Resilience in the Face of Cancer: On the Importance of Defining and Studying Resilience as a Dynamic Process of Adaptation
Abstract
:1. Resilience in the Face of Cancer
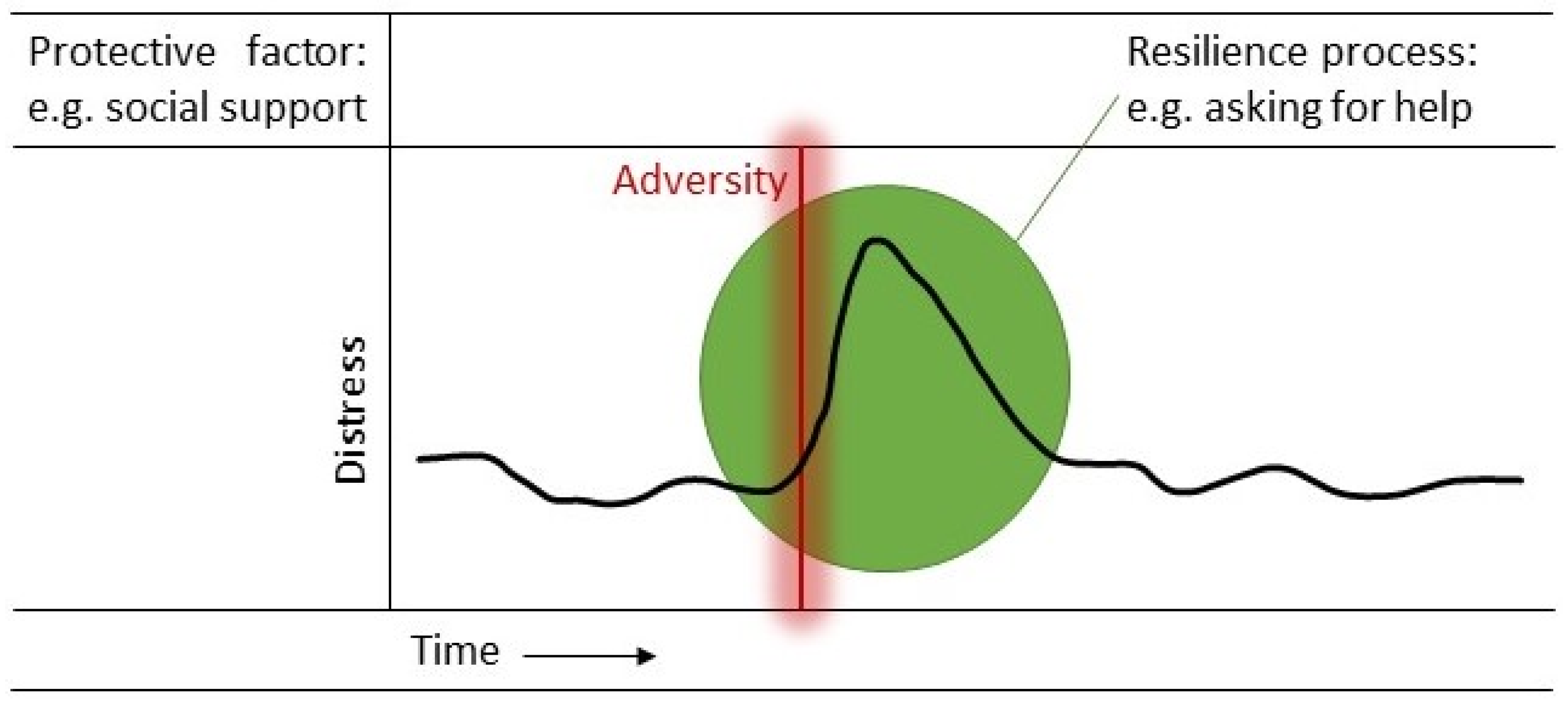
2. The Potential of Resilience Research
3. Defining Resilience as a Dynamic Process
4. Informing Clinical Practice
5. Studying Resilience as a Dynamic Process
5.1. Qualitative Approach
5.2. Longitudinal Designs
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mehnert, A.; Hartung, T.J.; Friedrich, M.; Vehling, S.; Brähler, E.; Härter, M.; Keller, M.; Schulz, H.; Wegscheider, K.; Weis, J.; et al. One in Two Cancer Patients Is Significantly Distressed: Prevalence and Indicators of Distress. Psychooncology 2018, 27, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Carlson, L.E.; Zelinski, E.L.; Toivonen, K.I.; Sundstrom, L.; Jobin, C.T.; Damaskos, P.; Zebrack, B. Prevalence of Psychosocial Distress in Cancer Patients across 55 North American Cancer Centers. J. Psychosoc. Oncol. 2019, 37, 5–21. [Google Scholar] [CrossRef] [PubMed]
- Burton, C.L.; Galatzer-Levy, I.R.; Bonanno, G.A. Treatment Type and Demographic Characteristics as Predictors for Cancer Adjustment: Prospective Trajectories of Depressive Symptoms in a Population Sample. Health Psychol. 2015, 34, 602–609. [Google Scholar] [CrossRef] [PubMed]
- Luthar, S.S.; Cicchetti, D.; Becker, B. The Construct of Resilience: A Critical Evaluation and Guidelines for Future Work. Child. Dev. 2000, 71, 543–562. [Google Scholar] [CrossRef] [PubMed]
- Southwick, S.M.; Bonanno, G.A.; Masten, A.S.; Panter-Brick, C.; Yehuda, R. Resilience Definitions, Theory, and Challenges: Interdisciplinary Perspectives. Eur. J. Psychotraumatol. 2014, 5, 25338. [Google Scholar] [CrossRef] [PubMed]
- Infurna, F.J. What Does Resilience Signify? An Evaluation of Concepts and Directions for Future Research. Gerontology 2020, 66, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Kalisch, R.; Baker, D.G.; Basten, U.; Boks, M.P.; Bonanno, G.A.; Brummelman, E.; Chmitorz, A.; Fernàndez, G.; Fiebach, C.J.; Galatzer-Levy, I.; et al. The Resilience Framework as a Strategy to Combat Stress-Related Disorders. Nat. Hum. Behav. 2017, 1, 784–790. [Google Scholar] [CrossRef]
- Molina, Y.; Yi, J.C.; Martinez-Gutierrez, J.; Reding, K.W.; Yi-Frazier, J.P.; Rosenberg, A.R. Resilience among Patients across the Cancer Continuum: Diverse Perspectives. Clin. J. Oncol. Nurs. 2014, 18, 93–101. [Google Scholar] [CrossRef]
- Eicher, M.; Matzka, M.; Dubey, C.; White, K. Resilience in Adult Cancer Care: An Integrative Literature Review. Oncol. Nurs. Forum 2015, 42, E3–E16. [Google Scholar] [CrossRef]
- Deshields, T.L.; Heiland, M.F.; Kracen, A.C.; Dua, P. Resilience in Adults with Cancer: Development of a Conceptual Model. Psychooncology 2016, 25, 11–18. [Google Scholar] [CrossRef]
- George, T.; Shah, F.; Tiwari, A.; Gutierrez, E.; Ji, J.; Kuchel, G.A.; Cohen, H.J.; Sedrak, M.S. Resilience in Older Adults with Cancer: A Scoping Literature Review. J. Geriatr. Oncol. 2023, 14, 101349. [Google Scholar] [CrossRef] [PubMed]
- Sihvola, S.; Kuosmanen, L.; Kvist, T. Resilience and Related Factors in Colorectal Cancer Patients: A Systematic Review. Eur. J. Oncol. Nurs. 2022, 56, 102079. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-Y.; Lee, H.; Fawcett, J.; Park, J.-H. Resilience in Koreans With Cancer. J. Hosp. Palliat. Nurs. 2019, 21, 358–364. [Google Scholar] [CrossRef]
- Aizpurua-Perez, I.; Perez-Tejada, J. Resilience in Women with Breast Cancer: A Systematic Review. Eur. J. Oncol. Nurs. 2020, 49, 101854. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A. Loss, Trauma, and Human Resilience: Have We Underestimated the Human Capacity to Thrive after Extremely Aversive Events? Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef]
- Henselmans, I.; Helgeson, V.S.; Seltman, H.; de Vries, J.; Sanderman, R.; Ranchor, A.V. Identification and Prediction of Distress Trajectories in the First Year After a Breast Cancer Diagnosis. Health Psychol. 2010, 29, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Lam, W.W.T.; Shing, Y.T.; Bonanno, G.A.; Mancini, A.D.; Fielding, R. Distress Trajectories at the First Year Diagnosis of Breast Cancer in Relation to 6 Years Survivorship. Psychooncology 2012, 21, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Zebrack, B.; Embry, L.; Freyer, D.R.; Aguilar, C.; Cole, S. Profiles of Emotional Distress and Growth among Adolescents and Young Adults with Cancer: A Longitudinal Study. Health Psychol. 2020, 39, 370–380. [Google Scholar] [CrossRef] [PubMed]
- Cordova, M.J.; Riba, M.B.; Spiegel, D. Post-Traumatic Stress Disorder and Cancer. Lancet Psychiatry 2017, 4, 330–338. [Google Scholar] [CrossRef]
- Bremner, J.D. Traumatic Stress: Effects on the Brain. Dialogues Clin. Neurosci. 2006, 8, 445–461. [Google Scholar] [CrossRef]
- Costanzo, E.S.; Stawski, R.S.; Ryff, C.D.; Coe, C.L.; Almeida, D.M. Cancer Survivors’ Responses to Daily Stressors: Implications for Quality of Life. Health Psychol. 2012, 31, 360–370. [Google Scholar] [CrossRef] [PubMed]
- Schultze-Lutter, F.; Schimmelmann, B.G.; Schmidt, S.J. Resilience, Risk, Mental Health and Well-Being: Associations and Conceptual Differences. Eur. Child. Adolesc. Psychiatry 2016, 25, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.S.; Beatty, L.; Koczwara, B. Do Cancer Patients Use the Term Resilience? A Systematic Review of Qualitative Studies. Support. Care Cancer 2018, 27, 43–56. [Google Scholar] [CrossRef]
- Stainton, A.; Chisholm, K.; Kaiser, N.; Rosen, M.; Upthegrove, R.; Ruhrmann, S.; Wood, S.J. Resilience as a Multimodal Dynamic Process. Early Interv. Psychiatry 2019, 13, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Fergus, S.; Zimmerman, M.A. Adolescent Resilience: A Framework for Understanding Healthy Development in the Face of Risk. Annu. Rev. Public Health 2004, 26, 399–419. [Google Scholar] [CrossRef]
- Masten, A.S.; Lucke, C.M.; Nelson, K.M.; Stallworthy, I.C. Resilience in Development and Psychopathology: Multisystem Perspectives. Annu. Rev. Clin. Psychol. 2021, 17, 1–29. [Google Scholar] [CrossRef] [PubMed]
- Ungar, M. Resilience across Cultures. Br. J. Soc. Work 2008, 38, 218–235. [Google Scholar] [CrossRef]
- Lin, C.; Diao, Y.; Dong, Z.; Song, J.; Bao, C. The Effect of Attention and Interpretation Therapy on Psychological Resilience, Cancer-Related Fatigue, and Negative Emotions of Patients after Colon Cancer Surgery. Ann. Palliat. Med. 2020, 9, 3261–3270. [Google Scholar] [CrossRef]
- Rosenberg, A.R.; Zhou, C.; Bradford, M.C.; Salsman, J.M.; Sexton, K.; O’Daffer, A.; Yi-Frazier, J.P. Assessment of the Promoting Resilience in Stress Management Intervention for Adolescent and Young Adult Survivors of Cancer at 2 Years: Secondary Analysis of a Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e2136039. [Google Scholar] [CrossRef]
- Ludolph, P.; Kunzler, A.M.; Stoffers-Winterling, J.; Helmreich, I.; Lieb, K. Interventions to Promote Resilience in Cancer Patients. Dtsch. Arztebl. Int. 2019, 116, 865–872. [Google Scholar] [CrossRef]
- Ang, W.R.; Ang, W.H.D.; Cham, S.Q.G.; de Mel, S.; Chew, H.S.J.; Devi, M.K. Effectiveness of Resilience Interventions among Cancer Patients—A Systematic Review, Meta-Analysis, and Meta-Regression of Randomised Controlled Trials. Eur. J. Oncol. Nurs. 2023, 67, 102446. [Google Scholar] [CrossRef]
- Ding, X.; Zhao, F.; Wang, Q.; Zhu, M.; Kan, H.; Fu, E.; Wei, S.; Li, Z. Effects of Interventions for Enhancing Resilience in Cancer Patients: A Systematic Review and Network Meta-Analysis. Clin. Psychol. Rev. 2024, 108, 102381. [Google Scholar] [CrossRef] [PubMed]
- Pan, S.; Ali, K.; Kahathuduwa, C.; Baronia, R.; Ibrahim, Y. Meta-Analysis of Positive Psychology Interventions on the Treatment of Depression. Cureus 2022, 14, e21933. [Google Scholar] [CrossRef] [PubMed]
- Bolier, L.; Haverman, M.; Westerhof, G.J.; Riper, H.; Smit, F.; Bohlmeijer, E. Positive Psychology Interventions: A Meta-Analysis of Randomized Controlled Studies. BMC Public Health 2013, 13, 119. [Google Scholar] [CrossRef]
- Amonoo, H.L.; El-Jawahri, A.; Deary, E.C.; Traeger, L.N.; Cutler, C.S.; Antin, J.A.; Huffman, J.C.; Lee, S.J. Yin and Yang of Psychological Health in the Cancer Experience: Does Positive Psychology Have a Role? J. Clin. Oncol. 2022, 40, 2402–2407. [Google Scholar] [CrossRef]
- Hodgson, K.D.; Hutchinson, A.D.; Wilson, C.J.; Nettelbeck, T. A Meta-Analysis of the Effects of Chemotherapy on Cognition in Patients with Cancer. Cancer Treat. Rev. 2013, 39, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Windle, G.; Bennett, K.M.; Noyes, J. A Methodological Review of Resilience Measurement Scales. Health Qual. Life Outcomes 2011, 9, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Chmitorz, A.; Neumann, R.J.; Kollmann, B.; Ahrens, K.F.; Öhlschläger, S.; Goldbach, N.; Weichert, D.; Schick, A.; Lutz, B.; Plichta, M.M.; et al. Longitudinal Determination of Resilience in Humans to Identify Mechanisms of Resilience to Modern-Life Stressors: The Longitudinal Resilience Assessment (LORA) Study. Eur. Arch. Psychiatry Clin. Neurosci. 2021, 271, 1035–1051. [Google Scholar] [CrossRef]
- Campo, R.A.; Wu, L.M.; Austin, J.; Valdimarsdottir, H.; Rini, C. Personal Resilience Resources Predict Post-Stem Cell Transplant Cancer Survivors’ Psychological Outcomes through Reductions in Depressive Symptoms and Meaning-Making. J. Psychosoc. Oncol. 2017, 35, 666–687. [Google Scholar] [CrossRef]
- Morin, R.T.; Galatzer-Levy, I.R.; Maccallum, F.; Bonanno, G.A. Do Multiple Health Events Reduce Resilience When Compared with Single Events? Health Psychol. 2017, 36, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Bull, A.; Meyerowitz, B.; Hart, S.; Mosconi, P.; Apolone, G.; Liberati, A. Quality of Life in Women with Recurrent Breast Cancer. Breast Cancer Res. Treat. 1999, 54, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Köhler, N.; Friedrich, M.; Gansera, L.; Holze, S.; Thiel, R.; Roth, S.; Rebmann, U.; Stolzenburg, J.-U.; Truss, M.C.; Fahlenkamp, D.; et al. Psychological Distress and Adjustment to Disease in Patients before and after Radical Prostatectomy. Results of a Prospective Multi-Centre Study. Eur. J. Cancer Care 2014, 23, 795–802. [Google Scholar] [CrossRef]
- Lee, P.W.H.; Kwan, T.T.C.; Kwong, D.L.W.; Sham, J.S.T.; Pow, E.H.N.; McMillan, A.S.; Au, G.K.H. A Prospective Study of the Impact of Nasopharyngeal Cancer and Radiotherapy on the Psychosocial Condition of Chinese Patients. Cancer 2007, 109, 1344–1354. [Google Scholar] [CrossRef] [PubMed]
- Dunn, L.B.; Aouizerat, B.E.; Langford, D.J.; Cooper, B.A.; Dhruva, A.; Cataldo, J.K.; Baggott, C.R.; Merriman, J.D.; Dodd, M.; West, C.; et al. Cytokine Gene Variation Is Associated with Depressive Symptom Trajectories in Oncology Patients and Family Caregivers. Eur. J. Oncol. Nurs. 2013, 17, 346–353. [Google Scholar] [CrossRef]
- Schultebraucks, K.; Choi, K.W.; Galatzer-Levy, I.R.; Bonanno, G.A. Discriminating Heterogeneous Trajectories of Resilience and Depression After Major Life Stressors Using Polygenic Scores. JAMA Psychiatry 2021, 78, 744. [Google Scholar] [CrossRef]
- Smith, J.A.; Flowers, P.; Larkin, M. Interpretative Phenomenological Analysis: Theory, Method and Research; SAGE Publications: London, UK, 2009. [Google Scholar]
- Bootsma, T.I.; Schellekens, M.P.J.; van Woezik, R.A.M.; van der Lee, M.L.; Slatman, J. Experiencing and Responding to Chronic Cancer-Related Fatigue: A Meta-Ethnography of Qualitative Research. Psychooncology 2020, 29, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Almeida, S.N.; Elliott, R.; Silva, E.R.; Sales, C.M.D. Fear of Cancer Recurrence: A Qualitative Systematic Review and Meta-Synthesis of Patients’ Experiences. Clin. Psychol. Rev. 2019, 68, 13–24. [Google Scholar] [CrossRef]
- Bootsma, T.I.; Schellekens, M.P.J.; van Woezik, R.A.M.; Slatman, J.; van der Lee, M.L. Forming New Habits in the Face of Chronic Cancer-Related Fatigue: An Interpretative Phenomenological Study. Support. Care Cancer 2021, 29, 6651–6659. [Google Scholar] [CrossRef] [PubMed]
- Zwanenburg, L.C.; van der Lee, M.L.; Koldenhof, J.J.; Suijkerbuijk, K.P.M.; Schellekens, M.P.J. What Patients with Advanced Cancer Experience as Helpful in Navigating Their Life with a Long-Term Response: A Qualitative Study. Support. Care Cancer 2024, 32, 222. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Diminich, E.D. Positive Adjustment to Adversity–Trajectories of Minimal–Impact Resilience and Emergent Resilience. J. Child Psychol. Psychiatry 2013, 54, 378–401. [Google Scholar] [CrossRef]
- Keyes, C.L.M. Mental Illness and/or Mental Health? Investigating Axioms of the Complete State Model of Health. J. Consult. Clin. Psychol. 2005, 73, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Watson, D.; Tellegen, A.; Wiese, D.; Vidya, J. The Two General Activation Systems of Affect. J. Pers. Soc. Psychol. 1999, 76, 820–838. [Google Scholar] [CrossRef]
- Fredrickson, B.L. The Value of Positive Emotions: The Emerging Science of Positive Psychology Is Coming to Understand Why It’s Good to Feel Good. Am. Sci. 2003, 91, 330–335. [Google Scholar] [CrossRef]
- Keyes, C.L.M.; Dhingra, S.S.; Simoes, E.J. Change in Level of Positive Mental Health as a Predictor of Future Risk of Mental Illness. Am. J. Public Health 2010, 100, 2366–2371. [Google Scholar] [CrossRef] [PubMed]
- Wood, A.M.; Joseph, S. The Absence of Positive Psychological (Eudemonic) Well-Being as a Risk Factor for Depression: A Ten Year Cohort Study. J. Affect. Disord. 2010, 122, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Rusk, R.D.; Waters, L.E. Tracing the Size, Reach, Impact, and Breadth of Positive Psychology. J. Posit. Psychol. 2013, 8, 207–221. [Google Scholar] [CrossRef]
- Kalisch, R.; Köber, G.; Binder, H.; Ahrens, K.F.; Basten, U.; Chmitorz, A.; Choi, K.W.; Fiebach, C.J.; Goldbach, N.; Neumann, R.J.; et al. The Frequent Stressor and Mental Health Monitoring-Paradigm: A Proposal for the Operationalization and Measurement of Resilience and the Identification of Resilience Processes in Longitudinal Observational Studies. Front. Psychol. 2021, 12, 710493. [Google Scholar] [CrossRef]
- Asselmann, E.; Wittchen, H.-U.; Lieb, R.; Beesdo-Baum, K. A 10-Year Prospective-Longitudinal Study of Daily Hassles and Incident Psychopathology among Adolescents and Young Adults: Interactions with Gender, Perceived Coping Efficacy, and Negative Life Events. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 1353–1362. [Google Scholar] [CrossRef]
- Csikszentmihalyi, M.; Larson, R. Validity and Reliability of the Experience-Sampling Method. J. Nerv. Ment. Dis. 1987, 175, 526–536. [Google Scholar] [CrossRef]
- Mestdagh, M.; Dejonckheere, E. Ambulatory Assessment in Psychopathology Research: Current Achievements and Future Ambitions. Curr. Opin. Psychol. 2021, 41, 1–8. [Google Scholar] [CrossRef]
- van Os, J.; Verhagen, S.; Marsman, A.; Peeters, F.; Bak, M.; Marcelis, M.; Drukker, M.; Reininghaus, U.; Jacobs, N.; Lataster, T.; et al. The Experience Sampling Method as an MHealth Tool to Support Self-Monitoring, Self-Insight, and Personalized Health Care in Clinical Practice. Depress. Anxiety 2017, 34, 481–493. [Google Scholar] [CrossRef] [PubMed]
- De Calheiros Velozo, J.; Vaessen, T.; Lafit, G.; Claes, S.; Myin-Germeys, I. Is Daily-Life Stress Reactivity a Measure of Stress Recovery? An Investigation of Laboratory and Daily-Life Stress. Stress Health 2023, 39, 638–650. [Google Scholar] [CrossRef] [PubMed]
- Nahum-Shani, I.; Smith, S.N.; Spring, B.J.; Collins, L.M.; Witkiewitz, K.; Tewari, A.; Murphy, S.A. Just-in-Time Adaptive Interventions (JITAIs) in Mobile Health: Key Components and Design Principles for Ongoing Health Behavior Support. Ann. Behav. Med. 2018, 52, 446–462. [Google Scholar] [CrossRef] [PubMed]
- Kampshoff, C.S.; Verdonck-de Leeuw, I.M.; Oijen, M.G.; Sprangers, M.A.; Buffart, L.M. Ecological Momentary Assessments among Patients with Cancer: A Scoping Review. Eur. J. Cancer Care 2019, 28, e13095. [Google Scholar] [CrossRef] [PubMed]
- Simons, C.J.P.; Hartmann, J.A.; Kramer, I.; Menne-Lothmann, C.; Höhn, P.; van Bemmel, A.L.; Myin-Germeys, I.; Delespaul, P.; van Os, J.; Wichers, M. Effects of Momentary Self-Monitoring on Empowerment in a Randomized Controlled Trial in Patients with Depression. Eur. Psychiatry 2015, 30, 900–906. [Google Scholar] [CrossRef] [PubMed]
- Wichers, M.; Simons, C.J.P.; Kramer, I.M.A.; Hartmann, J.A.; Lothmann, C.; Myin-Germeys, I.; van Bemmel, A.L.; Peeters, F.; Delespaul, P.; van Os, J. Momentary Assessment Technology as a Tool to Help Patients with Depression Help Themselves. Acta Psychiatr. Scand. 2011, 124, 262–272. [Google Scholar] [CrossRef]
- Piot, M.; Mestdagh, M.; Riese, H.; Weermeijer, J.; Brouwer, J.M.A.; Kuppens, P.; Dejonckheere, E.; Bos, F.M. Practitioner and Researcher Perspectives on the Utility of Ecological Momentary Assessment in Mental Health Care: A Survey Study. Internet Interv. 2022, 30, 100575. [Google Scholar] [CrossRef]
| Review | Type of Review (Population) | Study Design | Questionnaire | Resilience Operationalized in Terms of Pre- and Post-Adversity Assessments of Mental Health |
|---|---|---|---|---|
| Eicher et al. (2015) [9] | Integrative literature review (mixed cancer) | Longitudinal (n = 4) Cross-sectional (n = 7) | Resilience (n = 11) | 0/11 |
| Lee et al. (2019) [13] | Scoping review (Korean, mixed cancer) | Pre-post intervention (n = 3) Cross-sectional (n = 14) | Resilience (n = 17) | 0/17 |
| Aizpurua-Perez et al. (2020) [14] | Systematic review (breast cancer) | Longitudinal (n = 1) Cross-sectional (n = 38) | Resilience (n = 39) | 0/39 |
| Sihvola et al. (2022) [12] | Systematic review (colorectal cancer) | RCT (n = 1) cross-sectional (n = 10) | Resilience (n = 11) | 0/11 |
| George et al. (2023) [11] * | Scoping literature review (mixed cancer) | Longitudinal (n = 17) (R)CT ** (n = 4) Pre-post intervention (n = 2) Qualitative (n = 3) | Resilience (n = 5) Mental health (n = 21) | 7/26 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schellekens, M.P.J.; Zwanenburg, L.C.; van der Lee, M.L. Resilience in the Face of Cancer: On the Importance of Defining and Studying Resilience as a Dynamic Process of Adaptation. Curr. Oncol. 2024, 31, 4003-4014. https://doi.org/10.3390/curroncol31070297
Schellekens MPJ, Zwanenburg LC, van der Lee ML. Resilience in the Face of Cancer: On the Importance of Defining and Studying Resilience as a Dynamic Process of Adaptation. Current Oncology. 2024; 31(7):4003-4014. https://doi.org/10.3390/curroncol31070297
Chicago/Turabian StyleSchellekens, Melanie P. J., Laura C. Zwanenburg, and Marije L. van der Lee. 2024. "Resilience in the Face of Cancer: On the Importance of Defining and Studying Resilience as a Dynamic Process of Adaptation" Current Oncology 31, no. 7: 4003-4014. https://doi.org/10.3390/curroncol31070297






