Formulating a Stable Mannitol Infusion while Maintaining Hyperosmolarity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Powder X-ray Diffraction (PXRD)
2.2.2. Differential Scanning Calorimetry (DSC)
2.2.3. Cambridge Structural Database (CSD) Analysis
2.2.4. Equilibrium Solubility Measurements
2.2.5. Continuous Cooling Experiments
2.2.6. Induction Time Experiments
3. Results and Discussion
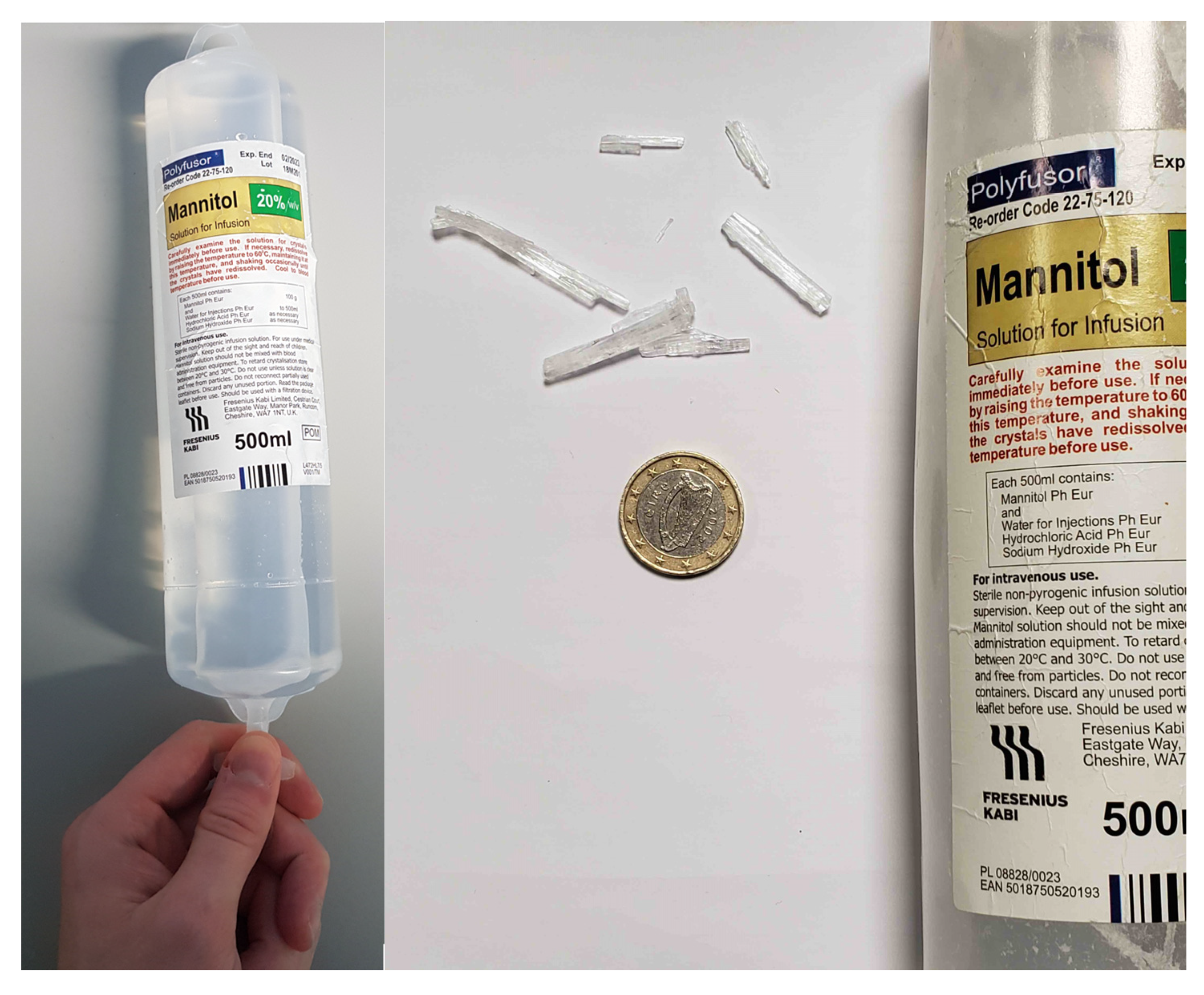
3.1. Characterisation of Crystals within Mannitol 20% w/v Infusion Solution
3.2. Mannitol Solubility and Nucleation Characteristics in the 20% w/v Infusion Solution
3.3. Mannitol Solubility in the Presence of Additives and Implications for Clinical Translation
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Iaccarino, C.; Carretta, A.; Nicolosi, F.; Morselli, C. Epidemiology of severe traumatic brain injury. J. Neurosurg. Sci. 2018, 62, 535–541. [Google Scholar]
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.E.; Hung, Y.C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the global incidence of traumatic brain injury. J. Neurosurg. 2019, 130, 1080–1097. [Google Scholar] [CrossRef] [Green Version]
- Ghajar, J. Traumatic brain injury. In Proceedings of the Lancet; Elsevier Limited: Amsterdam, The Netherlands, 2000; Volume 356, pp. 923–929. [Google Scholar]
- Ropper, A.H. Hyperosmolar Therapy for Raised Intracranial Pressure. N. Engl. J. Med. 2012, 367, 746–752. [Google Scholar] [CrossRef] [Green Version]
- Kochanek, P.M.; Tasker, R.C.; Carney, N.; Totten, A.M.; Adelson, P.D.; Selden, N.R.; Davis-O’Reilly, C.; Hart, E.L.; Bell, M.J.; Bratton, S.L.; et al. Guidelines for the Management of Pediatric Severe Traumatic Brain Injury, Third Edition: Update of the Brain Trauma Foundation Guidelines. Pediatr. Crit. Care Med. 2019, 20, S1–S82. [Google Scholar] [CrossRef] [Green Version]
- Knapp, J.M. Hyperosmolar therapy in the treatment of severe head injury in children: Mannitol and hypertonic saline. AACN Clin. Issues 2005, 16, 199–211. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Huang, H.; Huang, Y.; Sun, H.; Xu, H. Hypertonic saline or mannitol for treating elevated intracranial pressure in traumatic brain injury: A meta-analysis of randomized controlled trials. Neurosurg. Rev. 2019, 42, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Mangat, H.S.; Wu, X.; Gerber, L.M.; Schwarz, J.T.; Fakhar, M.; Murthy, S.B.; Stieg, P.E.; Ghajar, J.; Härtl, R. Hypertonic Saline is Superior to Mannitol for the Combined Effect on Intracranial Pressure and Cerebral Perfusion Pressure Burdens in Patients with Severe Traumatic Brain Injury. Neurosurgery 2020, 86, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Boone, M.D.; Oren-Grinberg, A.; Robinson, T.M.; Chen, C.C.; Kasper, E.M. Mannitol or hypertonic saline in the setting of traumatic brain injury: What have we learned? Surg. Neurol. Int. 2015, 6. [Google Scholar] [CrossRef]
- Li, M.; Chen, T.; Chen, S.; Cai, J.; Hu, Y. Comparison of Equimolar Doses of Mannitol and Hypertonic Saline for the Treatment of Elevated Intracranial Pressure After Traumatic Brain Injury. Medicine 2015, 94, 668. [Google Scholar] [CrossRef]
- ISRCTN16075091 Sugar or Salt (SOS) Trial: Comparing Two Current Treatments for Patients with a Brain Injury. Available online: http://www.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN16075091 2019 (accessed on 10 December 2019).
- Lionel, K.R.; Hrishi, A.P. Mannitol Shower: The Artefactual Air Embolism! J. Neurosurg. Anesthesiol. 2018, 30, 84–85. [Google Scholar] [CrossRef]
- Cornel, J.; Kidambi, P.; Mazzotti, M. Precipitation and transformation of the three polymorphs of d-mannitol. Ind. Eng. Chem. Res. 2010, 49, 5854–5862. [Google Scholar] [CrossRef]
- Kelly, F.J.; Robinson, R.A.; Stokes, R.H. The thermodynamics of the ternary system mannitol-sodium chloride-water at 25 °C from solubility and vapor pressure measurements. J. Phys. Chem. 1961, 65, 1958–1960. [Google Scholar] [CrossRef]
- Pitkänen, I.; Perkkalainen, P.; Rautiainen, H. Thermoanalytical studies on phases of D-mannitol. Thermochim. Acta 1993, 214, 157–162. [Google Scholar] [CrossRef]
- O’Sullivan, B.; Glennon, B. Application of in situ FBRM and ATR-FTIR to the monitoring of the polymorphic transformation of D-mannitol. Org. Process Res. Dev. 2005, 9, 884–889. [Google Scholar] [CrossRef]
- Nau, R. Osmotherapy for elevated intracranial pressure: A critical reappraisal. Clin. Pharmacokinet. 2000, 38, 23–40. [Google Scholar] [CrossRef] [PubMed]
- Hao, H.; Su, W.; Barrett, M.; Caron, V.; Healy, A.M.; Glennon, B. A calibration-free application of raman spectroscopy to the monitoring of mannitol crystallization and its polymorphic transformation. Org. Process Res. Dev. 2010, 14, 1209–1214. [Google Scholar] [CrossRef]
- Yu, L.; Milton, N.; Groleau, E.G.; Mishra, D.S.; Vansickle, R.E. Existence of a mannitol hydrate during freeze-drying and practical implications. J. Pharm. Sci. 1999, 88, 196–198. [Google Scholar] [CrossRef]
- Rowe, P.J.; Sheskey, M.E.Q. Handbook of Pharmaceutical Excipients; Pharmaceutical Press: London, UK, 2009; pp. 449–453. [Google Scholar]
- Rodríguez-Hornedo, N.; Murphy, D. Significance of controlling crystallization mechanisms and kinetics in pharmaceutical systems. J. Pharm. Sci. 1999, 88, 651–660. [Google Scholar] [CrossRef]
- Vesga, M.J.; McKechnie, D.; Mulheran, P.A.; Johnston, K.; Sefcik, J. Conundrum of γ glycine nucleation revisited: To stir or not to stir? CrystEngComm 2019, 21, 2234–2243. [Google Scholar] [CrossRef] [Green Version]
- Kulkarni, S.A.; Kadam, S.S.; Meekes, H.; Stankiewicz, A.I.; Ter Horst, J.H. Crystal nucleation kinetics from induction times and metastable zone widths. Cryst. Growth Des. 2013, 13, 2435–2440. [Google Scholar] [CrossRef]
- Dunitz, J.D.; Bernstein, J. Disappearing Polymorphs. Acc. Chem. Res. 1995, 28, 193–200. [Google Scholar] [CrossRef]
- Le, A.S.; Mulderrig, K.B. Sorbitol and Mannitol. In Alternative Sweetners; Nabours O’Brien, L., Ed.; Marcel Dekker: New York, NY, USA, 2001; pp. 317–334. ISBN 0824704371. [Google Scholar]
- Upadhyay, P.; Tripathi, V.N.; Singh, R.P.; Sachan, D. Role of hypertonic saline and mannitol in the management of raised intracranial pressure in children: A randomized comparative study. J. Pediatr. Neurosci. 2010, 5, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Jo, Y.H.; Kim, K.; Ahn, S.; Oh, Y.K.; Lee, H.; Shin, J.; Chin, H.J.; Na, K.Y.; Lee, J.B.; et al. Efficacy and safety of rapid intermittent correction compared with slow continuous correction with hypertonic saline in patients with moderately severe or severe symptomatic hyponatremia: Study protocol for a randomized controlled trial (SALSA trial). Trials 2017, 18, 147. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Formulation (w/v) | Stable to (°C) | Mannitol mOsmol·L−1 | Additive mOsmol·L−1 |
|---|---|---|---|
| Mannitol (20%) | 21 | 1098 | - |
| Mannitol/Sorbitol (10%/10%) | 10 | 549 | 549 |
| Mannitol/Glycerol (10%/5%) | 15 | 549 | 549 |
| Mannitol/NaCl (7.54%/2%) | 7 | 413.6 | 684.4 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kavanagh, O.; Hogan, F.; Murphy, C.; Croker, D.; Walker, G. Formulating a Stable Mannitol Infusion while Maintaining Hyperosmolarity. Pharmaceutics 2020, 12, 187. https://doi.org/10.3390/pharmaceutics12020187
Kavanagh O, Hogan F, Murphy C, Croker D, Walker G. Formulating a Stable Mannitol Infusion while Maintaining Hyperosmolarity. Pharmaceutics. 2020; 12(2):187. https://doi.org/10.3390/pharmaceutics12020187
Chicago/Turabian StyleKavanagh, Oisín, Fiona Hogan, Caoimhe Murphy, Denise Croker, and Gavin Walker. 2020. "Formulating a Stable Mannitol Infusion while Maintaining Hyperosmolarity" Pharmaceutics 12, no. 2: 187. https://doi.org/10.3390/pharmaceutics12020187
APA StyleKavanagh, O., Hogan, F., Murphy, C., Croker, D., & Walker, G. (2020). Formulating a Stable Mannitol Infusion while Maintaining Hyperosmolarity. Pharmaceutics, 12(2), 187. https://doi.org/10.3390/pharmaceutics12020187





