The Economics of a Bed Shortage: Certificate-of-Need Regulation and Hospital Bed Utilization during the COVID-19 Pandemic
Abstract
:1. Introduction
Certain patients deemed less likely to survive may not get a bed in the intensive care unit. Nurses may be asked to treat many more patients than is normally considered safe. Patients may have to be discharged from the hospital before they would normally go home, and some patients who would usually be admitted for hospital care might have to be denied(Stone 2021).
2. Materials and Methods
2.1. Hospital Bed Utilization
2.2. Certificate-of-Need
2.3. Hospital Bed CON
suspended to the extent necessary to allow hospitals that would otherwise be subject to certificate of need requirements to temporarily increase their number of licensed hospital beds at any location or temporarily establish hospital and diagnostic services at any location, if necessary for the treatment of COVID-19 patient(Lee 2020).
2.4. Regressions
3. Results
4. Discussion
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
| 1 | For an overview, see Mitchell et al. (2021). |
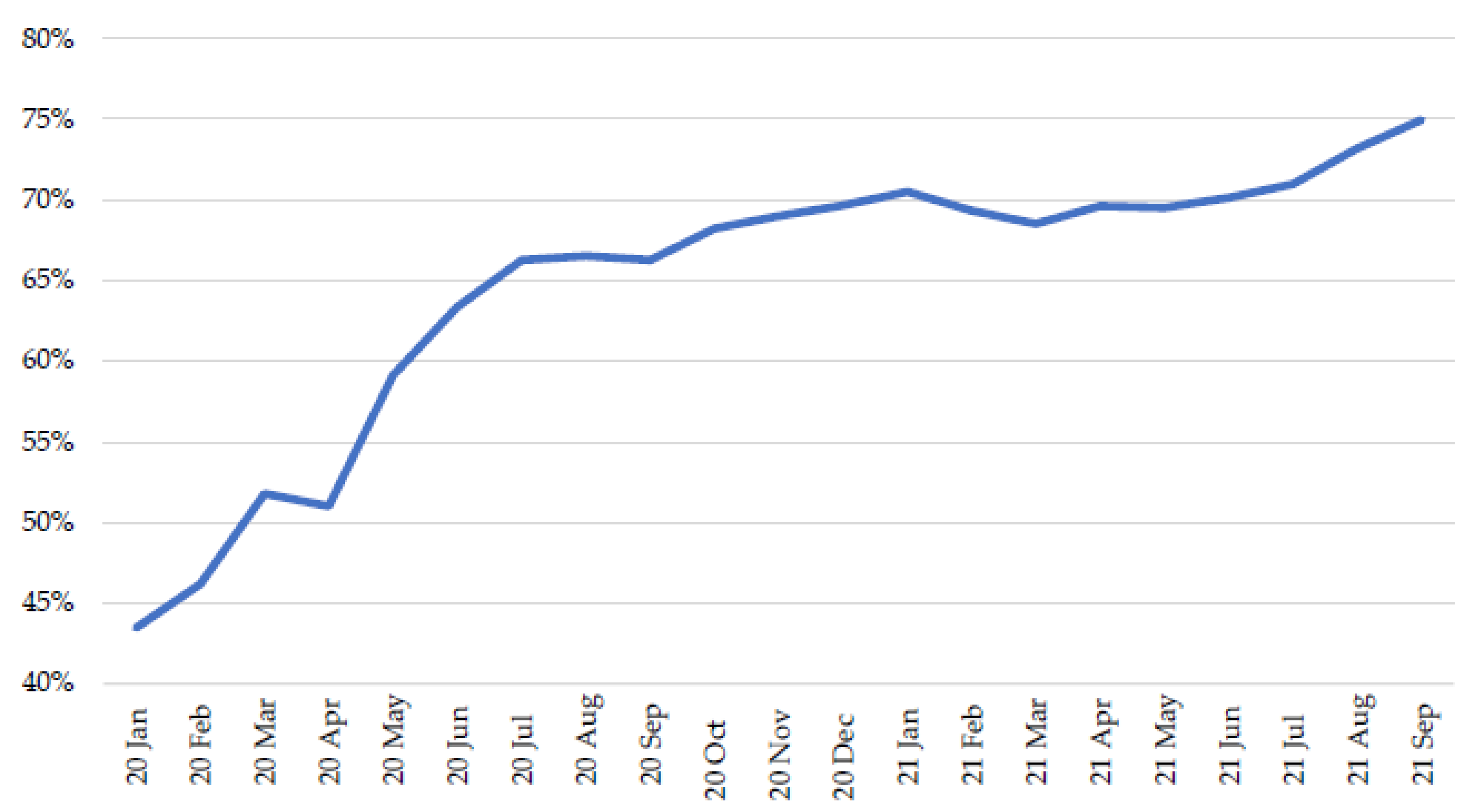
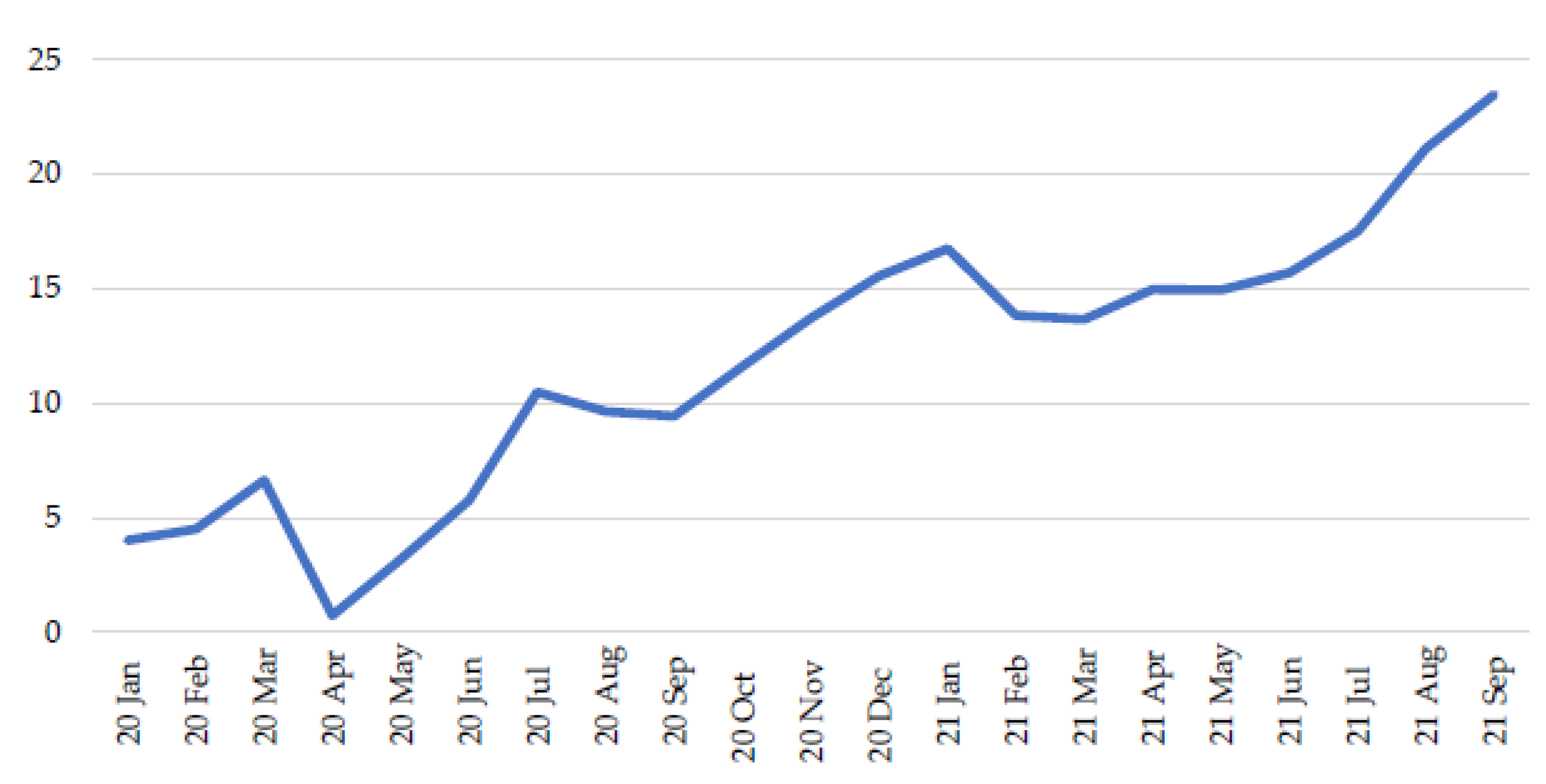
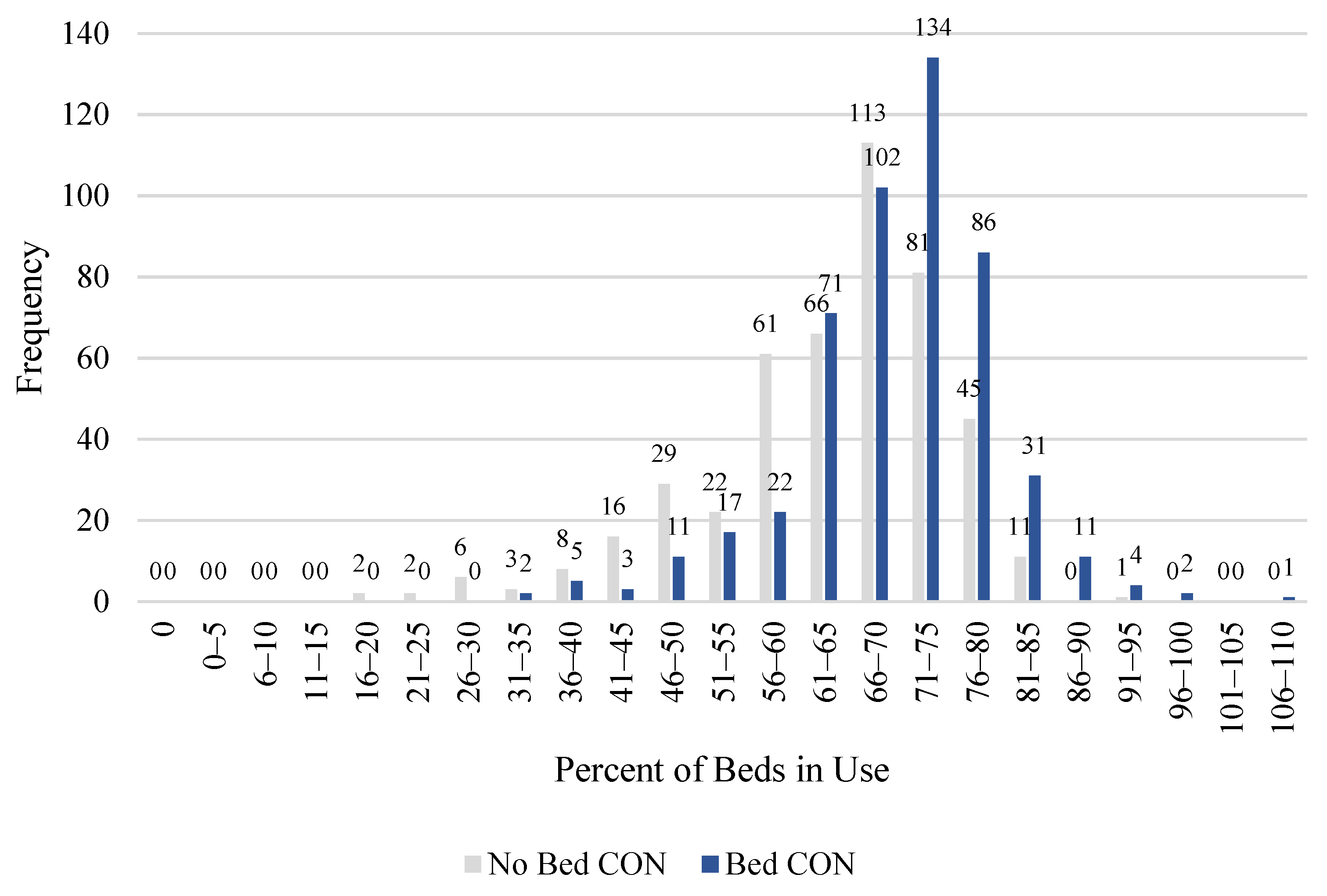
| 2 | In this figure, the data are national; they are not averaged across states. In other words, it shows the total number of occupied beds in the country, divided by the total number of beds in the country. In subsequent analysis, however, we use state-aggregated data. |
| 3 | Owing to missing data in the first two months of the pandemic, we have 968 observations, one for each state-month combination. |
| 4 | A state or a hospital’s bed utilization rate can exceed 100 percent if it has more patients than beds to accommodate them. |
| 5 | (National Health Planning and Resources Development Act of 1974 1975) Due to repeated postponement, this was a threat that never materialized (Conover and Bailey 2020, p. 2). |
| 6 | Mark Botti of the Antitrust Division of the Department of Justice noted the implications of this change in testimony before the Georgia State Assembly in 2007: “In addition to the fact that CON laws have been ineffective in serving their original purpose, CON laws should be reexamined because the reimbursement methodologies that may in theory have justified them initially have changed significantly since the 1970s. The federal government no longer reimburses on a cost-plus basis” (Botti 2007). |
| 7 | One of us is preparing a survey of the CON literature and has identified over 70 peer reviewed empirical studies. |
| 8 | Our data are derived from Mitchell et al. (2021). |
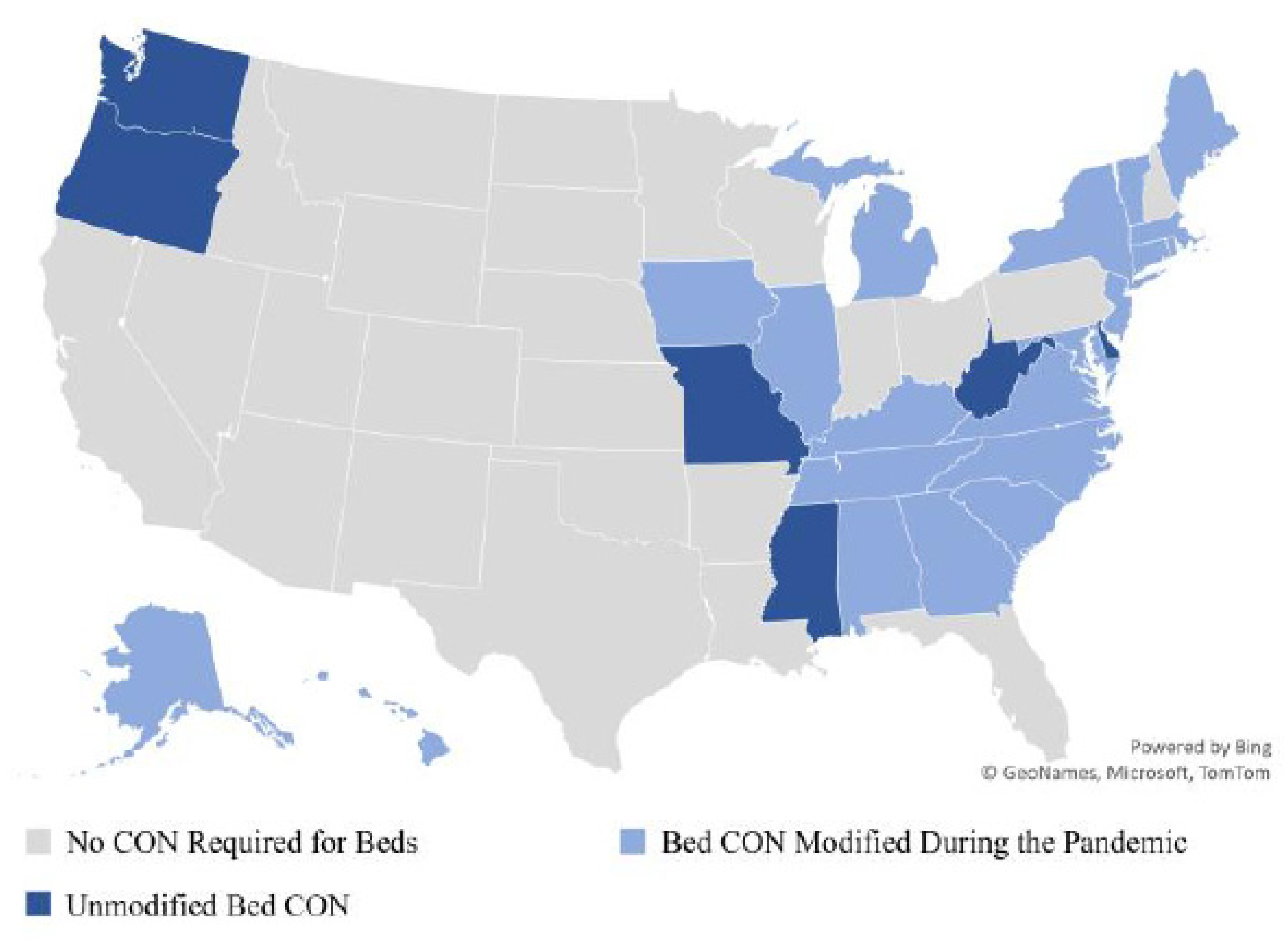
| 9 | Other states relaxed their CON laws, but 20 of these modifications affected bed CON requirements. To obtain this data, we began with initial research conducted by Angela C. Erikson of the Pacific Legal Foundation (Erickson 2021). We then updated this information by reviewing state executive orders and by contacting states’ CON regulatory authorities for comment. In instances where we were unable to contact a state’s CON regulatory authority, we relied on textual examination of a state’s executive orders and emergency declarations to obtain the status and substance of the CON relaxation. If a relaxation occurred (ended) in the first 15 days of the month, then it is coded to have occurred (ended) in that month. If the relaxation occurred (ended) after the first 15 days of a month, then it is coded to have occurred (ended) in the following month. |
| 10 | We obtained Percent Black and Percent Hispanic data from the Census Bureau. We obtained per capita income data from the Bureau of Economic Analysis. The percent of adults (age 18 or older) with diabetes was obtained from the Centers for Disease Control and Prevention. Additionally, the number of new cases was obtained from the Healthdata.gov website maintained by the DHS and converted to per capita figures using state population totals obtained from the Census (American Community Survey n.d.; US Department of Commerce, B. E. A. n.d.; National Diabetes Statistics Report 2020; United States COVID-19 Cases and Deaths by State over Time n.d.). |
References
- American Community Survey—ACS. n.d. The United States Census Bureau. Available online: https://www.census.gov/programs-surveys/acs (accessed on 8 October 2021).
- Bailey, James. 2018. The Effect of Certificate of Need Laws on All-Cause Mortality. Health Services Research 53: 49–62. [Google Scholar] [CrossRef]
- Bailey, James. 2019. Can Health Spending Be Reined in through Supply Restraints? An Evaluation of Certificate-of-Need Laws. Journal of Public Health 27: 755–60. [Google Scholar] [CrossRef]
- Baker, Matthew C., and Thomas Stratmann. 2021. Barriers to Entry in the Healthcare Markets: Winners and Losers from Certificate-of-Need Laws. Socio-Economic Planning Sciences 2021: 101007. [Google Scholar] [CrossRef]
- Barclay, Eliza, Dylan Scott, and Christina Animashaun. 2020. The US Doesn’t Just Need to Flatten the Curve. It Needs to ‘Raise the Line’. Vox. April 7. Available online: https://www.vox.com/2020/4/7/21201260/coronavirus-usa-chart-mask-shortage-ventilators-flatten-the-curve (accessed on 8 October 2021).
- Boone, Rebecca, Iris Samuels, and Lindsey Tanner. 2021. EXPLAINER: What Are ‘Crisis Standards of Care?’. AP NEWS. September 17. Available online: https://apnews.com/article/business-health-public-health-coronavirus-pandemic-montana-4f68683b175340bf525c45aa133045ba (accessed on 8 October 2021).
- Botti, Mark. 2007. Competition In Healthcare And Certificates Of Need. In Testimony Before A Joint Session of The Health and Human Services Committee of the State Senate and The CON Special Committee of the State House of Representatives of the General Assembly of the State of Georgia. Washington, DC: U.S. Department of Justice Antitrust Division, Available online: https://www.justice.gov/atr/competition-healthcare-and-certificates-need#N_16_ (accessed on 8 October 2021).
- Cantor, Joel C., Derek DeLia, Amy Tiedemann, Ava Stanley, and Karl Kronebusch. 2009. Reducing Racial Disparities In Coronary Angiography. Health Affairs 28: 1521–31. [Google Scholar] [CrossRef] [Green Version]
- Carlson, Melissa D. A., Elizabeth H. Bradley, Qingling Du, and R. Sean Morrison. 2010. Geographic Access to Hospice in the United States. Journal of Palliative Medicine 13: 1331–38. [Google Scholar] [CrossRef] [Green Version]
- Cavanaugh, Jaimie, Caroline Grace Brothers, Adam Griffin, Richard Hoover, Melissa LoPresti, and John Wrench. 2020. Conning the Competition: A Nationwide Survey of Certificate of Need Laws. Arlington: Institute for Justice, Available online: https://ij.org/wp-content/uploads/2020/08/Conning-the-Competition-WEB-08.11.2020.pdf (accessed on 8 October 2021).
- Chiu, Kevin. 2021. The Impact of Certificate of Need Laws on Heart Attack Mortality: Evidence from County Borders. Journal of Health Economics 79: 102518. [Google Scholar] [CrossRef]
- Conover, Christopher J., and James Bailey. 2020. Certificate of Need Laws: A Systematic Review and Cost-Effectiveness Analysis. BMC Health Services Research 20: 748. [Google Scholar] [CrossRef]
- COVID-19 Reported Patient Impact and Hospital Capacity by Facility. 2021. HealthData.Gov. November 1. Available online: https://healthdata.gov/Hospital/COVID-19-Reported-Patient-Impact-and-Hospital-Capa/anag-cw7u (accessed on 8 October 2021).
- COVID-19 Reported Patient Impact and Hospital Capacity by State Timeseries. 2021. HealthData.Gov. October 1. Available online: https://healthdata.gov/Hospital/COVID-19-Reported-Patient-Impact-and-Hospital-Capa/g62h-syeh (accessed on 8 October 2021).
- Cutler, David M., Robert S. Huckman, and Jonathan T. Kolstad. 2010. Input Constraints and the Efficiency of Entry: Lessons from Cardiac Surgery. American Economic Journal: Economic Policy 2: 51–76. [Google Scholar] [CrossRef]
- D’Aunno, Thomas, Melissa Succi, and Jeffrey A. Alexander. 2000. The Role of Institutional and Market Forces in Divergent Organizational Change. Administrative Science Quarterly 45: 679–703. [Google Scholar] [CrossRef] [Green Version]
- DeLia, Derek, Joel C. Cantor, Amy Tiedemann, and Cecilia S. Huang. 2009. Effects of Regulation and Competition on Health Care Disparities: The Case of Cardiac Angiography in New Jersey. Journal of Health Politics, Policy and Law 34: 63–91. [Google Scholar] [CrossRef] [PubMed]
- Eichmann, Traci L., and Rexford E. Santerre. 2011. Do Hospital Chief Executive Officers Extract Rents from Certificate of Need Laws. Journal of Health Care Finance 37: 1–14. [Google Scholar] [PubMed]
- Erickson, Angela. 2021. States Are Suspending Certificate of Need Laws in the Wake of COVID-19 but the Damage Might Already Be Done. Pacific Legal Foundation (Blog). January 11. Available online: https://pacificlegal.org/certificate-of-need-laws-covid-19/ (accessed on 8 October 2021).
- Eriksson, Carl O., Ryan C. Stoner, Karen B. Eden, Craig D. Newgard, and Jeanne-Marie Guise. 2017. The Association Between Hospital Capacity Strain and Inpatient Outcomes in Highly Developed Countries: A Systematic Review. Journal of General Internal Medicine 32: 686–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fayissa, Bichaka, Saleh Alsaif, Fady Mansour, Tesa E. Leonce, and Franklin G. Mixon. 2020. Certificate-Of-Need Regulation and Healthcare Service Quality: Evidence from the Nursing Home Industry. Healthcare (Basel, Switzerland) 8: 423. [Google Scholar] [CrossRef] [PubMed]
- Federal Trade Commission and U.S. Department of Justice. 2016. Joint Statement of the Federal Trade Commission and the Antitrust Division of the U.S. Department of Justice on Certificate-of-Need Laws and South Carolina House Bill 3250. Available online: https://www.ftc.gov/policy/policy-actions/advocacy-filings/2016/01/joint-statement-federal-trade-commission-antitrust (accessed on 8 October 2021).
- Ford, Jon M., and David L. Kaserman. 1993. Certificate-of-Need Regulation and Entry: Evidence from the Dialysis Industry. Southern Economic Journal 59: 783–91. [Google Scholar] [CrossRef]
- Ghosh, Sriparna, Agnitra Roy Choudhury, and Alicia Plemmons. 2020. Certificate-of-Need Laws and Healthcare Utilization During COVID-19 Pandemic. SSRN Scholarly Paper ID 3663547. Rochester: Social Science Research Network. [Google Scholar] [CrossRef]
- Harrington, Charlene, James H. Swan, John A. Nyman, and Helen Carrillo. 1997. The Effect of Certificate of Need and Moratoria Policy on Change in Nursing Home Beds in the United States. Medical Care 35: 574–88. [Google Scholar] [CrossRef] [PubMed]
- Hellinger, Fred J. 1976. The Effect of Certificate-of-Need Legislation on Hospital Investment. Inquiry 13: 187–93. [Google Scholar] [PubMed]
- Hellinger, Fred J. 2009. The Effect of Certificate-of-Need Laws on Hospital Beds and Healthcare Expenditures: An Empirical Analysis. The American Journal of Managed Care 15: 737–44. [Google Scholar]
- Ho, Vivian, Joseph S. Ross, Brahmajee K. Nallamothu, and Harlan M. Krumholz. 2007. Cardiac Certificate of Need Regulations and the Availability and Use of Revascularization Services. American Heart Journal 154: 767–75. [Google Scholar] [CrossRef] [Green Version]
- Ho, Vivian, Meei-Hsiang Ku-Goto, and James G Jollis. 2009. Certificate of Need (CON) for Cardiac Care: Controversy over the Contributions of CON. Health Services Research 44: 483–500. [Google Scholar] [CrossRef]
- Hoover, Kent. 2012. Doctors Challenge Virginia’s Certificate-of-Need Requirement. The Business Journals. June 5. Available online: http://www.bizjournals.com/bizjournals/washingtonbureau/2012/06/05/doctors-challenge-virginias.html (accessed on 8 October 2021).
- Joskow, Paul L. 1980. The Effects of Competition and Regulation on Hospital Bed Supply and the Reservation Quality of the Hospital. The Bell Journal of Economics 11: 421–47. [Google Scholar] [CrossRef]
- Kessler, Carson. 2020. Emergency Mission: Hasidic Women Battle Male EMS for an Ambulance of Their Own. THE CITY. August 6. Available online: https://www.thecity.nyc/health/2020/8/6/21358050/hasidic-women-ambulance-brooklyn-ems-hatzalah-pandemic (accessed on 8 October 2021).
- Knight, Frank H. 1921. Risk Uncertainty and Profit. Boston: Hart, Schaffner & Marx. [Google Scholar]
- Kolstad, Jonathan T. 2009. Essays on Information, Competition and Quality in Health Care Provider Markets. Ph.D. dissertation, Harvard University, Boston, MA, USA. Available online: https://healthpolicy.fas.harvard.edu/people/jonathan-kolstad (accessed on 8 October 2021).
- Lee, Bill. 2020. Tennessee Exec. Order No. 15, 10. Available online: https://publications.tnsosfiles.com/pub/execorders/exec-orders-lee15.pdf (accessed on 8 October 2021).
- Lorch, S. A., P. Maheshwari, and O. Even-Shoshan. 2012. The Impact of Certificate of Need Programs on Neonatal Intensive Care Units. Journal of Perinatology: Official Journal of the California Perinatal Association 32: 39–44. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, Matthew D., Anne Philpot, and Jessica McBirney. 2021. CON Laws in 2020: About the Update. Arlington: Mercatus Center at George Mason University, Available online: https://www.mercatus.org/publications/healthcare/con-laws-2020-about-update (accessed on 8 October 2021).
- Mitchell, Matthew, Thomas Stratmann, and James Bailey. 2020. Raising the Bar: ICU Beds and Certificates of Need. Arlington: Mercatus Center at George Mason University, Available online: https://www.mercatus.org/publications/covid-19-crisis-response/raising-bar-icu-beds-and-certificates-need (accessed on 8 October 2021).
- Mitchell, Matthew. 2016. Do Certificate-of-Need Laws Limit Spending? Mercatus Working Paper. Arlington: Mercatus Center at George Mason University, Available online: https://www.mercatus.org/system/files/mercatus-mitchell-con-healthcare-spending-v3.pdf (accessed on 8 October 2021).
- Myers, Molly S., and Kathleen M. Sheehan. 2020. The Impact of Certificate of Need Laws on Emergency Department Wait Times. Journal of Private Enterprise 35: 59–75. [Google Scholar]
- National Diabetes Statistics Report. 2020. Centers for Disease Control and Prevention. February 11. Available online: https://www.cdc.gov/diabetes/library/features/diabetes-stat-report.html (accessed on 8 October 2021).
- National Health Planning and Resources Development Act of 1974. 1975. U.S.C. Vol. 88. Available online: https://www.gpo.gov/fdsys/pkg/STATUTE-88/pdf/STATUTE-88-Pg2225.pdf (accessed on 8 October 2021).
- Noether, Monica. 1988. Competition Among Hospitals. Journal of Health Economics 7: 259–84. [Google Scholar] [CrossRef]
- Northam, Ralph. 2020. Virginia Exc. Order No. 52 Amended, 1. Available online: https://www.governor.virginia.gov/media/governorvirginiagov/executive-actions/EO-52-AMENDED---Extension-of-Increases-in-Hospital-Bed-Capacity-in-Response-to-Novel-Coronavirus-(COVID-19).pdf (accessed on 8 October 2021).
- Ohsfeldt, Robert L., and Pengxiang Li. 2018. State Entry Regulation and Home Health Agency Quality Ratings. Journal of Regulatory Economics 53: 1–19. [Google Scholar] [CrossRef] [Green Version]
- Popescu, Iona, Mary S. Vaughan-Sarrazin, and Gary E. Rosenthal. 2006. Certificate of Need Regulations and Use of Coronary Revascularization After Acute Myocardial Infarction. The Journal of the American Medical Association 295: 2141–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pub. L. 99-660, § 701, 100 Stat. 3799. 1986.
- Robinson, Jamie L., David B. Nash, Elizabeth Moxey, and John P. O’Connor. 2001. Certificate of Need and the Quality of Cardiac Surgery. American Journal of Medical Quality: The Official Journal of the American College of Medical Quality 16: 155–60. [Google Scholar] [CrossRef]
- Salkever, David S., and Thomas W. Bice. 1976. The Impact of Certificate-of Need Controls on Hospital Investment. The Milbank Memorial Fund Quarterly. Health and Society 54: 185–214. [Google Scholar] [CrossRef]
- Sánchez-Úbeda, Eugenio F., Pedro Sánchez-Martín, Macarena Torrego-Ellacuría, Ángel Del Rey-Mejías, Manuel F. Morales-Contreras, and José-Luis Puerta. 2021. Flexibility and Bed Margins of the Community of Madrid’s Hospitals during the First Wave of the SARS-CoV-2 Pandemic. International Journal of Environmental Research and Public Health 18: 3510. [Google Scholar] [CrossRef]
- Short, Marah N., Thomas A. Aloia, and Vivian Ho. 2008. Certificate of Need Regulations and the Availability and Use of Cancer Resections. Annals of Surgical Oncology 15: 1837–45. [Google Scholar] [CrossRef]
- Sloan, Frank A. 1981. Regulation and the Rising Cost of Hospital Care. The Review of Economics and Statistics 63: 479–87. [Google Scholar] [CrossRef]
- Sloan, Frank A., and Bruce Steinwald. 1980. Effects of Regulation on Hospital Costs and Input Use. The Journal of Law & Economics 23: 81–109. [Google Scholar]
- Spektor, Brandon. 2020. Coronavirus: What Is ‘flattening the Curve,’ and Will It Work? Live Science. March 16. Available online: https://www.livescience.com/coronavirus-flatten-the-curve.html (accessed on 8 October 2021).
- Stone, Will. 2021. A COVID Surge Is Overwhelming U.S. Hospitals, Raising Fears Of Rationed Care. NPR, September 5. sec. The Coronavirus Crisis. Available online: https://www.npr.org/sections/health-shots/2021/09/05/1034210487/covid-surge-overwhelming-hospitals-raising-fears-rationed-care (accessed on 8 October 2021).
- Stratmann, Thomas, and Christopher Koopman. 2016. Entry Regulation and Rural Health Care: Certificate-of-Need Laws, Ambulatory Surgical Centers, and Community. Working Paper. Arlington: Mercatus Center at George Mason University, Available online: http://mercatus.org/sites/default/files/Stratmann-Rural-Health-Care-v1.pdf (accessed on 8 October 2021).
- Stratmann, Thomas, and David Wille. 2016. Certificate of Need Laws and Hospital Quality. Mercatus Working Paper. Arlington: Mercatus Center at George Mason University, Available online: https://www.mercatus.org/system/files/mercatus-stratmann-wille-con-hospital-quality-v1.pdf (accessed on 8 October 2021).
- Stratmann, Thomas, and Jacob Russ. 2014. Do Certificate-of-Need Laws Increase Indigent Care? Working Paper 14–20. Arlington: Mercatus Center at George Mason University. Available online: http://mercatus.org/sites/default/files/Stratmann-Certificate-of-Need.pdf (accessed on 8 October 2021).
- Stratmann, Thomas, and Matthew Baker. 2020. Examining Certificate-of-Need Laws in the Context of the Rural Health Crisis. Mercatus Working Paper. Arlington: Mercatus Center at George Mason University, Available online: https://www.mercatus.org/publications/healthcare/examining-certificate-need-laws-context-rural-health-crisis (accessed on 8 October 2021).
- Stratmann, Thomas, and Steven Monaghan. 2017. The Effect of Interest Group Pressure on Favorable Regulatory Decisions: The Case of Certificate-of-Need Laws. Mercatus Working Paper. Arlington: Mercatus Center at George Mason University, Available online: https://www.mercatus.org/publications/interest-group-pressure-favorable-regulatory-decisions-certificate-of-need (accessed on 8 October 2021).
- United States COVID-19 Cases and Deaths by State over Time. n.d. HealthData.Gov. Available online: https://healthdata.gov/dataset/United-States-COVID-19-Cases-and-Deaths-by-State-o/hiyb-zgc2 (accessed on 1 October 2021).
- US Department of Commerce, B. E. A. n.d. Bureau of Economic Analysis. National Income and Product Accounts Tables. Available online: http://www.bea.gov/iTable/iTable.cfm?ReqID=9&step=1#reqid=9&step=1&isuri=1 (accessed on 6 December 2013).
- Vaughan Sarrazin, Mary S., Levent Bayman, and Peter Cram. 2010. Trends during 1993–2004 in the Availability and Use of Revascularization after Acute Myocardial Infarction in Markets Affected by Certificate of Need Regulations. Medical Care Research and Review: MCRR 67: 213–31. [Google Scholar] [CrossRef] [PubMed]
- Vaughan-Sarrazin, Mary S., Edward L. Hannan, Carol J. Gormley, and Gary E. Rosenthal. 2002. Mortality in Medicare Beneficiaries Following Coronary Artery Bypass Graft Surgery in States with and without Certificate of Need Regulation. JAMA 288: 1859–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Obs | Mean | Std. Dev. | Min | Max | |
|---|---|---|---|---|---|
| Outcome Variables | |||||
| Average Share of Beds Used per Month per State | 968 | 66.56 | 11.17 | 17.50 | 106.13 |
| Number of Days per Month in Which More than 70 Percent of Beds in Use | 968 | 12.82 | 12.61 | 0.00 | 31.00 |
| Explanatory Variables of Interest | |||||
| Bed CON | 968 | 0.52 | 0.50 | 0.00 | 1.00 |
| Bed CON Relaxed | 968 | 0.32 | 0.46 | 0.00 | 1.00 |
| Control Variables | |||||
| Percent Black | 968 | 10.65 | 9.43 | 0.50 | 38.00 |
| Percent Hispanic | 968 | 12.13 | 10.44 | 1.40 | 49.10 |
| Real per Capita Personal Income, $2017 | 968 | 48,624.15 | 4814.192 | 40,118 | 63,366 |
| Percent of Adults with Diabetes | 968 | 9.41 | 1.61 | 6.20 | 13.20 |
| New Cases per Population | 968 | 0.68 | 0.71 | 0.00 | 4.55 |
| States That Do Not Require a CON for Hospital Beds | |||||
|---|---|---|---|---|---|
| Variable | Obs | Mean | Std. Dev. | Min | Max |
| Outcome Variables | |||||
| Average Share of Beds Used per Month per State | 466 | 63.27 | 11.72 | 17.50 | 92.58 |
| Number of Days per Month in Which More than 70 Percent of Beds in Use | 466 | 9.64 | 11.60 | 0.00 | 31.00 |
| Control Variables | |||||
| Percent Black | 466 | 7.37 | 6.86 | 0.50 | 32.40 |
| Percent Hispanic | 466 | 15.38 | 13.18 | 3.60 | 49.10 |
| Real per Capita Personal Income, 2017 | 466 | 48,470.55 | 4290.456 | 40,118 | 56,114 |
| Percent of Adults with Diabetes | 466 | 9.03 | 1.53 | 6.20 | 12.10 |
| New Cases per Population | 466 | 0.73 | 0.77 | 0.00 | 4.55 |
| States That Require a CON for Hospital Beds | |||||
| Obs | Mean | Std. Dev. | Min | Max | |
| Outcome Variables | |||||
| Average Share of Beds Used per Month per State | 502 | 69.61 | 9.70 | 30.56 | 106.13 |
| Number of Days per Month in Which More than 70 Percent of Beds in Use | 502 | 15.78 | 12.79 | 0.00 | 31.00 |
| Control Variables | |||||
| Percent Black | 502 | 13.70 | 10.42 | 1.20 | 38.00 |
| Percent Hispanic | 502 | 9.11 | 5.50 | 1.40 | 20.60 |
| Real per Capita Personal Income, 2017 | 502 | 48,766.75 | 5254.157 | 40,195 | 63,366 |
| Percent of Adults with Diabetes | 502 | 9.76 | 1.60 | 7.30 | 13.20 |
| New Cases per Population | 502 | 0.63 | 0.66 | 0.00 | 3.42 |
| Obs | Mean | Std. Dev. | Min | Max | |
|---|---|---|---|---|---|
| Outcome Variables | |||||
| 100 Percent or More of Facility’s Beds In Use | 259,149 | 0.01 | 0.09 | 0 | 1 |
| Explanatory Variables of Interest | |||||
| Bed CON | 259,149 | 0.43 | 0.50 | 0 | 1 |
| Bed CON Relaxed | 259,149 | 0.29 | 0.45 | 0 | 1 |
| Control Variables | |||||
| Percent Black | 259,149 | 12.44 | 8.66 | 0.50 | 38.00 |
| Percent Hispanic | 259,149 | 15.54 | 12.88 | 1.40 | 49.10 |
| Real per Capita Personal Income, $2017 | 259,149 | 48,535.13 | 3937.40 | 40,118.00 | 63,366.00 |
| Percent of Adults with Diabetes | 259,149 | 9.81 | 1.41 | 6.2 | 13.2 |
| New Cases per Population | 259,149 | 0.01 | 0.01 | 0.00 | 0.05 |
| Rural Indicator | 259,149 | 0.18 | 0.38 | 0 | 1 |
| Critical Access Hospital Indicator | 259,149 | 0.22 | 0.42 | 0 | 1 |
| Long-Term Care Facility Indicator | 259,149 | 0.08 | 0.27 | 0 | 1 |
| States That Do Not Require a CON for Hospital Beds | |||||
|---|---|---|---|---|---|
| Obs | Mean | Std. Dev. | Min | Max | |
| Outcome Variables | |||||
| 100 Percent or More of Facility’s Beds In Use | 147,264 | 0.01 | 0.08 | 0 | 1 |
| Control Variables | |||||
| Percent Black | 147,264 | 9.89 | 6.78 | 0.50 | 32.40 |
| Percent Hispanic | 147,264 | 20.05 | 14.84 | 3.60 | 49.10 |
| Real per Capita Personal Income, $2017 | 147,264 | 48,355.09 | 3148.40 | 40,118.00 | 56,114.00 |
| Percent of Adults with Diabetes | 147,264 | 9.60 | 1.32 | 6.20 | 12.10 |
| New Cases per Population | 147,264 | 0.01 | 0.01 | 0.00 | 0.05 |
| Rural Indicator | 147,264 | 0.17 | 0.37 | 0 | 1 |
| Critical Access Hospital Indicator | 147,264 | 0.23 | 0.42 | 0 | 1 |
| Long-Term Care Facility Indicator | 147,264 | 0.09 | 0.28 | 0 | 1 |
| States That Require a CON for Hospital Beds | |||||
| Obs | Mean | Std. Dev. | Min | Max | |
| Outcome Variables | |||||
| 100 Percent or More of Facility’s Beds In Use | 111,885 | 0.01 | 0.11 | 0 | 1 |
| Control Variables | |||||
| Percent Black | 111,885 | 15.80 | 9.67 | 1.20 | 38.00 |
| Percent Hispanic | 111,885 | 9.61 | 5.72 | 1.40 | 20.60 |
| Real per Capita Personal Income, $2017 | 111,885 | 48,772.09 | 4771.05 | 40,195.00 | 63,366.00 |
| Percent of Adults with Diabetes | 111,885 | 10.09 | 1.49 | 7.3 | 13.2 |
| New Cases per Population | 111,885 | 0.01 | 0.01 | 0.00 | 0.03 |
| Rural Indicator | 111,885 | 0.19 | 0.39 | 0 | 1 |
| Critical Access Hospital Indicator | 111,885 | 0.21 | 0.41 | 0 | 1 |
| Long-Term Care Facility Indicator | 111,885 | 0.06 | 0.24 | 0 | 1 |
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Variables | Full Model | Limited Model | More Limited Model | Univariate Model |
| Bed CON | 7.571 *** | 7.694 *** | 7.674 *** | 6.344 *** |
| (2.659) | (2.663) | (2.620) | (1.883) | |
| Bed CON Relaxed | −2.168 | −1.962 | −1.096 | |
| (2.344) | (2.366) | (2.207) | ||
| Percent Black | 0.203 * | 0.246 ** | 0.224 ** | |
| (0.109) | (0.104) | (0.102) | ||
| Percent Hispanic | 0.261 *** | 0.261 *** | 0.263 *** | |
| (0.0619) | (0.0643) | (0.0639) | ||
| New Cases per Population | 1.523 * | 1.574 * | 4.569 *** | |
| (0.867) | (0.848) | (0.457) | ||
| Real per Capita Personal Income, $2017 | 0.000232 | |||
| (0.000211) | ||||
| Percent of Adults with Diabetes | 0.623 | |||
| (0.560) | ||||
| Constant | 27.73 * | 44.33 *** | 54.26 *** | 63.27 *** |
| (14.25) | (8.062) | (2.155) | (1.401) | |
| Month Effects | Yes | Yes | No | No |
| Observations | 968 | 968 | 968 | 968 |
| R-Squared | 0.50 | 0.50 | 0.25 | 0.08 |
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Variables | Full Model | Limited Model | More Limited Model | Univariate Model |
| Bed CON | 5.675 * | 5.968 * | 6.818 ** | 6.146 ** |
| (3.121) | (3.199) | (3.040) | (2.379) | |
| Bed CON Relaxed | 0.563 | 0.901 | 0.224 | |
| (3.204) | (3.377) | (3.110) | ||
| Percent Black | 0.186 | 0.282 * | 0.263 | |
| (0.180) | (0.157) | (0.157) | ||
| Percent Hispanic | 0.324 *** | 0.325 *** | 0.329 *** | |
| (0.0849) | (0.0920) | (0.0900) | ||
| New Cases per Population | 1.408 | 1.533 | 4.368 *** | |
| (1.188) | (1.229) | (0.663) | ||
| Real per Capita Personal Income, $2017 | 0.000445 ** | |||
| (0.000218) | ||||
| Percent of Adults with Diabetes | 1.322 | |||
| (0.883) | ||||
| Constant | −37.76 ** | −4.735 | −0.532 | 9.637 *** |
| (16.16) | (3.058) | (2.264) | (1.601) | |
| Month Effects | Yes | Yes | No | No |
| Observations | 968 | 968 | 968 | 968 |
| R-Squared | 0.39 | 0.37 | 0.22 | 0.06 |
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Variables | Full Model | Limited Model | More Limited Model | Univariate Model |
| Bed CON | 0.268 ** | 0.250 ** | 0.264 ** | 0.244 ** |
| (0.125) | (0.120) | (0.112) | (0.101) | |
| Bed CON Relaxed | 0.091 | 0.058 | −0.001 | |
| (0.125) | (0.122) | (0.125) | ||
| Percent Black | −0.002 | 0.001 | 0.003 | |
| (0.00753) | (0.00572) | (0.00580) | ||
| Percent Hispanic | 0.002 | 0.002 | 0.002 | |
| (0.00488) | (0.00532) | (0.00532) | ||
| New Cases per Population | 14.43 ** | 19.11 *** | 10.66 ** | |
| (6.570) | (5.882) | (4.140) | ||
| Real per Capita Personal Income, $2017 | −3.12 × 10−5 ** | |||
| (1.30 × 10−5) | ||||
| Percent of Adults with Diabetes | −0.00730 | |||
| (0.0569) | ||||
| Rural Indicator | −0.0936 | −0.0717 | −0.0602 | |
| (0.110) | (0.102) | (0.0983) | ||
| Critical Access Hospital Indicator | −0.138 | −0.124 | −0.124 | |
| (0.104) | (0.0973) | (0.0951) | ||
| Long-Term Care Facility Indicator | 0.00903 | 0.0225 | 0.0250 | |
| (0.0857) | (0.0819) | (0.0806) | ||
| Month Effects | Yes | Yes | No | No |
| Observations | 259,149 | 259,149 | 259,149 | 259,149 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitchell, M.; Stratmann, T. The Economics of a Bed Shortage: Certificate-of-Need Regulation and Hospital Bed Utilization during the COVID-19 Pandemic. J. Risk Financial Manag. 2022, 15, 10. https://doi.org/10.3390/jrfm15010010
Mitchell M, Stratmann T. The Economics of a Bed Shortage: Certificate-of-Need Regulation and Hospital Bed Utilization during the COVID-19 Pandemic. Journal of Risk and Financial Management. 2022; 15(1):10. https://doi.org/10.3390/jrfm15010010
Chicago/Turabian StyleMitchell, Matthew, and Thomas Stratmann. 2022. "The Economics of a Bed Shortage: Certificate-of-Need Regulation and Hospital Bed Utilization during the COVID-19 Pandemic" Journal of Risk and Financial Management 15, no. 1: 10. https://doi.org/10.3390/jrfm15010010
APA StyleMitchell, M., & Stratmann, T. (2022). The Economics of a Bed Shortage: Certificate-of-Need Regulation and Hospital Bed Utilization during the COVID-19 Pandemic. Journal of Risk and Financial Management, 15(1), 10. https://doi.org/10.3390/jrfm15010010