Insights into the Impact of Organizational Factors and Burnout on the Employees of a For-Profit Psychiatric Hospital during the Third Wave of the COVID-19 Pandemic
Abstract
:1. Introduction and Background
2. Case: A CMO’s Assessment during Crisis of Compassion and Leadership
3. Methodology
4. Survey Results
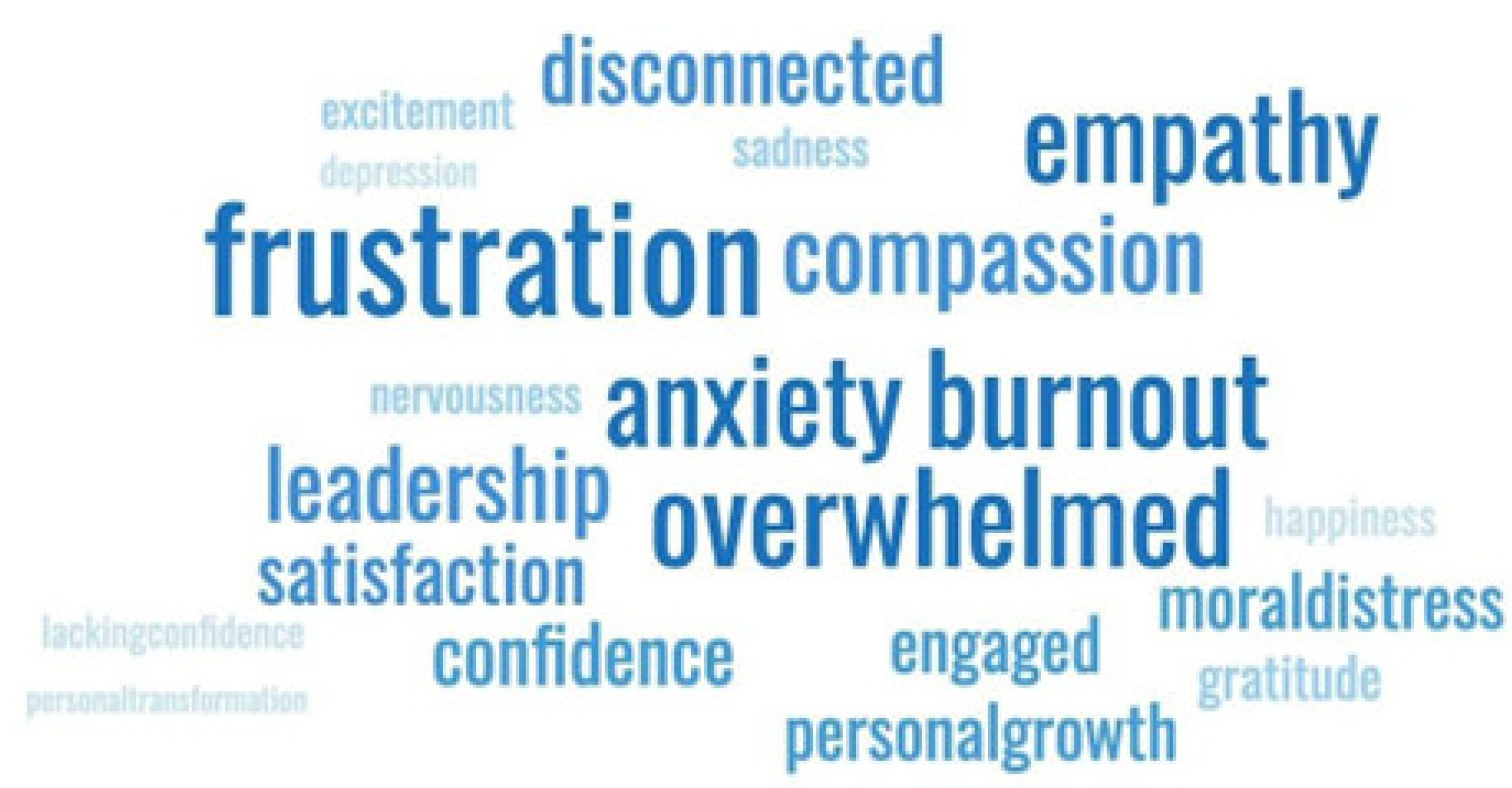
5. Thematic Results
5.1. Organizational Factors and Their Relationships to Job Demands
5.2. Burnout, Affective Commitment, and Their Relationship to Job Satisfaction
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dyrbye, L.; Shanafelt, T. Burnout Among Healthcare Professionals: A Call to Explore and Address This Underrecognized Threat to Safe, High Quality Care. Natl. Acad. Med. 2017, 7, 1–11. [Google Scholar]
- Reith, T.P. Burnout in United States Healthcare Professionals: A Narrative Review. Cureus 2018, 10, 12. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, S.L.; Bakker, A.B.; Gruman, J.A.; Macey, W.H.; Saks, A.M. Employee engagement, human resource management practices and competitive advantage: An integrated approach. J. Organ. Eff. 2015, 2, 7–35. [Google Scholar] [CrossRef]
- Greco, P.; Laschinger, H.K.S.; Wong, C. Leader empowering behaviours, staff nurse empowerment and work engagement/burnout. Can. J. Nurs. Leadersh. 2006, 19, 41–56. [Google Scholar] [CrossRef] [PubMed]
- Leary, T.G.; Green, R.; Denson, K.; Schoenfeld, G.; Henley, T.; Langford, H. The relationship among dysfunctional leadership dispositions, employee engagement, job satisfaction, and burnout. Psychol. Manag. J. 2013, 16, 112. [Google Scholar] [CrossRef]
- Spence Laschinger, H.K.; Wong, C.A.; Greco, P. The impact of staff nurse empowerment on person-job fit and work engagement/burnout. Nurs. Adm. Q. 2006, 30, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Prentice, S.; Elliott, T.; Dorstyn, D.; Benson, J. Burnout, wellbeing and how they relate: A qualitative study in general practice trainees. Med. Educ. 2023, 57, 243. [Google Scholar] [CrossRef] [PubMed]
- Abdollahimohammad, A.; Firouzkouhi, M. Future Perspectives of Nurses with COVID 19. J. Patient Exp. 2020, 7, 640–641. [Google Scholar] [CrossRef]
- Aloweni, F.; Ayre, T.C.; Wong, W.H.M.; Tan, H.K.; Teo, I. The Impact of the Work Environment, Workplace Support and Individual-Related Factors on Burnout Experience of Nurses during the COVID-19 Pandemic. J. Nurs. Patient Saf. 2020, 1, 2766–9653. [Google Scholar]
- Kakemam, E.; Chegini, Z.; Rouhi, A.; Ahmadi, F.; Majidi, S. Burnout and its relationship to self-reported quality of patient care and adverse events during COVID-19: A cross-sectional online survey among nurses. J. Nurs. Manag. 2021, 29, 7. [Google Scholar] [CrossRef]
- Rangachari, P.; Woods, J.L. Preserving organizational resilience, patient safety, and staff retention during covid-19 requires a holistic consideration of the psychological safety of healthcare workers. Int. J. Environ. Res. Public Health 2020, 17, 4267. [Google Scholar] [CrossRef] [PubMed]
- Phungsoonthorn, T.; Charoensukmongkol, P. How does mindfulness help university employees cope with emotional exhaustion during the COVID-19 crisis? The mediating role of psychological hardiness and the moderating effect of workload. Scand. J. Psychol. 2022, 63, 449. [Google Scholar] [CrossRef] [PubMed]
- Figley, C.R. Compassion fatigue: Psychotherapists’ chronic lack of self care. J. Clin. Psychol. 2002, 58, 1433–1441. [Google Scholar] [CrossRef] [PubMed]
- Fourie, C. The Ethical Significance of Moral Distress: Inequality and Nurses’ Constraint-Distress. Am. J. Bioeth. 2016, 16, 23–25. [Google Scholar] [CrossRef] [PubMed]
- Jameton, A. A Reflection on Moral Distress in Nursing Together with a Current Application of the Concept. J. Bioethical Inq. 2013, 10, 297–308. [Google Scholar] [CrossRef] [PubMed]
- Delfrate, F.; Ferrara, P.; Spotti, D.; Terzoni, S.; Lamiani, G.; Canciani, E.; Bonetti, L. Moral Distress (MD) and burnout in mental health nurses: A multicenter survey. Med. Lav. 2018, 109, 2. [Google Scholar]
- Ohnishi, K.; Kitaoka, K.; Bower, L.; Duncan, S.; Van Der Merwe, M.; Nakano, M.; Ohgushi, Y.; Tanaka, H.; Fujii, H. Comparison of moral distress and burnout experienced by mental health nurses in Japan and England: A cross-sectional questionnaire survey. J. Japan Health Med. Assoc. 2011, 20, 73–86. [Google Scholar]
- Pearson, G.S. Moral Distress and Psychiatric Nursing. J. Am. Psychiatr. Nurses Assoc. 2021, 27, 441–442. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.Y.; Han, W.L.; Qin, W.; Yin, H.X.; Zhang, C.F.; Kong, C.; Wang, Y.L. Extent of compassion satisfaction, compassion fatigue and burnout in nursing: A meta-analysis. J. Nurs. Manag. 2018, 26, 810–819. [Google Scholar] [CrossRef]
- Van Woerkom, M.; Bakker, A.B.; Nishii, L.H. Accumulative job demands and support for strength use: Fine-tuning the job demands-resources model using conservation of resources theory. J. App. Psychol. 2016, 101, 141. [Google Scholar] [CrossRef]
- Liu, N.; Zhang, F.; Wei, C.; Jia, Y.; Shang, Z.; Sun, L.; Wu, L.; Sun, Z.; Zhou, Y.; Wang, Y.; et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020, 287, 112921. [Google Scholar] [CrossRef] [PubMed]
- Puyod, J.V.; Charoensukmongkol, P. Interacting effect of social media crisis communication and organizational citizenship behavior on Employees’ resistance to change during the COVID-19 crisis: Evidence from university employees in The Philippines. Asia-Pacific Soc. Sci. Rev. 2021, 21, 13. [Google Scholar]
- Sidwell, A.J. Psychological hardiness and self-leadership: Leading yourself to effective stress coping. Int. J. Existent. Posit. Psychol. 2019, 8, 12. [Google Scholar]
- Ye, B.; Zhao, S.; Zeng, Y.; Chen, C.; Zhang, Y. Perceived parental support and college students’ depressive symptoms during the COVID-19 pandemic: The mediating roles of emotion regulation strategies and resilience. Curr. Psychol. 2023, 42, 20275. [Google Scholar] [CrossRef]
- Mathieu, F. Running on empty: Compassion fatigue in health professionals. Rehab. Community Care Med. 2007, 4, 1–7. [Google Scholar]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef]
- Van Bogaert, P.; Clarke, S.; Willems, R.; Mondelaers, M. Staff engagement as a target for managing work environments in psychiatric hospitals: Implications for workforce stability and quality of care. J. Clin. Nurs. 2013, 22, 11–12. [Google Scholar] [CrossRef] [PubMed]
- Abdirahman, H.I.H.; Najeemdeen, I.S.; Abidemi, B.T.; Ahmad, R. The Relationship between Job Satisfaction, Work-Life Balance and Organizational Commitment on Employee Performance. Adv. Bus. Res. Int. J. 2020, 4, 42–52. [Google Scholar] [CrossRef]
- Lamiani, G.; Borghi, L.; Argentero, P. When healthcare professionals cannot do the right thing: A systematic review of moral distress and its correlates. J. Health Psychol. 2017, 22, 51–67. [Google Scholar] [CrossRef]
- Najeemdeen, I.S.; Taofik Abidemi, B.; Rahmat, F.D.; Bulus, D. Perceived Organizational Culture and Perceived Organizational Support on Work Engagement. Acad. J. Econ. Stud. 2018, 4, 199–208. [Google Scholar]
- Alsaraireh, F.; Quinn Griffin, M.T.; Ziehm, S.R.; Fitzpatrick, J.J. Job satisfaction and turnover intention among Jordanian nurses in psychiatric units. Int. J. Ment. Health Nurs. 2014, 23, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Bamber, M. An investigation of occupational stress among nurse tutors. Nurs. Pract. 1991, 4, 19–22. [Google Scholar] [CrossRef]
- Baum, A.; Kagan, I. Job Satisfaction and Intent to Leave Among Psychiatric Nurses: Closed Versus Open Wards. Arch. Psychiatr. Nurs. 2015, 29, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Yanchus, N.J.; Periard, D.; Moore, S.C.; Carle, A.C.; Osatuke, K. Predictors of Job Satisfaction and Turnover Intention in VHA Mental Health Employees: A Comparison Between Psychiatrists, Psychologists, Social Workers, and Mental Health Nurses. Hum. Serv. Organ. Manag. Leadersh. Gov. 2015, 39, 219–244. [Google Scholar] [CrossRef]
- Maslach, C. Job Burnout: New Directions in Research and Intervention. Curr. Dir. Psychol. Sci. 2003, 12, 189–192. [Google Scholar] [CrossRef]
- Maslach, C.; Leiter, M.P. Early Predictors of Job Burnout and Engagement. J. Appl. Psychol. 2008, 93, 498. [Google Scholar] [CrossRef] [PubMed]
- Rabei, S.H.; El Fatah, W.O. Assessing COVID19-related anxiety in an Egyptian sample and correlating it to knowledge and stigma about the virus. Middle East Curr. Psychiatr. 2021, 28, 1–7. [Google Scholar] [CrossRef]
- Raval, N. Mental health implications of COVID-19 in India. Indian J. Health Well-Being. 2020, 11, 276. [Google Scholar]
- Padmanabhanunni, A.; Pretorius, T.B. Job satisfaction goes a long way: The Mediating Role of Teaching Satisfaction in the Relationship between Role Stress and Indices of Psychological Well-Being in the Time of COVID-19. Int. J. Environ. Res. Public Health. 2022, 19, 17071. [Google Scholar] [CrossRef]
- Ivbijaro, G.; Brooks, C.; Kolkiewicz, L.; Sunkel, C.; Long, A. Psychological impact and psychosocial consequences of the COVID 19 pandemic Resilience, mental well-being, and the coronavirus pandemic. Indian J. Psychiatry 2020, 62, S395–S403. [Google Scholar] [CrossRef]
- Bridget Duffy, M. Now is the time to redefine safety in healthcare. Healthc. Manag. Forum 2021, 34, 6. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, C.; Ashcroft, R.; Bobbette, N.; Mills, C.; Mofina, A.; Tran, T.; Vader, K.; Williams, A.; Gill, S.; Miller, J. Interprofessional primary care during COVID-19: A survey of the provider perspective. BMC Fam. Pract. 2021, 22, 31. [Google Scholar] [CrossRef] [PubMed]
- Hebles, M.; Trincado-Munoz, F.; Ortega, K. Stress and Turnover Intentions Within Healthcare Teams: The Mediating Role of Psychological Safety, and the Moderating Effect of COVID-19 Worry and Supervisor Support. Front. Psychol. 2022, 12, 758438. [Google Scholar] [CrossRef] [PubMed]
- Stafford, J.L.; Leon-Castelao, E.; Klein Ikkink, A.J.; Qvindesland, S.A.; Garcia-Font, M.; Szyld, D.; Diaz-Navarro, C. Clinical debriefing during the COVID-19 pandemic: Hurdles and opportunities for healthcare teams. Adv. Simul. 2021, 6, 32. [Google Scholar] [CrossRef] [PubMed]
- Walton, M.; Murray, E.; Christian, M.D. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Veleva, M. “Liquid Society”: The Decline of Values and its Reflection on Contemporary Leadership. Izvestia J. Union Sci. Varna. Econ. Sci. Ser. 2017, 1, 148–157. [Google Scholar]
- Dalal, R.S. A meta-analysis of the relationship between organizational citizenship behavior and counterproductive work behavior. J. Appl. Psychol. 2005, 90, 1241. [Google Scholar] [CrossRef] [PubMed]
- Cénat, J.M.; Farahi, S.M.M.M.; Dalexis, R.D.; Darius, W.P.; Bekarkhanechi, F.M.; Poisson, H.; Broussard, C.; Ukwu, G.; Auguste, E.; Nguyen, D.D.; et al. The global evolution of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis of longitudinal studies. J. Affect. Disord. 2022, 315, 70–95. [Google Scholar] [CrossRef] [PubMed]
- Kola, L.; Kohrt, B.A.; Hanlon, C.; Naslund, J.A.; Sikander, S.; Balaji, M.; Benjet, C.; Cheung, E.Y.L.; Eaton, J.; Gonsalves, P.; et al. COVID-19 mental health impact and responses in low-income and middle-income countries: Reimagining global mental health. Lancet Psychiatry 2021, 8, 535–550. [Google Scholar] [CrossRef]
- Li, S. Correlation among mental health, work stress and job burnout of rural teachers. Rev. Argent. Clin. Psicol. 2020, 29, 1345. [Google Scholar]
- Morgantini, L.A.; Naha, U.; Wang, H.; Francavilla, S.; Acar, Ö.; Flores, J.M.; Crivellaro, S.; Moreira, D.; Abern, M.; Eklund, M.; et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PLoS ONE 2020, 15, e0239393. [Google Scholar] [CrossRef] [PubMed]
- Nochaiwong, S.; Ruengorn, C.; Thavorn, K.; Hutton, B.; Awiphan, R.; Phosuya, C.; Ruanta, Y.; Wongpakaran, N.; Wongpakaran, T. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 10173. [Google Scholar] [CrossRef]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Hassamal, S.; Dong, F.; Hassamal, S.; Lee, C.; Ogunyemi, D.; Neeki, M.M. The psychological impact of COVID-19 on hospital staff. West J. Emerg. Med. 2021, 22, 346. [Google Scholar] [CrossRef] [PubMed]
- Chhablani, N.; Choudhari, S.G. Behind the frontline: A review on the impact of COVID-19 pandemic on healthcare workers. Cureus 2022, 14, 9. [Google Scholar] [CrossRef] [PubMed]
- Li, J.N.; Jiang, X.M.; Zheng, Q.X.; Lin, F.; Chen, X.Q.; Pan, Y.Q.; Zhu, Y.; Liu, R.L.; Huang, L. Mediating effect of resilience between social support and compassion fatigue among intern nursing and midwifery students during COVID-19: A cross-sectional study. BMC Nurs. 2023, 22, 42. [Google Scholar] [CrossRef]
- Kong, D.T.; Belkin, L.Y. You Don’t Care for me, So What’s the Point for me to Care for Your Business? Negative Implications of Felt Neglect by the Employer for Employee Work Meaning and Citizenship Behaviors Amid the COVID-19 Pandemic. J. Bus. Ethics. 2022, 181, 645–660. [Google Scholar] [CrossRef] [PubMed]
- Chew, N.W.S.; Lee, G.K.H.; Tan, B.Y.Q.; Jing, M.; Goh, Y.; Ngiam, N.J.H.; Yeo, L.L.L.; Ahmad, A.; Ahmed Khan, F.; Napolean Shanmugam, G.; et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020, 88, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef]
- Furfaro, H. What’s behind the ‘Momentous’ Move to Close a WA State for Profit Psychiatric Hospital? Seattle Times. 2023. Available online: https://www.seattletimes.com/seattle-news/mental-health/whats-behind-the-momentous-move-to-close-a-wa-for-profit-psych-hospital/#:~:text=Amid%20few%20details%2C%20some%20in,the%20shuttering%20of%20some%20wards (accessed on 13 March 2024).
- Padmanabhanunni, A.; Pretorius, T.B.; Isaacs, S.A. We Are Not Islands: The Role of Social Support in the Relationship between Perceived Stress during the COVID-19 Pandemic and Psychological Distress. Int. J. Environ. Res. Public Health. 2023, 20, 3179. [Google Scholar] [CrossRef]
- Jiménez, P.; Bregenzer, A.; Kallus, K.W.; Fruhwirth, B.; Wagner-Hartl, V. Enhancing resources at the workplace with health-promoting leadership. Int. J. Environ. Res. Public Health 2017, 14, 1264. [Google Scholar] [CrossRef] [PubMed]
- Ashfaq, F.; Abid, G.; Ilyas, S. Impact of ethical leadership on employee engagement: Role of self-efficacy and organizational commitment. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 962. [Google Scholar] [CrossRef] [PubMed]
- Maben, J.; Conolly, A.; Abrams, R.; Rowland, E.; Harris, R.; Kelly, D.; Kent, B.; Couper, K. ‘You can’t walk through water without getting wet’ UK nurses’ distress and psychological health needs during the Covid-19 pandemic: A longitudinal interview study. Int. J. Nurs. Stud. 2022, 131, 104242. [Google Scholar] [CrossRef] [PubMed]
- Abid, G.; Contreras, F.; Rank, S.; Ilyas, S. Sustainable leadership and wellbeing of healthcare personnel: A sequential mediation model of procedural knowledge and compassion. Front. Psychol. 2023, 13, 1039456. [Google Scholar] [CrossRef] [PubMed]
- Seppala, E.; Cameron, K. Proof That Positive Work Cultures Are More Productive. Harv. Bus. Rev. 2015, 12, 44–50. [Google Scholar]
- Kuluski, K.; Reid, R.J.; Baker, G.R. Applying the principles of adaptive leadership to person-centred care for people with complex care needs: Considerations for care providers, patients, caregivers and organizations. Health Expect. 2021, 24, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Cresswell, J.W.; Plano-Clark, V.L.; Gutmann, M.L.; Hanson, W.E. Advanced mixed methods research designs. In Handbook Mixed Methods in Social & Behavioral Research; Sage Publications: Thousand Oaks, CA, USA, 2003; pp. 209–240. [Google Scholar]
- Longnecker, D.E.; Patton, M.; Dickler, R.M. Roles and responsibilities of chief medical officers in member organizations of the Association of American Medical Colleges. Acad. Med. 2007, 82, 258–263. [Google Scholar] [CrossRef]
- Sonnenberg, M. Chief Medical Officer: Changing Roles and Skill Sets. Phys. Leadersh. J. 2015, 2, 16. [Google Scholar]
- Bodini, L.; Bonetto, C.; Cheli, S.; Del Piccolo, L.; Rimondini, M.; Rossi, A.; Carta, A.; Porru, S.; Amaddeo, F.; Lasalvia, A. Effectiveness of a Mindful Compassion Care Program in reducing burnout and psychological distress amongst frontline hospital nurses during the COVID-19 pandemic: A study protocol for a randomized controlled trial. Trials 2022, 23, 734. [Google Scholar] [CrossRef]
- Cresswell, J.W.; Plano-Clark, V.L.; Gutmann, M.L.; Hanson, W.E. An Expanded Typology for Classifying Mixed Methods Research into Designs. In Handbook of Mixed Methods in Social and Behavioral Research; Sage: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Polit, D.; Beck, C. Essentials of Nursing Research: Appraising Evidence for Nursing Practice; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2020. [Google Scholar]
- Morgeson, F.P.; Humphrey, S.E. The Work Design Questionnaire (WDQ): Developing and validating a comprehensive measure for assessing job design and the nature of work. J. Appl. Psychol. 2006, 91, 1321. [Google Scholar] [CrossRef] [PubMed]
- Eldh, A.C.; Årestedt, L.; Berterö, C. Quotations in Qualitative Studies: Reflections on Constituents, Custom, and Purpose. Int. J. Qual. Methods 2020, 19, 1609406920969268. [Google Scholar] [CrossRef]
- Ibrahim, I.; Ali, K.; Alzoubi, I.A.; Alzubi, M.M.; AL-Tahitah, A.; Kadhim, K.G. Impact of Employee’s Engagement and Task Identity on Employee’s Retention Strategy Mediated by Job Satisfaction. Lect. Notes Netw. Syst. 2023, 40, 599–613. [Google Scholar]
- Junça-Silva, A.; Menino, C. How Job Characteristics Influence Healthcare Workers’ Happiness: A Serial Mediation Path Based on Autonomous Motivation and Adaptive Performance. Sustainability 2022, 14, 21. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. Job demands-resources theory: Taking stock and looking forward. J. Occup. Health Psychol. 2017, 22, 273. [Google Scholar] [CrossRef] [PubMed]
- Singh, H. Employee Energy and Engagement: Keys to Clinician and Organization Well-Being in a Crisis. Front. Health Serv. Manag. 2021, 38, 39–44. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, M.; Shimoinaba, K.; Zhong, Y.; Peyton, S. Self-compassion training in palliative care during COVID-19: A pilot study. Palliat. Support. Care. 2022, 10, 1–6. [Google Scholar]
- She, R.; Wong, K.; Lin, J.; Leung, K.; Zhang, Y.; Yang, X. How COVID-19 stress related to schooling and online learning affects adolescent depression and Internet gaming disorder: Testing Conservation of Resources theory with sex difference. J. Behav. Addict. 2021, 10, 953. [Google Scholar] [PubMed]
- Ye, B.; Wu, D.; Im, H.; Liu, M.; Wang, X.; Yang, Q. Stressors of COVID-19 and stress consequences: The mediating role of rumination and the moderating role of psychological support. Child. Youth Serv. Rev. 2020, 118, 05466. [Google Scholar] [CrossRef]
- Bertuzzi, V.; Semonella, M.; Bruno, D.; Manna, C.; Edbrook-Childs, J.; Giusti, E.M.; Castelnuovo, G.; Pietrabissa, G. Psychological support interventions for healthcare providers and informal caregivers during the COVID-19 pandemic: A systematic review of the literature. Int. J. Environ. Res. Public Health 2021, 18, 6939. [Google Scholar] [CrossRef]
- Suleiman-Martos, N.; Gomez-Urquiza, J.L.; Aguayo-Estremera, R.; Cañadas-De La Fuente, G.A.; De La Fuente-Solana, E.I.; Albendín-García, L. The effect of mindfulness training on burnout syndrome in nursing: A systematic review and meta-analysis. J. Adv. Nurs. 2020, 76, 1124. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım, M.; Çiçek, İ.; Şanlı, M.E. Coronavirus stress and COVID-19 burnout among healthcare staffs: The mediating role of optimism and social connectedness. Curr. Psychol. 2021, 40, 5763. [Google Scholar] [CrossRef] [PubMed]
- Ponti, M.A.D.; Devet, R. Transforming nursing leadership roles: From CNO to CEO. Nurs. Adm. Q. 2012, 36, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Raftery, C.; Sassenberg, A.M.; Bamford-Wade, A. Business acumen for nursing leaders, optional or essential in today’s health system? A discussion paper. Collegian 2021, 28, 610. [Google Scholar] [CrossRef] [PubMed]
- Okuyan, C.B.; Begen, M.A. Working from home during the COVID-19 pandemic, its effects on health, and recommendations: The pandemic and beyond. Perspect. Psychiatr. Care 2021, 58, 173. [Google Scholar] [CrossRef] [PubMed]
- Lown, B.A. Translational, Transformative Compassion to Support the Healthcare Workforce. J. Healthc. Manag. 2021, 66, 254–257. [Google Scholar] [CrossRef]
- Thienprayoon, R.; Sinclair, S.; Lown, B.A.; Pestian, T.; Awtrey, E.; Winick, N.; Kanov, J. Organizational Compassion: Ameliorating Healthcare Workers’ Suffering and Burnout. J. Wellness 2022, 4, 1. [Google Scholar] [CrossRef]



| Organizational Factors | |||
|---|---|---|---|
Job related factors:
| Knowledge Characteristics:
| Justice Aspects:
| Social Characteristics:
|
| Psychological Factors | |||
| Burnout | |||
| Attitudinal Factors | |||
|
|
| |
| Variables | I Do not Intend to Quit My Job for Another Job (n = 10) | I Intend to Quit My Job for Another Job (n = 9) | Total (n = 19) | p-Value |
|---|---|---|---|---|
| ||||
| N Missing | 1 | 0 | 1 | 0.62 |
| 20–30 yr | 3 (33.3%) | 1 (11.1%) | 4 (22.2%) | |
| 30–45 yr | 3 (33.3%) | 5 (55.6%) | 8 (44.4%) | |
| 45–60 yr | 3 (33.3%) | 3 (33.3%) | 6 (33.3%) | |
| ||||
| N Missing | 1 | 0 | 1 | 0.99 |
| Female | 8 (88.9%) | 7 (77.8%) | 15 (83.3%) | |
| Male | 1 (11.1%) | 2 (22.2%) | 3 (16.7%) | |
| ||||
| N Missing | 1 | 0 | 1 | 0.25 |
| Asian | 2 (22.2%) | 0 | 2 (11.1%) | |
| Black or African American | 0 | 2 (22.2%) | 2 (11.1%) | |
| Hispanic or Latin | 1 (11.1%) | 0 | 1 (5.6%) | |
| Mixed | 1 (11.1%) | 3 (33.3%) | 4 (22.2%) | |
| White | 5 (55.6%) | 4 (44.4%) | 9 (50.0%) | |
| ||||
| N Missing | 1 | 0 | 1 | 0.14 |
| 1. 30,000–49,999 | 1 (11.1%) | 4 (44.4%) | 5 (27.8%) | |
| 2. 50,000–99,999 | 6 (66.7%) | 2 (22.2%) | 8 (44.4%) | |
| 3. 100,000–124,999 | 1 (11.1%) | 0 | 1 (5.6%) | |
| 4. 150,000–199,999 | 1 (11.1%) | 3 (33.3%) | 4 (22.2%) | |
| ||||
| 1. <1 Year | 8 (80.0%) | 4 (44.4%) | 12 (63.2%) | 0.34 |
| 2. 1–2 Year | 1 (10.0%) | 3 (33.3%) | 4 (21.1%) | |
| 3. >2 Years | 1 (10.0%) | 2 (22.2%) | 3 (15.8%) | |
| ||||
| N Missing | 4 | 4 | 8 | 0.14 |
| Entry Level | 1 (16.7%) | 0 | 1 (9.1%) | |
| Mid Level | 0 | 1 (20.0%) | 1 (9.1%) | |
| Nursing | 3 (50.0%) | 0 | 3 (27.3%) | |
| Physician | 0 | 2 (40.0%) | 2 (18.2%) | |
| Technician | 2 (33.3%) | 2 (40.0%) | 4 (36.4%) | |
| ||||
| Mean (SD) | 44.4 (5.0) | 45.9 (7.2) | 45.2 (6.1) | 0.90 |
| Median (Q1, Q3) | 45.0 (40.0, 48.0) | 44.5 (42.0, 49.0) | 45.0 (40.0, 48.0) |
| Question Number | Question Details | Variable | p-Value |
|---|---|---|---|
| Q18 | I feel pressured by my employer to meet my objectives | Ability to Achieve Objectives | 0.05 ** |
| Q42 | Some days I feel tired even before I get to work | Burnout | 0.01 ** |
| Q43 | During my workdays I often feel emotionally drained | Burnout | 0.03 ** |
| Question Number | Question Details | Variable | p-Value |
|---|---|---|---|
| Q 11 | I have some control over what I am supposed to accomplish | Work Autonomy | 0.023 ** |
| Q16 | My job allows me to complete work I start | Ability to Achieve Objectives | 0.002 *** |
| Q19 | I feel that my objectives are realistic | Ability to Achieve Objectives | 0.04 ** |
| Q20 | Reaching my objective gives me access to compensation (salary and bonuses) | Distributive Justice | <0.0001 *** |
| Q35 | I am fairly compensated for work well done | Distributive Justice | 0.02 ** |
| Q37 | The procedures are applied consistently and uniformly | Procedural Justice | 0.05 * |
| Q45 | I am very satisfied with my current job | Job Satisfaction | 0.01 ** |
| Q46 | Stress levels are manageable at work | Burnout | 0.04 ** |
| Q48 | I am proud to belong to this organization | Affective Commitment | 0.003 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seyffert, M.; Wu, C.; Özkan-Seely, G.F. Insights into the Impact of Organizational Factors and Burnout on the Employees of a For-Profit Psychiatric Hospital during the Third Wave of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2024, 21, 484. https://doi.org/10.3390/ijerph21040484
Seyffert M, Wu C, Özkan-Seely GF. Insights into the Impact of Organizational Factors and Burnout on the Employees of a For-Profit Psychiatric Hospital during the Third Wave of the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2024; 21(4):484. https://doi.org/10.3390/ijerph21040484
Chicago/Turabian StyleSeyffert, Michael, Chunyi Wu, and Gülru F. Özkan-Seely. 2024. "Insights into the Impact of Organizational Factors and Burnout on the Employees of a For-Profit Psychiatric Hospital during the Third Wave of the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 21, no. 4: 484. https://doi.org/10.3390/ijerph21040484
APA StyleSeyffert, M., Wu, C., & Özkan-Seely, G. F. (2024). Insights into the Impact of Organizational Factors and Burnout on the Employees of a For-Profit Psychiatric Hospital during the Third Wave of the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 21(4), 484. https://doi.org/10.3390/ijerph21040484





