Diagnostic Limitations and Aspects of the Lumbosacral Transitional Vertebrae (LSTV)
Abstract
:1. Introduction
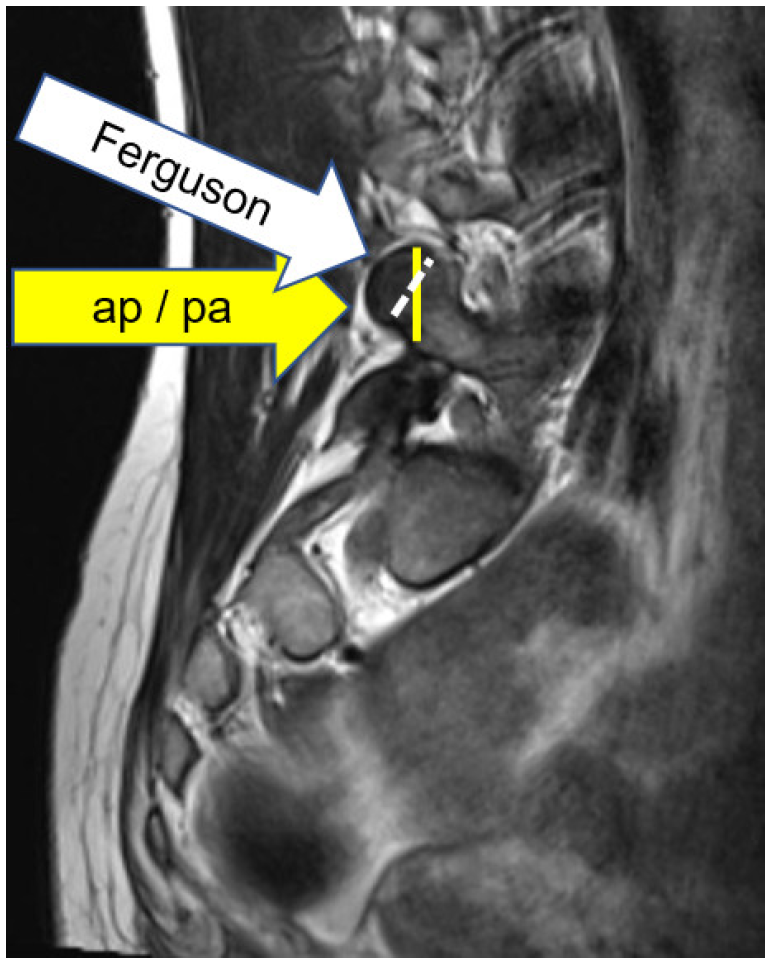
2. Materials and Methods
3. Results
4. Discussion
- Castellvi type I:
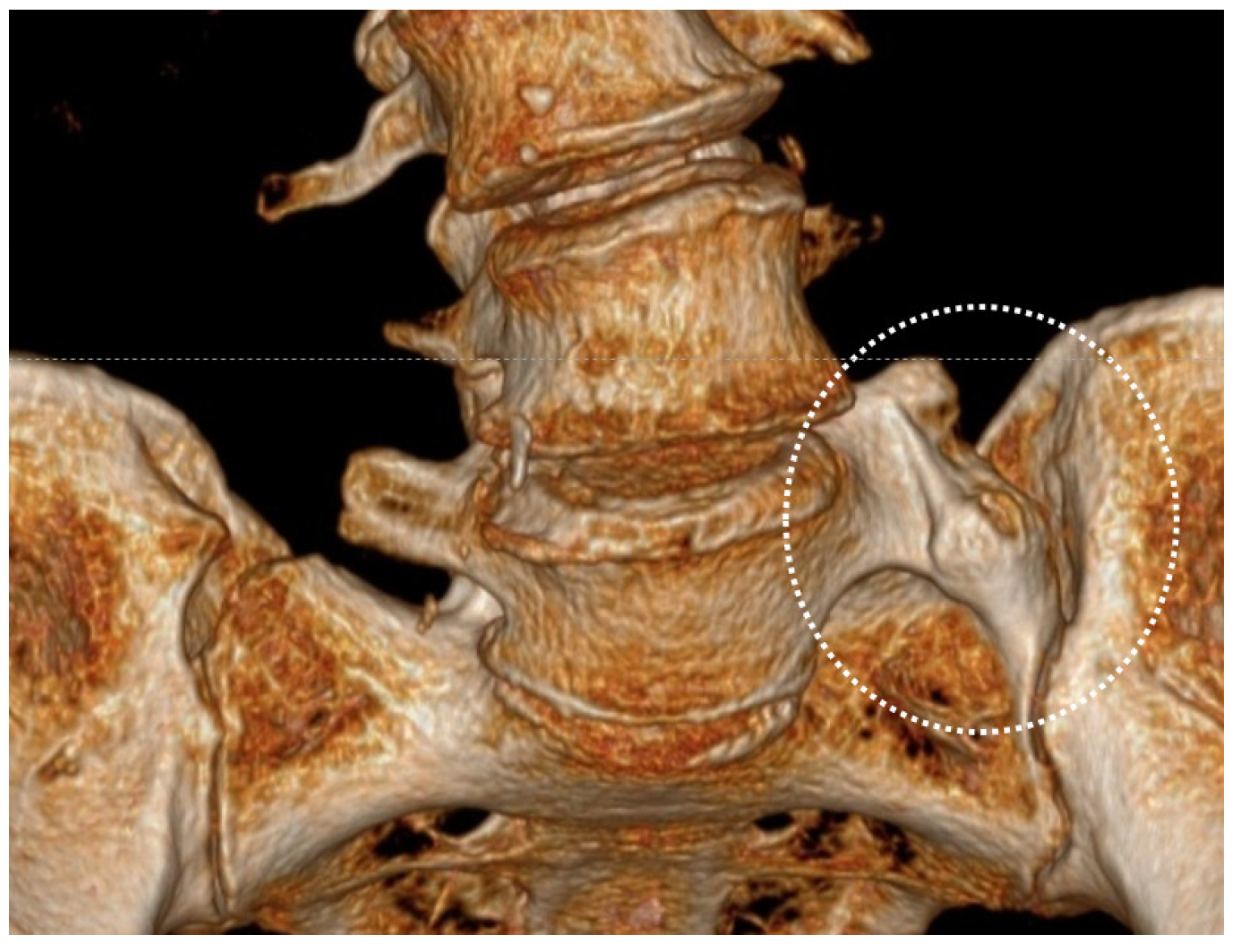
- LSTV type II:
- LSTV type III:
- LSTV type IV:
- Disc degeneration:
- Disc model:
- Limitation of own data:
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| LSTV | Lumbo Sacral Transitional Vertebra |
| IVD | InterVertebral Disc |
| MRI | Magnetic resonance imaging |
| FEM | Finite Element Model |
| IDR | Intervertebral Disc Regeneration |
| LBP | Low-Back Pain |
References
- Apazidis, A.; Ricart, P.A.; Diefenbach, C.M.; Spivak, J.M. The prevalence of transitional vertebrae in the lumbar spine. Spine J. 2011, 11, 858–862. [Google Scholar] [CrossRef] [PubMed]
- Tang, M.; Yang, X.F.; Yang, S.W.; Han, P.; Ma, Y.M.; Yu, H.; Zhu, B. Lumbosacral transitional vertebra in a population-based study of 5860 individuals: Prevalence and relationship to low back pain. Eur. J. Radiol. 2014, 83, 1679–1682. [Google Scholar] [CrossRef] [PubMed]
- O’Driscoll, C.M.; Irwin, A.; Saifuddin, A. Variations in morphology of the lumbosacral junction on sagittal MRI: Correlation with plain radiography. Skelet. Radiol. 1996, 25, 225–230. [Google Scholar] [CrossRef]
- Farshad, M.; Aichmair, A.; Hughes, A.P.; Herzog, R.J.; Farshad-Amacker, N.A. A reliable measurement for identifying a lumbosacral transitional vertebra with a solid bony bridge on a single-slice midsagittal MRI or plain lateral radiograph. Bone Jt. J. 2013, 95, 1533–1537. [Google Scholar] [CrossRef]
- Okamoto, M.; Hasegawa, K.; Hatsushikano, S.; Kobayashi, K.; Sakamoto, M.; Ohashi, M.; Watanabe, K. Influence of lumbosacral transitional vertebrae on spinopelvic parameters using biplanar slot scanning full body stereoradiography-analysis of 291 healthy volunteers. J. Orthop. Sci. 2022, 27, 751–759. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Du, L.; Liu, X.; Wang, Q.; Zhao, J.; Lv, Y.; Yang, H. Quantitative measurements at the lumbosacral junction are more reliable parameters for identifying and numbering lumbosacral transitional vertebrae. Eur. Radiol. 2022, 32, 5650–5658. [Google Scholar] [CrossRef]
- Konin, G.P.; Walz, D.M. Lumbosacral transitional vertebrae: Classification, imaging findings, and clinical relevance. Am. J. Neuroradiol. 2010, 31, 1778–1786. [Google Scholar] [CrossRef] [Green Version]
- Hughes, R.J.; Saifuddin, A. Numbering of lumbosacral transitional vertebrae on MRI: Role of the iliolumbar ligaments. Am. J. Roentgenol. 2006, 187, W59–W65. [Google Scholar] [CrossRef]
- Farshad-Amacker, N.A.; Lurie, B.; Herzog, R.J.; Farshad, M. Is the iliolumbar ligament a reliable identifier of the L5 vertebra in lumbosacral transitional anomalies? Eur. Radiol. 2014, 24, 2623–2630. [Google Scholar] [CrossRef]
- McGrath, K.A.; Lee, J.; Thompson, N.R.; Kanasz, J.; Steinmetz, M.P. Identifying the relationship between lumbar sacralization and adjacent ligamentous anatomy in patients with Bertolotti syndrome and healthy controls. J. Neurosurg. Spine 2022, 37, 200–207. [Google Scholar] [CrossRef]
- Zhang, B.; Wang, L.; Wang, H.; Guo, Q.; Lu, X.; Chen, D. Lumbosacral Transitional Vertebra: Possible Role in the Pathogenesis of Adolescent Lumbar Disc Herniation. World Neurosurg. 2017, 107, 983–989. [Google Scholar] [CrossRef] [PubMed]
- Ashour, A.; Hassan, A.; Aly, M.; Nafady, M.A. Prevalence of Bertolotti’s Syndrome in Lumbosacral Surgery Procedures. Cureus 2022, 14, e26341. [Google Scholar] [CrossRef] [PubMed]
- Kanematsu, R.; Hanakita, J.; Takahashi, T.; Minami, M.; Tomita, Y.; Honda, F. Extraforaminal entrapment of the fifth lumbar spinal nerve by nearthrosis in patients with lumbosacral transitional vertebrae. Eur. Spine J. 2020, 29, 2215–2221. [Google Scholar] [CrossRef] [PubMed]
- Hinterdorfer, P.; Parsaei, B.; Stieglbauer, K.; Sonnberger, M.; Fischer, J.; Wurm, G. Segmental innervation in lumbosacral transitional vertebrae (LSTV): A comparative clinical and intraoperative EMG study. J. Neurol. Neurosurg. Psychiatry 2010, 81, 734–741. [Google Scholar] [CrossRef]
- Abbas, J.; Peled, N.; Hershkovitz, I.; Hamoud, K. Is Lumbosacral Transitional Vertebra Associated with Degenerative Lumbar Spinal Stenosis? Biomed. Res. Int. 2019, 10, 2019. [Google Scholar] [CrossRef] [Green Version]
- Mahato, N.K. Trabecular bone structure in lumbosacral transitional vertebrae: Distribution and densities across sagittal vertebral body segments. Spine J. 2013, 13, 932–937. [Google Scholar] [CrossRef]
- Golubovsky, J.L.; Colbrunn, R.W.; Klatte, R.S.; Nagle, T.F.; Briskin, I.N.; Chakravarthy, V.B.; Gillespie, C.M.; Reith, J.D.; Jasty, N.; Benzel, E.C.; et al. Development of a novel in vitro cadaveric model for analysis of biomechanics and surgical treatment of Bertolotti syndrome. Spine J. 2020, 20, 638–656. [Google Scholar] [CrossRef]
- Bertolotti, M. Contributo alla conoscenza dei vizi di differenziazione regionale del rachide con speciale riguardo all assimilazione sacrale della v. lombare. Radiol. Med. 1917, 4, 113–144. [Google Scholar]
- Quinlan, J.F.; Duke, D.; Eustace, S. Bertolotti’s syndrome: A cause of back pain in young people. J. Bone Jt. Surg. Br. 2006, 88, 1183–1186. [Google Scholar] [CrossRef]
- Apaydin, M.; Uluc, M.E.; Sezgin, G. Lumbosacral transitional vertebra in the young men population with low back pain: Anatomical considerations and degenerations (transitional vertebra types in the young men population with low back pain). Radiol. Med. 2019, 124, 375–381. [Google Scholar] [CrossRef]
- McGrath, K.; Schmidt, E.; Rabah, N.; Abubakr, M.; Steinmetz, M. Clinical assessment and management of Bertolotti Syndrome: A review of the literature. Spine J. 2021, 21, 1286–1296. [Google Scholar] [CrossRef] [PubMed]
- Ulger, F.E.B.; Illeez, O.G. The Effect of Lumbosacral Transitional Vertebrae (LSTV) on Paraspinal Muscle Volume in Patients with Low Back Pain. Acad. Radiol. 2020, 27, 944–950. [Google Scholar] [CrossRef] [PubMed]
- Becker, L.; Ziegeler, K.; Diekhoff, T.; Palmowski, Y.; Pumberger, M.; Schömig, F. Musculature adaption in patients with lumbosacral transitional vertebrae: A matched-pair analysis of 46 patients. Skelet. Radiol. 2021, 50, 1697–1704. [Google Scholar] [CrossRef] [PubMed]
- Hanhivaara, J.; Määttä, J.H.; Karppinen, J.; Niinimäki, J.; Nevalainen, M.T. The Association of Lumbosacral Transitional Vertebrae with Low Back Pain and Lumbar Degenerative Findings in MRI: A Large Cohort Study. Spine 2022, 47, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Mahato, N.K. Lumbosacral transitional vertebrae: Variations in low back structure, biomechanics, and stress patterns. J. Chiropr. Med. 2012, 11, 134–135. [Google Scholar] [CrossRef] [Green Version]
- Morimoto, M.; Sugiura, K.; Higashino, K.; Manabe, H.; Tezuka, F.; Wada, K.; Yamashita, K.; Takao, S.; Sairyo, K. Association of spinal anomalies with spondylolysis and spina bifida occulta. Eur. Spine J. 2022, 31, 858–864. [Google Scholar] [CrossRef]
- Sharma, A.; Kumar, A.; Kapila, A. Co-existence of spina bifida occulta and lumbosacral transitional vertebra in patients presenting with lower back pain. Reumatologia 2022, 60, 70–75. [Google Scholar] [CrossRef]
- Fidan, F.; Çay, N.; Asiltürk, M.; Veizi, E. The incidence of congenital lumbosacral malformations in young male Turkish military school candidates population. J. Orthop. Sci. 2021, 11, S0949–S2658. [Google Scholar] [CrossRef]
- Vinha, A.; Bártolo, J.; Lemos, C.; Cordeiro, F.; Rodrigues-Pinto, R. Lumbosacral transitional vertebrae: Prevalence in a southern European population and its association with low back pain. Eur. Spine J. 2022, 1–7. [Google Scholar] [CrossRef]
- Garg, B.; Mehta, N.; Goyal, A.; Rangaswamy, N.; Upadhayay, A. Variations in the Number of Thoracic and Lumbar Vertebrae in Patients With Adolescent Idiopathic Scoliosis: A Retrospective, Observational Study. Int. J. Spine Surg. 2021, 15, 359–367. [Google Scholar] [CrossRef]
- Becker, L.; Schönnagel, L.; Mihalache, T.V.; Haffer, H.; Schömig, F.; Schmidt, H.; Pumberger, M. Lumbosacral transitional vertebrae alter the distribution of lumbar mobility-Preliminary results of a radiographic evaluation. PLoS ONE 2022, 17, e0274581. [Google Scholar] [CrossRef] [PubMed]
- Becker, L.; Taheri, N.; Haffer, H.; Muellner, M.; Hipfl, C.; Ziegeler, K.; Diekhoff, T.; Pumberger, M. Lumbosacral Transitional Vertebrae Influence on Acetabular Orientation and Pelvic Tilt. J. Clin. Med. 2022, 11, 5153. [Google Scholar] [CrossRef]
- McGrath, K.A.; Thompson, N.R.; Fisher, E.; Kanasz, J.; Golubovsky, J.L.; Steinmetz, M.P. Quality-of-life and postoperative satisfaction following pseudoarthrectomy in patients with Bertolotti syndrome. Spine J. 2022, 22, 1292–1300. [Google Scholar] [CrossRef] [PubMed]
- Becker, L.; Amini, D.A.; Ziegeler, K.; Muellner, M.; Diekhoff, T.; Hughes, A.P.; Pumberger, M. Approach-related anatomical differences in patients with lumbo-sacral transitional vertebrae undergoing lumbar fusion surgery at level L4/5. Arch. Orthop. Trauma Surg. 2022, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.M.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Hanhivaara, J.; Määttä, J.H.; Niinimäki, J.; Nevalainen, M.T. Lumbosacral transitional vertebrae are associated with lumbar degeneration: Retrospective evaluation of 3855 consecutive abdominal CT scans. Eur. Radiol. 2020, 30, 3409–3416. [Google Scholar] [CrossRef] [Green Version]
- Griffith, J.F.; Xiao, F.; Hilkens, A.; Han, I.; Griffith, Y.; Chi, J.; Leung, S. Increased vertebral body area, disc and facet joint degeneration throughout the lumbar spine in patients with lumbosacral transitional vertebrae. Eur. Radiol. 2022, 32, 6238–6246. [Google Scholar] [CrossRef]
- Guerrero, J.; Häckel, S.; Croft, A.S.; Hoppe, S.; Albers, C.E.; Gantenbein, B. The nucleus pulposus microenvironment in the intervertebral disc: The fountain of youth? Eur. Cell. Mater. 2021, 41, 707–738. [Google Scholar] [CrossRef]
- Bermudez-Lekerika, P.; Crump, K.B.; Tseranidou, S.; Nüesch, A.; Kanelis, E.; Alminnawi, A.; Baumgartner, L.; Muñoz-Moya, E.; Compte, R.; Gualdi, F.; et al. Immuno-Modulatory Effects of Intervertebral Disc Cells. Front. Cell Dev. Biol. 2022, 10, 924692. [Google Scholar] [CrossRef]
- Cheng, L.; Jiang, C.; Huang, J.; Jin, J.; Guan, M.; Wang, Y. Lumbosacral Transitional Vertebra Contributed to Lumbar Spine Degeneration: An MR Study of Clinical Patients. J. Clin. Med. 2022, 11, 2339. [Google Scholar] [CrossRef]



| (1) Introduction: Presentation of current literature of LSTV: Prevalence, diagnosis, Castellvi classification, LBP, Bertolotti syndrome, scoliosis, etc. Flow diagram to Disc: PubMed (12 October 2022): | ||||||||
| LSTV n = 150 | ||||||||
| Prevalence n = 50 | ||||||||
| Castellvi classification n = 51 | ||||||||
| LBP n = 59 | ||||||||
| Bertolotti syndrome n = 19 | ||||||||
| Disc n = 45 | ||||||||
| Scoliosis n = 16 | ||||||||
| Surgery n = 80 | ||||||||
(2) Materials and Methods:
| ||||||||
| (3) Results: Results of own LSTV-data (2014–2021) (gender, age, Castellvi classification, total number of vertebral bodies, low-back pain, scoliosis, concomitant pathologies, family history). | ||||||||
| Castellvi classification | ||||||||
| total number of vertebral bodies | ||||||||
| low-back pain (Bertolotti syndrome) | ||||||||
| scoliosis | ||||||||
| gender | ||||||||
| age | ||||||||
| concomitant pathologies | ||||||||
| family history | ||||||||
(4) Discussion of the literature and own data of LSTV:
| ||||||||
| (5) Summary: LSTV as an experimental model for intervertebral disc degeneration/regeneration | ||||||||
| Spine patients (all) | n-1482 | |||
| LSTV (all) ♀ n-83 ♂ n-32 | n-115 | |||
| Castellvi | IIA | n-55 | IIB | n-24 |
| IIIA | n-20 | IIIB | n-10 | |
| IV | n-6 | |||
| Lumbalgia (all) ♀ n-46 ♂ n-18 | n-64 | |||
| Castellvi | IIA | n-30 | IIB | n-13 |
| IIIA | n-11 | IIIB | n-5 | |
| IV | n-5 | |||
| Scoliosis (all) ♀ n-58 ♂ n-14 | n-72 | |||
| Castellvi | IIA | n-42 | IIB | n-11 |
| IIIA | n-14 | IIIB | n-3 | |
| IV | n-2 | |||
| Own Data Type II–IV | Literature Type I–IV | ||
|---|---|---|---|
| LSTV total | 7.8% | 20.9% (+14.7% Type I) | [1] |
| 15.8% | [2] | ||
| 10.7% (+21.3% Type I) | [20] | ||
| 21.1% | [24] | ||
| 12.9% | [28] | ||
| 9.3% (+19.7% Type I) | [36] | ||
| 31% | [37] | ||
| LBP total | 4.3% | 4.6% | [19] |
| Bertolotti syndrome | 55.7% | 40.0% | [13] |
| 30% | [11] | ||
| 24.9% | [29] | ||
| Scoliosis and LSTV | 62.6% | 18.2% | [30] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Landauer, F.; Trieb, K. Diagnostic Limitations and Aspects of the Lumbosacral Transitional Vertebrae (LSTV). Appl. Sci. 2022, 12, 10830. https://doi.org/10.3390/app122110830
Landauer F, Trieb K. Diagnostic Limitations and Aspects of the Lumbosacral Transitional Vertebrae (LSTV). Applied Sciences. 2022; 12(21):10830. https://doi.org/10.3390/app122110830
Chicago/Turabian StyleLandauer, Franz, and Klemens Trieb. 2022. "Diagnostic Limitations and Aspects of the Lumbosacral Transitional Vertebrae (LSTV)" Applied Sciences 12, no. 21: 10830. https://doi.org/10.3390/app122110830
APA StyleLandauer, F., & Trieb, K. (2022). Diagnostic Limitations and Aspects of the Lumbosacral Transitional Vertebrae (LSTV). Applied Sciences, 12(21), 10830. https://doi.org/10.3390/app122110830






