Meta-Analysis of Internet Gaming Disorder Prevalence: Assessing the Impacts of DSM-5 and ICD-11 Diagnostic Criteria
Abstract
1. Introduction
1.1. Differences in Prevalence under Different Diagnostic Criteria
1.2. The Impact of Cultural Background
1.3. The Present Study
2. Method
2.1. Protocol and Registration
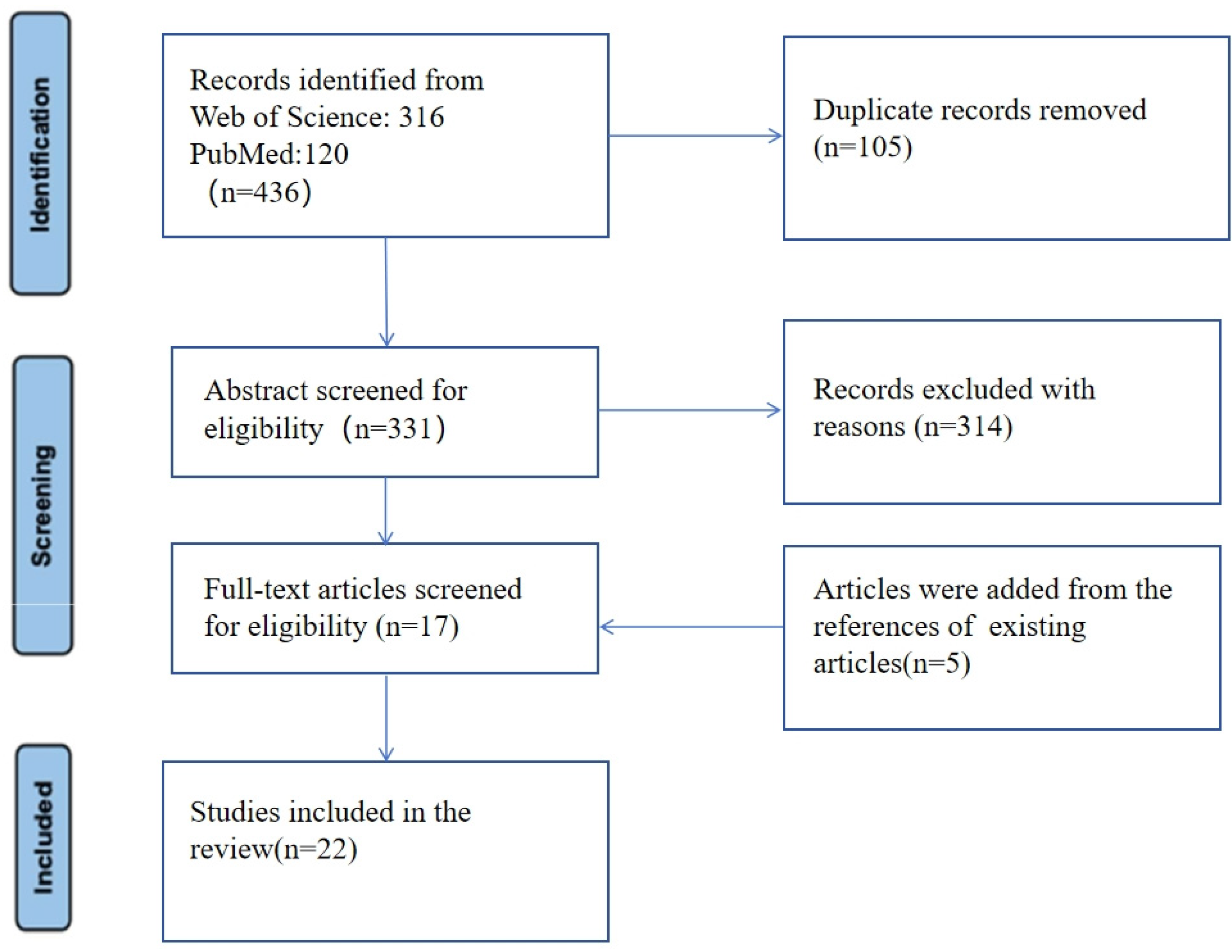
2.2. Search Strategy and Study Selection
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction
2.5. Quality Evaluation
- 1.
- Define the source of information (survey, record review);
- 2.
- List inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications;
- 3.
- Indicate time period used for identifying patients;
- 4.
- Indicate whether or not subjects were consecutive if not population-based;
- 5.
- Indicate whether evaluators of subjective components of study were masked to other aspects of the status of the participants;
- 6.
- Describe any assessments undertaken for quality assurance purposes (e.g., test/retest of primary outcome measurements);
- 7.
- Explain any patient exclusions from analysis;
- 8.
- Describe how confounding was assessed and/or controlled;
- 9.
- If applicable, explain how missing data were handled in the analysis;
- 10.
- Summarize patient response rates and completeness of data collection;
- 11.
- Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained.
2.6. Statistical Analyses
3. Results
3.1. Study Characteristics
3.2. Prevalence of IGD
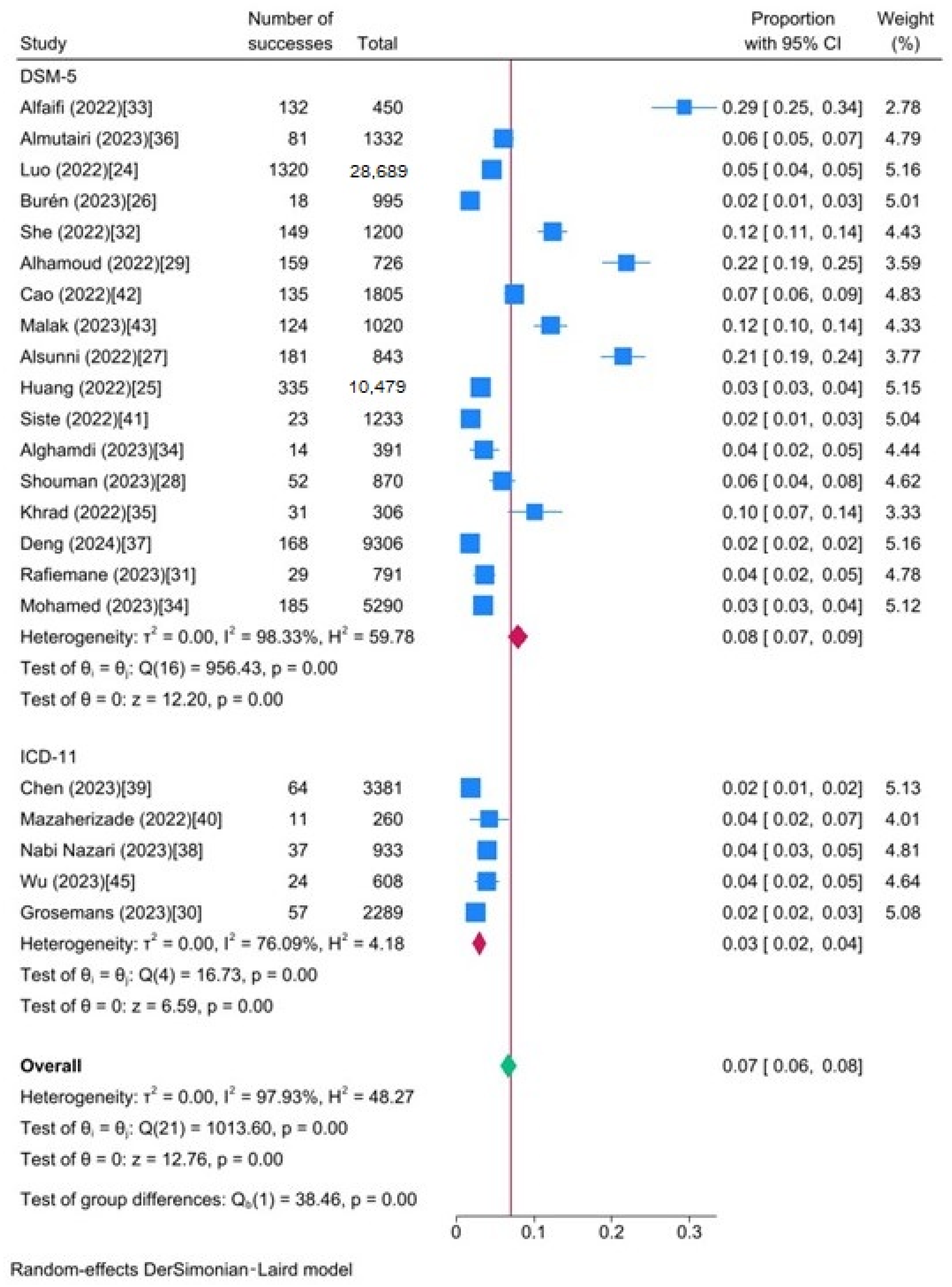
3.3. Subgroup and Meta-Regression Analyses
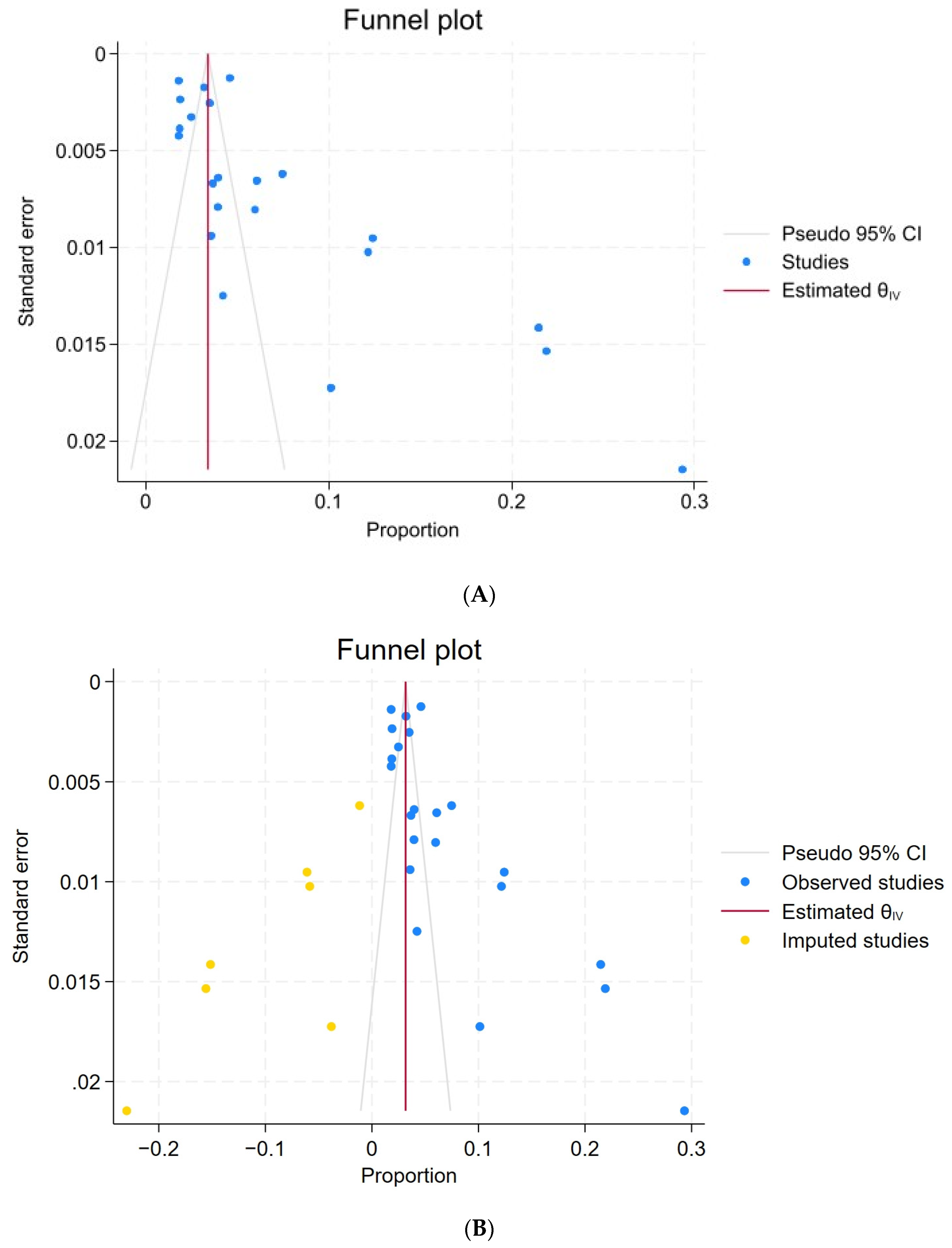
3.4. Publication Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Higuchi, S.; Osaki, Y.; Kinjo, A.; Mihara, S.; Maezono, M.; Kitayuguchi, T.; Matsuzaki, T.; Nakayama, H.; Rumpf, H.-J.; Saunders, J.B. Development and Validation of a Nine-Item Short Screening Test for ICD-11 Gaming Disorder (GAMES Test) and Estimation of the Prevalence in the General Young Population. J. Behav. Addict. 2021, 10, 263–280. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Jeong, J.-E.; Cho, H.; Jung, D.-J.; Kwak, M.; Rho, M.J.; Yu, H.; Kim, D.-J.; Choi, I.Y. Personality Factors Predicting Smartphone Addiction Predisposition: Behavioral Inhibition and Activation Systems, Impulsivity, and Self-Control. PLoS ONE 2016, 11, e0159788. [Google Scholar] [CrossRef]
- Liao, Z.; Huang, Q.; Huang, S.; Tan, L.; Shao, T.; Fang, T.; Chen, X.; Lin, S.; Qi, J.; Cai, Y.; et al. Prevalence of Internet Gaming Disorder and Its Association with Personality Traits and Gaming Characteristics Among Chinese Adolescent Gamers. Front. Psychiatry 2020, 11, 598585. [Google Scholar] [CrossRef] [PubMed]
- Granic, I.; Lobel, A.; Engels, R.C.M.E. The Benefits of Playing Video Games. Am. Psychol. 2014, 69, 66–78. [Google Scholar] [CrossRef]
- Reed, G.M.; First, M.B.; Kogan, C.S.; Hyman, S.E.; Gureje, O.; Gaebel, W.; Maj, M.; Stein, D.J.; Maercker, A.; Tyrer, P.; et al. Innovations and Changes in the ICD-11 Classification of Mental, Behavioural and Neurodevelopmental Disorders. World Psychiatry 2019, 18, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.-Y.; Cheng, C. Psychometric Evaluation and Comparison of Two Gaming Disorder Measures Derived From the DSM-5 and ICD-11 Frameworks. Front. Psychiatry 2020, 11, 577366. [Google Scholar] [CrossRef] [PubMed]
- Tuncturk, M.; Karacetin, G.; Ermis, C.; Ciray, R.O.; Can, M.; Yesilkaya, C.; Atay, A.; Alkas, G.E.; Kasap, D.; Guney, O.; et al. Rate of Overlap between ICD-11 Gaming Disorder and DSM-5 Internet Gaming Disorder along with Turkish Reliability of the Gaming Disorder Scale for Adolescents (GADIS-A). Dubai Med. J. 2023, 6, 291–300. [Google Scholar] [CrossRef]
- Starcevic, V.; Choi, T.Y.; Kim, T.H.; Yoo, S.-K.; Bae, S.; Choi, B.-S.; Han, D.H. Internet Gaming Disorder and Gaming Disorder in the Context of Seeking and Not Seeking Treatment for Video-Gaming. J. Psychiatr. Res. 2020, 129, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.S.; Bhang, S.Y.; Choi, J.S.; Lee, H.K.; Lee, S.Y.; Kweon, Y.-S. Clinical Characteristics of Diagnosis for Internet Gaming Disorder: Comparison of DSM-5 IGD and ICD-11 GD Diagnosis. J. Clin. Med. 2019, 8, 945. [Google Scholar] [CrossRef]
- Pontes, H.M.; Schivinski, B.; Sindermann, C.; Li, M.; Becker, B.; Zhou, M.; Montag, C. Measurement and Conceptualization of Gaming Disorder According to the World Health Organization Framework: The Development of the Gaming Disorder Test. Int. J. Ment. Health Addict. 2021, 19, 508–528. [Google Scholar] [CrossRef]
- Stavropoulos, V.; Baynes, K.L.; O’Farrel, D.L.; Gomez, R.; Mueller, A.; Yucel, M.; Griffiths, M. Inattention and Disordered Gaming: Does Culture Matter? Psychiatr. Q. 2020, 91, 333–348. [Google Scholar] [CrossRef] [PubMed]
- Mihara, S.; Higuchi, S. Cross-sectional and Longitudinal Epidemiological Studies of I Nternet Gaming Disorder: A Systematic Review of the Literature. Psychiatry Clin. Neurosci. 2017, 71, 425–444. [Google Scholar] [CrossRef] [PubMed]
- Stevens, M.W.; Dorstyn, D.; Delfabbro, P.H.; King, D.L. Global Prevalence of Gaming Disorder: A Systematic Review and Meta-Analysis. Aust. N. Z. J. Psychiatry 2021, 55, 553–568. [Google Scholar] [CrossRef] [PubMed]
- Paschke, K.; Austermann, M.I.; Thomasius, R. Assessing ICD-11 Gaming Disorder in Adolescent Gamers: Development and Validation of the Gaming Disorder Scale for Adolescents (GADIS-A). J. Clin. Med. 2020, 9, 993. [Google Scholar] [CrossRef] [PubMed]
- Király, O.; Bőthe, B.; Ramos-Diaz, J.; Rahimi-Movaghar, A.; Lukavska, K.; Hrabec, O.; Miovsky, M.; Billieux, J.; Deleuze, J.; Nuyens, F.; et al. Ten-Item Internet Gaming Disorder Test (IGDT-10): Measurement Invariance and Cross-Cultural Validation across Seven Language-Based Samples. Psychol. Addict. Behav. 2019, 33, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Jo, S.; Yim, H.W.; Lee, H.; Lee, H.C.; Choi, J.; Baek, K. The Internet Game Use-Elicited Symptom Screen Proved to Be a Valid Tool for Adolescents Aged 10–19 Years. Acta Paediatr. 2018, 107, 511–516. [Google Scholar] [CrossRef]
- Stavropoulos, V.; Anderson, E.E.; Beard, C.; Latifi, M.Q.; Kuss, D.; Griffiths, M. A Preliminary Cross-Cultural Study of Hikikomori and Internet Gaming Disorder: The Moderating Effects of Game-Playing Time and Living with Parents. Addict. Behav. Rep. 2019, 9, 100137. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulos, V.; Frost, T.M.J.; Brown, T.; Gill, P.; Footitt, T.A.; Kannis-Dymand, L. Internet Gaming Disorder Behaviours: A Preliminary Exploration of Individualism and Collectivism Profiles. BMC Psychiatry 2021, 21, 262. [Google Scholar] [CrossRef] [PubMed]
- Liao, Z.; Chen, X.; Huang, Q.; Shen, H. Prevalence of Gaming Disorder in East Asia: A Comprehensive Meta-Analysis. J. Behav. Addict. 2022, 11, 727–738. [Google Scholar] [CrossRef]
- Imataka, G.; Sakuta, R.; Maehashi, A.; Yoshihara, S. Current Status of Internet Gaming Disorder (IGD) in Japan: New Lifestyle-Related Disease in Children and Adolescents. J. Clin. Med. 2022, 11, 4566. [Google Scholar] [CrossRef]
- Zeng, X.; Zhang, Y.; Kwong, J.S.W.; Zhang, C.; Li, S.; Sun, F.; Niu, Y.; Du, L. The Methodological Quality Assessment Tools for Preclinical and Clinical Studies, Systematic Review and Meta-analysis, and Clinical Practice Guideline: A Systematic Review. J. Evid. Based Med. 2015, 8, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M. How to Understand and Report Heterogeneity in a Meta-Analysis: The Difference between I-Squared and Prediction Intervals. Integr. Med. Res. 2023, 12, 101014. [Google Scholar] [CrossRef]
- IntHout, J.; Ioannidis, J.P.A.; Rovers, M.M.; Goeman, J.J. Plea for Routinely Presenting Prediction Intervals in Meta-Analysis. BMJ Open 2016, 6, e010247. [Google Scholar] [CrossRef] [PubMed]
- Luo, T.; Wei, D.; Guo, J.; Hu, M.; Chao, X.; Sun, Y.; Sun, Q.; Xiao, S.; Liao, Y. Diagnostic Contribution of the DSM-5 Criteria for Internet Gaming Disorder. Front. Psychiatry 2022, 12, 777397. [Google Scholar] [CrossRef]
- Huang, X.; Shi, H.; Li, H.; Guo, W.; Luo, D.; Xu, J. Differential Effects of Anxiety on Internet Gaming Disorder: A Large-Scale Cross-Sectional Survey. Front. Psychiatry 2022, 12, 802513. [Google Scholar] [CrossRef] [PubMed]
- Burén, J.; Nutley, S.B.; Crisci, G.; Thorell, L.B. Evidence of a Two-Factor Structure for Internet Gaming Disorder and Social Media Disorder: Psychometric Properties of a New Screening Instrument for Adolescents and Adults. J. Psychopathol. Behav. Assess. 2023, 45, 702–715. [Google Scholar] [CrossRef]
- Alsunni, A.; Latif, R. Internet Gaming Disorder and Its Correlates among University Students, Saudi Arabia. J. Fam. Community Med. 2022, 29, 217. [Google Scholar] [CrossRef] [PubMed]
- Shouman, A.; Elez, W.A.; Ibrahim, I.M.A.; Elwasify, M. Internet Gaming Disorder and Psychological Well-Being among University Students in Egypt. BMC Psychol. 2023, 11, 367. [Google Scholar] [CrossRef] [PubMed]
- Alhamoud, M.; Alkhalifah, A.; Althunyan, A.; Mustafa, T.; Alqahtani, H.; Al Awad, F. Internet Gaming Disorder: Its Prevalence and Associated Gaming Behavior, Anxiety, and Depression among High School Male Students, Dammam, Saudi Arabia. J. Fam. Community Med. 2022, 29, 93. [Google Scholar] [CrossRef]
- Grosemans, E.; Dupont, B.; Smits, T.; Bradt, L.; Zaman, B.; De Cock, R. Moving the Margins: Setting up Pathway Research Studying Adolescent Video Gaming, Simulated Gambling and Monetary Engagement. In Proceedings of the DiGRA 2023 Conference: Limits and Margins of Games, Sevilla, Spain, 19–23 June 2023. [Google Scholar]
- Rafiemanesh, H.; Farnam, R.; Sangchooli, A.; Rahimi, J.; Hamzehzadeh, M.; Ghani, K.; Jobehdar, M.M.; Amin-Esmaeili, M.; Shadloo, B.; Demetrovics, Z.; et al. Online Gaming and Internet Gaming Disorder in Iran: Patterns, Motivations, and Correlates. Curr. Psychol. 2023, 42, 13517–13531. [Google Scholar] [CrossRef]
- She, R.; Zhang, Y.; Yang, X. Parental Factors Associated with Internet Gaming Disorder Among First-Year High School Students: Longitudinal Study. JMIR Serious Games 2022, 10, e33806. [Google Scholar] [CrossRef] [PubMed]
- Alfaifi, A.J.; Mahmoud, S.S.; Elmahdy, M.H.; Gosadi, I.M. Prevalence and Factors Associated with Internet Gaming Disorder among Adolescents in Saudi Arabia: A Cross-Sectional Study. Medicine 2022, 101, e29789. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, M.H.; Alghamdi, M.M. Prevalence of Internet Gaming Disorder Among Intermediate and High School Students in Albaha, Saudi Arabia: A Cross-Sectional Study. Cureus 2023, 15, e37115. [Google Scholar] [CrossRef] [PubMed]
- Khrad, H.; Marhoomi, A.; Alkhiri, A.; Alshomrani, A.; Bajabir, D.; Mosli, M. Prevalence of Internet Gaming Disorder among Saudi Arabian University Students: Relationship with Psychological Distress. Heliyon 2022, 8, e12334. [Google Scholar] [CrossRef] [PubMed]
- Almutairi, T.A.; Almutairi, K.S.; Ragab, K.M.; Nourelden, A.Z.; Assar, A.; Matar, S.; Rashid, H.H.; Elsayed, M.; Fathallah, A.H.; Spitzer, M.; et al. Prevalence of Internet Gaming Disorder and Its Association with Psychiatric Comorbidities among a Sample of Adults in Three Arab Countries. Middle East Curr. Psychiatry 2023, 30, 8. [Google Scholar] [CrossRef]
- Deng, X.; Hu, Y.-B.; Liu, C.-Y.; Li, Q.; Yang, N.; Zhang, Q.-Y.; Liu, L.; Qiu, J.-N.; Xu, H.-B.; Xue, L.; et al. Psychological Distress and Aggression among Adolescents with Internet Gaming Disorder Symptoms. Psychiatry Res. 2024, 331, 115624. [Google Scholar] [CrossRef] [PubMed]
- Nazari, N.; Shabbir, M.S.; Sevbitov, A.V.; Sadeghi, M.; Griffiths, M.D. Psychometric Evaluation of the Russian Version of the Gaming Disorder Scale for Adolescents. Curr. Psychol. 2023, 42, 13754–13768. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.-H.; Chang, Y.-L.; Yang, Y.-N.; Yeh, Y.-C.; Ahorsu, D.K.; Adjorlolo, S.; Strong, C.; Hsieh, Y.-P.; Huang, P.-C.; Pontes, H.M.; et al. Psychometric Properties and Development of the Chinese Versions of Gaming Disorder Test (GDT) and Gaming Disorder Scale for Adolescents (GADIS-A). Asian J. Psychiatry 2023, 86, 103638. [Google Scholar] [CrossRef] [PubMed]
- Mazaherizadeh, A.; Taherifar, Z.; Farahani, H. Psychometric Properties of the Farsi Version of the Gaming Disorder Scale for Adolescents (GADIS-A). BMC Psychol. 2022, 10, 195. [Google Scholar] [CrossRef]
- Siste, K.; Hanafi, E.; Sen, L.T.; Damayanti, R.; Beatrice, E.; Ismail, R.I. Psychometric Properties of the Indonesian Ten-Item Internet Gaming Disorder Test and a Latent Class Analysis of Gamer Population among Youths. PLoS ONE 2022, 17, e0269528. [Google Scholar] [CrossRef]
- Cao, H.; Zhang, K.; Ye, D.; Cai, Y.; Cao, B.; Chen, Y.; Hu, T.; Chen, D.; Li, L.; Wu, S.; et al. Relationships Between Job Stress, Psychological Adaptation and Internet Gaming Disorder Among Migrant Factory Workers in China: The Mediation Role of Negative Affective States. Front. Psychol. 2022, 13, 837996. [Google Scholar] [CrossRef] [PubMed]
- Malak, M.Z.; Shuhaiber, A.H.; Alsswey, A.; Tarawneh, A. Social Support as the Mediator for the Relationship between Internet Gaming Disorder and Psychological Problems among University Students. J. Psychiatr. Res. 2023, 164, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, N.F.; Ab Manan, N.; Muhammad Firdaus Chan, M.F.; Rahmatullah, B.; Abd Wahab, R.; Baharudin, S.N.A.; Govindasamy, P.; Abdulla, K. The Prevalence of Internet Gaming Disorders and the Associated Psychosocial Risk Factors among Adolescents in Malaysian Secondary Schools. Clin. Child Psychol. Psychiatry 2023, 28, 1420–1434. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.-Y.; Huang, S.-W.; Chen, J.-S.; Ruckwongpatr, K.; Kukreti, S.; Strong, C.; Pontes, H.M.; Lin, I.-C.; Lin, C.-Y.; Potenza, M.N.; et al. Translation and Validation of the Gaming Disorder Test and Gaming Disorder Scale for Adolescents into Chinese for Taiwanese Young Adults. Compr. Psychiatry 2023, 124, 152396. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Yao, B.; Zhang, H.; Xia, L.; Yu, S.; Peng, X.; Xiang, D.; Liu, Z. Comorbidity of Epilepsy and Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis. J. Neurol. 2023, 270, 4201–4213. [Google Scholar] [CrossRef]
- Kim, H.S.; Son, G.; Roh, E.-B.; Ahn, W.-Y.; Kim, J.; Shin, S.-H.; Chey, J.; Choi, K.-H. Prevalence of Gaming Disorder: A Meta-Analysis. Addict. Behav. 2022, 126, 107183. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.-X.; Wang, J.-Y.; Dong, G.-H. The Prevalence and Possible Risk Factors of Internet Gaming Disorder among Adolescents and Young Adults: Systematic Reviews and Meta-Analyses. J. Psychiatr. Res. 2022, 154, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Kuss, D.J.; Van Rooij, A.J.; Shorter, G.W.; Griffiths, M.D.; Van De Mheen, D. Internet Addiction in Adolescents: Prevalence and Risk Factors. Comput. Hum. Behav. 2013, 29, 1987–1996. [Google Scholar] [CrossRef]
- Yuan, G.; Elhai, J.D.; Hall, B.J. The Influence of Depressive Symptoms and Fear of Missing out on Severity of Problematic Smartphone Use and Internet Gaming Disorder among Chinese Young Adults: A Three-Wave Mediation Model. Addict. Behav. 2021, 112, 106648. [Google Scholar] [CrossRef]
- Teng, Z.; Pontes, H.M.; Nie, Q.; Griffiths, M.D.; Guo, C. Depression and Anxiety Symptoms Associated with Internet Gaming Disorder before and during the COVID-19 Pandemic: A Longitudinal Study. JBA 2021, 10, 169–180. [Google Scholar] [CrossRef]
- Pontes, H.M.; Schivinski, B.; Brzozowska-Woś, M.; Stavropoulos, V. Laxer Clinical Criteria for Gaming Disorder May Hinder Future Efforts to Devise an Efficient Diagnostic Approach: A Tree-Based Model Study. J. Clin. Med. 2019, 8, 1730. [Google Scholar] [CrossRef]
- Dahl, D.; Bergmark, K.H. Persistence in Problematic Internet Use—A Systematic Review and Meta-Analysis. Front. Sociol. 2020, 5, 30. [Google Scholar] [CrossRef]
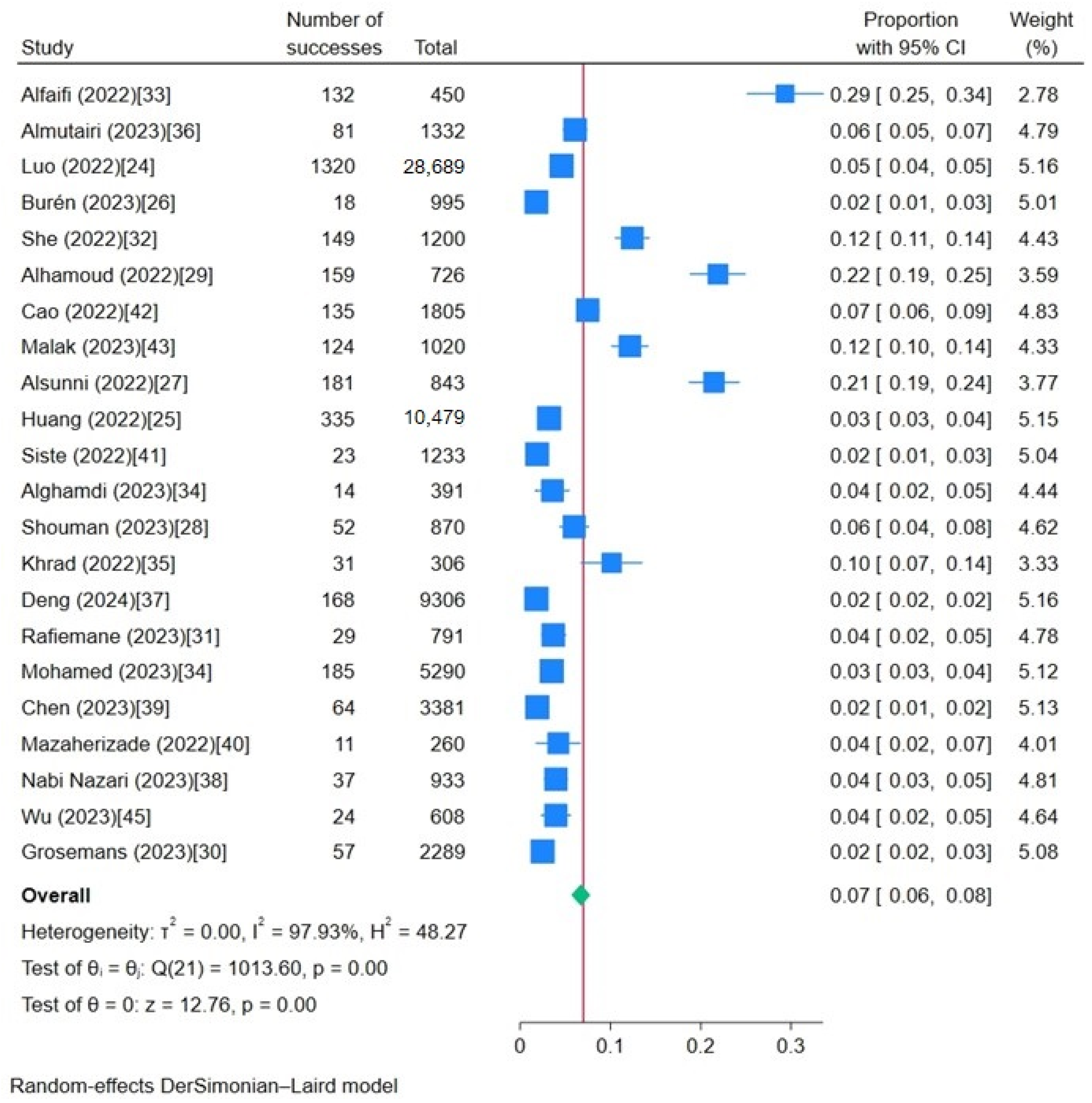

| Study | Study Location | Sample Size | Adolescents /Adult | Scale | DSM-5 /ICD-11 | QS | Prevalence |
|---|---|---|---|---|---|---|---|
| Alfaifi (2022) [33] | Saudi Arabia | 450 | adolescents | IGD-20 | DSM-5 | 7 | 0.293 |
| Almutairi (2023) [36] | Three Arab countries | 1332 | adult | IGD-20 | DSM-5 | 8 | 0.061 |
| Luo (2022) [24] | China | 28,689 | adolescents | IGDS9-SF | DSM-5 | 8 | 0.046 |
| Burén (2023) [26] | Sweden and Italy | 995 | adult | GSMQ-9 | DSM-5 | 7 | 0.018 |
| She (2022) [32] | China | 1200 | adolescents | DSM-5IGD Checklist | DSM-5 | 7 | 0.124 |
| Alhamoud (2022) [29] | Saudi | 726 | adolescent | IGDS9-SF | DSM-5 | 9 | 0.219 |
| Cao (2022) [42] | China | 1805 | adult | DSM-5 IGD Checklist | DSM-5 | 7 | 0.075 |
| Malak (2023) [43] | Jordan | 1020 | adult | IGD-20 | DSM-5 | 9 | 0.122 |
| Alsunni (2022) [27] | Saudi Arabia | 843 | adult | DSM-5 IGD Checklist | DSM-5 | 9 | 0.215 |
| Huang (2022) [25] | China | 10,479 | adolescent | IGDS9-SF | DSM-5 | 10 | 0.032 |
| Siste (2022) [41] | Indonesia | 1233 | adult | IGDT-10 | DSM-5 | 8 | 0.019 |
| Alghamdi (2023) [34] | Saudi Arabia | 391 | adolescent | IGD-20 | DSM-5 | 9 | 0.035 |
| Shouman (2023) [28] | Egypt | 870 | adult | IGDSF-9 | DSM-5 | 9 | 0.060 |
| Khrad (2022) [35] | Saudi Arabia | 306 | adult | IGD-20 | DSM-5 | 8 | 0.101 |
| Deng (2024) [37] | China | 9306 | adolescent | IGD-20 | DSM-5 | 9 | 0.018 |
| Rafiemane (2023) [31] | Iranian | 791 | adult | IGDT-10 | DSM-5 | 9 | 0.037 |
| Mohamed (2023) [34] | Malaysia | 5290 | adolescents | IGDS9-SF | DSM-5 | 10 | 0.035 |
| Chen (2023) [39] | China | 3381 | adult | GADIS-A | ICD-11 | 8 | 0.019 |
| Mazaherizade (2022) [40] | Iran | 260 | adult | GADIS-A | ICD-11 | 8 | 0.042 |
| Nabi Nazari (2023) [38] | Russian | 933 | adolescent | GADIS-A | ICD-11 | 8 | 0.040 |
| Wu (2023) [45] | China | 608 | adult | GADIS-A | ICD-11 | 9 | 0.039 |
| Grosemans (2023) [30] | Belgium | 2289 | adolescent | GADIS-A | ICD-11 | 7 | 0.025 |
| Variable | Subgroup | k | Prevalence | 95% CI | p Significance Test(s) | |
|---|---|---|---|---|---|---|
| Study location | Asia | 19 | 0.075 | 0.063 | 0.086 | p < 0.01 ** |
| European | 3 | 0.026 | 0.016 | 0.037 | ||
| Sample size | >1000 | 11 | 0.049 | 0.038 | 0.06 | p < 0.01 ** |
| <1000 | 11 | 0.097 | 0.062 | 0.132 | ||
| Adolescents/Adult | ||||||
| Adolescents | 10 | 0.071 | 0.056 | 0.085 | p = 0.651 | |
| Adult | 12 | 0.065 | 0.045 | 0.085 | ||
| Diagnostic criteria | DSM-5 | 17 | 0.079 | 0.066 | 0.092 | p < 0.01 ** |
| ICD-11 | 5 | 0.030 | 0.021 | 0.039 | ||
| QS | <9 | 12 | 0.061 | 0.047 | 0.075 | p = 0.115 |
| ≥9 | 10 | 0.079 | 0.061 | 0.097 | ||
| Scale | DSM-5 IGD Checklist | 3 | 0.137 | 0.066 | 0.208 | p < 0.01 ** |
| IGD-20 | 6 | 0.102 | 0.054 | 0.149 | ||
| IGDS9-SF | 4 | 0.066 | 0.048 | 0.083 | ||
| GSMQ-9 | 1 | 0.018 | 0.010 | 0.026 | ||
| IGDT-10 | 2 | 0.027 | 0.009 | 0.044 | ||
| GADIS-A | 5 | 0.030 | 0.021 | 0.039 | ||
| IGDSF-9 | 1 | 0.060 | 0.044 | 0.076 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, R.; Morita, N.; Ogai, Y.; Saito, T.; Zhang, X.; Yang, W.; Yang, F. Meta-Analysis of Internet Gaming Disorder Prevalence: Assessing the Impacts of DSM-5 and ICD-11 Diagnostic Criteria. Int. J. Environ. Res. Public Health 2024, 21, 700. https://doi.org/10.3390/ijerph21060700
Zhou R, Morita N, Ogai Y, Saito T, Zhang X, Yang W, Yang F. Meta-Analysis of Internet Gaming Disorder Prevalence: Assessing the Impacts of DSM-5 and ICD-11 Diagnostic Criteria. International Journal of Environmental Research and Public Health. 2024; 21(6):700. https://doi.org/10.3390/ijerph21060700
Chicago/Turabian StyleZhou, Ruoyu, Nobuaki Morita, Yasukazu Ogai, Tamaki Saito, Xinyue Zhang, Wenjie Yang, and Fan Yang. 2024. "Meta-Analysis of Internet Gaming Disorder Prevalence: Assessing the Impacts of DSM-5 and ICD-11 Diagnostic Criteria" International Journal of Environmental Research and Public Health 21, no. 6: 700. https://doi.org/10.3390/ijerph21060700
APA StyleZhou, R., Morita, N., Ogai, Y., Saito, T., Zhang, X., Yang, W., & Yang, F. (2024). Meta-Analysis of Internet Gaming Disorder Prevalence: Assessing the Impacts of DSM-5 and ICD-11 Diagnostic Criteria. International Journal of Environmental Research and Public Health, 21(6), 700. https://doi.org/10.3390/ijerph21060700






