Clinical Outcome of Arthroscopic Repair for Isolated Meniscus Tear in Athletes
Abstract
1. Introduction
2. Methods
2.1. Study Design
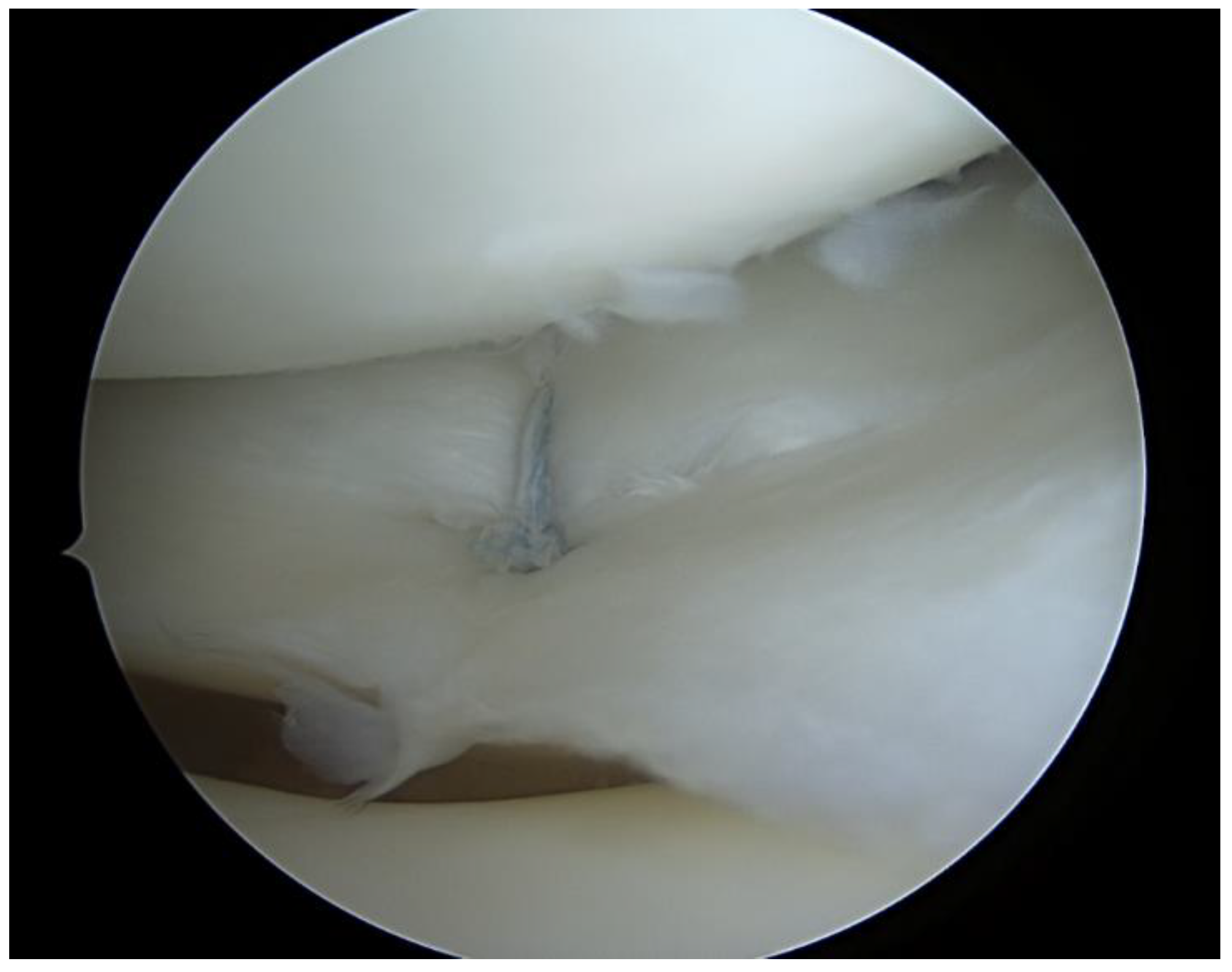
2.2. Surgical Technique
2.3. Rehabilitation
2.4. Statistical Analysis
3. Results
3.1. Study and Patients Characteristics
3.2. Main Study Findings
3.3. Subjective Outcome Scores
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dhollander, A.; Verdonk, P.; Verdonk, R. Treatment of Painful, Irreparable Partial Meniscal Defects with a Polyurethane Scaffold: Midterm Clinical Outcomes and Survival Analysis: Midterm Clinical Outcomes and Survival Analysis. Am. J. Sports Med. 2016, 44, 2615–2621. [Google Scholar] [CrossRef] [PubMed]
- Carter, T.E.; Taylor, K.A.; Spritzer, C.E.; Utturkar, G.M.; Taylor, D.C.; Moorman, C.T., 3rd; Garrett, W.E.; Guilak, F.; McNulty, A.L.; DeFrate, L.E. In Vivo Cartilage Strain Increases Following Medial Meniscal Tear and Correlates with Synovial Fluid Matrix Metalloproteinase Activity. J. Biomech. 2015, 48, 1461–1468. [Google Scholar] [CrossRef] [PubMed]
- Eberbach, H.; Zwingmann, J.; Hohloch, L.; Bode, G.; Maier, D.; Niemeyer, P.; Südkamp, N.P.; Feucht, M.J. Sport-Specific Outcomes after Isolated Meniscal Repair: A Systematic Review. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 762–771. [Google Scholar] [CrossRef] [PubMed]
- DePhillipo, N.N.; LaPrade, R.F.; Zaffagnini, S.; Mouton, C.; Seil, R.; Beaufils, P. The Future of Meniscus Science: International Expert Consensus. J. Exp. Orthop. 2021, 8, 24. [Google Scholar] [CrossRef]
- Nakayama, H.; Kanto, R.; Kambara, S.; Kurosaka, K.; Onishi, S.; Yoshiya, S.; Yamaguchi, M. Clinical Outcome of Meniscus Repair for Isolated Meniscus Tear in Athletes. Asia Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2017, 10, 4–7. [Google Scholar] [CrossRef] [PubMed]
- Lutz, C.; Dalmay, F.; Ehkirch, F.P. Meniscectomy versus Meniscal Repair: 233 10 Years Radiological and Clinical Results in Vertical Lesions in Stable Knee. Orthop. Traumatol. Surg. Res. 2015, 101, S327–S331. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Zhao, J. A Meta-Analysis Comparing Meniscal Repair with Meniscectomy in the Treatment of Meniscal Tears: The More Meniscus, the Better Outcome? Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Mosich, G.M.; Lieu, V.; Ebramzadeh, E.; Beck, J.J. Operative Treatment of Isolated Meniscus Injuries in Adolescent Patients: A Meta-Analysis and Review. Sports Health 2018, 10, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Blanchard, E.R.; Hadley, C.J.; Wicks, E.D.; Emper, W.; Cohen, S.B. Return to Play after Isolated Meniscal Repairs in Athletes: A Systematic Review. Orthop. J. Sports Med. 2020, 8, 2325967120962093. [Google Scholar] [CrossRef] [PubMed]
- Paxton, E.S.; Stock, M.V.; Brophy, R.H. Meniscal Repair versus Partial Meniscectomy: A Systematic Review Comparing Reoperation Rates and Clinical Outcomes. Arthroscopy 2011, 27, 1275–1288. [Google Scholar] [CrossRef] [PubMed]
- Stein, T.; Mehling, A.P.; Welsch, F.; von Eisenhart-Rothe, R.; Jäger, A. Long-Term Outcome after Arthroscopic Meniscal Repair versus Arthroscopic Partial Meniscectomy for Traumatic Meniscal Tears. Am. J. Sports Med. 2010, 38, 1542–1548. [Google Scholar] [CrossRef] [PubMed]
- Logan, M.; Watts, M.; Owen, J.; Myers, P. Meniscal Repair in the Elite Athlete: Results of 45 Repairs with a Minimum 5-Year Follow-up: Results of 45 Repairs with a Minimum 5-Year Follow-Up. Am. J. Sports Med. 2009, 37, 1131–1134. [Google Scholar] [CrossRef] [PubMed]
- Marcacci, M.; Marcheggiani Muccioli, G.M.; Grassi, A.; Ricci, M.; Tsapralis, K.; Nanni, G.; Bonanzinga, T.; Zaffagnini, S. Arthroscopic Meniscus Allograft Transplantation in Male Professional Soccer Players: A 36-Month Follow-up Study: A 36-Month Follow-up Study. Am. J. Sports Med. 2014, 42, 382–388. [Google Scholar] [CrossRef] [PubMed]
- Andrade, R.; Vasta, S.; Papalia, R.; Pereira, H.; Oliveira, J.M.; Reis, R.L.; Espregueira-Mendes, J. Prevalence of Articular Cartilage Lesions and Surgical Clinical Outcomes in Football (Soccer) Players’ Knees: A Systematic Review. Arthroscopy 2016, 32, 1466–1477. [Google Scholar] [CrossRef] [PubMed]
- Aune, K.T.; Andrews, J.R.; Dugas, J.R.; Cain, E.L., Jr. Return to Play after Partial Lateral Meniscectomy in National Football League Athletes. Am. J. Sports Med. 2014, 42, 1865–1872. [Google Scholar] [CrossRef] [PubMed]
- Spang, R.C., III; Nasr, M.C.; Mohamadi, A.; DeAngelis, J.P.; Nazarian, A.; Ramappa, A.J. Rehabilitation Following Meniscal Repair: A Systematic Review. BMJ Open Sport Exerc. Med. 2018, 4, e000212. [Google Scholar] [CrossRef] [PubMed]
- Casp, A.J.; Bodkin, S.G.; Gwathmey, F.W.; Werner, B.C.; Miller, M.D.; Diduch, D.R.; Brockmeier, S.F.; Hart, J.M. Effect of Meniscal Treatment on Functional Outcomes 6 Months after Anterior Cruciate Ligament Reconstruction. Orthop. J. Sports Med. 2021, 9, 232596712110312. [Google Scholar] [CrossRef] [PubMed]
- Zimmerer, A.; Sobau, C.; Nietschke, R.; Schneider, M.; Ellermann, A. Long-Term Outcome after All inside Meniscal Repair Using the FasT-Fix System. J. Orthop. 2018, 15, 602–605. [Google Scholar] [CrossRef] [PubMed]

| Age, (years) | 25.5 (range, 12–57) |
| Male:female, n | 38:14 |
| Type of injury, n (contact:non-contact) | 14:38 |
| Follow-up period (months) | 33.3 (range, 10–80) |
| Pre-Operative Tegner | Post-Operative Tegner | Post-Operative Lysholm | Post-Operative † KOOS | Post-Operative ‡ IKDC | |
|---|---|---|---|---|---|
| Mean (±sd) | 7.1 (±2.1) | 6.2 (±2.2) | 90.3 (±10.7) | 89 (±11.1) | 88.8 (±17.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vrgoč, G.; Vuletić, F.; Matolić, G.; Ivković, A.; Hudetz, D.; Bulat, S.; Bukvić, F.; Janković, S. Clinical Outcome of Arthroscopic Repair for Isolated Meniscus Tear in Athletes. Int. J. Environ. Res. Public Health 2023, 20, 5088. https://doi.org/10.3390/ijerph20065088
Vrgoč G, Vuletić F, Matolić G, Ivković A, Hudetz D, Bulat S, Bukvić F, Janković S. Clinical Outcome of Arthroscopic Repair for Isolated Meniscus Tear in Athletes. International Journal of Environmental Research and Public Health. 2023; 20(6):5088. https://doi.org/10.3390/ijerph20065088
Chicago/Turabian StyleVrgoč, Goran, Filip Vuletić, Grgur Matolić, Alan Ivković, Damir Hudetz, Stjepan Bulat, Frane Bukvić, and Saša Janković. 2023. "Clinical Outcome of Arthroscopic Repair for Isolated Meniscus Tear in Athletes" International Journal of Environmental Research and Public Health 20, no. 6: 5088. https://doi.org/10.3390/ijerph20065088
APA StyleVrgoč, G., Vuletić, F., Matolić, G., Ivković, A., Hudetz, D., Bulat, S., Bukvić, F., & Janković, S. (2023). Clinical Outcome of Arthroscopic Repair for Isolated Meniscus Tear in Athletes. International Journal of Environmental Research and Public Health, 20(6), 5088. https://doi.org/10.3390/ijerph20065088






