Spray-Dried Inhalable Powder Formulations of Gentamicin Designed for Pneumonic Plague Therapy in a Mouse Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Powder Formulations
2.3. Scanning Electron Microscopy (SEM)
2.4. Particle Size
2.5. Differential Scanning Calorimetry (DSC)
2.6. X-ray Powder Diffraction (XRPD)
2.7. Density and Fluidity
2.8. Hygroscopicity and Hygroscopic Curve
2.9. High-Performance Liquid Chromatography (HPLC)
2.10. Aerodynamic Particle Size Distribution Analysis
2.11. Pharmacodynamic Study In Vivo
2.11.1. Animals
2.11.2. Bacteria Strain
2.11.3. Animal Administration and Treatment
2.11.4. Clinical Signs and Survival Rate
2.11.5. Bacterial Count
2.11.6. Histopathology
2.12. Statistical Analysis
3. Results
3.1. Optimization of Spray-Drying Process Parameters
3.2. Physicochemical Properties of the Optimized GM Spray-Dried Powders
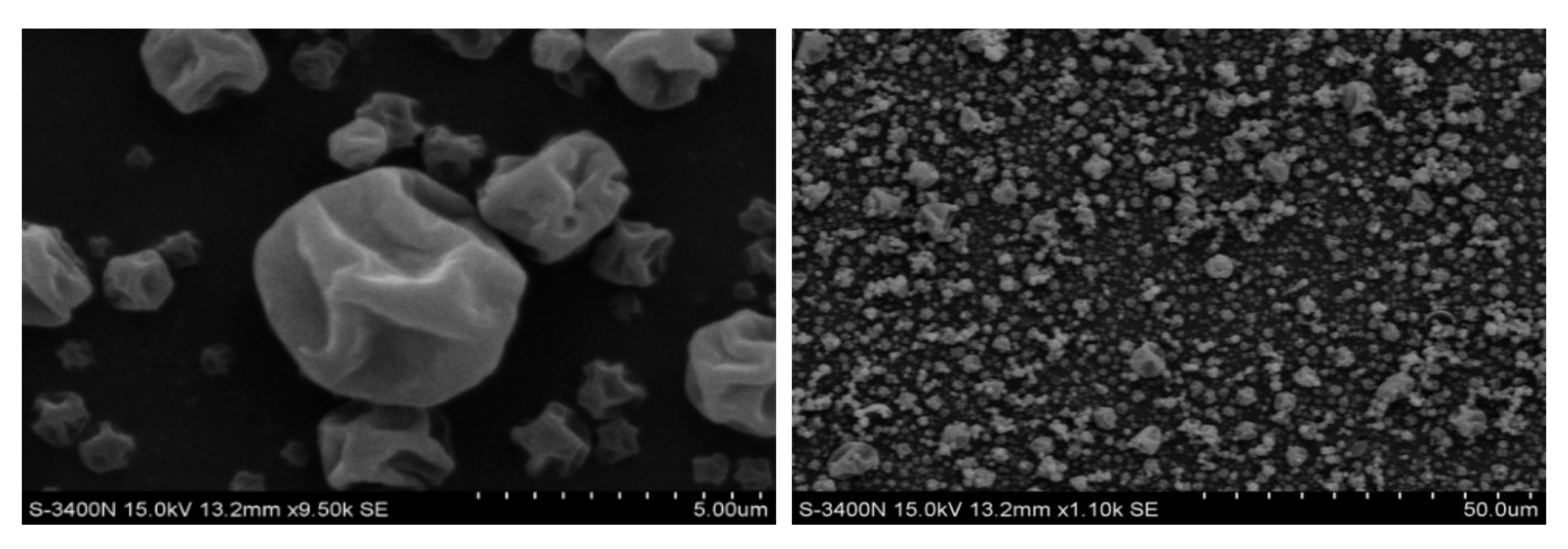
3.2.1. Particle Morphology
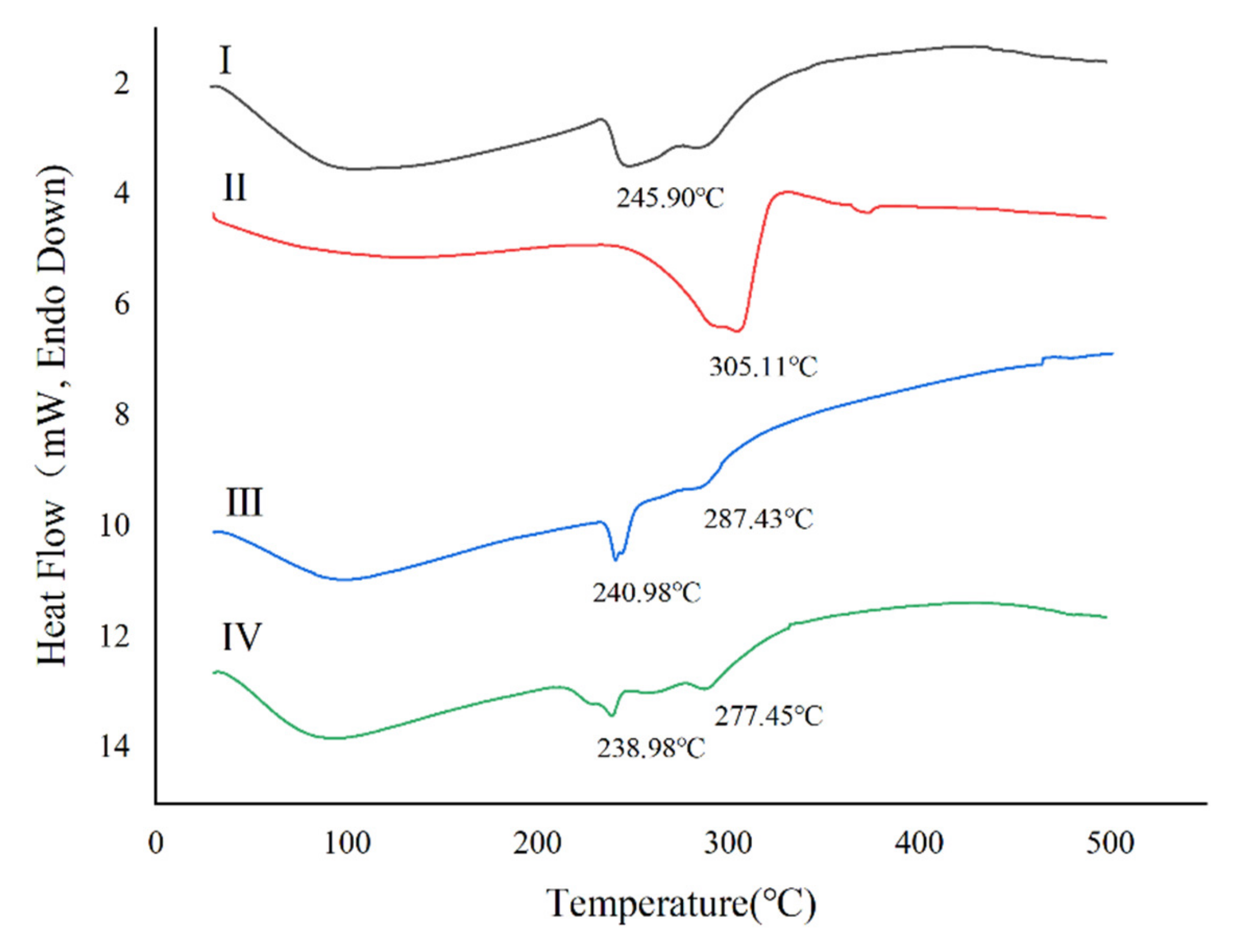
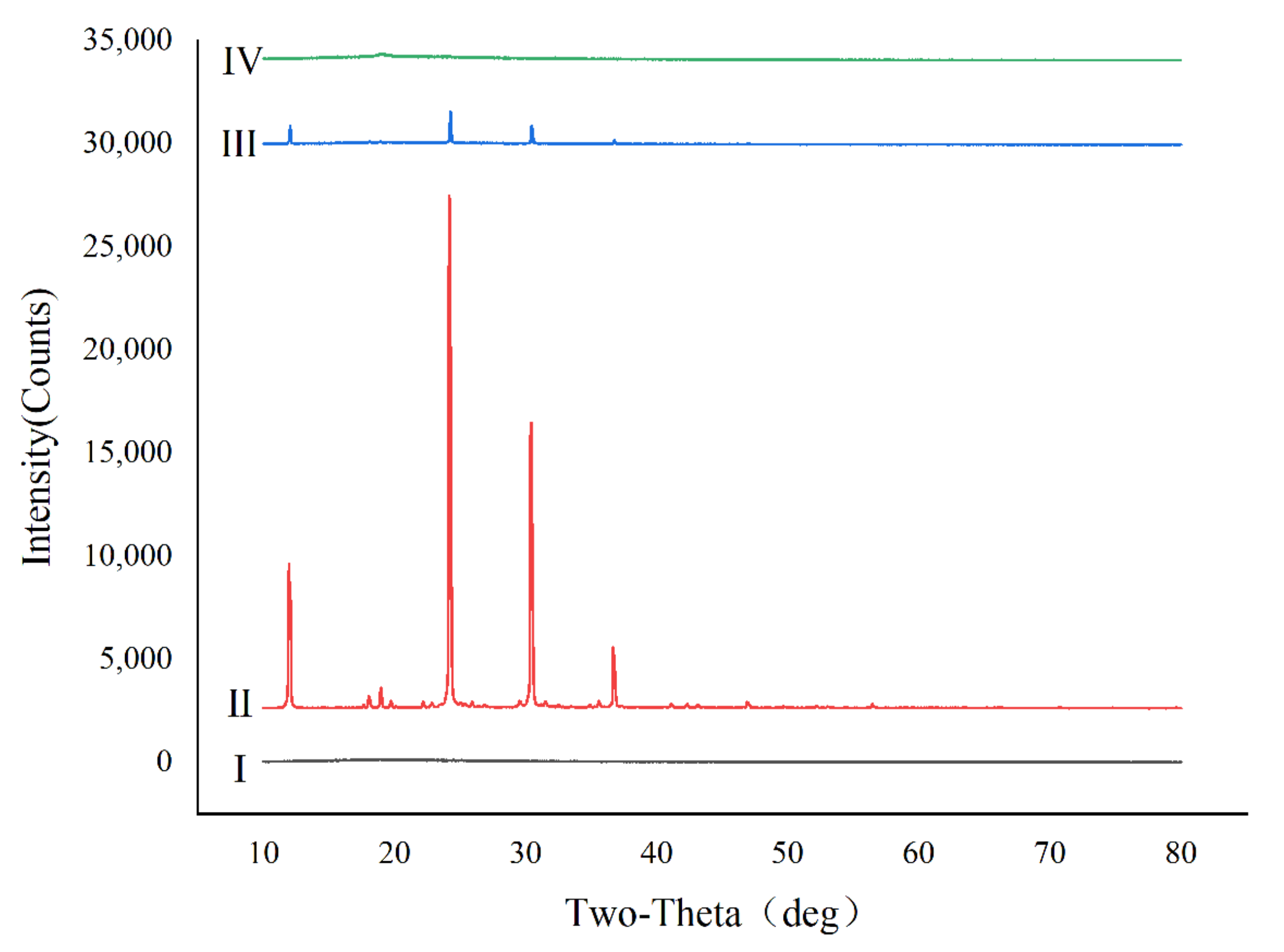
3.2.2. Thermal Analysis and Powder Crystallinity
3.2.3. The Tapped Density, Fluidity, and Hygroscopicity
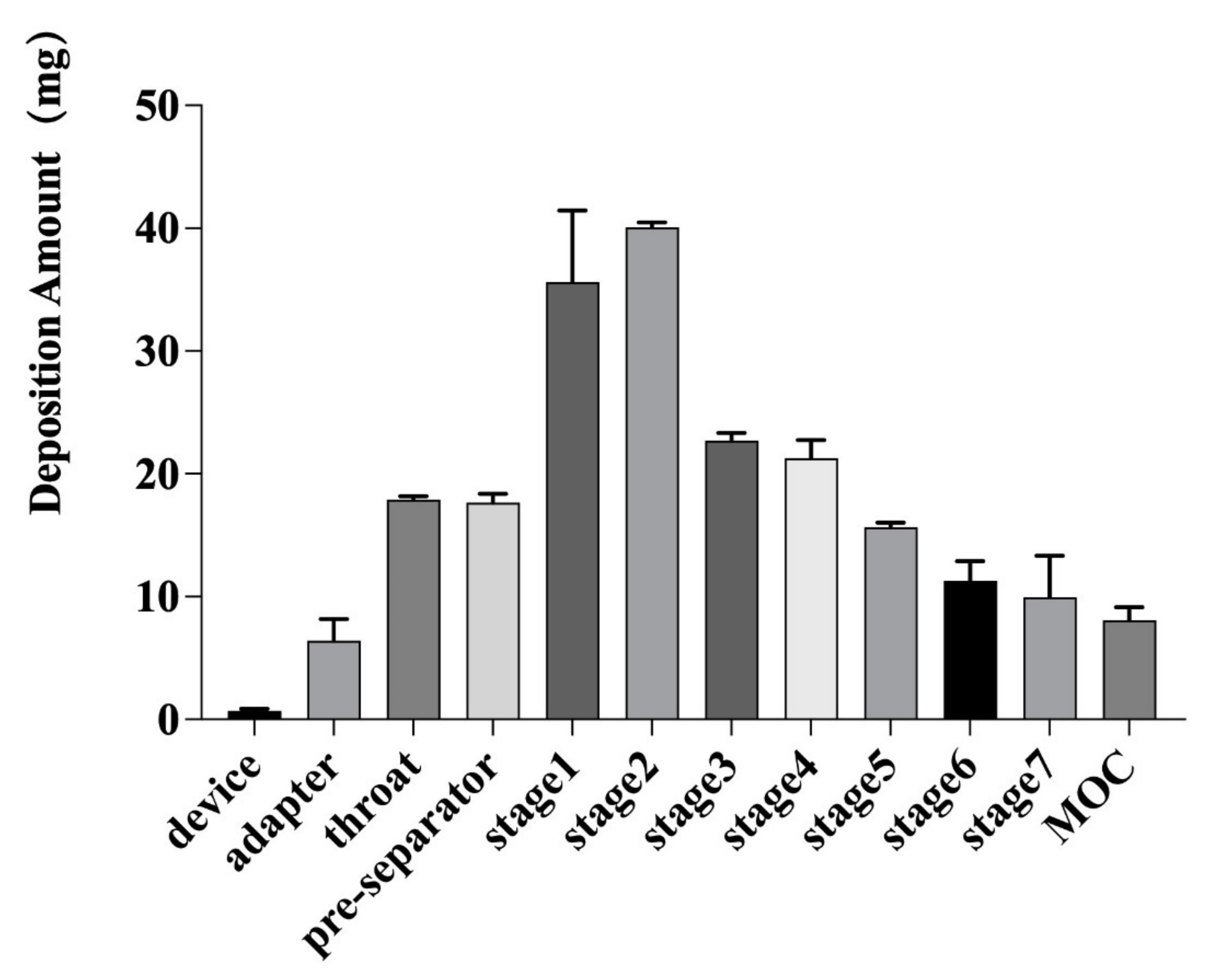
3.2.4. In Vitro Lung Deposition Rate
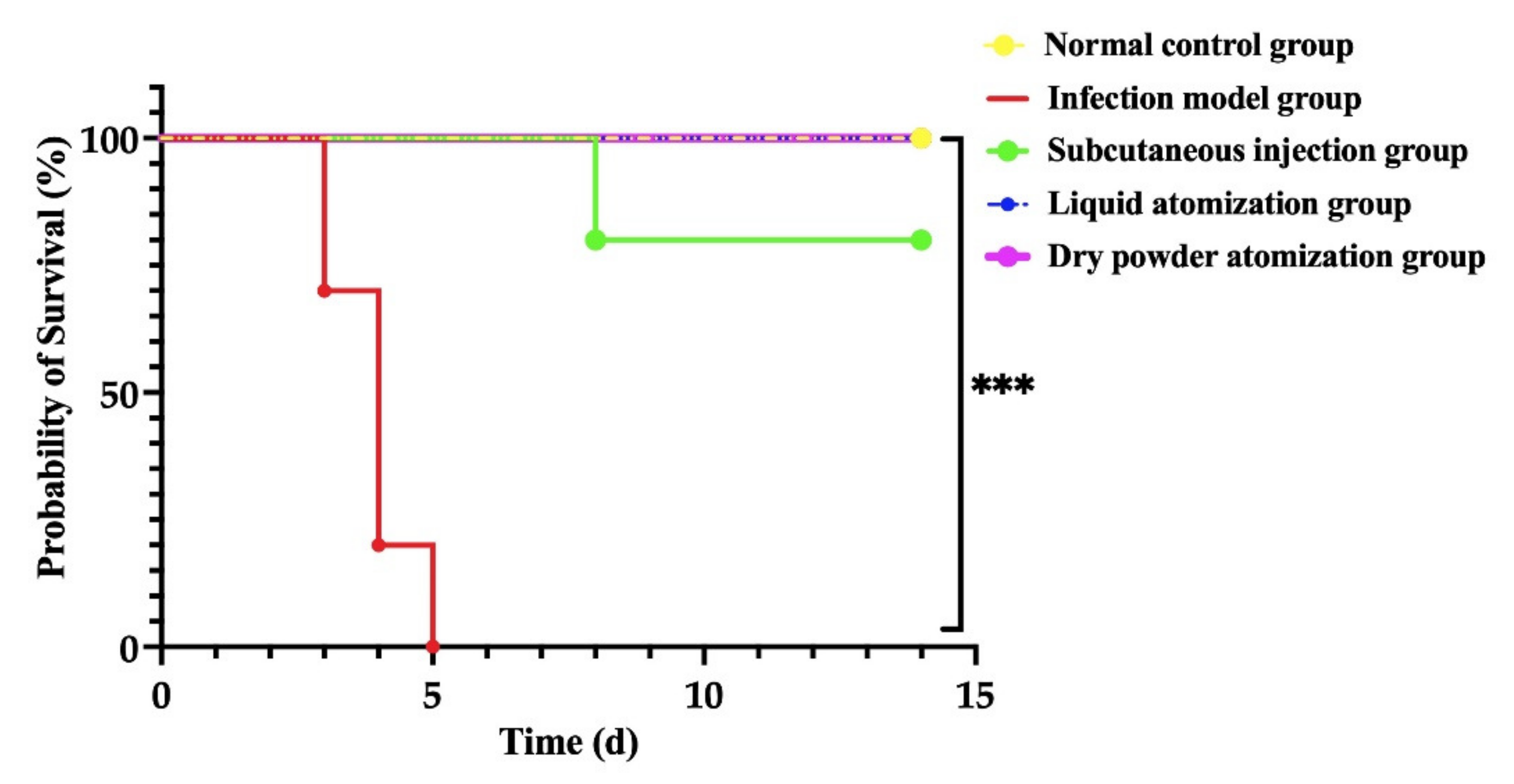
3.3. GM Spray-Dried Powders Effectively Protected Mice Infected with Y. pestis
3.3.1. Protection Efficacy after Aerosol Challenge with 50× LD50 of Y. pestis Strain 201
3.3.2. Bacterial Enumeration from Mouse Organs after Administration of GM
3.3.3. Histopathological Analysis of Mouse Tissues after Immunization and Challenge
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Welch, T.J.; Fricke, W.F.; McDermott, P.F.; White, D.G.; Rosso, M.; Rasko, D.A.; Mammel, M.K.; Eppinger, M.; Rosovitz, M.J.; Wagner, D.; et al. Multiple Antimicrobial Resistance in Plague: An Emerging Public Health Risk. PLoS ONE 2007, 2, e309. [Google Scholar] [CrossRef] [Green Version]
- Hamblin, K.A.; Armstrong, S.J.; Barnes, K.B.; Davies, C.; Laws, T.; Blanchard, J.D.; Harding, S.V.; Atkins, H.S. Inhaled Liposomal Ciprofloxacin Protects against a Lethal Infection in a Murine Model of Pneumonic Plague. Front. Microbiol. 2017, 8, 91. [Google Scholar] [CrossRef] [PubMed]
- Godfred-Cato, S.; Cooley, K.M.; Fleck-Derderian, S.; Becksted, H.A.; Russel, Z.; Meaney-Delman, D.; Mead, P.S.; Nelson, C.A. Treatment of Human Plague: A Systematic Review of Published Aggregate Data on Antimicrobial Efficacy, 1939–2019. Clin. Infect. Dis. 2020, 70, S11–S19. [Google Scholar] [CrossRef] [PubMed]
- Qazi, S.; Ullah, I.; Jabbar, A.; Junaid Tahir, M. Plague Outbreaks in Africa—A Gesture of New Pandemic. Disaster Med. Public Health Prep. 2022. [Google Scholar] [CrossRef] [PubMed]
- Rahelinirina, S.; Harimalala, M.; Margueron, T.; Ramihangihajason, T.; Mansotte, F.; Rajerison, M.; Pagès, F.; Boyer, S. Risk of maritime introduction of plague from Madagascar to Mayotte. Acta Trop. 2018, 187, 140–143. [Google Scholar] [CrossRef]
- Nguyen, V.K.; Parra-Rojas, C.; Hernandez-Vargas, E.A. The 2017 plague outbreak in Madagascar: Data descriptions and epidemic modelling. Epidemics 2018, 25, 20–25. [Google Scholar] [CrossRef]
- Inglesby, T.V.; Dennis, D.T.; Henderson, D.A.; Bartlett, J.G.; Ascher, M.S.; Eitzen, E.; Fine, A.D.; Friedlander, A.M.; Hauer, J.; Koerner, J.F.; et al. Plague as a biological weapon: Medical and public health management. JAMA 2000, 283, 2281–2290. [Google Scholar] [CrossRef]
- Kugeler, K.J.; Staples, J.E.; Hinckley, A.F.; Gage, K.L.; Mead, P.S. Epidemiology of human plague in the United States, 1900–2012. Emerg. Infect. Dis. 2015, 21, 16–22. [Google Scholar] [CrossRef]
- Ansari, I.; Grier, G.; Byers, M. Deliberate release: Plague—A review. J. Biosaf. Biosecur. 2020, 2, 10–22. [Google Scholar] [CrossRef]
- Richard, V.; Riehm, J.M.; Herindrainy, P.; Soanandrasana, R.; Ratsitoharina, M.; Rakotomanana, F.; Andrianalimanana, S.; Scholz, H.C.; Rajerison, M. Pneumonic plague outbreak, Northern Madagascar, 2011. Emerg. Infect. Dis. 2015, 21, 8–15. [Google Scholar] [CrossRef]
- Gur, D.; Glinert, I.; Aftalion, M.; Vagima, Y.; Levy, Y.; Rotem, S.; Zauberman, A.; Tidhar, A.; Tal, A.; Maoz, S.; et al. Inhalational gentamicin treatment is effective against pneumonic plague in a mouse model. Front Microbiol. 2018, 9, 741. [Google Scholar] [CrossRef]
- Kool, J.L.; Weinstein, R.A. Risk of person-to-person transmission of pneumonic plague. Clin. Infect. Dis. 2005, 40, 1166–1172. [Google Scholar] [CrossRef]
- Nelson, C.A.; Fleck-Derderian, S.; Cooley, K.M.; Meaney-Delman, D.; Becksted, H.A.; Russell, Z.; Renaud, B.; Bertherat, E.; Mead, P.S. Antimicrobial Treatment of Human Plague: A Systematic Review of the Literature on Individual Cases, 1937–2019. Clin. Infect. Dis. 2020, 70, S3–S10. [Google Scholar] [CrossRef]
- Nelson, C.A.; Meaney-Delman, D.; Fleck-Derderian, S.; Cooley, K.M.; Yu, P.A.; Mead, P.S. Antimicrobial treatment and prophylaxis of plague: Recommendations for naturally acquired infections and bioterrorism response. MMWR Recomm. Rep. 2021, 70, 1–27. [Google Scholar] [CrossRef]
- Boulanger, L.L.; Ettestad, P.; Fogarty, J.D.; Dennis, D.T.; Romig, D.; Mertz, G. Gentamicin and tetracyclines for the treatment of human plague: Review of 75 cases in new Mexico, 1985–1999. Clin. Infect. Dis. 2004, 38, 663–669. [Google Scholar] [CrossRef] [Green Version]
- Mwengee, W.; Butler, T.; Mgema, S.; Mhina, G.; Almasi, Y.; Bradley, C.; Formanik, J.B.; Rochester, C.G. Treatment of plague with gentamicin or doxycycline in a randomized clinical trial in Tanzania. Clin. Infect. Dis. 2006, 42, 614–621. [Google Scholar] [CrossRef]
- Yi, X.C.; Zhang, L.X.; Zhang, Y.N. Progress of pestis treatment strategy. Chin. J. Zoohoses 2022, 38, 830–838. [Google Scholar] [CrossRef]
- Douafer, H.; Andrieu, V.; Brunel, J.M. Scope and limitations on aerosol drug delivery for the treatment of infectious respiratory diseases. J. Control Release 2020, 325, 276–292. [Google Scholar] [CrossRef]
- Flume, P.A.; VanDevanter, D.R. Clinical applications of pulmonary delivery of antibiotics. Adv. Drug. Deliv. Rev. 2015, 85, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.Y.; Yang, F.F.; Liao, Y.H. Application of prodrug technology in the development of pulmonary inhaled drugs. Acta Pharm. Sin. 2021, 56, 2597–2611. [Google Scholar] [CrossRef]
- Zhou, X.H.; Zhang, C.F.; Yang, M.; Miao, Z.J.; Wang, Y.J. Research progress in evaluation methods of pulmonary inhalation preparations. Drug Eval. Res. 2019, 42, 1891–1895. [Google Scholar] [CrossRef]
- Garcia-Contreras, L.; Yadav, K.S. Inhaled Formulation Design for the Treatment of Lung Infections. Curr. Pharm. Des. 2015, 21, 3875–3901. [Google Scholar] [CrossRef] [PubMed]
- Shiehzadeh, F.; Tafaghodi, M.; Dehghani, M.L.; Mashhoori, F.; FazlyBazzaz, B.S.; Imenshahidi, M. Preparation and characterization of a dry powder inhaler composed of plga large porous particles encapsulating gentamicin sulfate. Adv. Pharm. Bull. 2019, 9, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Alhajj, N.; O’Reilly, N.J.; Cathcart, H. Leucine as an excipient in spray dried powder for inhalation. Drug Discov. Today 2021, 26, 2384–2396. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Wan, W.; Lu, J.; Quan, G.; Pan, X.; Liu, P. Effects of L-leucine on the properties of spray-dried swellable microparticles with wrinkled surfaces for inhalation therapy of pulmonary fibrosis. Int. J. Pharm. 2021, 610, 121223. [Google Scholar] [CrossRef]
- Chew, N.Y.; Shekunov, B.Y.; Tong, H.H.; Chow, A.H.; Savage, C.; Wu, J.; Chan, H.K. Effect of amino acids on the dispersion of disodium cromoglycate powders. J. Pharm. Sci. 2005, 94, 2289–2300. [Google Scholar] [CrossRef]
- Li, H.; Zhang, M.; Xiong, L.; Feng, W.; Williams, R.O., 3rd. Bioavailability improvement of carbamazepine via oral administration of modified-release amorphous solid dispersions in rats. Pharmaceutics 2020, 12, 1023. [Google Scholar] [CrossRef]
- Zhang, W.; Song, X.; Zhai, L.; Guo, J.; Zheng, X.; Zhang, L.; Lv, M.; Hu, L.; Zhou, D.; Xiong, X.; et al. Complete Protection Against Yersinia pestis in BALB/c Mouse Model Elicited by Immunization with Inhalable Formulations of rF1-V10 Fusion Protein via Aerosolized Intratracheal Inoculation. Front. Immunol. 2022, 13, 793382. [Google Scholar] [CrossRef]
- Russo, P.; Stigliani, M.; Prota, L.; Auriemma, G.; Crescenzi, C.; Porta, A.; Aquino, R.P. Gentamicin and leucine inhalable powder: What about antipseudomonal activity and permeation through cystic fibrosis mucus? Int. J. Pharm. 2013, 440, 250–255. [Google Scholar] [CrossRef]
- Lee, M.J.; Seo, D.Y.; Lee, H.E.; Wang, I.C.; Kim, W.S.; Jeong, M.Y.; Choi, G.J. In line NIR quantification of film thickness on pharmaceutical pellets during a fluid bed coating process. Int. J. Pharm. 2011, 403, 66–72. [Google Scholar] [CrossRef]
- Parlati, C.; Colombo, P.; Buttini, F.; Young, P.M.; Adi, H.; Ammit, A.J.; Traini, D. Pulmonary spray dried powders of tobramycin containing sodium stearate to improve aerosolization efficiency. Pharm. Res. 2009, 26, 1084–1092. [Google Scholar] [CrossRef]
- Puri, V.; Chaudhary, K.R.; Singh, A.; Singh, C. Inhalation potential of N-Acetylcysteine loaded PLGA nanoparticles for the management of tuberculosis: In vitro lung deposition and efficacy studies. Curr. Res. Pharmacol. Drug Discov. 2022, 18, 100084. [Google Scholar] [CrossRef]
- Young, P.M.; Edge, S.; Traini, D.; Jones, M.D.; Price, R.; El-Sabawi, D.; Urry, C.; Smith, C. The influence of dose on the performance of dry powder inhalation systems. Int. J. Pharm. 2005, 296, 26–33. [Google Scholar] [CrossRef]
- Nemati, E.; Mokhtarzadeh, A.; Panahi-Azar, V.; Mohammadi, A.; Hamishehkar, H.; Mesgari-Abbasi, M.; Dolatabadi, J.E.N.; de la Guardia, M. Ethambutol-loaded solid lipid nanoparticles as dry powder inhalable formulation for tuberculosis therapy. AAPS Pharmscitech. 2019, 20, 120. [Google Scholar] [CrossRef]
- Geller, D.E. Aerosol antibiotics in cystic fibrosis. Respir Care 2009, 54, 658–670. [Google Scholar] [CrossRef]
- Dolatabadi, J.E.N.; Hamishehkar, H.; Valizadeh, H. Development of dry powder inhaler formulation loaded with alendronate solid lipid nanoparticles: Solid-state characterization and aerosol dispersion performance. Drug Dev. Ind. Pharm. 2015, 41, 1431–1437. [Google Scholar] [CrossRef]
- Zhou, Q.; Loh, Z.H.; Yu, J.; Sun, S.P.; Gengenbach, T.; Denman, J.A.; Li, J.; Chan, H.K. How Much Surface Coating of Hydrophobic Azithromycin Is Sufficient to Prevent Moisture-Induced Decrease in Aerosolisation of Hygroscopic Amorphous Colistin Powder? AAPS J. 2016, 18, 1213–1224. [Google Scholar] [CrossRef]
- Vasanthavada, M.; Tong, W.Q.; Joshi, Y.; Kislalioglu, M.S. Phase behavior of amorphous molecular dispersions I: Determination of the degree and mechanism of solid solubility. Pharm. Res. 2004, 21, 1598–1606. [Google Scholar] [CrossRef]
- Wang, X.; Michoel, A.; Mooter, G.V.D. Solid state characteristics of ternary solid dispersions composed of PVPVA64, Myrj 52 and itraconazole. Int. J. Pharm. 2005, 303, 54–61. [Google Scholar] [CrossRef]
- National Pharmacopoeia Commission. Pharmacopoeia of the People’s Republic of China, 2020 Edition Part 4; China Medical Science and Technology Press: Beijing, China, 2020; pp. 485–486. [Google Scholar]
- Zhao, J.; Liu, T.; Cai, B.Y.; Liu, P.; Qian, L. Determination of gentamicin residues in raw milk by HPLC. Food R&D 2015, 36, 94–97. [Google Scholar] [CrossRef]
- Della Porta, G.; Adami, R.; Del Gaudio, P.; Prota, L.; Aquino, R.; Reverchon, E. Albumin/gentamicin microspheres produced by supercritical assisted atomization: Optimization of size, drug loading and release. J. Pharm. Sci. 2010, 99, 4720–4729. [Google Scholar] [CrossRef] [PubMed]
- Kuehl, P.J.; De, S.; Eppler, B.; Marsters, J.; Matthews, L.; Reed, M.D.; Talton, J.D. Development and validation of an HPLC assay for dual detection of gentamicin sulfate and leucine from a novel dry powder for inhalation. J. Anal. Bioanal. Tech. 2012, 3, 1–4. [Google Scholar] [CrossRef]
- Hoe, S.; Young, P.M.; Chan, H.K.; Traini, D. Introduction of the electrical next generation impactor (eNGI) and investigation of its capabilities for the study of pressurized metered dose inhalers. Pharm. Res. 2009, 26, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.; Haghi, M.; Young, P.M.; Kappl, M.; Traini, D.; Jain, S. Highly respirable dry powder inhalable formulation of voriconazole with enhanced pulmonary bioavailability. Expert. Opin. Drug Deliv. 2016, 13, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Alipour, S.; Montaseri, H.; Tafaghodi, M. Preparation and characterization of biodegradable paclitaxel loaded alginate microparticles for pulmonary delivery. Colloids Surf. B Biointerfaces 2010, 81, 521–529. [Google Scholar] [CrossRef]
- Bakhtiary, Z.; Barar, J. Microparticles containing erlotinib-loaded solid lipid nanoparticles for treatment of non-small cell lung cancer. Drug Dev. Ind. Pharm. 2017, 43, 1244–1253. [Google Scholar] [CrossRef]
- Zhang, Q.; Wang, Q.; Tian, G.; Qi, Z.; Zhang, X.; Wu, X.; Qiu, Y.; Bi, Y.; Yang, X.; Xin, Y.; et al. Yersinia pestis biovar Microtus strain 201, an avirulent strain to humans, provides protection against bubonic plague in rhesus macaques. Hum. Vaccin. Immunother. 2014, 10, 368–377. [Google Scholar] [CrossRef] [Green Version]
- Yang, F.; Ke, Y.; Tan, Y.; Bi, Y.; Shi, Q.; Yang, H.; Qiu, J.; Wang, X.; Guo, Z.; Ling, H.; et al. Cell membrane is impaired, accompanied by enhanced type III secretion system expression in Yersinia pestis deficient in RovA regulator. PLoS ONE 2010, 5, e12840. [Google Scholar] [CrossRef] [Green Version]
- Feng, J.; Deng, Y.; Fu, M.; Hu, X.; Luo, W.; Lu, Z.; Dai, L.; Yang, H.; Zhao, X.; Du, Z.; et al. Construction of a live-attenuated vaccine strain of yersiniapestis EV76-B-shudpla and evaluation of its protection efficacy in a mouse model by aerosolized intratracheal inoculation. Front. Cell Infect. Microbiol. 2020, 10, 473. [Google Scholar] [CrossRef]
- Mao, L.; Hughes, A.; Evans, C. Application of effective data analysis (EDA) and abbreviated impaction method (AIM) in the metered dose inhaler (MDI) product screening. J. Aerosol. Med. Pulm. Drug Deliv. 2017, 30, A17. [Google Scholar]
- Pal, M.; Tsegaye, M.; Girzaw, F.; Bedada, H.; Godishala, V.; Kandi, V. An overview on biological weapons and bioterrorism. J. Biomed. Res. 2017, 5, 24–34. [Google Scholar] [CrossRef]
- Cipolla, D.; Blanchard, J.; Gonda, I. Development of liposomal ciprofloxacin to treat lung infections. Pharmaceutics 2016, 8, 6. [Google Scholar] [CrossRef] [Green Version]
- Littringer, E.M.; Mescher, A.; Eckhard, S.; Schröttner, H.; Langes, C.; Fries, M.; Griesser, U.; Walzel, P.; Urbanetz, N.A. Spray drying of mannitol as a drug carrier—The impact of process parameters on product properties. Dry Technol. 2012, 30, 114–124. [Google Scholar] [CrossRef]
- Aquino, R.P.; Prota, L.; Auriemma, G.; Santoro, A.; Mencherini, T.; Colombo, G.; Russo, P. Dry powder inhalers of gentamicin and leucine: Formulation parameters, aerosol performance and in vitro toxicity on CuFi1 cells. Int. J. Pharm. 2012, 426, 100–107. [Google Scholar] [CrossRef]
- Chew, N.Y.; Chan, H.K. Use of solid corrugated particles to enhance powder aerosol performance. Pharm. Res. 2001, 18, 1570–1577. [Google Scholar] [CrossRef]


| Independent Factors | Values Used, Actual (Coded Value) | ||
|---|---|---|---|
| Low (1) | Medium (2) | High (3) | |
| A—Leu content (%, w/w) | 5 | 10 | 15 |
| B—inlet temperature (°C) | 100 | 120 | 140 |
| C—pump rate (%) | 10 | 15 | 20 |
| Dependent variables | Constraint | ||
| Y | Minimize | ||
| Batch | A | B | C | d50 (μm) | Yield (%) | Y |
|---|---|---|---|---|---|---|
| A1B1C3 | 1 | 1 | 3 | 5.67 | 73.21 | 0.30 |
| A1B2C2 | 1 | 2 | 2 | 5.18 | 74.20 | 0.23 |
| A1B2C1 | 1 | 2 | 1 | 5.89 | 74.03 | 0.32 |
| A2B3C1 | 2 | 3 | 1 | 4.76 | 76.11 | 0.16 |
| A2B1C3 | 2 | 1 | 3 | 4.03 | 80.06 | 0.05 |
| A2B1C2 | 2 | 1 | 2 | 4.10 | 78.47 | 0.07 |
| A3B2C2 | 3 | 2 | 2 | 3.90 | 85.43 | 0.00 |
| A3B3C1 | 3 | 3 | 1 | 4.41 | 81.25 | 0.09 |
| A3B3C3 | 3 | 3 | 3 | 4.20 | 83.39 | 0.05 |
| k1 | 0.85 | 0.42 | 0.57 | |||
| k2 | 0.28 | 0.55 | 0.30 | |||
| k3 | 0.14 | 0.30 | 0.40 | |||
| R | 0.71 | 0.25 | 0.27 |
| Factors | Sum of Squares | n | F | P |
|---|---|---|---|---|
| A | 0.059 | 2 | 39.493 | 0.025 |
| B | 0.001 | 2 | 1.000 | 0.500 |
| C | 0.004 | 2 | 2.843 | 0.260 |
| Error | 0.001 | 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, M.; Zhang, D.; Zhang, L.; Zhao, L.; Xu, L.; Wang, B.; Zhang, X.; Chen, J.; Bei, Z.; Wang, H.; et al. Spray-Dried Inhalable Powder Formulations of Gentamicin Designed for Pneumonic Plague Therapy in a Mouse Model. Pharmaceutics 2022, 14, 2646. https://doi.org/10.3390/pharmaceutics14122646
Zhu M, Zhang D, Zhang L, Zhao L, Xu L, Wang B, Zhang X, Chen J, Bei Z, Wang H, et al. Spray-Dried Inhalable Powder Formulations of Gentamicin Designed for Pneumonic Plague Therapy in a Mouse Model. Pharmaceutics. 2022; 14(12):2646. https://doi.org/10.3390/pharmaceutics14122646
Chicago/Turabian StyleZhu, Menghuan, Dongna Zhang, Lili Zhang, Liangliang Zhao, Likun Xu, Baogang Wang, Xinyu Zhang, Jinwei Chen, Zhuchun Bei, Hong Wang, and et al. 2022. "Spray-Dried Inhalable Powder Formulations of Gentamicin Designed for Pneumonic Plague Therapy in a Mouse Model" Pharmaceutics 14, no. 12: 2646. https://doi.org/10.3390/pharmaceutics14122646





