Abstract
Microneedles are a well-known transdermal or transdermal drug delivery system. Different from intramuscular injection, intravenous injection, etc., the microneedle delivery system provides unique characteristics for immunotherapy administration. Microneedles can deliver immunotherapeutic agents to the epidermis and dermis, where immune cells are abundant, unlike conventional vaccine systems. Furthermore, microneedle devices can be designed to respond to certain endogenous or exogenous stimuli including pH, reactive oxygen species (ROS), enzyme, light, temperature, or mechanical force, thereby allowing controlled release of active compounds in the epidermis and dermis. In this way, multifunctional or stimuli-responsive microneedles for immunotherapy could enhance the efficacy of immune responses to prevent or mitigate disease progression and lessen systemic adverse effects on healthy tissues and organs. Since microneedles are a promising drug delivery system for accurate delivery and controlled drug release, this review focuses on the progress of using reactive microneedles for immunotherapy, especially for tumors. Limitations of current microneedle system are summarized, and the controllable administration and targeting of reactive microneedle systems are examined.
1. Introduction
As a drug delivery tool that has developed rapidly in recent years, microneedles have been widely used in the delivery of various nucleic acids [1,2], small molecules [3,4,5,6], proteins [7,8,9], nanoparticles [10,11,12], and other payloads, proving that microneedles as a new type of drug delivery system have strong flexibility. In particular, a variety of immunotherapeutic agents delivered by microneedles have achieved a strong increase in the immune level in animal experiments, such as fully inactivated influenza virus [13], hepatitis B virus plasmid DNA [14], and Bacillus anthracis protein antigens [15]. Vaccines have long been considered one of the most cost-effective medical interventions to preventing and controlling disease [16]. With the COVID-19 pandemic, due to the rich technical potential of microneedles for vaccine delivery, how to achieve efficient and accurate immunotherapeutic agent delivery has come under intense scrutiny.
As one of the most important immune organs, the skin is an attractive target for immunomodulation [17]. Transcutaneous immunization (TCI) has been reported to induce a stronger immune response than has intramuscular injection, which has a dose disadvantage [18,19,20]. Therefore, the application of microneedles in TCI has received extensive attention.
In terms of immunotherapeutic agent delivery, compared with traditional intramuscular and subcutaneous injections, microneedles can deliver loaded immunotherapeutic agents to the epidermis and dermis, which include many antigen-presenting cells, including dermal dendritic cells and epidermal Langerhans cells. These cells have the ability to capture antigens and stimulate lymphocytes to induce an immune response [21]. Based on the above-mentioned advantages of transdermal drug delivery, research on microneedles is also very popular in the field of influenza prevention and treatment. Currently, there are many microneedle-based immunotherapies in preclinical or clinical development, such as influenza vaccines [22], a measles-rubella vaccine [23], a rabies vaccine [24], and a spinal cord gray matter vaccine [25]. Compared with traditional subcutaneous injections, microneedle-based immunotherapy has the following advantages: (1) minimal invasiveness and painless administration [26]; (2) capacity to carry immunotherapeutic agents in dry form, improving thermal stability and reducing storage or transportation costs; and (3) a high potential for self-administration without the need for any special equipment or applicators [27]. The skin is full of immune cells targeted by the immunotherapy, which produces stronger immune effects than does subcutaneous injection and reduces the immunotherapeutic agent dose. Clinical studies have shown that microneedle-based immunotherapy can induce immune effects comparable or even better than those of traditional subcutaneous injections [28,29,30]. Early microneedle-based immunotherapy has mainly consisted of hollow microneedles. For example, the injection microneedle used in Fluzone Intradermal (IDflu, Intanza) [31], a flu vaccine launched in 2011 with Sanofi, is BD’s Soluvia hollow microneedle delivery system [32]. However, such vaccines are still in liquid form, which is not conducive to storage or transportation. In order to solve this problem, a growing number of researchers have begun to focus on the development of dissolvable microneedle-based immunotherapy. There are the related studies on soluble microneedles in the development of various vaccines such as novel coronavirus, Ebola virus [33], AIDS virus, influenza, polio, and rabies [34]. Targeted delivery of immunotherapeutic agents to immune cells enables dose reduction and enhanced immune response [35,36,37]. Additionally, microneedle transdermal drug delivery has the advantages of high compliance, moderate invasiveness, and convenient use [38,39,40]. The development of a responsive microneedle system can further control the spatiotemporal release of payloads more effectively.
Stimulus conditions for responsive microneedles can be classified into internal and external stimuli according to where the stimulus occurs. In this review, we classify responsive microneedles for immunotherapy into the above two categories, and introduce the materials, structures, and functions of stimuli-responsive microneedles, as well as their applications in medicine and biology. All stimulus-triggering methods and diseases are summarized in the tables.
2. Microneedles Triggered by Internal Stimuli
2.1. pH-Responsive Microneedles
pH-responsive microneedles are mostly made of polymers [41,42]. Changes in the pH of the environment can cause the polymer to degrade, swell, rupture, or collapse to release the loaded immunotherapeutic agents. These materials typically consist of hydrophilic and ionically functional polymer chains. Low pH has been intensively studied as a significant factor in the development of several pH-responsive microneedle-based drug delivery systems at the sites of chronic wounds, inflammatory processes, and cancer [43,44,45,46]. For example, the pH of most tumor microenvironments is lower than that of normal tissues, so this responsive approach has important practical value in cancer immunotherapy [47,48,49,50,51,52].
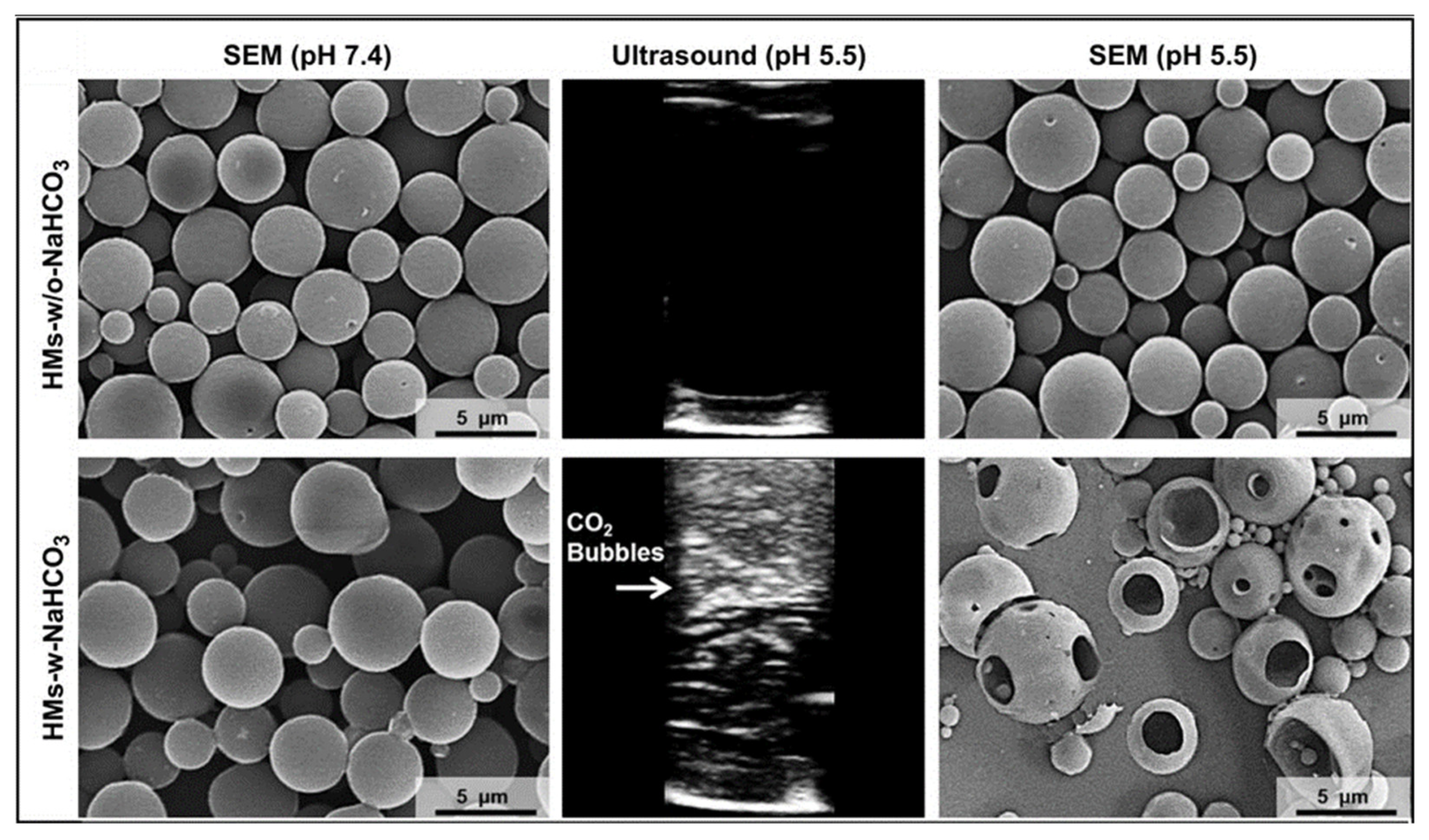
In a previous study, a pH-responsive drug delivery system was developed by encapsulating hollow microspheres of lactic acid–glycolic acid copolymers in polyvinylpyrrolidone (PVP) microneedles [53,54]. Two drugs were used for simultaneously delivery. The PVP microneedles loaded with the first drug and hollow microspheres dissolved immediately after being inserted into the skin for a few minutes, releasing the first drug and hollow microspheres in the environment. In the acidic pH skin environment, protons (H+) could freely and quickly pass through the PLGA shell membrane, react with NaHCO3 in the microspheres, and generate a large number of CO2 bubbles (Figure 1). These bubbles created holes and ruptured the PLGA spherical shell membrane, thereby releasing the second encapsulated drug in the microspheres. This approach could become a powerful technique for the continuous direct transdermal delivery of multiple drugs into the epidermis for clinical applications.
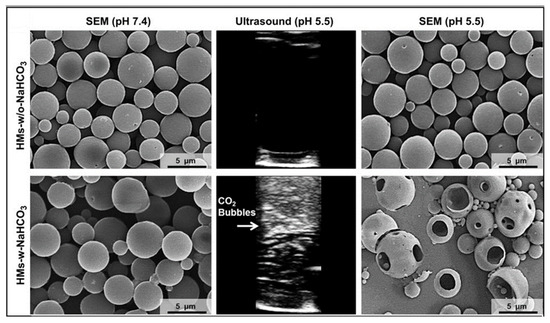
Figure 1.
Both unloaded and loaded NaHCO3 microspheres were intact at pH 7.4. In the acidic environment of pH 5.5, the microspheres containing NaHCO3 were swollen by CO2 gas and a large number of holes were ruptured. Reprinted with permission from [54]. Copyright 2012, Elsevier.
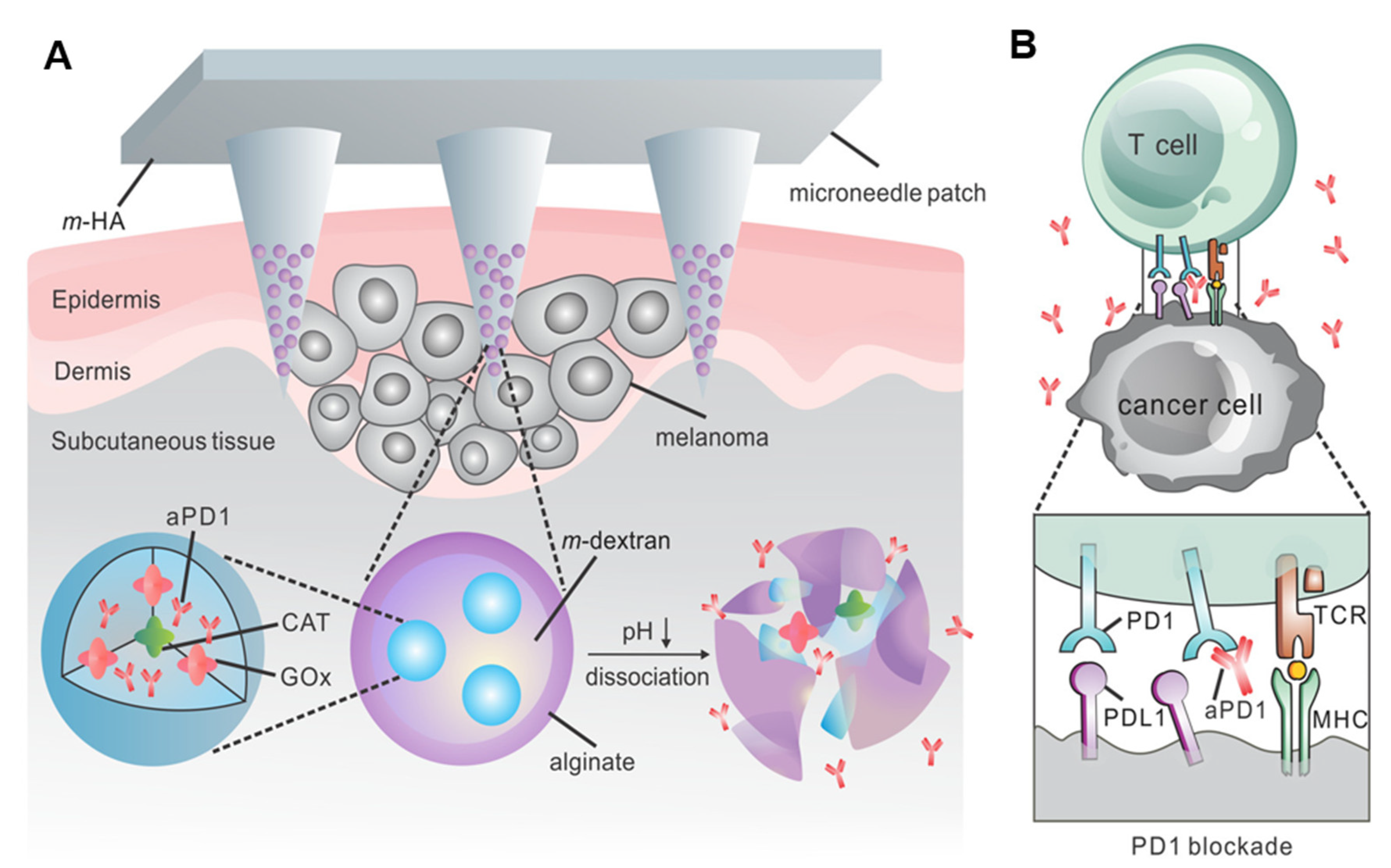
In another study, a self-degradable biocompatible hyaluronic acid microneedle was loaded with pH-sensitive glucose nanoparticles that encapsulate antiprogrammed death 1 (aPD1) antibody and glucose oxidase (GOx), which converts blood glucose to gluconic acid (Figure 2A) [55,56]. The generation of an acidic environment facilitated the self-dissociation of nanoparticles, which subsequently resulted in a massive release of aPD1. Skin is a perfect tissue for triggering an associated immune response [57,58,59]. aPD1 acts as an immune checkpoint inhibitor to prevent T-cell apoptosis by blocking the PD-1 receptor on the surface of T cells [60]. This enables T cells to effectively fight tumor cells. In this work, pH-responsive dextran nanoparticles were prepared by a double-emulsion (oil-in-water) solvent evaporation/extraction method. Compared with systems without triggered release or intratumoral injection, pH-responsive microneedles had a more pronounced therapeutic effect in eradicating a mouse model of melanoma [61,62,63,64,65]. Overall, the microneedle delivery system has great potential and biomedical promise in the treatment of skin cancer.
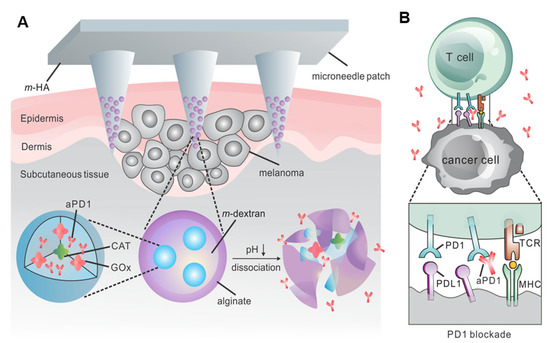
Figure 2.
Schematic diagram of the microneedle-responsive patch delivery of aPD1 for skin cancer treatment. (A) Two enzymes are encapsulated in the nanoparticles. Under the action of enzymes in the physiological environment, blood glucose is converted into gluconic acid to promote the continuous dissociation of NPs, thereby releasing aPD1. (B) aPD1 blocks PD-1, and the activated immune system kills skin cancer cells. Reprinted with permission from [56]. Copyright 2016 American Chemical Society.
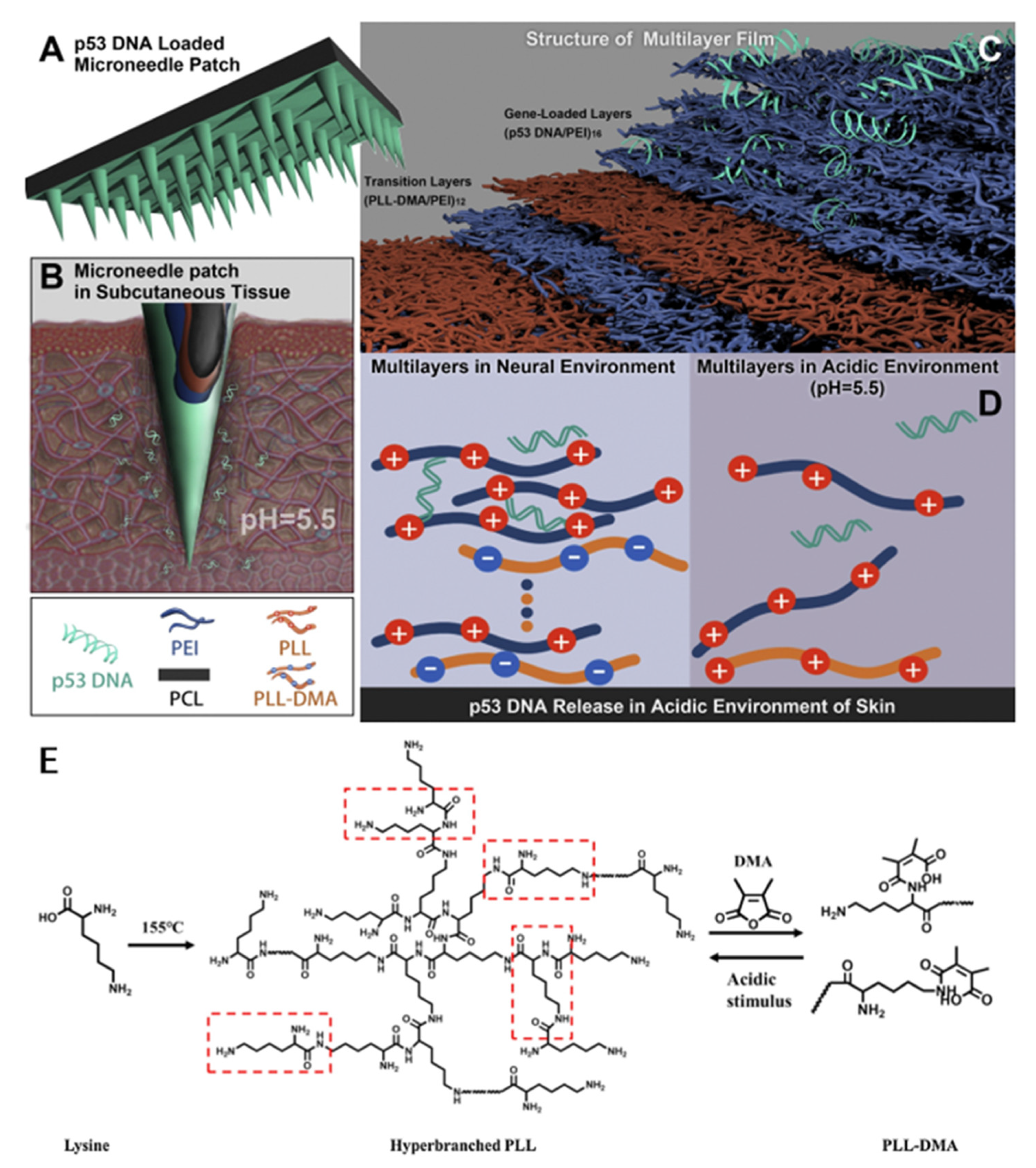
Unlike the above two works that used microneedles to encapsulate pH-responsive nanoparticles, the following work developed a microneedle responsive to cancer acidic skin [48,66]. A pH-responsive polyelectrolyte multilayer film (PEM) was coated on the surface of polycaprolactone (PCL) microneedles using a stepwise multilayer assembly for gene release in skin cancer. The PEM consists of a transition layer, a charge-reversible polymer, a dimethylmaleic anhydride-modified polylysine (PLL-DMA), and a gene-loading layer (p53 expression plasmid/polyethyleneimine; Figure 3). When the microneedle coating contacts the intradermal microenvironment, the negatively charged PLL-DMA becomes a positively charged PLL due to the low pH environment. Rapid dissolution of the transition layer accelerates the release of the p53 DNA in outermost layer. The results of in vivo experiments showed that the pH-responsive microneedles could effectively inhibit tumor growth in mice, and the tumor mass of nonresponsive microneedles or mice injected intravenously was 5 to 10 times that of pH-responsive microneedles.
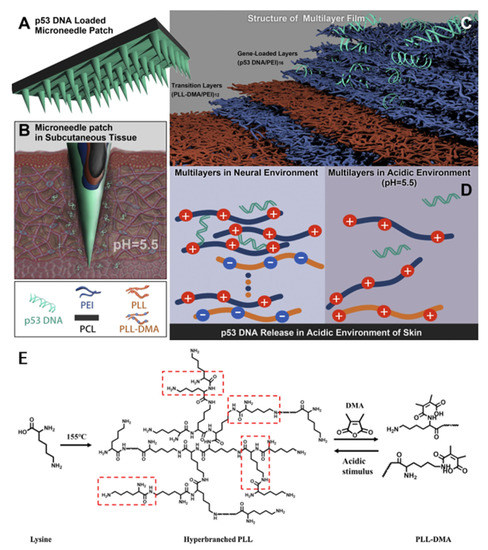
Figure 3.
Scheme of a microneedle patch modified with pH-responsive transition layers and gene-loaded layers using layer-by-layer assembly. (A–D) The two layers of a layered structure are composed of a pH-sensitive transition layer and a gene-loaded layer. When a microneedle patch is placed on the skin, the microneedle coating contacts the skin microenvironment, the negatively charged portion of the PLL-DMA will transform into a positively charged one. The transition layer will then collapse, which will accelerate the release of the outermost p53 DNA. (E) The synthetic path of PLL and PLL-DMA. Reprinted with permission from [66]. Copyright 2019, Elsevier.
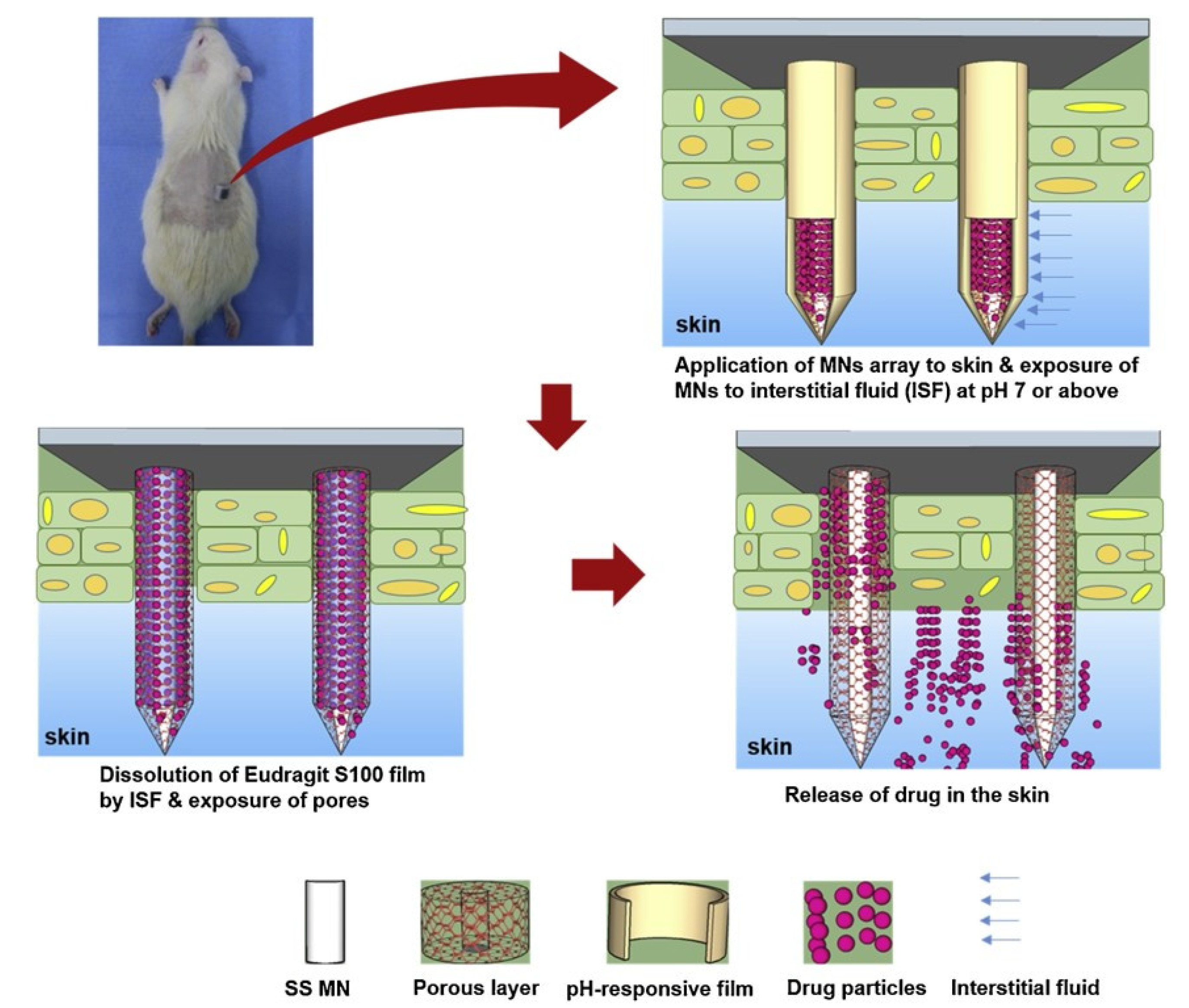
Lastly, a pH-responsive wound coating was proposed on porous polymers, which covered the pores of drug-filled porous microneedles to prevent drug leakage and drug release in the wound pH environment (Figure 4). At the pH of healthy skin (4.5), drug release from the microneedles was negligible [67]. In contrast, significant release occurred in the wound pH environment. This kind of microneedle model that can be produced in large quantities was developed, and coating materials with different reaction conditions were combined with antibacterial agents and anti-inflammatory drugs to increase the treatment of wound infections.
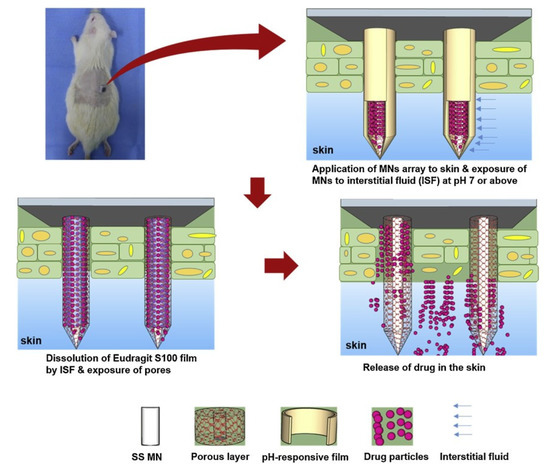
Figure 4.
After the microneedles are exposed to the medium at alkaline pH (vulnus pH), the drug encapsulation film is dissolved, and the pores on the microneedle are exposed, which releases the encapsulated payload in the vulnus pH microenvironment. Reprinted with permission from [67]. Copyright 2021, Elsevier.
2.2. Reactive Oxygen Species-Responsive Microneedles
Reactive oxygen species (ROS) are important signals for biological metabolism and intercellular communication. In various pathological processes such as diabetes, inflammation, aging, neurodegenerative diseases, and cancer, ROS levels are significantly higher than normal due to metabolic abnormalities [68,69,70,71,72,73]. By exploiting the difference in ROS levels between normal and diseased tissues, various ROS responsive groups have been developed for ROS-specific responsive drug delivery systems. Currently, ROS-responsive microneedles are mainly used for the treatment of diabetes. We focus on the application of ROS-responsive microneedle-based immunotherapy design for the prospect of being applicable to other diseases.
Commonly used ROS-responsive polymers have two main responsive mechanisms. One is the change of hydrophilicity and hydrophobicity under the action of ROS, and the other is the cutting change of structure affected by ROS [74,75,76,77,78]. For one, ROS can oxidize chalcogenide elements and increase their valence. During this process, oxygen and sulfur atoms form covalent bonds, and polar groups form hydrogen bonds with ambient water molecules, thereby initiating a hydrophobic–hydrophobic–hydrophilic transition of the polymer backbone without disrupting the polymer’s chemical structure [79]. For another, ROS can react with chemical structures such as thioketals (TKs), phenylboronic acids/esters (PBAs/PBEs), vinyl disulfides, and proline oligomers, resulting in the cleavage of these structures [80]. A variety of ROS-responsive microneedles were designed through these two mechanisms.
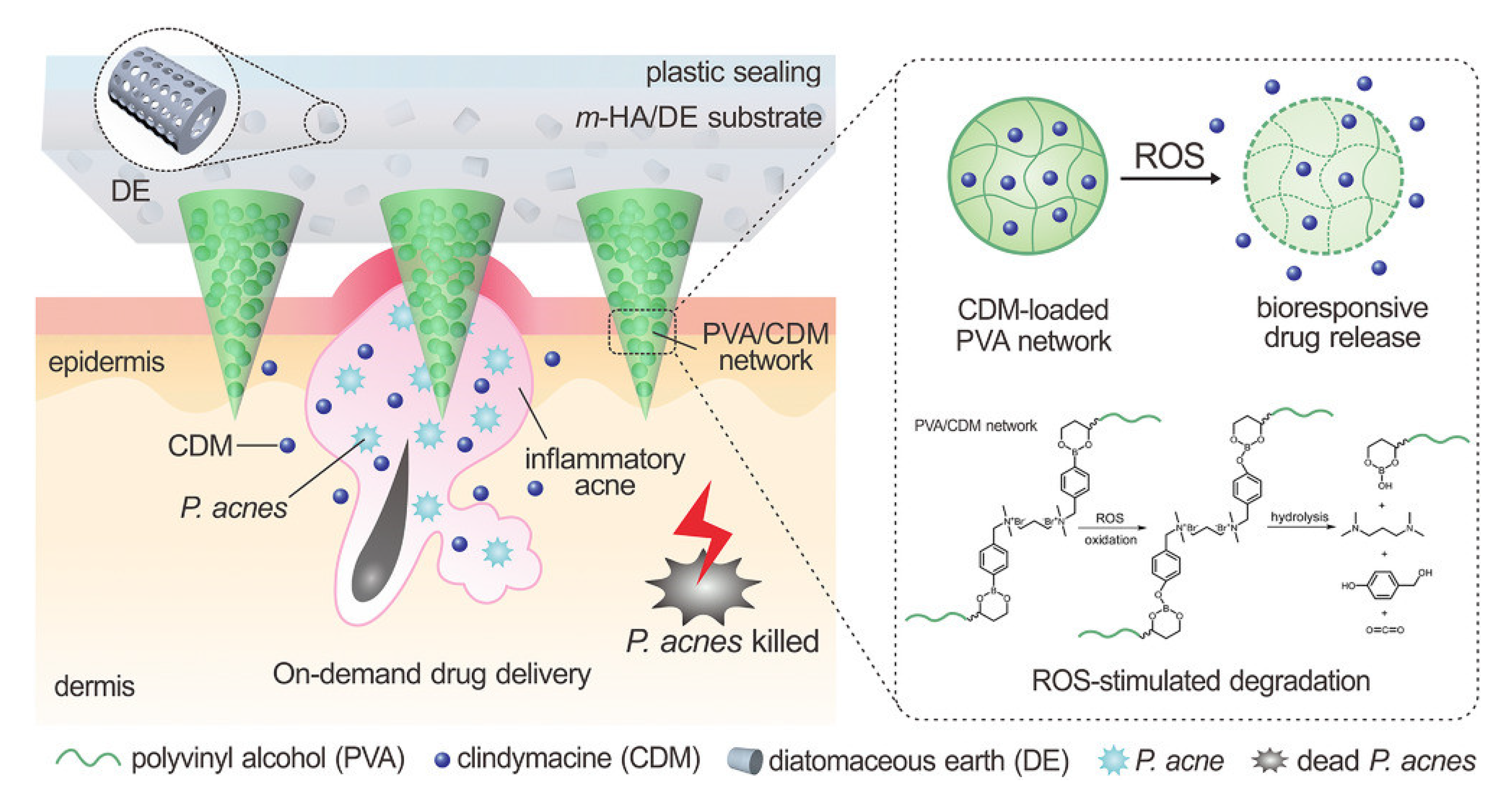
Authors have proposed a new drug delivery method for antiacne treatment using ROS-responsive microneedle patches (Figure 5) [81]. This method avoids the risk of destroying intestinal flora and other risks caused by oral antibiotics or isotretinoin. Compared with commonly used acne creams, microneedles can enhance the efficacy of dermal lesions through skin penetration. Controlled and sustained release of drugs to counter the overproduction of reactive oxygen species in acne is also important for improving antimicrobial efficacy and reducing side effects. Therefore, microneedles were fabricated from drug-loaded ROS-reactive poly (vinyl alcohol) (RR-PVA) matrices to achieve on-demand drug release and reduce side effects. In addition, a matrix containing methacryloyl hyaluronic acid (m-HA)/diatomaceous earth (DE) was used as a support matrix for the microneedles, which can absorb pus and other purulent exudates and debris to promote healing, potentially preventing future relapse. The related study shows that this ROS-responsive microneedle patch can effectively transfer antibiotics to the dermis and can also attach functions such as adsorbing harmful substances in the wound to eliminate acne in a convenient manner.
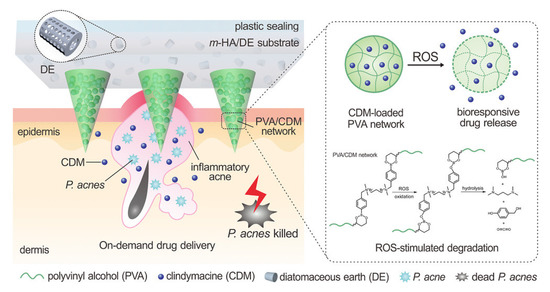
Figure 5.
The mechanism diagram of a microneedle patch responding to ROS in an acne pathological environment. In order to adsorb pus and cell debris and their necrotic cell by-products, diatomite (DE) was used as one of the materials. For more softness and better biocompatibility, methacrylic acid esterified hyaluronic acid was used. Both promote wound healing and prevent potential recurrence. Drug-responsive polyvinyl alcohol (RR-PVA)-ROS was released on demand under pathological conditions to reduce side effects. Reprinted with permission from [81]. Copyright 2018, John Wiley and Sons.
2.3. Enzyme-Responsive Microneedles
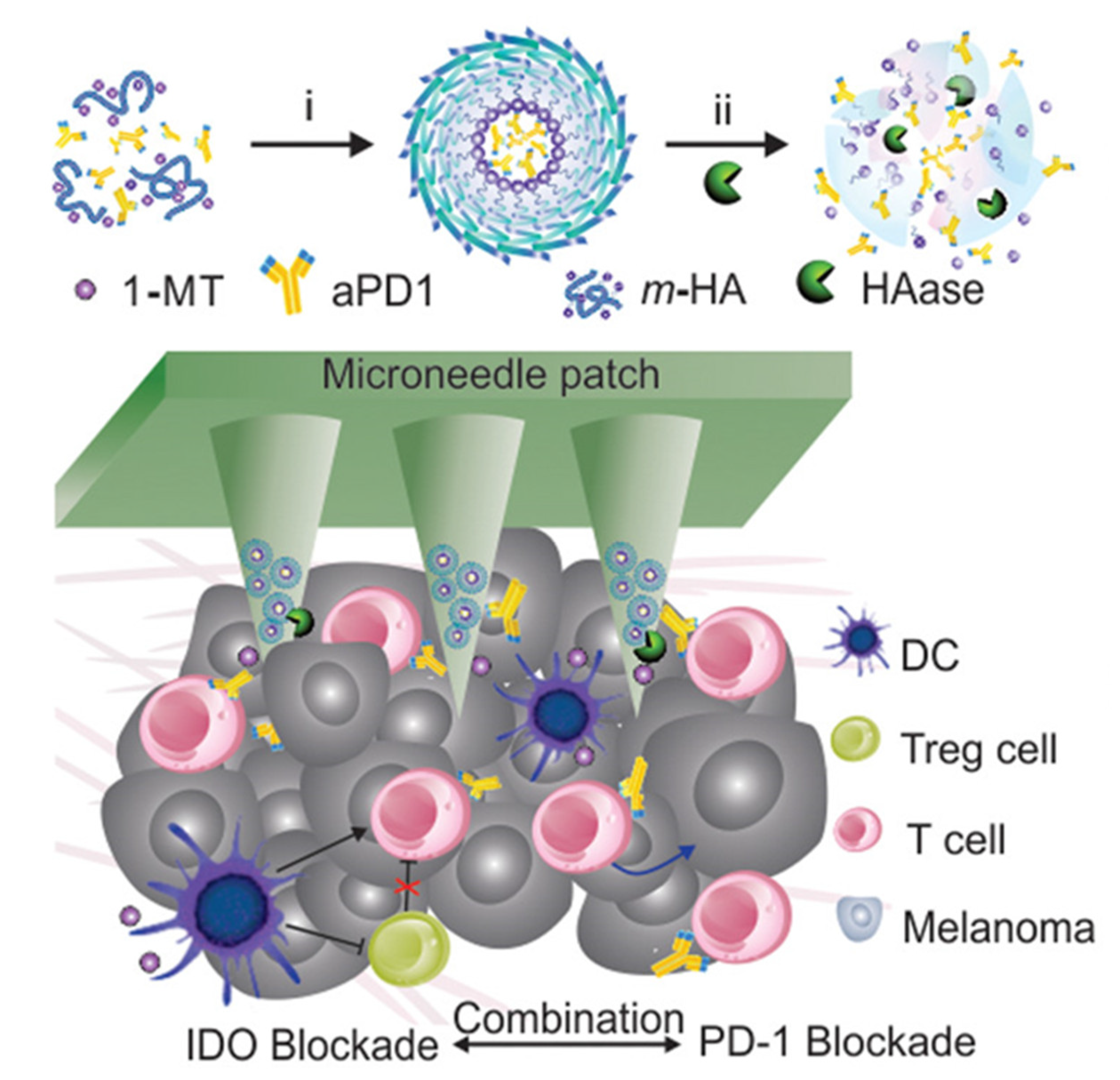
Enzymes are ubiquitous in metabolic reactions in the body and play a vital role in healthy metabolic homeostasis. When diseases occur, the function of enzymes and the content of specific enzymes are mostly abnormal, especially in tumors. It was found that the expression level of enzymes is correlated with the stage of cancer development at all stages of cancer. Because of the high availability of hyaluronidase, it has been used as a key target in many works to design enzyme-responsive drugs [82,83,84,85]. The overexpression of hyaluronidase in the tumor microenvironment is used to achieve enzyme-responsive drug release in the tumor area [86,87]. In one work, hyaluronic acid-loaded anti-PD1 antibody (aPD1)-entrapped immunotherapeutic nanoparticles were combined with the IDO inhibitor 1-methyl-DL-tryptophan (1-MT) to assemble nanoneedles (Figure 6) [88]. The designed enzyme-responsive microneedle drug delivery device could trigger sustained release and enhance the retention of checkpoint inhibitors in the tumor microenvironment. Compared with the absence of hyaluronidase, aPD1 and 1-MT release increased to 4 and 2 times in the presence of hyaluronidase, respectively. This enzyme-responsive microneedle produced enhanced T-cell immunity in a B16 mouse melanoma model, alleviated local immunosuppression, effectively inhibited melanoma growth in mice, and contributed effectively to antitumor immunotherapy.
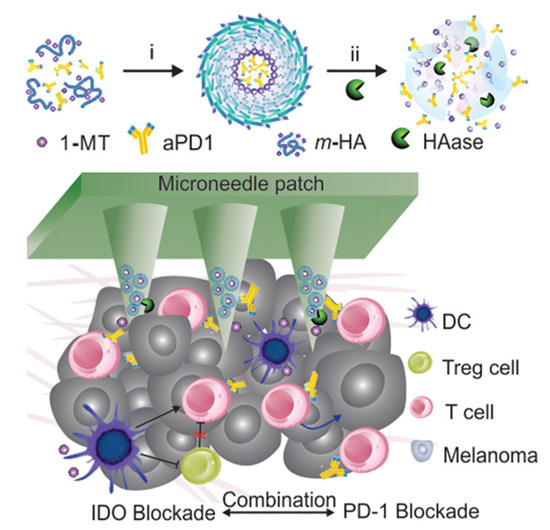
Figure 6.
A schematic diagram of the hyaluronic acid enzyme-response microneedle patch combined with immune adjuvant therapy. The self-assembled nanoparticles (NP) of IDO and aPD1 were dissociated from the microneedles under the action of HAase and combined with DC cells and T cells to exert immunotherapy. Reprinted with permission from [88]. Copyright 2016, American Chemical Society.
In addition to tumor immunotherapy, enzyme-responsive microneedles also have outstanding applications in antibacterial therapy. Studies reported that the expression of gelatinase at the wound site was significantly upregulated [89,90], indicating favorable conditions for the use of gelatinase-responsive microneedle for antimicrobial therapy and wound healing. X Lei et al., designed a degradable microneedles patch made of physically inert polymer PVP K-30 and recombinant type III collagen, which released antibacterial peptides encapsulated in gelatin nanoparticles in the presence of overexpressed gelatinase at the wound, achieving antibacterial treatment and healing of chronic wounds as well as remarkable therapeutic effects in mouse models [91].
The advantage of enzyme-responsive microneedle systems is that they can utilize the differences in enzyme expression levels between the pathological microenvironment and the normal physiological environment to achieve specific treatment and minimize the potential toxicity of drugs to normal cells and tissues. Nevertheless, it is difficult to achieve a complete controlled release of drugs based on enzyme response alone, and there is the possibility of the early release of drugs. Therefore, the combination of enzyme response with other response methods will effectively improve the utilization efficiency of drugs.
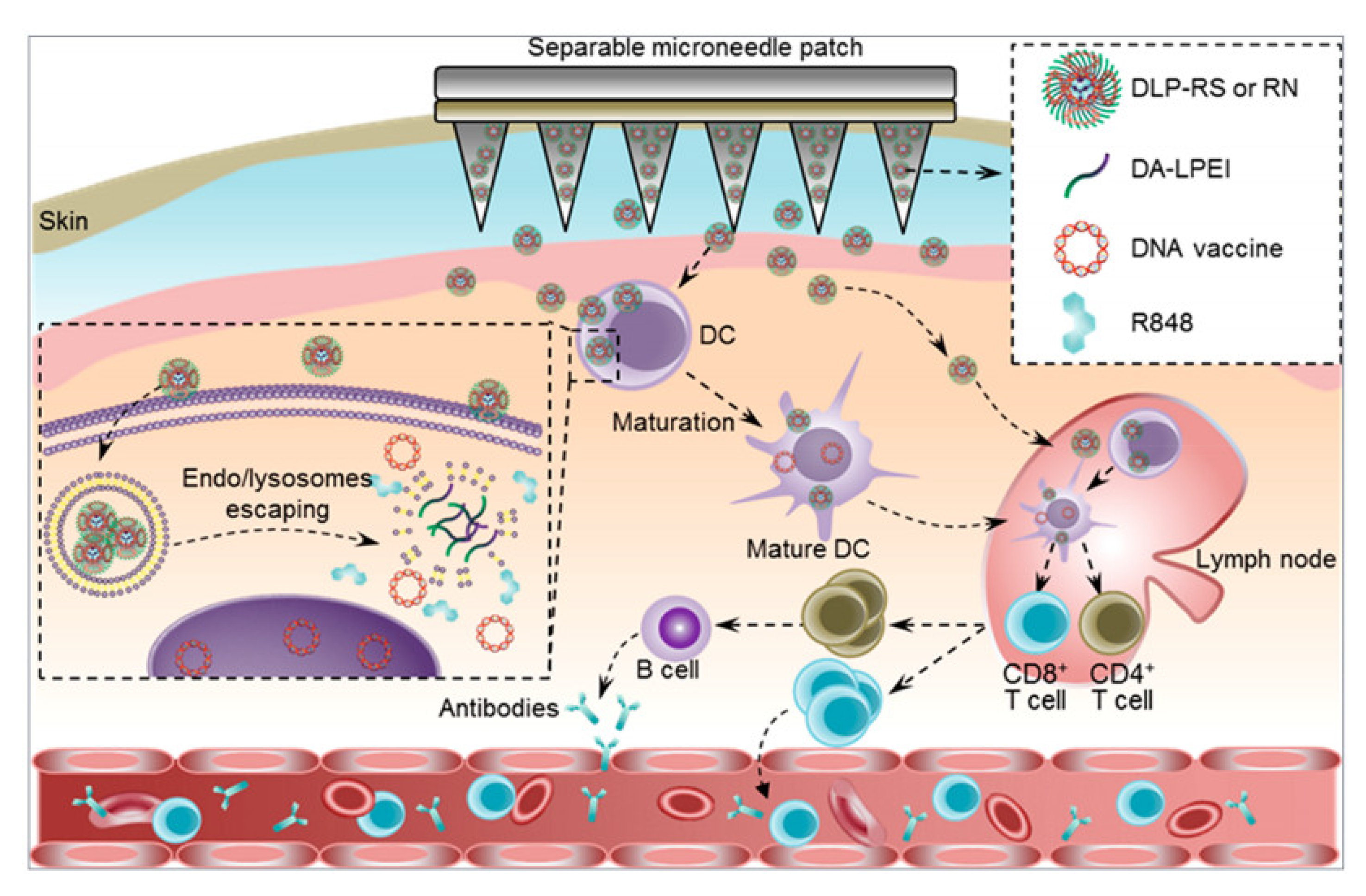
2.4. Temperature-Responsive Microneedles
Temperature response is an important research aspect of smart biomaterial response. Temperature-responsive microneedles utilize the property of phase change of heat-sensitive polymers according to the body temperature to achieve the controlled release of drugs. At present, a variety of heat-sensitive polymers have been used for the preparation of temperature-responsive microneedles [92,93,94]. The body surface temperature is around 33–37 °C. Under some pathological conditions, the skin temperature will increase or decrease depending on the type and process of disease [95]. Therefore, the change of body surface temperature according to the pathological conditions can be used as an effective stimulus for the temperature-responsive microneedles to release drugs. The traditional microneedle systems need the patch to adhere to the skin for a long time to achieve sustained drug release, which poses a challenge to the adhesion of microneedle patch. Many studies have focused on enhancing the adhesion effect by changing the morphology of the microneedles or replacing the substrate material [96,97]. However, some studies have considered the controllable separation of the tip and the substrate by adding a heat-sensitive polymer in the microneedle system so as to achieve more reliable sustained drug release [98,99,100]. Yue Yin and colleagues used temperature response in developing a separable microneedle system capable of delivering DNA vaccines and immune adjuvants [99]. Firstly, deoxycholic acid conjugated low-molecular weight polyethylenimines (DA-LPEI) nanoparticles coated with an immune-stimulating agent R848 are prepared, a DNA vaccine is then adsorbed on the surface of the nanoparticles via electrostatic interaction, and finally the nanoparticles are encapsulated at the tip of a microneedle. PNIPAM-B is added between the tip and a PVA substrate as a separation layer. PNIPAM-B has a low critical solution temperature (14–16 °C), is insoluble in water at room temperature (~22 °C), and is highly soluble at or below 14 °C. After the microneedles are embedded into the skin, the tip and the substrate can be separated by reducing the skin temperature to 14–16 °C for several minutes, with the tip being retained in the dermis layer to continuously release the DNA vaccine. The results showed that the microneedles could stably store the DNA vaccine at room temperature for up to 30 days, and the tip could be effectively separated from the substrate by temperature control, resulting in a durable and strong antiviral immune response (Figure 7).
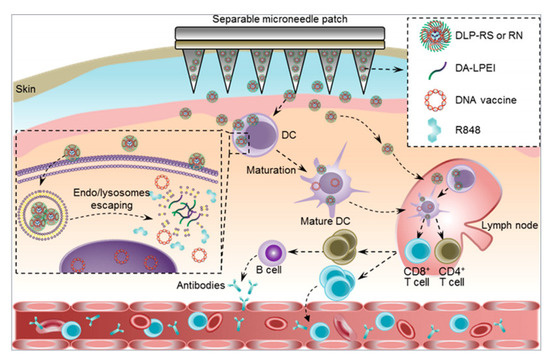
Figure 7.
Schematic illustration of the separable microneedle patch mediated intracutaneous delivery of DNA nanovaccines for fighting the SARS-CoV-2 virus. Deoxycholic acid-conjugated low-molecular weight polyethylenimines (DA-LPEI) was applied to encapsulate both R848 and S-or N-protein-encoding DNA vaccines (DLP-RS or RN). The microneedle patch can painlessly penetrate the epidermis into the dermis layer, where it releases the DLP-RS or DLP-RN nanoparticles. Reprinted with permission from [99]. Copyright 2021, American Chemical Society.
For certain temperature-sensitive and fragile active drugs such as mRNA, achieving effective in vivo delivery is environmentally demanding, and it is delivered mainly via intramuscular injection, which usually causes pain. Moreover, conventional microneedles cannot meet the temperature-sensitive requirements for the delivery of active drugs. Meanwhile, the materials used to prepare the microneedles must meet certain strength and hardness requirements to achieve a successful puncture, which limits the selection of materials and thus restricts the application of the microneedles. Therefore, cryomicroneedle technology has arisen at a historic moment.
Cryomicroneedles are capable of delivering a variety of active substances based on aqueous materials without impairing the activity of biological substances, with the tip remaining in the skin to continuously release the drug after the ice base melts under the influence of body temperature. Xiaoxuan Zhang et al., selected various types of materials, including water, temperature-curable materials, light-curable materials, and ion-crosslinked cured materials, which achieved significant strength enhancement after freezing and enabled effective delivery of small-molecule drugs (RhB), macromolecular drugs (fluorescein isothiocyanate-labeled BSA, erythropoietin), and microorganisms (bacillus subtilis) [88]. Jinming Yu et al., mixed mRNA with HA solution and prepared cryomicroneedles which can effectively puncture the skin by freezing [2]. Compared with PEI or liposome carrying the mRNA, the freezing operation did not affect the transfection efficiency of mRNA in HA microneedles. Specific B-cell and T-cell immune responses were successfully induced in mouse experiments. Although there are still some challenges to be solved, such as disinfection methods and dose control, the flexibility of carrying active drugs on cryomicroneedles is still encouraging for the development of a new generation of microneedles [101].
As shown in Table 1, in addition to the work specifically described above, we also outline several representative responsive microneedles triggered by internal stimuli, outlining their microneedle design methods. It is hoped this can inspire methods and ideas for the comprehensive design of microneedle-based immunotherapy.

Table 1.
Representative responsive microneedle triggered by internal stimuli.
3. Microneedles Triggered by External Stimuli
In this section, we introduce the functions and structures of responsive compounds for externally triggered responsive microneedles and their biomedical applications.
3.1. Optical-Activated Microneedles
Optical triggering has the advantages of noninvasiveness, high spatial resolution, and temporal controllability [105,106]. Light-activated nanomaterials for cancer phototherapy include photothermal conversion materials, photosensitizer materials, and nanoplatforms containing photo-responsive parts [107,108,109]. Photothermal conversion nanomaterials are a type of material that can absorb light energy and convert it into heat energy leading to the death of cancer cells [110]. In general, photothermal conversion nanomaterials can be divided into organic materials and inorganic materials. Organic photothermal conversion nanomaterials can be synthesized by modifying organic dye molecules (i.e., indocyanine green; ICG) or using semiconductor polymers to prepare nanoparticles. Inorganic photothermal conversion nanomaterials include noble metal materials (i.e., gold nanomaterials), transition metal sulfides and oxides (i.e., copper sulfide nanoparticles), or carbon-based materials (i.e., graphene oxide). Using these materials to design controllable, light corresponding microneedles can realize the synergistic effect of chemotherapy and photothermal therapy (PTT) in tumor treatment.
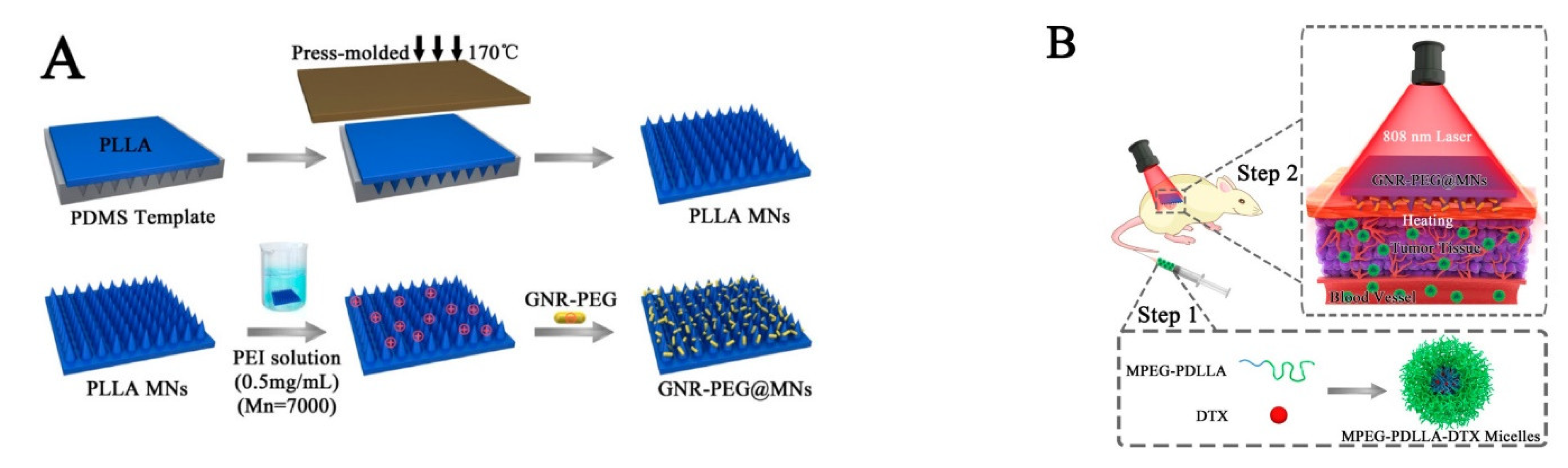
PTT is a promising therapeutic approach, with minimal invasiveness and good curative effect in cancer treatment. Under the irradiation of an external laser, these materials absorb light energy and convert it into heat energy, thereby killing tumor cells [111,112,113]. In one study, a near-infrared (NIR) responsive polyethylene glycol gold nanorod (GNR-PEG) coated poly (L-lactide) microneedle system (GNR-PEG@MN) was developed to improve the antitumor efficiency of docetaxel-loaded MPEG-PDLLA (MPEG-PDLLA-DTX) micelles for the treatment of A431 tumors (Figure 8) [114]. This system showed excellent heating ability both in vitro and in vivo. Moreover, GNR-PEG@MN has good skin insertion ability (with a height of 480 μm) and excellent biosafety. GNR-PEG@MN also exhibited good heat transfer ability in vivo, and the temperature of tumor site reached to 50 °C within 5 min. Compared with only chemotherapy or PTT treatment, this combination of GNR-PEG@MNs and MPEG-PDLLA-DTX micelles completely inhibited the growth of A431 tumors in vivo without recurrence, showing a significant synergistic effect.
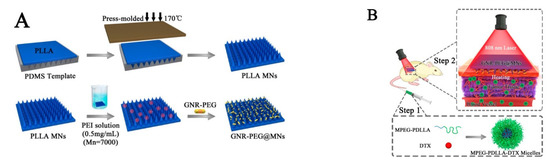
Figure 8.
(A) The schematic diagram of the preparation process of PLLA microneedles and GNR-PEG@MN. (B) GNR-PEG@MN and MPEG-PDLLA-DTX micelles respond to near-infrared light and combined with chemotherapy to synergistically treat A431 tumors. In the first step, DTX micelles were injected. In the second step, microneedles were pressed on the tumor site and irradiated with an 808 nm laser at a power of 2 W/cm2 for 5 min. Reprinted with permission from [114]. Copyright 2017, American Chemical Society.
3.2. Mechanical Force-Responsive Microneedles
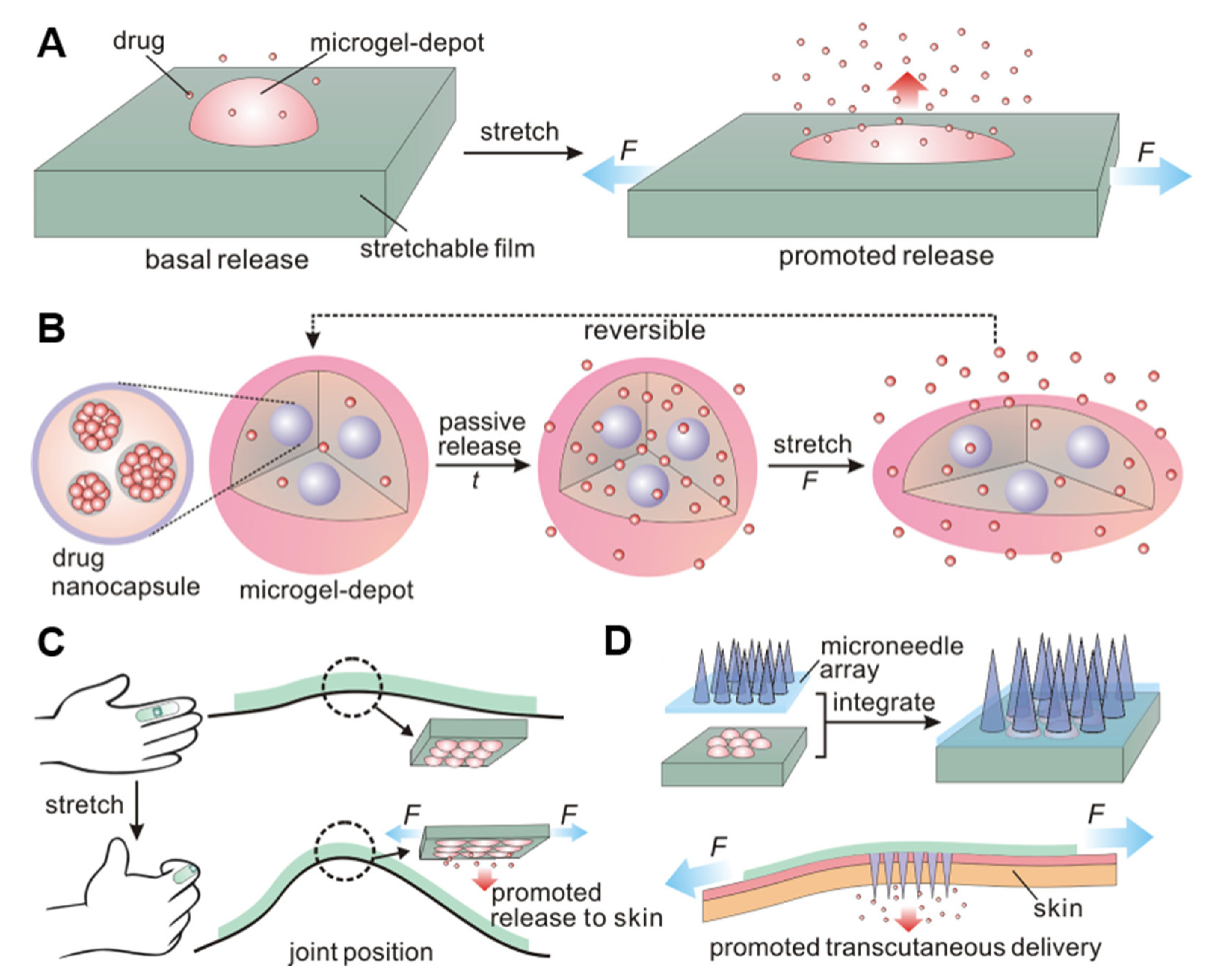
Stimulus-triggered drug delivery systems can achieve controlled release of dose, space and/or time and add many entry points for the design of a sustained release system. Many “smart” formulations developed thus far have been based on multiple stimuli, which can be physiological internal stimuli, such as ROS, redox potential, PH, ATP, and enzyme activity, or external physical triggers, such as NIR, thermal, ultrasound, and magnetism. Meanwhile, the method of triggering drug release based on mechanical forces such as stretching, pressing, and rotation is often transformed into clinical practice. Due to individual differences and complex physiological environments, it is impossible to accurately control the drug release dose, and the external trigger-mediated method is limited by additional instruments. Mechanical strain-based stimuli, accompanied by frequent daily motion, can provide a reliable and easy way to promote drug release in space and time (Figure 9) [35]. This strain change can be easily achieved through skeletal muscle elongation and shortening as well as bone, tendon, and joint cooperation. Furthermore, strain-triggered delivery systems are expected to release analgesics or rescue drugs from self-administration through simple body movements.
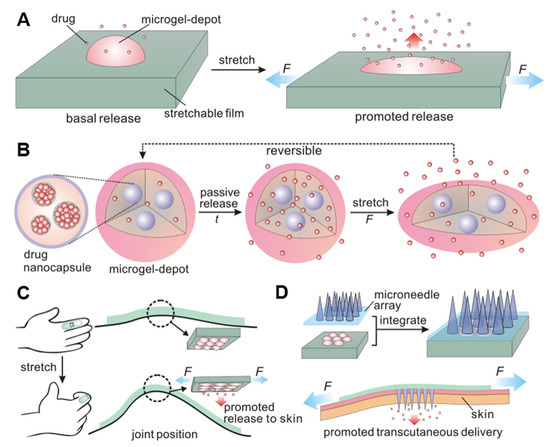
Figure 9.
Diagram of the mechanical force response delivery system. (A,B) The elastomeric substrate deforms under stretching, releasing the drug from the microreservoir. (C) The drug-loaded patch is attached to the finger joint, and the drug release is triggered by bending the finger. (D) The drug-loaded patch is combined with the microneedle array patch, and the drug released from the drug-loaded library is transdermally administered through the microneedles. Reprinted with permission from [35]. Copyright 2015, American Chemical Society.
Microneedle systems based on mechanical force response are roughly divided into two types. One type functions to achieve controlled drug release by increasing the specific surface area of elastic microneedles through mechanical stretching. For example, the stretchable microneedle system developed by J Di and colleagues consists of hydrogel microneedles containing nanoparticles loaded with drugs on an elastic substrate [115]. The drugs are rapidly released in response to stretching by mechanical forces. However, this system has certain problems in accurate drug delivery because the quantitative relationship between the tensile force and the responsive release is difficult to control. The other type involves separating the microneedle tip from the substrate by mechanical stretching. Most microneedles systems face the problem that the microneedle patch easily falls off the skin before completing the release of drugs. The separation of the microneedle tip and the substrate through mechanical force response can solve this problem well. The rapid response microneedle patch developed by the Hyesun Jun team consist of a soluble HA tip and an insoluble PCL substrate [116]. After the microneedles are inserted into the skin, the HA tip is quickly separated from the substrate by the piercing mechanical force and remains in the skin to continuously release the drug.
Although there are few self-developed miniature-controlled drugs delivery systems mainly using pressure, these systems still provide us with a free, controllable, and convenient method of drug delivery. Combined with microneedles triggered by mechanical force, different trigger strengths and trigger angles can be designed to facilitate controllable and autonomous drug delivery. Table 2 summarizes the construction, payload, and application of representative responsive vaccines triggered by external stimuli.

Table 2.
Representative responsive microneedle-based immunotherapy triggered by external stimulus.
4. Responsive Microneedle for Cancer Immunotherapy
Responsive microneedle-based immunotherapies, which are triggered in multiple forms and combined with multiple therapies, are an outstanding representative of on-demand drug delivery technology, meeting the treatment expectations of improving treatment efficacy and reducing systemic side effects [128,129]. This type of therapy can overcome the shortcomings of traditional drug carriers, can accurately control the drug release site, and can increase the therapeutic effect against diseases [130]. The internal stimuli mentioned in this paper, as well as the various external stimuli such as magnetism, temperature, and light, are constantly being explored by designers based on these factors. However, since single-responsive nanodrug carriers are sometimes not highly sensitive to a single factor, researchers are now focusing on the design of dual- and multiresponsive nanodrug carriers, such as pH/reduction, pH/temperature, reduction/enzyme, or pH/reduction/enzyme. More importantly, responsive microneedle-based immunotherapy is friendly to the human body [126] and easy to develop and biodegrade [131].
Tumor immunotherapy is a promising strategy to preventing cancer proliferation by activating the immune system to fight tumors. Some biological vaccine preparations, such as Sipuleucel-T (autologous active immune cell therapy) [132,133,134,135], have been used clinically. Inhibition of tumor progression by inducing immune responses has become a research hotspot. In immunotherapy, checkpoint inhibitors, such as anti-PD-1 [136], have been widely introduced into clinical practice. As another immunotherapy-based strategy, tumor vaccine can also open up a new field for tumor immunotherapy because it can induce antigen-specific immune response and activate immune memory [137,138,139]. However, systemic toxicity and low immunogenicity limit its wide clinical application. In addition, The application of tumor vaccine is also limited by the off-target effect of cytokine induction and immune stimulation adjuvant. Fortunately, biomaterials such as polymers [140,141,142], scaffolds [14], liposome [143,144,145], microneedle, and others [53,146,147,148] provide a possible answer due to their valuable properties, including excellent biosafety and biometabolism, on-demand control of size, high load of immune-related components, and multiple sites of immune ligand binding. Therefore, various biocompatible carriers are being used in tumor vaccines to enhance the immunogenicity of tumor antigens so that antigens can effectively and freely exert antigen presentation [149,150,151]. Combined with the above-mentioned responsive materials, microneedles can improve immune responses of various cancer immunotherapies. Here, we will briefly outline several representative works on responsive microneedles cancer immunotherapy.
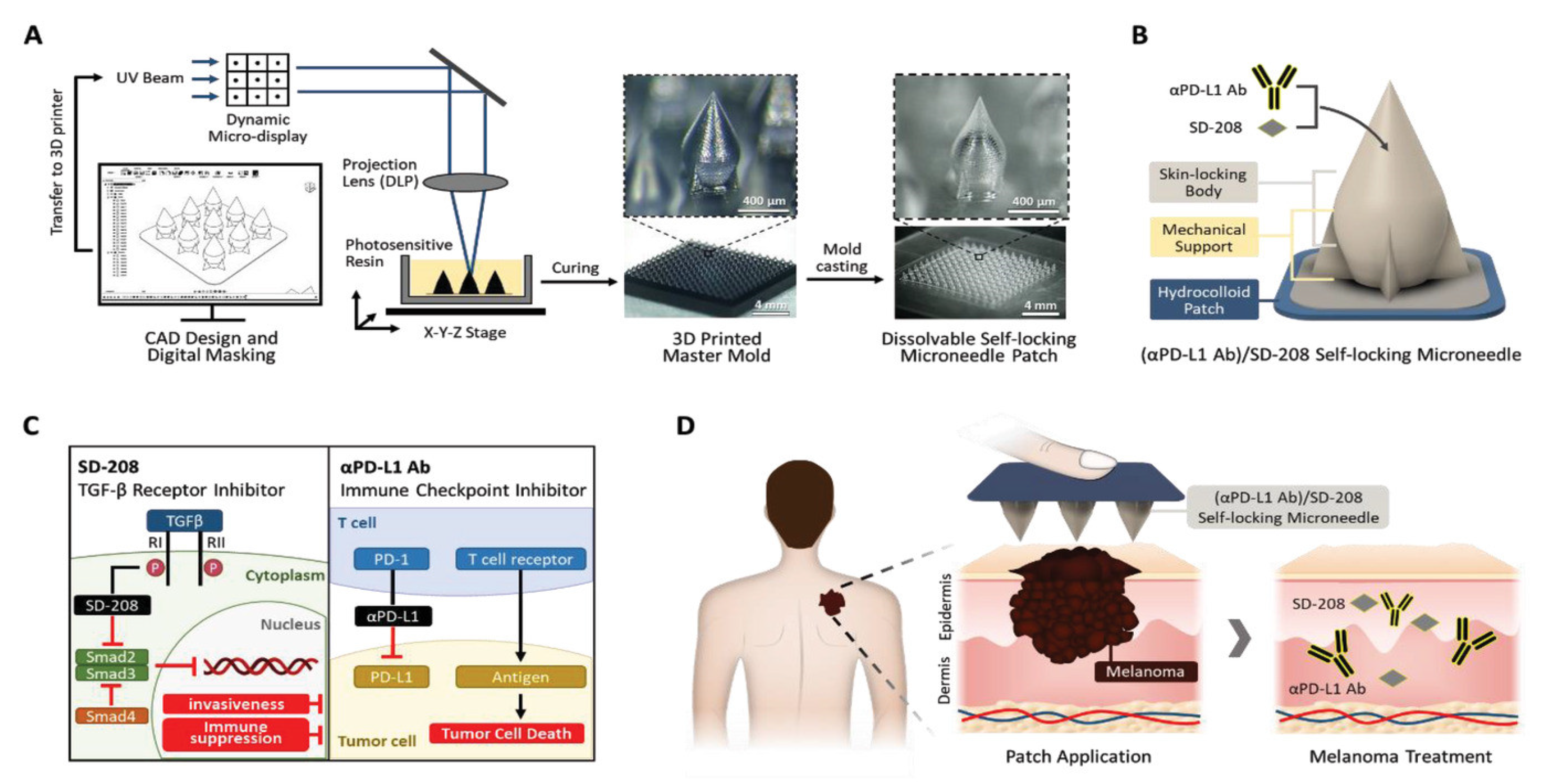
Traditionally, due to the limited machining capacity, dissolvable microneedles were mostly made into conical or polygonal conical geometric shapes, and the stability of microneedles entering the skin is insufficient [152,153,154,155,156,157]. One study overcame the limitations of the conventional microneedle. Self-locking microneedles fabricated by a novel projection microstereolithography 3D printer greatly increased the adhesive dose and transdermal drug delivery after insertion into the skin [158]. Self-locking microneedles attached to a flexible hydrogel patch, consisting of a narrow base with mechanical support, a sharp skin penetrating tip, and a wide skin interlock (Figure 10). This design greatly improves the accuracy of the microneedle’s penetration of irregular skin surfaces, especially for the irregular and uneven surface of melanoma skin. In terms of immune strategy, the combination of a new transforming growth factor-β (TGF-β) inhibitor (SD-208) and immune checkpoint anti-PD-L1 strongly inhibited tumor proliferation and metastasis, showing enhanced immunotherapy. Compared with that of intratumoral injection, the effective dose of self-locking microneedle-based immunotherapy to inhibit tumor is significantly lower.
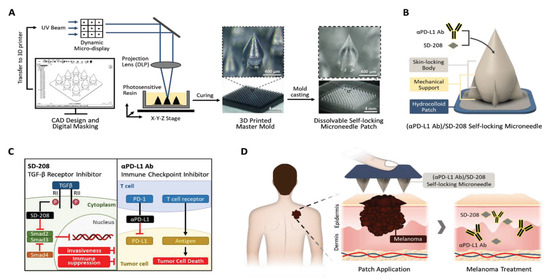
Figure 10.
Fabrication of a self-locking microneedle patch. (A) The process of making the self-locking microneedle patch with a 3D printer based on surface projection microstereolithography technology. (B) The geometric structure of the self-locking microneedle: the sharp tip penetrates the skin, and the wide body and support structure at the bottom strengthen the bonding strength between the microneedle and the skin. (C) The mechanism of action of TGF-β receptor inhibitor SD-208 and immune checkpoint inhibitor αPD-L1Ab. (D) Schematic diagram of drug-loaded self-locking microneedles applied to melanoma. Reprinted with permission from [159]. Copyright 2023, John Wiley and Sons.
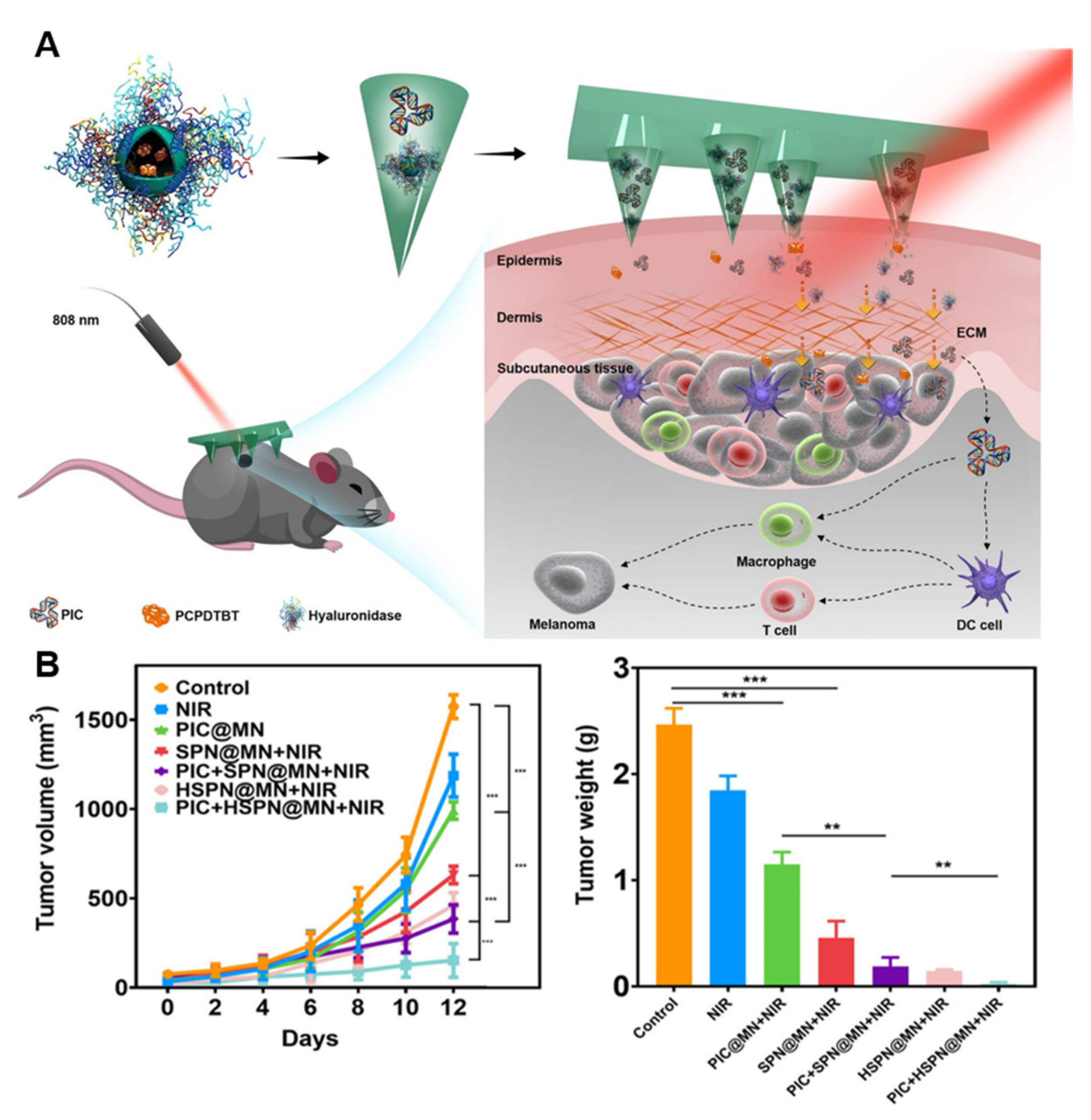
Due to the objective existence of the tumor matrix barrier, the killing effect of drugs and immune cells will be limited and cannot be deepened, thereby impairing the efficacy of cancer immunotherapy. One study reported an innovative synergistic PTT and immunotherapy [160]. Hyaluronidase and the semiconducting polymer poly(cyclopentadithio-phene-alt-benzothiadiazole) were used as microneedle substrates to deliver the immune adjuvant, polyinosinic acid (PIC). After the microneedles penetrated into the skin, hyaluronidase dissolved into the extracellular matrix, and semiconductor polymer nanoparticles and PIC were released into the tumor microenvironment (Figure 11A). Under laser irradiation, the microneedles interacted with PIC to activate immune cells, enhance T-cell immune response, and inhibit tumor growth and spread. For the in vivo experiments, hyaluronic acid-responsive microneedles encapsulated with semiconductor polymers and immune adjuvants showed excellent tumor growth inhibition ability (Figure 11B). This work developed an efficient microneedle platform that combines PTT with immunotherapy. This solved the obstacle of the tumor matrix barrier and effectively realized the immunotherapy of melanoma in a mouse model.
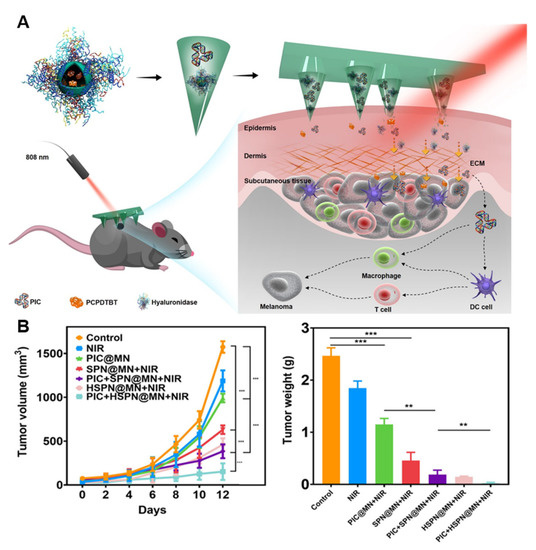
Figure 11.
Photothermal microneedle for cancer immunotherapy. (A) Schematic of the microneedle system for synergetic cancer therapy. (B) Tumor inhibition effect of the mouse model. The statistical significance was assessed through one-way ANOVA statistical analysis or paired Student’s t tests: (**) for p < 0.01, and (***) for p < 0.001. Statistical significance was considered as p < 0.05. Reprinted with permission from [160]. Copyright 2021, American Chemical Society.
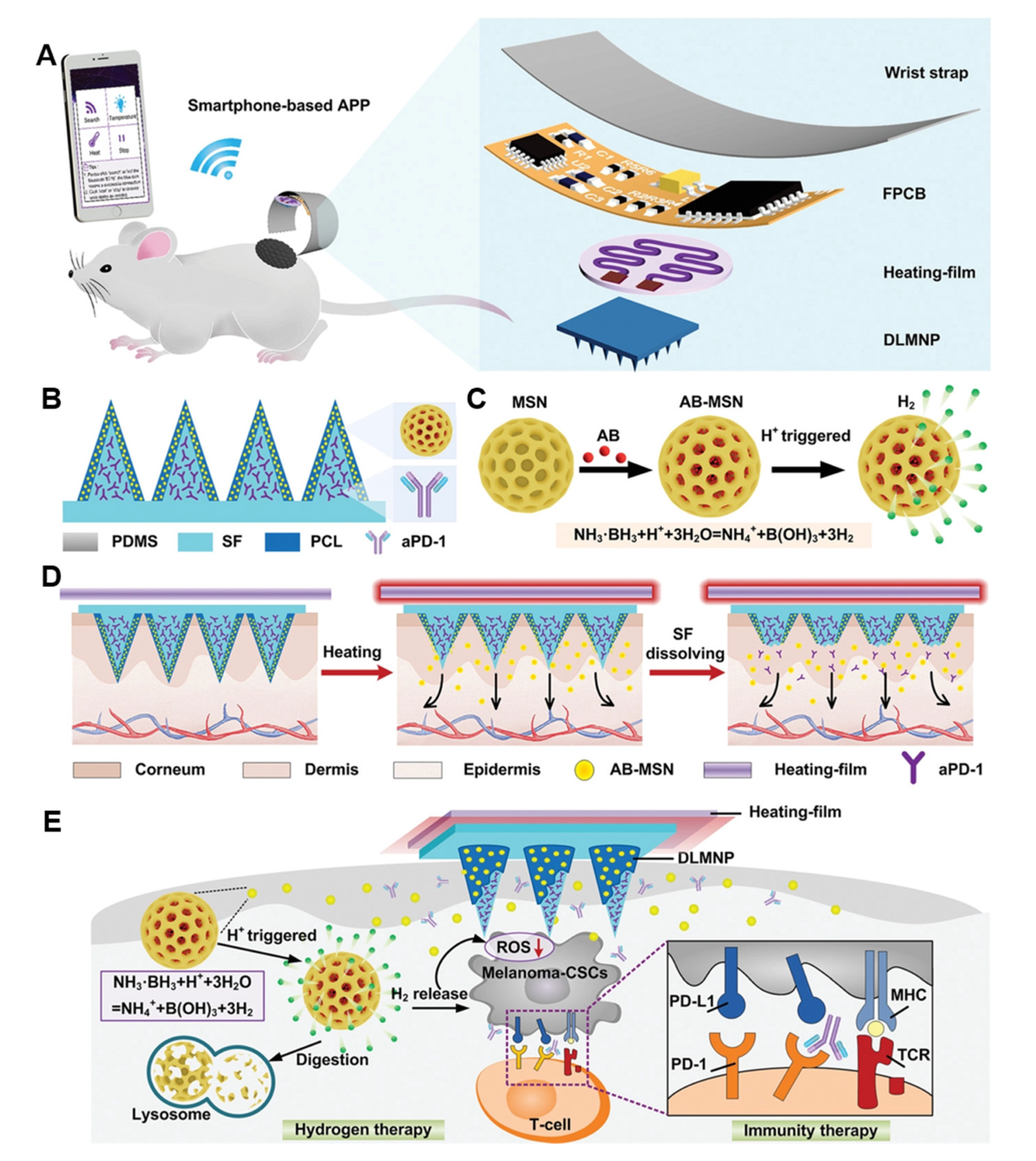
Cancer stem cells (CSCs) are the main cause of tumor recurrence, progression, and treatment failure [159,161,162,163,164]. Although aPD1 antibody can be used to treat CSCs, its therapeutic effect is greatly reduced due to the immune escape evolution of CSCs [165]. In one study, a wearable silk microneedle device (SMND) was developed combining synergistic immunization and hydrogen therapy. The device is made of a double-layer microneedle patch (DLMNP) and drug-loaded APD1 silk fibroin (SF) as an internal matrix for immunotherapy [166]. Ammoniaborane-loaded mesoporous silica nanoparticle (AB-MSN) coated polycaprolactone releases hydrogen in the layer upon thermal stimulation. The highlight of SMND is that the release of responsive drugs can be controlled by smartphones to achieve sustained anti-CSC therapy (Figure 12). The experimental results of the melanoma model using B16F10-CSCs tumor-bearing mice showed that the synergistic treatment strategy had minimal systemic toxicity and could achieve satisfactory antitumor and anti-CSCs effects. In summary, the intelligent and collaborative design of SMND has elevated the diversity and controllability of microneedle-based immunotherapy treatment methods to a new level.
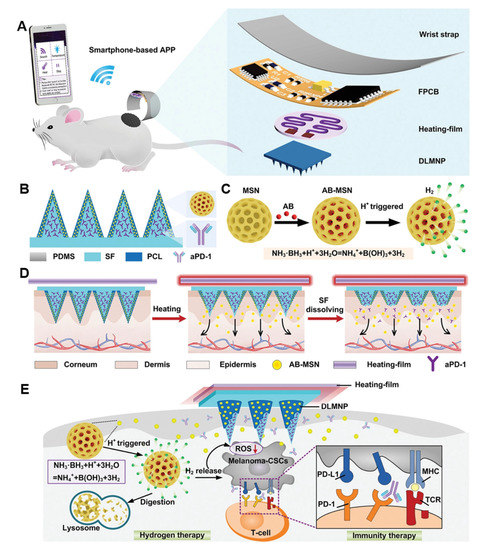
Figure 12.
The schematic diagram of SMND preparation and the intelligent drug delivery scheme. (A) The SMND patch is mainly composed of a microneedle patch layer, a heating layer, and a flexible circuit layer (FPCB), which is controlled by a smartphone application (APP). (B) The structure and composition of the microneedle patch layer. The SF loaded with aPD-1 is inside the microneedle, and the PCA-coated AB-MSN is a thermally responsive outer coating. (C) The acid-triggered decomposition and release H2 diagram of AB-MSN. (D) The drug release diagram of SMND under APP control. (E) The mechanism of SMND synergistic immune/hydrogen therapy for CSCs. Reprinted with permission from [167]. Copyright 2022, John Wiley and Sons.
Table 3 lists several of the immune microneedle anticancer vaccines with practical value and market prospects, outlining their design ideas, response methods, and applicable diseases. We hope to provide effective ideas for the design of anticancer microneedle-based immunotherapy.

Table 3.
Representative responsive microneedle vaccine for cancer immunotherapy.
5. The Limitations of the Microneedle-Based Drug Delivery System
Although the microneedle-based drug delivery systems have many advantages and market application prospects, some physical and chemical limitations still need to be addressed in future. The molecular weight of the drug planned for use in the microneedle-based drug delivery system should be less than 500 Da [174], and the lipophilic LogP should be 1–3 in order to diffuse smoothly in the skin [175]. Therefore, the application of peptides and macromolecular drugs in microneedle drug delivery systems may be limited. Although bionic needle tips and precision 3D printing can improve the skin adhesion of microneedle patches, they are also accompanied by high equipment costs and optimal needle tip configurations that have not yet been clinically approved.
Dissolvable microneedles account for a large proportion of microneedle drug delivery. Because most of the needle tip materials are biodegradable polymers, it is necessary to uniformly disperse the drug in the microneedle or encapsulate the drug in the hollow needle tip, so the one-time administration dose is limited. Moreover, due to the characteristics of biocompatibility, dissolvable microneedles are not easy to preserve, and drugs can easily lose their activity, which greatly increases the preservation cost and limits production.
There are also issues such as the drug loading of the microneedle transdermal drug delivery devices, the stability of biological agents [176], and the unpredictable drug release rate in the skin [156], which require further investigation by researchers and pharmaceutical companies. Moreover, the time from production to final treatment is several months or so. Therefore, the microneedle needs to have stable mechanical strength, and the payload must remain safe and active. Pretreatment sterilization methods such as high temperature and ultraviolet irradiation can reduce the active ingredients of the immunotherapeutic agents. A micromechanical tester can be used to test the performance of microneedles with controllable mechanical force and compression time. Vaccines can be administered to suitable animals and then further characterized for immune responses. Overall, proper storage methods can greatly preserve the performance of microneedle-based immunotherapy.
6. Future Perspectives and Clinical Translation
Responsive microneedle-based immunotherapy combines multiple responses and multiple therapies, providing new possibilities for the precise treatment of diseases and the reduction of physical side effects from the perspective of materials and technology. This type of therapy overcomes the shortcomings of traditional drug carriers, can accurately control the drug release site, and can increase the therapeutic effect on diseases. Thus far, 143 clinical applications of microneedles have been reported: 47 on skin diseases, 15 on vaccines, 9 on diabetes, and 9 on eye diseases. There are many scientific studies being conducted on responsive microneedles, but the transfer to clinical application has been very limited. Researchers continue to explore methods of internal and external stimulation according to the needs of enhancing immunotherapy. Because single-response microneedles are sometimes insensitive to a single factor, researchers are currently focusing on the design of dual-response and multiresponse nanodrug carriers. Whether they will provide better vaccine delivery or immune system activation requires more research and exploration to determine. As further research overcomes hurdles, microneedle-based immunotherapy delivery could play an important role in the way vaccinations are delivered in the future.
Author Contributions
Writing—original draft preparation, X.L. and H.S.; writing—review and editing, T.S. and H.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- You, Y.; Tian, Y.; Yang, Z.; Shi, J.; Kwak, K.J.; Tong, Y.; Estania, A.P.; Cao, J.; Hsu, W.-H.; Liu, Y.; et al. Intradermally delivered mRNA-encapsulating extracellular vesicles for collagen-replacement therapy. Nat. Biomed. Eng. 2023. [Google Scholar] [CrossRef]
- Yang, T.; Huang, D.; Li, C.; Zhao, D.; Li, J.; Zhang, M.; Chen, Y.; Wang, Q.; Liang, Z.; Liang, X.-J.; et al. Rolling microneedle electrode array (RoMEA) empowered nucleic acid delivery and cancer immunotherapy. Nano Today 2021, 36, 101017. [Google Scholar] [CrossRef]
- Kearney, M.-C.; Caffarel-Salvador, E.; Fallows, S.J.; McCarthy, H.O.; Donnelly, R.F. Microneedle-mediated delivery of donepezil: Potential for improved treatment options in Alzheimer’s disease. Eur. J. Pharm. Biopharm. 2016, 103, 43–50. [Google Scholar] [CrossRef] [PubMed]
- McCrudden, M.T.C.; Alkilani, A.Z.; McCrudden, C.M.; McAlister, E.; McCarthy, H.O.; Woolfson, A.D.; Donnelly, R.F. Design and physicochemical characterisation of novel dissolving polymeric microneedle arrays for transdermal delivery of high dose, low molecular weight drugs. J. Control. Release 2014, 180, 71–80. [Google Scholar] [CrossRef]
- Iachina, I.; Eriksson, A.H.; Bertelsen, M.; Petersson, K.; Jansson, J.; Kemp, P.; Engell, K.M.; Brewer, J.R.; Nielsen, K.T. Dissolvable microneedles for transdermal drug delivery showing skin pentation and modified drug release. Eur. J. Pharm. Sci. 2023, 182, 106371. [Google Scholar] [CrossRef]
- Wang, R.; Zhong, T.; Bian, Q.; Zhang, S.; Ma, X.; Li, L.; Xu, Y.; Gu, Y.; Yuan, A.; Hu, W.; et al. PROTAC Degraders of Androgen Receptor-Integrated Dissolving Microneedles for Androgenetic Alopecia and Recrudescence Treatment via Single Topical Administration. Small Methods 2023, 7, e2201293. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Wang, L.; Yu, H.; Li, C.; Feng, J.; Haq, F.; Khan, A.; Khan, R.U. Preparation, properties and challenges of the microneedles-based insulin delivery system. J. Control. Release 2018, 288, 173–188. [Google Scholar] [CrossRef] [PubMed]
- Jamaledin, R.; Di Natale, C.; Onesto, V.; Taraghdari, Z.B.; Zare, E.N.; Makvandi, P.; Vecchione, R.; Netti, P.A. Progress in microneedle-mediated protein delivery. J. Clin. Med. 2020, 9, 542. [Google Scholar] [CrossRef]
- Liu, T.; Chen, M.; Fu, J.; Sun, Y.; Lu, C.; Quan, G.; Pan, X.; Wu, C. Recent advances in microneedles-mediated transdermal delivery of protein and peptide drugs. Acta Pharm. Sin. B 2021, 11, 2326–2343. [Google Scholar] [CrossRef]
- Chen, Q.; Xiao, Z.; Wang, C.; Chen, G.; Zhang, Y.; Zhang, X.; Han, X.; Wang, J.; Ye, X.; Prausnitz, M.R.; et al. Microneedle Patches Loaded with Nanovesicles for Glucose Transporter-Mediated Insulin Delivery. ACS Nano 2022, 16, 18223–18231. [Google Scholar] [CrossRef]
- Hu, S.; Zhu, D.; Li, Z.; Cheng, K. Detachable Microneedle Patches Deliver Mesenchymal Stromal Cell Factor-Loaded Nanoparticles for Cardiac Repair. ACS Nano 2022, 16, 15935–15945. [Google Scholar] [CrossRef] [PubMed]
- Bui, V.D.; Son, S.; Xavier, W.; Nguyen, V.Q.; Jung, J.M.; Lee, J.; Shin, S.; Um, W.; An, J.Y.; Kim, C.H.; et al. Dissolving microneedles for long-term storage and transdermal delivery of extracellular vesicles. Biomaterials 2022, 287, 121644. [Google Scholar] [CrossRef]
- Liu, S.; Yang, G.; Li, M.; Sun, F.; Li, Y.; Wang, X.; Gao, Y.; Yang, P. Transcutaneous immunization via dissolving microneedles protects mice from lethal influenza H7N9 virus challenge. Vaccine 2022, 40, 6767–6775. [Google Scholar] [CrossRef] [PubMed]
- Mikszta, J.A.; Alarcon, J.B.; Brittingham, J.M.; Sutter, D.E.; Pettis, R.J.; Harvey, N.G. Improved genetic immunization via micromechanical disruption of skin-barrier function and targeted epidermal delivery. Nat. Med. 2002, 8, 415–419. [Google Scholar] [CrossRef]
- Mikszta, J.A.; Sullivan, V.J.; Dean, C.; Waterston, A.M.; Alarcon, J.B.; Dekker, J.P.; Brittingham, J.M.; Huang, J.; Hwang, C.R.; Ferriter, M.; et al. Protective immunization against inhalational anthrax: A comparison of minimally invasive delivery platforms. J. Infect. Dis. 2005, 191, 278–288. [Google Scholar] [CrossRef]
- Rappuoli, R. Vaccines: Science, health, longevity, and wealth. Proc. Natl. Acad. Sci. USA 2014, 111, 12282. [Google Scholar] [CrossRef]
- Chen, Z.; Lv, Y.; Qi, J.; Zhu, Q.; Lu, Y.; Wu, W. Overcoming or circumventing the stratum corneum barrier for efficient transcutaneous immunization. Drug Discov. Today 2018, 23, 181–186. [Google Scholar] [CrossRef]
- Hammond, S.A.; Guebre-Xabier, M.; Yu, J.; Glenn, G.M. Transcutaneous immunization: An emerging route of immunization and potent immunostimulation strategy. Crit. Rev. Ther. Drug Carr. Syst. 2001, 18, 503–526. [Google Scholar] [CrossRef]
- Engelke, L.; Winter, G.; Hook, S.; Engert, J. Recent insights into cutaneous immunization: How to vaccinate via the skin. Vaccine 2015, 33, 4663–4674. [Google Scholar] [CrossRef]
- Sallam, M.A.; Prakash, S.; Kumbhojkar, N.; Shields, C.W.; Mitragotri, S. Formulation-based approaches for dermal delivery of vaccines and therapeutic nucleic acids: Recent advances and future perspectives. Bioeng. Transl. Med. 2021, 6, e10215. [Google Scholar] [CrossRef]
- Amani, H.; Shahbazi, M.A.; D’Amico, C.; Fontana, F.; Abbaszadeh, S.; Santos, H.A. Microneedles for painless transdermal immunotherapeutic applications. J. Control. Release 2021, 330, 185–217. [Google Scholar] [CrossRef]
- Mistilis, M.J.; Joyce, J.C.; Esser, E.S.; Skountzou, I.; Compans, R.W.; Bommarius, A.S.; Prausnitz, M.R. Long-term stability of influenza vaccine in a dissolving microneedle patch. Drug Deliv. Transl. Res. 2017, 7, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Joyce, J.C.; Collins, M.L.; Rota, P.A.; Prausnitz, M.R. Thermostability of Measles and Rubella Vaccines in a Microneedle Patch. Adv. Ther. 2021, 4, 2100095. [Google Scholar] [CrossRef]
- Arya, J.M.; Dewitt, K.; Scott-Garrard, M.; Chiang, Y.W.; Prausnitz, M.R. Rabies vaccination in dogs using a dissolving microneedle patch. J. Control. Release 2016, 239, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Mansoor, I.; Eassa, H.A.; Mohammed, K.H.A.; Abd El-Fattah, M.A.; Abdo, M.H.; Rashad, E.; Eassa, H.A.; Saleh, A.; Amin, O.M.; Nounou, M.I.; et al. Microneedle-Based Vaccine Delivery: Review of an Emerging Technology. AAPS PharmSciTech 2022, 23, 103. [Google Scholar] [CrossRef]
- Ma, G.; Wu, C. Microneedle, bio-microneedle and bio-inspired microneedle: A review. J. Control. Release 2017, 251, 11–23. [Google Scholar] [CrossRef]
- Yu, J.; Kuwentrai, C.; Gong, H.R.; Li, R.; Zhang, B.Z.; Lin, X.; Wang, X.; Huang, J.D.; Xu, C. Intradermal delivery of mRNA using cryomicroneedles. Acta Biomater. 2022, 148, 133–141. [Google Scholar] [CrossRef]
- Hirobe, S.; Azukizawa, H.; Hanafusa, T.; Matsuo, K.; Quan, Y.-S.; Kamiyama, F.; Katayama, I.; Okada, N.; Nakagawa, S. Clinical study and stability assessment of a novel transcutaneous influenza vaccination using a dissolving microneedle patch. Biomaterials 2015, 57, 50–58. [Google Scholar] [CrossRef]
- Rouphael, N.G.; Paine, M.; Mosley, R.; Henry, S.; McAllister, D.V.; Kalluri, H.; Pewin, W.; Frew, P.M.; Yu, T.; Thornburg, N.J.; et al. The safety, immunogenicity, and acceptability of inactivated influenza vaccine delivered by microneedle patch (TIV-MNP 2015): A randomised, partly blinded, placebo-controlled, phase 1 trial. Lancet 2017, 390, 649–658. [Google Scholar] [CrossRef] [PubMed]
- Ono, A.; Ito, S.; Sakagami, S.; Asada, H.; Saito, M.; Quan, Y.-S.; Kamiyama, F.; Hirobe, S.; Okada, N. Development of Novel Faster-Dissolving Microneedle Patches for Transcutaneous Vaccine Delivery. Pharmaceutics 2017, 9, 27. [Google Scholar] [CrossRef]
- Robertson, C.A.; Tsang, P.; Landolfi, V.A.; Greenberg, D.P. Fluzone(R) Intradermal Quadrivalent Influenza Vaccine. Expert Rev. Vaccines 2016, 15, 1245–1253. [Google Scholar] [CrossRef]
- Ita, K. Ceramic microneedles and hollow microneedles for transdermal drug delivery: Two decades of research. J. Drug Deliv. Sci. Technol. 2018, 44, 314–322. [Google Scholar] [CrossRef]
- Liu, Y.; Ye, L.; Lin, F.; Gomaa, Y.; Flyer, D.; Carrion, R., Jr.; Patterson, J.L.; Prausnitz, M.R.; Smith, G.; Glenn, G.; et al. Intradermal Vaccination With Adjuvanted Ebola Virus Soluble Glycoprotein Subunit Vaccine by Microneedle Patches Protects Mice Against Lethal Ebola Virus Challenge. J. Infect. Dis. 2018, 218 (Suppl. S5), S545–S552. [Google Scholar] [CrossRef] [PubMed]
- Ray, S.; Wirth, D.M.; Ortega-Rivera, O.A.; Steinmetz, N.F.; Pokorski, J.K. Dissolving Microneedle Delivery of a Prophylactic HPV Vaccine. Biomacromolecules 2022, 23, 903–912. [Google Scholar] [CrossRef]
- Frew, P.M.; Paine, M.B.; Rouphael, N.; Schamel, J.; Chung, Y.; Mulligan, M.J.; Prausnitz, M.R. Acceptability of an inactivated influenza vaccine delivered by microneedle patch: Results from a phase I clinical trial of safety, reactogenicity, and immunogenicity. Vaccine 2020, 38, 7175–7181. [Google Scholar] [CrossRef] [PubMed]
- Banchereau, J.; Steinman, R.M. Dendritic cells and the control of immunity. Nature 1998, 392, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.-L.; Zhan, Y.; Villadangos, J.A.; Lew, A.M. The cell biology of cross-presentation and the role of dendritic cell subsets. Immunol. Cell Biol. 2008, 86, 353–362. [Google Scholar] [CrossRef]
- Qin, M.; Du, G.; Sun, X. Recent Advances in the Noninvasive Delivery of mRNA. Acc. Chem. Res. 2021, 54, 4262–4271. [Google Scholar] [CrossRef]
- Zhu, H.; Mah Jian Qiang, J.; Wang, C.G.; Chan, C.Y.; Zhu, Q.; Ye, E.; Li, Z.; Loh, X.J. Flexible polymeric patch based nanotherapeutics against non-cancer therapy. Bioact. Mater. 2022, 18, 471–491. [Google Scholar] [CrossRef]
- Xu, G.; Mao, Y.; Jiang, T.; Gao, B.; He, B. Structural design strategies of microneedle-based vaccines for transdermal immunity augmentation. J. Control. Release 2022, 351, 907–922. [Google Scholar] [CrossRef]
- Ramirez-Garcia, P.D.; Retamal, J.S.; Shenoy, P.; Imlach, W.; Sykes, M.; Truong, N.; Constandil, L.; Pelissier, T.; Nowell, C.J.; Khor, S.Y.; et al. A pH-responsive nanoparticle targets the neurokinin 1 receptor in endosomes to prevent chronic pain. Nat. Nanotechnol. 2019, 14, 1150–1159. [Google Scholar] [CrossRef] [PubMed]
- Duong, H.T.T.; Yin, Y.; Thambi, T.; Nguyen, T.L.; Giang Phan, V.H.; Lee, M.S.; Lee, J.E.; Kim, J.; Jeong, J.H.; Lee, D.S. Smart vaccine delivery based on microneedle arrays decorated with ultra-pH-responsive copolymers for cancer immunotherapy. Biomaterials 2018, 185, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Lamkanfi, M.; Dixit, V.M. Mechanisms and functions of inflammasomes. Cell 2014, 157, 1013–1022. [Google Scholar] [CrossRef]
- Jager, E.; Murthy, S.; Schmidt, C.; Hahn, M.; Strobel, S.; Peters, A.; Staubert, C.; Sungur, P.; Venus, T.; Geisler, M.; et al. Calcium-sensing receptor-mediated NLRP3 inflammasome response to calciprotein particles drives inflammation in rheumatoid arthritis. Nat. Commun. 2020, 11, 4243. [Google Scholar] [CrossRef]
- Cui, W.; Chen, S.; Chi, Z.; Guo, X.; Zhang, X.; Zhong, Y.; Han, H.; Yao, K. Screening-based identification of xanthone as a novel NLRP3 inflammasome inhibitor via metabolic reprogramming. Clin. Transl. Med. 2021, 11, e496. [Google Scholar] [CrossRef]
- Permana, A.D.; Anjani, Q.K.; Sartini; Utomo, E.; Volpe-Zanutto, F.; Paredes, A.J.; Evary, Y.M.; Mardikasari, S.A.; Pratama, M.R.; Tuany, I.N.; et al. Selective delivery of silver nanoparticles for improved treatment of biofilm skin infection using bacteria-responsive microparticles loaded into dissolving microneedles. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 120, 111786. [Google Scholar] [CrossRef]
- Chi, J.; Zhang, X.; Chen, C.; Shao, C.; Zhao, Y.; Wang, Y. Antibacterial and angiogenic chitosan microneedle array patch for promoting wound healing. Bioact. Mater. 2020, 5, 253–259. [Google Scholar] [CrossRef]
- Rainu, S.; Parameswaran, S.; Krishnakumar, S.; Singh, N. Dual-sensitive fluorescent nanoprobes for detection of matrix metalloproteinases and low pH in a 3D tumor microenvironment. J. Mater. Chem. B 2022, 10, 5388–5401. [Google Scholar] [CrossRef]
- Dai, L.; Li, X.; Zheng, X.; Fu, Z.; Yao, M.; Meng, S.; Zhang, J.; Han, B.; Gao, Q.; Chang, J.; et al. TGF-beta blockade-improved chemo-immunotherapy with pH/ROS cascade-responsive micelle via tumor microenvironment remodeling. Biomaterials 2021, 276, 121010. [Google Scholar] [CrossRef]
- Mathesh, M.; Sun, J.; van der Sandt, F.; Wilson, D.A. Supramolecular nanomotors with “pH taxis” for active drug delivery in the tumor microenvironment. Nanoscale 2020, 12, 22495–22501. [Google Scholar] [CrossRef] [PubMed]
- Kuchuk, O.; Tuccitto, A.; Citterio, D.; Huber, V.; Camisaschi, C.; Milione, M.; Vergani, B.; Villa, A.; Alison, M.R.; Carradori, S.; et al. pH regulators to target the tumor immune microenvironment in human hepatocellular carcinoma. Oncoimmunology 2018, 7, e1445452. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Luo, Z.; Zhang, J.; Luo, T.; Zhou, J.; Zhao, X.; Cai, K. Hollow mesoporous silica nanoparticles facilitated drug delivery via cascade pH stimuli in tumor microenvironment for tumor therapy. Biomaterials 2016, 83, 51–65. [Google Scholar] [CrossRef]
- Lala, A.; Johnson, K.W.; Januzzi, J.L.; Russak, A.J.; Paranjpe, I.; Richter, F.; Zhao, S.; Somani, S.; Van Vleck, T.; Vaid, A.; et al. Prevalence and Impact of Myocardial Injury in Patients Hospitalized With COVID-19 Infection. J. Am. Coll. Cardiol. 2020, 76, 533–546. [Google Scholar] [CrossRef]
- Ke, C.-J.; Lin, Y.-J.; Hu, Y.-C.; Chiang, W.-L.; Chen, K.-J.; Yang, W.-C.; Liu, H.-L.; Fu, C.-C.; Sung, H.-W. Multidrug release based on microneedle arrays filled with pH-responsive PLGA hollow microspheres. Biomaterials 2012, 33, 5156–5165. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Ye, Y.; Hochu, G.M.; Sadeghifar, H.; Gu, Z. Enhanced Cancer Immunotherapy by Microneedle Patch-Assisted Delivery of Anti-PD1 Antibody. Nano Lett. 2016, 16, 2334–2340. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Liu, H.; Shi, Z.; Lin, L.; Li, Y.; Wang, M.; Pan, G.; Lei, Y.; Xue, L. Responsive hydrogel-based microneedle dressing for diabetic wound healing. J. Mater. Chem. B 2022, 10, 3501–3511. [Google Scholar] [CrossRef]
- Yang, Y.; Zhou, R.; Wang, Y.; Zhang, Y.; Yu, J.; Gu, Z. Recent Advances in Oral and Transdermal Protein Delivery Systems. Angew. Chem. Int. Ed. Engl. 2022, 62, e202214795. [Google Scholar] [CrossRef]
- Hirama, H.; Ishikura, Y.; Kano, S.; Hayase, M.; Mekaru, H. Monodispersed sodium hyaluronate microcapsules for transdermal drug delivery systems. Mater. Adv. 2021, 2, 7007–7016. [Google Scholar] [CrossRef]
- Rawlings, J.S.; Rosler, K.M.; Harrison, D.A. The JAK/STAT signaling pathway. J. Cell Sci. 2004, 117 Pt 8, 1281–1283. [Google Scholar] [CrossRef]
- Ou, B.S.; Saouaf, O.M.; Baillet, J.; Appel, E.A. Sustained delivery approaches to improving adaptive immune responses. Adv. Drug Deliv. Rev. 2022, 187, 114401. [Google Scholar] [CrossRef]
- Kim, J.; Park, S.; Nam, G.; Choi, Y.; Woo, S.; Yoon, S.H. Bioinspired microneedle insertion for deep and precise skin penetration with low force: Why the application of mechanophysical stimuli should be considered. J. Mech. Behav. Biomed. Mater. 2018, 78, 480–490. [Google Scholar] [CrossRef] [PubMed]
- Chu, S.; Shi, X.; Tian, Y.; Gao, F. pH-Responsive Polymer Nanomaterials for Tumor Therapy. Front. Oncol. 2022, 12, 855019. [Google Scholar] [CrossRef]
- Li, X.; Zhao, Z.; Zhang, M.; Ling, G.; Zhang, P. Research progress of microneedles in the treatment of melanoma. J. Control. Release 2022, 348, 631–647. [Google Scholar] [CrossRef] [PubMed]
- Mu, M.; Liang, X.; Chuan, D.; Zhao, S.; Yu, W.; Fan, R.; Tong, A.; Zhao, N.; Han, B.; Guo, G. Chitosan coated pH-responsive metal-polyphenol delivery platform for melanoma chemotherapy. Carbohydr. Polym. 2021, 264, 118000. [Google Scholar] [CrossRef]
- Wei, S.; Quan, G.; Lu, C.; Pan, X.; Wu, C. Dissolving microneedles integrated with pH-responsive micelles containing AIEgen with ultra-photostability for enhancing melanoma photothermal therapy. Biomater. Sci. 2020, 8, 5739–5750. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Xu, Q.; Zhang, P.; Zhao, X.; Wang, Y. Cutaneous microenvironment responsive microneedle patch for rapid gene release to treat subdermal tumor. J. Control. Release 2019, 314, 72–80. [Google Scholar] [CrossRef]
- Ullah, A.; Jang, M.; Khan, H.; Choi, H.J.; An, S.; Kim, D.; Kim, Y.-R.; Kim, U.-K.; Kim, G.M. Microneedle array with a pH-responsive polymer coating and its application in smart drug delivery for wound healing. Sens. Actuators B Chem. 2021, 345, 130441. [Google Scholar] [CrossRef]
- Perillo, B.; Di Donato, M.; Pezone, A.; Di Zazzo, E.; Giovannelli, P.; Galasso, G.; Castoria, G.; Migliaccio, A. ROS in cancer therapy: The bright side of the moon. Exp. Mol. Med. 2020, 52, 192–203. [Google Scholar] [CrossRef]
- Chio, I.I.C.; Tuveson, D.A. ROS in Cancer: The Burning Question. Trends Mol. Med. 2017, 23, 411–429. [Google Scholar] [CrossRef]
- Balzano-Nogueira, L.; Ramirez, R.; Zamkovaya, T.; Dailey, J.; Ardissone, A.N.; Chamala, S.; Serrano-Quilez, J.; Rubio, T.; Haller, M.J.; Concannon, P.; et al. Integrative analyses of TEDDY Omics data reveal lipid metabolism abnormalities, increased intracellular ROS and heightened inflammation prior to autoimmunity for type 1 diabetes. Genome Biol. 2021, 22, 39. [Google Scholar] [CrossRef]
- De Maranon, A.M.; Iannantuoni, F.; Abad-Jimenez, Z.; Canet, F.; Diaz-Pozo, P.; Lopez-Domenech, S.; Jover, A.; Morillas, C.; Marino, G.; Apostolova, N.; et al. Relationship between PMN-endothelium interactions, ROS production and Beclin-1 in type 2 diabetes. Redox Biol. 2020, 34, 101563. [Google Scholar] [CrossRef]
- Idelchik, M.; Begley, U.; Begley, T.J.; Melendez, J.A. Mitochondrial ROS control of cancer. Semin. Cancer Biol. 2017, 47, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, W.; Ijaz, B.; Shabbiri, K.; Ahmed, F.; Rehman, S. Oxidative toxicity in diabetes and Alzheimer’s disease: Mechanisms behind ROS/RNS generation. J. Biomed. Sci. 2017, 24, 76. [Google Scholar] [CrossRef]
- Lv, J.; Yang, Z.; Wang, C.; Duan, J.; Ren, L.; Rong, G.; Feng, Q.; Li, Y.; Cheng, Y. Efficient intracellular and in vivo delivery of toxin proteins by a ROS-responsive polymer for cancer therapy. J. Control. Release 2023, 355, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, W.; Zhu, J.; Zhai, Z.; Xie, J.; Zhou, J.; Feng, X.; Feng, B.; Pan, Q.; Li, S.; Venkatesan, R.; et al. ROS-responsive polymer nanoparticles with enhanced loading of dexamethasone effectively modulate the lung injury microenvironment. Acta Biomater. 2022, 148, 258–270. [Google Scholar] [CrossRef]
- Zheng, M.; Liu, Y.; Wang, Y.; Zhang, D.; Zou, Y.; Ruan, W.; Yin, J.; Tao, W.; Park, J.B.; Shi, B. ROS-Responsive Polymeric siRNA Nanomedicine Stabilized by Triple Interactions for the Robust Glioblastoma Combinational RNAi Therapy. Adv. Mater. 2019, 31, e1903277. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, Y.; Ru, Z.; Song, W.; Chen, L.; Ma, H.; Sun, L. A ROS-responsive polymeric prodrug nanosystem with self-amplified drug release for PSMA (-) prostate cancer specific therapy. J. Nanobiotechnol. 2019, 17, 91. [Google Scholar] [CrossRef]
- Mohammed, F.; Ke, W.; Mukerabigwi, J.F.; AAM, M.J.; Ibrahim, A.; Wang, Y.; Zha, Z.; Lu, N.; Zhou, M.; Ge, Z. ROS-Responsive Polymeric Nanocarriers with Photoinduced Exposure of Cell-Penetrating Moieties for Specific Intracellular Drug Delivery. ACS Appl. Mater. Interfaces 2019, 11, 31681–31692. [Google Scholar] [CrossRef]
- Cao, Z.; Li, D.; Wang, J.; Yang, X. Reactive oxygen species-sensitive polymeric nanocarriers for synergistic cancer therapy. Acta Biomater. 2021, 130, 17–31. [Google Scholar] [CrossRef]
- Ye, H.; Zhou, Y.; Liu, X.; Chen, Y.; Duan, S.; Zhu, R.; Liu, Y.; Yin, L. Recent Advances on Reactive Oxygen Species-Responsive Delivery and Diagnosis System. Biomacromolecules 2019, 20, 2441–2463. [Google Scholar] [CrossRef]
- Zhang, Y.; Feng, P.; Yu, J.; Yang, J.; Zhao, J.; Wang, J.; Shen, Q.; Gu, Z. ROS-Responsive Microneedle Patch for Acne Vulgaris Treatment. Adv. Ther. 2018, 1, 1800035. [Google Scholar] [CrossRef]
- Liu, Y.; Zhao, H.; Gao, N.; Yang, C.; Zhang, R.; Zhang, X. An efficient FRET based theranostic nanoprobe for hyaluronidase detection and cancer therapy in vitro. Sens. Actuators B Chem. 2021, 344, 130201. [Google Scholar] [CrossRef]
- Fatima, K.; Masood, N.; Ahmad Wani, Z.; Meena, A.; Luqman, S. Neomenthol prevents the proliferation of skin cancer cells by restraining tubulin polymerization and hyaluronidase activity. J. Adv. Res 2021, 34, 93–107. [Google Scholar] [CrossRef]
- Guan, X.; Chen, J.; Hu, Y.; Lin, L.; Sun, P.; Tian, H.; Chen, X. Highly enhanced cancer immunotherapy by combining nanovaccine with hyaluronidase. Biomaterials 2018, 171, 198–206. [Google Scholar] [CrossRef]
- Stern, R. Hyaluronidases in cancer biology. Semin. Cancer Biol. 2008, 18, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Xia, R.; Huang, Y.; Zhao, W.; Li, J.; Zhang, X.; Wang, P.; Venkataramanan, R.; Fan, J.; Xie, W.; et al. An immunostimulatory dual-functional nanocarrier that improves cancer immunochemotherapy. Nat. Commun. 2016, 7, 13443. [Google Scholar] [CrossRef] [PubMed]
- Nayak-Kapoor, A.; Hao, Z.; Sadek, R.; Dobbins, R.; Marshall, L.; Vahanian, N.N.; Jay Ramsey, W.; Kennedy, E.; Mautino, M.R.; Link, C.J.; et al. Phase Ia study of the indoleamine 2,3-dioxygenase 1 (IDO1) inhibitor navoximod (GDC-0919) in patients with recurrent advanced solid tumors. J. Immunother. Cancer 2018, 6, 61. [Google Scholar] [CrossRef]
- Ye, Y.; Wang, J.; Hu, Q.; Hochu, G.M.; Xin, H.; Wang, C.; Gu, Z. Synergistic Transcutaneous Immunotherapy Enhances Antitumor Immune Responses through Delivery of Checkpoint Inhibitors. ACS Nano 2016, 10, 8956–8963. [Google Scholar] [CrossRef]
- Power, G.; Moore, Z.; O’Connor, T. Measurement of pH, exudate composition and temperature in wound healing: A systematic review. J. Wound Care 2017, 26, 381–397. [Google Scholar] [CrossRef]
- Villalba-Rodríguez, A.M.; Martínez-González, S.; Sosa-Hernández, J.E.; Parra-Saldívar, R.; Bilal, M.; Iqbal, H.M.N. Nanoclay/Polymer-Based Hydrogels and Enzyme-Loaded Nanostructures for Wound Healing Applications. Gels 2021, 7, 59. [Google Scholar] [CrossRef]
- Lei, X.; Li, M.; Wang, C.; Cui, P.; Qiu, L.; Zhou, S.; Jiang, P.; Li, H.; Zhao, D.; Ni, X.; et al. Degradable microneedle patches loaded with antibacterial gelatin nanoparticles to treat staphylococcal infection-induced chronic wounds. Int. J. Biol. Macromol. 2022, 217, 55–65. [Google Scholar] [CrossRef]
- Donnelly, R.F.; Singh, T.R.R.; Garland, M.J.; Migalska, K.; Majithiya, R.; McCrudden, C.M.; Kole, P.L.; Mahmood, T.M.T.; McCarthy, H.O.; Woolfson, A.D. Hydrogel-Forming Microneedle Arrays for Enhanced Transdermal Drug Delivery. Adv. Funct. Mater. 2012, 22, 4879–4890. [Google Scholar] [CrossRef]
- Kim, M.; Jung, B.; Park, J.-H. Hydrogel swelling as a trigger to release biodegradable polymer microneedles in skin. Biomaterials 2012, 33, 668–678. [Google Scholar] [CrossRef]
- Thakur, R.R.S.; Fallows, S.J.; McMillan, H.L.; Donnelly, R.F.; Jones, D.S. Microneedle-mediated intrascleral delivery of in situ forming thermoresponsive implants for sustained ocular drug delivery. J. Pharm. Pharmacol. 2014, 66, 584–595. [Google Scholar] [CrossRef]
- Dini, V.; Salvo, P.; Janowska, A.; Di Francesco, F.; Barbini, A.; Romanelli, M. Correlation Between Wound Temperature Obtained With an Infrared Camera and Clinical Wound Bed Score in Venous Leg Ulcers. Wounds 2015, 27, 274–278. [Google Scholar]
- Roh, H.; Yoon, Y.J.; Park, J.S.; Kang, D.-H.; Kwak, S.M.; Lee, B.C.; Im, M. Fabrication of High-Density Out-of-Plane Microneedle Arrays with Various Heights and Diverse Cross-Sectional Shapes. Nano-Micro Lett. 2021, 14, 24. [Google Scholar] [CrossRef]
- Seong, K.-Y.; Seo, M.-S.; Hwang, D.Y.; O’Cearbhaill, E.D.; Sreenan, S.; Karp, J.M.; Yang, S.Y. A self-adherent, bullet-shaped microneedle patch for controlled transdermal delivery of insulin. J. Control. Release 2017, 265, 48–56. [Google Scholar] [CrossRef]
- Li, W.; Terry, R.N.; Tang, J.; Feng, M.R.; Schwendeman, S.P.; Prausnitz, M.R. Rapidly separable microneedle patch for the sustained release of a contraceptive. Nat. Biomed. Eng. 2019, 3, 220–229. [Google Scholar] [CrossRef]
- Yin, Y.; Su, W.; Zhang, J.; Huang, W.; Li, X.; Ma, H.; Tan, M.; Song, H.; Cao, G.; Yu, S.; et al. Separable Microneedle Patch to Protect and Deliver DNA Nanovaccines Against COVID-19. ACS Nano 2021, 15, 14347–14359. [Google Scholar] [CrossRef]
- Li, J.Y.; Feng, Y.H.; He, Y.T.; Hu, L.F.; Liang, L.; Zhao, Z.Q.; Chen, B.Z.; Guo, X.D. Thermosensitive hydrogel microneedles for controlled transdermal drug delivery. Acta Biomater. 2022, 153, 308–319. [Google Scholar] [CrossRef]
- Cui, M.; Zheng, M.; Wiraja, C.; Chew SW, T.; Mishra, A.; Mayandi, V.; Lakshminarayanan, R.; Xu, C. Ocular delivery of predatory bacteria with cryomicroneedles against eye infection. Adv. Sci. 2021, 8, 2102327. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, J.; Yu, J.; Wen, D.; Kahkoska, A.R.; Lu, Y.; Zhang, X.; Buse, J.B.; Gu, Z. Bioresponsive Microneedles with a Sheath Structure for H(2) O(2) and pH Cascade-Triggered Insulin Delivery. Small 2018, 14, e1704181. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Lu, C.; Qin, W.; Chen, M.; Quan, G.; Liu, H.; Wang, L.; Bai, X.; Pan, X.; Wu, C. Construction of a core-shell microneedle system to achieve targeted co-delivery of checkpoint inhibitors for melanoma immunotherapy. Acta Biomater. 2020, 104, 147–157. [Google Scholar] [CrossRef] [PubMed]
- GhavamiNejad, A.; Li, J.; Lu, B.; Zhou, L.; Lam, L.; Giacca, A.; Wu, X.Y. Glucose-Responsive Composite Microneedle Patch for Hypoglycemia-Triggered Delivery of Native Glucagon. Adv. Mater. 2019, 31, e1901051. [Google Scholar] [CrossRef] [PubMed]
- Hao, Y.; Chen, Y.; He, X.; Yang, F.; Han, R.; Yang, C.; Li, W.; Qian, Z. Near-infrared responsive 5-fluorouracil and indocyanine green loaded MPEG-PCL nanoparticle integrated with dissolvable microneedle for skin cancer therapy. Bioact. Mater. 2020, 5, 542–552. [Google Scholar] [CrossRef]
- Chen, M.C.; Ling, M.H.; Wang, K.W.; Lin, Z.W.; Lai, B.H.; Chen, D.H. Near-infrared light-responsive composite microneedles for on-demand transdermal drug delivery. Biomacromolecules 2015, 16, 1598–1607. [Google Scholar] [CrossRef]
- Fan, J.; Zhang, Z.; Wang, Y.; Lin, S.; Yang, S. Photo-responsive degradable hollow mesoporous organosilica nanoplatforms for drug delivery. J. Nanobiotechnol. 2020, 18, 91. [Google Scholar] [CrossRef]
- Sun, L.; Li, Z.; Su, R.; Wang, Y.; Li, Z.; Du, B.; Sun, Y.; Guan, P.; Besenbacher, F.; Yu, M. Phase-Transition Induced Conversion into a Photothermal Material: Quasi-Metallic WO(2.9) Nanorods for Solar Water Evaporation and Anticancer Photothermal Therapy. Angew. Chem. Int. Ed. Engl. 2018, 57, 10666–10671. [Google Scholar] [CrossRef]
- Liang, R.; Tian, R.; Ma, L.; Zhang, L.; Hu, Y.; Wang, J.; Wei, M.; Yan, D.; Evans, D.G.; Duan, X. A Supermolecular Photosensitizer with Excellent Anticancer Performance in Photodynamic Therapy. Adv. Funct. Mater. 2014, 24, 3144–3151. [Google Scholar] [CrossRef]
- Zha, Z.; Yue, X.; Ren, Q.; Dai, Z. Uniform polypyrrole nanoparticles with high photothermal conversion efficiency for photothermal ablation of cancer cells. Adv. Mater. 2013, 25, 777–782. [Google Scholar] [CrossRef]
- Alamdari, S.G.; Amini, M.; Jalilzadeh, N.; Baradaran, B.; Mohammadzadeh, R.; Mokhtarzadeh, A.; Oroojalian, F. Recent advances in nanoparticle-based photothermal therapy for breast cancer. J. Control. Release 2022, 349, 269–303. [Google Scholar] [CrossRef]
- Wu, F.; Zhang, Q.; Sun, B.; Chu, X.; Zhang, M.; She, Z.; Li, Z.; Zhou, N.; Wang, J.; Li, A. MoO(3-x) nanosheets-based platform for single NIR laser induced efficient PDT/PTT of cancer. J. Control. Release 2021, 338, 46–55. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, J.; Chen, Z.; Zhang, F.; Wang, Q.; Guo, W.; Wang, K.; Lin, H.; Qu, F. Construct of MoSe(2)/Bi(2)Se(3) nanoheterostructure: Multimodal CT/PT imaging-guided PTT/PDT/chemotherapy for cancer treating. Biomaterials 2019, 217, 119282. [Google Scholar] [CrossRef]
- Hao, Y.; Dong, M.; Zhang, T.; Peng, J.; Jia, Y.; Cao, Y.; Qian, Z. Novel Approach of Using Near-Infrared Responsive PEGylated Gold Nanorod Coated Poly(l-lactide) Microneedles to Enhance the Antitumor Efficiency of Docetaxel-Loaded MPEG-PDLLA Micelles for Treating an A431 Tumor. ACS Appl. Mater. Interfaces 2017, 9, 15317–15327. [Google Scholar] [CrossRef]
- Di, J.; Yao, S.; Ye, Y.; Cui, Z.; Yu, J.; Ghosh, T.K.; Zhu, Y.; Gu, Z. Stretch-Triggered Drug Delivery from Wearable Elastomer Films Containing Therapeutic Depots. ACS Nano 2015, 9, 9407–9415. [Google Scholar] [CrossRef]
- Jun, H.; Ahn, M.-H.; Choi, I.-J.; Baek, S.-K.; Park, J.-H.; Choi, S.-O. Immediate separation of microneedle tips from base array during skin insertion for instantaneous drug delivery. RSC Adv. 2018, 8, 17786–17796. [Google Scholar] [CrossRef]
- Choi, I.J.; Kang, A.; Ahn, M.H.; Jun, H.; Baek, S.K.; Park, J.H.; Na, W.; Choi, S.O. Insertion-responsive microneedles for rapid intradermal delivery of canine influenza vaccine. J. Control. Release 2018, 286, 460–466. [Google Scholar] [CrossRef]
- Fan, L.; Zhang, X.; Nie, M.; Xu, Y.; Wang, Y.; Shang, L.; Zhao, Y.; Zhao, Y. Photothermal Responsive Microspheres-Triggered Separable Microneedles for Versatile Drug Delivery. Adv. Funct. Mater. 2021, 32, 2110746. [Google Scholar] [CrossRef]
- Semple, S.C.; Akinc, A.; Chen, J.; Sandhu, A.P.; Mui, B.L.; Cho, C.K.; Sah, D.W.Y.; Stebbing, D.; Crosley, E.J.; Yaworski, E.; et al. Rational design of cationic lipids for siRNA delivery. Nat. Biotechnol. 2010, 28, 172–176. [Google Scholar] [CrossRef]
- Huang, H.; Hu, D.; Chen, Z.; Xu, J.; Xu, R.; Gong, Y.; Fang, Z.; Wang, T.; Chen, W. Immunotherapy for type 1 diabetes mellitus by adjuvant-free Schistosoma japonicum-egg tip-loaded asymmetric microneedle patch (STAMP). J. Nanobiotechnol. 2022, 20, 377. [Google Scholar] [CrossRef]
- Zheng, Y.; Ye, R.; Gong, X.; Yang, J.; Liu, B.; Xu, Y.; Nie, G.; Xie, X.; Jiang, L. Iontophoresis-driven microneedle patch for the active transdermal delivery of vaccine macromolecules. Microsyst. Nanoeng. 2023, 9, 35. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Niu, B.; Zhao, Y.; Fu, J.; Wen, T.; Liao, K.; Quan, G.; Pan, X.; Wu, C. Multifunctional nanoreactors-integrated microneedles for cascade reaction-enhanced cancer therapy. J. Control. Release 2021, 339, 335–349. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Cao, Y.; Lin, S.; Niu, H.; Zhang, H.; Guan, L.; Shu, C.; Wu, A.; Bian, Y.; Zhu, Y. A responsive microneedle system for efficient anti-melanoma by combining self-enhanced chemodynamic therapy with photothermal therapy. Chem. Eng. J. 2022, 431, 133466. [Google Scholar] [CrossRef]
- Zhang, X.; Chen, G.; Liu, Y.; Sun, L.; Sun, L.; Zhao, Y. Black Phosphorus-Loaded Separable Microneedles as Responsive Oxygen Delivery Carriers for Wound Healing. ACS Nano 2020, 14, 5901–5908. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chai, D.; Gao, M.; Xu, B.; Jiang, G. Thermal ablation of separable microneedles for transdermal delivery of metformin on diabetic rats. Int. J. Polym. Mater. Polym. Biomater. 2018, 68, 850–858. [Google Scholar] [CrossRef]
- Hardy, J.G.; Larraneta, E.; Donnelly, R.F.; McGoldrick, N.; Migalska, K.; McCrudden, M.T.; Irwin, N.J.; Donnelly, L.; McCoy, C.P. Hydrogel-Forming Microneedle Arrays Made from Light-Responsive Materials for On-Demand Transdermal Drug Delivery. Mol. Pharm. 2016, 13, 907–914. [Google Scholar] [CrossRef]
- Zhang, X.; Chen, G.; Fu, X.; Wang, Y.; Zhao, Y. Magneto-Responsive Microneedle Robots for Intestinal Macromolecule Delivery. Adv. Mater. 2021, 33, e2104932. [Google Scholar] [CrossRef]
- Yu, J.; Zhang, Y.; Ye, Y.; DiSanto, R.; Sun, W.; Ranson, D.; Ligler, F.S.; Buse, J.B.; Gu, Z. Microneedle-array patches loaded with hypoxia-sensitive vesicles provide fast glucose-responsive insulin delivery. Proc. Natl. Acad. Sci. USA 2015, 112, 8260–8265. [Google Scholar] [CrossRef]
- Makvandi, P.; Jamaledin, R.; Chen, G.; Baghbantaraghdari, Z.; Zare, E.N.; Di Natale, C.; Onesto, V.; Vecchione, R.; Lee, J.; Tay, F.R.; et al. Stimuli-responsive transdermal microneedle patches. Mater. Today 2021, 47, 206–222. [Google Scholar] [CrossRef]
- Jin, Z.; Zhao, B.; Wan, W.; Li, Y.; Bai, X.; Hu, C.; Wang, J.; Li, Y.; Xin, W.; Kang, L.; et al. Application of microneedle-based vaccines in biosecurity. J. Biosaf. Biosecur. 2022, 4, 75–83. [Google Scholar] [CrossRef]
- Long, L.; Liu, W.; Hu, C.; Yang, L.; Wang, Y. Construction of multifunctional wound dressings with their application in chronic wound treatment. Biomater. Sci. 2022, 10, 4058–4076. [Google Scholar] [CrossRef]
- Higano, C.S.; Small, E.J.; Schellhammer, P.; Yasothan, U.; Gubernick, S.; Kirkpatrick, P.; Kantoff, P.W. Sipuleucel-T. Nat. Rev. Drug Discov. 2010, 9, 513–514. [Google Scholar] [CrossRef]
- Kon, M.; Kiffin, R.; Koga, H.; Chapochnick, J.; Macian, F.; Varticovski, L.; Cuervo, A.M. Chaperone-mediated autophagy is required for tumor growth. Sci. Transl. Med. 2011, 3, 109ra117. [Google Scholar] [CrossRef]
- Tombal, B. Continuous improvement versus innovation: The case for sipuleucel-T. Eur. Urol. 2012, 61, 648–649; discussion 650–641. [Google Scholar] [CrossRef]
- Su, W.; Tan, M.; Wang, Z.; Zhang, J.; Huang, W.; Song, H.; Wang, X.; Ran, H.; Gao, Y.; Nie, G.; et al. Targeted Degradation of PD-L1 and Activation of the STING Pathway by Carbon-Dot-Based PROTACs for Cancer Immunotherapy. Angew. Chem. Int. Ed. Engl. 2023, 62, e202218128. [Google Scholar] [CrossRef]
- Han, X.; Cheng, K.; Xu, Y.; Wang, Y.; Min, H.; Zhang, Y.; Zhao, X.; Zhao, R.; Anderson, G.J.; Ren, L.; et al. Modularly Designed Peptide Nanoprodrug Augments Antitumor Immunity of PD-L1 Checkpoint Blockade by Targeting Indoleamine 2,3-Dioxygenase. J. Am. Chem. Soc. 2020, 142, 2490–2496. [Google Scholar] [CrossRef]
- Moral, J.A.; Leung, J.; Rojas, L.A.; Ruan, J.; Zhao, J.; Sethna, Z.; Ramnarain, A.; Gasmi, B.; Gururajan, M.; Redmond, D.; et al. ILC2s amplify PD-1 blockade by activating tissue-specific cancer immunity. Nature 2020, 579, 130–135. [Google Scholar] [CrossRef]
- Lee, J.; Le, Q.V.; Yang, G.; Oh, Y.K. Cas9-edited immune checkpoint blockade PD-1 DNA polyaptamer hydrogel for cancer immunotherapy. Biomaterials 2019, 218, 119359. [Google Scholar] [CrossRef]
- Gao, M.; Lin, M.; Moffitt, R.A.; Salazar, M.A.; Park, J.; Vacirca, J.; Huang, C.; Shroyer, K.R.; Choi, M.; Georgakis, G.V.; et al. Direct therapeutic targeting of immune checkpoint PD-1 in pancreatic cancer. Br. J. Cancer 2019, 120, 88–96. [Google Scholar] [CrossRef]
- Ye, Y.; Yu, J.; Wen, D.; Kahkoska, A.R.; Gu, Z. Polymeric microneedles for transdermal protein delivery. Adv. Drug Deliv. Rev. 2018, 127, 106–118. [Google Scholar] [CrossRef]
- Raphael, A.P.; Prow, T.W.; Crichton, M.L.; Chen, X.; Fernando, G.J.; Kendall, M.A. Targeted, needle-free vaccinations in skin using multilayered, densely-packed dissolving microprojection arrays. Small 2010, 6, 1785–1793. [Google Scholar] [CrossRef] [PubMed]
- Gupta, J.; Gill, H.S.; Andrews, S.N.; Prausnitz, M.R. Kinetics of skin resealing after insertion of microneedles in human subjects. J. Control. Release 2011, 154, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Jia, F.; Huang, W.; Yin, Y.; Jiang, Y.; Yang, Q.; Huang, H.; Nie, G.; Wang, H. Stabilizing RNA Nanovaccines with Transformable Hyaluronan Dynamic Hydrogel for Durable Cancer Immunotherapy. Adv. Funct. Mater. 2022, 33, 2204636. [Google Scholar] [CrossRef]
- Martin, J.R.; Howard, M.T.; Wang, S.; Berger, A.G.; Hammond, P.T. Oxidation-Responsive, Tunable Growth Factor Delivery from Polyelectrolyte-Coated Implants. Adv. Healthc. Mater. 2021, 10, e2001941. [Google Scholar] [CrossRef] [PubMed]
- Barberio, A.E.; Smith, S.G.; Correa, S.; Nguyen, C.; Nhan, B.; Melo, M.; Tokatlian, T.; Suh, H.; Irvine, D.J.; Hammond, P.T. Cancer Cell Coating Nanoparticles for Optimal Tumor-Specific Cytokine Delivery. ACS Nano 2020, 14, 11238–11253. [Google Scholar] [CrossRef]
- Zhang, Q.; Dehaini, D.; Zhang, Y.; Zhou, J.; Chen, X.; Zhang, L.; Fang, R.H.; Gao, W.; Zhang, L. Neutrophil membrane-coated nanoparticles inhibit synovial inflammation and alleviate joint damage in inflammatory arthritis. Nat. Nanotechnol. 2018, 13, 1182–1190. [Google Scholar] [CrossRef]
- Tan, H.; Song, Y.; Chen, J.; Zhang, N.; Wang, Q.; Li, Q.; Gao, J.; Yang, H.; Dong, Z.; Weng, X.; et al. Platelet-Like Fusogenic Liposome-Mediated Targeting Delivery of miR-21 Improves Myocardial Remodeling by Reprogramming Macrophages Post Myocardial Ischemia-Reperfusion Injury. Adv. Sci. 2021, 8, e2100787. [Google Scholar] [CrossRef]
- Sun, J.J.; Chen, Y.C.; Huang, Y.X.; Zhao, W.C.; Liu, Y.H.; Venkataramanan, R.; Lu, B.F.; Li, S. Programmable co-delivery of the immune checkpoint inhibitor NLG919 and chemotherapeutic doxorubicin via a redox-responsive immunostimulatory polymeric prodrug carrier. Acta Pharmacol. Sin. 2017, 38, 823–834. [Google Scholar] [CrossRef]
- Wang, S.; Chen, Y.; Ling, Z.; Li, J.; Hu, J.; He, F.; Chen, Q. The role of dendritic cells in the immunomodulation to implanted biomaterials. Int. J. Oral Sci. 2022, 14, 52. [Google Scholar] [CrossRef]
- Bookstaver, M.L.; Zeng, Q.; Oakes, R.S.; Kapnick, S.M.; Saxena, V.; Edwards, C.; Venkataraman, N.; Black, S.K.; Zeng, X.; Froimchuk, E.; et al. Self-Assembly of Immune Signals to Program Innate Immunity through Rational Adjuvant Design. Adv. Sci. 2022, 10, e2202393. [Google Scholar] [CrossRef]
- Leach, D.G.; Young, S.; Hartgerink, J.D. Advances in immunotherapy delivery from implantable and injectable biomaterials. Acta Biomater. 2019, 88, 15–31. [Google Scholar] [CrossRef]
- Chen, Z.; Lin, Y.; Lee, W.; Ren, L.; Liu, B.; Liang, L.; Wang, Z.; Jiang, L. Additive Manufacturing of Honeybee-Inspired Microneedle for Easy Skin Insertion and Difficult Removal. ACS Appl. Mater. Interfaces 2018, 10, 29338–29346. [Google Scholar] [CrossRef]
- Kost, J.; Mathiowitz, E.; Azagury, A. Advances in Drug Delivery and Theranostics. Adv. Funct. Mater. 2021, 31, 2108838. [Google Scholar] [CrossRef]
- Zhang, X.; Chen, G.; Sun, L.; Ye, F.; Shen, X.; Zhao, Y. Claw-inspired microneedle patches with liquid metal encapsulation for accelerating incisional wound healing. Chem. Eng. J. 2021, 406, 126741. [Google Scholar] [CrossRef]
- Abramson, A.; Caffarel-Salvador, E.; Soares, V.; Minahan, D.; Tian, R.Y.; Lu, X.; Dellal, D.; Gao, Y.; Kim, S.; Wainer, J.; et al. A luminal unfolding microneedle injector for oral delivery of macromolecules. Nat. Med. 2019, 25, 1512–1518. [Google Scholar] [CrossRef]
- Gniadecka, M.; Jemec, G.B. Quantitative evaluation of chronological ageing and photoageing in vivo: Studies on skin echogenicity and thickness. Br. J. Dermatol. 1998, 139, 815–821. [Google Scholar] [CrossRef]
- Guo, M.; Wang, Y.; Gao, B.; He, B. Shark Tooth-Inspired Microneedle Dressing for Intelligent Wound Management. ACS Nano 2021, 15, 15316–15327. [Google Scholar] [CrossRef]
- van der Heijden, M.; Vermeulen, L. Stem cells in homeostasis and cancer of the gut. Mol. Cancer 2019, 18, 66. [Google Scholar] [CrossRef]
- Joo, S.H.; Kim, J.; Hong, J.; Fakhraei Lahiji, S.; Kim, Y.H. Dissolvable Self-Locking Microneedle Patches Integrated with Immunomodulators for Cancer Immunotherapy. Adv. Mater. 2022, 35, 2209966. [Google Scholar] [CrossRef]
- He, T.; Luo, Y.; Zhang, Q.; Men, Z.; Su, T.; Fan, L.; Chen, H.; Shen, T. Hyalase-Mediated Cascade Degradation of a Matrix Barrier and Immune Cell Penetration by a Photothermal Microneedle for Efficient Anticancer Therapy. ACS Appl. Mater. Interfaces 2021, 13, 26790–26799. [Google Scholar] [CrossRef]
- Thong, T.; Forte, C.A.; Hill, E.M.; Colacino, J.A. Environmental exposures, stem cells, and cancer. Pharmacol. Ther. 2019, 204, 107398. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Tian, N.; Liu, F.; Zhang, Y.; Su, J.; Gao, Y.; Deng, M.; Wei, L.; Ye, J.; Li, H.; et al. A novel dephosphorylation targeting chimera selectively promoting tau removal in tauopathies. Signal Transduct. Target. Ther. 2021, 6, 269. [Google Scholar] [CrossRef] [PubMed]
- Du, L.; Cheng, Q.; Zheng, H.; Liu, J.; Liu, L.; Chen, Q. Targeting stemness of cancer stem cells to fight colorectal cancers. Semin. Cancer Biol. 2022, 82, 150–161. [Google Scholar] [CrossRef] [PubMed]
- Lan, L.; Behrens, A. Are There Specific Cancer Stem Cell Markers? Cancer Res. 2023, 83, 170–172. [Google Scholar] [CrossRef]
- Wang, C.; Li, Y.; Jia, L.; Kim, J.K.; Li, J.; Deng, P.; Zhang, W.; Krebsbach, P.H.; Wang, C.Y. CD276 expression enables squamous cell carcinoma stem cells to evade immune surveillance. Cell Stem Cell 2021, 28, 1597–1613.e7. [Google Scholar] [CrossRef]
- Lee, J.; Jang, E.H.; Kim, J.H.; Park, S.; Kang, Y.; Park, S.; Lee, K.; Kim, J.H.; Youn, Y.N.; Ryu, W. Highly flexible and porous silk fibroin microneedle wraps for perivascular drug delivery. J. Control. Release 2021, 340, 125–135. [Google Scholar] [CrossRef]
- Yang, J.; Li, G.; Yuan, J.; Jing, S.; Wang, X.; Yang, F.; Liu, Y.; Ding, Y.; Li, G.; Xie, G.; et al. A Smart Silk-Based Microneedle for Cancer Stem Cell Synergistic Immunity/Hydrogen Therapy. Adv. Funct. Mater. 2022, 32, 2206406. [Google Scholar] [CrossRef]
- Békés, M.; Langley, D.R.; Crews, C.M. PROTAC targeted protein degraders: The past is prologue. Nat. Rev. Drug Discov. 2022, 21, 181–200. [Google Scholar] [CrossRef]
- Cole, G.; Ali, A.A.; McErlean, E.; Mulholland, E.J.; Short, A.; McCrudden, C.M.; McCaffrey, J.; Robson, T.; Kett, V.L.; Coulter, J.A.; et al. DNA vaccination via RALA nanoparticles in a microneedle delivery system induces a potent immune response against the endogenous prostate cancer stem cell antigen. Acta Biomater. 2019, 96, 480–490. [Google Scholar] [CrossRef]
- Chang, H.; Wen, X.; Li, Z.; Ling, Z.; Zheng, Y.; Xu, C. Co-delivery of dendritic cell vaccine and anti-PD-1 antibody with cryomicroneedles for combinational immunotherapy. Bioeng. Transl. Med. 2022, e10457. [Google Scholar] [CrossRef]
- Xu, J.; Xu, B.; Tao, J.; Yang, Y.; Hu, Y.; Huang, Y. Microneedle-Assisted, DC-Targeted Codelivery of pTRP-2 and Adjuvant of Paclitaxel for Transcutaneous Immunotherapy. Small 2017, 13, 1700666. [Google Scholar] [CrossRef]
- Chen, M.; Yang, D.; Sun, Y.; Liu, T.; Wang, W.; Fu, J.; Wang, Q.; Bai, X.; Quan, G.; Pan, X.; et al. In Situ Self-Assembly Nanomicelle Microneedles for Enhanced Photoimmunotherapy via Autophagy Regulation Strategy. ACS Nano 2021, 15, 3387–3401. [Google Scholar] [CrossRef]
- Chen, S.X.; Ma, M.; Xue, F.; Shen, S.; Chen, Q.; Kuang, Y.; Liang, K.; Wang, X.; Chen, H. Construction of microneedle-assisted co-delivery platform and its combining photodynamic/immunotherapy. J. Control. Release 2020, 324, 218–227. [Google Scholar] [CrossRef]
- Dalvi, M.; Kharat, P.; Thakor, P.; Bhavana, V.; Singh, S.B.; Mehra, N.K. Panorama of dissolving microneedles for transdermal drug delivery. Life Sci. 2021, 284, 119877. [Google Scholar] [CrossRef]
- Dangol, M.; Yang, H.; Li, C.G.; Lahiji, S.F.; Kim, S.; Ma, Y.; Jung, H. Innovative polymeric system (IPS) for solvent-free lipophilic drug transdermal delivery via dissolving microneedles. J. Control. Release 2016, 223, 118–125. [Google Scholar] [CrossRef]
- Alkilani, A.Z.; Nasereddin, J.; Hamed, R.; Nimrawi, S.; Hussein, G.; Abo-Zour, H.; Donnelly, R.F. Beneath the Skin: A Review of Current Trends and Future Prospects of Transdermal Drug Delivery Systems. Pharmaceutics 2022, 14, 1152. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).