A Multi-Element-Doped Porous Bioactive Glass Coating for Implant Applications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Surface Pretreatment of Titanium Discs
2.3. Preparation of 58S and Doped Porous Bioactive Glass Coatings
2.4. Characterization of the Bioactive Glass Coatings
2.5. Surface Nanohardness Test
2.6. In Vitro Coating Degradation Test
2.7. In Vitro Bioactivity Test
2.8. Cell Cytotoxicity Assay
2.9. Antibacterial Test
2.10. Statistical Analysis
3. Results
3.1. Bioactive Glass Coating Characterization
3.2. Nanohardness of the Bioactive Glass Coatings
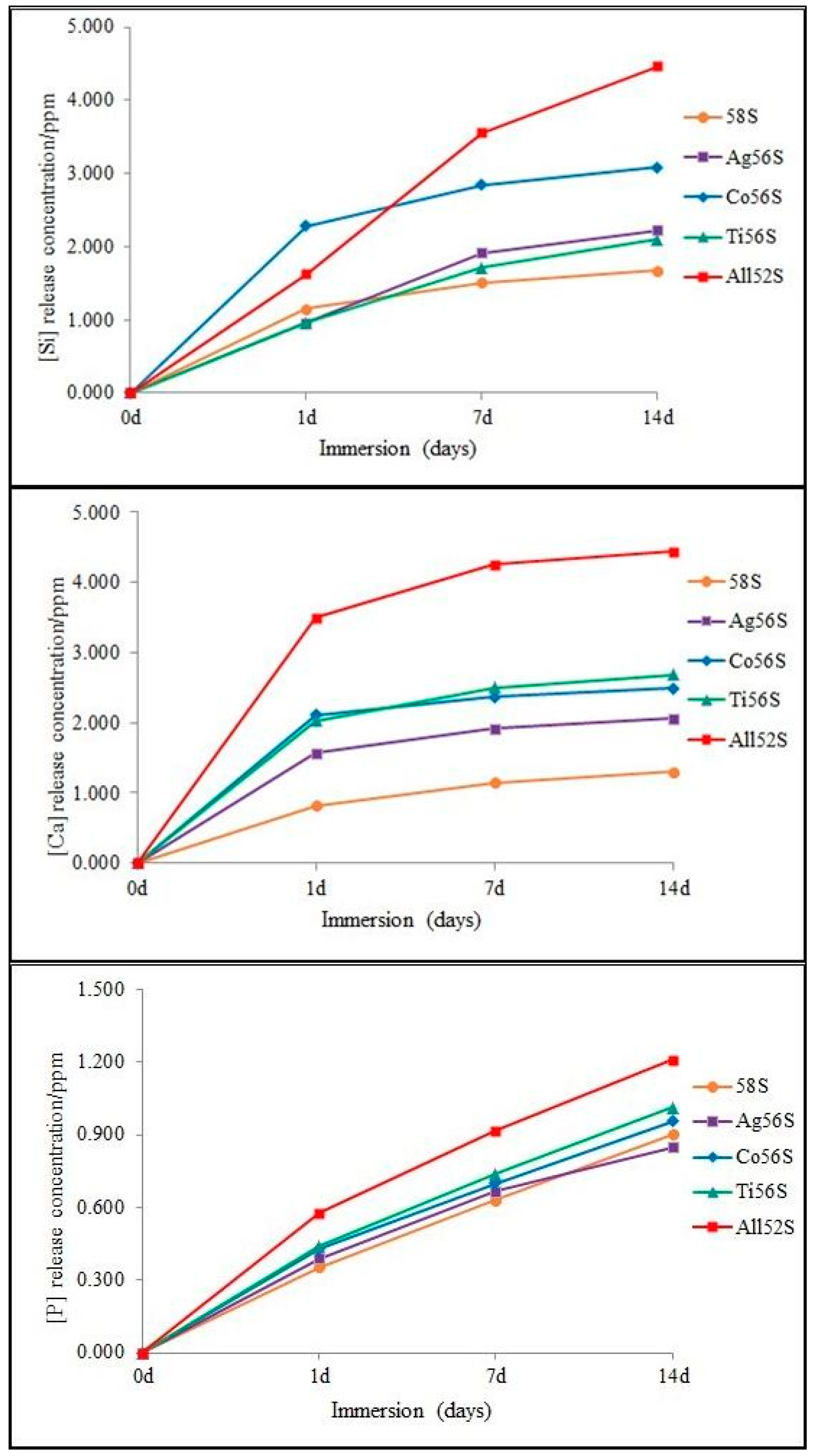
3.3. Degradation Test
3.4. In Vitro Bioactivity Test
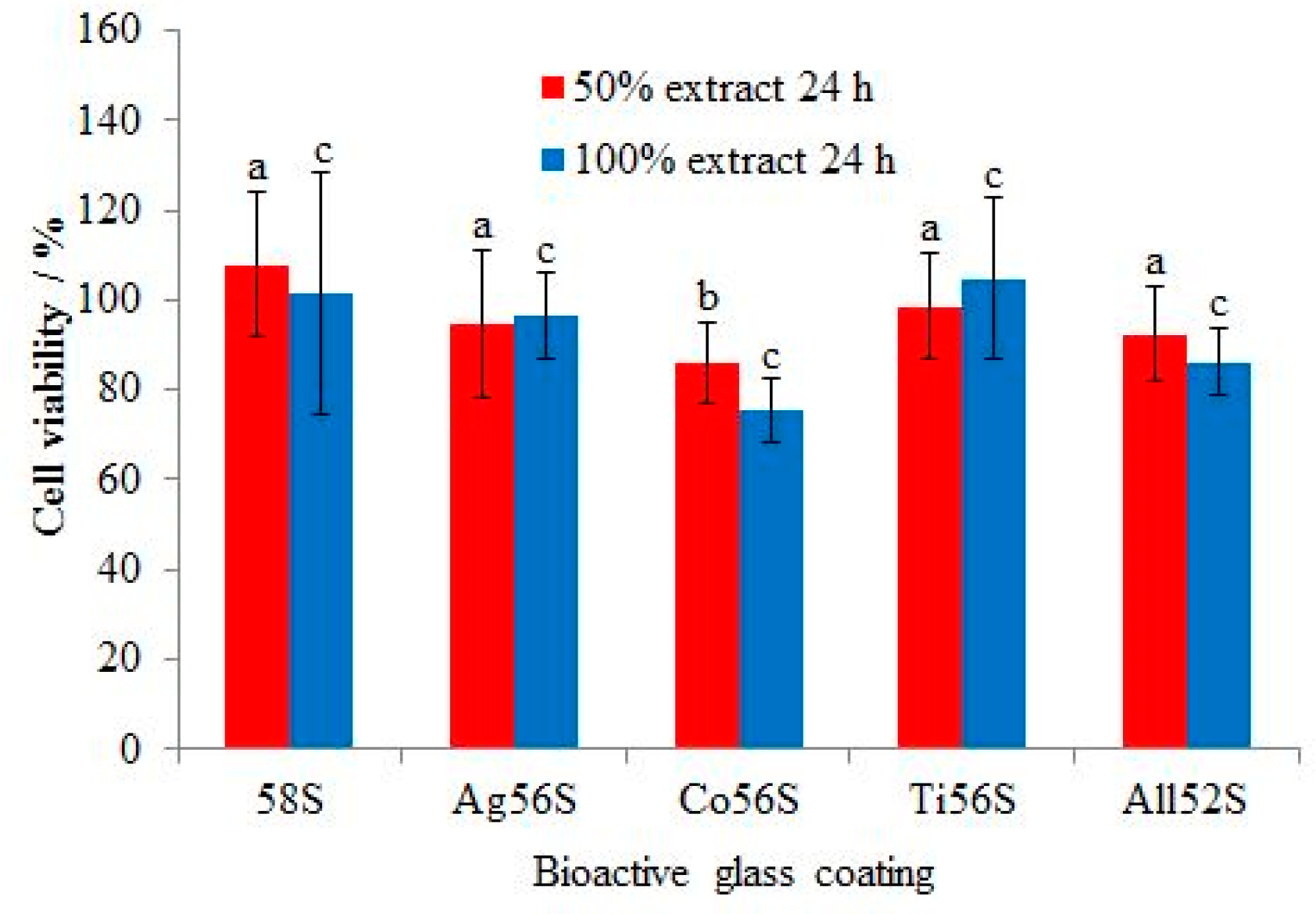
3.5. Cell Cytotoxicity Test
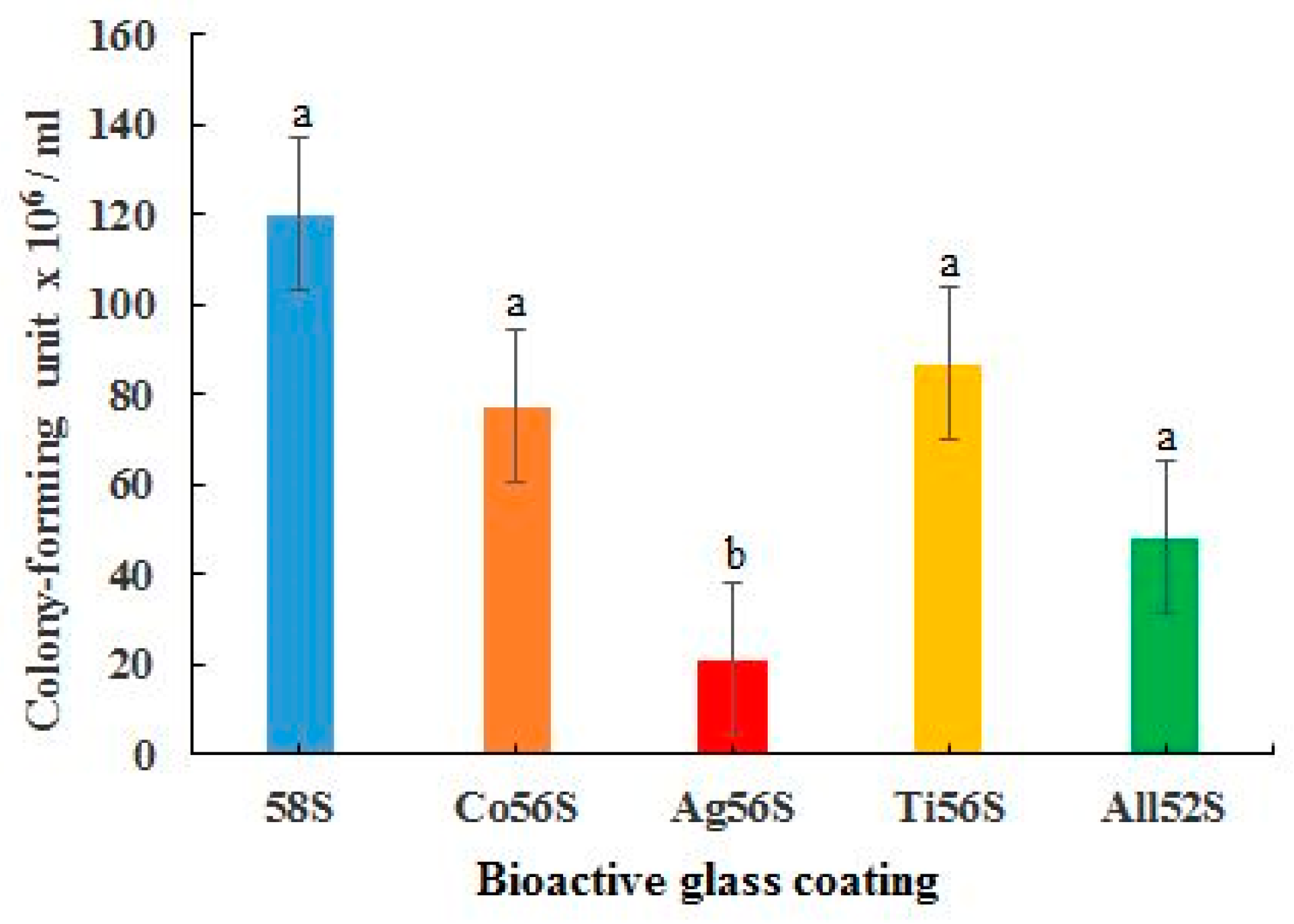
3.6. Antibacterial Test
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Lang, N.P.; Matinlinna, J.P. Titanium in implant dentistry. In Handbook of Oral Biomaterials; Matinlinna, J.P., Ed.; Pan Stanford Publishing: Singapore, 2014; pp. 339–358. [Google Scholar]
- Guo, C.Y.; Tang, A.T.H.; Matinlinna, J.P. Insights into surface treatment methods of titanium dental implants. J. Adhes. Sci. Technol. 2012, 26, 189–205. [Google Scholar]
- Marenzi, G.; Impero, F.; Scherillo, F.; Sammartino, J.C.; Squillace, A.; Spagnuolo, G. Effect of different surface treatments on titanium dental implant micro-morphology. Materials 2019, 12, 733. [Google Scholar] [CrossRef] [Green Version]
- An, Y.Z.; Lee, J.H.; Heo, Y.K.; Lee, J.S.; Jung, U.W.; Choi, S.H. Surgical treatment of severe peri-implantitis using a round titanium brush for implant surface decontamination: A case report with clinical reentry. J. Oral Implant. 2017, 43, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Yoda, I.; Koseki, H.; Tomita, M.; Shida, T.; Horiuchi, H.; Sakoda, H.; Osaki, M. Effect of surface roughness of biomaterials on Staphylococcus epidermidis adhesion. BMC Microbiol. 2014, 14, 234. [Google Scholar] [CrossRef] [Green Version]
- Hupa, L.; Fagerlund, S. Bioactive glasses. In Handbook of oral Biomaterials; Matinlinna, J.P., Ed.; Pan Stanford Publishing: Singapore, 2014; pp. 281–316. [Google Scholar]
- Baino, F.; Hamzehlou, S.; Kargozar, S. Bioactive glasses: Where are we and where are we going? J. Funct. Biomater. 2018, 9, 25. [Google Scholar] [CrossRef] [Green Version]
- Gao, C.; Liu, T.; Shuai, C.; Peng, S. Enhancement mechanisms of graphene in nano-58S bioactive glass scaffold: Mechanical and biological performance. Sci. Rep. 2014, 4, 4712. [Google Scholar] [CrossRef]
- Ignjatovic, N.; Ajduković, Z.; Rajković, J.; Najman, S.; Mihailović, D.; Uskoković, D. Enhanced osteogenesis of nanosized cobalt-substituted hydroxyapatite. J. Bionic. Eng. 2015, 12, 604–612. [Google Scholar] [CrossRef]
- Fan, W.; Crawford, R.; Xiao, Y. Enhancing in vivo vascularized bone formation by cobalt chloride-treated bone marrow stromal cells in a tissue engineered periosteum model. Biomaterials 2010, 31, 3580–3589. [Google Scholar] [CrossRef] [Green Version]
- Heidaria, S.; Hooshmand, T.; Yekta, B.E.; Tarlani, A.; Noshiri, N.; Tahriri, M. Effect of addition of titanium on structural, mechanical and biological properties of 45S5 glass-ceramic. Ceram. Int. 2018, 44, 11682–11692. [Google Scholar] [CrossRef]
- Gold, K.; Slay, B.; Knackstedt, M.; Gaharwar, A.K. Antimicrobial activity of metal and metal-oxide based nanoparticles. Adv. 2018, 1, 1700033. [Google Scholar] [CrossRef]
- Zhao, X.S.; Su, F.; Yan, Q.; Guo, W.; Bao, X.Y.; Lv, L.; Zhou, Z. Templating methods for preparation of porous structures. J. Mater. Chem. 2006, 16, 637–648. [Google Scholar] [CrossRef]
- Mour, M.; Das, D.; Winkler, T.; Hoenig, E.; Mielke, G.; Morlock, M.M.; Schilling, A.F. Advances in porous biomaterials for dental and orthopaedic applications. Materials 2010, 3, 2947–2974. [Google Scholar] [CrossRef] [Green Version]
- de Souza, G.B.; Lepienski, C.M.; Foerster, C.E.; Kuromoto, N.K.; Soares, P.; de Araújo Ponte, H. Nanomechanical and nanotribological properties of bioactive titanium surfaces prepared by alkali treatment. J. Mech. Behav. Biomed. Mater. 2011, 4, 756–765. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Qu, F.; Li, W.; Lin, H.; Jin, Y. Synthesis of hierarchically porous bioactive glasses using natural plants as template for bone tissue regeneration. J. Sol. Gel. Sci. Technol. 2012, 63, 416–424. [Google Scholar] [CrossRef] [Green Version]
- Alvarado-Rivera, J.; Munoz-Saldana, J.; Ramirez-Bon, R. Nanoindentation testing of SiO2-PMMA hybrid films on acrylic substrates with variable coupling agent content. J. Sol. Gel. Sci. Technol. 2010, 54, 312–318. [Google Scholar] [CrossRef]
- Ni, S.; Du, R.; Ni, S. The Influence of Na and Ti on the in vitro degradation and bioactivity in 58S sol-gel bioactive glass. Adv. Mater. Sci. Eng. 2012, 2012, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Omar, S.A.; Ballarre, J.; Castro, Y.; Campos, E.M.; Schreiner, W.; Duran, A.; Cere, S.M. 58S and 68S sol-gel glass-like bioactive coatings for enhancing the implant performance of AZ91D magnesium alloy. Surf. Coat. Technol. 2020, 400, 126224. [Google Scholar] [CrossRef]
- Das, I.; De, G.; Hupa, L.; Vallittu, P.K. Porous SiO2 nanofiber grafted novel bioactive glass-ceramic coating: A structural scaffold for uniform apatite precipitation and oriented cell proliferation on inert implant. Mater. Sci. Eng. C 2016, 62, 206–214. [Google Scholar] [CrossRef]
- Abdalla, M.M.; Lung, C.Y.; Neelakantan, P.; Matinlinna, J.P. A novel, doped calcium silicate bioceramic synthesized by sol–gel method: Investigation of setting time and biological properties. J. Biomed. Mater. Res. B Appl. Biomater. 2020, 108, 56–66. [Google Scholar] [CrossRef]
- International Organization for Standardization. ISO 10993-5. Biological Evaluation of Medical Devices—Part 5. Tests for In Vitro Cytotoxicity; ISO: Geneva, Switzerland, 2009. [Google Scholar]
- Cordero, H.P.; Cid, R.C.; Dosque, M.D.; Ibacache, R.C.; Fluxá, P.P. Li-doped bioglass® 45S5 for potential treatment of prevalent oral diseases. J. Dent. 2020, 29, 103575. [Google Scholar]
- Chan, Y.H. Biostatistics 102: Quantitative Data—Parametric & non-parametric tests. Singap. Med. J. 2003, 44, 391–396. [Google Scholar]
- Rabieea, S.M.; Nazparvar, N.; Azizian, M.; Vashaee, D.; Tayebi, L. Effect of ion substitution on properties of bioactive glasses: A review. Ceram. Int. 2015, 41, 7241–7251. [Google Scholar] [CrossRef]
- Nishiguchi, S.; Fujibayashi, S.; Kim, H.M.; Kokubo, T.; Nakamura, T. Biology of alkali- and heat-treated titanium implants. J. Mater. Sci. Res. Part A 2003, 67, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Cai, S.; Dou, Y.; Xu, G.; Huang, K.; Ren, M.; Wang, X. Bioactive glass–ceramic coating for enhancing the in vitro corrosion resistance of biodegradable Mg alloy. Appl. Surf. Sci. 2012, 259, 799–805. [Google Scholar] [CrossRef]
- El Sawy, A.A.; Shaarawy, M.A. Evaluation of metal ion release from Ti6Al4V and Co-Cr-Mo casting alloys: In vivo and in vitro study. J. Prosthodont. 2014, 23, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, H.R.; Gaddam, A.; Rebelo, A.; Brazete, D.; Stan, G.E.; Ferreira, J.M.F. Bioactive glasses and glass-ceramics for healthcare applications in bone regeneration and tissue engineering. Materials 2018, 11, 2530. [Google Scholar] [CrossRef] [Green Version]
- Brunello, G.; Elsayed, H.; Biasetto, L. Bioactive glass and silicate-based ceramic coatings on metallic implants: Open challenge or outdated topic? Materials 2019, 12, 2929. [Google Scholar] [CrossRef] [Green Version]
- Jamroz, E.; Kulawik, P.; Kopel, P. The effect of nanofillers on the functional properties of biopolymer-based films: A review. Polymers 2019, 11, 675. [Google Scholar] [CrossRef] [Green Version]
- Srivastava, A.K.; Ram, P. Characterization of ZnO substituted 45S5 bioactive glasses and glass—Ceramics. J. Mater. Sci. Res. 2012, 1, 202–220. [Google Scholar] [CrossRef] [Green Version]
- Nandi, S.K.; Mahato, A.; Kundu, B.; Mukherjee, P.; Zorzi, A.R. Doped bioactive glass materials in bone regeneration. In Advanced Techniques in Bone Regeneration 2016; de Miranda, J.B., Ed.; Intech Open: London, UK, 2016; pp. 285–286. [Google Scholar] [CrossRef] [Green Version]
- Hong, W.; Guo, F.; Hu, L.; Wang, X.; Xing, C.; Tan, Y.; Zhao, X.; Xiao, P. A hierarchically porous bioactive glass-ceramic microsphere with enhanced bioactivity for bone tissue engineering. Ceram. Int. 2019, 45, 13579–13583. [Google Scholar] [CrossRef]
- Kokubo, T.; Takadama, H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials 2006, 27, 2907–2915. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.R. Review of bioactive glass: From Hench to hybrids. Acta Biomater. 2013, 9, 4457–4486. [Google Scholar] [CrossRef] [PubMed]
- Bejarano, J.; Caviedes, P.; Palza, H. Sol–gel synthesis and in vitro bioactivity of copper and zinc-doped silicate bioactive glasses and glass-ceramics. Biomed. Mater. 2015, 10, 5001. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fleury, C.; Petit, A.; Mwale, F.; Antoniou, J.; Zukor, D.J.; Tabrizian, M.; Huk, O.L. Effect of cobalt and chromium ions on human MG-63 osteoblasts in vitro: Morphology, cytotoxicity, and oxidative stress. Biomaterials 2006, 27, 3351–3360. [Google Scholar] [CrossRef]
- Chattopadhyay, S.; Dash, S.K.; Tripathy, S.; Das, B.; Mandal, D.; Pramanik, P.; Roy, S. Toxicity of cobalt oxide nanoparticles to normal cells; an in vitro and in vivo study. Chem. Biol. Interact. 2015, 226, 58–71. [Google Scholar] [CrossRef]
- Yin, I.X.; Zhang, J.; Zhao, I.S.; Mei, M.L.; Li, Q.; Chu, C.H. The antibacterial mechanism of silver nanoparticles and its application in dentistry. Int. J. Nanomed. 2020, 15, 2555–2562. [Google Scholar] [CrossRef] [Green Version]
- Raghunath, A.; Perumal, E. Metal oxide nanoparticles as antimicrobial agents: A promise for the future. Int. J. Antimicrob. Agents 2017, 49, 137–152. [Google Scholar] [CrossRef] [PubMed]
- Subbiahdoss, G.; Kuijer, R.; Grijpma, D.W.; van der Mei, H.C.; Busscher, H.J. Microbial biofilm growth vs. tissue integration: ‘‘The race for the surface” experimentally studied. Acta Biomater. 2009, 5, 1399–1404. [Google Scholar] [CrossRef] [PubMed]
- Aranya, A.K.; Pushalkar, S.; Zhao, M.; LeGeros, R.Z.; Zhang, Y.; Saxena, D. Antibacterial and bioactive coatings on titanium implant surfaces. J. Biomed. Mater. Res. Part A 2017, 105, 2218–2227. [Google Scholar] [CrossRef] [Green Version]


| Bioactive Glass Formulation | Chemical Composition/mol% | ||||
|---|---|---|---|---|---|
| SiO2 | CaO | P2O5 | TiO2 | CoO | |
| 58S | 58 | 37 | 5 | 0 | 0 |
| Ag56S | 56 | 37 | 5 | 0 | 0 |
| Co56S | 56 | 37 | 5 | 0 | 2 |
| Ti56S | 56 | 37 | 5 | 2 | 0 |
| All52S | 52 | 37 | 5 | 2 | 2 |
| Bioactive Glass Group | Mean Nanohardness ± SD/MPa |
|---|---|
| 58S | 49.99 ± 17.37 a |
| Ag56S | 118.71 ± 19.1 b |
| Co56S | 107.18 ± 8.29 b |
| Ti56S | 139.66 ± 49.52 b |
| All52S | 124.44 ± 24.7 b |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lung, C.Y.K.; Abdalla, M.M.; Chu, C.H.; Yin, I.; Got, S.-R.; Matinlinna, J.P. A Multi-Element-Doped Porous Bioactive Glass Coating for Implant Applications. Materials 2021, 14, 961. https://doi.org/10.3390/ma14040961
Lung CYK, Abdalla MM, Chu CH, Yin I, Got S-R, Matinlinna JP. A Multi-Element-Doped Porous Bioactive Glass Coating for Implant Applications. Materials. 2021; 14(4):961. https://doi.org/10.3390/ma14040961
Chicago/Turabian StyleLung, Christie Y. K., Mohamed M. Abdalla, Chun Hung Chu, Iris Yin, Sofiya-Roksolana Got, and Jukka P. Matinlinna. 2021. "A Multi-Element-Doped Porous Bioactive Glass Coating for Implant Applications" Materials 14, no. 4: 961. https://doi.org/10.3390/ma14040961
APA StyleLung, C. Y. K., Abdalla, M. M., Chu, C. H., Yin, I., Got, S.-R., & Matinlinna, J. P. (2021). A Multi-Element-Doped Porous Bioactive Glass Coating for Implant Applications. Materials, 14(4), 961. https://doi.org/10.3390/ma14040961







