To Enhance Mucus Penetration and Lung Absorption of Drug by Inhalable Nanocrystals-In-Microparticles
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Preparation of CN-NS and CN-INMPs
2.2.2. Particles Size and Zeta Potential Assay of CN-NS
2.2.3. Transmission Electron Microscopy (TEM)
2.2.4. In Vitro Interaction between CN-NS and Mucin
2.2.5. Mucus Diffusion Analysis
2.2.6. D Visualization Evaluation of Particles Penetration Ability
2.2.7. The Reconstitution Ability of CN-INMPs
2.2.8. In Vitro Drug Release of CN-INMPs
2.2.9. Scanning Electron Microscopy (SEM)
2.2.10. Differential Scanning Calorimetry (DSC)
2.2.11. Powder X-ray Diffraction (PXRD)
2.2.12. In Vitro Aerodynamic Performance of CN-INMPs
2.2.13. Cell Viability and Cell Uptake
2.2.14. Pharmacokinetic Study in Rats of CN-INMPs
Drug Retention in Lung
Statistical Analysis
3. Results and Discussion
3.1. The Particle Size and Morphology of CN-NS
3.2. The Mucointeraction between Mucin and CN-NS
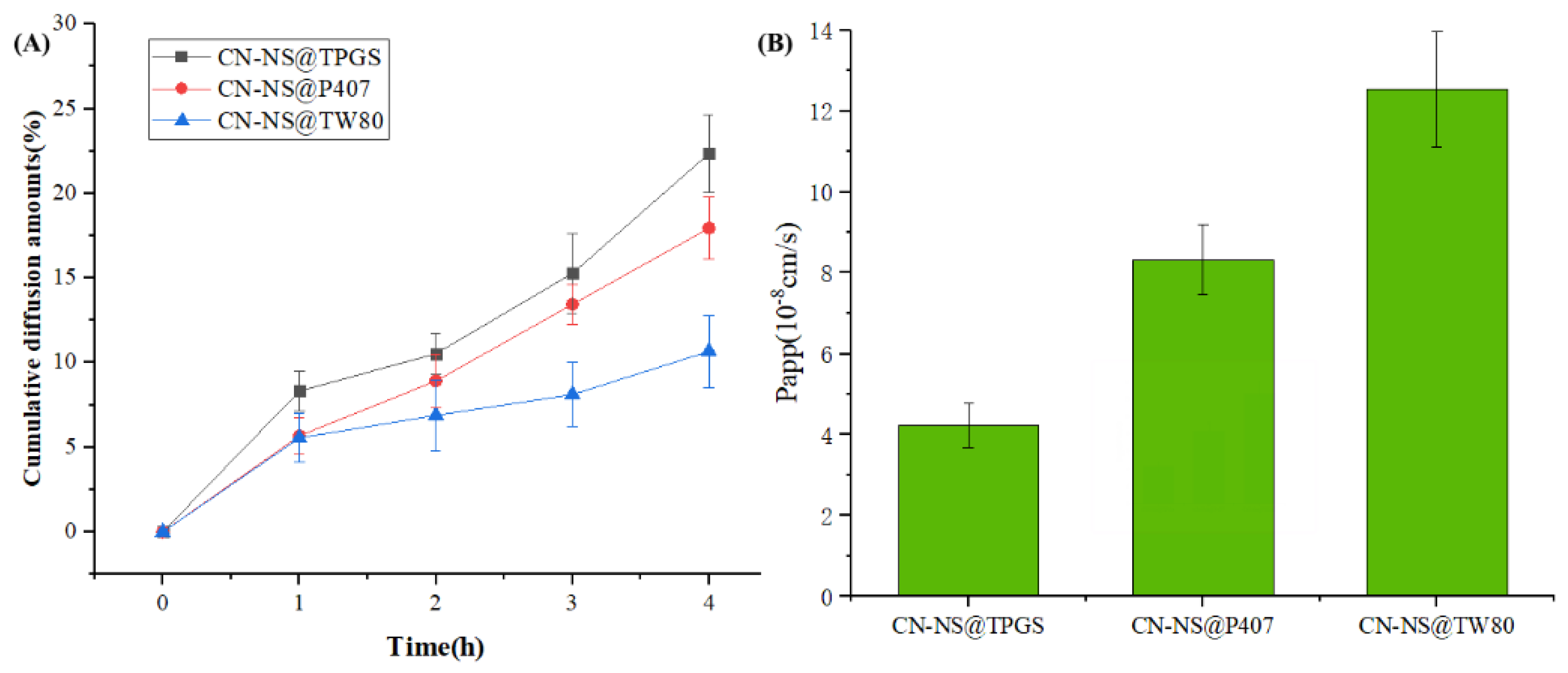
3.3. The Mucus Penetration Ability of CN-NC in Mucus
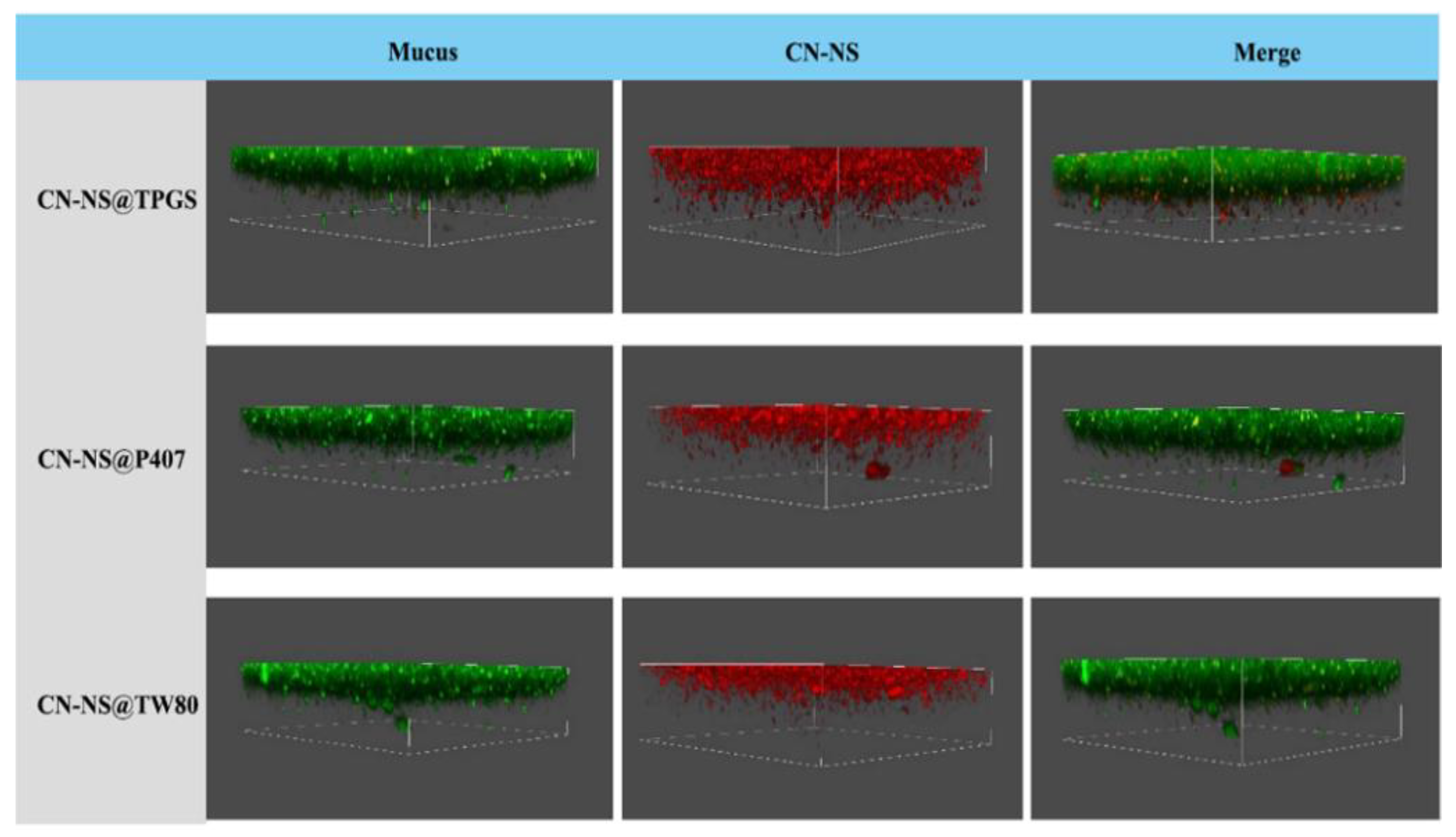
3.4. The Mucus Penetration Evaluation of CN-NS in Mucus by CLSM
3.5. The Aerodynamic Performance and Redispersibility Evaluation of CN-INMP
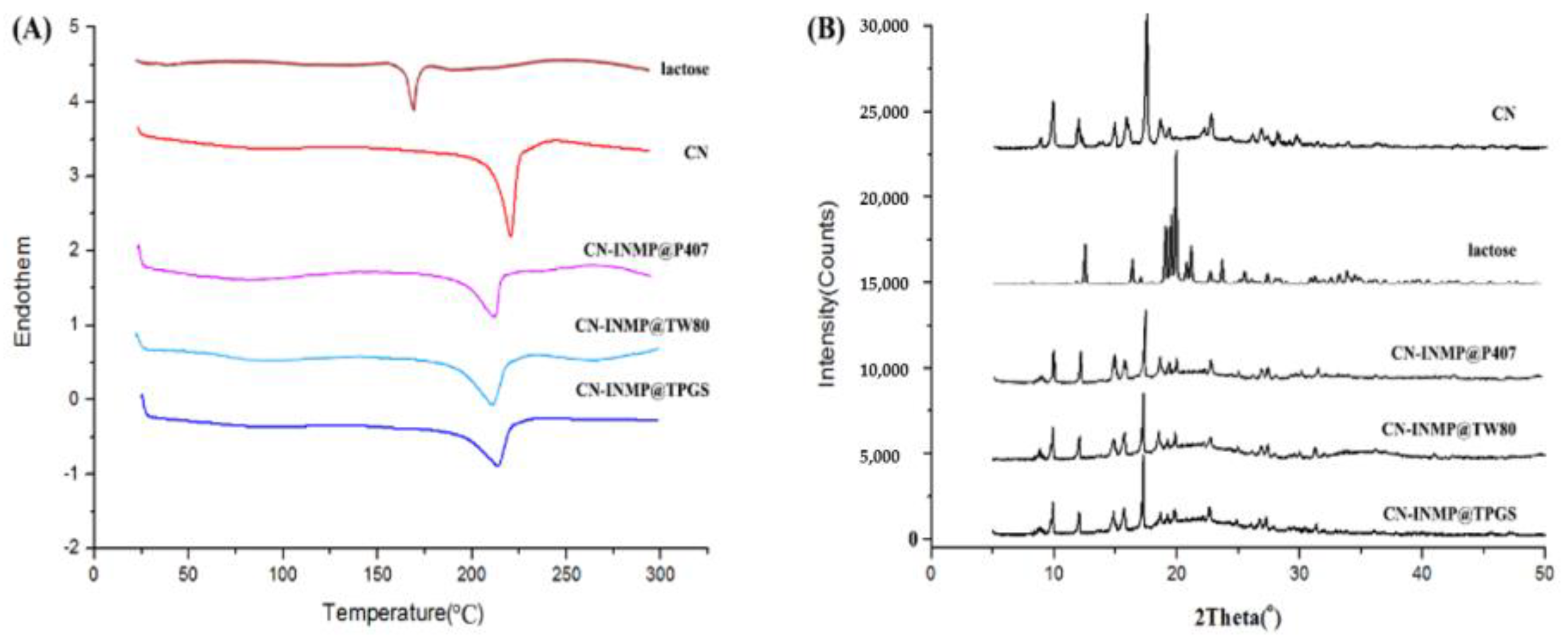
3.6. Crystallinity of Spray-Dried CN-INMPs
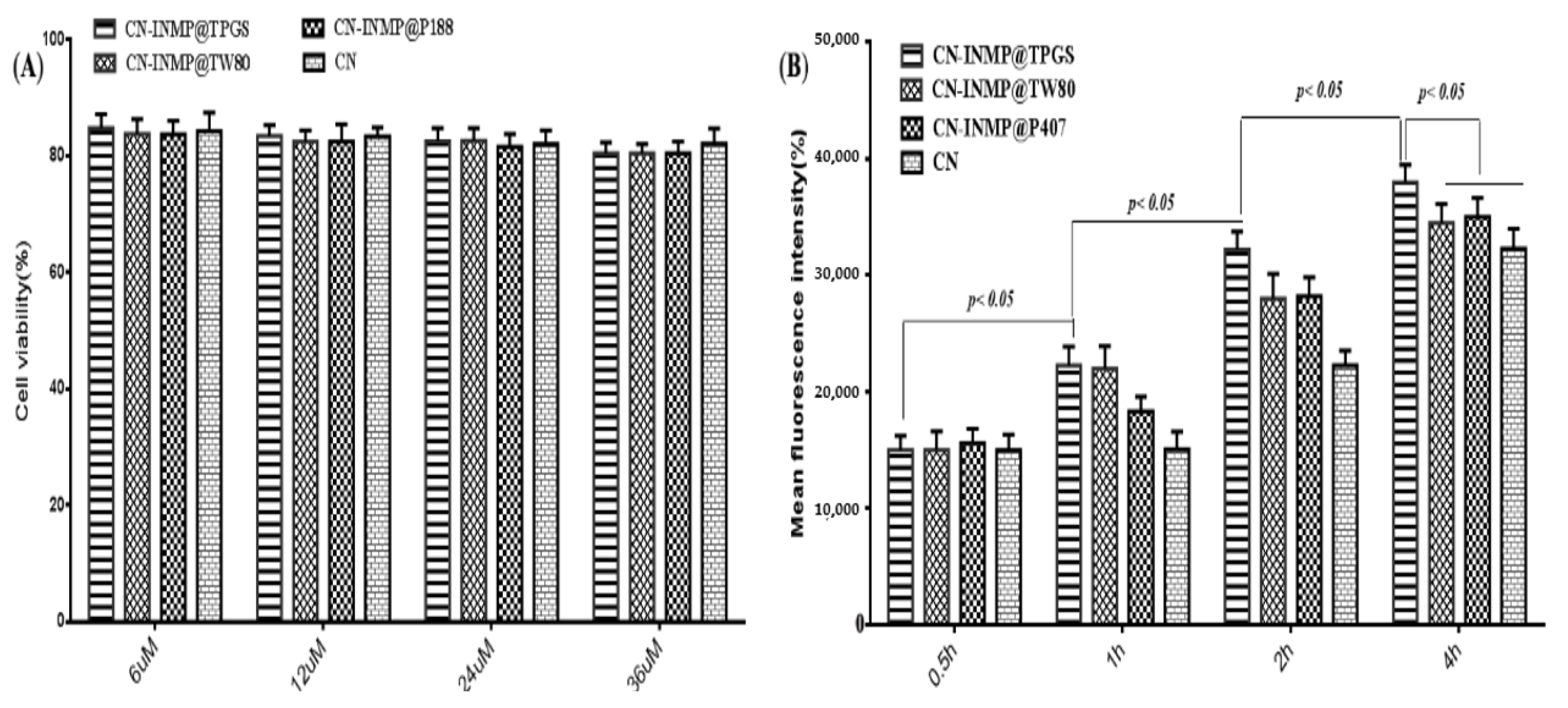
3.7. Cell Viability and Cell Toxicity
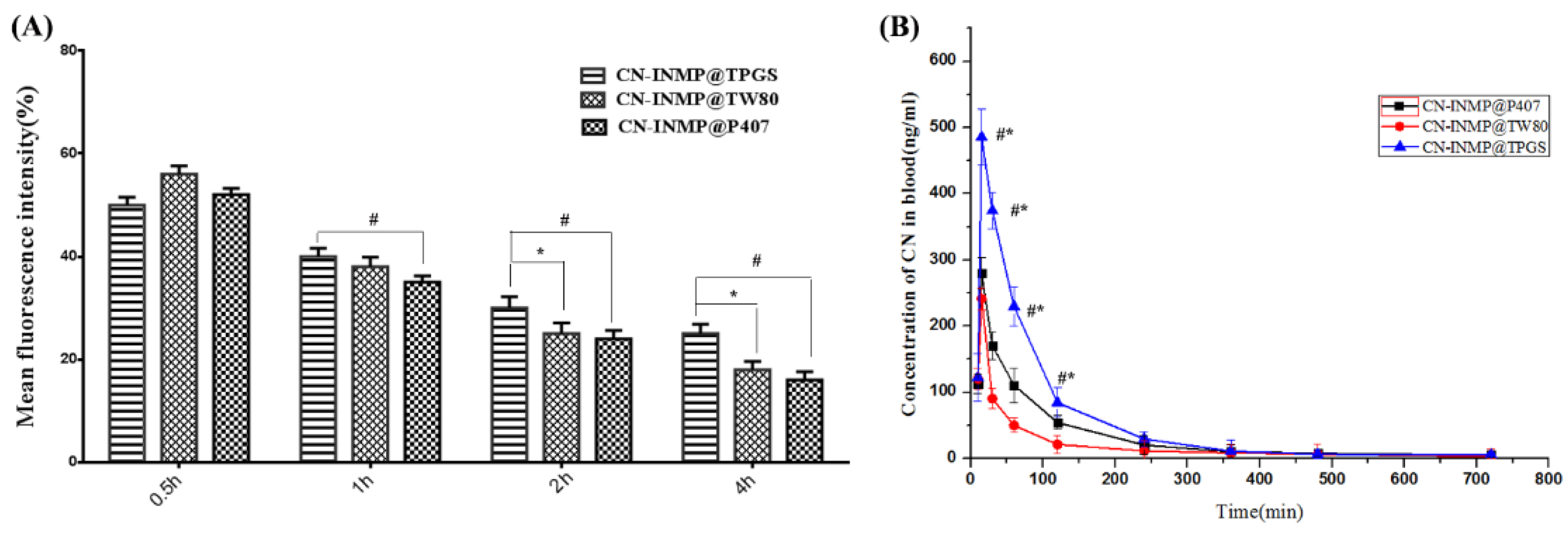
3.8. In Vivo Pharmacokinetic Study of CN-INMPs
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mansour, L.Z.; Rhee, Y.S.; Wu, X. Nanomedicine in pulmonary delivery. Int. J. Nanomed. 2009, 4, 299–319. [Google Scholar] [CrossRef] [PubMed]
- Labiris, N.R.; Dolovich, M.B. Pulmonary drug delivery. Part I: Physiological factors affecting therapeutic effectiveness of aerosolized medications. Br. J. Clin. Pharmacol. 2003, 56, 588–599. [Google Scholar] [CrossRef] [PubMed]
- Byron, P.R.; Patton, J.S. Inhaling medicines: Delivering drugs to the body through the lungs. Nat. Rev. Drug Discov. 2007, 6, 67–74. [Google Scholar]
- Elsayed, M.M.A.; Shalash, A.O. Modeling the performance of carrier-based dry powder inhalation formulations: Where are we, and how to get there? J. Control. Release 2018, 279, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.Y.; Chan, J.G.Y.; Chan, H.K. Pulmonary drug delivery by powder aerosols. J. Control. Release 2014, 193, 228–240. [Google Scholar] [CrossRef]
- Onoue, S.; Aoki, Y.; Kawabata, Y.; Matsui, T.; Yamamoto, K.; Sato, H.; Yamauchi, Y.; Yamada, S. Development of inhalable nanocrystalline solid dispersion of tranilast for airway inflammatory diseases. J. Pharm. Sci. 2011, 100, 622–633. [Google Scholar] [CrossRef]
- Ling, X.; Shen, Y.; Sun, C.M.; Tu, J.S. Current progress on pulmonary drug delivery. J. Pharm. Res. 2014, 33, 711–714. [Google Scholar]
- Loira-Pastoriza, C.; Todoroff, J.; Vanbever, R. Delivery strategies for sustained drug release in the lungs. Adv. Drug Deliv. Rev. 2014, 75, 81–91. [Google Scholar] [CrossRef]
- Kurakula, M.; A. Ahmed, T. Co-delivery of atorvastatin nanocrystals in PLGA based in situ gel for anti-hyperlipidemic efficacy. Curr. Drug Deliv. 2016, 13, 211–220. [Google Scholar] [CrossRef]
- Kurakula, M.; Sobahi, T.R.; El-Helw, A.M.; Abdelaal, M.Y. Development and validation of a RP-HPLC method for assay of atorvastatin and its application in dissolution studies on thermosensitive hydrogel-based nanocrystals. Trop. J. Pharm. Res. 2014, 13, 1681–1687. [Google Scholar] [CrossRef]
- Ni, R.; Zhao, J.; Liu, Q.; Liang, Z.; Muenster, U.; Mao, S. Nanocrystals embedded in chitosan-based respirable swellable microparticles as dry powder for sustained pulmonary drug delivery. Eur. J. Pharm. Sci. 2017, 99, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Han, M.; Tian, F.; Cun, D.; Rantanen, J.; Yang, M. Budesonide nanocrystal-loaded hyaluronic acid microparticles for inhalation: In vitro and in vivo evaluation. Carbohydr. Polym. 2018, 181, 1143–1152. [Google Scholar] [CrossRef] [PubMed]
- Ruge, C.A.; Bohr, A.; Beck-Broichsitter, M.; Nicolas, V.; Tsapis, N.; Fattal, E. Disintegration of nano-embedded microparticles after deposition on mucus: A mechanistic study. Colloids Surf. B Biointerfaces 2016, 139, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Baghdan, E.; Duse, L.; Schüer, J.J.; Pinnapireddy, S.R.; Pourasghar, M.; Schäfer, J.; Schneider, M.; Bakowsky, U. Development of inhalable curcumin loaded Nano-in-Microparticles for bronchoscopic photodynamic therapy. Eur. J. Pharm. Sci. 2019, 132, 63–71. [Google Scholar] [CrossRef]
- Bansil, R.; Turner, B.S. Mucin structure, aggregation, physiological functions and biomedical applications. Curr. Opin. Colloid Int. Sci. 2006, 11, 164–170. [Google Scholar] [CrossRef]
- María, G.D.; Ditlev, B.; Feng, W.; Nielsen, H.M. The role of mucus as an invisible cloak to transepithelial drug delivery by nanoparticles. Adv. Drug Deliv. Rev. 2018, 124, 107–124. [Google Scholar]
- He, Y.; Liang, Y.; Mak, J.C.W.; Liao, Y.; Li, T.; Yan, R.; Li, H.F.; Zheng, Y. Size effect of curcumin nanocrystals on dissolution, airway mucosa penetration, lung tissue distribution and absorption by pulmonary delivery. Colloids Surf. B Biointerfaces 2020, 186, 110703. [Google Scholar] [CrossRef]
- Guo, Y.; Luo, J.; Tan, S.; Otieno, B.O.; Zhang, Z. The applications of vitamin E TPGS in drug delivery. Eur. J. Pharm. Sci. 2013, 49, 175–186. [Google Scholar] [CrossRef]
- Ahmad, M.Z.; Alkahtani, S.A.; Akhter, S.; Ahmad, F.J.; Ahmad, J.; Akhtar, M.S.; Mohsin, N.; Abdel-Wahab, B.A. Progress in nanotechnology-based drug carrier in designing of curcumin nanomedicines for cancer therapy: Current state-of-the-art. J. Drug Target. 2016, 24, 273–293. [Google Scholar] [CrossRef]
- Anand, P.; Kunnumakkara, A.B.; Newman, R.A.; Aggarwal, B.B. Bioavailability of curcumin: Problems and promises. Mol. Pharm. 2007, 4, 807–818. [Google Scholar] [CrossRef]
- Di Martino, R.M.C.; Bisi, A.; Rampa, A.; Gobbi, S.; Belluti, F. Recent progress on curcumin-based therapeutics: A patent review (2012–2016). Part II: Curcumin derivatives in cancer and neurodegeneration. Exp. Opin. Ther. Pat. 2017, 27, 953–965. [Google Scholar] [CrossRef] [PubMed]
- Giordano, A.; Tommonaro, G. Curcumin and cancer. Nutrients 2019, 11, 2376. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; Xie, J.; Shuai, S.; Wei, S.; Chen, Y.; Guan, Z.; Zheng, Q.; Yue, P.; Wang, C. Nose-to-brain delivery of drug nanocrystals by using Ca2+ responsive deacetylated gellan gum based in situ-nanogel. Int. J. Pharm. 2021, 594, 120182. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; He, Y.; Zhang, H.; Zhang, Y.; Gao, T.; Wang, J.H.; Wang, S. Zwitterion-functionalized mesoporous silica nanoparticles for enhancing oral delivery of protein drugs by overcoming multiple gastrointestinal barriers. J. Colloid Interface Sci. 2021, 582, 364–375. [Google Scholar] [CrossRef] [PubMed]
- Poinard, B.; Kamaluddin, S.; Tan, A.Q.Q.; Neoh, K.G.; Kah, J.C.Y. Polydopamine coating enhances mucopenetration and cell uptake of nanoparticles. ACS Appl. Mater. Interfaces 2019, 11, 4777–4789. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Gui, Y.; Luo, Y.; Liu, Y.; Tu, L.; Ma, Y.; Yue, P.; Yang, M. Design and evaluation of inhalable nanocrystals embedded microparticles with enhanced redispersibility and bioavailability for breviscapine. Powder Technol. 2021, 377, 128–138. [Google Scholar] [CrossRef]
- Ni, R.; Muenster, U.; Zhao, J.; Zhang, L.; Becker-Pelster, E.M.; Rosenbruch, M.; Mao, S. Exploring polyvinylpyrrolidone in the engineering of large porous PLGA microparticles via single emulsion method with tunable sustained release in the lung: In vitro and in vivo characterization. J. Control. Release 2017, 249, 11–22. [Google Scholar] [CrossRef]
- Kurakula, M.; El-Helw, A.M.; Sobahi, T.R.; Abdelaal, M.Y. Chitosan based atorvastatin nanocrystals: Effect of cationic charge on particle size, formulation stability, and in-vivo efficacy. Int. J. Nanomed. 2015, 10, 321–334. [Google Scholar] [CrossRef]
- Bandi, S.P.; Kumbhar, Y.S.; Venuganti, V. Effect of particle size and surface charge of nanoparticles in penetration through intestinal mucus barrier. J. Nanoparticle Res. 2020, 22, 62. [Google Scholar] [CrossRef]
- Lai, S.K.; Wang, Y.Y.; Hanes, J. Mucus-penetrating nanoparticles for drug and gene delivery to mucosal tissues. Adv. Drug Deliv. Rev. 2009, 61, 158–171. [Google Scholar] [CrossRef]
- Maisel, K.; Ensign, L.; Reddy, M.; Cone, R.; Hanes, J. Effect of surface chemistry on nanoparticle interaction with gastrointestinal mucus and distribution in the gastrointestinal tract following oral and rectal administration in the mouse. J. Control. Release 2015, 197, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Ensign, L.M.; Cone, R.; Hanes, J. Oral drug delivery with polymeric nanoparticles: The gastrointestinal mucus barriers. Adv. Drug Deliv. Rev. 2012, 64, 557–570. [Google Scholar] [CrossRef] [PubMed]
- Murgia, X.; Pawelzyk, P.; Schaefer, U.F.; Wagner, C.; Willenbacher, N.; Lehr, C.M. Size-limited penetration of nanoparticles into porcine respiratory mucus after aerosol deposition. Biomacromolecules 2016, 17, 1536–1542. [Google Scholar] [CrossRef]
- Date, A.A.; Halpert, G.; Babu, T.; Ortiz, J.; Kanvinde, P.; Dimitrion, P.; Narayan, J.; Zierden, H.; Betageri, K.; Musmanno, O.; et al. Mucus-penetrating budesonide nanosuspension enema for local treatment of inflammatory bowel disease. Biomaterials 2018, 185, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Huckaby, J.T.; Lai, S.K. PEGylation for enhancing nanoparticle diffusion in mucus. Adv. Drug Deliv. Rev. 2018, 124, 125–139. [Google Scholar] [CrossRef] [PubMed]
- Kho, K.; Hadinoto, K. Dry powder inhaler delivery of amorphous drug nanoparticles: Effects of the lactose carrier particle shape and size. Powder Technol. 2013, 233, 303–311. [Google Scholar] [CrossRef]
- Pazesh, S.; Lazorova, L.; Berggren, J.; Alderborn, G.; Gråsjö, J. Considerations on the quantitative analysis of apparent amorphicity of milled lactose by Raman spectroscopy. Int. J. Pharm. 2016, 511, 488–504. [Google Scholar] [CrossRef]
- Luo, Y.; Zhang, Z.; Huang, G.; Yu, H.; Ma, Y.; Zheng, Q.; Yue, P. Roles of maltodextrin and inulin as matrix formers on particle performance of inhalable drug nanocrystal-embedded microparticles. Carbohydr. Polym. 2020, 235, 115937. [Google Scholar] [CrossRef]
- Xu, Q.; Ensign, G.; Boylan, L.M.; Schon, N.J.A.; Gong, X.Q.; Yang, J.C.; Lamb, N.W.; Cai, S.T.; Yu, T.; Freire, E.; et al. Impact of surface polyethylene glycol (PEG) density on biodegradable nanoparticle transport in mucus ex vivo and distribution in vivo. ACS Nano 2015, 9, 9217–9227. [Google Scholar] [CrossRef]




| Stabilizer | Formers/Drug Ratio (%) | Carr Index (CI) | ρ | ADe (μm) | FPF% |
|---|---|---|---|---|---|
| TPGS | 100% | 29.13 | 0.352 | 4.537 ± 0.050 | 31.32 ± 0.020 |
| 200% | 27.41 | 0.392 | 3.924 ± 0.010 | 46.737 ± 0.020 | |
| P407 | 100% | 27.52 | 0.412 | 4.210 ± 0.123 | 42.31 ± 0.020 |
| 200% | 24.35 | 0.431 | 3.722 ± 0.020 | 51.25 ± 0.010 | |
| TW80 | 100% | 34.67 | 0.302 | 4.582 ± 0.132 | 25.32 ± 0.110 |
| 200% | 31.12 | 0.341 | 4.221 ± 0.451 | 31.302 ± 0.300 |
| Formulation | Cmax (µg/L) | Tmax (h) | MRT(0-t) (h) | AUC(0-∞) (µg/L h) |
| CN-INMP@TPGS | 485.23 ± 18.11 a,b | 3.37 ± 1.37 a,b | 4.24 ± 1.14 a,b | 2413.18 ± 432.41 a,b |
| CN-INMP@P407 | 289.26 ± 15.38 c | 2.12 ± 1.09 | 2.67 ± 0.42 c | 1612.35 ± 261.35 c |
| CN-INMP@TW80 | 242.42 ± 13.59 | 2.16 ± 1.08 | 1.75 ± 0.35 | 777.59 ± 196.81 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, G.; Shuai, S.; Zhou, W.; Chen, Y.; Shen, B.; Yue, P. To Enhance Mucus Penetration and Lung Absorption of Drug by Inhalable Nanocrystals-In-Microparticles. Pharmaceutics 2022, 14, 538. https://doi.org/10.3390/pharmaceutics14030538
Huang G, Shuai S, Zhou W, Chen Y, Shen B, Yue P. To Enhance Mucus Penetration and Lung Absorption of Drug by Inhalable Nanocrystals-In-Microparticles. Pharmaceutics. 2022; 14(3):538. https://doi.org/10.3390/pharmaceutics14030538
Chicago/Turabian StyleHuang, Guiting, Shuyuan Shuai, Weicheng Zhou, Yingchong Chen, Baode Shen, and Pengfei Yue. 2022. "To Enhance Mucus Penetration and Lung Absorption of Drug by Inhalable Nanocrystals-In-Microparticles" Pharmaceutics 14, no. 3: 538. https://doi.org/10.3390/pharmaceutics14030538
APA StyleHuang, G., Shuai, S., Zhou, W., Chen, Y., Shen, B., & Yue, P. (2022). To Enhance Mucus Penetration and Lung Absorption of Drug by Inhalable Nanocrystals-In-Microparticles. Pharmaceutics, 14(3), 538. https://doi.org/10.3390/pharmaceutics14030538






