Material Extrusion Based Fabrication of Surgical Implant Template and Accuracy Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Acquisition
2.2. Implant Planning and Guide Design
2.3. Guide Template Fabrication
2.4. Accuracy Measurements
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Venskutonis, T.; Plotino, G.; Juodzbalys, G.; Mickevieiene, L. The importance of cone-beam computed tomography in the management of endodontic problems: A review of the literature. J. Endodont. 2014, 40, 1895–1901. [Google Scholar] [CrossRef] [PubMed]
- Cunha, R.M.; Souza, F.A.; Hadad, H.; Poli, P.P.; Maiorana, C.; Carvalho, P. Accuracy evaluation of computer-guided implant surgery associated with prototyped surgical guides. J. Prosthet. Dent. 2021, 125, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Sanna, A.M.; Molly, L.; van Steenberghe, D. Immediately loaded cad-cam manufactured fixed complete dentures using flapless implant placement procedures: A cohort study of consecutive patients. J. Prosthet. Dent. 2007, 97, 331–339. [Google Scholar] [CrossRef]
- Vasak, C.; Strbac, G.D.; Huber, C.D.; Lettner, S.; Gahleitner, A.; Zechner, W. Evaluation of three different validation procedures regarding the accuracy of template-guided implant placement: An in vitro study. Clin. Implant Dent. Relat. Res. 2015, 17, 142–149. [Google Scholar] [CrossRef]
- Matta, R.; Bergauer, B.; Adler, W.; Wichmann, M.; Nickenig, H. The impact of the fabrication method on the three-dimensional accuracy of an implant surgery template. J. Cranio Maxill. Surg. 2017, 45, 804–808. [Google Scholar] [CrossRef]
- Herschdorfer, L.; Negreiros, W.M.; Gallucci, G.O.; Hamilton, A. Comparison of the accuracy of implants placed with cad-cam surgical templates manufactured with various 3d printers: An in vitro study. J. Prosthet. Dent. 2021, 125, 905–910. [Google Scholar] [CrossRef]
- Assche, N.V.; Steenberghe, D.V.; Guerrero, M.E.; Hirsch, E.; Jacobs, R. Accuracy of implant placement based on pre-surgical planning of three-dimensional cone-beam images: A pilot study. J. Clin. Periodontol. 2007, 34, 816–821. [Google Scholar] [CrossRef]
- Fang, Y.; An, X.; Jeong, S.M.; Choi, B.H. Accuracy of computer-guided implant placement in anterior regions. J. Prosthet. Dent. 2019, 121, 836–842. [Google Scholar] [CrossRef]
- Bover-Ramos, F.; Vina-Almunia, J.; Cervera-Ballester, J.; Penarrocha-Diago, M.; Garcia-Mira, B. Accuracy of implant placement with computer-guided surgery: A systematic review and meta-analysis comparing cadaver, clinical, and in vitro studies. Int. J. Oral Maxillofac. Implant. 2018, 33, 101–115. [Google Scholar] [CrossRef]
- Wagner, M.A.; Hadian, A.; Sebastian, T.; Clemens, F.; Schweizer, T.; Rodriguez-Arbaizar, M.; Carreño-Morelli, E.; Spolenak, R. Fused filament fabrication of stainless steel structures—From binder development to sintered properties. Addit. Manuf. 2021, 49, 102472. [Google Scholar] [CrossRef]
- Wang, H.; Masood, S.; Iovenitti, P.; Harvey, E.C. Application of Fused Deposition Modeling Rapid Prototyping System to the Development of Microchannels; SPIE: Bellingham, WA, USA, 2001. [Google Scholar]
- Singh, S.; Singh, G.; Prakash, C.; Ramakrishna, S. Current status and future directions of fused filament fabrication. J. Manuf. Process. 2020, 55, 288–306. [Google Scholar] [CrossRef]
- Zhang, B.; Wang, L.; Song, P.; Pei, X.; Sun, H.; Wu, L.; Zhou, C.; Wang, K.; Fan, Y.; Zhang, X. 3d printed bone tissue regenerative pla/ha scaffolds with comprehensive performance optimizations. Mater. Des. 2021, 201, 109490. [Google Scholar] [CrossRef]
- Baro, M.; Sánchez, E.; Delgado, A.; Perera, A.; Évora, C. In vitro-in vivo characterization of gentamicin bone implants. J. Control. Release 2002, 83, 353–364. [Google Scholar] [CrossRef]
- Pugliese, R.; Beltrami, B.; Regondi, S.; Lunetta, C. Polymeric biomaterials for 3d printing in medicine: An overview. Ann. 3D Print. Med. 2021, 2, 100011. [Google Scholar] [CrossRef]
- Narayanan, G.; Vernekar, V.N.; Kuyinu, E.L.; Laurencin, C.T. Poly (lactic acid)-based biomaterials for orthopaedic regenerative engineering. Adv. Drug Deliv. Rev. 2016, 107, 247–276. [Google Scholar] [CrossRef]
- Serra, T.; Planell, J.A.; Navarro, M. High-resolution pla-based composite scaffolds via 3-d printing technology. Acta Biomater. 2013, 9, 5521–5530. [Google Scholar] [CrossRef]
- Afonso, J.A.; Alves, J.L.; Caldas, G.; Gouveia, B.P.; Santana, L.; Belinha, J. Influence of 3d printing process parameters on the mechanical properties and mass of pla parts and predictive models. Rapid Prototyp. J. 2021, 27, 487–495. [Google Scholar] [CrossRef]
- Mishra, P.K.; Ponnusamy, S.; Nallamilli, M.S.R. The influence of process parameters on the impact resistance of 3d printed pla specimens under water-absorption and heat-treated conditions. Rapid Prototyp. J. 2021, 27, 1108–1123. [Google Scholar] [CrossRef]
- von Windheim, N.; Collinson, D.W.; Lau, T.; Brinson, L.C.; Gall, K. The influence of porosity, crystallinity and interlayer adhesion on the tensile strength of 3d printed polylactic acid (pla). Rapid Prototyp. J. 2021, 27, 1327–1336. [Google Scholar] [CrossRef]
- Pettersson, A.; Komiyama, A.; Hultin, M.; Näsström, K.; Klinge, B. Accuracy of virtually planned and template guided implant surgery on edentate patients. Clin. Implant. Dent. Relat. Res 2012, 14, 527–537. [Google Scholar] [CrossRef] [Green Version]
- Zimmermann, M.; Ender, A.; Mehl, A. Local accuracy of actual intraoral scanning systems for single-tooth preparations in vitro. J. Am. Dent. Assoc. 2020, 151, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Ding, Q.; Tang, L.; Zhang, L.; Sun, Y.; Xie, Q. Accuracy of a chairside fused deposition modeling 3d-printed single-tooth surgical template for implant placement: An in vitro comparison with a light cured template. J. Cranio Maxill. Surg. 2019, 47, 1216–1221. [Google Scholar] [CrossRef] [PubMed]
- Widmann, G.; Berggren, J.P.M.; Fischer, B.; Pichler-Dennhardt, A.R.; Schullian, P.; Bale, R.; Puelacher, W. Accuracy of image-fusion stereolithographic guides: Mapping ct data with three-dimensional optical surface scanning. Clin. Implant. Dent. Relat. Res 2015, 17, e736–e744. [Google Scholar] [CrossRef] [PubMed]
- Molinero-Mourelle, P.; Canals, S.; Gómez-Polo, M.; Solá-Ruiz, M.F.; Highsmith, J.R.; Viñuela, A.C. Polylactic acid as a material for three-dimensional printing of provisional restorations. Int. J. Prosthodont. 2018, 31, 349–350. [Google Scholar] [CrossRef] [PubMed]
- Hultin, M.; Svensson, K.G.; Trulsson, M. Clinical advantages of computer-guided implant placement: A systematic review. Clin. Oral Implan. Res. 2012, 23, 124–135. [Google Scholar] [CrossRef]
- Sharafi, S.; Santare, M.H.; Gerdes, J.; Advani, S.G. A review of factors that influence the fracture toughness of extrusion-based additively manufactured polymer and polymer composites. Addit. Manuf. 2021, 38, 101830. [Google Scholar] [CrossRef]
- Yeung, M.; Abdulmajeed, A.; Carrico, C.K.; Deeb, G.R.; Bencharit, S. Accuracy and precision of 3d-printed implant surgical guides with different implant systems: An in vitro study. J. Prosthet. Dent. 2020, 123, 821–828. [Google Scholar] [CrossRef]
- Baruffaldi, A.; Poli, P.P.; Baruffaldi, A.; Giberti, L.; Pigozzo, M.; Maiorana, C. Computer-aided flapless implant surgery and immediate loading. A technical note. Oral Maxillofac. Surg. 2016, 20, 313–319. [Google Scholar] [CrossRef]
- Neumeister, A.; Schulz, L.; Glodecki, C. Investigations on the accuracy of 3d-printed drill guides for dental implantology. Int. J. Comput. Dent. 2017, 20, 35–51. [Google Scholar]
- Tan, P.L.; Layton, D.M.; Wise, S.L. In vitro comparison of guided versus freehand implant placement: Use of a new combined trios surface scanning, implant studio, cbct, and stereolithographic virtually planned and guided technique. Int. J. Prosthodont. 2018, 21, 87–95. [Google Scholar]
- George, E.; Liacouras, P.; Rybicki, F.J.; Mitsouras, D. Measuring and establishing the accuracy and reproducibility of 3d printed medical models. Radiographics 2017, 37, 1424–1450. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Yang, X.; Chen, L.; Wang, Y.; Sun, Y. Application of fdm three-dimensional printing technology in the digital manufacture of custom edentulous mandible trays. Sci. Rep.-UK 2016, 6, 19207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Katatny, I.; Masood, S.H.; Morsi, Y.S. Error analysis of fdm fabricated medical replicas. Rapid Prototyp. J. 2010, 16, 36–43. [Google Scholar] [CrossRef]
- Assche, N.V.; Vercruyssen, M.; Coucke, W.; Teughels, W.; Jacobs, R.; Quirynen, M. Accuracy of computer-aided implant placement. Clin. Oral Implan. Res. 2012, 23, 112–123. [Google Scholar] [CrossRef]
- Cushen, S.E.; Turkyilmaz, I. Turkyilmaz, Impact of operator experience on the accuracy of implant placement with stereolithographic surgical templates: An in vitro study. J. Prosthet. Dent. 2013, 109, 248–254. [Google Scholar] [CrossRef]
- Szymor, P.; Kozakiewicz, M.; Olszewski, R. Accuracy of open-source software segmentation and paper-based printed three-dimensional models. J. Cranio-Maxillo-Facial Surg. 2016, 44, 202–209. [Google Scholar] [CrossRef]
- Kim, T.; Lee, S.; Kim, G.B.; Hong, D.; Kwon, J.; Park, J.-W.; Kim, N. Accuracy of a simplified 3d-printed implant surgical guide. J. Prosthet. Dent. 2020, 124, 195–201.e2. [Google Scholar] [CrossRef]
- Deeb, G.R.; Allen, R.K.; Hall, V.P.; Whitley, D.; Laskin, D.M.; Bencharit, S. How accurate are implant surgical guides produced with desktop stereolithographic 3-dimentional printers? J. Oral Maxillofac. Surg. 2017, 75, 2559.e1–2559.e8. [Google Scholar] [CrossRef]



| Quality | Fill | Speed and Temperature | Material | |||||
|---|---|---|---|---|---|---|---|---|
| Build Volume (mm) | Layer Thickness (mm) | Nozzle Size (mm) | Bottom/Top Thickness (mm) | Fill Density (%) | Speed (mm/s) | Print Temperature (°C) | Filament Type | Filament Diameter (mm) |
| 120 × 120 × 100 | 0.1 | 0.3 | 0.8 | 100 | 30 | 200 | PLA | 1.75 |
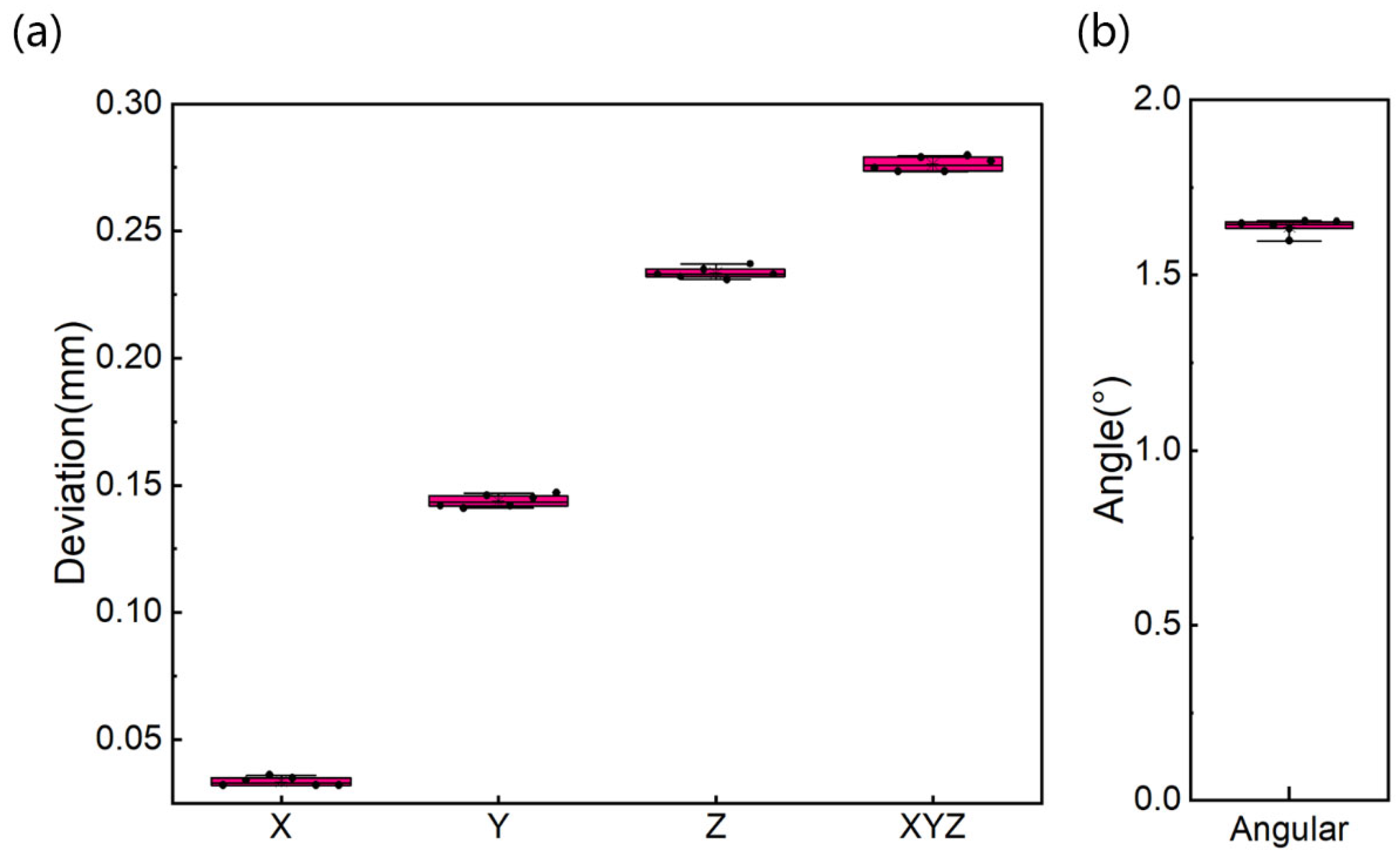
| Min | Max | Mean | SD | CV | |
|---|---|---|---|---|---|
| X (vestibule-oral, mm) | 0.032 | 0.036 | 0.034 | 0.002 | 0.053 |
| Y (mesio-distal, mm) | 0.141 | 0.147 | 0.144 | 0.002 | 0.017 |
| Z (cranio-caudal, mm) | 0.231 | 0.237 | 0.234 | 0.002 | 0.009 |
| dXYZ (mm) | 0.273 | 0.280 | 0.276 | 0.003 | 0.010 |
| Angle (°) | 1.598 | 1.655 | 1.638 | 0.021 | 0.013 |
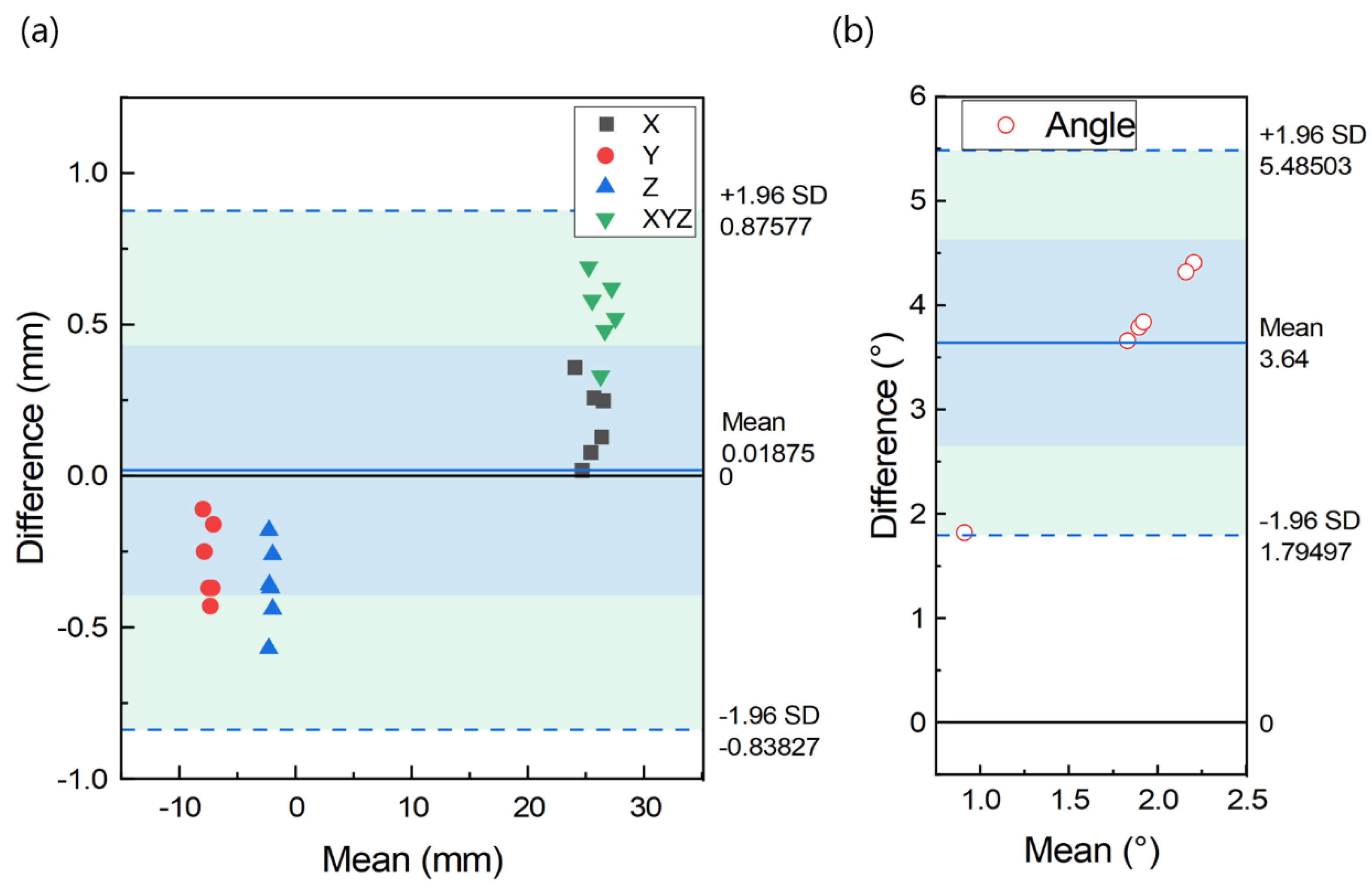
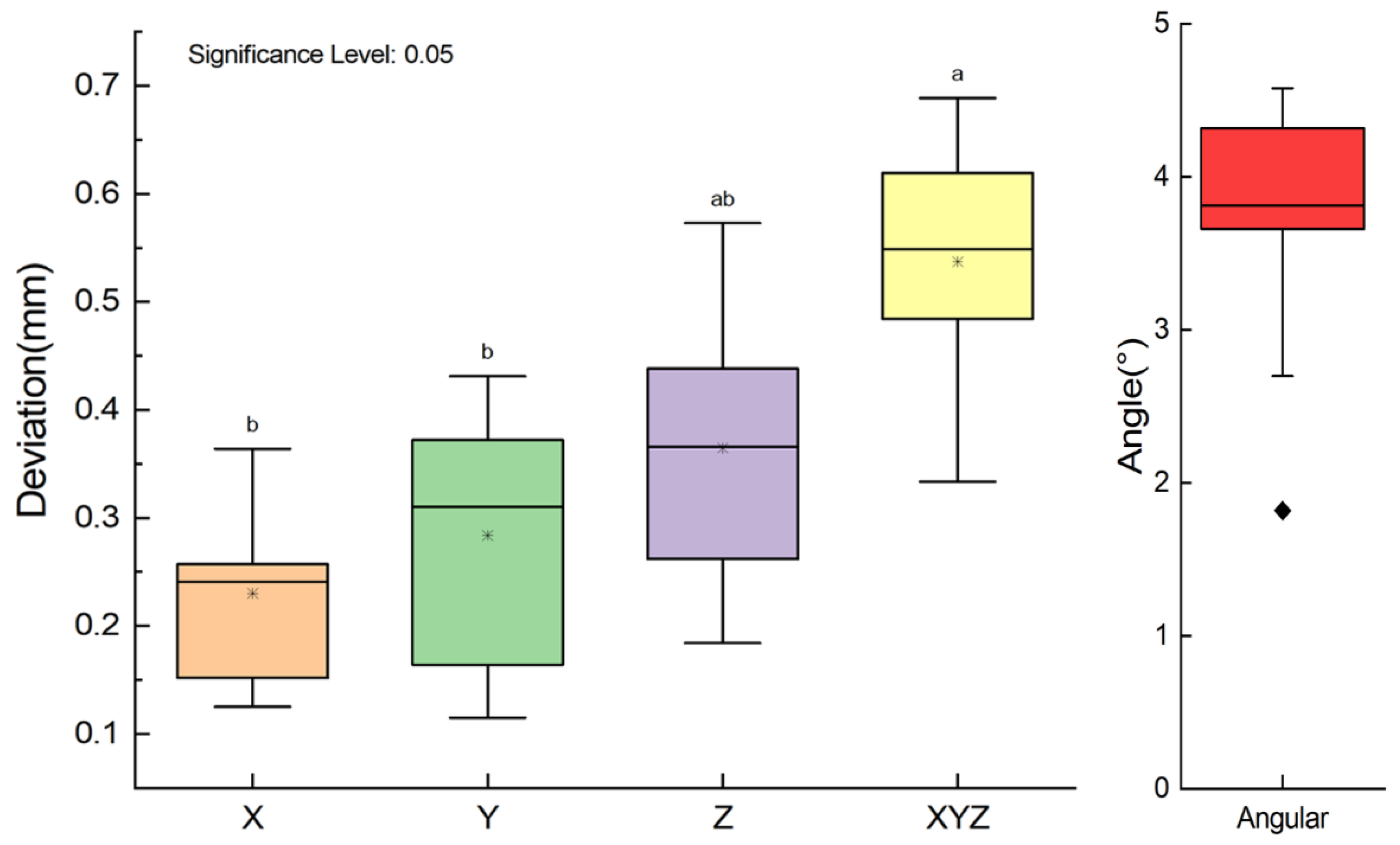
| Min | Max | Mean | SD | |
|---|---|---|---|---|
| X (vestibule-oral, mm) | 0.125 | 0.364 | 0.230 | 0.085 |
| Y (mesio-distal, mm) | 0.115 | 0.431 | 0.284 | 0.127 |
| Z (cranio-caudal, mm) | 0.184 | 0.573 | 0.365 | 0.136 |
| dXYZ (mm) | 0.333 | 0.689 | 0.537 | 0.123 |
| Angle (°) | 1.820 | 4.410 | 3.640 | 0.941 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, C.; Yuan, Y.; Chen, J. Material Extrusion Based Fabrication of Surgical Implant Template and Accuracy Analysis. Materials 2022, 15, 1738. https://doi.org/10.3390/ma15051738
Zhang C, Yuan Y, Chen J. Material Extrusion Based Fabrication of Surgical Implant Template and Accuracy Analysis. Materials. 2022; 15(5):1738. https://doi.org/10.3390/ma15051738
Chicago/Turabian StyleZhang, Chengyu, Yanping Yuan, and Jimin Chen. 2022. "Material Extrusion Based Fabrication of Surgical Implant Template and Accuracy Analysis" Materials 15, no. 5: 1738. https://doi.org/10.3390/ma15051738






