee injury rates: An epidemiological analysis of 228,344 knee injuries over 20 years. Lancet Reg. Health West. Pac. 2022, 21, 100409. [Google Scholar] [CrossRef]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: An updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br. J. Sport. Med. 2014, 48, 1543–1552. [Google Scholar] [CrossRef]
- Nwachukwu, B.; Adjei, J.; Rauck, R.; Chahla, J.; Okoroha, K.; Verma, N.; Allen, A.; Williams, R. How Much Do Psychological Factors Affect Lack of Return to Play After Anterior Cruciate Ligament Reconstruction? A Systematic Review. Orthop. J. Sport. Med. 2019, 7, 2325967119845313. [Google Scholar] [CrossRef]
- Brewer, B.W.; Cornelius, A.E.; Van Raalte, J.L.; Brickner, J.C.; Sklar, J.H.; Corsetti, J.R.; Pohlman, M.H.; Ditmar, T.D.; Emery, K. Rehabilitation adherence and anterior cruciate ligament reconstruction outcome. Psychol. Health Med. 2004, 9, 163–175. [Google Scholar] [CrossRef]
- Padaki, A.S.; Noticewala, M.S.; Levine, W.N.; Ahmad, C.S.; Popkin, M.K.; Popkin, C.A. Prevalence of Posttraumatic Stress Disorder Symptoms Among Young Athletes After Anterior Cruciate Ligament Rupture. Orthop. J. Sport. Med. 2018, 6, 2325967118787159. [Google Scholar] [CrossRef]
- Aron, C.M.; Harvey, S.; Hainline, B.; Hitchcock, M.E.; Reardon, C.L. Post-traumatic stress disorder (PTSD) and other trauma-related mental disorders in elite athletes: A narrative review. Br. J. Sport. Med. 2019, 53, 779–784. [Google Scholar] [CrossRef]
- Bateman, A.; Morgan, K.A.D. The Postinjury Psychological Sequelae of High-Level Jamaican Athletes: Exploration of a Posttraumatic Stress Disorder-Self-Efficacy Conceptualization. J. Sport Rehabil. 2019, 28, 144–152. [Google Scholar] [CrossRef]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Whitehead, T.; Webster, K. Psychological responses matter in returning to pre-injury level of sport after anterior cruciate ligament reconstruction surgery. Am. J. Sport. Med. 2013, 41, 1549–1555. [Google Scholar] [CrossRef]
- Flanigan, D.; Everhart, J.; Pedroza, A.; Smith, T.; Kaeding, C. Fear of reinjury (kinesiophobia) and persistent knee symptoms are common factors for lack of return to sport after anterior cruciate ligament reconstruction. Arthroscopy 2013, 29, 1322–1329. [Google Scholar] [CrossRef]
- Nwachukwu, B.U.; Voleti, P.B.; Berkanish, P.; Chang, B.; Cohn, M.R.; Williams, R.J.; Allen, A.A. Return to play and patient satisfaction after ACL reconstruction: Study with minimum 2-year follow-up. J. Bone Jt. Surg. 2017, 99, 720–725. [Google Scholar] [CrossRef]
- APA. Fear. APA Dictionary of Psychology. Available online: https://dictionary.apa.org/fear (accessed on 1 November 2022).
- Ardern, C.L.; Osterberg, A.; Tagesson, S.; Gauffin, H.; Webster, K.E.; Kvist, J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br. J. Sport. Med. 2014, 48, 1613–1619. [Google Scholar] [CrossRef]
- Ardern, C.L.; Taylor, N.; Feller, J.; Webster, K. A systematic review of the psychological factors associated with returning to sport following injury. Br. J. Sport. Med. 2012, 47, 1120–1126. [Google Scholar] [CrossRef]
- Ardern, C.L.; Webster, K.E.; Taylor, N.F.; Feller, J.A. Return to sport following anterior cruciate ligament reconstruction surgery: A systematic review and meta-analysis of the state of play. Br. J. Sport. Med. 2011, 45, 596–606. [Google Scholar] [CrossRef]
- Kvist, J.; Ek, A.; Sporrstedt, K.; Good, L. Fear of re-injury: A hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg. Sport. Traumatol. Arthrosc. 2005, 13, 393–397. [Google Scholar] [CrossRef]
- Burland, J.; Toonstra, J.; Werner, L.; Mattacola, G.C.; Howell, M.D.; Howard, S.J. Decision to Return to Sport After Anterior Cruciate Ligament Reconstruction, Part I: A Qualitative Investigation of Psychosocial Factors. J. Athl. Train. 2018, 53, 452–463. [Google Scholar] [CrossRef]
- DiSanti, J.; Lisee, C.; Erickson, K.; Bell, D.; Shingles, M.; Kuenze, C. Perceptions of Rehabilitation and Return to Sport Among High School Athletes With Anterior Cruciate Ligament Reconstruction: A Qualitative Research Study. J. Orthop. Sport. Phys. Ther. 2018, 48, 951–959. [Google Scholar] [CrossRef]
- Ross, A.C.; Clifford, A.; Louw, A.Q. Factors informing fear of reinjury after anterior cruciate ligament reconstruction. Physiother. Theory Pract. 2017, 33, 103–114. [Google Scholar] [CrossRef]
- Scott, M.S.; Perry, A.M.; Sole, G. “Not always a straight path”: Patients’ perspectives following anterior cruciate ligament rupture and reconstruction. Disabil. Rehabil. 2018, 40, 2311–2317. [Google Scholar] [CrossRef] [PubMed]
- Tjong, V.K.; Murnaghan, M.L.; Nyhof-Young, J.M.; Ogilvie-Harris, D.J. A qualitative investigation of the decision to return to sport after anterior cruciate ligament reconstruction: To play or not to play. Am. J. Sport. Med. 2014, 42, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, H.; Phillips, L.A.; Burns, E. The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. J. Behav. Med. 2016, 39, 935–946. [Google Scholar] [CrossRef] [PubMed]
- Bunzli, S.; Smith, A.; Schütze, R.; Lin, I.; O’Sullivan, P. Making Sense of Low Back Pain and Pain-Related Fear. J. Orthop. Sport. Phys. 2017, 47, 628–636. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, B.I.R.; Smith, A.J.; O’Sullivan, P.P.B.; Haebich, S.; Fick, D.; Khan, R.; Bunzli, S. ‘My hip is damaged’: A qualitative investigation of people seeking care for persistent hip pain. Br. J. Sport. Med. 2020, 54, 858–865. [Google Scholar] [CrossRef]
- Beales, D.; Slater, H.; Palsson, T.; O’Sullivan, P. Understanding and managing pelvic girdle pain from a person-centred biopsychosocial perspective. Musculoskelet Sci. Pract. 2020, 48, 102152. [Google Scholar] [CrossRef]
- Thorne, S.; Kirkham, S.R.; O’Flynn-Magee, K. The Analytic Challenge in Interpretive Description. Int. J. Qual. Methods 2004, 3, 1–11. [Google Scholar] [CrossRef]
- Thorne, S.; Reimer, K.S.; MacDonald-Emes, J. Interpretive description: A noncategorical qualitative alternative for developing nursing knowledge. Res. Nurs. Health 1997, 20, 169–177. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Successful Qualitative Research: A Practical Guide for Beginners; SAGE Publications Ltd.: London, UK, 2013. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Healthc. 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm. Policy Ment. Health 2015, 42, 533–544. [Google Scholar] [CrossRef]
- Burgi, C.R.; Peters, S.; Ardern, C.L.; Magill, J.R.; Gomez, C.D.; Sylvain, J.; Reiman, M.P. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. Br. J. Sport. Med. 2019, 53, 1154–1161. [Google Scholar] [CrossRef]
- Chalmers, P.N.; Mall, N.A.; Moric, M.; Sherman, S.L.; Paletta, G.P.; Cole, B.J. Does ACL reconstruction alter natural history? A systematic literature review of long-term outcomes. J. Bone Jt. Surg. Am. 2014, 96A, 292–300. [Google Scholar] [CrossRef]
- Delincé, P.; Ghafil, D. Anterior cruciate ligament tears: Conservative or surgical treatment? A critical review of the literature. Knee Surg. Sport. Traumatol. Arthrosc. 2012, 20, 48–61. [Google Scholar] [CrossRef]
- Filbay, S.R.; Culvenor, A.G.; Ackerman, I.N.; Russell, T.G.; Crossley, K.M. Quality of life in anterior cruciate ligament-deficient individuals: A systematic review and meta-analysis. Br. J. Sport. Med. 2015, 49, 1033–1041. [Google Scholar] [CrossRef]
- Harris, K.P.; Driban, J.B.; Sitler, M.R.; Cattano, N.M.; Balasubramanian, E.; Hootman, J.M. Tibiofemoral osteoarthritis after surgical or nonsurgical treatment of anterior cruciate ligament rupture: A systematic review. J. Athl. Train. 2015, 52, 507–517. [Google Scholar] [CrossRef]
- Smith, T.O.; Postle, K.; Penny, F.; McNamara, I.; Mann, C.J.V. Is reconstruction the best management strategy for anterior cruciate ligament rupture? A systematic review and meta-analysis comparing anterior cruciate ligament reconstruction versus non-operative treatment. Knee 2014, 21, 462–470. [Google Scholar] [CrossRef]
- Muaidi, Q.I.; Nicholson, L.L.; Refshauge, K.M.; Herbert, R.D.; Maher, C.G. Prognosis of conservatively managed anterior cruciate ligament injury: A systematic review. Sport. Med. 2007, 37, 703–716. [Google Scholar] [CrossRef]
- Kovalak, E.; Atay, T.; Çetin, C.; Atay, İ.M.; Serbest, M. OIs ACL reconstruction a prerequisite for the patients having recreational sporting activities? Acta Orthop. Traumatol. Turc. 2018, 52, 37–43. [Google Scholar] [CrossRef]
- Saueressig, T.; Braun, T.; Steglich, N.; Diemer, F.; Zebisch, J.; Herbst, M.; Zinser, W.; Owen, P.; Belavy, D.L. Primary surgery versus primary rehabilitation for treating anterior cruciate ligament injuries: A living systematic review and meta-analysis. Br. J. Sport. Med. 2022, 56, 1241–1251. [Google Scholar] [CrossRef]
- Webster, K.E.; Feller, J.A.; Lambros, C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys. Ther. Sport 2008, 9, 9–15. [Google Scholar] [CrossRef]
- Ardern, C.L.; Glasgow, P.; Schneiders, A.; Witvrouw, E.; Clarsen, B.; Cools, A.; Gojanovic, B.; Griffin, S.; Khan, K.M.; Moksnes, H.; et al. 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br. J. Sport. Med. 2016, 50, 853. [Google Scholar] [CrossRef] [PubMed]
- Campbell, P.; Bishop, A.; Dunn, K.; Main, J.C.; Thomas, E.; Foster, E.N. Conceptual overlap of psychological constructs in low back pain. Pain 2013, 154, 1783–1791. [Google Scholar] [CrossRef] [PubMed]
- Bunzli, S.; Smith, A.; Schütze, R.; O’Sullivan, P. Beliefs underlying pain-related fear and how they evolve: A qualitative investigation in people with chronic back pain and high pain-related fear. BMJ Open 2015, 5, e008847. [Google Scholar] [CrossRef] [PubMed]
- Bowen, G.A. Naturalistic inquiry and the saturation concept: A research note. Qual. Res. 2008, 8, 137–152. [Google Scholar] [CrossRef]
- O’Reilly, M.; Parker, N. ‘Unsatisfactory Saturation’: A critical exploration of the notion of saturated sample sizes in qualitative research. Qual. Res. 2012, 13, 190–197. [Google Scholar] [CrossRef]
- Morse, J.M.; Field, P.A. Qualitative Research Methods for Health Professionals; SAGE Publications: Thousand Oaks, CA, USA, 1995. [Google Scholar]
- Thompson, B.J.; Thorne, S.; Sandhu, G. Interpretive description: A flexible qualitative methodology for medical education research. Med. Educ. 2021, 55, 336–343. [Google Scholar] [CrossRef]
- Staniszewska, S.; Brett, J.; Simera, I.; Seers, K.; Mockford, C.; Goodlad, S.; Altman, D.G.; Moher, D.; Barber, R.; Denegri, S.; et al. GRIPP2 reporting checklists: Tools to improve reporting of patient and public involvement in research. Bmj 2017, 358, j3453. [Google Scholar] [CrossRef]
- Mahood, C.; Perry, M.; Gallagher, P.; Sole, G. Chaos and confusion with confidence: Managing fear of Re-Injury after anterior cruciate ligament reconstruction. Phys. Ther. Sport 2020, 45, 145–154. [Google Scholar] [CrossRef]
- Darlow, B.; Dowell, A.; Baxter, G.D.; Mathieson, F.; Perry, M.; Dean, S. The enduring impact of what clinicians say to people with low back pain. Ann. Fam. Med. 2013, 11, 527–534. [Google Scholar] [CrossRef]
- Howick, J.; Moscrop, A.; Mebius, A.; Fanshawe, T.R.; Lewith, G.; Bishop, F.L.; Mistiaen, P.; Roberts, N.W.; Dieninytė, E.; Hu, X.-Y.; et al. Effects of empathic and positive communication in healthcare consultations: A systematic review and meta-analysis. J. R. Soc. Med. 2018, 111, 240–252. [Google Scholar] [CrossRef]
- Christino, M.A.; Fantry, A.J.; Vopat, B.G. Psychological Aspects of Recovery Following Anterior Cruciate Ligament Reconstruction. J. Am. Acad. Orthop. Surg. 2015, 23, 501–509. [Google Scholar] [CrossRef]
- Lie, H.C.; Juvet, L.K.; Street, R.L.; Gulbrandsen, P.; Mellblom, A.V.; Brembo, E.A.; Eide, H.; Heyn, L.; Saltveit, K.H.; Strømme, H.; et al. Effects of Physicians’ Information Giving on Patient Outcomes: A Systematic Review. J. Gen. Intern. Med. 2022, 37, 651–663. [Google Scholar] [CrossRef]
- Ivarsson, A.; Tranaeus, U.; Johnson, U.; Stenling, A. Negative psychological responses of injury and rehabilitation adherence effects on return to play in competitive athletes: A systematic review and meta-analysis. Open Access J. Sport. Med. 2017, 8, 27–32. [Google Scholar] [CrossRef]
- Brewer, B.W.; Cornelius, A.E. Self-Protective Changes in Athletic Identity Following Anterior Cruciate Ligament Reconstruction. Psychol. Sport Exerc. 2010, 11, 1–5. [Google Scholar] [CrossRef]
- Truong, L.K.; Mosewich, A.D.; Holt, C.J.; Le, C.Y.; Miciak, M.; Whittaker, J.L. Psychological, social and contextual factors across recovery stages following a sport-related knee injury: A scoping review. Br. J. Sport. Med. 2020, 54, 1149–1156. [Google Scholar] [CrossRef]
- Ohji, S.; Aizawa, J.; Hirohata, K.; Mitomo, S.; Ohmi, T.; Jinno, T.; Koga, H.; Yagishita, K. Athletic identity and sport commitment in athletes after anterior cruciate ligament reconstruction who have returned to sports at their pre-injury level of competition. BMC Sport. Sci. Med. Rehabil. 2021, 13, 37. [Google Scholar] [CrossRef]
- George, S.Z.; Lentz, T.A.; Zeppieri, G.; Lee, D.; Chmielewski, T.L. Analysis of shortened versions of the tampa scale for kinesiophobia and pain catastrophizing scale for patients after anterior cruciate ligament reconstruction. Clin. J. Pain 2012, 28, 73–80. [Google Scholar] [CrossRef]
- Rex, C.C.; Metzler, J.N. Development of the Sport Injury Anxiety Scale. Meas. Phys. Educ. Exerc. Sci. 2016, 20, 146–158. [Google Scholar] [CrossRef]
- Bittencourt, N.F.N.; Meeuwisse, W.H.; Mendonça, L.D.; Nettel-Aguirre, A.; Ocarino, J.M.; Fonseca, S.T. Complex systems approach for sports injuries: Moving from risk factor identification to injury pattern recognition—Narrative review and new concept. Br. J. Sport. Med. 2016, 50, 1309. [Google Scholar] [CrossRef]
- Gatchel, R.J.; Peng, Y.B.; Peters, M.L.; Fuchs, P.N.; Turk, D.C. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychol. Bull. 2007, 133, 581–624. [Google Scholar] [CrossRef]
- Orbell, S.; Johnston, M.; Rowley, D.; Espley, A.; Davey, P. Cognitive representations of illness and functional and affective adjustment following surgery for osteoarthritis. Soc. Sci. Med. 1998, 47, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Hanusch, B.; O’connor, D.; Ions, P.; Scott, A.; Gregg, P. Effects of psychological distress and perceptions of illness on recovery from total knee replacement. Bone Jt. J. 2014, 96, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Bijsterbosch, J.; Scharloo, M.; Visser, A.; Watt, I.; Meulenbelt, I.; Huizinga, T.; Kaptein, A.; Kloppenburg, M. Illness perceptions in patients with osteoarthritis: Change over time and association with disability. Arthritis Care Res. 2009, 61, 1054–1061. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Campbell, P.; Strauss, V.Y.; Foster, N.E.; Jordan, K.P.; Dunn, K.M. Trajectories and predictors of the long-term course of low back pain: Cohort study with 5-year follow-up. Pain 2018, 159, 252. [Google Scholar] [CrossRef]
- Caneiro, J.P.; Bunzli, S.; O’Sullivan, P. Beliefs about the body and pain: The critical role in musculoskeletal pain management. Braz. J. Phys. 2021, 25, 17–29. [Google Scholar] [CrossRef]
- Roelofs, J.; Goubert, L.; Peters, M.L.; Vlaeyen, J.W.; Crombez, G. The Tampa Scale for Kinesiophobia: Further examination of psychometric properties in patients with chronic low back pain and fibromyalgia. Eur. J. Pain 2004, 8, 495–502. [Google Scholar] [CrossRef]
| ID | P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 | P9 | P10 | P11 | P12 | P13 | P14 | P15 | P16 | P17 | P18 | Mean (SD) | Median (IQR) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 22 | 25 | 33 | 28 | 24 | 22 | 28 | 32 | 23 | 44 | 31 | 33 | 32 | 31 | 24 | 23 | 36 | 25 | 28.0 (5.86) | 28.0 (23.8, 32.3) |
| Sex | F | F | M | F | F | F | M | M | F | F | F | F | F | F | M | M | F | F | M:5, F:13 | |
| Tampa Scale of Kinesiophobia 1 | 19 | 17 | 33 | 23 | 23 | 18 | 21 | 17 | 17 | 21 | 31 | 25 | 17 | 22 | 25 | 30 | 18 | 30 | 22.6 (5.35) | 21.5 (17.8, 26.3) |
| Anterior Cruciate Ligament Return to Sport Index 2 | 39.4 | 34.2 | 25.8 | 41.7 | 52.5 | 28.3 | 53.3 | 63.3 | 66.7 | 66.7 | 20.0 | 16.7 | 65.8 | 18.3 | 31.7 | 47.5 | 41.7 | 15.8 | 40.5 (17.93) | 40.6 (24.4, 55.8) |
| Fear of movement 3 | 1 | 4 | 3 | 0 | 4 | 2 | 0 | 0 | 0 | 3 | 10 | 0 | 0 | 6 | 3 | 8 | 2 | 2 | 2.67 (2.91) | 2.0 (0, 4) |
| Distress/Anxiety related to knee movements 3 | 1 | 1 | 5 | 1 | 4 | 0 | 0 | 0 | 0 | 3 | 8 | 5 | 0 | 6 | 4 | 7 | 3 | 1 | 2.72 (2.65) | 2.0 (0, 5) |
| Lack of confidence in knee movements 3 | 0 | 8 | 7 | 2 | 5 | 2 | 0 | 0 | 0 | 7 | 10 | 5 | 0 | 6 | 4 | 6 | 5 | 4 | 3.94 (3.15) | 4.5 (0.0, 6.25) |
| Pain 3 | 1 | 7 | 2 | 1 | 6 | 0 | 2 | 0 | 0 | 6 | 3 | 0 | 0 | 6 | 1 | 2 | 3 | 1 | 2.28 (2.4) | 1.5 (0.0, 3.8) |
| Surgery | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | N | Y:16, N:2 | |
| Psychological support provided | N | Y | N | N | N | N | N | Y | N | N | N | N | N | N | N | N | N | N | Y:2, N:16 | |
| Return to previous level of function 4 | 2 | 2 | 0 | 2 | 3 | 2 | 3 | 1 | 3 | 1 | 2 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | Count 5: 0:1 1:8 2:6 3:3 | |
| Year(s) of ACL injury 6 | ’16 | ’17 ’18 | ‘16 | ’16 | ’17 | ’11 ’16 | ‘17 | ’11 ‘12 | ‘15 | ‘18 | ‘15 | ‘08 | ‘08 | ’06 ‘09 ’13 | ‘19 | ‘19 | ‘06 | ‘19 | ||
| Messages from society | |
| Q1.1 | If you just hear ‘ACL’ it kicks in that fear like, ‘wow, this is bad’. (P9) |
| Q1.2 | … seeing idols and professional athletes, the people that you look up to on a day-to-day basis, seeing them with ACL injuries and then just hearing their stories that they can’t go back and perform at a level which they used to (P14) |
| Q1.3 | Since knowing that it’s an ACL injury … I don’t go running. (P11) |
| Messages from healthcare professionals | |
| Q1.4 | He said (the surgeon) to take up golf. He was really angry about the last one (referring to a rerupture of surgically repaired ligament) because it ruined all of his beautiful work. (P14) |
| Q1.5 | He said (the surgeon) it was ‘One of the worst injuries he had seen that year’ and he said, ‘you must have been in a world of pain at the time’ (P13) |
| The difficulty of the rehabilitation process and its psychological effects | |
| Q2.1 | Any time that I did feel anything that twitched the knee, or it buckled or it didn’t feel right in that first six months, it was almost as detrimental mentally than it did the knee. I was, like, ‘Whoa, I’ve got a long way to go’. every time, every time’. (P14) |
| Q2.2 | … the rehab just felt like a chore that I had to do rather than something that I wasn’t really invested in…I wasn’t really great at that … (P10) |
| Q2.3 | when you tear your ACL, you’ve got yourself to deal with and you’ve got to push yourself through it all (P15) |
| Q2.4 | I remember waking up from surgery, and it hurt and I was just like, “Oh, why did I do this?” This is really painful now. That was really annoying. I second-guessed why I got the surgery done. (P6) |
| Q2.5 | When I was in the Zimmer splint for my friend’s wedding, we were quite high up and I just kind of had, like, a quick thought of, what if I jumped—it got pretty dark. (P14) |
| Q2.6 | I didn’t have a great time when I was in the splint, I pretty much was just at home in bed for that whole month and couldn’t walk around much. That was very miserable. I was like, ‘I would really hate to have to do all that again’. (P5) |
| Loneliness during rehabilitation | |
| Q2.7 | The loneliness was every lift I ever did, every workout I ever did, every preinjury (exercise) … you have got to do 90% of it on your own. (P2) |
| Q2.8 | It was very isolating and it’s just so monotonous. You don’t feel anything and that sucks. (P5) |
| Q2.9 | you know they’re in for that long recovery and going back to that like loneliness… it’s like your road to recovery … you just feel lonely through the whole process (P1) |
| Q2.10 | You go from a hospital bed, everyone’s there for you, and then suddenly, everyone has to go to work… and everything is by yourself. (P2) |
| The duration of the rehabilitation and recovery process | |
| Q2.11 | I’ll be like crying too some nights. Like is it ever going to end or whatever (P1) |
| Q2.12 | An ACL sucks up a good six to 12 months … minimum. In whatever plans I might have for getting myself together, you might as well write off 12 months of that. I don’t have enough 12 months left while I’m motivated and I’m feeling youngish (P10) |
| Q2.13 | there was a period of time within my recovery… and I just was really over it and I remember that’s when I was quite disheartened (P9) |
| Changes to self-identity as an athlete/sports person/competitor | |
| Q3.1 | I wasn’t able to be that sporty person and always be out training, playing sport … That whole perception of me being the sporty person, yeah, it just kind of went out the window. (P1) |
| Q3.2 | It was just one of those things where I was now the knee person, the person with the knee injury. I used to be the person that would say yes to anything. I would just say, ‘Yes, let’s do it, give it a try’. Now I don’t. (P12) |
| Q3.3 | I can’t play basketball anymore because of my knees, and I’m like, I’m 25 … it’s disabling a little bit. Physically, I can do those things, but it’s the mental factor that’s stopping me. It’s frustrating, the fear is what’s stopping me. (P2) |
| Q3.4 | I was very competitive at hockey, I was playing a good grade, and I just wouldn’t be able to get back to that (P4) |
| Q3.5 | Everyone said I should have been right to play, so I did go back to try and play. I was just like, ‘No, I can’t. There’s something wrong, so I can’t keep playing’. … I just never went and tried playing again (P12) |
| Changes to independence | |
| Q3.6 | The lack of Independence… not being able to do things for myself and then relying on other people, that stresses me out (P14). |
| Q3.7 | it’s quite humiliating to have to get on the tram in crutches, that sense of I want to be independent in that sense with my own movement and it’s that sense of uselessness (P18) |
| Q3.8 | Having to ask someone to help you get up and go to the toilet or something like that. You just feel like a … burden. (P7) |
| Impact on work, career, and/or financial situation | |
| Q4.1 | Wow. I wasn’t able to work for basically nine months. I was pretty new in my career at that point in time, so there went work (P4) |
| Q4.2 | My Mum is very watchful of money, so if I was doing something that maybe she thought could hurt me again, she would be like, ‘You don’t want to have to pay for a surgery and blah, blah, blah’. If I were to say to my Mum I was going to play lacrosse again, she would be like, ‘I don’t think that’s a good idea’. (P18) |
| Q4.3 | Well, I have a very expensive left knee. I don’t want to make it more expensive than it currently is. I think I’ve spent enough money on it (P6) |
| Q4.4 | Oh, it left me pretty devastated. Losing my job…but then having to go and find another job and all that stuff was pretty difficult and hard to take just because of a stupid soccer injury. (P3) |
| Impact on friendships and social grouping | |
| Q4.5 | Friendships changed. I just moved away from a lot of friends. I wasn’t able to drive initially. It’s changed my entire friendship group (P4) |
| Q4.6 | I would have liked to have taken up more you know activities, you know dance or you know something different, but I just feel like I can’t because of my knee (P14) |
| Anxiety, rumination, and avoidance | |
| Q5.1 | It makes me anxious as well, like in the future…if I get pregnant… is my knee is going to hold up during that time as well. (P14) |
| Q5.2 | In your brain, you can go, ‘Oh, if you’re a really active person, maybe really active people are more likely to do an ACL twice. Maybe I’ll just be a less active person, then I’ll avoid that possibility’. (P10) |
| Q5.3 | My risk of re-tearing my knee is astronomical… I think about skiing and I go, ‘Woah, no’, but I would love to ski. (P2) |
| Q5.4 | It’s constantly on my mind now in everyday life whether that’s walking, running or standing up. (P15) |
| Q5.5 | I think the fear ultimately stems from doing it again, the pain of that, the cost of that and the time that will take from my life again. I just don’t want to be a victim to it again. (P18) |
| Q5.6 | Constant analysis … instead of being able to go out and 100% enjoy something, you spend 50%, 75% of the time thinking or analyzing your knee … If I’ve got any unexplained pain in my knee that I can’t explain away … then I’m really afraid to do anything other than just walking. (P8) |
| Q5.7 | After I had done all my rehab, if people… frightened me or got too close, I actually started having what I could call panic attacks, like hyperventilating and just shutting down. (P5) |
| Q5.8 | It’s constantly on my mind now in everyday life whether that’s walking, running or standing up. (P15) |
| Trauma associated with the initial injury | |
| Q5.9 | … from watching AFL… hear them say, oh I felt the pop, and it sends shivers down your spine … it’s so easy to do, it looks so easy. I was scared to go back so I never … I still think about it because it just triggers those memories and stuff again. (P1) |
| Q5.10 | I used to have flashbacks … I’d just be driving or walking or anything and I’d just have these flashbacks to it happening. (P2) |
| Q5.11 | Probably the most painful thing that’s ever happened to me. I remember when it happened, I just physically collapsed … I could’ve been shot by a bullet, I could’ve been hit by a bus, I had no idea. (P18) |
| Q5.12 | I know the feeling of the pop as well, it’s like I can still imagine it to this day … that’s had such an effect on my life. (P1) |
| Q5.13 | It was very painful and excruciating. I remember every part of it. Everything that I did that was cringy during it because I felt my knee twist, I felt a pop. I screamed, ‘I heard a pop’. (P16) |
| Gain strong support from family and friends | |
| Q6.1 | … Good family and friends’ support to begin with. The best thing for me is that one of my very good friends he did his ACL about a week after me. We ended up being able to, I guess just talk about it. Being each other’s own little support network (P4) |
| Q6.2 | Previously I’d had to get my boyfriend to hold me up on the bike, try and pedal and it’s like in my mind I couldn’t do it. Then as soon as he (the surgeon) told me that (I could ride) the next morning I said, ‘I’m going to go try and ride around the block’. It was like I could just do it. (P18) |
| Q6.4 | It’s nice to relate to someone about an injury and talk about things that you might be feeling with it not feeling 100% (P13) |
| Obtain clear guidance on rehabilitation program | |
| Q6.7 | If I didn’t have (such) a good relationship with my physios, I don’t think I would have had as good of an outcome. (P7) |
| Q6.8 | The owners of the gym, they helped me accept it in that they validated that it is an injury and it’s okay that it has a big impact on my life. Just because other people might be going through really, really bad things, my life experiences are different to the next person. If this is the worst thing that ever happened to me, that’s okay. (P4) |
| Q6.9 | My physio was fantastic and he always, yeah, gave me a lot of reassurance (P9) |
| Q6.10 | My physios and the doc and my surgeon were really good at outlining … the stages and the roadmap of how we’re going to get back…and always available to answer questions (P7) |
| Maintain connection with sporting clubs or organizations | |
| Q6.11 | Once I could start walking around my Frisbee team gave me an assistant coach position or a training coach position and so that meant I could start going down to trainings and watching and try help coach and learn things from that perspective. I think that that’s when my rehab and getting back into sport really picked up. (P5) |
| Q6.12 | People knew that you’re always coming back and so it was, “Just do as much as you can no one’s going to judge you for it. We know that you are worthy of being on this team no matter what level you’re playing at”. (P5) |
| Conduct private research on injury and rehabilitation best practice | |
| Q6.13 | I’d read up with athletes and a lot of athletes go through very public rehabs these days, so you have some kind of idea and understanding of what it’s going to be like. (P7) |
| Q6.14 | I was gathering information from people in the (online) community who had torn their ACLs before…Finding out how to go through it the best way is something that gave me a lot of peace (P16) |
| Q6.15 | After being diagnosed with a torn ACL, that’s when I started doing some research and I was like, “Okay, Oh, this is pretty common, and this is where the ligament is, blah, blah, blah” … Just that sense of not knowing that was all (that made) me distressed. (P11) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Little, C.; Lavender, A.P.; Starcevich, C.; Mesagno, C.; Mitchell, T.; Whiteley, R.; Bakhshayesh, H.; Beales, D. Understanding Fear after an Anterior Cruciate Ligament Injury: A Qualitative Thematic Analysis Using the Common-Sense Model. Int. J. Environ. Res. Public Health 2023, 20, 2920. https://doi.org/10.3390/ijerph20042920
Little C, Lavender AP, Starcevich C, Mesagno C, Mitchell T, Whiteley R, Bakhshayesh H, Beales D. Understanding Fear after an Anterior Cruciate Ligament Injury: A Qualitative Thematic Analysis Using the Common-Sense Model. International Journal of Environmental Research and Public Health. 2023; 20(4):2920. https://doi.org/10.3390/ijerph20042920
Chicago/Turabian StyleLittle, Cameron, Andrew P. Lavender, Cobie Starcevich, Christopher Mesagno, Tim Mitchell, Rodney Whiteley, Hanieh Bakhshayesh, and Darren Beales. 2023. "Understanding Fear after an Anterior Cruciate Ligament Injury: A Qualitative Thematic Analysis Using the Common-Sense Model" International Journal of Environmental Research and Public Health 20, no. 4: 2920. https://doi.org/10.3390/ijerph20042920
APA StyleLittle, C., Lavender, A. P., Starcevich, C., Mesagno, C., Mitchell, T., Whiteley, R., Bakhshayesh, H., & Beales, D. (2023). Understanding Fear after an Anterior Cruciate Ligament Injury: A Qualitative Thematic Analysis Using the Common-Sense Model. International Journal of Environmental Research and Public Health, 20(4), 2920. https://doi.org/10.3390/ijerph20042920










