Dual-Enhanced Pluronic Nanoformulated Methotrexate-Based Treatment Approach for Breast Cancer: Development and Evaluation of In Vitro and In Vivo Efficiency
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Plain Mixed Pluronic Nanomicelles (MNMs) and MTX-Loaded MNMs (MTX-NMs)
2.3. Preparation of Plain Pluronic Nanomicelles (NMs) and PIP-Loaded NMs (PIP-NMs)
2.4. Characterization
2.5. In Vitro Drug Release Study
2.6. In Vitro Cytotoxicity Assay
2.7. Apoptosis/Necrosis Assay by Flow Cytometry
2.8. Cell Cycle Analysis
2.9. In Vivo Assessment
2.9.1. Tumor Weight and Volume Monitoring
2.9.2. Tumor Growth Biomarkers Measurements
2.9.3. Histopathological and Immunohistopathological Assessment
3. Results
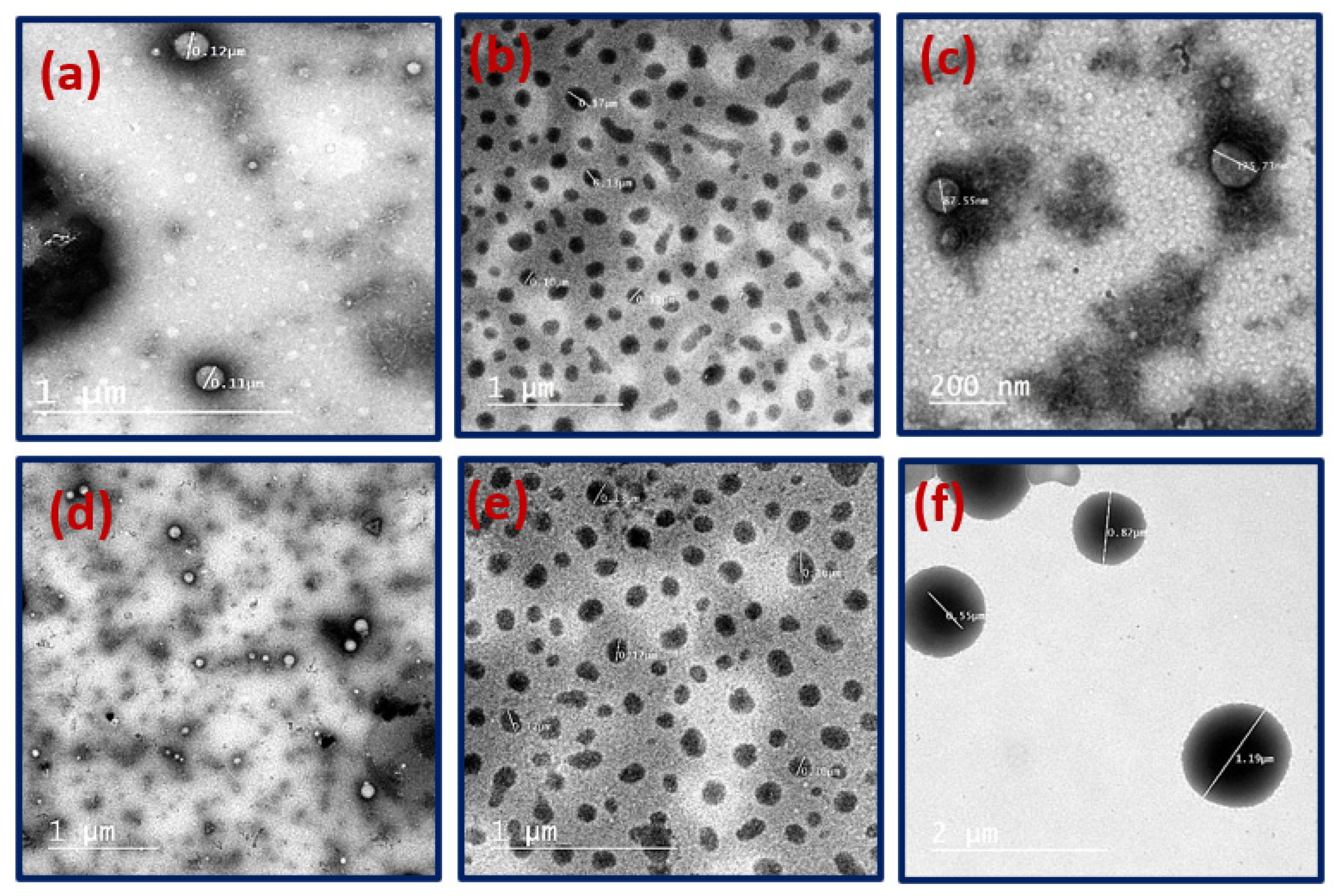
3.1. Preparation and Characterization of Plain and Drugs-Loaded Pluronic Nanomicelles
3.2. In Vitro Drug Release
3.3. In Vitro Cytotoxicity
3.4. Apoptosis/Necrosis Assay and Cell Cycle Analysis by Flow Cytometry
3.5. In Vivo Assessment
3.5.1. Tumor Volume and Weight Reduction Measurements
3.5.2. Tumor Growth Biomarkers Measurements
Cyclin D1 Concentration Assessment
p-38 MAPK Levels Assessment
Oxidative Stress Assessment
AKT Assessment and Tunnel Assay
3.5.3. Histopathology and Immunohistochemical Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- DeSantis, C.E.; Bray, F.; Ferlay, J.; Lortet-Tieulent, J.; Anderson, B.O.; Jemal, A. International variation in female breast cancer incidence and mortality rates. Cancer Epidemiol. Biomark. Prev. 2015, 24, 1495–1506. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Reddy Allugunti, V. Breast cancer detection based on thermographic images using machine learning and deep learning algorithms Healthcare View project Breast cancer detection based on thermographic images using machine learning and deep learning algorithms. Comput. Sci. 2022, 4, 49–56. [Google Scholar]
- Waks, A.G.; Winer, E.P. Breast Cancer Treatment: A Review. J. Am. Med. Assoc. 2019, 321, 288–300. [Google Scholar] [CrossRef]
- Brian, P.; Monahan, C.J.A. Cancer Chemotherapy: Principles and Practice. In Cancer Chemotherapy: Principles and Practice, 4th ed.; JB Lippincott: Philadelphia, PA, USA, 1990; pp. 110–153. [Google Scholar]
- Subramanian, S.; Kaufman, B.T. Interaction of methotrexate, folates, and pyridine nucleotides with dihydrofolate reductase: Calorimetric and spectroscopic binding studies. Proc. Natl. Acad. Sci. USA 1978, 75, 3201–3205. [Google Scholar] [CrossRef] [PubMed]
- Kaasgaard, T.; Andresen, T.L.; Jensen, S.S.; Holte, R.O.; Jensen, L.T.; Jørgensen, K. Liposomes containing alkylated methotrexate analogues for phospholipase A2 mediated tumor targeted drug delivery. Chem. Phys. Lipids 2009, 157, 94–103. [Google Scholar] [CrossRef]
- Cerqueira, P.; Noro, J.; Moura, S.; Guimarães, D.; Silva, C.; Cavaco-Paulo, A.; Loureiro, A. PTS micelles for the delivery of hydrophobic methotrexate. Int. J. Pharm. 2019, 566, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Bertino, J.R.; Göker, E.; Gorlick, R.; Li, W.W.; Banerjee, D. Resistance mechanisms to methotrexate in tumors. Stem Cells 1996, 14, 5–9. [Google Scholar] [CrossRef]
- Nobacci, G. Neoadjuvant chemotherapy for osteosarcoma of the extremities with synchronous lung metastases: Treatment with cisplatin, adriamycin and high dose of methotrexate and ifosfamide. Oncol. Rep. 2000, 7, 339–346. [Google Scholar] [CrossRef]
- Li, S.; Xiong, Y.; Zhang, X. Poloxamer surface modified trimethyl chitosan nanoparticles for the effective delivery of methotrexate in osteosarcoma. Biomed. Pharmacother. 2017, 90, 872–879. [Google Scholar] [CrossRef]
- Garg, N.K.; Singh, B.; Jain, A.; Nirbhavane, P.; Sharma, R.; Tyagi, R.K.; Kushwah, V.; Jain, S.; Katare, O.P. Fucose decorated solid-lipid nanocarriers mediate efficient delivery of methotrexate in breast cancer therapeutics. Colloids Surf. B Biointerfaces 2016, 146, 114–126. [Google Scholar] [CrossRef] [PubMed]
- Matsuoka, H.; Ohi, N.; Mihara, M.; Suzuki, H.; Miyamoto, K.; Maruyama, N.; Tsuji, K.; Kato, N.; Akimoto, T.; Takeda, Y.; et al. Antirheumatic agents: Novel methotrexate derivatives bearing a benzoxazine or benzothiazine moiety. J. Med. Chem. 1997, 40, 105–111. [Google Scholar] [CrossRef]
- Nair, M.G.; Wang, Y.; Galivan, J. Acquisition of Resistance to Antifolates Caused by Enhanced γ-Glutamyl Hydrolase Activity. Cancer Res. 1993, 53, 2227–2230. [Google Scholar]
- Chan, E.S.L.; Fernandez, P.; Cronstein, B.N. Methotrexate in rheumatoid arthritis. Expert Rev. Clin. Immunol. 2007, 3, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Hannoodee, M.; Mittal, M. Methotrexate. In Statpearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2022. [Google Scholar]
- Yousefi, G.; Foroutan, S.M.; Zarghi, A.; Shafaati, A. Synthesis and characterization of methotrexate polyethylene glycol esters as a drug delivery system. Chem. Pharm. Bull. 2010, 58, 147–153. [Google Scholar] [CrossRef]
- Kasim, N.A.; Whitehouse, M.; Ramachandran, C.; Bermejo, M.; Lennernäs, H.; Hussain, A.S.; Junginger, H.E.; Stavchansky, S.A.; Midha, K.K.; Shah, V.P.; et al. Molecular properties of WHO essential drugs and provisional biopharmaceutical classification. Mol. Pharm. 2004, 1, 85–96. [Google Scholar] [CrossRef]
- Crivellari, D.; Bonetti, M.C.-G. Burdens and Benefits of Adjuvant Cyclophosphamide, Methotrexate, and Fluorouracil and Tamoxifen for Elderly Patients With Breast Cancer: The International Breast Cancer Study Group Trial VII. J. Clin. Oncol. 2019, 18, 1412–1422. [Google Scholar] [CrossRef] [PubMed]
- Colleoni, M.; Rocca, A.; Sandri, M.T.; Zorzino, L.; Masci, G.; Nolè, F.; Peruzzotti, G.; Robertson, C.; Orlando, L.; Cinieri, S.; et al. Low-dose oral methotrexate and cyclophosphamide in metastatic breast cancer: Antitumor activity and correlation with vascular endothelial growth factor levels. Ann. Oncol. 2002, 13, 73–80. [Google Scholar] [CrossRef]
- Poole, C.J.; Earl, H.M.; Hiller, L.; Dunn, J.A.; Bathers, S.; Grieve, R.J.; Spooner, D.A.; Agrawal, R.K.; Fernando, I.N.; Brunt, M.; et al. Epirubicin and Cyclophosphamide, Methotrexate, and Fluorouracil as Adjuvant Therapy for Early Breast Cancer. N. Engl. J. Med. 2006, 355, 687–696. [Google Scholar] [CrossRef]
- Gulfam, M.; Matini, T.; Monteiro, P.F.; Riva, R.; Collins, H.; Spriggs, K.; Howdle, S.M.; Jérôme, C.; Alexander, C. Bioreducible cross-linked core polymer micelles enhance: In vitro activity of methotrexate in breast cancer cells. Biomater. Sci. 2017, 5, 532–550. [Google Scholar] [CrossRef]
- Zhao, L.; Huo, M.; Liu, J.; Yao, Z.; Li, D.; Zhao, Z.; Tang, J. In vitro investigation on the magnetic thermochemotherapy mediated by magnetic nanoparticles combined with methotrexate for breast cancer treatment. J. Nanosci. Nanotechnol. 2013, 13, 741–745. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhang, W.; Gu, J.; Ren, Q.; Fan, Z.; Zhong, W.; Fang, X.; Sha, X. Enhanced antitumor efficacy by methotrexate conjugated Pluronic mixed micelles against KBv multidrug resistant cancer. Int. J. Pharm. 2013, 452, 421–433. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, K.; Yaoi, T.; Koshiba, H.; Yoshida, T.; Maoka, T.; Fujiwara, Y.; Yamamoto, Y.; Mori, K. Photochemical Isomerization of Piperine, a Pungent Constituent in Pepper. Food Sci. Technol. Int. Tokyo 1996, 2, 24–29. [Google Scholar] [CrossRef]
- Elnaggar, Y.S.R.; Etman, S.M.; Abdelmonsif, D.A.; Abdallah, O.Y. Novel piperine-loaded Tween-integrated monoolein cubosomes as brain-targeted oral nanomedicine in Alzheimer’s disease: Pharmaceutical, biological, and toxicological studies. Int. J. Nanomed. 2015, 10, 5459–5473. [Google Scholar] [CrossRef]
- Wang-sheng, C.; Jie, A.; Jian-jun, L.; Lan, H.; Zeng-bao, X.; Chang-qing, L. Piperine attenuates lipopolysaccharide (LPS)-induced inflammatory responses in BV2 microglia. Int. Immunopharmacol. 2017, 42, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Taqvi, S.I.H.; Shah, A.J.; Gilani, A.H. Blood pressure lowering and vasomodulator effects of piperine. J. Cardiovasc. Pharmacol. 2008, 52, 452–458. [Google Scholar] [CrossRef]
- Lai, L.H.; Fu, Q.H.; Liu, Y.; Jiang, K.; Guo, Q.M.; Chen, Q.Y.; Yan, B.; Wang, Q.Q.; Shen, J.G. Piperine suppresses tumor growth and metastasis in vitro and in vivo in a 4T1 murine breast cancer model. Acta Pharmacol. Sin. 2012, 33, 523–530. [Google Scholar] [CrossRef]
- Bhardwaj, R.K.; Glaeser, H.; Becquemont, L.; Klotz, U.; Gupta, S.K.; Fromm, M.F. Piperine, a major constituent of black pepper, inhibits human P-glycoprotein and CYP3A4. J. Pharmacol. Exp. Ther. 2002, 302, 645–650. [Google Scholar] [CrossRef]
- Volak, L.P.; Ghirmai, S.; Cashman, J.R.; Court, M.H. Curcuminoids inhibit multiple human cytochrome P 450 (CYP). Drug Metab. Dispos. 2008, 36, 1594–1605. [Google Scholar] [CrossRef]
- Katiyar, S.S.; Muntimadugu, E.; Rafeeqi, T.A.; Domb, A.J.; Khan, W. Co-delivery of rapamycin- and piperine-loaded polymeric nanoparticles for breast cancer treatment. Drug Deliv. 2016, 23, 2608–2616. [Google Scholar] [CrossRef] [PubMed]
- Kakarala, M.; Brenner, D.E.; Korkaya, H.; Cheng, C.; Tazi, K.; Ginestier, C.; Liu, S.; Dontu, G.; Wicha, M.S. Targeting breast stem cells with the cancer preventive compounds curcumin and piperine. Breast Cancer Res. Treat. 2010, 122, 777–785. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, B.; Ferreira, C.; Passos, C.L.A.; Silva, J.L.; Fialho, E. Resveratrol, curcumin and piperine alter human glyoxalase 1 in mcf-7 breast cancer cells. Int. J. Mol. Sci. 2020, 21, 5244. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Roy, S.; Kumar, M. Pharmacokinetic study of Piperine in Wistar rats after oral and intravenous administration. Int. J. Drug Deliv. 2014, 6, 82–87. [Google Scholar]
- Moorthi, C.; Krishnan, K.; Manavalan, R.; Kathiresan, K. Preparation and characterization of curcumin-piperine dual drug loaded nanoparticles. Asian Pac. J. Trop. Biomed. 2012, 2, 841–848. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, J.; Ankola, D.D.; Beniwal, V.; Singh, D.; Kumar, M.N.V.R. Nanoparticle encapsulation improves oral bioavailability of curcumin by at least 9-fold when compared to curcumin administered with piperine as absorption enhancer. Eur. J. Pharm. Sci. 2009, 37, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Shi, Y.; Chen, Y.; Ye, J.; Sha, X.; Fang, X. Multifunctional Pluronic P123/F127 mixed polymeric micelles loaded with paclitaxel for the treatment of multidrug resistant tumors. Biomaterials 2011, 32, 2894–2906. [Google Scholar] [CrossRef] [PubMed]
- Pragatheeswaran, A.M.; Chen, S.B. Effect of chain length of PEO on the gelation and micellization of the pluronic F127 copolymer aqueous system. Langmuir 2013, 29, 9694–9701. [Google Scholar] [CrossRef]
- Bodratti, A.; Alexandridis, P. Formulation of Poloxamers for Drug Delivery. J. Funct. Biomater. 2018, 9, 11. [Google Scholar] [CrossRef]
- Valero, M.; Castiglione, F.; Mele, A.; Da Silva, M.A.; Grillo, I.; González-Gaitano, G.; Dreiss, C.A. Competitive and Synergistic Interactions between Polymer Micelles, Drugs, and Cyclodextrins: The Importance of Drug Solubilization Locus. Langmuir 2016, 32, 13174–13186. [Google Scholar] [CrossRef]
- Duncan, R.; Vicent, M.J. Polymer therapeutics-prospects for 21st century: The end of the beginning. Adv. Drug Deliv. Rev. 2013, 65, 60–70. [Google Scholar] [CrossRef]
- Alvarez-Lorenzo, C.; Sosnik, A.; Concheiro, A. PEO-PPO Block Copolymers for Passive Micellar Targeting and Overcoming Multidrug Resistance in Cancer Therapy. Curr. Drug Targets 2011, 12, 1112–1130. [Google Scholar] [CrossRef]
- Alakhova, D.Y.; Kabanov, A.V. Pluronics and MDR reversal: An update. Mol. Pharm. 2014, 11, 2566–2578. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhang, W.; Huang, Y.; Gao, F.; Sha, X.; Lou, K.; Fang, X. The therapeutic effect of methotrexate-conjugated pluronic-based polymeric micelles on the folate receptor-rich tumors treatment. Int. J. Nanomed. 2015, 10, 4043–4057. [Google Scholar] [CrossRef] [PubMed]
- Sedeky, A.S.; Khalil, I.A.; Hefnawy, A.; El-Sherbiny, I.M. Development of core-shell nanocarrier system for augmenting piperine cytotoxic activity against human brain cancer cell line. Eur. J. Pharm. Sci. 2018, 118, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Greenshields, A.L.; Doucette, C.D.; Sutton, K.M.; Madera, L.; Annan, H.; Yaffe, P.B.; Knickle, A.F.; Dong, Z.; Hoskin, D.W. Piperine inhibits the growth and motility of triple-negative breast cancer cells. Cancer Lett. 2015, 357, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Fawzi, M.; Mahmoud, M.Y.; Bakr, A.F.; Zaafar, D.; El-sherbiny, I.M. Switching indication of PEGylated lipid nanocapsules-loaded with rolapitant and deferasirox against breast cancer: Enhanced in-vitro and in-vivo cytotoxicity. Life Sci. 2022, 305, 120731. [Google Scholar] [CrossRef]
- Fuliaş, A.; Popoiu, C.; Vlase, G.; Vlase, T.; Oneţiu, D.; Sǎvoiu, G.; Simu, G.; Pǎtruţescu, C.; Ilia, G.; Ledeţi, I. Thermoanalytical and spectroscopic study on methotrexate—Active substance and tablet. Dig. J. Nanomater. Biostructures 2014, 9, 93–98. [Google Scholar]
- Armagan, A.; Uzar, E.; Uz, E.; Yilmaz, H.R.; Kutluhan, S.; Koyuncuoglu, H.R.; Soyupek, S.; Cam, H.; Serel, T.A. Caffeic acid phenethyl ester modulates methotrexate-induced oxidative stress in testes of rat. Hum. Exp. Toxicol. 2008, 27, 547–552. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.V.; Oesterreich, S.; Davidson, N.E. MCF-7 Cells—Changing the Course of Breast Cancer Research and Care for 45 Years. J. Natl. Cancer Inst. 2015, 107, djv073. [Google Scholar] [CrossRef]
- Chiappetta, D.A.; Sosnik, A. Poly(ethylene oxide)-poly(propylene oxide) block copolymer micelles as drug delivery agents: Improved hydrosolubility, stability and bioavailability of drugs. Eur. J. Pharm. Biopharm. 2007, 66, 303–317. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.C.; Leroux, J.C. Polymeric micelles—A new generation of colloidal drug carriers. Eur. J. Pharm. Biopharm. 1999, 48, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Guo, C.; Chen, S.; Junhe, M.; Wang, J.; Liang, X.; Zheng, L.; Liu, H. Effect of acid on the aggregation of poly(ethylene oxide)-poly(propylene oxide)-poly(ethylene oxide) block copolymers. J. Phys. Chem. B 2006, 110, 23068–23074. [Google Scholar] [CrossRef]
- Bezerra, D.P.; de Castro, F.; Alves, A.P.N.N.; Pessoa, C.; de Moraes, M.O.; Silveira, E.R.; Lima, M.A.S.; Elmiro, F.J.M.; De Alencar, N.M.N.; Mesquito, R.O.; et al. In vitro and in vivo antitumor effect of 5-FU combined with piplartine and piperine. J. Appl. Toxicol. 2008, 28, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Ozaslan, M.; Karagoz, I.D.; Kilic, I.H.; Guldur, M.E. Ehrlich ascites carcinoma. Afr. J. Biotechnol. 2011, 10, 2375–2378. [Google Scholar]
- Arnold, A.; Papanikolaou, A. Cyclin D1 in breast cancer pathogenesis. J. Clin. Oncol. 2005, 23, 4215–4224. [Google Scholar] [CrossRef]
- Schuuring, E. The involvement of the chromosome 11 ql 3 region in human malignancies: Cyclin D1 and EMS1 are two new candidate oncogenes—A review *. Gene 1995, 159, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Loesch, M.; Chen, G. The p38 MAPK stress pathway as a tumor suppressor or more? Front. Biosci. 2008, 13, 3581–3593. [Google Scholar] [CrossRef]
- McCord, J.M.; Fridovich, I. Superoxide dismutase an enzymtic function for erythrocuprein (hemocuprein). J. Biol. Chem. 1969, 244, 6049–6055. [Google Scholar] [CrossRef]
- Gönenç, A.; Özkan, Y.; Torun, M.; Şmşek, B. Plasma malondialdehyde (MDA) levels in breast and lung cancer patients. J. Clin. Pharm. Ther. 2001, 26, 141–144. [Google Scholar] [CrossRef]
- Zhou, H.; Li, X.M.; Meinkoth, J.; Pittman, R.N. Akt regulates cell survival and apoptosis at a postmitochondrial level. J. Cell Biol. 2000, 151, 483–494. [Google Scholar] [CrossRef]













| Formulation | PS (nm) | PDI | ZP (mV) |
|---|---|---|---|
| MNMs | 26.3 ± 0.1 | 0.43 | −4.42 |
| MTX-MNMs | 104.6 ± 1.7 | 0.29 | −3.47 |
| NMs | 96.3 ± 1.1 | 0.19 | −19.4 |
| PIP-NMs | 114.2 ± 0.3 | 0.26 | −8.02 |
| Drug μg/mL | IC50 Value | With 0.5 IC50 of Free PIP | With 0.5 IC50 of PIP-NMs |
|---|---|---|---|
| Free PIP (24 h) | 183 ± 5.63 | - | - |
| PIP-NMs (24 h) | 11.84 ± 0.46 | - | - |
| Free MTX (24 h) | 213 ± 9.02 | 45.23 ± 2.91 | - |
| Free MTX (48 h) | 115.32 ± 7.08 | 25.84 ± 1.28 | - |
| MTX-MNMs (24 h) | 3.47 ± 0.13 | 0.627 ± 0.03 | |
| MTX-MNMs (48 h) | 2.099 ± 0.08 | 0.128 ± 0.02 |
| Group | Cyclin D1 (ng/mL) | p-38 MAPK (ng/mL) |
|---|---|---|
| Control | 8.4 ± 0.21 | 16.6 ± 1.17 |
| MTX-MNMs | 2.2 ± 0.16 | 4.7 ± 0.08 |
| PIP-NMs/MTX-MNMs | 2.4 ± 0.12 | 3.1 ± 0.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mansour, A.; Mahmoud, M.Y.; Bakr, A.F.; Ghoniem, M.G.; Adam, F.A.; El-Sherbiny, I.M. Dual-Enhanced Pluronic Nanoformulated Methotrexate-Based Treatment Approach for Breast Cancer: Development and Evaluation of In Vitro and In Vivo Efficiency. Pharmaceutics 2022, 14, 2668. https://doi.org/10.3390/pharmaceutics14122668
Mansour A, Mahmoud MY, Bakr AF, Ghoniem MG, Adam FA, El-Sherbiny IM. Dual-Enhanced Pluronic Nanoformulated Methotrexate-Based Treatment Approach for Breast Cancer: Development and Evaluation of In Vitro and In Vivo Efficiency. Pharmaceutics. 2022; 14(12):2668. https://doi.org/10.3390/pharmaceutics14122668
Chicago/Turabian StyleMansour, Amira, Mohamed Y. Mahmoud, Alaa F. Bakr, Monira G. Ghoniem, Fatima A. Adam, and Ibrahim M. El-Sherbiny. 2022. "Dual-Enhanced Pluronic Nanoformulated Methotrexate-Based Treatment Approach for Breast Cancer: Development and Evaluation of In Vitro and In Vivo Efficiency" Pharmaceutics 14, no. 12: 2668. https://doi.org/10.3390/pharmaceutics14122668
APA StyleMansour, A., Mahmoud, M. Y., Bakr, A. F., Ghoniem, M. G., Adam, F. A., & El-Sherbiny, I. M. (2022). Dual-Enhanced Pluronic Nanoformulated Methotrexate-Based Treatment Approach for Breast Cancer: Development and Evaluation of In Vitro and In Vivo Efficiency. Pharmaceutics, 14(12), 2668. https://doi.org/10.3390/pharmaceutics14122668






