Improved Biosafety and Transdermal Delivery of Aconitine via Diethylene Glycol Monoethyl Ether-Mediated Microemulsion Assisted with Microneedles
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Detection of Aconitine and its Solubility
2.3. Preparation and Characterization of Aconitine-Loaded Microemulsion
2.4. In Vitro Release
2.5. In Vitro Transdermal Evaluation
2.6. In Vivo Microdialysis Experiments
2.7. Histopathology of Skin Sections
2.8. Cell Viability
2.9. Cell Uptake
2.10. Preliminary Skin Irritation Test
2.11. Data Analysis
3. Results
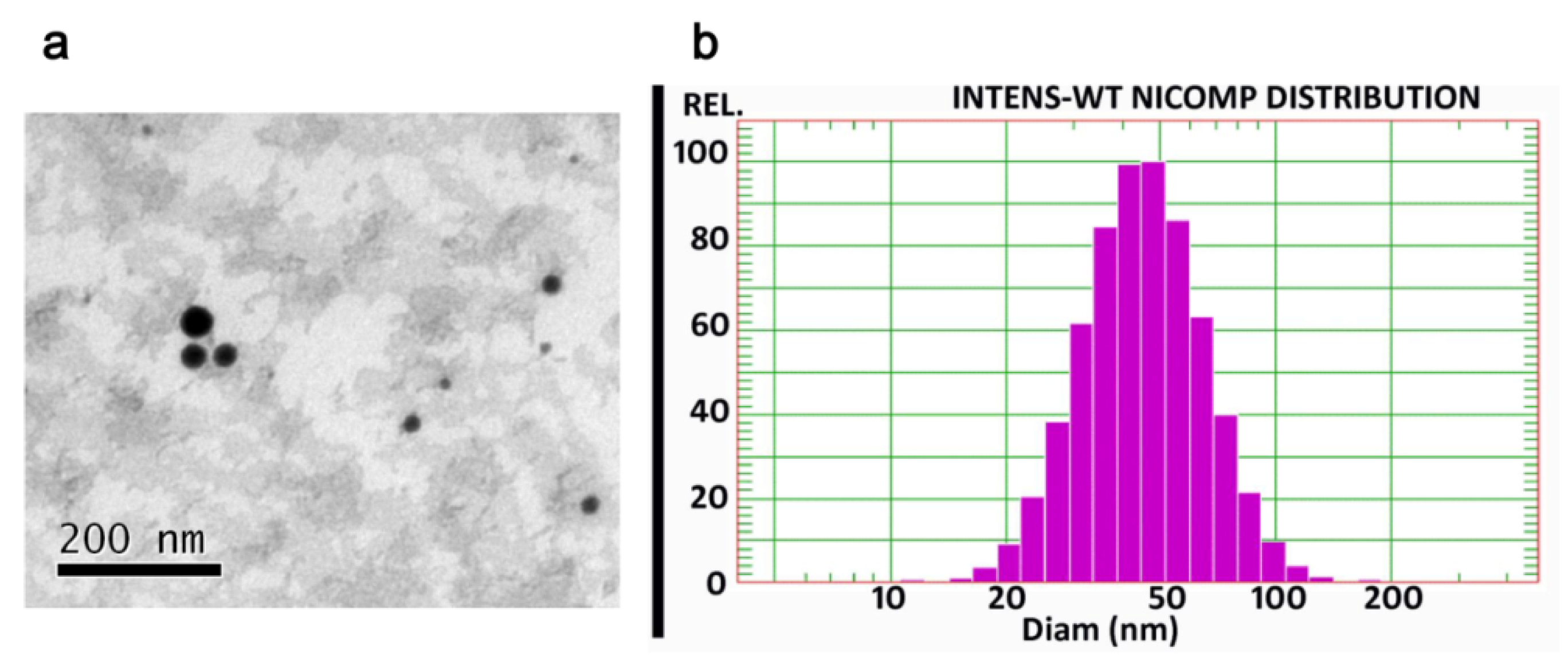
3.1. Characteristics of the Prepared Microemulsion
3.2. In Vitro Skin Permeation
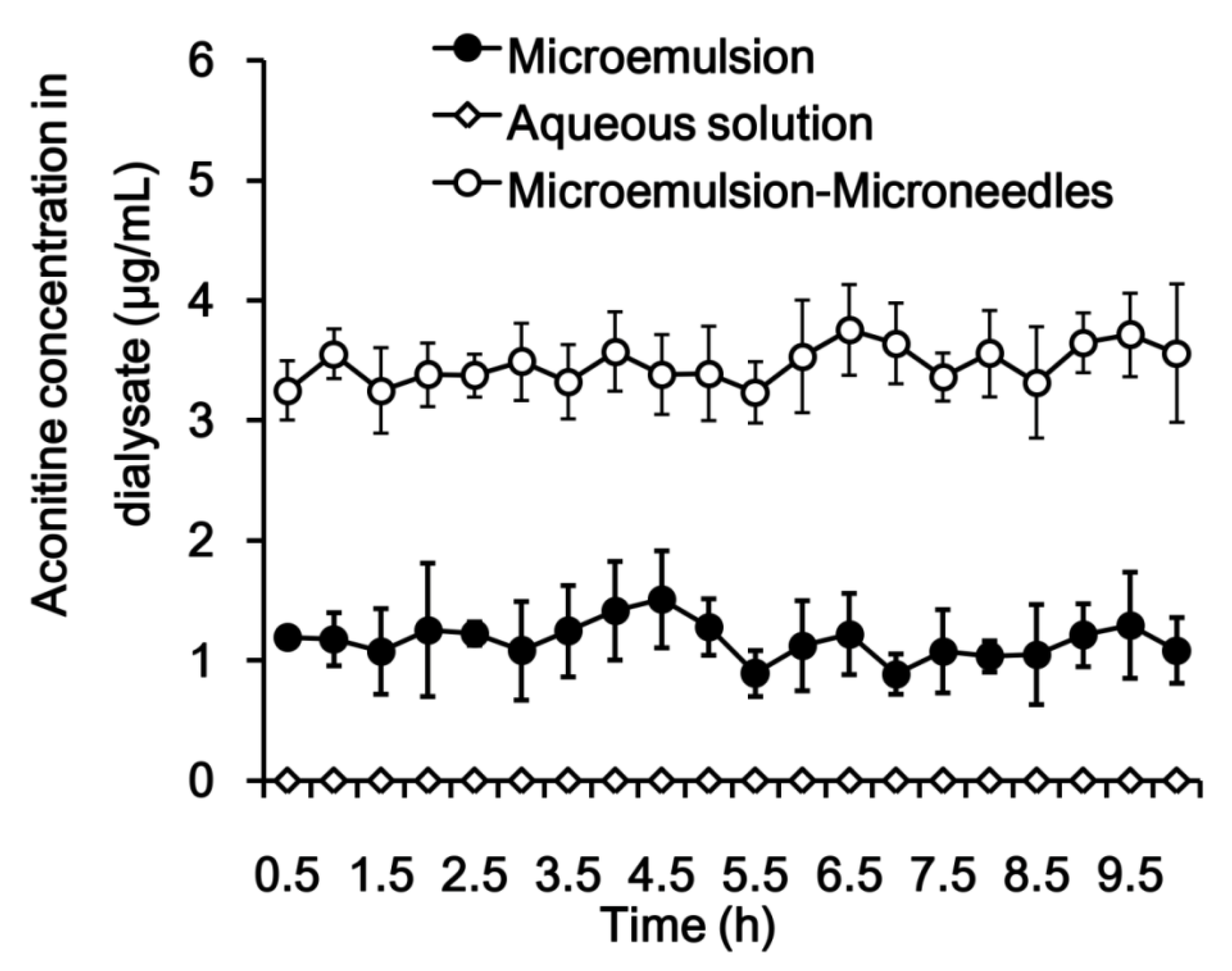
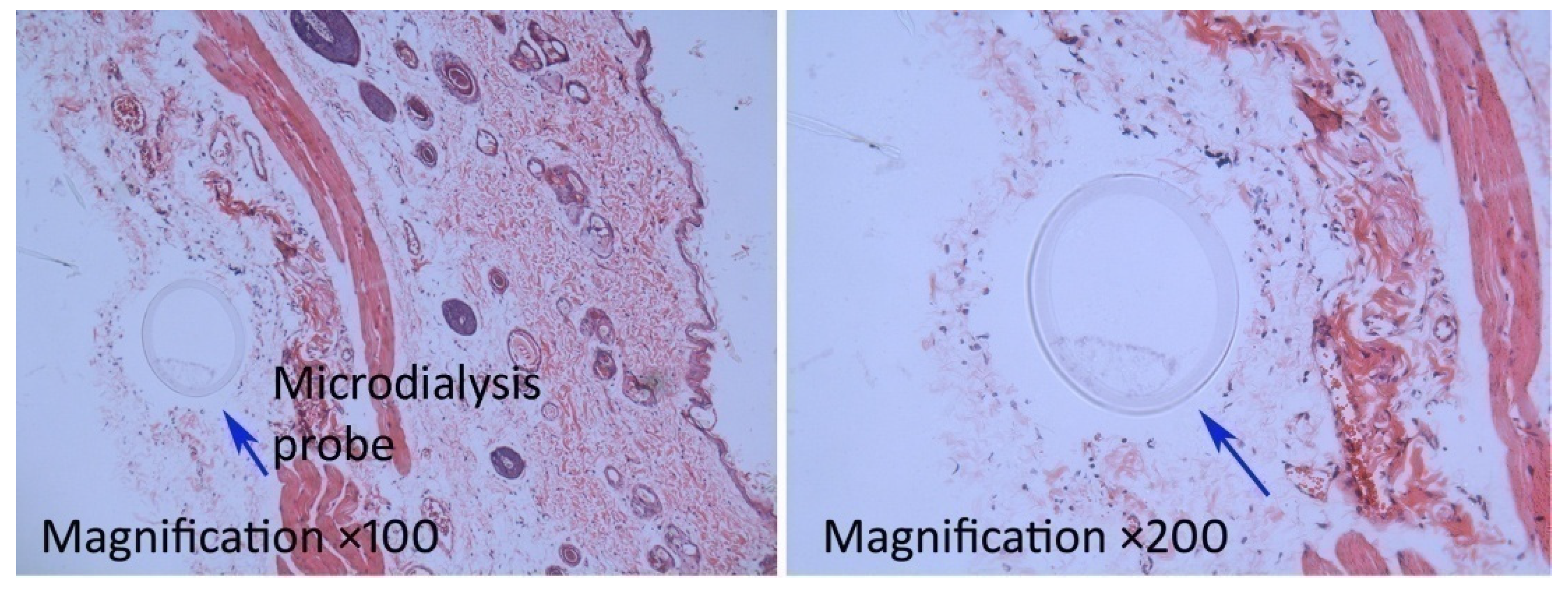
3.3. In Vivo Microdialysis
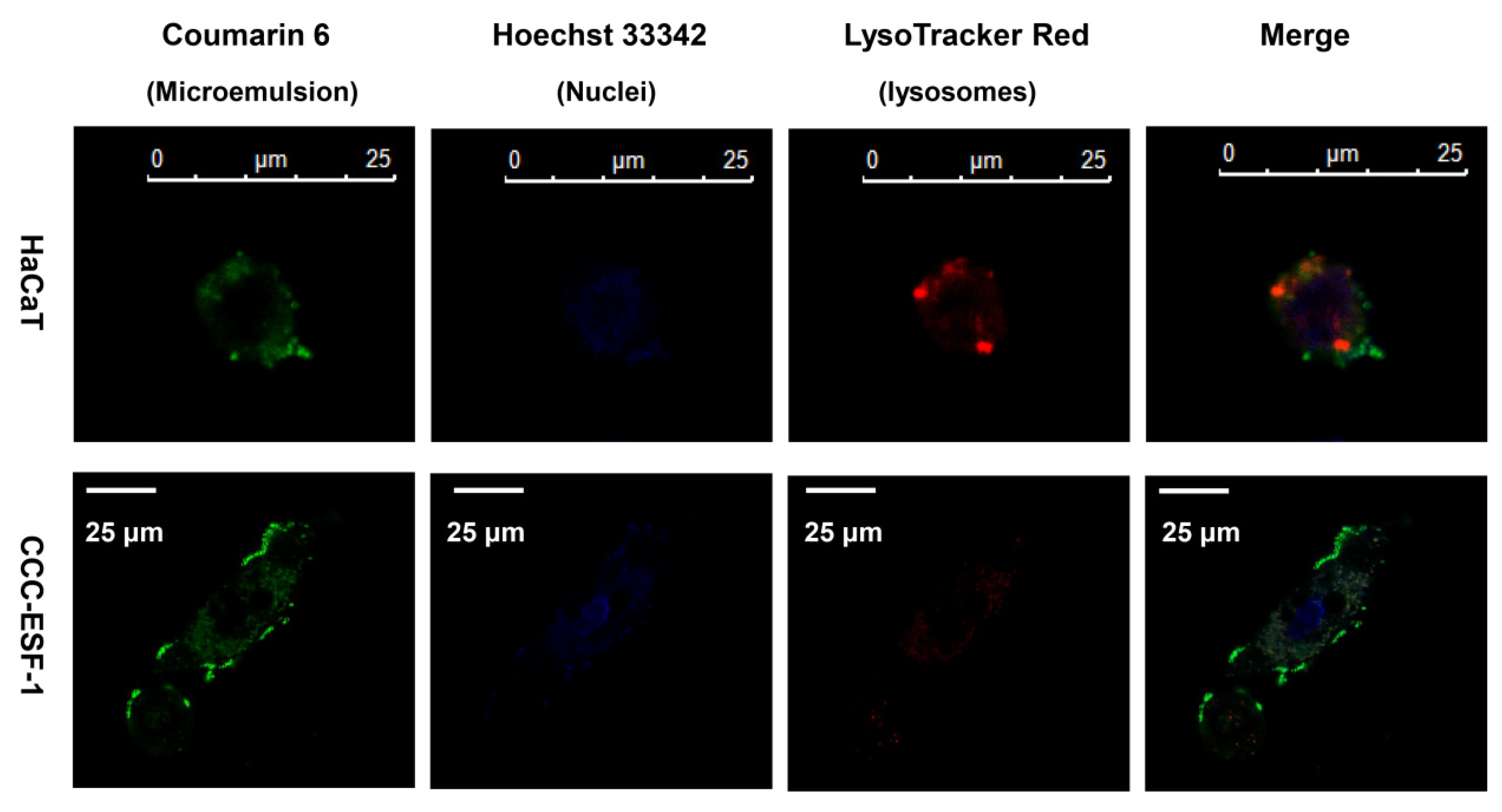
3.4. Intracellular Co-localization
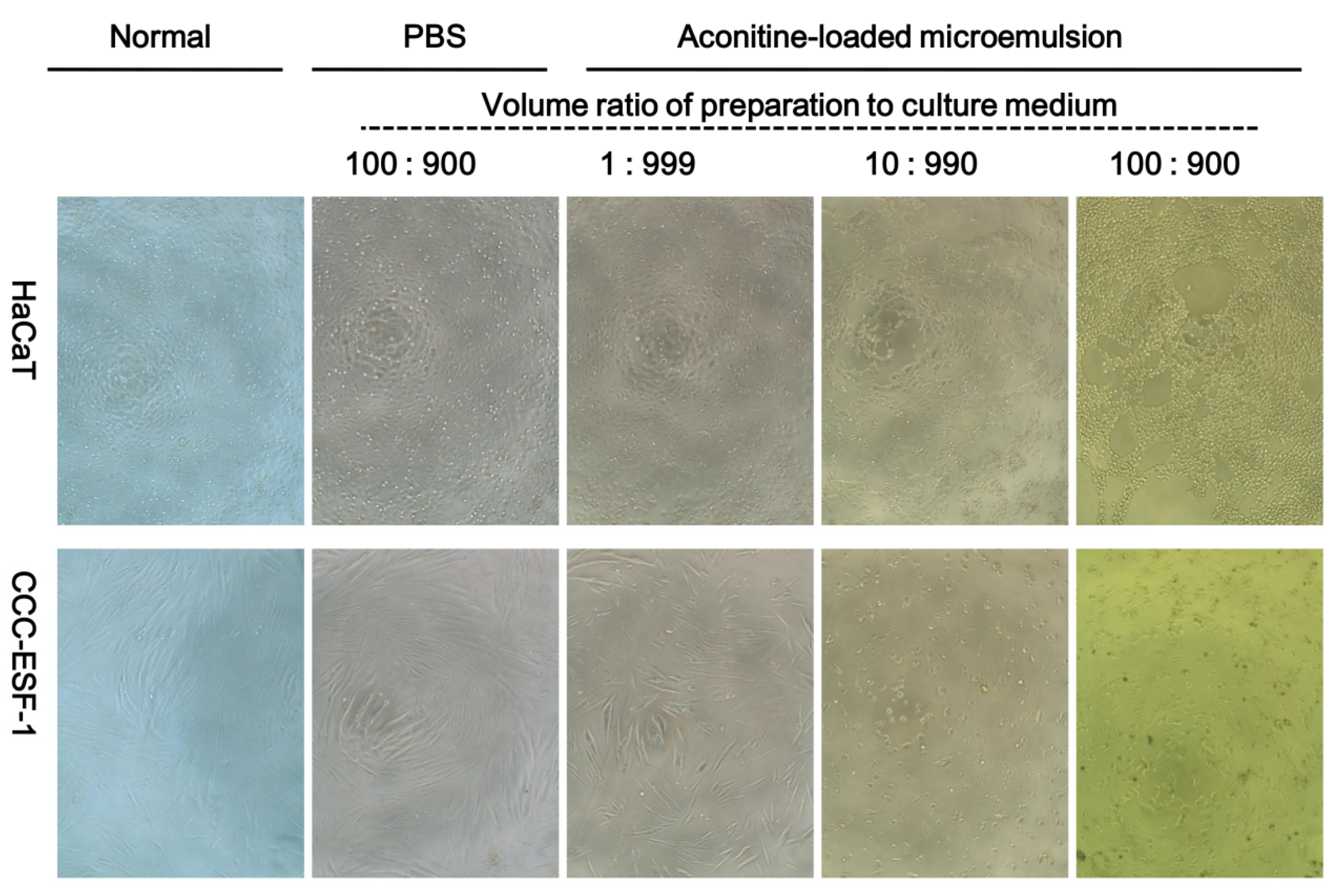
3.5. Cell Viability
3.6. Skin Irritation
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tai, C.J.; El-Shazly, M.; Wu, T.Y.; Lee, K.T.; Csupor, D.; Hohmann, J.; Chang, F.R.Y.; Wu, C. Clinical Aspects of Aconitum Preparations. Planta Med. 2015, 81, 1017–1028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Latter, G.; Grice, J.E.; Mohammed, Y.; Roberts, M.S.; Benson, H.A.E. Targeted Topical Delivery of Retinoids in the Management of Acne Vulgaris: Current Formulations and Novel Delivery Systems. Pharmaceutics 2019, 11, 490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarheed, O.; Shouqair, D.; Ramesh, K.; Khaleel, T.; Amin, M.; Boateng, J.; Drechsler, M. Formation of stable nanoemulsions by ultrasound-assisted two-step emulsification process for topical drug delivery: Effect of oil phase composition and surfactant concentration and loratadine as ripening inhibitor. Int. J. Pharm. 2019, 576, 118952. [Google Scholar] [CrossRef] [PubMed]
- Yi, T.; Zhang, J. Effects of Hydrophilic Carriers on Structural Transitions and In Vitro Properties of Solid Self-Microemulsifying Drug Delivery Systems. Pharmaceutics 2019, 11, 267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.T.; Wu, Z.H.; Zhang, K.; Zhao, J.H.; Ye, B.N.; Feng, N.P. An in vitro and in vivo comparison of solid and liquid-oil cores in transdermal aconitinenanocarriers. J. Pharm. Sci. 2014, 103, 3602–3610. [Google Scholar] [CrossRef] [PubMed]
- Abdelghany, S.; Tekko, I.A.; Vora, L.; Larrañeta, E.; Permana, A.D.; Donnelly, R.F. Nanosuspension-Based Dissolving Microneedle Arrays for Intradermal Delivery of Curcumin. Pharmaceutics 2019, 11, 308. [Google Scholar] [CrossRef] [Green Version]
- Lopez-Ramirez, M.A.; Soto, F.; Wang, C.; Rueda, R.; Shukla, S.; Silva-Lopez, C.; Kupor, D.; McBride, D.A.; Pokorski, J.K.; Nourhani, A.; et al. Built-In Active Microneedle Patch with Enhanced Autonomous Drug Delivery. Adv. Mater. 2019, 32, e1905740. [Google Scholar] [CrossRef]
- Zandi, A.; Khayamian, M.A.; Saghafi, M.; Shalileh, S.; Katebi, P.; Assadi, S.; Gilani, A.; SalemizadehParizi, M.; Vanaei, S.; Esmailinejad, M.R.; et al. Microneedle-Based Generation of Microbubbles in Cancer Tumors to Improve Ultrasound-Assisted Drug Delivery. Adv. Healthc. Mater. 2019, 8, e1900613. [Google Scholar] [CrossRef]
- Tham, H.P.; Xu, K.; Lim, W.Q.; Chen, H.; Zheng, M.; Thng, T.G.S.; Venkatraman, S.S.; Xu, C.; Zhao, Y. Microneedle-Assisted Topical Delivery of Photodynamically Active Mesoporous Formulation for Combination Therapy of Deep-Seated Melanoma. ACS Nano. 2018, 12, 11936–11948. [Google Scholar] [CrossRef]
- Mojeiko, G.; de Brito, M.; Salata, G.C.; Lopes, L.B. Combination of microneedles and microemulsions to increase celecoxib topical delivery for potential application in chemoprevention of breast cancer. Int. J. Pharm. 2019, 560, 365–376. [Google Scholar] [CrossRef]
- Kelchen, M.N.; Brogden, N.K. In Vitro Skin Retention and Drug Permeation through Intact and Microneedle Pretreated Skin after Application of Propranolol Loaded Microemulsions. Pharm. Res. 2018, 35, 228. [Google Scholar] [CrossRef] [PubMed]
- Mi, Y.; Mao, Y.; Cheng, H.; Ke, G.; Liu, M.; Fang, C.; Wang, Q. Studies of blood-brain barrier permeability of gastrodigenin in vitro and in vivo. Fitoterapia 2019, 140, 104447. [Google Scholar] [CrossRef] [PubMed]
- Rea, H.; Kirby, B. A Review of Cutaneous Microdialysis of Inflammatory Dermatoses. Acta Derm. Venereol. 2019, 99, 945–952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erdő, F.; Hashimoto, N.; Karvaly, G.; Nakamichi, N.; Kato, Y. Critical evaluation and methodological positioning of the transdermal microdialysis technique. A review. J. Control. Release. 2016, 233, 147–161. [Google Scholar] [CrossRef]
- Lukács, B.; Bajza, Á.; Kocsis, D.; Csorba, A.; Antal, I.; Iván, K.; Laki, A.J.; Erdő, F. Skin-on-a-Chip Device for Ex Vivo Monitoring of Transdermal Delivery of Drugs-Design, Fabrication, and Testing. Pharmaceutics 2019, 11, 445. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.T.; Shen, L.N.; Zhao, J.H.; Feng, N.P. Evaluation of psoralenethosomes for topical delivery in rats by using in vivo microdialysis. Int. J. Nanomedicine. 2014, 9, 669–678. [Google Scholar] [CrossRef] [Green Version]
- Gulati, G.K.; Berger, L.R.; Hinds, B.J. A preclinical evaluation of a programmable CNT membrane device for transdermal nicotine delivery in hairless Guinea pigs. J. Control. Release. 2019, 293, 135–143. [Google Scholar] [CrossRef]
- Zhang, Y.T.; Han, M.Q.; Shen, L.N.; Zhao, J.H.; Feng, N.P. Solid Lipid Nanoparticles Formulated for Transdermal Aconitine Administration and Evaluated In Vitro and In Vivo. J. Biomed. Nanotechnol. 2015, 11, 351–361. [Google Scholar]
- Hathout, R.M.; Mansour, S.; Mortada, N.D.; Geneidi, A.S.; Guy, R.H. Uptake of microemulsion components into the stratum corneum and their molecular effects on skin barrier function. Mol. Pharm. 2010, 7, 1266–1273. [Google Scholar] [CrossRef]
- Kiselmann, C.; Dobler, D.; Schmidts, T.; Eicher, A.C.; Möbs, C.; Pfützner, W.; Runkel, F. Development of a skin-friendly microemulsion for dermal allergen-specific immunotherapy. Int. J. Pharm. 2018, 550, 463–469. [Google Scholar] [CrossRef]
- Chen, H.; Chang, X.; Weng, T.; Zhao, X.; Gao, Z.; Yang, Y.; Xu, H.; Yang, X. A study of microemulsion systems for transdermal delivery of triptolide. J. Control. Release. 2004, 98, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Wan, T.; Xu, T.; Pan, J.; Qin, M.; Pan, W.; Zhang, G.; Wu, Z.; Wu, C.; Xu, Y. Microemulsion based gel for topical dermal delivery of pseudolaric acid B: In vitro and in vivo evaluation. Int. J. Pharm. 2015, 493, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Pajić, N.Z.B.; Todosijević, M.N.; Vuleta, G.M.; Cekić, N.D.; Dobričić, V.D.; Vučen, S.R.; Čalija, B.R.; Lukić, M.Ž.; Ilić, T.M.; Savić, S.D. Alkyl polyglucoside vs. ethoxylated surfactant-based microemulsions as vehicles for two poorly water-soluble drugs: Physicochemical characterization and in vivo skin performance. Acta Pharm. 2017, 67, 415–439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raber, A.S.; Mittal, A.; Schäfer, J.; Bakowsky, U.; Reichrath, J.; Vogt, T.; Schaefer, U.F.; Hansen, S.; Lehr, C.M. Quantification of nanoparticle uptake into hair follicles in pig ear and human forearm. J. Control. Release. 2014, 179, 25–32. [Google Scholar] [CrossRef]
- Blume-Peytavi, U.; Vogt, A. Human hair follicle: Reservoir function and selective targeting. Br. J. Dermatol. 2011, 165, 13–17. [Google Scholar] [CrossRef]
- Patzelt, A.; Mak, W.C.; Jung, S.; Knorr, F.; Meinke, M.C.; Richter, H.; Rühl, E.; Cheung, K.Y.; Tran, N.B.N.N.; Lademann, J. Do nanoparticles have a future in dermal drug delivery? J. Control. Release. 2017, 246, 174–182. [Google Scholar] [CrossRef]
- Shen, L.N.; Zhang, Y.T.; Wang, Q.; Xu, L.; Feng, N.P. Preparation and evaluation of microemulsion-based transdermal delivery of total flavone of rhizomaarisaematis. Int. J.Nanomedicine. 2014, 9, 3453–3464. [Google Scholar]
- Li, H.Q.; Xu, J.Y.; Fan, X.H.; Wu, S.S. Optimization of the traditional processing method for precision detoxification of CaoWu through biomimetic linking kinetics and human toxicokinetics of aconitine as toxic target marker. J. Ethnopharmacol. 2019, 242, 112053. [Google Scholar] [CrossRef]
- McCrudden, M.T.; McAlister, E.; Courtenay, A.J.; González-Vázquez, P.; Singh, T.R.; Donnelly, R.F. Microneedle applications in improving skin appearance. Exp. Dermatol. 2015, 24, 561–566. [Google Scholar] [CrossRef]
- Lee, K.J.; Jeong, S.S.; Roh, D.H.; Kim, D.Y.; Choi, H.K.; Lee, E.H. A practical guide to the development of microneedle systems-In clinical trials or on the market. Int. J. Pharm. 2020, 573, 118778. [Google Scholar] [CrossRef]




| Parameter | Unit | Microemulsion | Microemulsion-Microneedles |
|---|---|---|---|
| Cmax | μg/mL | 1.51 ± 0.03 | 4.04 ± 0.12 ** |
| AUC0–t | min/μg/mL | 684.76 ± 19.01 | 2026.62 ± 10.20 ** |
| MRT0–t | min | 303.07 ± 27.32 | 311.46 ± 2.04 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Hu, H.; Jing, Q.; Wang, Z.; He, Z.; Wu, T.; Feng, N.-P. Improved Biosafety and Transdermal Delivery of Aconitine via Diethylene Glycol Monoethyl Ether-Mediated Microemulsion Assisted with Microneedles. Pharmaceutics 2020, 12, 163. https://doi.org/10.3390/pharmaceutics12020163
Zhang Y, Hu H, Jing Q, Wang Z, He Z, Wu T, Feng N-P. Improved Biosafety and Transdermal Delivery of Aconitine via Diethylene Glycol Monoethyl Ether-Mediated Microemulsion Assisted with Microneedles. Pharmaceutics. 2020; 12(2):163. https://doi.org/10.3390/pharmaceutics12020163
Chicago/Turabian StyleZhang, Yongtai, Hongmei Hu, Qian Jing, Zhi Wang, Zehui He, Tong Wu, and Nian-Ping Feng. 2020. "Improved Biosafety and Transdermal Delivery of Aconitine via Diethylene Glycol Monoethyl Ether-Mediated Microemulsion Assisted with Microneedles" Pharmaceutics 12, no. 2: 163. https://doi.org/10.3390/pharmaceutics12020163






