Newly Developed Semi-Solid Formulations Containing Mellilotus officinalis Extract: Characterization, Assessment of Stability, Safety, and Anti-Inflammatory Activity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Plant Materials and Extract Preparation
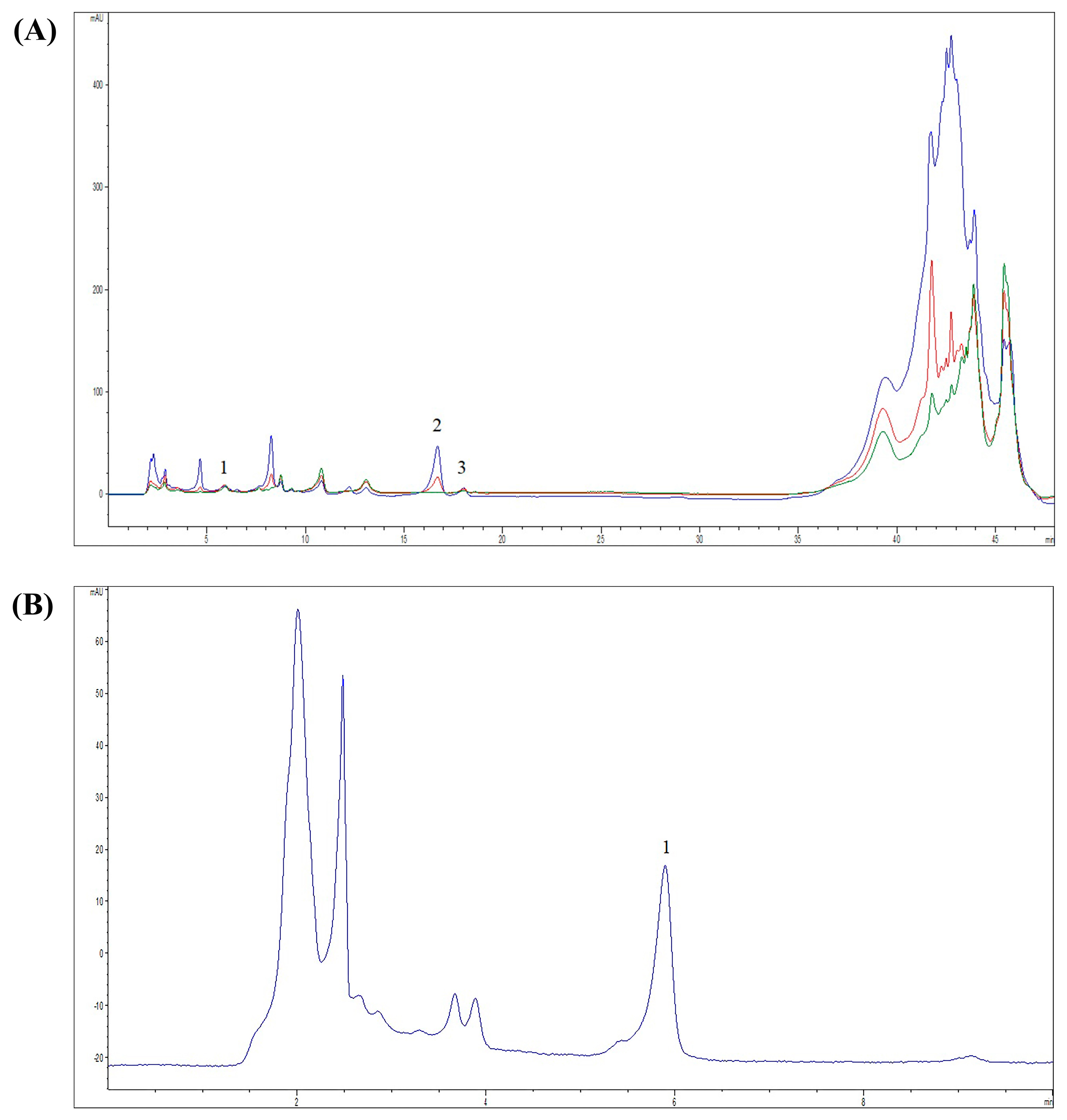
2.2. Chemical Characterization of M. officinalis Extract
2.3. Formulation of Semi-Solid Products: Gel and Cream
2.4. Assessment of Physical Properties of Gel and Cream Containing M. officinalis Extract
2.4.1. Determination of Organoleptic Properties
2.4.2. Determination of the pH Values
2.4.3. Determination of the Electrical Conductivity
2.4.4. Assessment of Long-Term Stability of the M. officinalis Extract-Based Formulations
2.4.5. Centrifugation Test
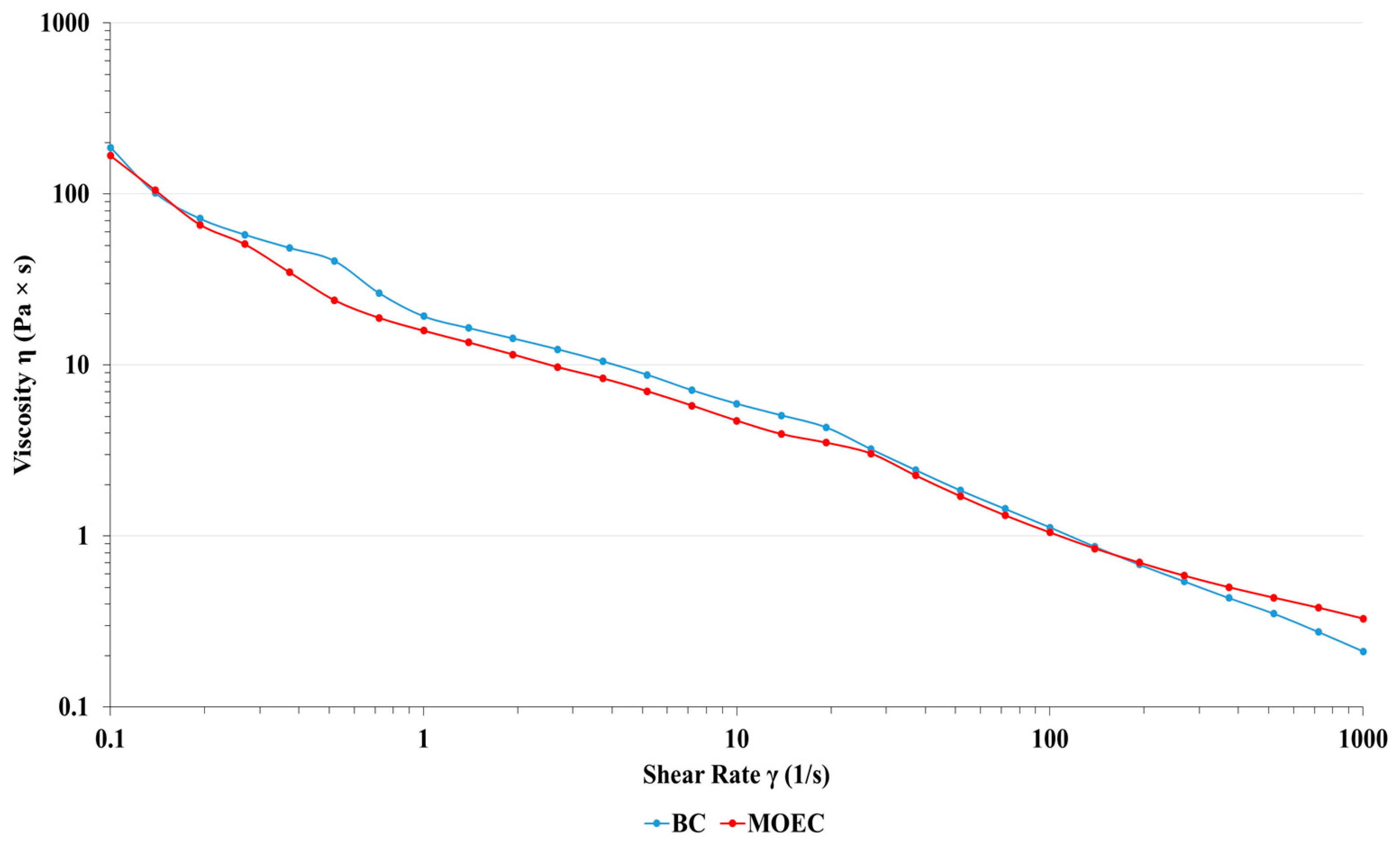
2.4.6. Rheological Characterization of Semi-Solid Formulations
2.5. In Vivo Experiments
2.5.1. Ethical Statement
2.5.2. Animals
2.5.3. Acute Dermal Irritation of Semi-Solid Formulations with M. officinalis Extract
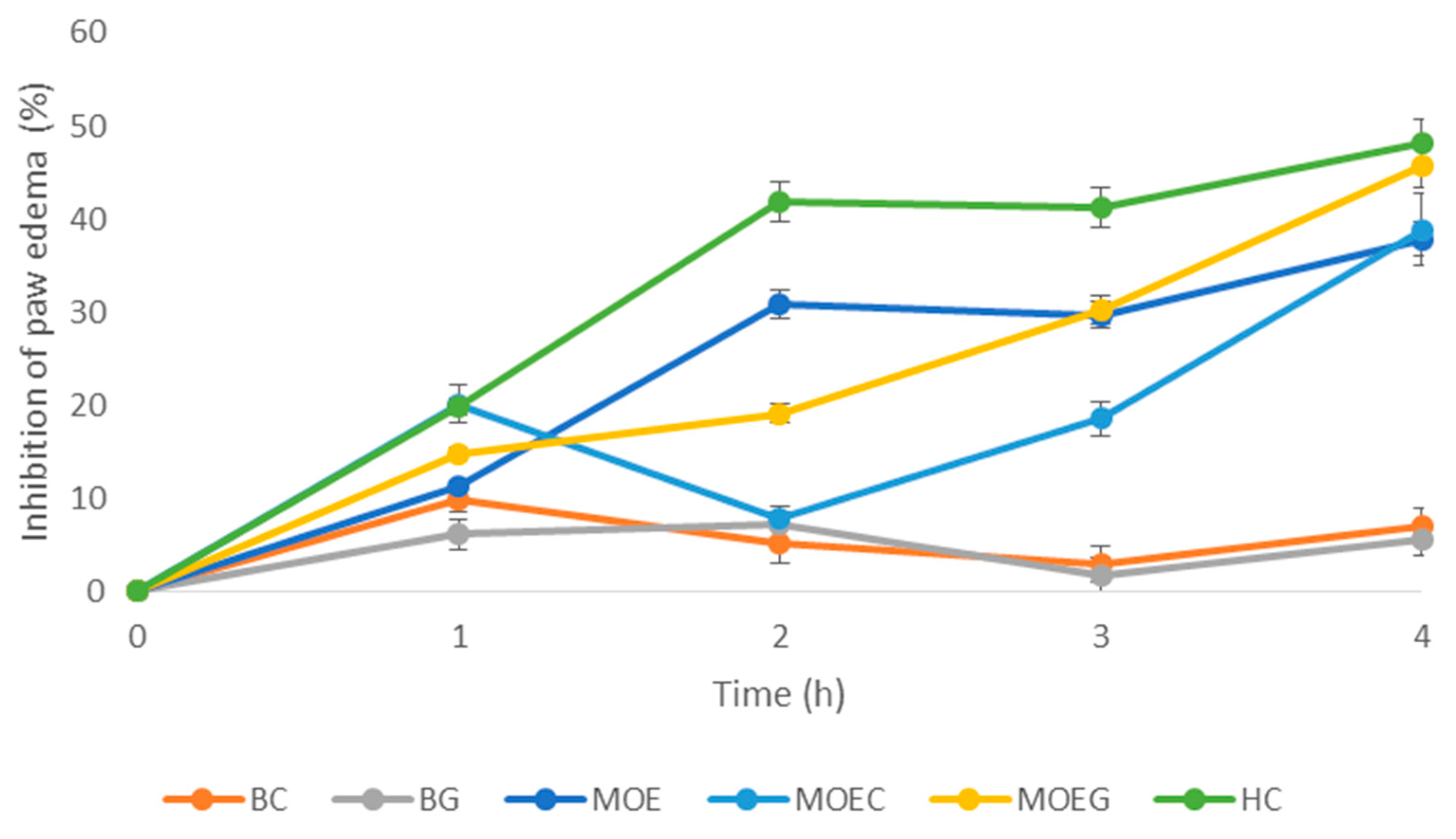
2.5.4. Anti-Inflammatory Effects of Semi-Solid Formulations with M. officinalis Extract in an Animal Model
2.6. Statistical Analyses
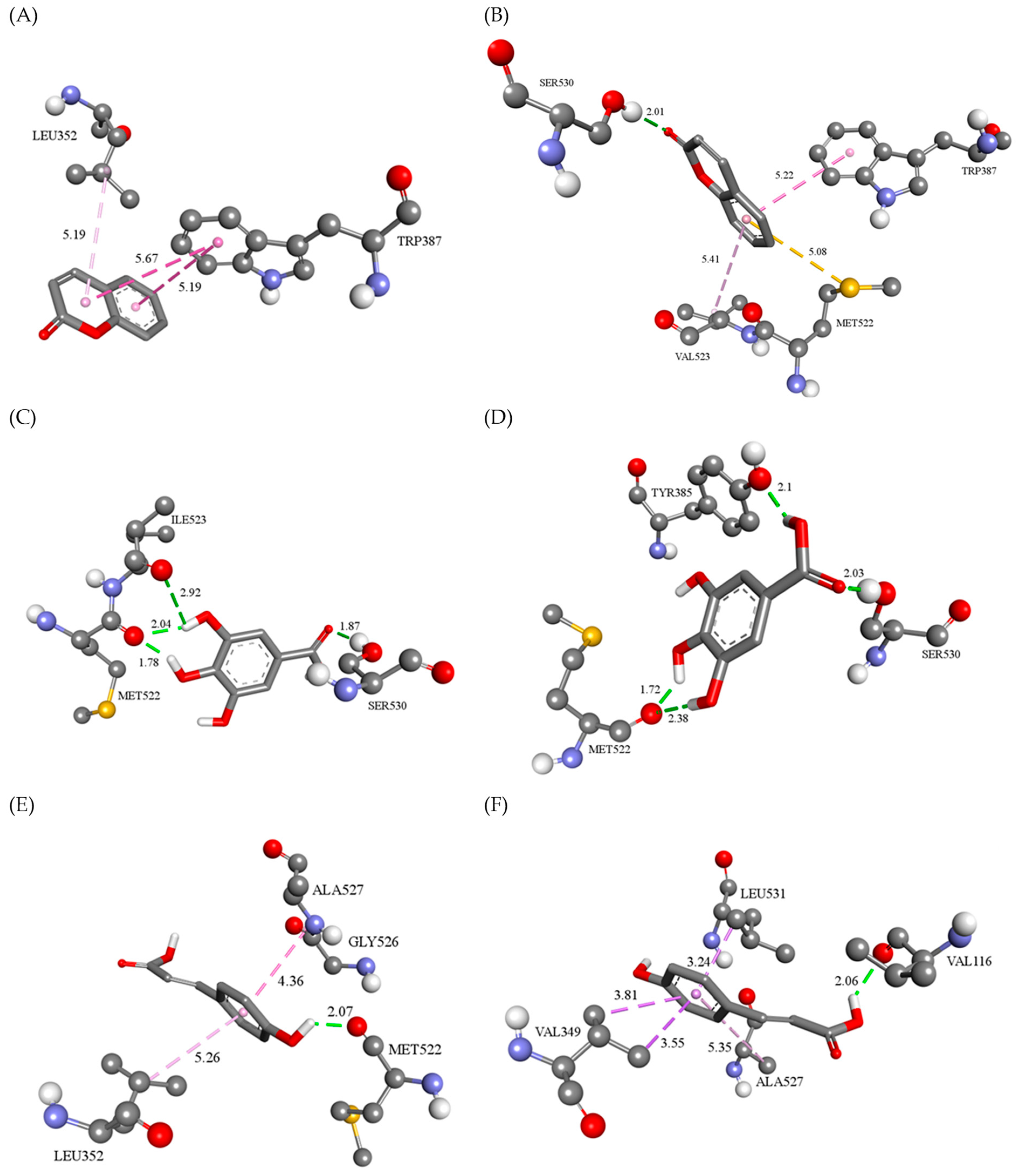
2.7. In Silico Studies of Anti-Inflammatory Effects of the Most Abundant Compounds from M. officinalis Extract
2.7.1. Molecular Docking Study
2.7.2. Molecular Dynamics Study
3. Results and Discussion
3.1. Chemical Composition of M. officinalis Extract
3.2. Physicochemical Characterization of M. officinalis Extract-Based Formulations
3.2.1. Organoleptic Characteristics and Physical Appearance of the Formulations
3.2.2. pH Values and Electrical Conductivity of the Formulations
3.2.3. Centrifugation Test
3.2.4. Rheological Characterization
3.3. Acute Dermal Toxicity of the M. officinalis-Based Formulations
3.4. Anti-Inflammatory Activity of M. officinalis-Based Formulations in a Rat Model
3.5. In Silico Assessment of Anti-Inflammatory Activity of the Major Compounds from M. officinalis Extract
3.5.1. Molecular Docking Analysis
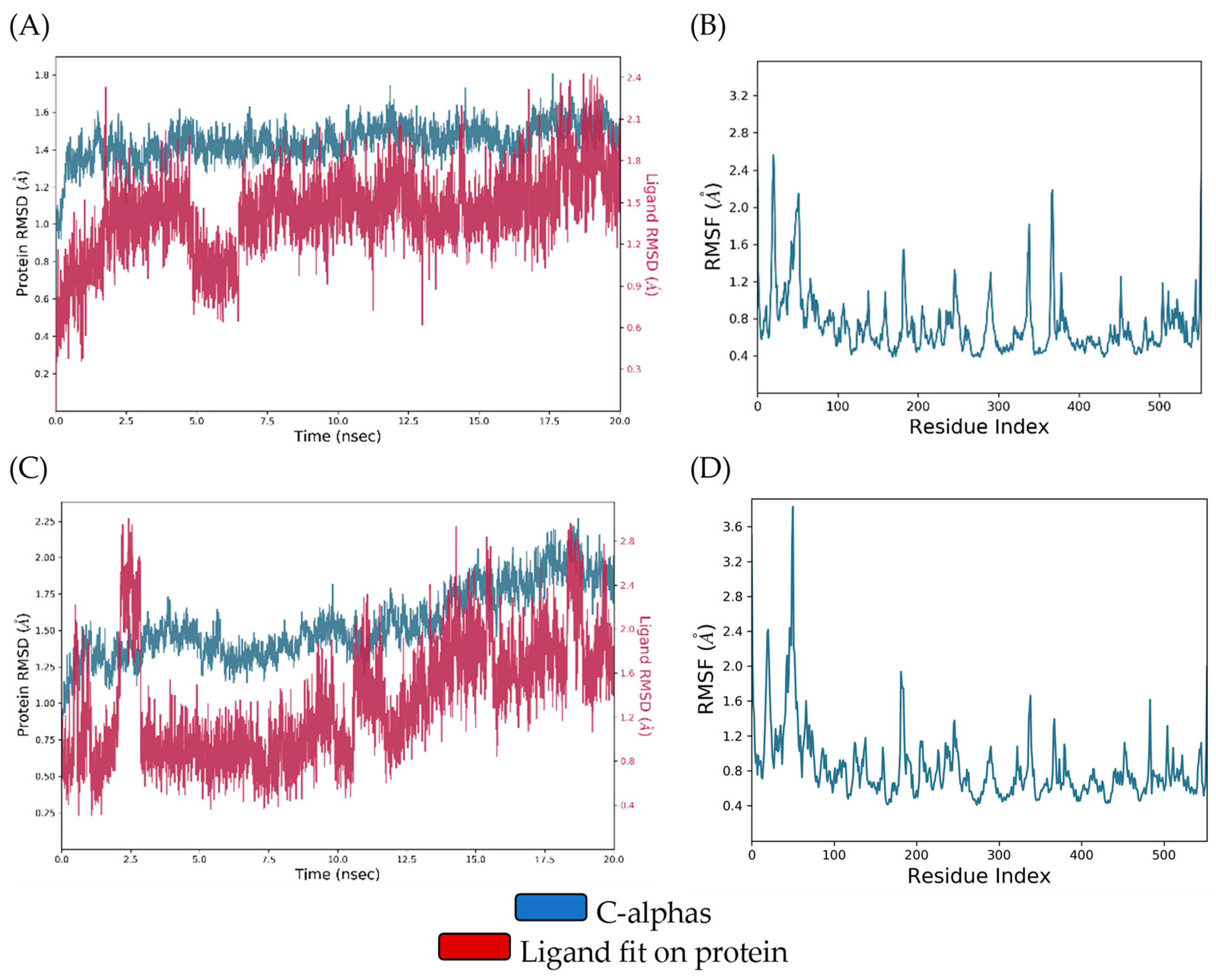
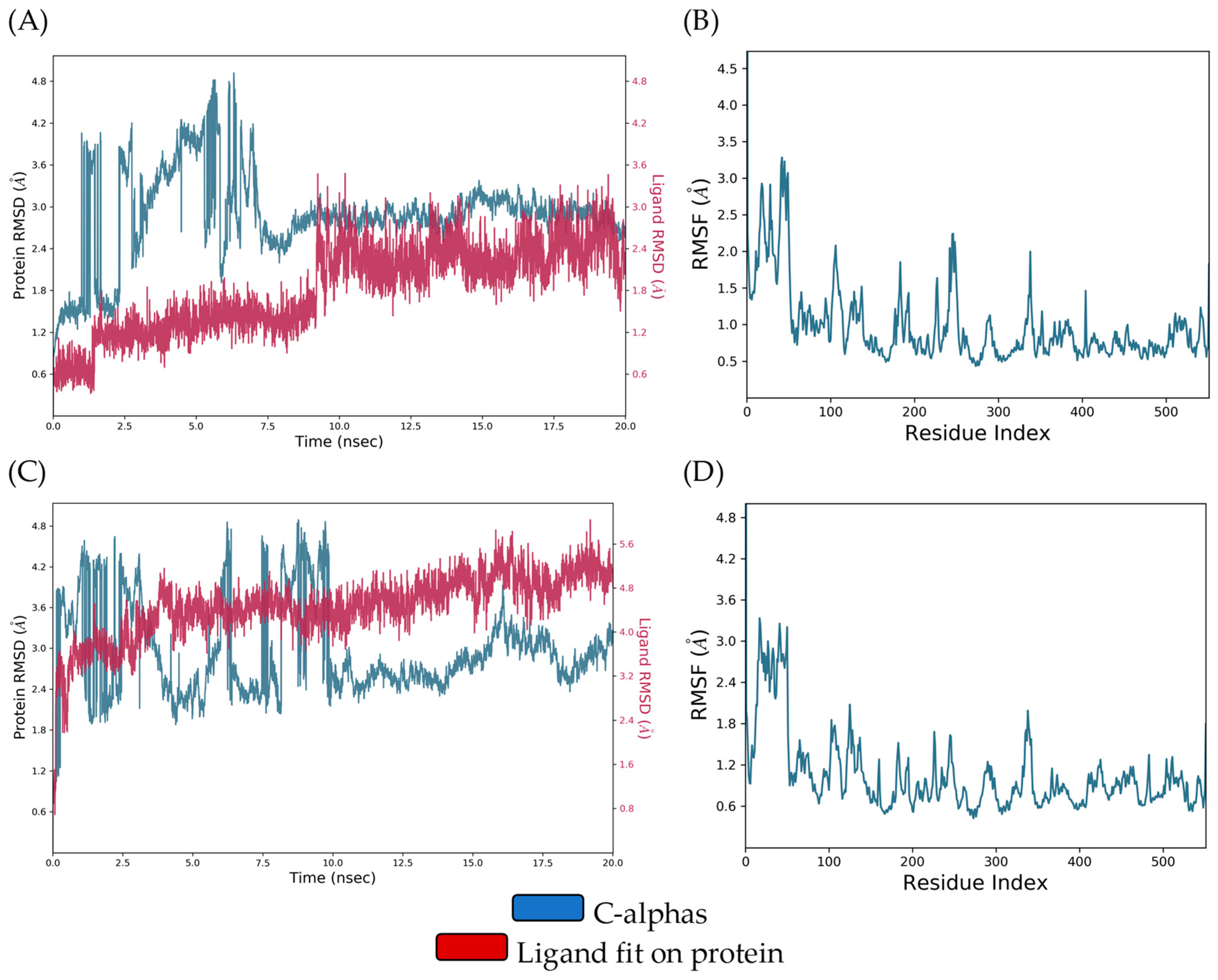
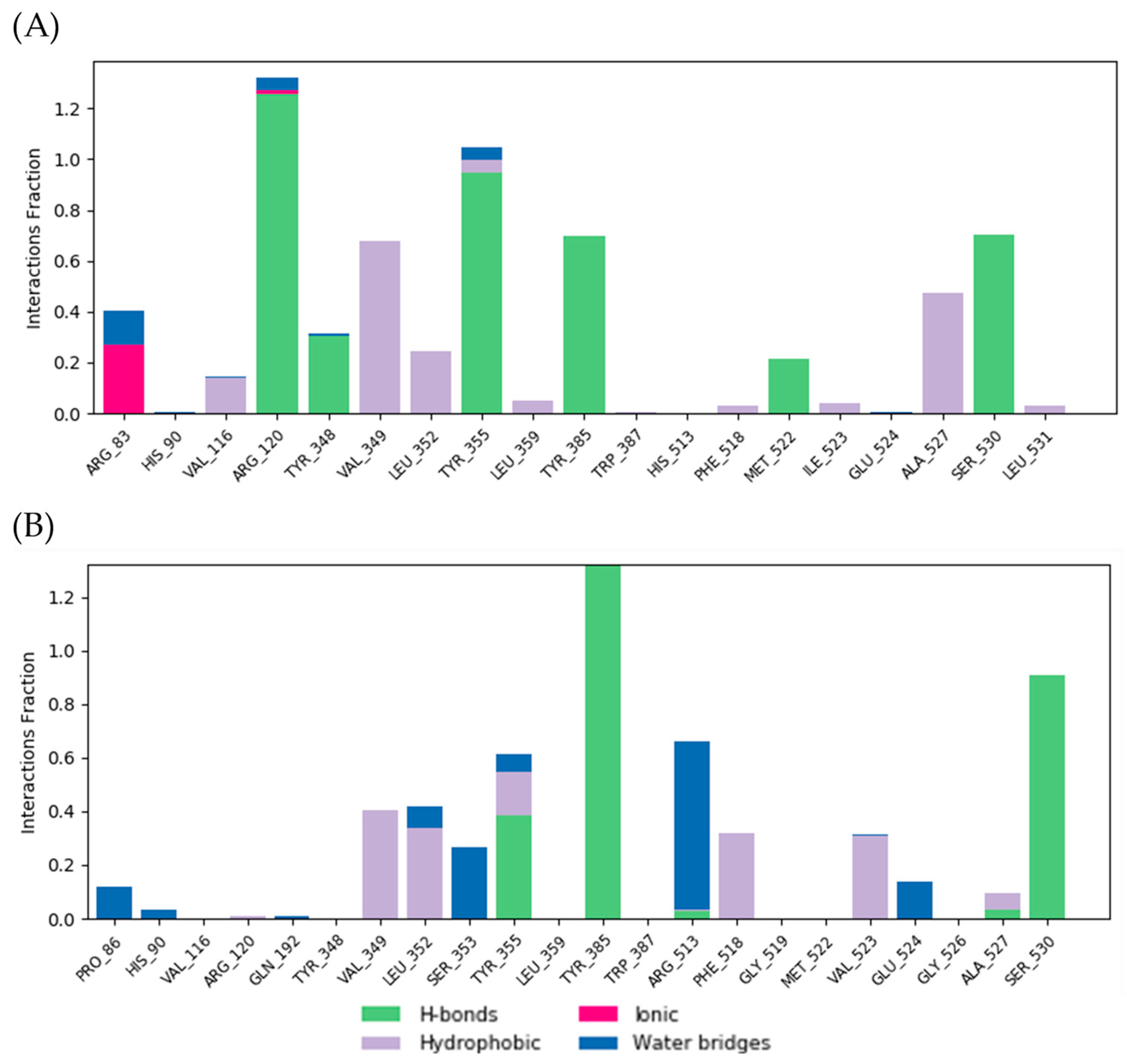
3.5.2. Molecular Dynamics Analysis and MM/GBSA Calculation
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Soto, M.L.; Parada, M.; Falqué, E.; Domínguez, H. Personal-Care Products Formulated with Natural Antioxidant Extracts. Cosmetics 2018, 5, 13. [Google Scholar] [CrossRef]
- Petkovic, A.; Jakovljevic, V.; Tomovic, M.; Jeremic, J.; Ristic, G.; Bradic, J. Improving Oxidative Stability of Cosmetic Emulsions with Plant Extracts: Current Status and Potential. J. Cosmet. Sci. 2021, 72, 189–199. [Google Scholar] [PubMed]
- Paun, G.; Neagu, E.; Albu, C.; Savin, S.; Radu, G.L. In Vitro Evaluation of Antidiabetic and Anti-Inflammatory Activities of Polyphenolic-Rich Extracts from Anchusa officinalis and Melilotus officinalis. ACS Omega 2020, 5, 13014–13022. [Google Scholar] [CrossRef]
- Hänsel, R.; Rimpler, H.; Keller, K.; Schneider, G.; Abel, G.; Bader, G.; Baumann, T.; Bertram, B.; Beyer, G.; Bodesheim, U.; et al. Hagers Handbuch der Pharmazeutischen Praxis; Springer: Berlin/Heidelberg, Germany, 1994. [Google Scholar] [CrossRef]
- Zhang, J.; Di, H.; Luo, K.; Jahufer, Z.; Wu, F.; Duan, Z.; Stewart, A.; Yan, Z.; Wang, Y. Coumarin Content, Morphological Variation, and Molecular Phylogenetics of Melilotus. Molecules 2018, 23, 810. [Google Scholar] [CrossRef]
- Liu, Y.T.; Gong, P.H.; Xiao, F.Q.; Shao, S.; Zhao, D.Q.; Yan, M.M.; Yang, X.W. Chemical Constituents and Antioxidant, Anti-Inflammatory and Anti-Tumor Activities of Melilotus officinalis (Linn.) Pall. Molecules 2018, 23, 271. [Google Scholar] [CrossRef]
- Pleşca-Manea, L.; Pârvu, A.E.; Pârvu, M.; Taămaş, M.; Buia, R.; Puia, M. Effects of Melilotus officinalis on acute inflammation. Phytother. Res. 2002, 16, 316–319. [Google Scholar] [CrossRef]
- Ma, Z.; Du, B.; Li, J.; Yang, Y.; Zhu, F. An Insight into Anti-Inflammatory Activities and Inflammation Related Diseases of Anthocyanins: A Review of Both In Vivo and In Vitro Investigations. Int. J. Mol. Sci. 2021, 22, 11076. [Google Scholar] [CrossRef]
- Draginic, N.; Andjic, M.; Jeremic, J.; Zivkovic, V.; Kocovic, A.; Tomovic, M.; Bozin, B.; Kladar, N.; Bolevich, S.; Jakovljevic, V.; et al. Anti-inflammatory and Antioxidant Effects of Melissa officinalis Extracts: A Comparative Study. Iran. J. Pharm. Res. 2022, 21, e126561. [Google Scholar] [CrossRef]
- Celeghini, R.; Vilegas, J.H.; Lanças, F.M. Extraction and quantitative HPLC analysis of coumarin in hydroalcoholic extracts of Mikania glomerata Spreng: (“guaco”) leaves. J. Braz. Chem. Soc. 2001, 12, 706–709. [Google Scholar] [CrossRef]
- Nikolic, M.; Andjic, M.; Bradic, J.; Kocovic, A.; Tomovic, M.; Samanovic, A.M.; Jakovljevic, V.; Veselinovic, M.; Capo, I.; Krstonosic, V.; et al. Topical Application of Siberian Pine Essential Oil Formulations Enhance Diabetic Wound Healing. Pharmaceutics 2023, 15, 2437. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.X.; Alexander, K.S.; Baki, G. Formulation and Evaluation of Antibacterial Creams and Gels Containing Metal Ions for Topical Application. J. Pharm. 2016, 2016, 5754349. [Google Scholar] [CrossRef]
- Sakiroff, L.M.; Chennell, P.; Yessaad, M.; Pereira, B.; Bouattour, Y.; Sautou, V. Evaluation of color changes during stability studies using spectrophotometric chromaticity measurements versus visual examination. Sci. Rep. 2022, 12, 8959. [Google Scholar] [CrossRef]
- Ma, B.; Yuan, J.; Chen, S.; Huang, K.; Wang, Q.; Ma, J.; Lin, R.; Zhang, L.; Zhou, Y.; Wang, T.; et al. Topical application of temperature-sensitive caerin 1.1 and 1.9 gel inhibits TC-1 tumor growth in mice. Am. J. Transl. Res. 2020, 12, 191–202. [Google Scholar]
- Tadić, V.M.; Žugić, A.; Martinović, M.; Stanković, M.; Maksimović, S.; Frank, A.; Nešić, I. Enhanced Skin Performance of Emulgel vs. Cream as Systems for Topical Delivery of Herbal Actives (Immortelle Extract and Hemp Oil). Pharmaceutics 2021, 13, 1919. [Google Scholar] [CrossRef]
- Dragicevic, N.; Krajisnik, D.; Milic, J.; Fahr, A.; Maibach, H. Development of hydrophilic gels containing coenzyme Q10-loaded liposomes: Characterization, stability and rheology measurements. Drug Dev. Ind. Pharm. 2019, 45, 43–54. [Google Scholar] [CrossRef]
- Stolić Jovanović, A.; Martinović, M.; Žugić, A.; Nešić, I.; Tosti, T.; Blagojević, S.; Tadić, V.M. Derivatives of L-Ascorbic Acid in Emulgel: Development and Comprehensive Evaluation of the Topical Delivery System. Pharmaceutics 2023, 15, 813. [Google Scholar] [CrossRef]
- Korhonen, M.; Hellen, L.; Hirvonen, J.; Yliruusi, J. Determination of optimal combination of surfactants in creams using rheology measurements. Int. J. Pharm. 2005, 197, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Andjić, M.; Draginić, N.; Kočović, A.; Jeremić, J.; Vučićević, K.; Jeremić, N.; Krstonošić, V.; Božin, B.; Kladar, N.; Čapo, I.; et al. Immortelle essential oil-based ointment improves wound healing in a diabetic rat model. Biomed. Pharmacother. 2022, 150, 112941. [Google Scholar] [CrossRef]
- Nedeljković, N.; Dobričić, V.; Bošković, J.; Vesović, M.; Bradić, J.; Anđić, M.; Kočović, A.; Jeremić, N.; Novaković, J.; Jakovljević, V.; et al. Synthesis and Investigation of Anti-Inflammatory Activity of New Thiourea Derivatives of Naproxen. Pharmaceuticals 2023, 16, 666. [Google Scholar] [CrossRef] [PubMed]
- Morris, G.M.; Huey, R.; Lindstrom, W.; Sanner, M.F.; Belew, R.K.; Goodsell, D.S.; Olson, A.J. AutoDock4 and AutoDockTools4: Automated docking with selective receptor flexibility. J. Comput. Chem. 2009, 30, 2785–2791. [Google Scholar] [CrossRef]
- Sidhu, R.S.; Lee, J.Y.; Yuan, C.; Smith, W.L. Comparison of cyclooxygenase-1 crystal structures: Cross-talk between monomers comprising cyclooxygenase-1 homodimers. Biochemistry 2010, 49, 7069–7079. [Google Scholar] [CrossRef]
- Rowlinson, S.W.; Kiefer, J.R.; Prusakiewicz, J.J.; Pawlitz, J.L.; Kozak, K.R.; Kalgutkar, A.S.; Stallings, W.C.; Kurumbail, R.G.; Marnett, L.J. A novel mechanism of cyclooxygenase-2 inhibition involving interactions with Ser-530 and Tyr-385. J. Biol. Chem. 2003, 278, 45763–45769. [Google Scholar] [CrossRef]
- BIOVIA. Dassault Systèmes, Discovery Studio Visualizer; 21.1.0.20298; Dassault Systèmes: San Diego, CA, USA, 2021. [Google Scholar]
- Schrödinger, L.; DeLano, W. PyMOL. Available online: https://www.pymol.org/pymol (accessed on 25 January 2023).
- Schrödinger Release 2020-4: Desmond Molecular Dynamics System; D. E. Shaw Research: New York, NY, USA, 2020.
- Harder, E.; Damm, W.; Maple, J.; Wu, C.; Reboul, M.; Xiang, J.Y.; Wang, L.; Lupyan, D.; Dahlgren, M.K.; Knight, J.L.; et al. OPLS3: A force field providing broad coverage of drug-like small molecules and proteins. J. Chem. Theory Comput. 2016, 12, 281–296. [Google Scholar] [CrossRef]
- Jorgensen, W.L.; Chandrasekhar, J.; Madura, J.D.; Impey, R.W.; Klein, M.L. Comparison of simple potential functions for simulating liquid water. J. Chem. Phys. 1983, 79, 926–935. [Google Scholar] [CrossRef]
- Genheden, S.; Ryde, U. The MM/PBSA and MM/GBSA methods to estimate ligand-binding affinities. Expert. Opin. Drug. Discov. 2015, 10, 449–461. [Google Scholar] [CrossRef]
- Jasicka-Misiak, I.; Makowicz, E.; Stanek, N. Polish Yellow Sweet Clover (Melilotus officinalis L.) Honey, Chromatogaphic Fingerprints, and Chemical Markers. Molecules 2017, 22, 138. [Google Scholar] [CrossRef]
- Limpongsa, E.; Tabboon, P.; Tuntiyasawasdikul, S.; Sripanidkulchai, B.; Pongjanyakul, T.; Jaipakdee, N. Formulation and In Vitro Evaluation of Mucoadhesive Sustained Release Gels of Phytoestrogen Diarylheptanoids from Curcuma comosa for Vaginal Delivery. Pharmaceutics 2023, 15, 264. [Google Scholar] [CrossRef]
- Agarwala, S. Electrically Conducting Hydrogels for Health care: Concept, Fabrication Methods, and Applications. Int. J. Bioprint 2020, 6, 273. [Google Scholar] [CrossRef]
- García-Villegas, A.; Fernández-Ochoa, Á.; Rojas-García, A.; Alañón, M.E.; Arráez-Román, D.; Cádiz-Gurrea, M.D.L.L.; Segura-Carretero, A. The Potential of Mangifera indica L. Peel Extract to Be Revalued in Cosmetic Applications. Antioxidants 2023, 12, 1892. [Google Scholar] [CrossRef]
- Xavier-Santos, J.B.; Passos, J.G.R.; Gomes, J.A.S.; Cruz, J.V.C.; Alves, J.S.F.; Garcia, V.B.; da Silva, R.M.; Lopes, N.P.; Araujo-Junior, R.F.; Zucolotto, S.M.; et al. Topical gel containing phenolic-rich extract from Ipomoea pes-capre leaf (Convolvulaceae) has anti-inflammatory, wound healing, and antiophidic properties. Biomed. Pharmacother. 2022, 149, 112921. [Google Scholar] [CrossRef]
- Opatha, S.A.T.; Titapiwatanakun, V.; Boonpisutiinant, K.; Chutoprapat, R. Preparation, Characterization and Permeation Study of Topical Gel Loaded with Transfersomes Containing Asiatic Acid. Molecules 2022, 27, 4865. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, L.M.; Sari, M.H.M.; Azambuja, J.H.; da Silveira, E.F.; Cervi, V.F.; Marchiori, M.C.L.; Maria-Engler, S.S.; Wink, M.R.; Azevedo, J.G.; Nogueira, C.W.; et al. Xanthan gum-based hydrogel containing nanocapsules for cutaneous diphenyl diselenide delivery in melanoma therapy. Investig. New Drug 2020, 38, 662–674. [Google Scholar] [CrossRef]
- Mansouri, M.T.; Hemmati, A.A.; Naghizadeh, B.; Mard, S.A.; Rezaie, A.; Ghorbanzadeh, B. A study of the mechanisms underlying the anti-inflammatory effect of ellagic acid in carrageenan-induced paw edema in rats. Indian. J. Pharmacol. 2015, 47, 292–298. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, X.; Retyunskiy, V.; Qiao, S.; Zhao, Y.; Tzeng, C.M. Alloferon-1 ameliorates acute inflammatory responses in λ-carrageenan-induced paw edema in mice. Sci. Rep. 2022, 12, 16689. [Google Scholar] [CrossRef]
- Amdekar, S.; Roy, P.; Singh, V.; Kumar, A.; Singh, R.; Sharma, P. Anti-inflammatory activity of lactobacillus on carrageenan-induced paw edema in male wistar rats. Int. J. Inflam. 2012, 2012, 752015. [Google Scholar] [CrossRef] [PubMed]
- Pashmforosh, M.; Rajabi Vardanjani, H.; Rajabi Vardanjani, H.; Pashmforosh, M.; Khodayar, M.J. Topical Anti-Inflammatory and Analgesic Activities of Citrullus colocynthis Extract Cream in Rats. Medicina 2018, 54, 51. [Google Scholar] [CrossRef] [PubMed]
- Jurca, T.; Józsa, L.; Suciu, R.; Pallag, A.; Marian, E.; Bácskay, I.; Mureșan, M.; Stan, R.L.; Cevei, M.; Cioară, F.; et al. Formulation of Topical Dosage Forms Containing Synthetic and Natural Anti-Inflammatory Agents for the Treatment of Rheumatoid Arthritis. Molecules 2020, 26, 24. [Google Scholar] [CrossRef] [PubMed]
- Maroon, J.C.; Bost, J.W.; Maroon, A. Natural anti-inflammatory agents for pain relief. Surg. Neurol. Int. 2010, 13, 1–80. [Google Scholar] [CrossRef]
- Hwang, J.; Lio, P.A. Topical corticosteroid withdrawal (‘steroid addiction’): An update of a systematic review. J. Dermatolog Treat. 2022, 33, 1293–1298. [Google Scholar] [CrossRef]
- Alsaif, N.A.; Bhat, M.A.; Al-Omar, M.A.; Al-Tuwajiri, H.M.; Naglah, A.M.; Al-Dhfyan, A. Synthesis of novel diclofenac hydrazones: Molecular docking, anti-inflammatory, analgesic, and ulcerogenic activity. J. Chem. 2020, 2020, 1–12. [Google Scholar] [CrossRef]
- Vyshnevska, L.; Severina, H.I.; Prokopenko, Y.; Shmalko, A. Molecular docking investigation of anti-inflammatory herbal compounds as potential LOX-5 and COX-2 inhibitors. Pharmacia 2022, 69, 733–744. [Google Scholar] [CrossRef]





| Formulations | Components | Quantity (g) |
|---|---|---|
| MOEG | M. officinalis extract | 2 |
| Carbomer 940 | 0.5 | |
| Propylene glycol | 10 | |
| Triethanolamine | q.s. | |
| Water | ad 100 | |
| MOEC | Stearic acid | 10 |
| Cetyl alcohol | 2 | |
| Cetearyl alcohol | 2 | |
| Polysorbate 60 | 2 | |
| Sweet almond oil | 4 | |
| Glycerol | 3 | |
| Phenoxyethanol | 0.8 | |
| Triethanolamine | q.s. | |
| M. officinalis extract | 2 | |
| Water | ad 100 |
| Compound | Retention Time (tR (min)) | Concentration (mg/g DE) | Uncertainty (U) |
|---|---|---|---|
| GALA * | 8.27 | 1.31 | 0.20 |
| COUMA * | 16.67 | 3.18 | 0.32 |
| QUE * | 18.02 | 0.36 | 0.03 |
| COUM # | 5.9 | 10.81 | 0.86 |
| MOEC | MOEG | |||||
|---|---|---|---|---|---|---|
| Parameters | 7 Day | 60 Days | 180 Days | 1 Day | 60 Days | 180 Days |
| Color | Light brown | Light brown | Light brown | Brownish | Brownish | Brownish |
| Odor | Characteristic odor of the extract | Characteristic odor of the extract | Characteristic odor of the extract | Characteristic odor of the extract | Characteristic odor of the extract | Characteristic odor of the extract |
| Consistency | Semi-solid | Semi-solid | Semi-solid | Semi-solid | Semi-solid | Semi-solid |
| Homogeneity | No phase separation | No phase separation | No phase separation | No phase separation | No phase separation | No phase separation |
| pH | Electrical Conductivity (µS/cm) | ||
|---|---|---|---|
| MOEC | 0 day | 5.98 ± 0.09 | 41.2 ± 0.23 |
| 60 days | 5.52 ± 0.11 | 40.8 ± 0.28 | |
| 180 days | 5.15 ± 0.15 * | 39.5 ± 0.21 | |
| MOEG | 0 day | 7.42 ± 0.10 | 177.6 ± 1.83 |
| 60 days | 7.32 ± 0.09 | 174.5 ± 1.26 | |
| 180 days | 6.88 ± 0.14 * | 170.7 ± 1.68 |
| Rat Paw Thickness (mm) (% of Inhibition) | |||||
|---|---|---|---|---|---|
| Groups | 0 h | 1 h | 2 h | 3 h | 4 h |
| BC | 1.45 ± 0.31 | 2.82 ± 0.40 (9.90%) | 5.22 ± 0.33 (5.09%) | 4.97 ± 0.40 (2.93%) | 4.67 ± 0.42 (6.97%) |
| BG | 1.53 ± 0.44 | 2.94 ± 0.60 (6.07%) | 5.11 ± 0.54 (7.09%) | 5.03 ± 0.51 (1.75%) | 4.74 ± 0.38 (5.57%) |
| MOE | 1.56 ± 0.02 | 2.78 ± 0.23 (11.80%) | 3.80 ± 0.46 (30.90%) * | 3.60 ± 0.31 (29.69%) * | 3.12 ± 0.23 (37.84%) * |
| MOEC | 1.76 ± 0.17 | 2.5 ± 0.13 (20.12%) | 5.07 ± 0.29 (7.81%) | 4.17 ± 0.35 (18.55%) * | 3.07 ± 0.21 (38.84%) * |
| MOEG | 1.72 ± 0.06 | 2.67 ± 0.20 (14.69%) | 4.45 ± 0.87 (19.09%) | 3.57 ± 0.76 (30.27%) * | 2.73 ± 0.16 (45.62%) * |
| HC | 1.64 ± 0.23 | 2.51 ± 0.35 (19.80%) | 3.20 ± 0.18 (41.81%) * | 3.01 ± 0.27 (41.21%) * | 2.60 ± 0.13 (48.21%) * |
| CTRL | 1.51 ± 0.16 | 3.13 ± 0.10 | 5.50 ± 0.17 | 5.12 ± 0.12 | 5.02 ± 0.42 |
| Complex | ΔGbind (kJ/mol) | Ki (µM) | ΔGIntermol. Energy (vdw + Hbond + desolv) (kJ/mol) | ΔGelec (kJ/mol) | ΔGFinal Intermol. Energy (kJ/mol) | ΔGtotal (kJ/mol) | ΔGtor (kJ/mol) | ΔGunb (kJ/mol) | LE * |
|---|---|---|---|---|---|---|---|---|---|
| DIC-COX-1 | −33.01 | 1.64 | −36.15 | −1.46 | −37.61 | −3.68 | 4.60 | −3.68 | −1.90 |
| DIC-COX-2 | −31.04 | 3.66 | −35.40 | −0.25 | −35.60 | −3.22 | 4.60 | −3.22 | −1.63 |
| COUM-COX-1 | −23.68 | 70.20 | −3.51 | −0.17 | −23.68 | 0 | 0 | 0 | −2.15 |
| COUM-COX-2 | −23.22 | 84.60 | −22.97 | −0.25 | −23.22 | 0 | 0 | 0 | −2.11 |
| COUMA-COX-1 | −19.29 | 416.74 | −23.76 | −0.13 | −23.89 | −0.29 | 4.60 | −0.29 | −1.61 |
| COUMA-COX-2 | −19.37 | 404.73 | −19.87 | −0.98 | −23.97 | −0.29 | 4.60 | −0.29 | −1.61 |
| GALA-COX-1 | −17.32 | 930.56 | −21.42 | −1.63 | −23.05 | −6.02 | 5.73 | −6.02 | −1.44 |
| GALA-COX-2 | −15.98 | 1570.00 | −20.83 | −0.92 | −21.75 | −5.90 | 5.73 | −5.90 | −1.33 |
| QUE-COX-1 | −28.37 | 10.67 | −34.56 | −0.71 | −35.27 | −9.95 | 6.9 | −9.95 | −1.29 |
| QUE-COX-2 | −29.62 | 6.43 | −35.73 | −0.79 | −36.52 | −10.00 | 6.9 | −10.00 | −1.35 |
| Target | Ligand | MM/GBSA ΔGavg ± SD * (kJ/mol) |
|---|---|---|
| COX-1 | DIC | −229.4443 ± 18.1586 |
| QUE | −168.2767 ± 22.0497 | |
| COX-2 | DIC | −172.9281 ± 10.4182 |
| QUE | −229.3945 ± 20.5434 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bradic, J.; Petrovic, A.; Nikolic, M.; Nedeljkovic, N.; Andjic, M.; Kladar, N.; Bolevich, S.; Jakovljevic, V.; Kocovic, A. Newly Developed Semi-Solid Formulations Containing Mellilotus officinalis Extract: Characterization, Assessment of Stability, Safety, and Anti-Inflammatory Activity. Pharmaceutics 2024, 16, 1003. https://doi.org/10.3390/pharmaceutics16081003
Bradic J, Petrovic A, Nikolic M, Nedeljkovic N, Andjic M, Kladar N, Bolevich S, Jakovljevic V, Kocovic A. Newly Developed Semi-Solid Formulations Containing Mellilotus officinalis Extract: Characterization, Assessment of Stability, Safety, and Anti-Inflammatory Activity. Pharmaceutics. 2024; 16(8):1003. https://doi.org/10.3390/pharmaceutics16081003
Chicago/Turabian StyleBradic, Jovana, Anica Petrovic, Milos Nikolic, Nikola Nedeljkovic, Marijana Andjic, Nebojsa Kladar, Stefani Bolevich, Vladimir Jakovljevic, and Aleksandar Kocovic. 2024. "Newly Developed Semi-Solid Formulations Containing Mellilotus officinalis Extract: Characterization, Assessment of Stability, Safety, and Anti-Inflammatory Activity" Pharmaceutics 16, no. 8: 1003. https://doi.org/10.3390/pharmaceutics16081003





