Shear Bond Strength between Orthodontic Brackets and Monolithic 4Y-TZP: An In Vitro Study
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- The shear bond strength (SBS) values between metal orthodontic brackets and monolithic zirconia, modified by different surface treatment methods, ranged from (3.92 ± 1.9) to (7.44 ± 2.9).
- The tribochemical coating group exhibited the highest bond strength (7.44 ± 2.9), which was not statistically different from the grinding (6.15 ± 3.1) or sandblasting (6.47 ± 3.3) groups.
- The bond strength achieved using the nano second fiber laser (4.3 ± 1.4) fell below the acceptable threshold range of 6–8 MPa.
- Additionally, the nano second fiber laser significantly altered the color of the monolithic zirconia specimens.
- The grinding, sandblasting and tribochemical coating techniques demonstrated clinically acceptable bond strength within the range of 6–8 MPa, suggesting their potential suitability for use in clinical practice.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bavbek, N.C.; Roulet, J.-F.; Ozcan, M. Evaluation of microshear bond strength of orthodontic resin cement to monolithic zirconium oxide as a function of surface conditioning method. J. Adhes. Dent. 2014, 16, 473–480. [Google Scholar] [CrossRef]
- Mehmeti, B.; Azizi, B.; Kelmendi, J.; Iljazi-Shahiqi, D.; Alar, Ž.; Anić-Milošević, S. Shear Bond Strength of Orthodontic Brackets Bonded to Zirconium Crowns. Acta Stomatol. Croat. 2017, 51, 99. [Google Scholar] [CrossRef]
- Mokhtarpur, H.; Nafisifard, M.; Dadgar, S.; Etemadi, A.; Chiniforush, N.; Sobouti, F. Shear Bond Strength of the Metal Bracket to Zirconium Ceramic Restoration Treated by the Nd: YAG Laser and Other Methods: An In Vitro Microscopic Study. J. Lasers Med. Sci. 2020, 11, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Elsayed, A.; Meyer, G.; Wille, S.; Kern, M. Influence of the yttrium content on the fracture strength of monolithic zirconia crowns after artificial aging. Quintessence Int. 2019, 50, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Michailova, M.; Elsayed, A.; Fabel, G.; Edelhoff, D.; Zylla, I.M.; Stawarczyk, B. Comparison between novel strength-gradient and color-gradient multilayered zirconia using conventional and high-speed sintering. J. Mech. Behav. Biomed. Mater. 2020, 111, 103977. [Google Scholar] [CrossRef]
- Wiedenmann, F.; Pfefferle, R.; Reichert, A.; Jerman, E.; Stawarczyk, B. Impact of high-speed sintering, layer thickness and artificial aging on the fracture load and two-body wear of zirconia crowns. Dent. Mater. 2020, 36, 846–853. [Google Scholar] [CrossRef] [PubMed]
- Juntavee, N.; Juntavee, A.; Wongnara, K.; Klomklorm, P.; Khechonnan, R. Shear bond strength of ceramic bracket bonded to different surface-treated ceramic materials. J. Clin. Exp. Dent. 2018, 10, e1167. [Google Scholar] [CrossRef] [PubMed]
- Zachrisson, Y.O.; Zachrisson, B.U.; Büyükyilmaz, T. Surface preparation for orthodontic bonding to porcelain. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Const. Soc. Am. Board Orthod. 1996, 109, 420–430. [Google Scholar] [CrossRef] [PubMed]
- Cevik, P.; Eraslan, O.; Eser, K.; Tekeli, S. Shear bond strength of ceramic brackets bonded to surface-treated feldspathic porcelain after thermocycling. Int. J. Artif. Organs 2018, 41, 160–167. [Google Scholar] [CrossRef]
- Jungbauer, R.; Proff, P.; Edelhoff, D.; Stawarczyk, B. Impact of different pretreatments and attachment materials on shear bond strength between monolithic zirconia restorations and metal brackets. Sci. Rep. 2022, 12, 8514. [Google Scholar] [CrossRef]
- Ghozy, E.A.; Shamaa, M.S.; El-Bialy, A.A. In vitro testing of shear bond strength of orthodontic brackets bonded to different novel CAD/CAM ceramics. J. Dent. Res. Dent. Clin. Dent. Prospects 2020, 14, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Altan, B.; Cinar, S.; Tuncelli, B. Evaluation of shear bond strength of zirconia-based monolithic CAD-CAM materials to resin cement after different surface treatments. Niger. J. Clin. Pract. 2019, 22, 1475–1482. [Google Scholar] [CrossRef] [PubMed]
- Fornaini, C.; Poli, F.; Merigo, E.; Brulat-Bouchard, N.; El Gamal, A.; Rocca, J.-P.; Selleri, S.; Cucinotta, A. Disilicate Dental Ceramic Surface Preparation by 1070 nm Fiber Laser: Thermal and Ultrastructural Analysis. Bioengineering 2018, 5, 10. [Google Scholar] [CrossRef] [Green Version]
- Korkmaz, F.M.; Aycan, S. Effect of fiber laser irradiation on the shear bond strength between acrylic resin and titanium. Scanning 2019, 2019, 5452919. [Google Scholar] [CrossRef]
- García-Sanz, V.; Paredes-Gallardo, V.; Bellot-Arcís, C.; Martínez-León, L.; Torres-Mendieta, R.; Montero, J.; Albaladejo, A. Femtosecond laser settings for optimal bracket bonding to zirconia. Lasers Med. Sci. 2019, 34, 297–304. [Google Scholar] [CrossRef]
- Dönmez, M.B.; Ballı Demirel, B.; Demirel, M.; Gündoğdu, Y.; Kılıç, H.Ş. Effect of Different Surface Treatments on the Surface Roughness and Orthodontic Bond Strength of Partially-stabilized Zirconia. Meandros Med. Dent. J. 2022, 23, 335–342. [Google Scholar] [CrossRef]
- Ju, G.-Y.; Lim, B.-S.; Moon, W.; Park, S.-Y.; Oh, S.; Chung, S.H. Primer-Treated Ceramic Bracket Increases Shear Bond Strength on Dental Zirconia Surface. Materials 2020, 13, 4106. [Google Scholar] [CrossRef]
- Kurt, İ.; Çehreli, Z.C.; Özçırpıcı, A.A.; Şar, Ç. Biomechanical evaluation between orthodontic attachment and three different materials after various surface treatments: A three-dimensional optical profilometry analysis. Angle Orthod. 2019, 89, 742–750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alzainal, A.H.; Majud, A.S.; Al-Ani, A.M.; Mageet, A.O. Orthodontic Bonding: Review of the Literature. Int. J. Dent. 2020, 2020, 8874909. [Google Scholar] [CrossRef] [PubMed]
- Francisco, I.; Travassos, R.; Nunes, C.; Ribeiro, M.; Marques, F.; Pereira, F.; Marto, C.M.; Carrilho, E.; Oliveiros, B.; Paula, A.B.; et al. What Is the Most Effective Technique for Bonding Brackets on Ceramic—A Systematic Review and Meta-Analysis. Bioengineering 2022, 9, 14. [Google Scholar] [CrossRef]
- Shamohammadi Heidari, M.; Moradinejad, M.; Tabatabaei, H.; Rakhshan, V. Effects of Three Novel Bracket Luting Agents Containing Zirconia Primer on Shear Bond Strength of Metal Orthodontic Brackets Attached to Monolithic Zirconia Crowns: A Preliminary In Vitro Study. Int. J. Dent. 2022, 2022, 7107526. [Google Scholar] [CrossRef]
- Recen, D.; Yildirim, B.; Othman, E.; Comlekoglu, E.; Aras, I. Bond strength of metal brackets to feldspathic ceramic treated with different surface conditioning methods: An in vitro study. Eur. Oral Res. 2021, 55, 1. [Google Scholar] [CrossRef] [PubMed]
- Bourke, B.M.; Rock, W.P. Factors affecting the shear bond strength of orthodontic brackets to porcelain. Br. J. Orthod. 1999, 26, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Schmage, P.; Nergiz, I.; Herrmann, W.; Ozcan, M. Influence of various surface-conditioning methods on the bond strength of metal brackets to ceramic surfaces. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Const. Soc. Am. Board Orthod. 2003, 123, 540–546. [Google Scholar] [CrossRef] [Green Version]
- Thurmond, J.W.; Barkmeier, W.W.; Wilwerding, T.M. Effect of porcelain surface treatments on bond strengths of composite resin bonded to porcelain. J. Prosthet. Dent. 1994, 72, 355–359. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; Peumans, M.; Poitevin, A.; Mine, A.; Van Ende, A.; Neves, A.; De Munck, J. Relationship between bond-strength tests and clinical outcomes. Dent. Mater. 2010, 26, e100–e121. [Google Scholar] [CrossRef] [PubMed]
- Akyil, M.S.; Uzun, I.H.; Bayindir, F. Bond strength of resin cement to yttrium-stabilized tetragonal zirconia ceramic treated with air abrasion, silica coating, and laser irradiation. Photomed. Laser Surg. 2010, 28, 801–808. [Google Scholar] [CrossRef]
- Abu Alhaija, E.S.J.; Abu AlReesh, I.A.; AlWahadni, A.M.S. Factors affecting the shear bond strength of metal and ceramic brackets bonded to different ceramic surfaces. Eur. J. Orthod. 2010, 32, 274–280. [Google Scholar] [CrossRef]
- Byeon, S.M.; Lee, M.H.; Bae, T.S. Shear Bond Strength of Al2O3 Sandblasted Y-TZP Ceramic to the Orthodontic Metal Bracket. Materials 2017, 10, 148. [Google Scholar] [CrossRef] [Green Version]
- Yang, B.; Barloi, A.; Kern, M. Influence of air-abrasion on zirconia ceramic bonding using an adhesive composite resin. Dent. Mater. 2010, 26, 44–50. [Google Scholar] [CrossRef]
- Tzanakakis, E.-G.C.; Tzoutzas, I.G.; Koidis, P.T. Is there a potential for durable adhesion to zirconia restorations? A systematic review. J. Prosthet. Dent. 2016, 115, 9–19. [Google Scholar] [CrossRef]
- Namvar, F.; Shahrebabak, M.Z.; Arab, S.; Tabrizi, M.A.; Ghasemi, A.; Safari, F. Shear bond strength of metallic orthodontic brackets to zirconium crowns treated by sandblasting compared to enamel using a universal adhesive: An in vitro study. Int. Orthod. 2022, 20, 100640. [Google Scholar] [CrossRef]
- Yi, Y.-A.; Ahn, J.-S.; Park, Y.-J.; Jun, S.-H.; Lee, I.-B.; Cho, B.-H.; Son, H.-H.; Seo, D.-G. The effect of sandblasting and different primers on shear bond strength between yttria-tetragonal zirconia polycrystal ceramic and a self-adhesive resin cement. Oper. Dent. 2015, 40, 63–71. [Google Scholar] [CrossRef]
- Kwon, S.M.; Min, B.K.; Kim, Y.K.; Kwon, T.Y. Influence of Sandblasting Particle Size and Pressure on Resin Bonding Durability to Zirconia: A Residual Stress Study. Materials 2020, 13, 5629. [Google Scholar] [CrossRef]
- Mehta, A.S.; Evans, C.A.; Viana, G.; Bedran-Russo, A.; Galang-Boquiren, M.T.S. Bonding of Metal Orthodontic Attachments to Sandblasted Porcelain and Zirconia Surfaces. Biomed Res. Int. 2016, 2016, 5762785. [Google Scholar] [CrossRef] [Green Version]
- Cevik, P.; Karacam, N.; Eraslan, O.; Sari, Z. Effects of different surface treatments on shear bond strength between ceramic systems and metal brackets. J. Adhes. Sci. Technol. 2017, 31, 1105–1115. [Google Scholar] [CrossRef]
- Cetik, S.; Ha, T.H.; Sitri, L.; Duterme, H.; Pham, V.; Atash, R. Comparison of Shear Strength of Metal and Ceramic Orthodontic Brackets Cemented to Zirconia Depending on Surface Treatment: AnIn VitroStudy. Eur. J. Dent. 2019, 13, 150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amer, J.Y.; Rayyan, M.M. Effect of different surface treatments and bonding modalities on the shear bond strength between metallic orthodontic brackets and glazed monolithic zirconia crowns. J. Orthod. Sci. 2018, 7, 23. [Google Scholar] [CrossRef] [PubMed]
- Pouyanfar, H.; Golshah, A.; Shekarbeigi, M. Shear Bond Strength of Metal and Ceramic Brackets to Composite Using Single Bond and Universal Adhesive. Open Access Maced. J. Med. Sci. 2020, 8, 1–6. [Google Scholar] [CrossRef]
- Elsaka, S.E. Influence of surface treatments on bond strength of metal and ceramic brackets to a novel CAD/CAM hybrid ceramic material. Odontology 2016, 104, 68–76. [Google Scholar] [CrossRef]
- Ates, S.M.; Korkmaz, F.M.; Caglar, I.S.; Duymus, Z.Y.; Turgut, S.; Bagis, E.A. The effect of ultrafast fiber laser application on the bond strength of resin cement to titanium. Lasers Med. Sci. 2017, 32, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Hoy, C.L.; Ferhanoǧlu, O.; Yildirim, M.; Kim, K.H.; Karajanagi, S.S.; Chan, K.M.C.; Kobler, J.B.; Zeitels, S.M.; Ben-Yakar, A. Clinical ultrafast laser surgery: Recent advances and future directions. IEEE J. Sel. Top. Quantum Electron. 2014, 20, 242–255. [Google Scholar] [CrossRef]
- Yin, R.; Lee, M.-H.; Bae, T.-S.; Song, K.-Y. Effect of finishing condition on fracture strength of monolithic zirconia crowns. Dent. Mater. J. 2019, 38, 203–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amaya-Pajares, S.P.; Ritter, A.V.; Vera Resendiz, C.; Henson, B.R.; Culp, L.; Donovan, T.E. Effect of Finishing and Polishing on the Surface Roughness of Four Ceramic Materials after Occlusal Adjustment. J. Esthet. Restor. Dent. Off. Publ. Am. Acad. Esthet. Dent. 2016, 28, 382–396. [Google Scholar] [CrossRef] [PubMed]


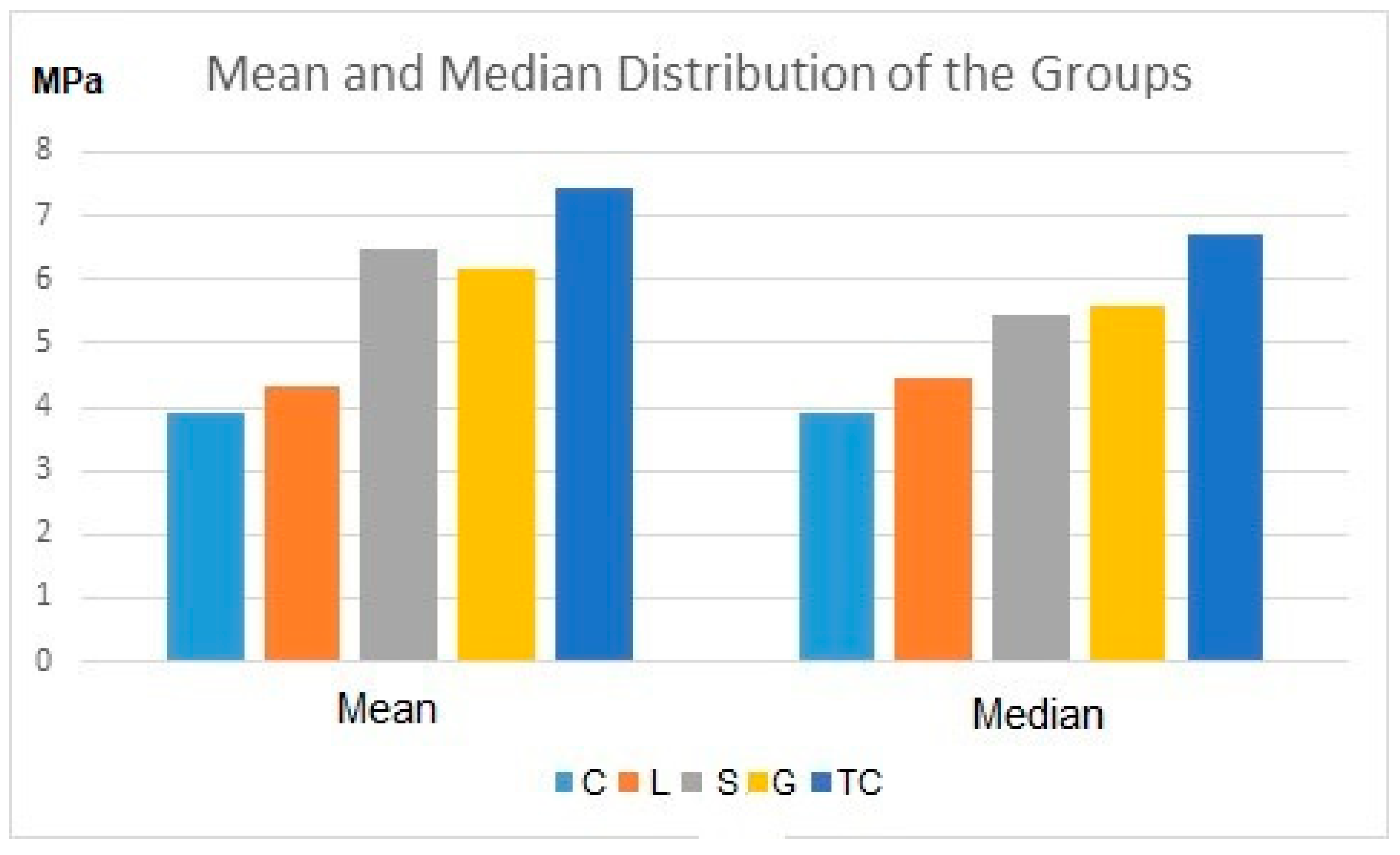
| Control | Nano Second Fiber Laser | Sandblasting | Grinding | Tribochemical Coating | |
|---|---|---|---|---|---|
| N | 10 | 10 | 10 | 10 | 10 |
| Mean | 3.927 a | 4.328 a | 6.477 ac | 6.155 ac | 7.448 c |
| SD | 1.900 | 1.466 | 3.317 | 3.125 | 2.978 |
| Median | 3.929 | 4.448 | 5.450 | 5.599 | 6.700 |
| Minimum | 0.423 | 2.297 | 3.578 | 3.078 | 3.518 |
| Maximum | 6.641 | 6.434 | 15.662 | 15.177 | 13.789 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cakir, E.; Duman, A.N.; Yildirim, A.Z.; Cevik, P. Shear Bond Strength between Orthodontic Brackets and Monolithic 4Y-TZP: An In Vitro Study. Materials 2023, 16, 5173. https://doi.org/10.3390/ma16145173
Cakir E, Duman AN, Yildirim AZ, Cevik P. Shear Bond Strength between Orthodontic Brackets and Monolithic 4Y-TZP: An In Vitro Study. Materials. 2023; 16(14):5173. https://doi.org/10.3390/ma16145173
Chicago/Turabian StyleCakir, Emre, Ayse Nurcan Duman, Arzu Zeynep Yildirim, and Pinar Cevik. 2023. "Shear Bond Strength between Orthodontic Brackets and Monolithic 4Y-TZP: An In Vitro Study" Materials 16, no. 14: 5173. https://doi.org/10.3390/ma16145173
APA StyleCakir, E., Duman, A. N., Yildirim, A. Z., & Cevik, P. (2023). Shear Bond Strength between Orthodontic Brackets and Monolithic 4Y-TZP: An In Vitro Study. Materials, 16(14), 5173. https://doi.org/10.3390/ma16145173







