Enhanced Efficacy of Thiosemicarbazone Derivative-Encapsulated Fibrin Liposomes against Candidiasis in Murine Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Animals
2.3. Microbial Strain and Inoculum Preparation for Infection
2.4. Physico-Chemical Properties of Compound 2C
2.5. Preparation of Samples
2.6. Preparation of 2C-Encapsulated Liposomes
2.7. Preparation of 2C-Encapsulated Fibrin Liposomes
2.8. Characterization of 2C-FL
2.8.1. Determination of Size and Surface Morphology
2.8.2. Determination of Zeta Potential
2.8.3. Determination of Entrapment Efficiency and Loading Efficiency
2.8.4. In-Vitro Release Kinetics
2.9. Stability in Human Serum
2.10. Pharmacokinetics and Biodistribution Studies
2.11. Toxicity Tests
2.12. Histopathological Examination of Tissue Sections
2.13. In Vitro Testing of 2C-FL against C. albicans Infection
2.13.1. Determination of Minimum Inhibitory Concentration (MIC)
2.13.2. Annexin-V Assay for Detecting Apoptosis
2.14. The Activity of 2C-FL against C. albicans Infection in a Mouse Model
2.14.1. Determination of 2C Dose for Treatment
2.14.2. Treatment Schedule
2.14.3. Fungal Burden Studies
2.14.4. Survival Studies
2.15. Statistical Analysis
3. Results
3.1. Physico-Chemical Properties of 2C
3.2. Characterization of 2C-FL
3.3. In-Vitro Release of 2C-FL
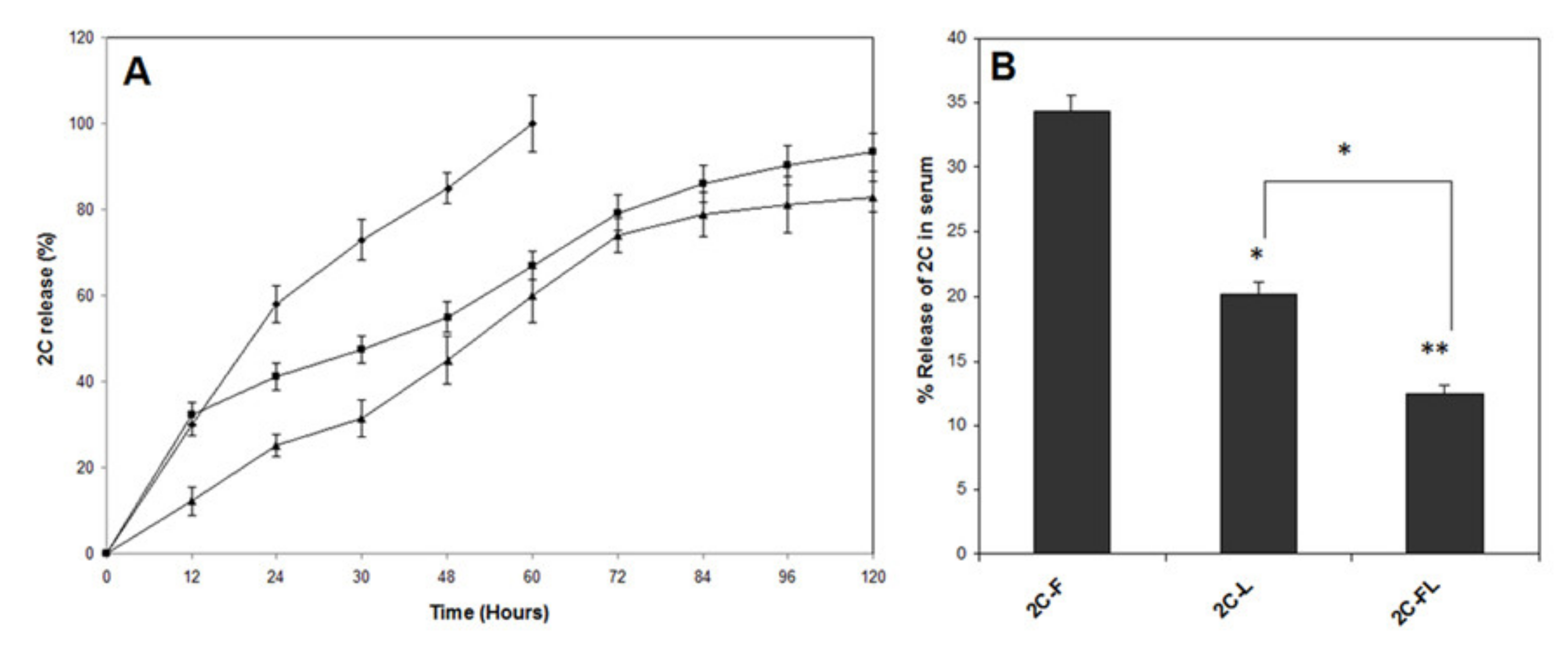
3.4. Stability of 2C-FL in Human Serum
3.5. Pharmacokinetics and Tissue Distribution of 2C-FL
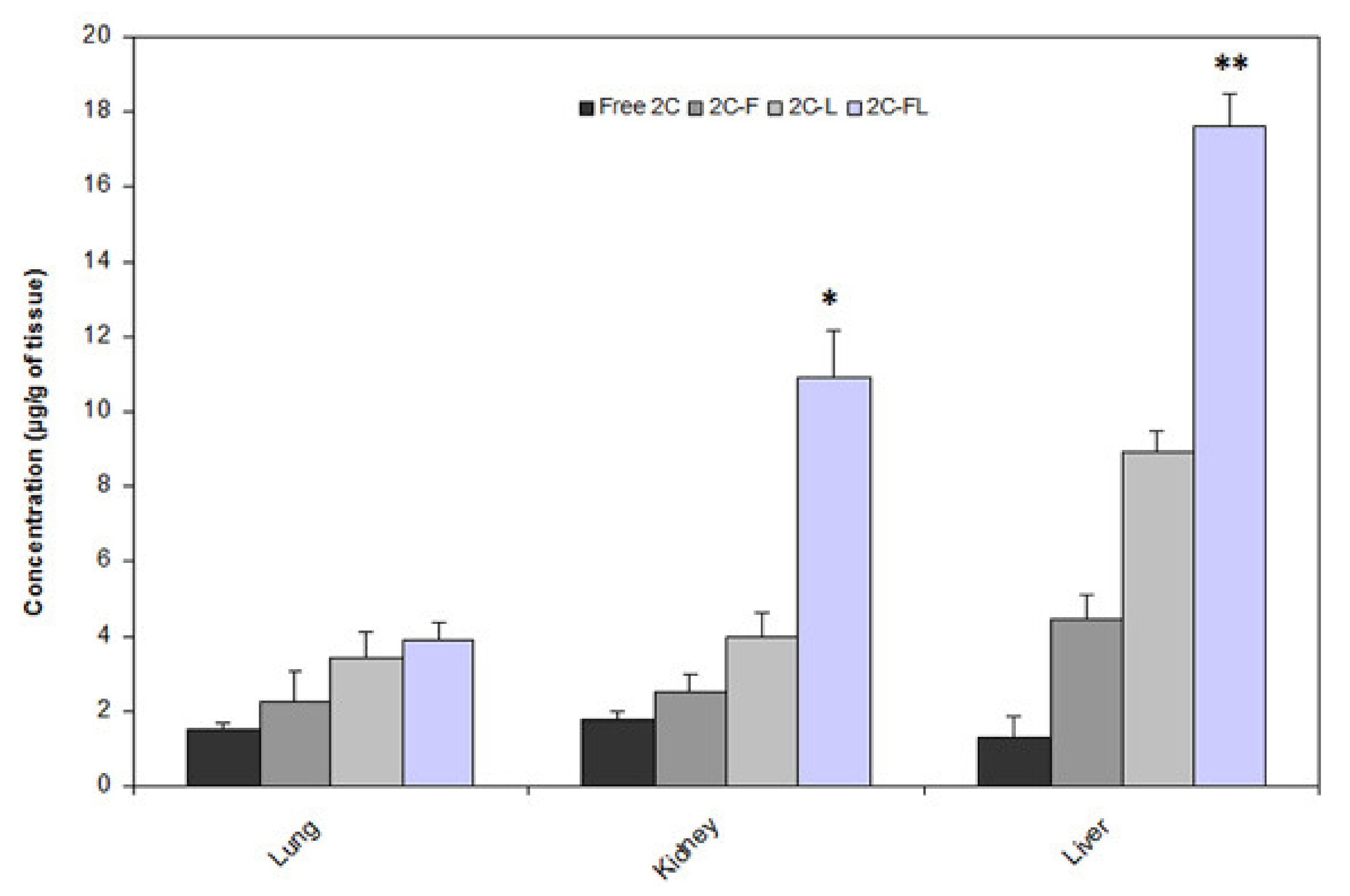
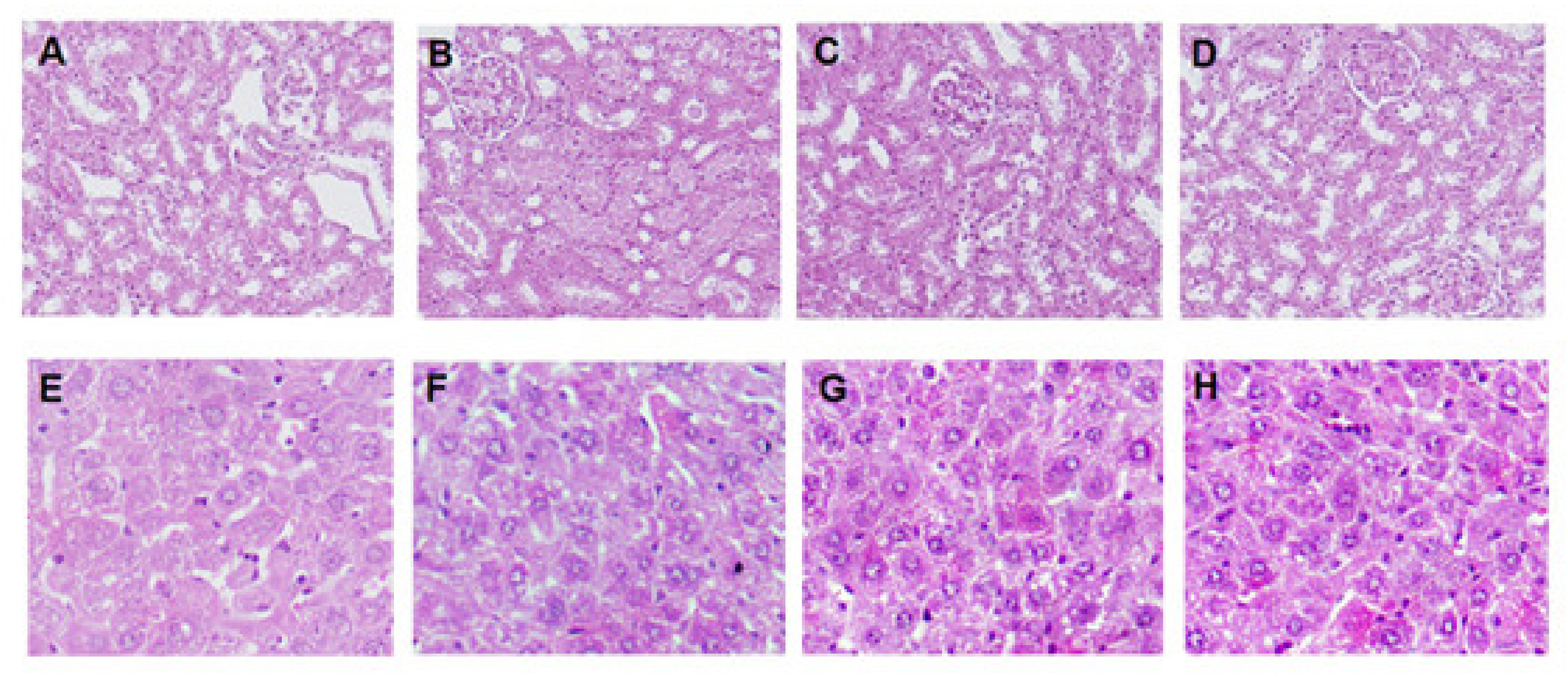
3.6. 2C-FL Toxicity In Vitro and In Vivo
3.7. Activity of 2C-FL against C. albicans Infection In Vitro
3.8. Therapeutic Efficacy of 2C-FL against C. albicans Infection
3.8.1. Dose of 2C for In Vivo Treatment
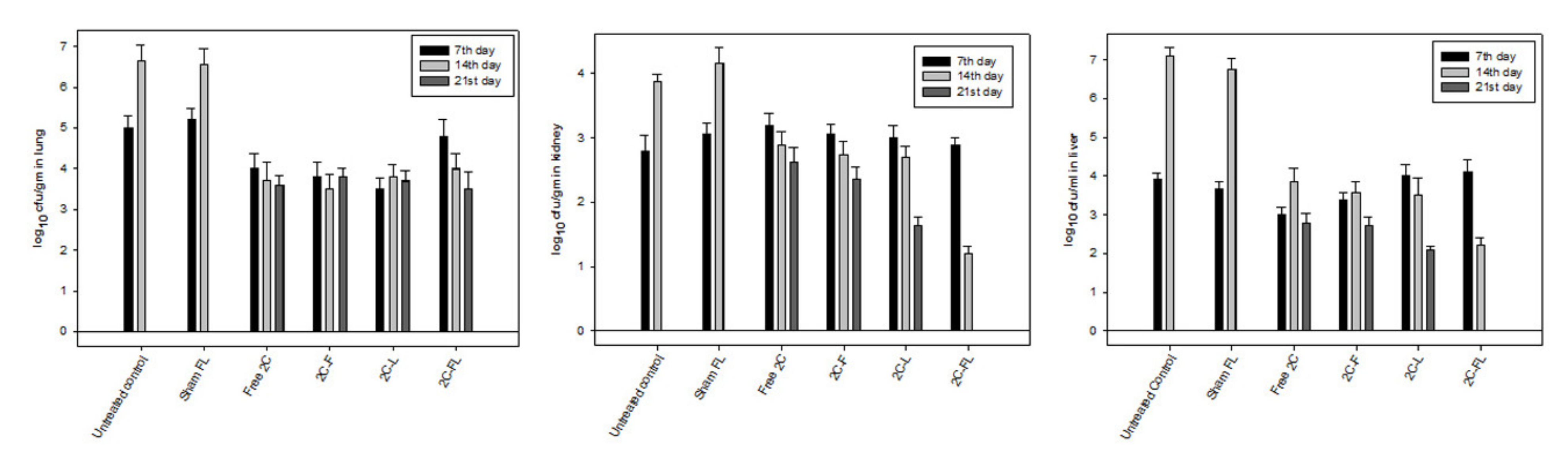
3.8.2. Fungal Burden in Treated Mice
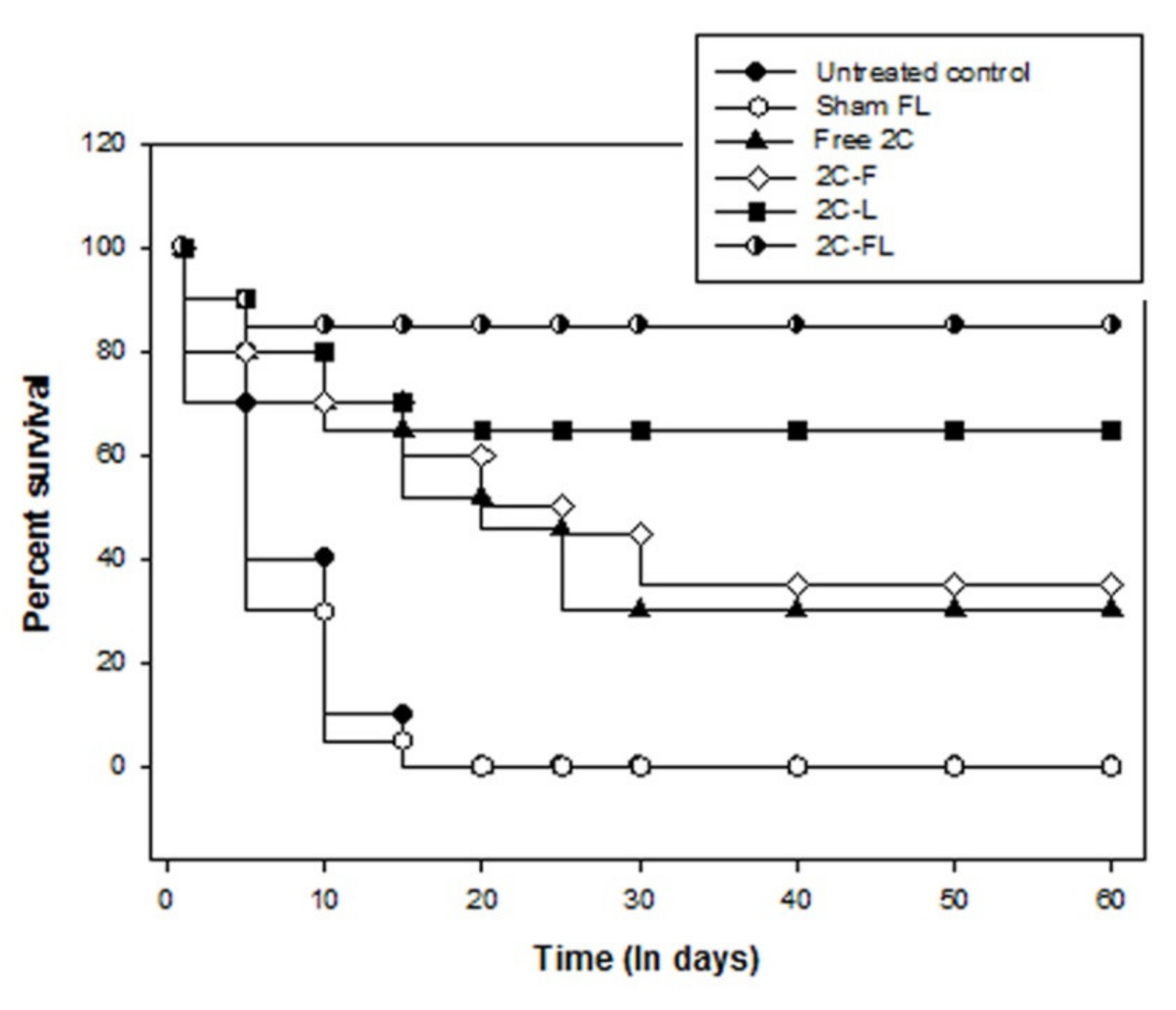
3.8.3. Survival of Treated Mice
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bongomin, F.; Gago, S.; Oladele, R.O.; David, W.D. Global and multi-national prevalence of fungal diseases—Estimate precision. J. Fungi (Basel) 2017, 3, 57. [Google Scholar] [CrossRef]
- Opletalova, V.; Dolezel, J.; Kucerova-Chlupacova, M. Synthesis and antifungal screening of 2-{[1-(5-Alkyl/arylalkylpyrazin-2-yl)ethylidene]hydrazono}-1,3-thiazolidin-4-ones. Molecules 2016, 21, 1592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, G.D.; Denning, D.W.; Gow, N.A.R.; Levitz, S.M.; Netea, M.G.; White, T.C. Human fungal infections: The Hidden Killers. Sci. Transl. Med. 2012, 4, 165rv13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poulain, D. Candida albicans, plasticity and pathogenesis. Crit. Rev. Microbiol. 2015, 41, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J.E. Candida species. In Principles and Practice of Infectious Diseases, 8th ed.; Bennett, J.E., Dolin, R., Blaser, M.J., Eds.; Elsevier: Amsterdam, The Netherlands, 2015; pp. 2879–2894. [Google Scholar]
- De Cremer, K.; Lanckacker, E.; Cools, T.L.; Bax, M.; De Brucker, K.; Cos, P.; Cammue, B.P.; Thevissen, K. Artemisinins, new miconazole potentiators resulting in increased activity against Candida albicans biofilms. Antimicrob. Agents Chemother. 2015, 59, 421–426. [Google Scholar] [CrossRef] [Green Version]
- Sobel, J.D. Recurrent vulvovaginal candidiasis. Am. J. Obstet. Gynecol. 2016, 214, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Department of Health and Human Services. CDC, Antibiotic Resistance Threats in the United States; CDC: Atlanta, GA, USA, 2019. [Google Scholar]
- Allen, D.; Wilson, D.; Drew, R.; Perfect, J. Azole antifungals: 35 years of invasive fungal infection management. Expert Rev. Anti-infect. Ther. 2015, 6, 787–798. [Google Scholar] [CrossRef]
- Stover, K.R.; Farley, J.M.; Kyle, P.B.; Cleary, J.D. Cardiac toxicity of some echinocandin antifungals. Expert Opin. Drug Saf. 2014, 2014, 5–14. [Google Scholar] [CrossRef]
- Pfaller, M.A. Antifungal drug resistance: Mechanisms, epidemiology, and consequences for treatment. Am. J. Med. 2012, 125, 3–13. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Castanheira, M.; Messer, S.A.; Moet, G.J.; Jones, R.N. Variation in Candida species. Distribution and antifungal resistance rates among bloodstream infection isolates by patient age: Report from the SENTRY Antimicrobial Surveillance Program (2008–2009). Diagn. Microbiol. Infect. Dis. 2010, 66, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Bharti, S.K.; Nath, G.; Tilak, R.; Singh, S.K. Synthesis, anti-bacterial and antifungal activities of some novel Schiff bases containing 2,4-disubstituted thiazole ring. Eur. J. Med. Chem. 2010, 45, 651–660. [Google Scholar] [CrossRef] [PubMed]
- Britta, E.A.; Scariot, D.B.; Falzirolli, H.; Ueda-Nakamura, T.; Silva, C.C.; Filho, B.P.; Borsali, R.; Nakamura, C.V. Cell death and ultrastructural alterations in Leish-mania amazonensis caused by new compound 4-Nitrobenzaldehyde thiosemicarbazone derived from S-limonene. BMC Microbiol. 2014, 14, 236–248. [Google Scholar] [CrossRef] [Green Version]
- Almeida, S.M.; Lafayette, E.A.; Silva, L.P.; Amorim, C.A.; Oliveira, T.B.; Ruiz, A.L.; Carvalho, J.E.; Moura, R.O.; Beltrao, E.I.; Lima, M.C.; et al. Synthesis, DNA binding, and antiproliferative activity of novel acridine-thiosemicarbazone derivatives. Int. J. Mol. Sci. 2015, 6, 13023–13042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dimmock, J.R.; McColl, J.M.; Wonko, S.L.; Thayer, R.S.; Hancock, D.S. Evaluation of the thiosemicarbazones of some aryl alkyl ketones and related compounds for anticonvulsant activities. Eur. J. Med. Chem. 1991, 26, 529–534. [Google Scholar] [CrossRef]
- Finkielsztein, L.M.; Castro, E.F.; Fabián, L.E.; Moltrasio, G.Y.; Campos, R.H.; Cavallaro, L.V.; Moglioni, A.G. New 1-indanone thiosemicarbazone derivatives active against BVDV. Eur. J. Med. Chem. 2008, 43, 1767–1773. [Google Scholar] [CrossRef]
- El-Sharief, M.A.M.S.; Abbas, S.Y.; El-Bayouki, K.A.M.; El-Gammal, E.W. Synthesis of thiosemicarbazones derived from N-(4-hippuric acid)thiosemicarbazide and different carbonyl compounds as antimicrobial agents. Eur. J. Med. Chem. 2013, 67, 263–268. [Google Scholar] [CrossRef]
- Zhang, X.M.; Guo, H.; Li, Z.S.; Song, F.H.; Wang, W.M.; Dai, H.Q.; Zhang, L.X.; Wang, J.G. Synthesis and evaluation of isatinb-thiosemicarbazones as novel agents against antibiotic-resistant Gram-positive bacterial species. Eur. J. Med. Chem. 2015, 101, 419–430. [Google Scholar] [CrossRef] [PubMed]
- Scotti, L.; Scotti, M.T.; Lima, E.O.; Silva, M.S.; Lima, M.C.A.; Pitta, I.R.; Moura, R.O.; Oliveira, J.G.B.; Cruz, R.M.D.; Mendonça Junior, F.J.B. Experimental methodologies and evaluations of computer-aided drug design methodologies applied to a series of 2-aminothiophene derivatives with antifungal activities. Molecules 2012, 17, 2298–2315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altintop, M.D.; Atli, O.; Ilgin, S.; Demirel, R.; Ozdemir, A.; Kaplancikli, Z.A. Synthesis and biological evaluation of new naphthalene substituted thiosemicarbazone derivatives as potent antifungal and anticancer agents. Eur. J. Med. Chem. 2016, 108, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Neto, L.N.A.; de Lima, M.C.A.; de Oliveira, J.F.; de Souza, E.R.; Buonafina, M.D.S.; Anjos, M.V.N.; Brayner, F.A.; Alves, L.C.; Neves, R.P.; Mendonça-Junior, F.J.B. Synthesis, cytotoxicity and antifungal activity of 5-nitro-thiophenethiosemicarbazones derivatives. Chemico-Biol. Interact. 2017, 272, 172–181. [Google Scholar] [CrossRef]
- Phan, T.P.D.; Pham, V.H.; Phan, D.C.; Vu, B.D. Synthesis and bioactivity of thiosemicarbazones containing adamantane skeletons. Molecules 2020, 25, 324. [Google Scholar] [CrossRef] [Green Version]
- Farag, A.M.; Mayhoub, A.S.; Barakat, S.E.; Bayomi, A.H. Synthesis of new N-phenylpyrazole derivatives with potent antimicrobial activity. Bioorg. Med. Chem. 2008, 16, 4569–4578. [Google Scholar] [CrossRef] [PubMed]
- Siwek, A.; Stefan´ska, J. Antimicrobial activity and SAR study of some novel thiosemicarbazide derivatives bearing piperidine moiety. J. Med. Chem. 2011, 7, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Wujec, M.; Kosikowska, U.; Paneth, P.; Malm, A. Reaction of Hydrazide of (Tetrazol-5-yl)acetic Acid with Isothiocyanates and Antimicrobial Investigations of Newly-Obtained Compounds. Heterocycles 2007, 71, 2617–2626. [Google Scholar] [CrossRef]
- Siwek, A.; Staczek, P.; Wujec, M.; Stefanska, J.; Kosikowska, U.; Malm, A.; Jankowski, S.; Paneth, P. Biological and docking studies of topoisomerase IV inhibition by thiosemicarbazides. J. Mol. Model. 2011, 17, 2297–2303. [Google Scholar] [CrossRef] [PubMed]
- Bhat, M.A.; Khan, A.A.; Khan, S.; Al-Omar, M.A.; Parvez, M.K.; Al-Dosari, M.S.; Al-Dhfyan, A. Synthesis and anti-Candidal activity of N-(4-aryl/cyclohexyl)2-(pyridine-4-yl carbonyl) hydrazinecarbothioamide. Bioorg. Med. Chem. Lett. 2014, 24, 1299–1302. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Jabeen, M.; Chauhan, A.; Owais, M. Vaccine potential of cytosolic proteins loaded fibrin microspheres of Cryptococcus neoformans in BALB/c mice. J. Drug Target. 2012, 20, 453–466. [Google Scholar] [CrossRef]
- Khan, A.A.; Alanazi, A.M.; Jabeen, M.; Khan, S.; Malik, A. Additive potential of combination therapy against cryptococcosis employing a novel amphotericin B and fluconazole loaded dual delivery system. Eur. J. Pharma. Sci. 2018, 119, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Amaral, A.C.; Marques, A.F.; Muñoz, J.E.; Bocca, A.L.; Simioni, A.R.; Tedesco, A.C.; Morais, P.C.; Travassos, L.R.; Taborda, C.P.; Felipe, M.S.S. Poly(lactic acid-glycolic acid) nanoparticles markedly improve immunological protection provided by peptide P10 against murine Paracoccidioidomycosis. Br. J. Pharmacol. 2010, 159, 1126–1132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saadat, E.; Dinarvand, R.; Ebrahimnejad, P. Encapsulation of nystatin in nanoliposomal formulation: Characterization, stability study and antifungal activity against Candida albicans. Pharm. Biomed. Res. 2016, 2, 44–54. [Google Scholar] [CrossRef]
- Veloso, D.F.M.C.; Benedetti; Naiara, I.G.M.; Avila, R.I.; Bastos, T.S.A.; Silva, T.C.; Silva, M.R.R.; Batista, A.C.; Valadares, M.C.; Lima, E.M. Intravenous delivery of a liposomal formulation of voriconazole improves drug pharmacokinetics, tissue distribution, and enhances antifungal activity. Drug Del. 2018, 25, 1585–1594. [Google Scholar] [CrossRef] [Green Version]
- Kenechukwu, F.C.; Attama, A.A.; Ibezim, E.C. Novel solidified reverse micellar solution-based mucoadhesive nano lipid gels encapsulating miconazole nitrate-loaded nanoparticles for improved treatment of oropharyngeal candidiasis. J. Microencapsul. 2017, 34, 592–609. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Liang, Y.; Zhu, Y.; Xie, C.; Yao, A.; Chen, L.; Jiang, Q.; Liu, T.; Wang, X.; Qian, Y.; et al. Anti-transferrin receptor-modified amphotericin B-loaded PLA–PEG nanoparticles cure candida meningitis and reduce drug toxicity. Int. J. Nanomed. 2015, 10, 6227. [Google Scholar] [CrossRef] [Green Version]
- Ling, X.; Huang, Z.; Wang, J.; Xie, J.; Feng, M.; Chen, Y.; Abbas, F.; Tu, J.; Wu, J.; Sun, C. Development of an itraconazole encapsulated polymeric nanoparticle platform for effective antifungal therapy. J. Mater. Chem. B 2016, 4, 1787–1796. [Google Scholar] [CrossRef]
- Khan, A.A.; Jabeen, M.; Alanazi, A.M.; Khan, A.A. Antifungal efficacy of amphotericin B encapsulated fibrin microsphere for treating Cryptococcus neoformans infection in Swiss albino mice. Braz. J. Infect. Dis. 2016, 20, 342–348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clinical Laboratory Standard Institute. Reference Method for Broth Dilution; Clinical Laboratory Standard Institute: Wayne, PA, USA, 2008; ISBN 1562388649. [Google Scholar]
- Khan, A.A.; Jabeen, M.; Khan, A.A.; Owais, M. Anticancer efficacy of a novel propofol–linoleic acid-loaded escheriosomal formulation against murine hepatocellular carcinoma. Nanomedicine 2013, 8, 1281–1294. [Google Scholar] [CrossRef]
- Tang, X.; Zhu, H.; Sun, L.; Hou, W.; Cai, S.; Zhang, R.; Liu, F. Enhanced antifungal effects of amphotericin B-TPGS-b-(PCL-ran-PGA) nanoparticles in vitro and in vivo. Int. J. Nanomed. 2014, 9, 5403–5413. [Google Scholar]
- Rauzi, F.; Smyth, E.; Emerson, M. Refinement of mouse protocols for the study of platelet thromboembolic responses in vivo. Thromb. Haemost. 2017, 117, 2283–2290. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Huo, M.; Zhou, J.; Xie, S. PKSolver: An add-in program for pharmacokinetic and pharmacodynamic data analysis in Microsoft Excel. Comput. Methods Programs Biomed. 2010, 99, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Zou, J.; Li, Z.; Tian, J.; Abdelalim, S.; Du, F.; She, R.; Wang, D.; Tan, C.; Wang, H.; et al. Study of histopathological and molecular changes of rat kidney under simulated weightlessness and resistance training protective effect. PLoS ONE 2011, 6, e20008. [Google Scholar] [CrossRef]
- Khan, A.A.; Alanazi, A.M.; Jabeen, M.; Hassan, I.; Bhat, M.A. Targeted nano-delivery of novel omega-3 conjugate against hepatocellular carcinoma: Regulating COX-2/bcl-2 expression in an animal model. Biomed. Pharmacother. 2016, 81, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Bhat, M.A.; Al-Dhfyan, A.; Naglah, A.M.; Khan, A.A.; Al-Omar, M.A. Lead optimization of 2-Cyclohexyl-N-[(Z)-(3-methoxyphenyl/3hydroxyphenyl)methylidene]hydrazinecarbothioamides for targeting the HER-2 overexpressed breast cancer cell line SKBr-3. Molecules 2015, 20, 18246–18263. [Google Scholar] [CrossRef] [Green Version]
- Bhat, M.A.; Khan, A.A.; Khan, S.; Al-Omar, M.A.; Khan, A.A. Synthesis and anti-Candidal activity of some new pyrazoline derivatives. Biomed. Res. 2017, 28, 3082–3087. [Google Scholar]
- Mohammud, M.A.; Jesmin, M.; Islam, M.K.; Khatun, F.; Azad, A.K. Antineoplastic activities of acetone thiosemicarbazone against Ehrlich Ascites carcinoma cells bearing mice. Med. J. Islamic World Acad. Sci. 2013, 21, 97–104. [Google Scholar]
- Ksiezopolska, E.; Gabald, T. Evolutionary emergence of drug resistance in Candida opportunistic pathogens. Genes 2018, 9, 461. [Google Scholar] [CrossRef] [Green Version]
- Kumari, A.; Yadav, S.K.; Yadav, S.C. Biodegradable polymeric nanoparticles based drug delivery systems. Colloids Surf. B Biointerfaces. 2010, 75, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Park, K. Controlled drug delivery systems: Past forward and future back. J. Control Release 2014, 190, 3–8. [Google Scholar] [CrossRef] [Green Version]
- Stone, N.R.H.; Bicanic, T.; Salim, R.; Hope, W. Liposomal amphotericin B (AmBisome®): A review of the pharmacokinetics, pharmacodynamics, clinical experience and future directions. Drugs 2016, 76, 485–500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soliman, G.M. Nanoparticles as safe and effective delivery systems of antifungal agents: Achievements and challenges. Int. J. Pharm. 2017, 523, 15–32. [Google Scholar] [CrossRef]
- Akhtar, N. Vesicles: A recently developed novel carrier for enhanced topical drug delivery. Curr. Drug Del. 2014, 11, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, E.; Fatima, M.T.; Owais, M.; Saleemuddin, M. Beaded plasma clot: A potent sustained-release, drug-delivery system. Thera. Del. 2011, 2, 573–583. [Google Scholar] [CrossRef] [PubMed]
- Burgess, B.L.; He, Y.; Baker, M.M.; Luo, B.; Carroll, S.F.; Forte, T.M.; Oda, M.N. NanoDisk containing super aggregated amphotericin B: A high therapeutic index antifungal formulation with enhanced potency. Int. J. Nanomed. 2013, 8, 4733–4743. [Google Scholar]
- Pattni, B.S.; Chupin, V.V.; Torchilin, V.P. New developments in liposomal drug delivery. Chem. Rev. 2015, 115, 10938–10966. [Google Scholar] [CrossRef]
- Lionakis, M.S.; Lim, J.K.; Lee, C.C.; Murphy, P.M. Organ-specific innate immune responses in a mouse model of invasive candidiasis. J. Innate Immun. 2011, 3, 180–199. [Google Scholar] [CrossRef] [Green Version]
- Jia, C.; Zhang, J.; Yu, L.; Wang, C.; Yang, Y.; Rong, X.; Xu, K.; Chu, M. Antifungal activity of coumarin against Candida albicans is related to apoptosis. Front Cell Infect. Microbiol. 2019, 8, 445. [Google Scholar] [CrossRef] [Green Version]
- Lone, S.A.; Wani, M.Y.; Fru, P.; Ahmad, A. Cellular apoptosis and necrosis as therapeutic targets for novel Eugenol Tosylate Congeners against Candida albicans. Sci. Rep. 2020, 10, 1191–1206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramsdale, M. Programmed cell death in pathogenic fungi. Biochim. Biophys. Acta. 2008, 1783, 1369–1380. [Google Scholar] [CrossRef] [Green Version]
- Rockenfeller, P.; Madeo, F. Apoptotic death of ageing yeast. Exp. Gerontol. 2008, 43, 876–881. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Formulations | Particle Size | Zeta Potential (mV) | Entrapment Efficiency (%) | Loading Efficiency (%) |
|---|---|---|---|---|
| 2C-L | 200–300 nm | −23.35 ± 1.2 | 78.5 ± 5.2 | 9.63 ± 1.2 |
| 2C-FL | 1.0–1.3 mm | −34.12 ± 3.3 | 72.6 ± 4.7 | 9.21 ± 2.3 |
| Formulations | Cmax (µg/mL) | AUC0–24 (µg/mL x h) | CL (mL/h) |
|---|---|---|---|
| Free 2C 2C-F 2C-L 2C-FL | 1.4 ± 0.25 2.8 ± 0.44 5.32 ± 1.8 * 6.81 ± 2.5 * | 0.91 ± 0.17 1.79 ± 0.32 4.35 ± 2.3 * 5.94 ± 3.7 * | 76.63 ± 7.7 66.73 ± 7.2 58.34 ± 5.2 43.31 ± 8.4 |
| Healthy Control | Free 2C | 2C-F | 2C-L | 2C-FL | ||
|---|---|---|---|---|---|---|
| Creatinine (mg%) | Day 0 Day 6 | 0.28 ± 0.07 0.29 ± 0.04 | 0.29 ± 0.06 0.34 ± 0.05 | 0.28 ± 0.03 0.31 ± 0.02 | 0.27 ± 0.03 0.30 ± 0.05 | 0.28 ± 0.02 0.26 ± 0.03 |
| ALT (U/I) | Day 0 Day 6 | 40.5 ± 6.5 40.2 ± 4.2 | 40.9 ± 7.3 45.1 ± 8.5 | 41.1 ± 5.6 42.6 ± 6.2 | 39.9 ± 6.6 41.4 ± 5.3 | 40.3 ± 8.2 40.9 ± 5.9 |
| Total Bilirubin | Day 0 Day 6 | 0.16 ± 0.06 0.18 ± 0.03 | 0.15 ± 0.04 0.21 ± 0.07 | 0.15 ± 0.07 0.20 ± 0.04 | 0.17 ± 0.02 0.19 ± 0.08 | 0.16 ± 0.01 0.17 ± 0.05 |
| Formulations | MIC (µg/mL) |
|---|---|
| Free 2C 2C-F 2C-L 2C-FL | 0.46 ± 0.05 2.63 ± 0.18 5.11 ± 0.32 4.92 ± 0.76 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, A.A.; Alanazi, A.M.; Alsaif, N.; Algrain, N.; Wani, T.A.; Bhat, M.A. Enhanced Efficacy of Thiosemicarbazone Derivative-Encapsulated Fibrin Liposomes against Candidiasis in Murine Model. Pharmaceutics 2021, 13, 333. https://doi.org/10.3390/pharmaceutics13030333
Khan AA, Alanazi AM, Alsaif N, Algrain N, Wani TA, Bhat MA. Enhanced Efficacy of Thiosemicarbazone Derivative-Encapsulated Fibrin Liposomes against Candidiasis in Murine Model. Pharmaceutics. 2021; 13(3):333. https://doi.org/10.3390/pharmaceutics13030333
Chicago/Turabian StyleKhan, Azmat Ali, Amer M. Alanazi, Nawaf Alsaif, Nasser Algrain, Tanveer Ahmad Wani, and Mashooq Ahmad Bhat. 2021. "Enhanced Efficacy of Thiosemicarbazone Derivative-Encapsulated Fibrin Liposomes against Candidiasis in Murine Model" Pharmaceutics 13, no. 3: 333. https://doi.org/10.3390/pharmaceutics13030333
APA StyleKhan, A. A., Alanazi, A. M., Alsaif, N., Algrain, N., Wani, T. A., & Bhat, M. A. (2021). Enhanced Efficacy of Thiosemicarbazone Derivative-Encapsulated Fibrin Liposomes against Candidiasis in Murine Model. Pharmaceutics, 13(3), 333. https://doi.org/10.3390/pharmaceutics13030333







