Investigating Tacrolimus Disposition in Paediatric Patients with a Physiologically Based Pharmacokinetic Model Incorporating CYP3A4 Ontogeny, Mechanistic Absorption and Red Blood Cell Binding
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals Used for In Vitro Experiments
2.2. In Vitro Experiments
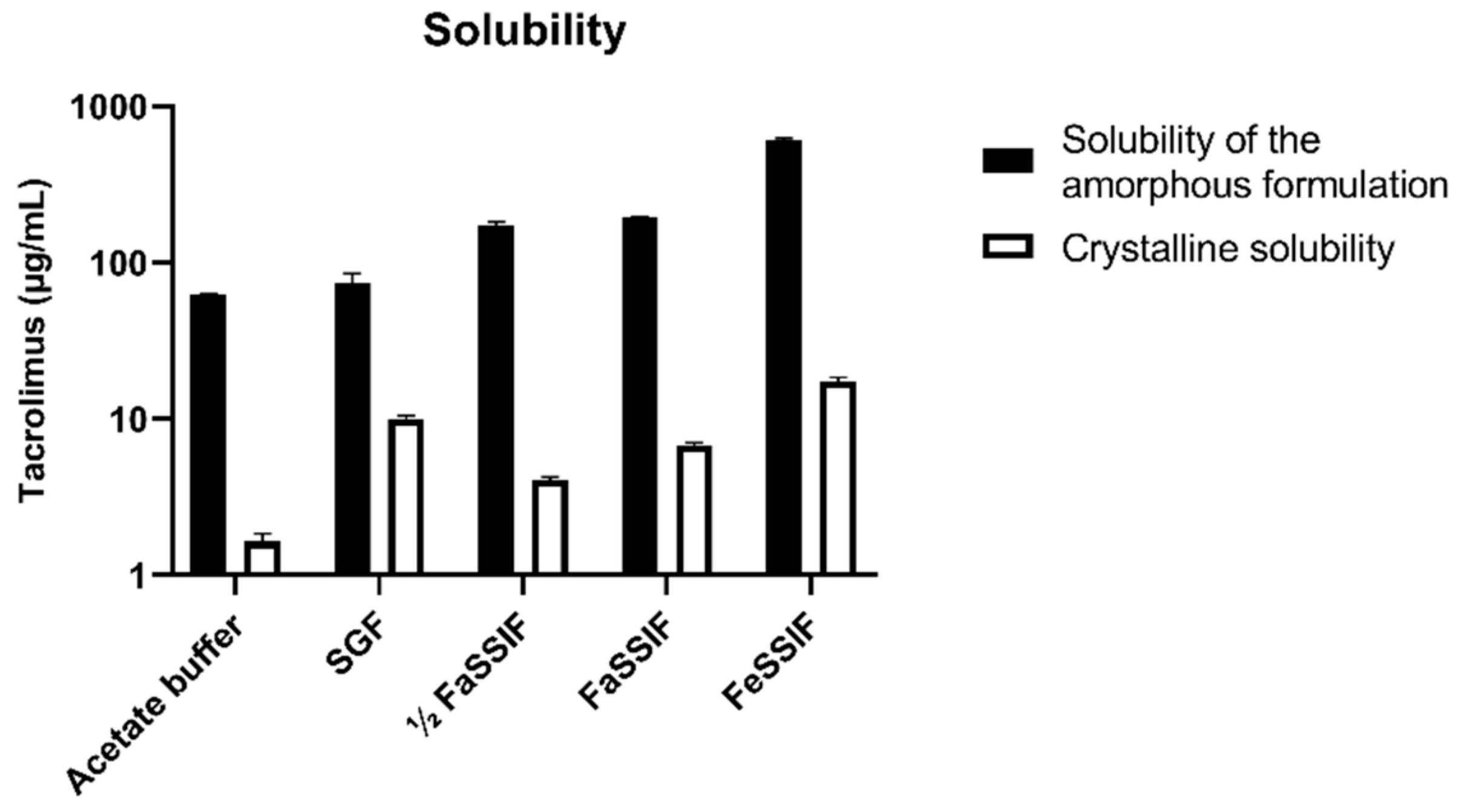
2.2.1. Solubility
2.2.2. Dissolution
2.2.3. Tacrolimus Analysis
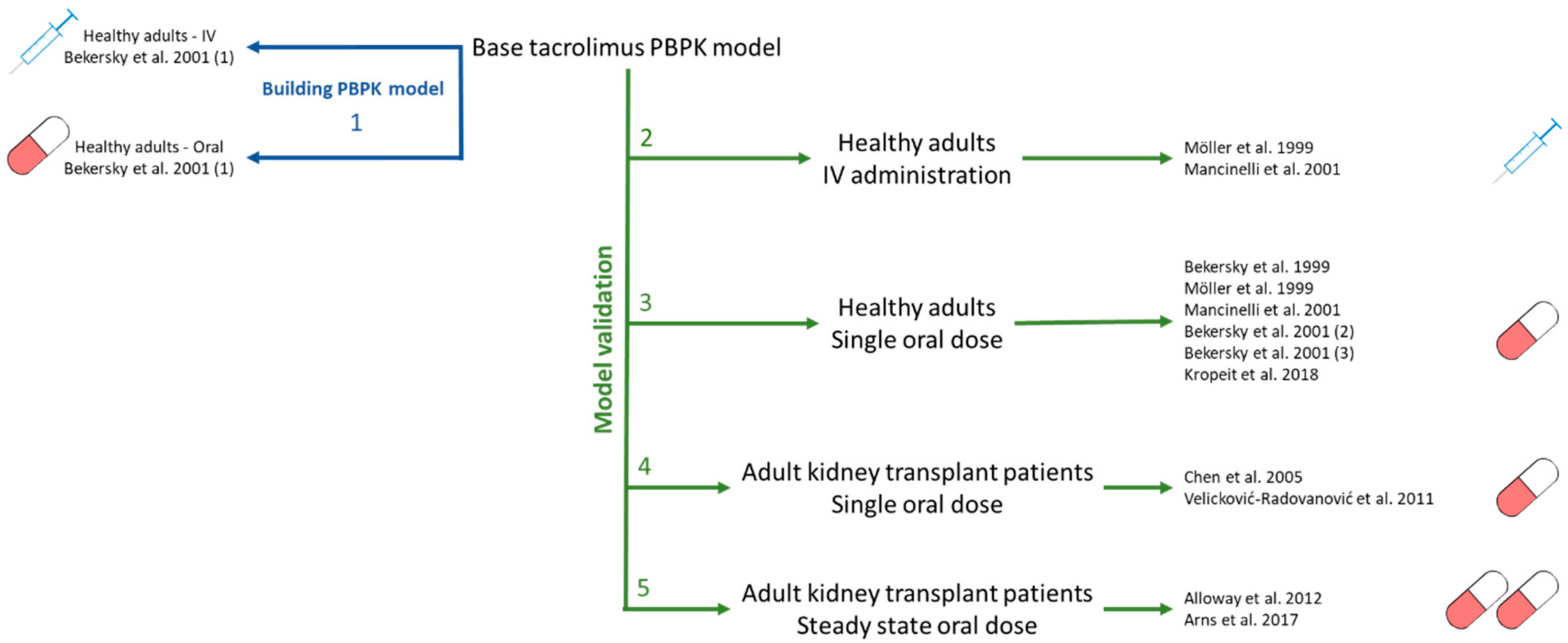
2.3. PBPK Model Building
2.3.1. Software Tools
2.3.2. Model Performance
2.3.3. SimCYP Model Building
Adult Model
| Adult Model | References | |
|---|---|---|
| Population | Healthy Volunteers | |
| Drug parameters | ||
| Physicochemical properties | ||
| Molecular weight (g/mol) | 804.02 | [36] |
| Log Po:w | 3.26 | [36] |
| Compound type | neutral | [36] |
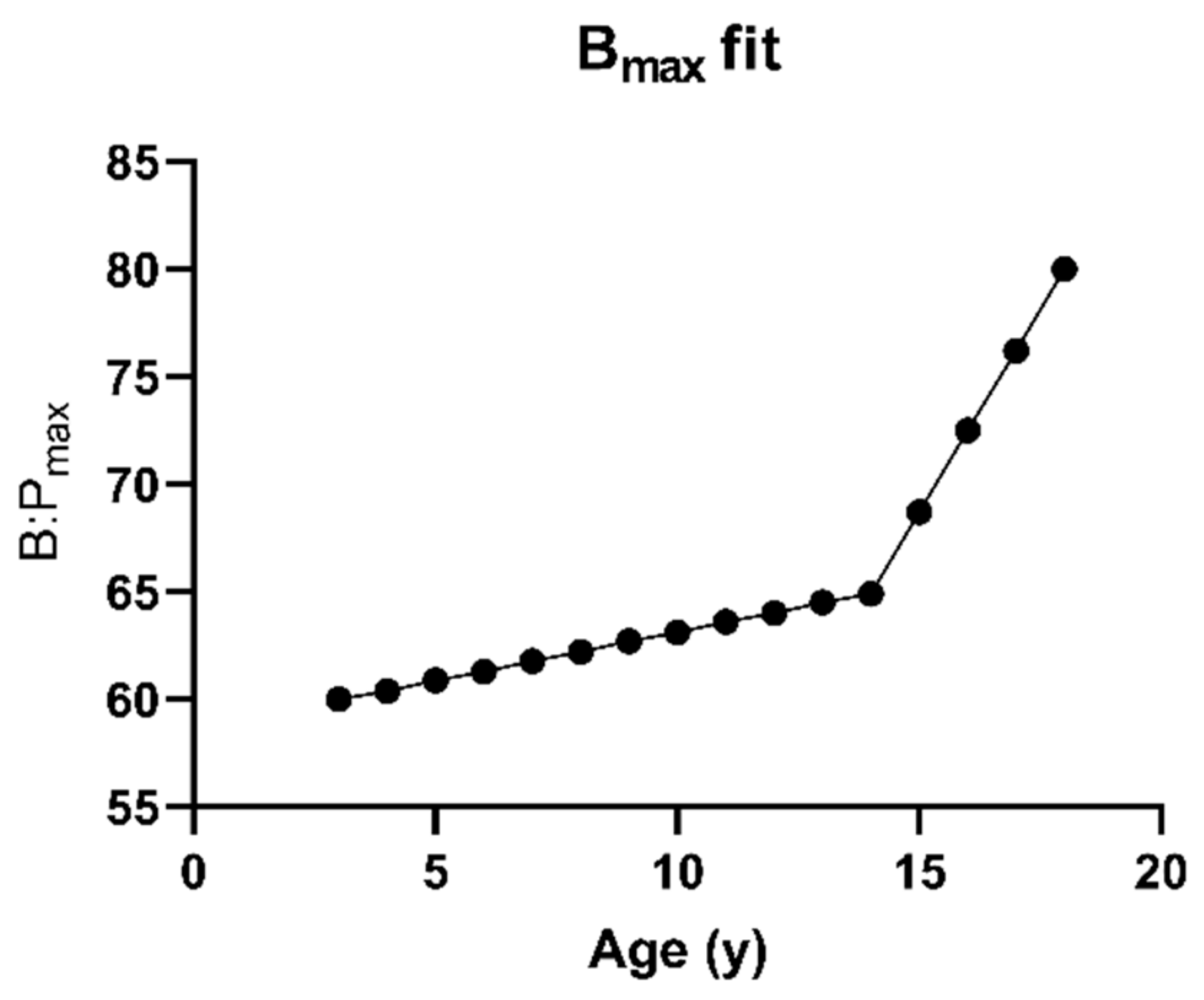
| Blood binding | ||
| Concentration-dependent B/P profile | ||
| Bmax (E:P) | 80 | [2] |
| KD (µM) | 0.004726 | [2] |
| Fraction unbound in plasma (%) | 1.2 | [37] |
| Absorption | ||
| ADAM model | ||
| Peff (10−4 cm/s) | 4.77 | [26] |
| DLM model intrinsic solubility (mg/mL) | 0.06257 | Aqueous buffer solubility for tacrolimus formulation |
| Logarithm of bile micelle:buffer partitioning coefficient (log Km:w) | 4.55 | Fitted using SIVA based on solubility data in acetate buffer, ½ FaSSIF, FaSSIF and FeSSIF |
| Monodispersed particle size distribution radius (µm) | 10 | Default SimCYP value |
| Distribution | ||
| Distribution model | Minimal PBPK | |
| kin (1/h) | 0.68 | [16] |
| kout (1/h) | 0.12 | Fitted based on IV data [25] |
| Vsac (L/kg) | 5.5 | Fitted based on IV data [25] |
| Kp scalar | 10 | Fitted based on IV data [25] |
| Predicted Vss (L/kg) | 9.68 | Predicted in SimCYP |
| Prediction method | Method 2 | |
| Elimination | ||
| Pathway 1 | ||
| CYP3A4 | ||
| Vmax (pmol/min/pmol CYP) | 8 | [1] |
| Km,u (µM) | 0.21 | [1] |
| CYP3A5 | ||
| Vmax (pmol/min/pmol CYP) | 17 | [1] |
| Km,u (µM) | 0.21 | [1] |
| Pathway 2 | ||
| CYP3A4 | ||
| Vmax (pmol/min/pmol CYP) | 0.6 | [1] |
| Km,u (µM) | 0.29 | [1] |
| CYP3A5 | ||
| Vmax (pmol/min/pmol CYP) | 1.4 | [1] |
| Km,u (µM) | 0.35 | [1] |
- Dissolution Model Comparison in the Adult Population
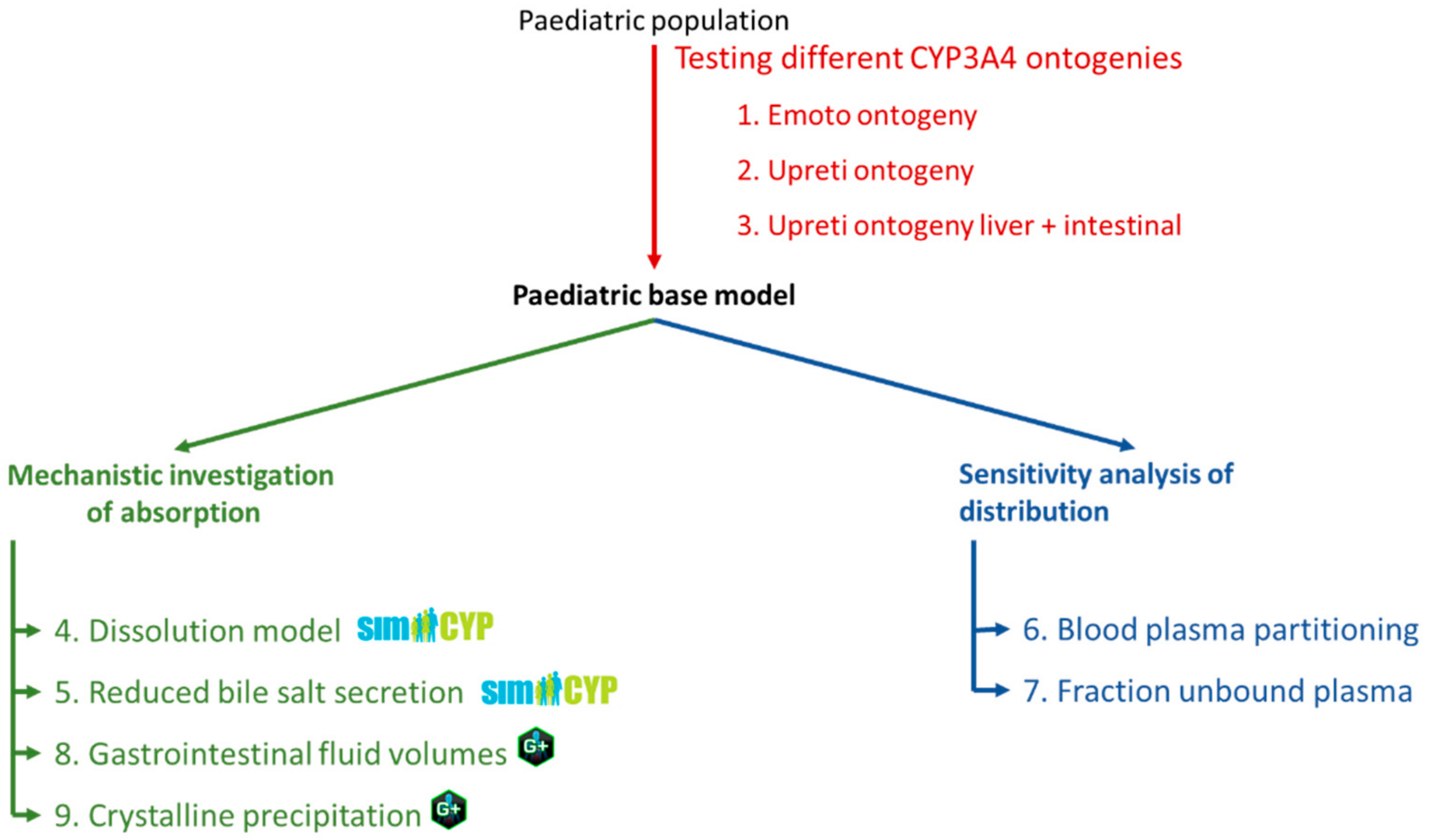
Extrapolation to Paediatrics
- Paediatric reference dataset for tacrolimus
- 2.
- Paediatric CYP3A4 and CYP3A5 ontogeny profiles
- 3.
- Exploring the impact of dissolution rate and bile salt levels on paediatric absorption of tacrolimus
- 4.
- Investigating impact of distribution on tacrolimus exposure
2.3.4. IVIVE Sensitivity Analysis on Tacrolimus Fraction Absorbed in Gastroplus
3. Results and Discussion
3.1. In Vitro Characterization
3.1.1. Solubility in Biorelevant Media
3.1.2. Dissolution Profiles
3.2. PBPK Modelling
3.2.1. Adult Population
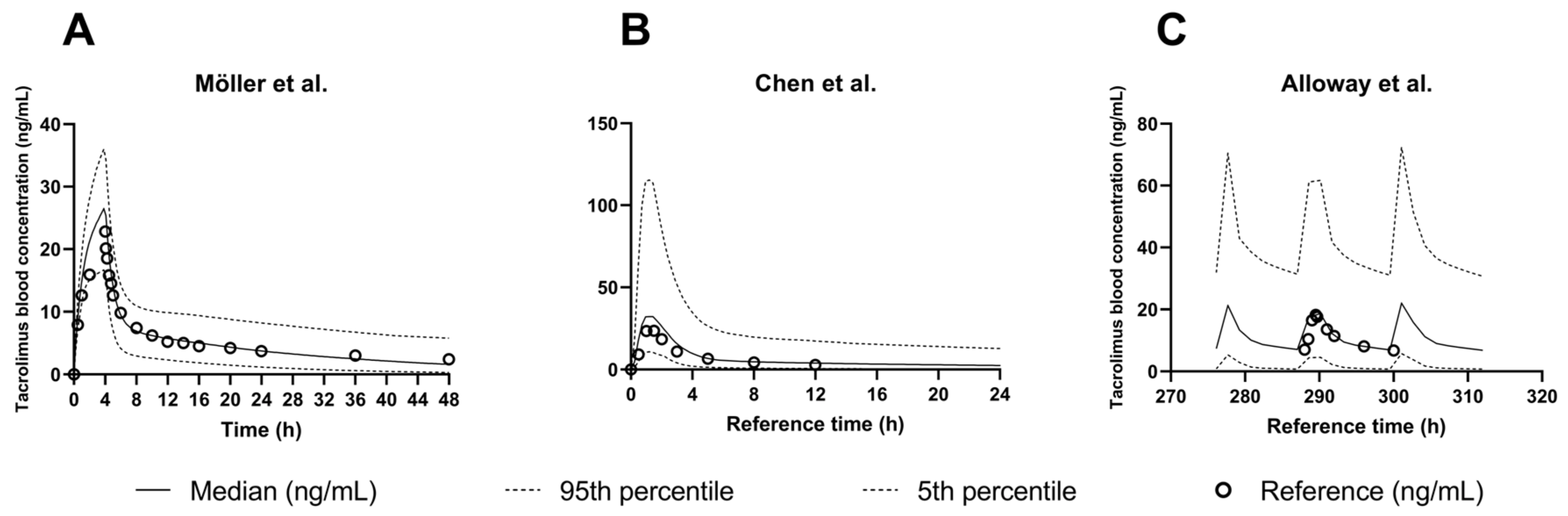
IV and Oral Administration
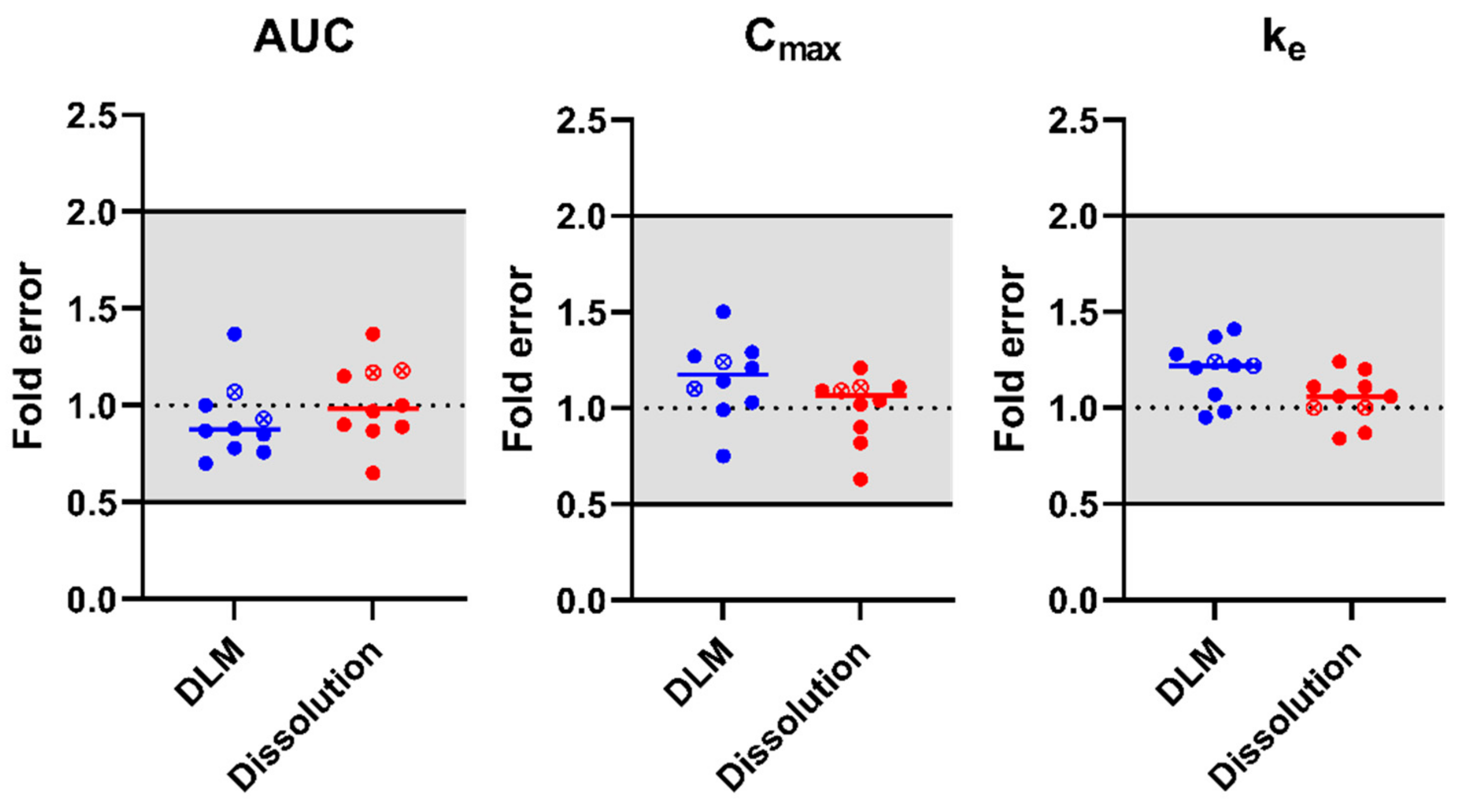
IVIVE to Explore the Impact of Dissolution Models on Tacrolimus Exposure
3.2.2. Paediatric Population
Exploration of the Impact of Dissolution Rate and Bile Salt Levels on Paediatric Absorption
Sensitivity Analysis of Tacrolimus Fraction Absorbed in Gastroplus
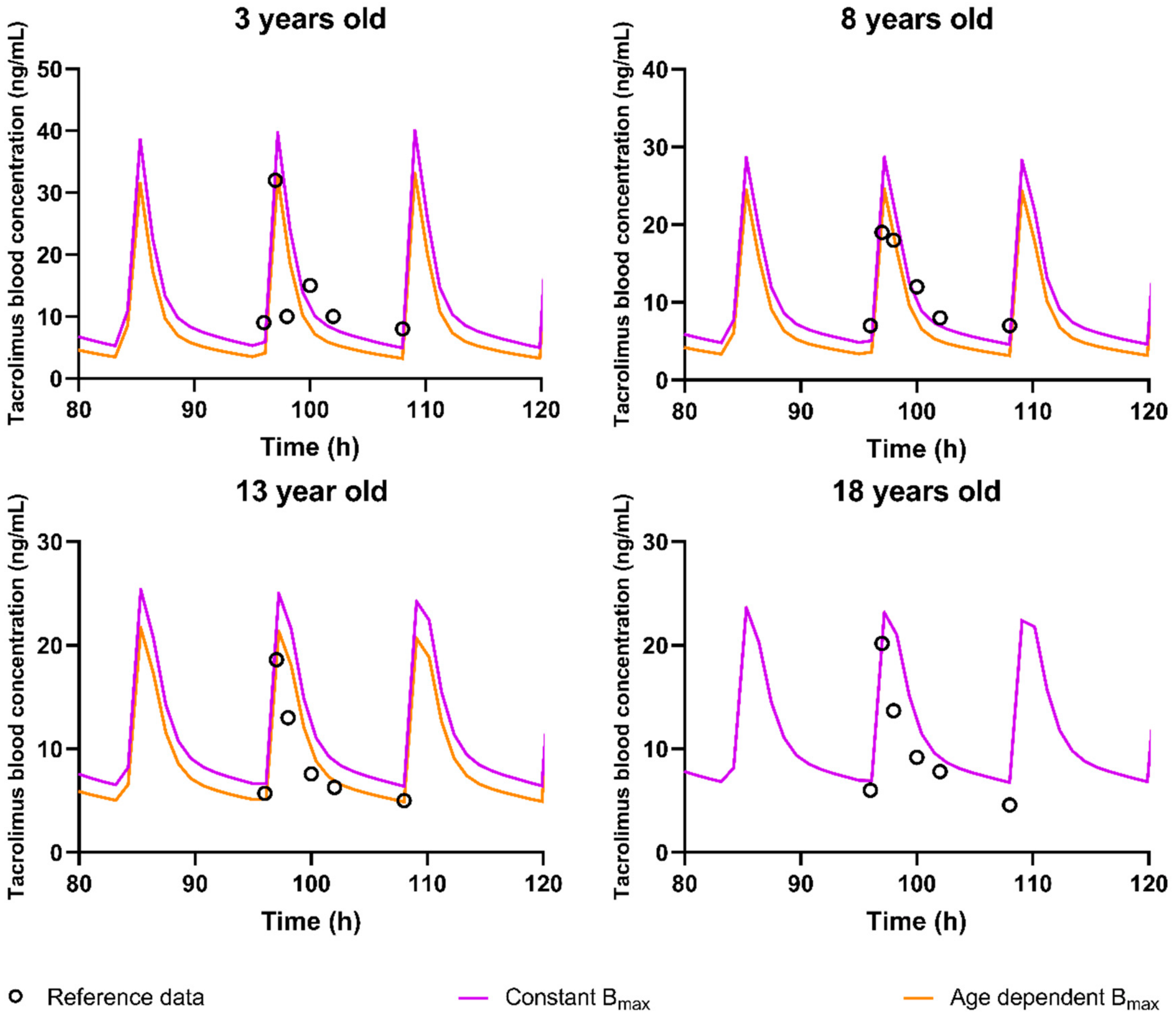
Exploring the Impact of Distribution on Tacrolimus Exposure Using Sensitivity Analysis
- Red blood cell partitioning
- 2.
- Fraction Unbound in Plasma
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dai, Y.; Hebert, M.F.; Isoherranen, N.; Davis, C.L.; Marsh, C.; Shen, D.D.; Thummel, K.E. Effect of CYP3A5 Polymorphism on Tacrolimus Metabolic Clearance In Vitro. Drug Metab. Dispos. 2006, 34, 836–847. [Google Scholar] [CrossRef]
- Jusko, W.J.; Piekoszewski, W.; Klintmalm, G.B.; Shaefer, M.S.; Hebert, M.F.; Piergies, A.A.; Lee, C.C.; Schechter, P.; Mekki, Q.A. Pharmacokinetics of Tacrolimus in Liver Transplant Patients. Clin. Pharmacol. Ther. 1995, 57, 281–290. [Google Scholar] [CrossRef] [PubMed]
- Möller, A.; Iwasaki, K.; Kawamura, A.; Teramura, Y.; Shiraga, T.; Hata, T.; Schäfer, A.; Undre, N.A. The Disposition of 14C-Labeled Tacrolimus after Intravenous and Oral Administration in Healthy Human Subjects. Drug Metab. Dispos. 1999, 27, 633–636. [Google Scholar] [PubMed]
- Wallemacq, P.E.; Verbeeck, R.K. Comparative Clinical Pharmacokinetics of Tacrolimus in Paediatric and Adult Patients. Clin. Pharmacokinet. 2001, 40, 283–295. [Google Scholar] [CrossRef] [PubMed]
- Van der Veken, M.; Brouwers, J.; Budts, V.; Lauwerys, L.; Pathak, S.M.; Batchelor, H.; Augustijns, P. Practical and Operational Considerations Related to Paediatric Oral Drug Formulation: An Industry Survey. Int. J. Pharm. 2022, 618, 121670. [Google Scholar] [CrossRef] [PubMed]
- Sager, J.E.; Yu, J.; Ragueneau-Majlessi, I.; Isoherranen, N. Physiologically Based Pharmacokinetic (PBPK) Modeling and Simulation Approaches: A Systematic Review of Published Models, Applications, and Model Verification. Drug Metab. Dispos. 2015, 43, 1823–1837. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Lu, X.; Zuo, M.; Wang, N.; Zhang, Y.; Chen, J.; Zhu, L.; Liu, W. Drug–Drug Interaction Comparison between Tacrolimus and Phenobarbital in Different Formulations for Paediatrics and Adults. Xenobiotica 2021, 51, 877–884. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Bu, F.; Li, L.; Jiao, Z.; Ma, G.; Cai, W.; Zhuang, X.; Lin, H.S.; Shin, J.G.; Xiang, X. Prediction of Drug–Drug Interaction between Tacrolimus and Principal Ingredients of Wuzhi Capsule in Chinese Healthy Volunteers Using Physiologically-Based Pharmacokinetic Modelling. Basic Clin. Pharmacol. Toxicol. 2018, 122, 331–340. [Google Scholar] [CrossRef]
- He, Q.; Bu, F.; Wang, Q.; Li, M.; Lin, J.; Tang, Z.; Mak, W.Y.; Zhuang, X.; Zhu, X.; Lin, H.S.; et al. Examination of the Impact of CYP3A4/5 on Drug–Drug Interaction between Schizandrol A/Schizandrol B and Tacrolimus (FK-506): A Physiologically Based Pharmacokinetic Modeling Approach. Int. J. Mol. Sci. 2022, 23, 4485. [Google Scholar] [CrossRef]
- Adiwidjaja, J.; Boddy, A.V.; McLachlan, A.J. Potential for Pharmacokinetic Interactions between Schisandra Sphenanthera and Bosutinib, but Not Imatinib: In Vitro Metabolism Study Combined with a Physiologically-Based Pharmacokinetic Modelling Approach. Br. J. Clin. Pharmacol. 2020, 86, 2080–2094. [Google Scholar] [CrossRef]
- Qian, C.Q.; Zhao, K.J.; Chen, Y.; Liu, L.; Liu, X.D. Simultaneously Predict Pharmacokinetic Interaction of Rifampicin with Oral versus Intravenous Substrates of Cytochrome P450 3A/P-glycoprotein to Healthy Human Using a Semi-Physiologically Based Pharmacokinetic Model Involving Both Enzyme and Transporter T. Eur. J. Pharm. Sci. 2019, 134, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Purohit, H.S.; Trasi, N.S.; Sun, D.D.; Chow, E.C.Y.; Wen, H.; Zhang, X.; Gao, Y.; Taylor, L.S. Investigating the Impact of Drug Crystallinity in Amorphous Tacrolimus Capsules on Pharmacokinetics and Bioequivalence Using Discriminatory In Vitro Dissolution Testing and Physiologically Based Pharmacokinetic Modeling and Simulation. J. Pharm. Sci. 2018, 107, 1330–1341. [Google Scholar] [CrossRef] [PubMed]
- Gao, G.F.; Ashtikar, M.; Kojima, R.; Yoshida, T.; Kaihara, M.; Tajiri, T.; Shanehsazzadeh, S.; Modh, H.; Wacker, M.G. Predicting Drug Release and Degradation Kinetics of Long-Acting Microsphere Formulations of Tacrolimus for Subcutaneous Injection. J. Control. Release 2021, 329, 372–384. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, S.; Yadav, L.; Aggarwal, D. Prediction of in Vivo Drug Performance Using in Vitro Dissolution Coupled with STELLA: A Study with Selected Drug Products. Drug Dev. Ind. Pharm. 2014, 41, 1667–1673. [Google Scholar] [CrossRef] [PubMed]
- Itohara, K.; Yano, I.; Nakagawa, S.; Yonezawa, A.; Omura, T.; Imai, S.; Nakagawa, T.; Sawada, A.; Kobayashi, T.; Tochio, A.; et al. Extrapolation of Physiologically Based Pharmacokinetic Model for Tacrolimus from Renal to Liver Transplant Patients. Drug Metab. Pharmacokinet. 2022, 42, 100423. [Google Scholar] [CrossRef] [PubMed]
- Emoto, C.; Johnson, T.N.; Hahn, D.; Christians, U.; Alloway, R.R.; Vinks, A.A.; Fukuda, T. A Theoretical Physiologically-Based Pharmacokinetic Approach to Ascertain Covariates Explaining the Large Interpatient Variability in Tacrolimus Disposition. CPT Pharmacomet. Syst. Pharmacol. 2019, 8, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Gérard, C.; Stocco, J.; Hulin, A.; Blanchet, B.; Verstuyft, C.; Durand, F.; Conti, F.; Duvoux, C.; Tod, M. Determination of the Most Influential Sources of Variability in Tacrolimus Trough Blood Concentrations in Adult Liver Transplant Recipients: A Bottom-up Approach. AAPS J. 2014, 16, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Gertz, M.; Houston, J.B.; Galetin, A. Physiologically Based Pharmacokinetic Modeling of Intestinal First-Pass Metabolism of CYP3A Substrates with High Intestinal Extraction. Drug Metab. Dispos. 2011, 39, 1633–1642. [Google Scholar] [CrossRef]
- Kirubakaran, R.; Stocker, S.L.; Hennig, S.; Day, R.O.; Carland, J.E. Population Pharmacokinetic Models of Tacrolimus in Adult Transplant Recipients: A Systematic Review; Springer International Publishing: Berlin/Heidelberg, Germany, 2020; Volume 59, ISBN 0123456789. [Google Scholar]
- Naesens, M.; Salvatierra, O.; Li, L.; Kambham, N.; Concepcion, W.; Sarwal, M. Maturation of Dose-Corrected Tacrolimus Predose Trough Levels in Pediatric Kidney Allograft Recipients. Transplantation 2008, 85, 1139–1145. [Google Scholar] [CrossRef]
- Knops, N.; Herman, J.; van Dyck, M.; Ramazani, Y.; Debbaut, E.; van Damme-Lombaerts, R.; Levtchenko, E.; van den Heuvel, L.P.; Fieuws, S.; Kuypers, D. Tacrolimus Dose Requirements in Paediatric Renal Allograft Recipients Are Characterized by a Biphasic Course Determined by Age and Bone Maturation. Br. J. Clin. Pharmacol. 2017, 83, 863–874. [Google Scholar] [CrossRef]
- Mudie, D.M.; Murray, K.; Hoad, C.L.; Pritchard, S.E.; Garnett, M.C.; Amidon, G.L.; Gowland, P.A.; Spiller, R.C.; Amidon, G.E.; Marciani, L. Quantification of Gastrointestinal Liquid Volumes and Distribution Following a 240 ML Dose of Water in the Fasted State. Mol. Pharm. 2014, 11, 3039–3047. [Google Scholar] [CrossRef] [PubMed]
- Van der Veken, M.; Aertsen, M.; Brouwers, J.; Stillhart, C.; Parrott, N.; Augustijns, P. Gastrointestinal Fluid Volumes in Pediatrics: A Retrospective MRI Study. Pharmaceutics 2022, 14, 1935. [Google Scholar] [CrossRef] [PubMed]
- Kuepfer, L.; Niederalt, C.; Wendl, T.; Schlender, J.F.; Willmann, S.; Lippert, J.; Block, M.; Eissing, T.; Teutonico, D. Applied Concepts in PBPK Modeling: How to Build a PBPK/PD Model. CPT Pharmacomet. Syst. Pharmacol. 2016, 5, 516–531. [Google Scholar] [CrossRef] [PubMed]
- Bekersky, I.; Dressler, D.; Alak, A.; Boswell, G.W.; Mekki, Q.A. Comparative Tacrolimus Pharmacokinetics: Normal versus Mildly Hepatically Impaired Subjects. J. Clin. Pharmacol. 2001, 41, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Tamura, S.; Ohike, A.; Ibuki, R.; Amidon, G.L.; Yamashita, S. Tacrolimus Is a Class II Low-Solubility High-Permeability Drug: The Effect of P-Glycoprotein Efflux on Regional Permeability of Tacrolimus in Rats. J. Pharm. Sci. 2002, 91, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Mancinelli, L.M.; Frassetto, L.; Floren, L.C.; Dressler, D.; Carrier, S.; Bekersky, I.; Benet, L.Z.; Christians, U. The Pharmacokinetics and Metabolic Disposition of Tacrolimus: A Comparison across Ethnic Groups. Clin. Pharmacol. Ther. 2001, 69, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Bekersky, I.; Dressler, D.; Colburn, W.; Mekki, Q. Bioequivalence of 1 and 5 Mg Tacrolimus Capsules Using a Replicate Study Design. J. Clin. Pharmacol. 1999, 39, 1032–1037. [Google Scholar] [CrossRef]
- Bekersky, I.; Dressler, D.; Mekki, Q. Effect of Time of Meal Consumption on Bioavailability of a Single Oral 5 Mg Tacrolimus Dose. J. Clin. Pharmacol. 2001, 41, 289–297. [Google Scholar] [CrossRef]
- Bekersky, I.; Dressler, D.; Mekki, Q.A. Effect of Low- and High-Fat Meals on Tacrolimus Absorption Following 5 Mg Single Oral Doses to Healthy Human Subjects. J. Clin. Pharmacol. 2001, 41, 176–182. [Google Scholar] [CrossRef]
- Kropeit, D.; von Richter, O.; Stobernack, H.P.; Rübsamen-Schaeff, H.; Zimmermann, H. Pharmacokinetics and Safety of Letermovir Coadministered With Cyclosporine A or Tacrolimus in Healthy Subjects. Clin. Pharmacol. Drug Dev. 2018, 7, 9–21. [Google Scholar] [CrossRef]
- Chen, Y.H.; Zheng, K.L.; Chen, L.Z.; Dai, Y.P.; Fei, J.G.; Qiu, J.; Li, J. Clinical Pharmacokinetics of Tacrolimus after the First Oral Administration in Combination with Mycophenolate Mofetil and Prednisone in Chinese Renal Transplant Recipients. Transplant. Proc. 2005, 37, 4246–4250. [Google Scholar] [CrossRef] [PubMed]
- Velicković-Radovanović, R.; Mikov, M.; Paunović, G.; Djordjević, V.; Stojanović, M.; Cvetković, T.; Djordjević, A.C. Gender Differences in Pharmacokinetics of Tacrolimus and Their Clinical Significance in Kidney Transplant Recipients. Gend. Med. 2011, 8, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Alloway, R.R.; Sadaka, B.; Trofe-Clark, J.; Wiland, A.; Bloom, R.D. A Randomized Pharmacokinetic Study of Generic Tacrolimus versus Reference Tacrolimus in Kidney Transplant Recipients. Am. J. Transplant. 2012, 12, 2825–2831. [Google Scholar] [CrossRef] [PubMed]
- Arns, W.; Huppertz, A.; Rath, T.; Ziefle, S.; Rump, L.C.; Hansen, A.; Budde, K.; Lehner, L.J.; Shipkova, M.; Baeumer, D.; et al. Pharmacokinetics and Clinical Outcomes of Generic Tacrolimus (Hexal) Versus Branded Tacrolimus in De Novo Kidney Transplant Patients: A Multicenter, Randomized Trial. Transplantation 2017, 101, 2780–2788. [Google Scholar] [CrossRef] [PubMed]
- Gertz, M.; Harrison, A.; Houston, J.B.; Galetin, A. Prediction of Human Intestinal First-Pass Metabolism of 25 CYP3A Substrates from In Vitro Clearance and Permeability Data. Drug Metab. Dispos. 2010, 38, 1147–1158. [Google Scholar] [CrossRef] [PubMed]
- Zahir, H.; Nand, R.A.; Brown, K.F.; Tattam, B.N.; McLachlan, A.J. Validation of Methods to Study the Distribution and Protein Binding of Tacrolimus in Human Blood. J. Pharmacol. Toxicol. Methods 2001, 46, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Trasi, N.S.; Purohit, H.S.; Taylor, L.S. Evaluation of the Crystallization Tendency of Commercially Available Amorphous Tacrolimus Formulations Exposed to Different Stress Conditions. Pharm. Res. 2017, 34, 2142–2155. [Google Scholar] [CrossRef] [PubMed]
- Salem, F.; Johnson, T.N.; Abduljalil, K.; Tucker, G.T.; Rostami-Hodjegan, A. A Re-Evaluation and Validation of Ontogeny Functions for Cytochrome P450 1A2 and 3A4 Based on in Vivo Data. Clin. Pharmacokinet. 2014, 53, 625–636. [Google Scholar] [CrossRef]
- Johnson, T.N.; Tanner, M.S.; Taylor, C.J.; Tucker, G.T. Enterocytic CYP3A4 in a Paediatric Population: Developmental Changes and the Effect of Coeliac Disease and Cystic Fibrosis. Br. J. Clin. Pharmacol. 2001, 51, 451–460. [Google Scholar] [CrossRef]
- Upreti, V.V.; Wahlstrom, J.L. Meta-Analysis of Hepatic Cytochrome P450 Ontogeny to Underwrite the Prediction of Pediatric Pharmacokinetics Using Physiologically Based Pharmacokinetic Modeling. J. Clin. Pharmacol. 2016, 56, 266–283. [Google Scholar] [CrossRef]
- Yoshikawa, N.; Yokota, T.; Matsuo, A.; Matsumoto, N.; Iwakiri, T.; Ikeda, R. Role of FK506 Binding Protein on Tacrolimus Distribution in Red Blood Cells. Pharm. Res. 2020, 37, 143. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.N.; Howgate, E.M.; De Wildt, S.N.; Turner, M.A.; Uk, C.; Simcyp, L.; Sheffield, S.; Tnj, U.K. Use of Developmental Midazolam and 1-Hydroxymidazolam Data with Pediatric Physiologically Based Modelling to Assess CYP3A4 and UGT2B4 Ontogeny. Drug Metab. Dispos. 2023, 51, 1035–1045. [Google Scholar] [CrossRef] [PubMed]
- Kiss, M.; Mbasu, R.; Nicolaï, J.; Barnouin, K.; Kotian, A.; Mooij, M.G.; Kist, N.; Wijnen, R.M.H.; Ungell, A.L.; Cutler, P.; et al. Ontogeny of Small Intestinal Drug Transporters and Metabolizing Enzymes Based on Targeted Quantitative ProteomicsS. Drug Metab. Dispos. 2021, 49, 1038–1046. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-T.; Trzoss, L.; Yang, D.; Yan, B. Ontogenic Expression of Human Carboxylesterase-2 and Cytochrome P450 3A4 in Liver and Duodenum: Postnatal Surge and Organ-Dependent Regulation. Toxicology 2015, 330, 55–61. [Google Scholar] [CrossRef]
- Fakhoury, M.; Litalien, C.; Medard, Y.; Cavé, H.; Ezzahir, N.; Peuchmaur, M.; Jacqz-Aigrain, E. Localization and mRNA expression of CYP3A and P-glycoprotein in human duodenum as a function of age. Drug Metab. Dispos. 2005, 33, 1603–1607. [Google Scholar] [CrossRef] [PubMed]
- Darwich, A.S.; Neuhoff, S.; Jamei, M.; Rostami-Hodjegan, A. Interplay of Metabolism and Transport in Determining Oral Drug Absorption and Gut Wall Metabolism: A Simulation Assessment Using the “Advanced Dissolution, Absorption, Metabolism (ADAM)” Model. Curr. Drug Metab. 2011, 11, 716–729. [Google Scholar] [CrossRef] [PubMed]
- Jogiraju, V.K.; Avvari, S.; Gollen, R.; Taft, D.R. Application of Physiologically Based Pharmacokinetic Modeling to Predict Drug Disposition in Pregnant Populations. Biopharm. Drug Dispos. 2017, 38, 426–438. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, K.L.R.; Aleksunes, L.M.; Brandys, B.; Giacoia, G.P.; Knipp, G.; Lukacova, V.; Meibohm, B.; Nigam, S.; Rieder, M.; Wildt, S. De Human Ontogeny of Drug Transporters: Review and Recommendations of the Pediatric Transporter Working Group. Clin. Pharmacol. Ther. 2015, 98, 266–287. [Google Scholar] [CrossRef]
- De Waal, T.; Brouwers, J.; Mols, R.; Hoffman, I.; Rayyan, M.; Augustijns, P. Characterization of Neonatal and Infant Enterostomy Fluids. Int. J. Pharm. 2023, 639, 122943. [Google Scholar] [CrossRef]
- Van Den Abeele, J.; Rayyan, M.; Hoffman, I.; Van de Vijver, E.; Zhu, W.; Augustijns, P. Gastric Fluid Composition in a Paediatric Population: Age-Dependent Changes Relevant for Gastrointestinal Drug Disposition. Eur. J. Pharm. Sci. 2018, 123, 301–311. [Google Scholar] [CrossRef]

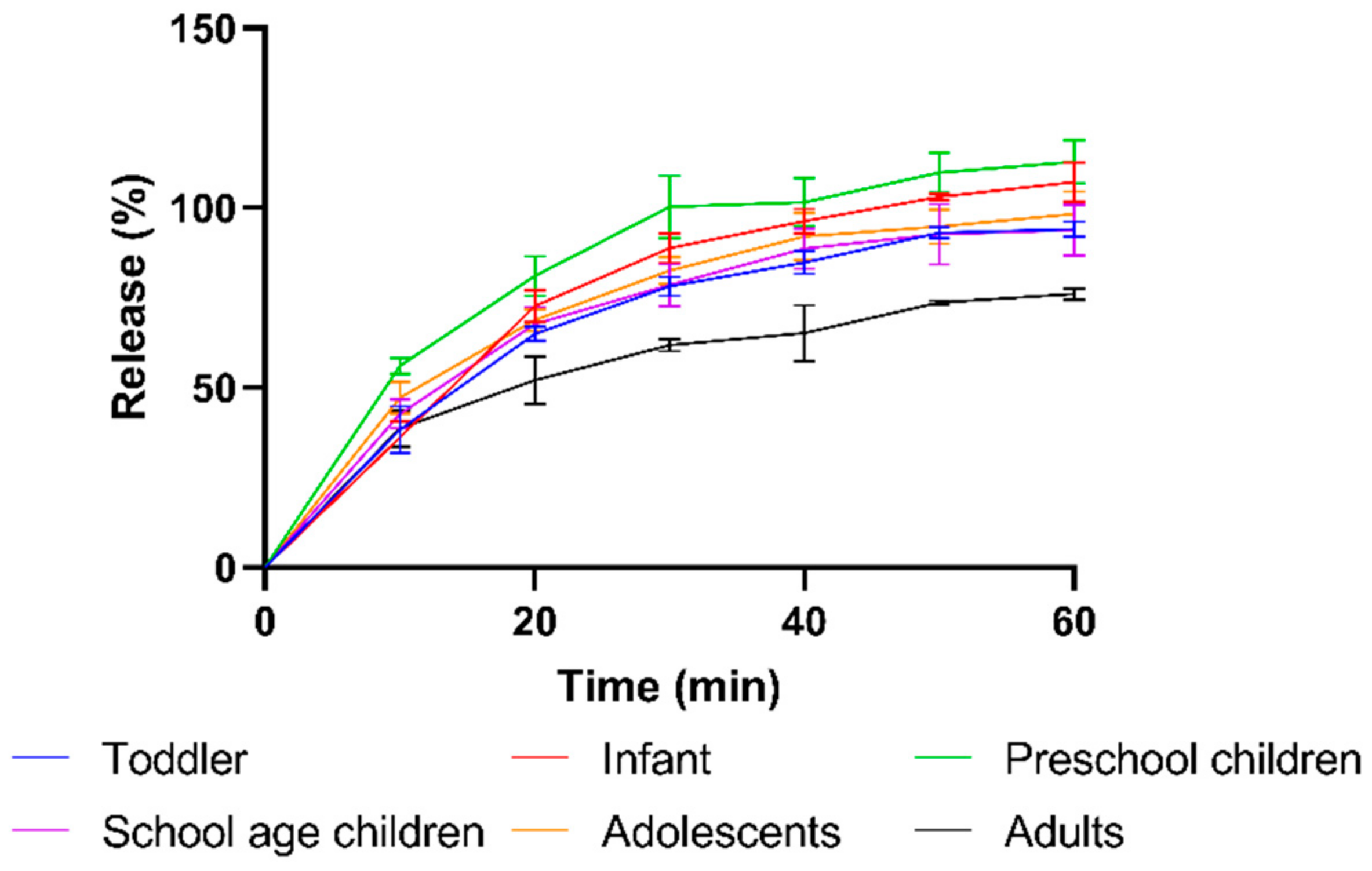

| Subpopulation | Average SIFV Reported (mL) | Volume Used In Vitro (mL) | Body Weight (kg) | Dose (mg) | Dose/Volume Ratio (mg/mL) |
|---|---|---|---|---|---|
| Infant (0.1–1 year) | 22.1 | 25 | 7.3 | 1.09 | 0.04 |
| Toddler (1–2 year) | 35.1 | 35 | 10.1 | 1.51 | 0.04 |
| Preschool child (2–5 year) | 38.5 | 40 | 10.8 | 1.63 | 0.04 |
| School-age child (6–11 year) | 48.5 | 50 | 22.0 | 3.30 | 0.07 |
| Adolescent (12–16 year) | 94.0 | 50 | 53.4 | 8.01 | 0.16 |
| Adult | 43.0 | 50 | 70.0 | 10.50 | 0.21 |
| MS Method | UV Method | ||||
|---|---|---|---|---|---|
| Column | Kinetex 2.6 µm XB-C18 100A 50 × 2.1 mm | Acquity UPLC BEH-C18 1.7 µm 50 mm × 2.1 mm | |||
| Flow (mL/min) | 0.6 | 0.8 | |||
| Column temperature (°C) | 55 | 60 | |||
| Injection volume | 5 | 80 | |||
| Time (min) | MP 1 (%) | MP 2 (%) | Time (min) | MP 3 (%) | MP 4 (%) |
| 0 | 25 | 75 | 0 | 55 | 45 |
| 0.5 | 97.5 | 2.5 | 8 | 45 | 55 |
| 2 | 25 | 75 | 8.5 | 55 | 45 |
| 3.2 | 25 | 75 | 12 | 55 | 45 |
| Detection | Tacrolimus-NH4 | 821.7 → 768.6 | UV | 210 nm | |
| Tacrolimus-NH4 D5 | 826.6 → 773.6 | ||||
| Name in This Paper | Liver CYP3A4 Ontogeny | Intestinal CYP3A4 Ontogeny | Liver CYP3A5 Ontogeny | Intestinal CYP3A5 Ontogeny |
|---|---|---|---|---|
| Salem ontogeny | SimCYP profile 1— Salem et al. | SimCYP default— Johnson et al. | SimCYP default— no ontogeny | SimCYP default—Johnson et al. |
| Upreti ontogeny | SimCYP profile 2— Upreti et al. | No ontogeny | ||
| Emoto ontogeny | Custom refitting of Salem et al. [16] | SimCYP default— Johnson et al. | ||
| Upreti liver + intestine ontogeny | SimCYP profile 2— Upreti et al. | SimCYP profile 2— Upreti et al. |
| Adult Model | References | |
|---|---|---|
| Population | Healthy Volunteers | |
| Drug Parameters | ||
| Physicochemical properties | ||
| Molecular weight (g/mol) | 804.02 | [36] |
| Log Po:w | 3.26 | [36] |
| Compound type | neutral | [36] |
| Absorption | ||
| ACAT model | ||
| Peff (10−4 cm/s) | 4.77 | [26] |
| Formulation | IR Capsule | |
| Solubility @ pH 4.5 ABS buffer—Amorphous formulation (mg/mL) (Reference solubility) | 0.06257 | In-house data |
| SGF solubility—Amorphous formulation (mg/mL) | 0.07412 | In-house data |
| FaSSIF Solubility—Amorphous formulation (mg/mL) | 0.19655 | In-house data |
| FeSSIF Solubility—Amorphous formulation (mg/mL) | 0.60547 | In-house data |
| Solubilization ratio—Amorphous formulation | 30300 | Gastroplus fitted |
| Solubility @ pH 4.5 ABS buffer—Crystalline (mg/mL) | 0.00165 | In-house data |
| SGF solubility—Crystalline (mg/mL) | 0.01003 | In-house data |
| FaSSIF Solubility—Crystalline (mg/mL) | 0.00678 | In-house data |
| FeSSIF Solubility—Crystalline (mg/mL) | 0.01746 | In-house data |
| Solubilization ratio—Crystalline | 11400 | Gastroplus fitted |
| Mean particle radius (µm) | 25 | Default value in Gastroplus |
| Mean precipitation time (sec) | 900 | Default value in Gastroplus |
| Particle density (g/mL) | 1.2 | Default value in Gastroplus |
| Distribution | ||
| Distribution model | none used | |
| PSA input | ||
| Dose (mg) | 10.5, 5, 2.5, 1.25 or 0.625 | |
| PSA analysis setup | Input value | |
| Small intestine fluid volume (minimum) | 0.28% filled (4.0 mL) | |
| Small intestine fluid volume (baseline) | 3.15% filled (45.2 mL) | |
| Small intestine fluid volume (maximum) | 15.75% filled (225.5 mL) | |
| Precipitation time (minimum) | 0.1 s | |
| Precipitation time (baseline) | 90 s | |
| Precipitation time (maximum) | 900 s | |
| Model # | Ontogeny Profile and Fit | AUC | Cmax (ng/mL) | C0 (ng/mL) | ke (ng/mL/h) | Individual Timepoints | |
|---|---|---|---|---|---|---|---|
| 1 | Liver: Emoto ontogeny | AFE | 1.30 | 1.77 | 0.88 | 1.23 | 1.28 |
| Intestine: Johnson ontogeny | AAFE | 1.40 | 1.86 | 1.34 | 1.37 | 1.61 | |
| Extra fit: n/a | Slope | −0.05 | −0.13 | −0.01 | −0.02 | −0.06 | |
| 2 | Liver: Upreti ontogeny | AFE | 1.98 | 2.34 | 1.62 | 0.98 | 1.87 |
| Intestine: No ontogeny | AAFE | 1.99 | 2.34 | 1.66 | 1.32 | 2.14 | |
| Extra fit: n/a | Slope | −0.04 | −0.12 | 0.00 | −0.01 | −0.05 | |
| 3 | Liver: Upreti ontogeny | AFE | 1.10 | 1.44 | 0.78 | 1.18 | 1.11 |
| Intestine: Upreti ontogeny | AAFE | 1.30 | 1.52 | 1.46 | 1.34 | 1.51 | |
| Extra fit: n/a | Slope | 0.01 | −0.03 | 0.03 | −0.02 | 0.01 | |
| 4 | Liver: Upreti ontogeny | AFE | 0.90 | 1.24 | 0.59 | 1.26 | 0.94 |
| Intestine: Upreti ontogeny | AAFE | 1.30 | 1.38 | 1.79 | 1.40 | 1.58 | |
| Extra fit: Bmax fit | Slope | 0.03 | −0.01 | 0.04 | −0.03 | 0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van der Veken, M.; Brouwers, J.; Ozbey, A.C.; Umehara, K.; Stillhart, C.; Knops, N.; Augustijns, P.; Parrott, N.J. Investigating Tacrolimus Disposition in Paediatric Patients with a Physiologically Based Pharmacokinetic Model Incorporating CYP3A4 Ontogeny, Mechanistic Absorption and Red Blood Cell Binding. Pharmaceutics 2023, 15, 2231. https://doi.org/10.3390/pharmaceutics15092231
Van der Veken M, Brouwers J, Ozbey AC, Umehara K, Stillhart C, Knops N, Augustijns P, Parrott NJ. Investigating Tacrolimus Disposition in Paediatric Patients with a Physiologically Based Pharmacokinetic Model Incorporating CYP3A4 Ontogeny, Mechanistic Absorption and Red Blood Cell Binding. Pharmaceutics. 2023; 15(9):2231. https://doi.org/10.3390/pharmaceutics15092231
Chicago/Turabian StyleVan der Veken, Matthias, Joachim Brouwers, Agustos Cetin Ozbey, Kenichi Umehara, Cordula Stillhart, Noël Knops, Patrick Augustijns, and Neil John Parrott. 2023. "Investigating Tacrolimus Disposition in Paediatric Patients with a Physiologically Based Pharmacokinetic Model Incorporating CYP3A4 Ontogeny, Mechanistic Absorption and Red Blood Cell Binding" Pharmaceutics 15, no. 9: 2231. https://doi.org/10.3390/pharmaceutics15092231
APA StyleVan der Veken, M., Brouwers, J., Ozbey, A. C., Umehara, K., Stillhart, C., Knops, N., Augustijns, P., & Parrott, N. J. (2023). Investigating Tacrolimus Disposition in Paediatric Patients with a Physiologically Based Pharmacokinetic Model Incorporating CYP3A4 Ontogeny, Mechanistic Absorption and Red Blood Cell Binding. Pharmaceutics, 15(9), 2231. https://doi.org/10.3390/pharmaceutics15092231







