Wear Morphology on the Surfaces of CoCrMo Unicompartmental Knee Joint Endoprostheses as Elements of Metal–Metal Friction Nodes
Abstract
1. Introduction
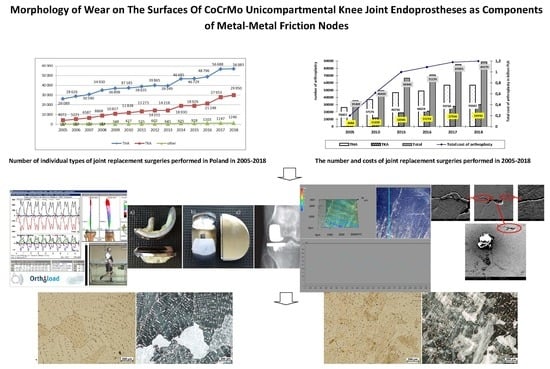
2. Statistical Evaluation of the Number of Surgeries and Costs of Joint Replacement in Poland
- 2020: THA—by 34% (to 498,000 replacements); TKA by 56% (to 1,065,000 replacements);
- 2025: THA—by 75% (to 652,000 replacements); TKA by 110% (to 1,272,000 replacements);
- 2030: THA—by 129% (to 850,000 replacements); TKA by 182% (to 1,921,000 replacements);
- 2040: THA—by 284% (to 1,429,000 replacements); TKA by 401% (to 3,416,000 replacements).
- (1)
- hip joint:
- cement alloplasty: in 2005: 9933–11,100 PLN (which translated into 2573–2876 EUR and 3047–3405 USD), in 2018: 10,000–11,700 PLN (which translated into 2325–2720 EUR and 2659–3112 USD);
- cementless arthroplasty: in 2005: 12,220–13,000 PLN (which translated into 3161–3368 EUR and 3742–3988 USD), in 2018: 13,000–23,000 PLN (which translated into 3023–5349 EUR and 3457–6117 USD);
- revision arthroplasty: in 2005: 20,835–24,095 PLN (which translated into 5398–6242 EUR and 6391–7391 USD), in 2018: 19,000–20,000 PLN (which translated into 4419–9070 EUR and 5053–5319 USD).
- (2)
- knee joint:
- cement arthroplasty: in 2005 13,590–17,456 PLN (which translated into 3521–4522 EUR and 4169–5355 USD); in 2018: 15,750–20,000 PLN (which translated into 3662–4651 EUR and 4189–5319 USD);
- revision arthroplasty: in 2005: 21,715–23,568 PLN (which translated into 5626–6106 EUR and 6661–7229 USD); in 2018: 12,500–20,000 PLN (which translated into 2907–4651 EUR and 3324–5319 USD).
3. Materials and Methods
4. Results and Discussion: Assessment of the Destruction of Surfaces of Unicompartmental Endoprostheses
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Haijie, L.; Dasen, L.; Tao, J.; Yi, Y.; Xiaodong, T.; Wei, G. Implant survival and complication profiles of endoprostheses for treating tumor around the knee in adults: A systematic review of the literature over the past 30 years. J. Arth. 2018, 33, 1275–1287. [Google Scholar] [CrossRef] [PubMed]
- Bergschmidt, P.; Ellenrieder, M.; Bader, R.; Kluess, D.; Finze, S.; Schwemmer, B.; Mittelmeier, W. Prospective comparative clinical study of ceramic and metallic femoral components for total knee arthroplasty over a five-year follow-up period. Knee 2016, 23, 871–876. [Google Scholar] [CrossRef] [PubMed]
- Winnock de Grave, P.; Barbier, J.; Luyckx, T.; Ryckaert, A.; Gunst, P.; Van den Daelen, L. Outcomes of a fixed-bearing, medial, cemented unicondylar knee arthroplasty design: Survival analysis and functional score of 460 cases. J. Arthroplast. 2018, 33, 2792–2799. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.W.; Smith, G.C.; Lee, S. A preliminary study to enhance the tribological performance of cocrmo alloy by fibre laser remelting for articular joint implant applications. Lubricants 2018, 6, 24. [Google Scholar] [CrossRef]
- Clinical Outcomes and Statistics of Knee Replacement. Available online: https://www.healthline.com/health/total-knee-replacement-surgery/outcomes-statistics-success-rate#takeaway (accessed on 5 April 2020).
- Singh, J.A.; Yu, S.; Chen, L.; Cleveland, J.D. Rates of total joint replacement in the United States: Future projections to 2020–2040 using the National Inpatient Sample. J. Rheumatol. 2019, 46, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Cook, M.J.; Sorial, A.K.; Lunt, M.; Board, T.N.; O’Neill, T.W. Effect of timing and duration of statin exposure on risk of hip or knee revision arthroplasty: A population-based cohort study. J. Rheumatol. 2020, 47, 441–448. [Google Scholar] [CrossRef]
- Endoprotezoplastyka Stawowa w 2012. Narodowy Fundusz Zdrowia. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=3&ved=2ahUKEwj6of6EmanpAhW3URUIHR1QDhkQFjACegQIAhAB&url=https%3A%2F%2Fwww.nfz.gov.pl%2Fdownload%2Fgfx%2Fnfz%2Fpl%2Fdefaultstronaopisowa%2F349%2F5%2F1%2F2013_05_07_endoprotezy_2012_analiza.pdf&usg=AOvVaw0Kjy-f2PbBqX9BcpYK1Rt7 (accessed on 5 April 2020).
- Realizacja Świadczeń Endoprotezoplastyki Stawowej w 2013. Narodowy Fundusz Zdrowia. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&uact=8&ved=2ahUKEwjSvq_ZmKnpAhWUunEKHcUNCNMQFjAAegQIBRAB&url=https%3A%2F%2Fwww.nfz.gov.pl%2Fdownload%2Fgfx%2Fnfz%2Fpl%2Fdefaultstronaopisowa%2F349%2F1%2F1%2F2014_06_02_endoprotezoplastyka_2013.pdf&usg=AOvVaw3U-6u-s3j5uaEjZ4BoLg3C (accessed on 5 April 2020).
- Realizacja Świadczeń Endoprotezoplastyki Stawowej w 2014. Narodowy Fundusz Zdrowia. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&uact=8&ved=2ahUKEwjDxI7CmKnpAhXUtXEKHV6BDt0QFjAAegQIBBAB&url=https%3A%2F%2Fwww.nfz.gov.pl%2Fdownload%2Fgfx%2Fnfz%2Fpl%2Fdefaultstronaopisowa%2F349%2F26%2F1%2Frealizacja_swiadczen_endoprotezoplastyki_stawowej_w_2014_r..pdf&usg=AOvVaw3TgHeBAknPBd8-BofF_iS1 (accessed on 5 April 2020).
- Realizacja Świadczeń Endoprotezoplastyki Stawowej w 2015. Narodowy Fundusz Zdrowia. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&uact=8&ved=2ahUKEwj_wYOomKnpAhVXTBUIHWMtBb0QFjAAegQIAhAB&url=https%3A%2F%2Fwww.nfz.gov.pl%2Fdownload%2Fgfx%2Fnfz%2Fpl%2Fdefaultstronaopisowa%2F349%2F30%2F1%2Fcbe_za_2015.pdf&usg=AOvVaw2t2rVJdLWx3J0AoiGffuZp (accessed on 5 April 2020).
- Realizacja Świadczeń Endoprotezoplastyki Stawowej w 2016. Narodowy Fundusz Zdrowia. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=2ahUKEwiIse_zl6npAhWStHEKHbbUBBsQFjAAegQIBhAB&url=https%3A%2F%2Fwww.nfz.gov.pl%2Fdownload%2Fgfx%2Fnfz%2Fpl%2Fdefaultstronaopisowa%2F349%2F34%2F1%2Fcbe_za_2016.pdf&usg=AOvVaw3rMSswyJvi9Kk4lTJ9eTib (accessed on 5 April 2020).
- Realizacja Świadczeń Endoprotezoplastyki Stawowej w 2017. Narodowy Fundusz Zdrowia. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=2ahUKEwjn5-nYl6npAhVYUhUIHQWDBEYQFjAAegQIBhAB&url=https%3A%2F%2Fwww.nfz.gov.pl%2Fdownload%2Fgfx%2Fnfz%2Fpl%2Fdefaultstronaopisowa%2F349%2F38%2F1%2Frealizacja_swiadczen_endoprotezoplastyki_stawowej_w_2017_r.pdf&usg=AOvVaw03lXZ58OJNIXfI1M9EAabT (accessed on 5 April 2020).
- Realizacja Świadczeń Endoprotezoplastyki Stawowej w 2018. Narodowy Fundusz Zdrowia. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=2&ved=2ahUKEwio75mAl6npAhUEXRUIHXzbAh4QFjABegQIAhAB&url=https%3A%2F%2Fwww.nfz.gov.pl%2Fdownload%2Fgfx%2Fnfz%2Fpl%2Fdefaultstronaopisowa%2F349%2F38%2F1%2Frealizacja_swiadczen_endoprotezoplastyki_stawowej_w_2017_r.pdf&usg=AOvVaw03lXZ58OJNIXfI1M9EAabT (accessed on 5 April 2020).
- Benazzo, F. Całkowita endoprotezoplastyka stawu kolanowego wchodzi w nową fazę. CeraNews 2015, 1, 3–4. [Google Scholar]
- Mittelmeierem, W. Przyszłość endoprotezoplastyki stawu kolanowego: Komponenty ceramiczne wchodzą do gry. CeraNews 2015, 1, 5–7. [Google Scholar]
- Bergschmidt, P.; Bader, R.; Ganzer, D.; Hauzeur, C.H.; Lohmann, C.H.; Krüger, A.; Rüther, W.; Tigani, D.; Rani, N.; Esteve, J.L.; et al. Prospective multi-centre study on a composite ceramic femoral component in total knee arthroplasty: Five-year clinical and radiological outcomes. Knee 2015, 22, 185–195. [Google Scholar] [CrossRef]
- Walker, T.; Zahn, N.; Bruckner, T.; Streit, M.R.; Mohr, G.; Aldinger, P.R.; Clarius, M.; Gotterbarm, T. Mid-term Results of Lateral Unicondylar Mobile Bearing Knee Arthroplasty: A Multicentre Study of 363 Cases. Bone Joint J. 2018, 100, 42–49. [Google Scholar] [CrossRef]
- Affatato, S.; Valigi, M.C.; Logozzo, S. Knee Wear Assessment: 3D Scanners Used as a Consolidated Procedure. Materials 2020, 13, 2349. [Google Scholar] [CrossRef] [PubMed]
- Błażewicz Stanisław, Marciniak Jan: Inżynieria Biomedyczna Podstawy i Zastosowanie. Tom 4. Biomateriały; EXIT: Warsaw, Poland, 2017.
- Romuald Będziński: Mechanika Techniczna. Biomechanika; Instytut Podstawowych Problemów Techniki Polskiej Akademii Nauk: Warsaw, Poland, 2011.
- Błaszczyk, J.W. Biomechanika Kliniczna; PZWL Wydawnictwo Lekarskie: Warsaw, Poland, 2019. [Google Scholar]
- Bao, Y.; Kudo, T.; Cao, S.; Munoz, A.I.; Mischler, S. Passivation Charge Density of CoCrMo Alloy in Different Aqueous Solutions. J. Bio Tribo-Corros. 2020, 6, 58. [Google Scholar] [CrossRef]
- Mell, S.P.; Fullam, S.; Wimmer, M.A.; Lundberg, H.J. Computational Parametric Studies for Preclinical Evaluation of Total Knee Replacements. CMBBE 2019, 36, 60–85. [Google Scholar] [CrossRef]
- Pronk, Y.; Paters, A.A.M.; Brinkman, J.M. No difference in patient satisfaction after mobile bearing or fixed bearing medial unicompartmental knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2020. [Google Scholar] [CrossRef]
- Szarek, A. Biomechaniczne i Biomateriałowe Determinanty Aseptycznego Obluzowania Endoprotez Stawu Biodrowego Człowieka; Publishing House of the Czestochowa University of Technology: Częstochowa, Poland, 2015. [Google Scholar]
- Świerczyńska-Machura, D.; Kieć-Świerczyńska, M.; Kręcisz, B.; Pałczyński, C. Alergia na składowe implantów. Alerg. Astma Immunol. 2004, 9, 128–132. [Google Scholar]
- Szarek, A. Mechanical Destruction of Joints Implants. Izdatel’stvo Nauka i Obrazovanie; Publishing House Education and Science s.r.o.: Praga—Dniepr, Czech Republic-Ukraine, 2018. [Google Scholar]
- www.OrthoLoad.com. Available online: https://orthoload.com/database/?implantId=1322&activityId=1536&activityIndentationLevel=3¶meterId=1¶meterIndentationLevel=-1&patientId=all&fileId=k8l_191211_1_107p&fileType=t&selectBox=file, (accessed on 5 April 2020).
- www.OrthoLoad.com. Available online: https://orthoload.com/database/?implantId=1322&activityId=2295&activityIndentationLevel=2¶meterId=880¶meterIndentationLevel=0&patientId=all&fileId=k1l_240309_3_183p&fileType=t&selectBox=file (accessed on 5 April 2020).
- Kusz, D.; Wojciechowski, P.; Cielinski, L.S.; Iwaniak, A.; Jurkojc, J.; Gasiorek, D. Stress distribution around TKR implant: Are lab results consistent with observational studies. Acta Bioeng. Biomech. 2008, 10, 21–26. [Google Scholar] [PubMed]
- Nardini, F.; Belvedere, C.; Sancisi, N.; Conconi, M.; Leardini, A.; Durante, S.; Parenti-Castelli, V. An Anatomical-Based Subject-Specific Model of In-Vivo Knee Joint 3D Kinematics From Medical Imaging. Appl. Sci. 2020, 10, 2100. [Google Scholar] [CrossRef]
- Stetter, B.J.; Ringhof, S.; Krafft, F.C.; Sell, S.; Stein, T. Estimation of Knee Joint Forces in Sport Movements Using Wearable Sensors and Machine Learning. Sensors 2019, 19, 3690. [Google Scholar] [CrossRef]
- Jiang, H.; Xiang, S.; Guo, Y.; Wang, Z. A wireless visualized sensing system with prosthesis pose reconstruction for total knee arthroplasty. Sensors 2019, 19, 2909. [Google Scholar] [CrossRef]
- Szarek, A.; Wolański, W.; Szyproski, J.; Kopuliński, Ł.; Radecki, M.; Bednarek, B. Using Engineering Tools for Choosing Hip Joint Endoprosthesis. Sovrem. Naucn. Vestn. 2013, 32, 82–92. [Google Scholar]
- Vitale, M.M.J.A.; Stucovitz, E.; Romagnoli, S. Simultaneous bilateral unicompartmental knee replacement improves gait parameters in patients with bilateral knee osteoarthritis. Knee 2019, 26, 1413–1420. [Google Scholar] [CrossRef]
- Kakara, R.S.; Fub, Y.C.; Kinseyc, T.L.; Brownd, C.N.; Mahoneyce, O.M.; Simpsone, K.J. Lower limb kinematics of unicompartmental knee arthroplasty individuals during stair ascent. J. Orthop. 2020, 22, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Kakar, R.S.; Fu, Y.C.; Mahoney, O.M.; Kinsey, T.L.; Simpson, K.J. Knee strength, power and stair performance of the elderly 5 years after unicompartmental knee arthroplasty. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 1411–1416. [Google Scholar] [CrossRef]
- NBP Exchange Rates. Available online: https://www.money.pl/pieniadze/nbp/srednie/?date=2005-12-30 (accessed on 5 April 2020).
- NBP Exchange Rates. Available online: https://www.money.pl/pieniadze/nbp/srednie/?date=2018-12-31 (accessed on 5 April 2020).
- Maśliński, S.L.; Ryżewski, J. Patofizjologia, 4th ed.; PZWL Wydawnictwo Lekarskie: Warsaw, Poland, 2019. [Google Scholar]
- Szarek, A. Assessment of wear of metal heads in heap joint prosthesis removed from human body due to aseptic loosening. Eng. Biomater. 2008, 11, 6–10. [Google Scholar]
- Aoki, H.; Kato, K. Studies on the application of apatite to dental materials. J. Dent. Eng. 1977, 18, 86–89. [Google Scholar]
- Anderson, F.C.; Pandy, M.G. Dynamic simulation of human motion in three dimensions. In Proceedings of the Sixth Internetional Symposium on the 3D Analysis of Human Movement, Cape Town, South Africa, 1–4 May 2000; pp. 1–4. [Google Scholar]
- Aoki, H. Medicalapplication of Hydroźyapatite; Ishiyaku euroamerica: Tokio, Japan, 1994. [Google Scholar]
- Akahori, T.; Niinomi, M. Fracture characteristic of fatigued Ti-6Al.-4V ELI as an implant material. Mater. Sci. Eng. 1998, 243, 237–243. [Google Scholar] [CrossRef]
- Jiang, X.J.; Whitehouse, D.V. Technological shifts in surface metrology. CIRP Manuf. Technol. 2012, 61, 815–836. [Google Scholar] [CrossRef]
- Leach, R. Characterization of Areal Surface Texture; Springer: Berlin, Germany, 2013. [Google Scholar]


















| Co [%] | Cr [%] | Mo [%] | Si [%] | C [%] |
|---|---|---|---|---|
| 63.17 | 27.67 | 4.94 | 0.79 | 3.42 |
| Sample Tested | HV100 | Re [MPa] | KIC [MPa•m1/2] |
|---|---|---|---|
| Tibial Component, New | |||
| Sample 1 Sample 2 | 365 360 359 360 362 358 Mean 360 Standard Deviation 2.50 | 122 120 119 120 120 119 Mean 120 Standard Deviation 1.09 | 108 104 106 105 108 105 Mean 106 Standard Deviation 1.67 |
| Tibial Component Used for 6 Years | |||
| Sample 1 Sample 2 Sample 3 | 376 378 380 384 380 378 377 388 382 Mean 380 Standard Deviation 3.81 | 125 126 127 128 127 126 126 129 127 Mean 127 Standard Deviation 1.20 | 97 101 102 100 101 102 99 97 101 Mean 100 Standard Deviation 1.94 |
| Tibial Component Used for 12 Years | |||
| Sample 1 | 432 428 431 Mean 430 Standard Deviation 2.52 | 144 142 14 Mean 143 Standard Deviation 1 | 77 77 77 Mean 77 Standard Deviation 0 |
| Unused Tibial Component | |||
| Sample 1 Sample 2 | 397 400 394 407 406 396 Mean 400 Standard Deviation 5.40 | 132 133 131 136 136 131 Mean 133 Standard Deviation 2.25 | 130 129 122 125 127 123 Mean 126 Standard Deviation 3.22 |
| Femoral Component Used for 6 Years | |||
| Sample 1 Sample 2 Sample 3 | 411 406 405 411 416 415 407 411 411 Mean 410 Standard Deviation 3.77 | 137 135 135 137 139 138 135 137 137 Mean 137 Standard Deviation 1.41 | 120 128 131 124 122 121 123 118 121 Mean 123 Standard Deviation 4.07 |
| Femoral Component Used for 12 Years | |||
| Sample 1 | 437 444 438 Mean 440 Standard Deviation 3.78 | 145 148 146 Mean 147 Standard Deviation 1.15 | 100 96 98 Mean 98 Standard Deviation 2 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szarek, A.; Stradomski, G.; Łukomska-Szarek, J.; Rydz, D.; Wolański, W.; Joszko, K. Wear Morphology on the Surfaces of CoCrMo Unicompartmental Knee Joint Endoprostheses as Elements of Metal–Metal Friction Nodes. Materials 2020, 13, 2689. https://doi.org/10.3390/ma13122689
Szarek A, Stradomski G, Łukomska-Szarek J, Rydz D, Wolański W, Joszko K. Wear Morphology on the Surfaces of CoCrMo Unicompartmental Knee Joint Endoprostheses as Elements of Metal–Metal Friction Nodes. Materials. 2020; 13(12):2689. https://doi.org/10.3390/ma13122689
Chicago/Turabian StyleSzarek, Arkadiusz, Grzegorz Stradomski, Justyna Łukomska-Szarek, Dariusz Rydz, Wojciech Wolański, and Kamil Joszko. 2020. "Wear Morphology on the Surfaces of CoCrMo Unicompartmental Knee Joint Endoprostheses as Elements of Metal–Metal Friction Nodes" Materials 13, no. 12: 2689. https://doi.org/10.3390/ma13122689
APA StyleSzarek, A., Stradomski, G., Łukomska-Szarek, J., Rydz, D., Wolański, W., & Joszko, K. (2020). Wear Morphology on the Surfaces of CoCrMo Unicompartmental Knee Joint Endoprostheses as Elements of Metal–Metal Friction Nodes. Materials, 13(12), 2689. https://doi.org/10.3390/ma13122689