Formulation and Characterization of New Experimental Dental Composites with Zirconium Filling in Different Forms
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Characterization
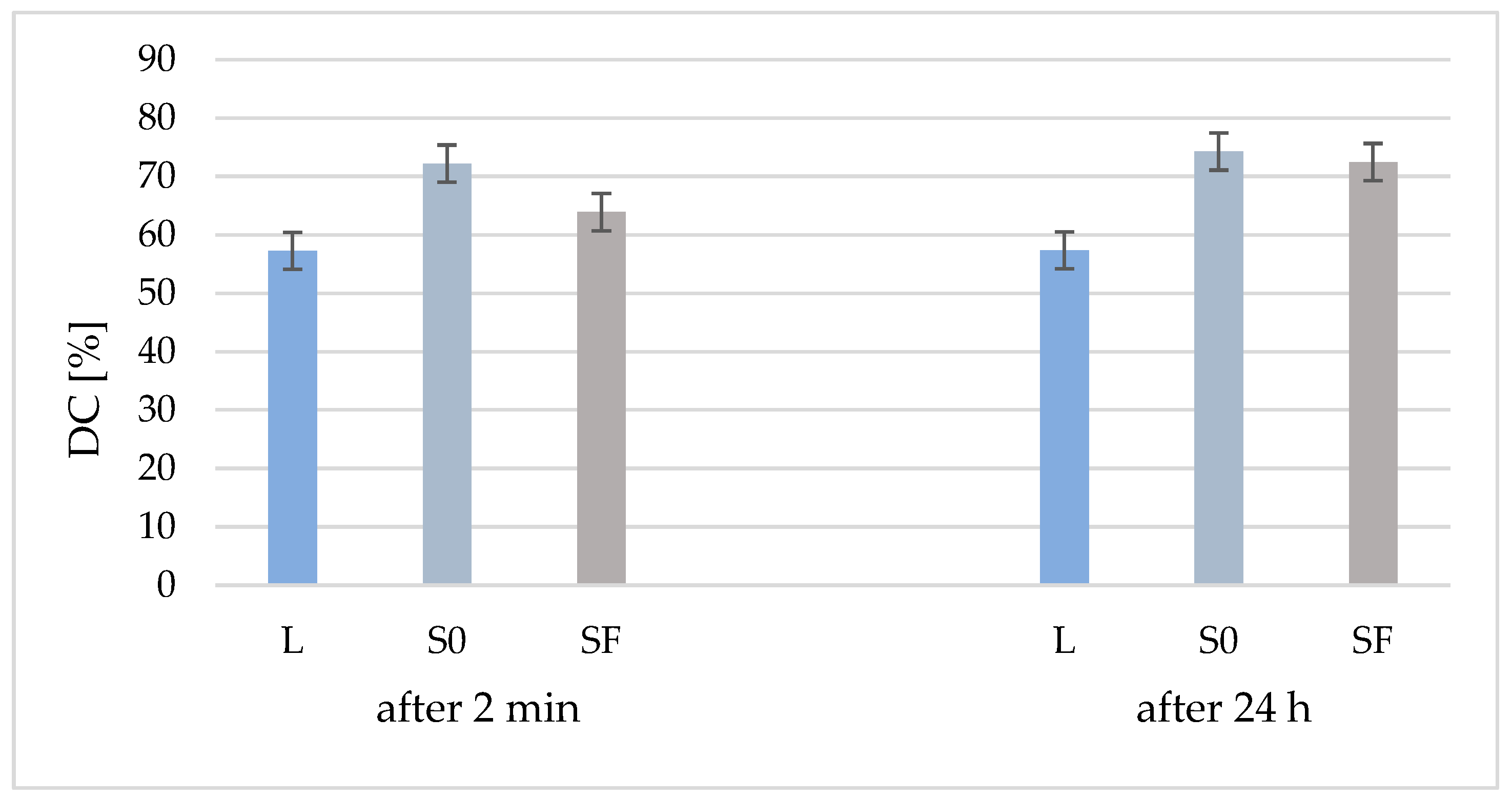
2.2.1. Degree of Conversion (DC)
2.2.2. Mechanical Resistance Tests
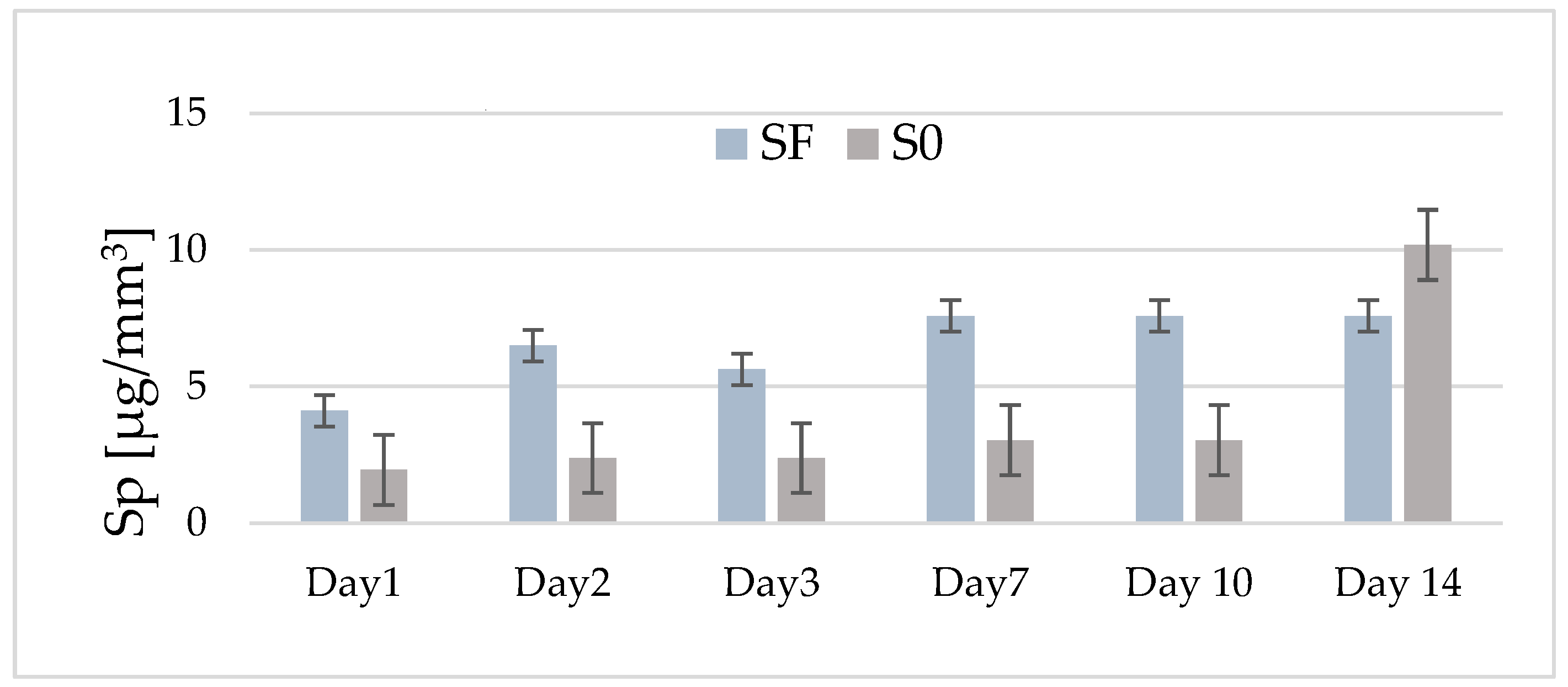
2.2.3. Water Sorption (WS)
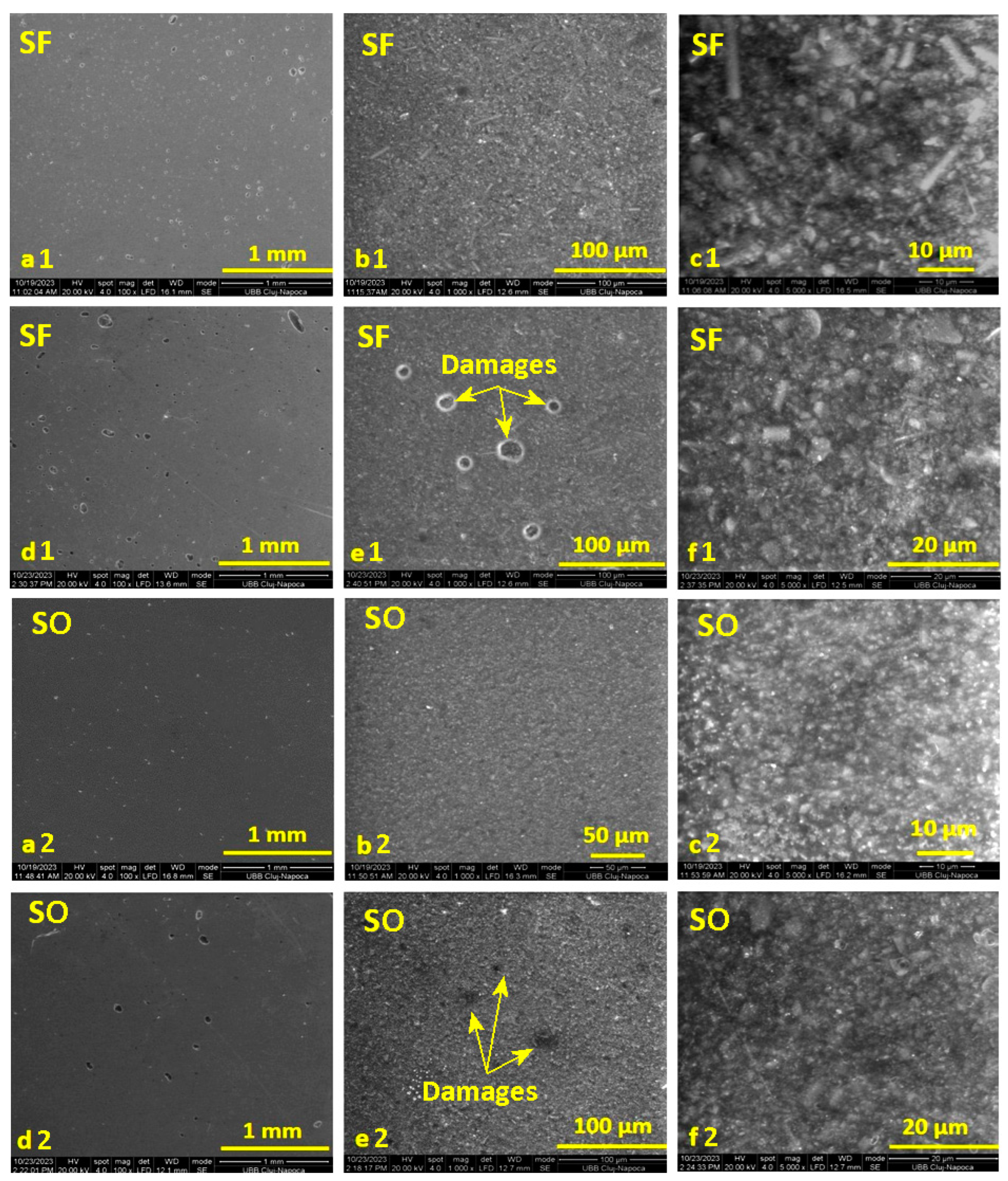
2.2.4. Scanning Electron Microscopy (SEM)
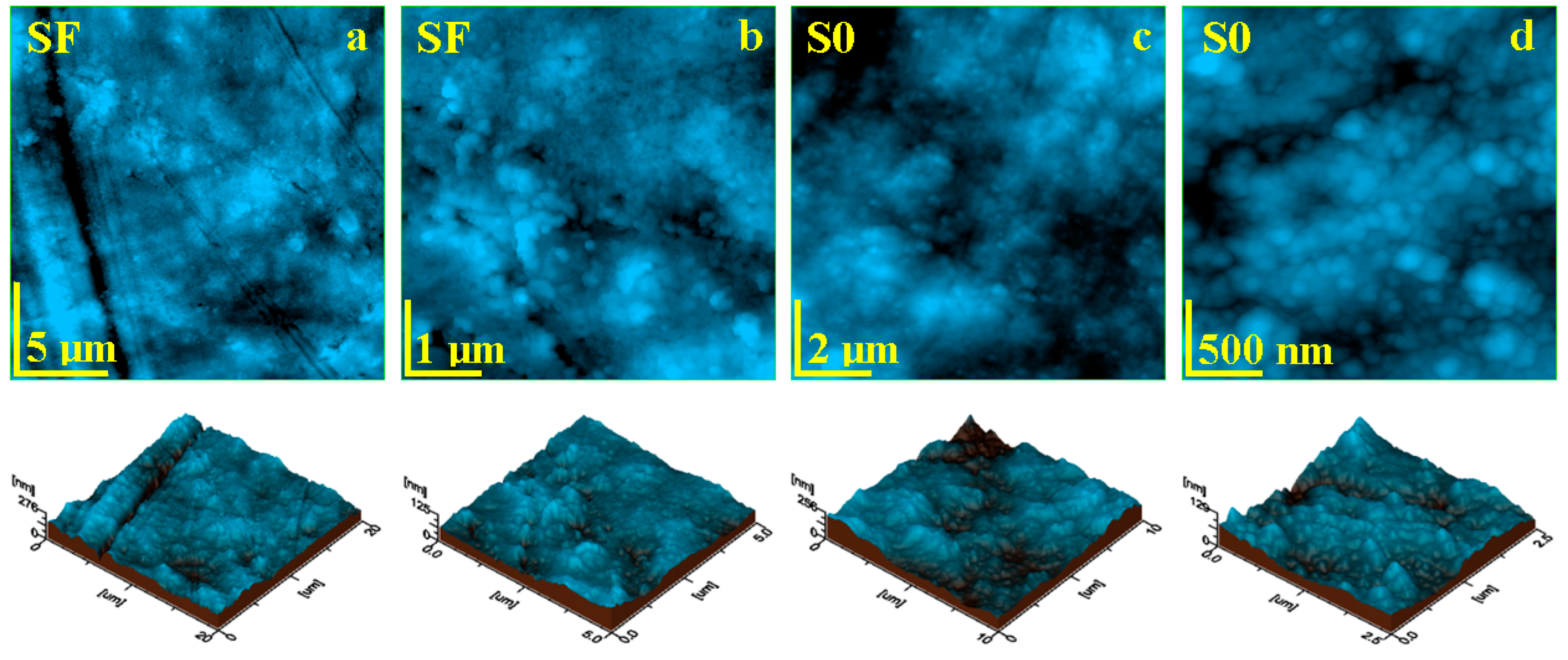
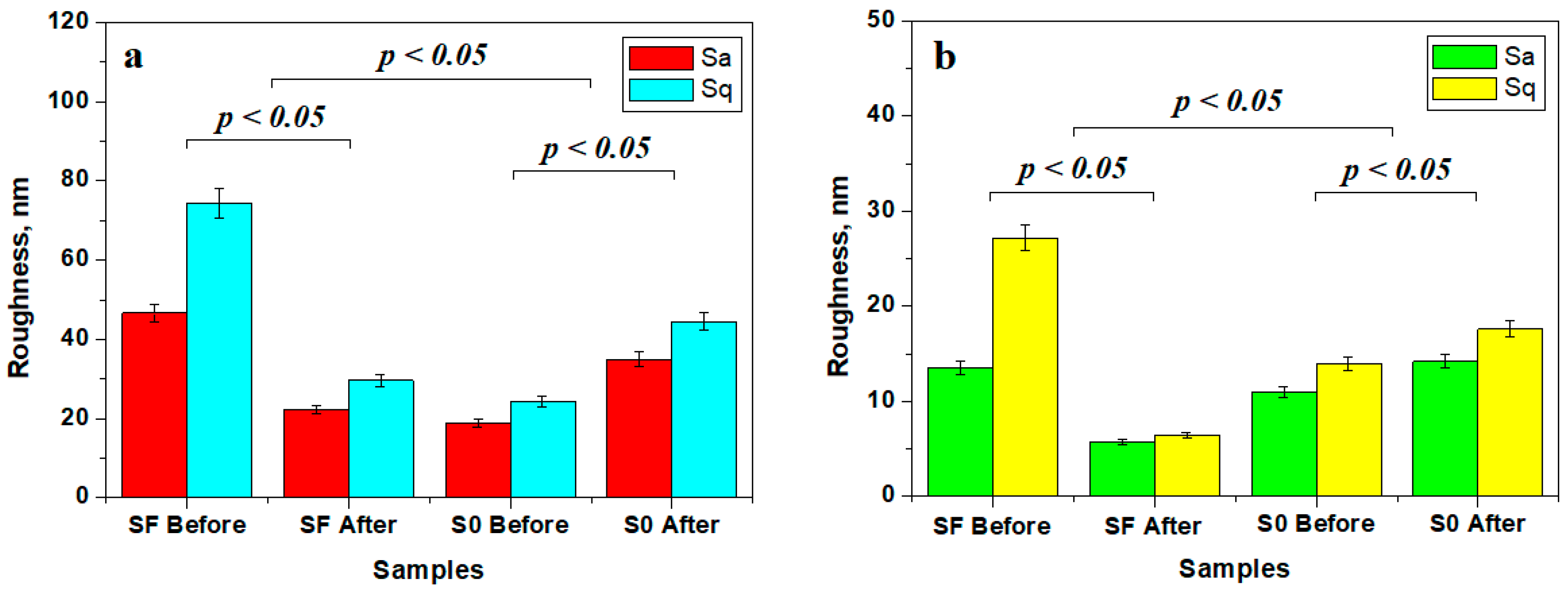
2.2.5. Atomic Force Microscopy (AFM)
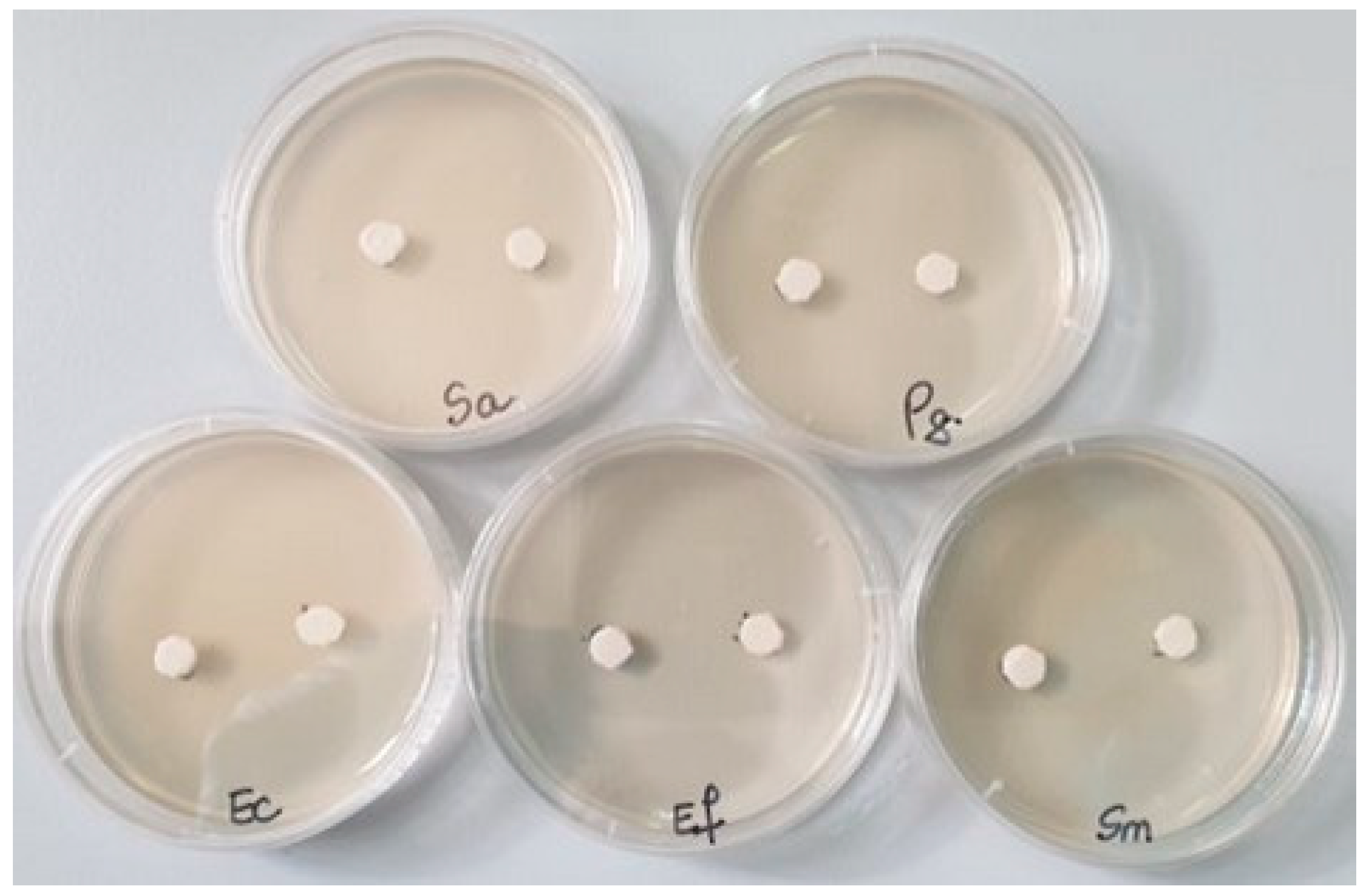
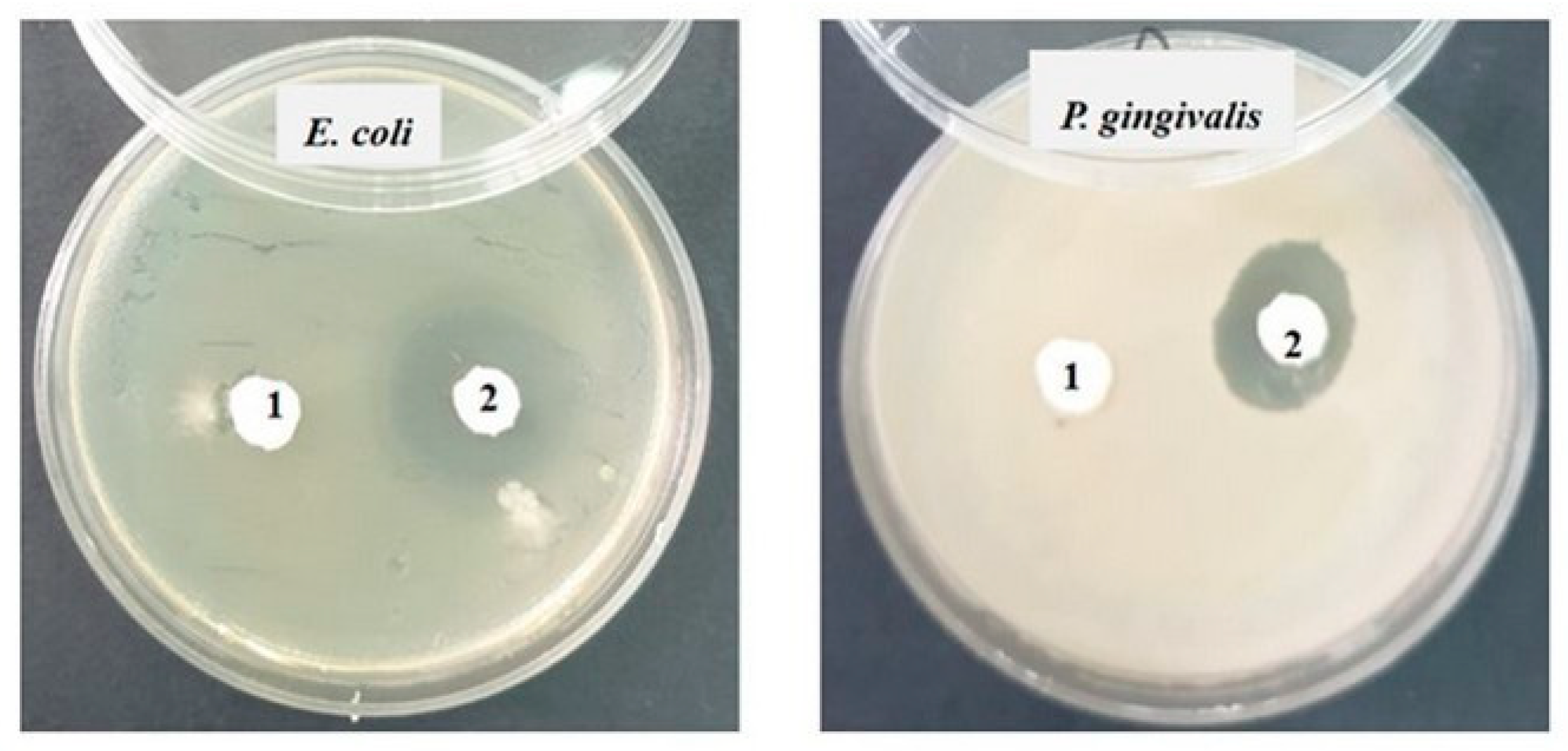
2.2.6. Antimicrobial Activity
3. Results
3.1. Degree of Conversion (DC)
3.2. Mechanical Properties and Statistical Analyses
3.3. Water Sorption (Sp)
3.4. Scanning Electron Microscopy (SEM)
3.5. Atomic Force Microscopy (AFM)
3.6. Antimicrobial Activity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lassila, L.; Keulemans, F.; Vallittu, P.K.; Garoushi, S. Characterization of restorative short-fiber reinforced dental composites. Dent. Mater. J. 2020, 39, 992–999. [Google Scholar] [CrossRef]
- Liu, J.; Zhang, H.; Sun, H.; Liu, Y.; Liu, W.; Su, B.; Li, S. The development of filler morphology in dental resin composites: A review. Materials 2021, 14, 5612. [Google Scholar] [CrossRef]
- Elfakhri, F.; Alkahtani, R.; Li, C.; Khaliq, J. Influence of filler characteristics on the performance of dental composites: A comprehensive review. Ceram. Int. 2022, 48, 27280–27294. [Google Scholar] [CrossRef]
- Safwat, E.M.; Khater, A.G.; Abd-Elsatar, A.G.; Khater, G.A. Glass fiber-reinforced composites in dentistry. Bull. Natl. Res. Cent. 2021, 45, 190. [Google Scholar] [CrossRef]
- Raju, R.; Rajan, G.; Farrar, P. Dimensional stability of short fibre reinforced flowable dental composites. Sci. Rep. 2021, 11, 4697. [Google Scholar] [CrossRef]
- Alshetiwi, D.S.D.; Muttlib, N.A.A.; El-Damanhoury, H.M. Evaluation of mechanical properties of anatomically customized fiber posts using E-glass short fiber-reinforced composite to restore weakened endodontically treated premolars. BMC Oral Health 2024, 24, 323. [Google Scholar] [CrossRef]
- Babu, R.; Goyal, S.; Dhingra, A. Direct application of fiber-reinforced compositein post-endodontic restorations. Guident 2024, 17, 4. [Google Scholar]
- Butterworth, C.; Ellakwa, A.E.; Shortall, A. Fibre-reinforced composites in restorative dentistry. Dent. Update 2003, 30, 300–306. [Google Scholar] [CrossRef]
- Bijelic-Donova, J. Discontinuous Fiber-Reinforced Composite for Dental Applications. Ph.D. Thesis, University of Turku, Turku, Finland, 2016. ISSN 2343-3213. [Google Scholar]
- Syed, M.R.; Bano, N.Z.; Ghafoor, S.; Khalid, H.; Zahid, S. Synthesis and characterization of bioactive glass fiber-based dental restorative composite. Ceram. Int. 2020, 46, 21623–21631. [Google Scholar] [CrossRef]
- Cho, K.; Rajan, G.; Farrar, P.; Prentice, L.; Prusty, B.G. Dental resin composites: A review on materials to product realizations. Compos. B Eng. 2022, 230, 109495. [Google Scholar] [CrossRef]
- Ranka, S.; Rao, A.S.; Shah, U.; Solanki, D.; Pawar, A.M.; Reda, R.; Zanza, A.; Testarelli, L. Comparative Evaluation of Two Different Fiber-Reinforced Composite Materials in Class 1 Post-Endodontic Restorations in Molars-A Randomized Clinical Study. Materials 2022, 15, 7858. [Google Scholar] [CrossRef] [PubMed]
- Sun, Q.; Zhang, L.; Bai, R.; Zhuang, Z.; Zhang, Y.; Yu, T.; Peng, L.; Xin, T.; Chen, S.; Han, B. Recent Progress in Antimicrobial Strategies for Resin-Based Restoratives. Polymers 2021, 13, 1590. [Google Scholar] [CrossRef] [PubMed]
- Go, H.B.; Lee, M.J.; Seo, J.Y. Mechanical properties and sustainable bacterial resistance effect of strontium-modified phosphate-based glass microfiller in dental composite resins. Sci. Rep. 2023, 13, 17763. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, M.; Dudea, D.; Cuc, S.; Sarosi, C.; Prodan, D.; Petean, I.; Ilie, N. Chemical and structural assessment of new dental composites with graphene exposed to staining agents. J. Funct. Biomater. 2023, 14, 163. [Google Scholar] [CrossRef] [PubMed]
- International Standard ISO 4049; Polymer-Based Filling, Restorative and Luting Materials. Technical Committee 106-Dentistry. International Standards Organization: Geneva, Switzerland, 2000.
- Standard by American Dental Association (ADA) Standard No. 27; Polymer-Based Restaurative Materials. American Dental Association: Chicago, IL, USA, 2022.
- Tisler, C.E.; Moldovan, M.; Petean, I.; Buduru, S.D.; Prodan, D.; Sarosi, C.; Leucuţa, D.-C.; Chifor, R.; Badea, M.E.; Ene, R. Human Enamel Fluorination Enhancement by Photodynamic Laser Treatment. Polymers 2022, 14, 2969. [Google Scholar] [CrossRef] [PubMed]
- Iosif, C.; Cuc, S.; Prodan, D.; Moldovan, M.; Petean, I.; Badea, M.E.; Sava, S.; Tonea, A.; Chifor, R. Effects of Acidic Environments on Dental Structures after Bracket Debonding. Int. J. Mol. Sci. 2022, 23, 15583. [Google Scholar] [CrossRef] [PubMed]
- Atlas, R.M. Handbook of Microbiological Media, 4th ed.; CRC Press: New York, NY, USA, 2010. [Google Scholar]
- Leclercq, R.; Canton, R.; Brown, D.F.J.; Giske, C.G.; Heisig, P.; MacGowan, A.P.; Mouton, J.W.; Nordmann, P.; Rodloff, A.C.; Rossolini, G.M.; et al. EUCAST expert rules in antimicrobial susceptibility testing. Clin. Microbiol. Infect. 2013, 19, 141–160. [Google Scholar] [CrossRef] [PubMed]
- Carpa, R.; Drăgan-Bularda, M.; Muntean, V. Microbiologie Generală Lucrări Practice; Editura Presa Universitară Clujeană: Cluj-Napoca, Romania, 2014. [Google Scholar]
- Suryawanshi, A.; Behera, N. Dental composite resin: A review of major mechanical properties, measurements and its influencing factors. MatWerk 2022, 53, 617–635. [Google Scholar] [CrossRef]
- Alshabib, A.; Jurado, C.A.; Tsujimoto, A. Short fiber-reinforced resin-based composites (SFRCs); Current status and future perspectives. Dent. Mater. J. 2022, 41, 647–654. [Google Scholar] [CrossRef]
- Shouha, P.S.; Ellakwa, A.E. Effect of short glass fibers on the polymerization shrinkage stress of dental composite. J. Biomed. Mater. Res.-B Appl. Biomater. 2017, 105, 1930–1937. [Google Scholar] [CrossRef]
- Putzeys, E.; De Nys, S.; Cokic, S.M.; Duca, R.C.; Vanoirbeek, J.; Godderis, L.; Van Meerbeek, B.; Van Landuyt, K.L. Long-term elution of monomers from resin-based dental composites. Dent. Mater. 2019, 35, 477–485. [Google Scholar] [CrossRef]
- Muradbegovic, A.; Par, M.; Panduric, V.; Zugec, P.; Tauböck, T.T.; Attin, T.; Marovic, D. Water-Induced Changes in Experimental Resin Composites Functionalized with Conventional (45S5) and Customized Bioactive Glass. J. Funct. Biomater. 2023, 14, 298. [Google Scholar] [CrossRef]
- Kouassi, A.Y.E.; Sangaré, M.K.; Boumbimba, R.M.; Koumba, N.; Gerard, P. Experimental and multiscale investigation of the elastic and impact properties of glass fibers/Elium acrylic modified nanoparticles laminate composites. Mater. Lett. 2024, 354, 135369. [Google Scholar] [CrossRef]
- Joshua, A.M.; Cheng, G.; Lau, E.V. Soft matter analysis via atomic force microscopy (AFM): A review. Appl. Surf. Sci. Adv. 2023, 17, 100448. [Google Scholar] [CrossRef]
- Thorat, S.B.; Diaspro, A.; Salerno, M. In vitro investigation of coupling-agent-free dental restorative composite based on nano-porous alumina fillers. J. Dent. 2014, 42, 279–286. [Google Scholar] [CrossRef]
- Makepeace, D.K.; Locatelli, P.; Lindsay, C.; Adams, J.M.; Keddie, J.L. Colloidal polymer composites: Are nano-fillers always better for improving mechanical properties? J. Colloid Interface Sci. 2018, 523, 45–55. [Google Scholar] [CrossRef]
- Cho, K.; Yasir, M.; Jung, M.; Willcox, M.D.P.; Stenzel, M.H.; Rajan, G.; Farrar, P.; Prusty, B.G. Hybrid engineered dental composites by multiscale reinforcements with chitosan-integrated halloysite nanotubes and S-glass fibers. Compos. Part B Eng. 2020, 202, 108448. [Google Scholar] [CrossRef]
- Iranmanesh, P.; Ehsani, A.; Khademi, A.; Asefnejad, A.; Shahriari, S.; Soleimani, M.; Ghadiri Nejad, M.; Saber-Samandari, S.; Khandan, A. Application of 3D bioprinters for dental pulp regeneration and tissue engineering (porous architecture). Transp. Porous Media 2022, 142, 265–293. [Google Scholar] [CrossRef]
- Ravandi, R.; Heris, S.Z.; Hemmati, S.; Aghazadeh, M.; Davaran, S.; Abdyazdani, N. Effects of chitosan and TiO2 nanoparticles on the antibacterial property and ability to self-healing of cracks and retrieve mechanical characteristics of dental composites. Heliyon 2024, 10, e27734. [Google Scholar] [CrossRef]
- Khandan, A.; Nassireslami, E.; Saber-Samandari, S.; Arabi, N. Fabrication and characterization of porous bioceramic-magnetite biocomposite for maxillofacial fractures application. Dent. Hypotheses 2020, 11, 74–85. [Google Scholar]
- Yaqoob, A.A.; Ahmad, H.; Parveen, T.; Ahmad, A.; Oves, M.; Ismail, I.M.; Qari, H.A.; Umar, K.; Mohamad Ibrahim, M.N. Recent advances in metal decorated nanomaterials and their various biological applications: A review. Front. Chem. 2020, 8, 341. [Google Scholar] [CrossRef]
- Slosarczyk, A.; Klapiszewska, I.; Skowronska, D.; Janczarek, M.; Jesionowski, T.; Klapiszewski, Ł. A comprehensive review of building materials modified with metal and metal oxide nanoparticles against microbial multiplication and growth. Chem. Eng. J. 2023, 466, 143276. [Google Scholar] [CrossRef]
- Chowdhury, M.A.; Hossain, N.; Shahid, M.A.; Alam, M.J.; Hossain, S.M.; Uddin, M.I.; Rana, M.M. Development of SiC–TiO2-Graphene neem extracted antimicrobial nano membrane for enhancement of multiphysical properties and future prospect in dental implant applications. Heliyon 2022, 8, 12345. [Google Scholar] [CrossRef]
- Uysal, I.; Yilmaz, B.; Evis, Z. Zn-doped hydroxyapatite in biomedical applications. J. Aust. Ceram. Soc. 2021, 57, 869–897. [Google Scholar] [CrossRef]
- Hanna, A.A.; Khorshed, L.; El-Beih, A.; Sherief, M.A.; El Khashen, A.; El-Bassyouni, G.T. Synthesis, Bioactivity, and Antimicrobial Studies on Zinc Oxide Incorporated into Nanohydrox-yapatite. Egypt. J. Chem. 2019, 62, 133–143. [Google Scholar] [CrossRef]
- Suparto, I.H.; Kurniawan, E. Synthesis and Characterization of Hydroxyapatite-Zinc Oxide (HAp-ZnO) as Antibacterial Bio-material. IOP Conf. Ser. Mater. Sci. Eng. 2019, 599, 012011. [Google Scholar] [CrossRef]


| Recipe | Organic Phase (25%) | Inorganic Phase (75%) | Initiation System (% Recipe) | |
|---|---|---|---|---|
| S0 | Bis-GMA 65%; TEGDMA 35%. | Glass A 20%, Quartz 40%, HA-Zn 10%. | Sr-Zr-glass powder 30% (particle size 0.01–0.035 µm and 2–6 nm) | 1% DMAEM 0.5% CQ |
| SF | Chopped Zr fiber powder 30% (50–100 µm length) | |||
| Test | No. of Specimen | Specimen Dimensions | Mechanical Test Characteristics |
|---|---|---|---|
| Flexural strength * | 10—S0 10—SF | 2 mm height, 2 mm width, 25 mm length | 3-point test compression test with a speed of 0.5 mm/min |
| Compression strength ** | 6 mm height, 3 mm diameter | compression test with a speed of 1 mm/min | |
| Diametral compression streangth ** | 3 mm height, 6 mm diameter | compression test with a loading rate of 0.5 mN/s |
| Sample | FS ± SD [MPa] | Young’s Modulus ± SD [GPa] | CS ± SD [MPa] | DTS ± SD [MPa] |
|---|---|---|---|---|
| S0 | 83.00 ± 14.456 | 21.4 ± 3.039 | 222.74 ± 19.464 | 172.02 ± 21.242 |
| SF | 83.85 ± 15.327 | 24.5 ± 5.509 | 222.79 ± 27.721 | 128.03 ± 15.265 |
| Anova p value | 0.94 | 0.02 | 0.96 | 0.00009 |
| Bacterial Strain | S0 (±SD) | SF (±SD) | |
|---|---|---|---|
| Samples | |||
| Staphylococcus aureus ATCC 25923 | 17 (±0.2) | 20 (±0.2) | |
| Enterococcus faecalis ATCC 29212 | 0 (±0) | 0 (±0) | |
| Escherichia coli ATCC 25922 | 0 (±0) | 15 (±0.2) | |
| Streptococcus mutans ATCC 25175 | 12 (±0.1) | 25 (±0.3) | |
| Porphyromonas gingivalis ATCC 33277 | 0 (±0) | 12 (±0.3) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohajon, D.R.; Prodan, D.; Moldovan, M.; Petean, I.; Cuc, S.; Filip, M.; Carpa, R.; Gheorghe, G.F.; Saroşi, C.L. Formulation and Characterization of New Experimental Dental Composites with Zirconium Filling in Different Forms. Materials 2024, 17, 2711. https://doi.org/10.3390/ma17112711
Mohajon DR, Prodan D, Moldovan M, Petean I, Cuc S, Filip M, Carpa R, Gheorghe GF, Saroşi CL. Formulation and Characterization of New Experimental Dental Composites with Zirconium Filling in Different Forms. Materials. 2024; 17(11):2711. https://doi.org/10.3390/ma17112711
Chicago/Turabian StyleMohajon, Dipa Rani, Doina Prodan, Marioara Moldovan, Ioan Petean, Stanca Cuc, Miuta Filip, Rahela Carpa, Georgiana Florentina Gheorghe, and Codruţa Liana Saroşi. 2024. "Formulation and Characterization of New Experimental Dental Composites with Zirconium Filling in Different Forms" Materials 17, no. 11: 2711. https://doi.org/10.3390/ma17112711
APA StyleMohajon, D. R., Prodan, D., Moldovan, M., Petean, I., Cuc, S., Filip, M., Carpa, R., Gheorghe, G. F., & Saroşi, C. L. (2024). Formulation and Characterization of New Experimental Dental Composites with Zirconium Filling in Different Forms. Materials, 17(11), 2711. https://doi.org/10.3390/ma17112711









