Abstract
(1) Context: Cancer triggers significant changes in family dynamics. It is noteworthy that coping and problem-solving skills, particularly in situations involving cancer in children and adolescents, have not been adequately explored in the context of family adaptation. This study aims to analyze the effectiveness of family interventions in coping to improve problem-solving skills in parents and/or caregivers of children and adolescents during and after oncological treatment. (2) Methods: This is a scoping review following the recommendations of the Joanna Briggs Institute and the Systematic Reviews and Meta-Analyses Extension for Scoping Review (PRISMA-ScR), from 2014 to 2024, in the databases LILACS, CINAHL, SCOPUS, Web of Science, and PUBMED. (3) Results: Forty-five studies were eligible. Coping strategies were categorized as follows: (1) positive attitudes (including a sense of courage and hope, family support to enhance resilience, and future planning), (2) caregiver empowerment (involving acceptance of diagnosis, emotional distancing, and coping through religiosity), and (3) communication skills (encompassing professional communication, horizontal dialogue with healthcare teams, and sincere communication with friends and family). (4) Conclusions: Over time, families develop coping and problem-solving strategies that influence changes in family functioning patterns, aiding them in accepting, reinterpreting, and reframing ideas and feelings associated with neoplasia.
1. Introduction
Pediatric cancer encompasses a wide range of malignant neoplasms with distinct characteristics, including varied incidence, diverse origins, different treatment options, variable overall survival rates, and potential acute and late adverse effects resulting from therapeutic interventions [1,2]. These neoplastic entities share a common propensity for unregulated proliferation of atypical cells and can manifest in any region of the body in individuals during childhood or adolescence. It is noteworthy that the demographic group studied, as defined by the guidelines of the Brazilian Society of Pediatrics, comprises individuals aged 0 to 19 years [3,4].
Although childhood and adolescent cancers often receive less attention due to their lower incidence compared to prevalent types in adult and elderly populations [5], there has been a significant improvement in the overall survival trajectory of these patients over the last five decades. In 2021, the overall survival rate reached 80%, contrasting with about 30% in the 1960s. However, despite this progress, childhood and adolescent cancer remain the second leading cause of death in children aged 5 to 14 years, both globally and in Latin America and the Caribbean [6].
In the context of providing care to patients with specific therapeutic needs, it is crucial to consider the demands of this group and the challenges faced by their caregiving families. These demands require constant and comprehensive attention, often resulting in physical and emotional burden for caregivers [7,8]. This burden can manifest through symptoms such as fatigue, stress, anxiety, depression, and social isolation, negatively impacting not only the caregivers’ quality of life but also that of the patients under their care. Furthermore, burden can be understood as a condition in which family members struggle to adequately meet the diverse needs of the patient [9].
Research dedicated to analyzing resilience and adaptation in the context of chronic conditions has revealed that, despite significant challenges, families have the capacity to develop behaviors and mobilize resources that alter their dynamics, making situations more manageable and acceptable [9,10,11]. This phenomenon can contribute to strengthening both parents and the family unit. In this context, it is crucial for professionals to be attentive to circumstances that may hinder or impede adaptation, encouraging families to adopt strategies that allow them to effectively cope with stressful situations [12,13,14].
Efforts directed at both individual and familial levels can be undertaken to mitigate the demands associated with childhood and adolescent cancer and to seek resources to deal with these situations. This approach is aligned with the Resilience, Stress, Adjustment, and Family Adaptation Model, which views such efforts as coping strategies [15]. Family coping entails coordinating behaviors aimed at problem-solving, with complementary individual efforts from its members, potentially resulting in a balance between demands and resources, and consequently, a reduction in faced difficulties [16,17]. Thus, coping refers to the way individuals interact with stressors and challenges, triggering various mechanisms to identify resources that help them develop enduring skills to manage crisis situations [18,19].
Thus, coping aims to explain the potential of parents and family members to deal with crisis situations, promoting understanding of the factors related to family adjustment and adaptation [15]. Coping and problem-solving (PSC) are understood in this research as actions for change. Their function is to restore and contribute to the balance between demands and resources while simultaneously removing or reducing the difficulties involved in the stressful situation [15].
Furthermore, it is crucial to emphasize that the manifestation of cancer within the family nucleus causes significant changes in family dynamics, necessitating a reorganization involving the redefinition of roles and responsibilities. This restructuring is necessary to empower the family to provide support to the affected individual, ensuring the satisfaction of their basic human needs such as hygiene, nutrition, rest, as well as the provision of emotional and financial support. Consequently, the daily demands associated with patient care impose a considerable burden of responsibility on the caregiver, often leading them to neglect their own needs in favor of the patient’s. Such a situation frequently results in physical, social, psychological, and spiritual overload for the caregiver [10,14].
Furthermore, it is important to emphasize that the dimensions of coping and problem-solving in contexts related to the diagnosis of childhood cancer [20,21,22] have not yet been adequately explored within the scope of family adaptation. This gap highlights the importance of conducting the present research, aiming to fill this knowledge gap and provide valuable insights for a more comprehensive understanding of the challenges faced by families in this specific context.
Furthermore, it is worth noting that this investigation is based on evidence regarding a set of actions, efforts, and behaviors established by families, which make situations related to childhood and adolescent cancer more manageable. Identifying, understanding, and anticipating the resources that families can use to adapt to the conditions associated with this disease will significantly contribute to guiding nurses in providing care and making decisions related to managing these situations.
This scoping review aims to analyze the effectiveness of family interventions in coping to improve problem-solving skills in parents and/or caregivers of children and adolescents during and after oncological treatment.
2. Materials and Methods
2.1. Ethical Aspects
As this is a scoping review, which used publicly available data and did not involve human subjects, there was no need for approval from the Research Ethics Committee (CEP). However, it is important to note that the studies selected for the final sample were duly referenced [23].
2.2. Study Design
This is a scoping review, developed following the recommendations of the international guideline Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) [24] and the Joanna Briggs Institute (JBI), 2020 version Reviewers Manual [25,26], with a research protocol registered on the Open Science Framework (OSF) platform [27]. It is noteworthy that a scoping review represents a novel approach to systematic literature reviews, with a growth in both national and international publications over the last decade. The method allows for examining evidence, existing gaps, and key concepts surrounding a specific study object [25,26]. During the construction of this study, the following structuring of steps was opted for, as conceptualized by Arksey and O’Malley: (1) establishment of the research question; (2) identification of relevant studies in national and international literature; (3) analysis and extraction of studies; (4) data organization; (5) compilation, synthesis, interpretation, and reporting of results [28].
2.3. Methodological Procedure
It is worth noting that, initially, a search was conducted in the scientific literature to identify reviews with a similar scope of research. Platforms such as the International Prospective Register of Systematic Reviews (PROSPERO), Open Science Framework (OSF), The Cochrane Library, JBI Clinical Online Network of Evidence for Care and Therapeutics (COnNECT+), and Database of Abstracts of Reviews of Effects (DARE) were examined. The search results revealed a gap in scientific publications concerning objectives like those of this scoping review.
To formulate the research question, the mnemonic combination ‘PCC’ was used, where ‘P’ stands for population, ‘C’ for concept, and ‘C’ for context [25]. The population consisted of studies involving children and adolescents (aged 0 to 19 years) diagnosed with childhood and adolescent cancer, undergoing oncological treatment. The key concept of this scoping review comprised studies detailing coping strategies of parents and/or caregivers within the family dynamic, considering the impact of childhood and adolescent cancer diagnosis on family relationships, parental responsibilities, communication among family members, family routines, as well as problem-solving. The defined context included the home environment, hospital setting, specialized oncology centers, and religious and cultural communities providing social support care. Based on this, the following research question was conceived: “What scientific evidence addresses the effectiveness of dynamic family coping intervention strategies, as well as elements for improving problem-solving skills, for parents and/or caregivers of children and adolescents, aged 0 to 19 years, during and after oncological treatment, considering the impact of childhood and adolescent cancer diagnosis within the family context?”.
2.4. Data Collection and Organization
Data collection took place between January and March 2024, from the following databases: PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Scopus, Web of Science, and Latin American and Caribbean Health Sciences Literature (LILACS).
The search strategy aimed to locate published studies and occurred in two stages. In the first stage, for the search and identification of studies, indexed descriptors in the Health Sciences Descriptors (DeCS) and the Medical Subject Headings (MeSH) were consulted, along with alternative terms suggested by the databases to adapt searches to Portuguese and English. The Boolean operators ‘AND’ and ‘OR’ and truncation were used for the cross-referencing of descriptors and keywords.
In the second stage, a new search using the identified keywords and descriptors was conducted in the databases. For the development of the search strategy, the assistance of an experienced librarian from the University of São Paulo (USP) was enlisted. Modified controlled vocabulary was used for each database. It is worth noting that the search strategy was adapted according to the specificities of each source used; however, combinations between descriptors were preserved; furthermore, time-restriction filters (2014 to 2024) and language-search filters were applied, focusing on Portuguese, English, and Spanish. Additionally, it is highlighted that Table 1 demonstrates the strategies devised with the descriptors used, aided by the Boolean operators ‘AND’ and ‘OR’ to compose the search, as well as quantifying the articles located and selected in each database.

Table 1.
Search strategies for articles in databases, 2014–2024.
2.5. Article Inclusion and Exclusion Criteria
This scoping review included qualitative and quantitative studies, focusing on coping strategies as well as elements for problem-solving, among parents and/or caregivers of children and adolescents, aged 0 to 19 years, undergoing oncological treatment, within the family care context. Qualitative studies of any theoretical and methodological approach were considered, as well as studies published in English, Spanish, or Portuguese, within the timeframe of 2014 to 2024. It is important to emphasize that as the year 2024 has not yet ended, and new studies can still be published in the literature, the search for articles took place up to 31 January 2024. This timeframe is justified due to the intensification of publications and discussions regarding the characterization of coping strategies and problem-solving directed towards childhood and adolescent cancer.
Studies that addressed other types of cancers without focusing on coping and problem-solving, based on literature or theory, were excluded. Additionally, opinion articles, theses, and studies that addressed coping strategies from the perspective of bereaved parents and caregivers were also excluded.
In addition to the criteria mentioned earlier, it is important to highlight the details of the exclusion criteria adopted in this study. Firstly, we excluded studies that did not specifically focus on coping strategies and problem-solving within the specific context of children and adolescents undergoing oncological treatment. This included studies that addressed other types of cancers without a clear emphasis on these specific strategies, as described in relevant studies or pertinent theories. Additionally, we chose to exclude studies that investigated coping strategies from the perspective of bereaved parents and caregivers to maintain thematic cohesion within our scope of review. These criteria were rigorously applied during the study-selection process to ensure the relevance of the included articles and consistency with the objectives and focus of the review.
2.6. Analysis of Results
The characterization of the results began by using the Content Analysis method, which allows for the critical and analytical description of classifying the components of the meaning of messages obtained in articles into different categories, resulting from the grouping of classes of elements that share common characteristics [29]. Discrepancies were resolved through discussion between the two reviewers and, when necessary, by a third reviewer.
All titles and abstracts retrieved in the searches were grouped in the Mendeley® reference-management database for identification and removal of duplicates. For selection, records were exported to the Rayyan web application [30], where duplicates were removed, and two reviewers independently conducted title and abstract screening in a blinded manner. Discrepancies between reviewers were resolved through a consensus meeting with a third reviewer. Subsequently, full-text reading was conducted dynamically. Additionally, a backward search in the references of selected articles was performed to identify possible relevant studies for inclusion in the results.
The classification regarding the level of evidence followed the classification system advocated by JBI [25,26], which comprises five levels of evidence: level 5 (expert opinion), level 4 (descriptive observational studies, such as cross-sectional studies, for example), level 3 (analytical observational studies, such as cohort and case-control studies, for example), level 2 (quasi-experimental studies), and level 1 (experimental studies including systematic reviews and randomized clinical trials). After this step, articles were characterized, and the results related to the research question were synthesized and described and grouped into guiding axes.
Furthermore, aligned with the JBI level of evidence, according to the Oxford Centre for Evidence-based Medicine [30], the lower the number assigned to the study, the better its level of evidence, while studies classified as ‘A’ are considered more relevant, with a higher degree of recommendation. Additionally, it is emphasized that data analysis occurred in tabular form, and data interpretation was descriptive narrative, with tables and statistics elaborated with absolute and relative frequencies. Moreover, the data were compiled into a synthesis table, and each article was randomly assigned an ‘E’ code (study).
Therefore, regarding the data filtering and analysis, it is confirmed that these issues were meticulously conducted as described in the method. After removing duplicates using the Rayyan platform [30], two reviewers independently and blindly screened titles and abstracts, with any discrepancies resolved through consensus in a meeting with a third reviewer. Full-text reading of selected articles was dynamically conducted to ensure accurate inclusion of relevant studies. The classification of evidence levels according to JBI [25,26] and the Oxford Centre for Evidence-based Medicine [30] was rigorously applied, with the synthesis of results organized into thematic axes to provide a clear and comprehensive understanding of the coping strategies and problem-solving approaches adopted by parents and caregivers of children and adolescents during and after oncological treatment.
3. Results
3.1. Search Results
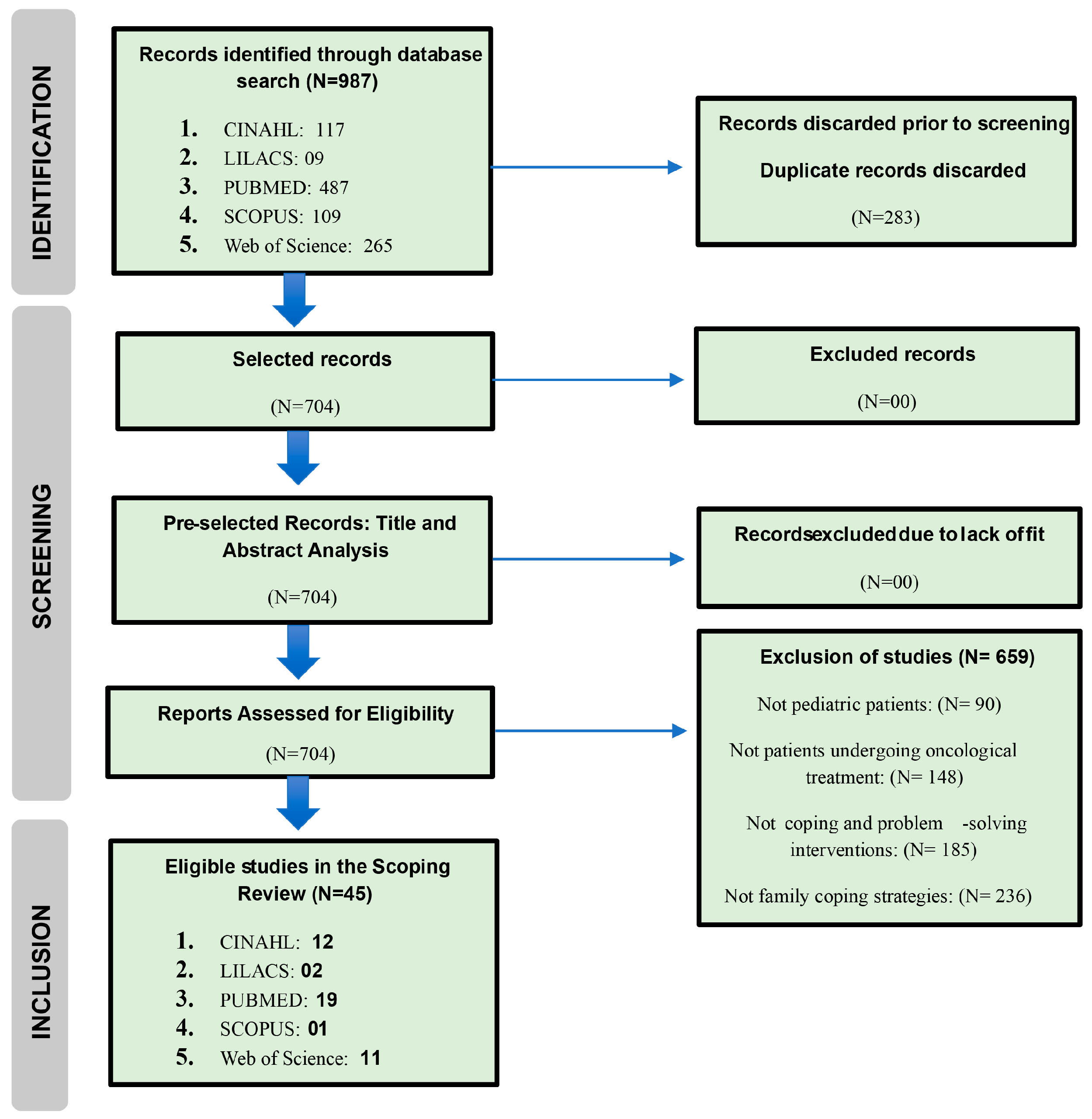
The identification of studies (Figure 1) through databases and records resulted in 987 works. Of this total, 92 studies were fully examined through article reading. Overall, 45 studies were included in the final sample.
Figure 1.
PRISMA flowchart of the study-selection process.
Table 2 summarizes the 45 studies with relevant information for the research question, illustrating the data synthesis, coping strategies employed by parents and/or caregivers, and problem-solving skills.

Table 2.
Synopsis of studies included in the scoping review.
3.2. Characteristics of Studies
Regarding the main characteristics observed through the final sampling of eligible studies in this scoping review, it is noteworthy that in terms of the study’s publication location, there was a considerable diversity of countries, totaling 23 nationalities. Additionally, it is highlighted that out of these 23 countries, only the continent of Antarctica was not encompassed in terms of study eligibility. Furthermore, it is inferred that the Asian continent exhibited the highest quantity of studies, comprising 45 studies in the sample (n = 17/37.8%), followed by the American continent (n = 15/33.3%), the European continent (n = 09/20.0%), the African continent (n = 03/6.7%), and the Oceanic continent (n = 01/2.2%). Analyzing each country independently, it is inferred that the United States of America (USA) presented the highest quantity of studies (n = 11/24.4%).
Regarding the methodology employed in each study that comprised the final sample, it is noted that the majority of studies presented level of evidence IV (n = 43/95.6%), indicating qualitative studies. However, it is important to note that although these 43 studies are qualitative, they adopted various methodological approaches, including cross-sectional, descriptive, exploratory, correlational, longitudinal, phenomenological, and mixed-methods studies. It is also noteworthy that two studies presented a level of evidence II (n = 02/4.4%).
Regarding the objectives outlined in each study, within the context of coping strategies and problem-solving, a diversity of purposes was observed, aiming to encompass a wide range of outcomes and, consequently, enhance the understanding of the theme under study. Thus, these objectives encompassed activities of investigation, analysis, identification, description, exploration, examination, evaluation, measurement, and explanation of coping strategies and problem-solving adopted by parents and responsible caregivers during the diagnosis and treatment of children and adolescents with cancer.
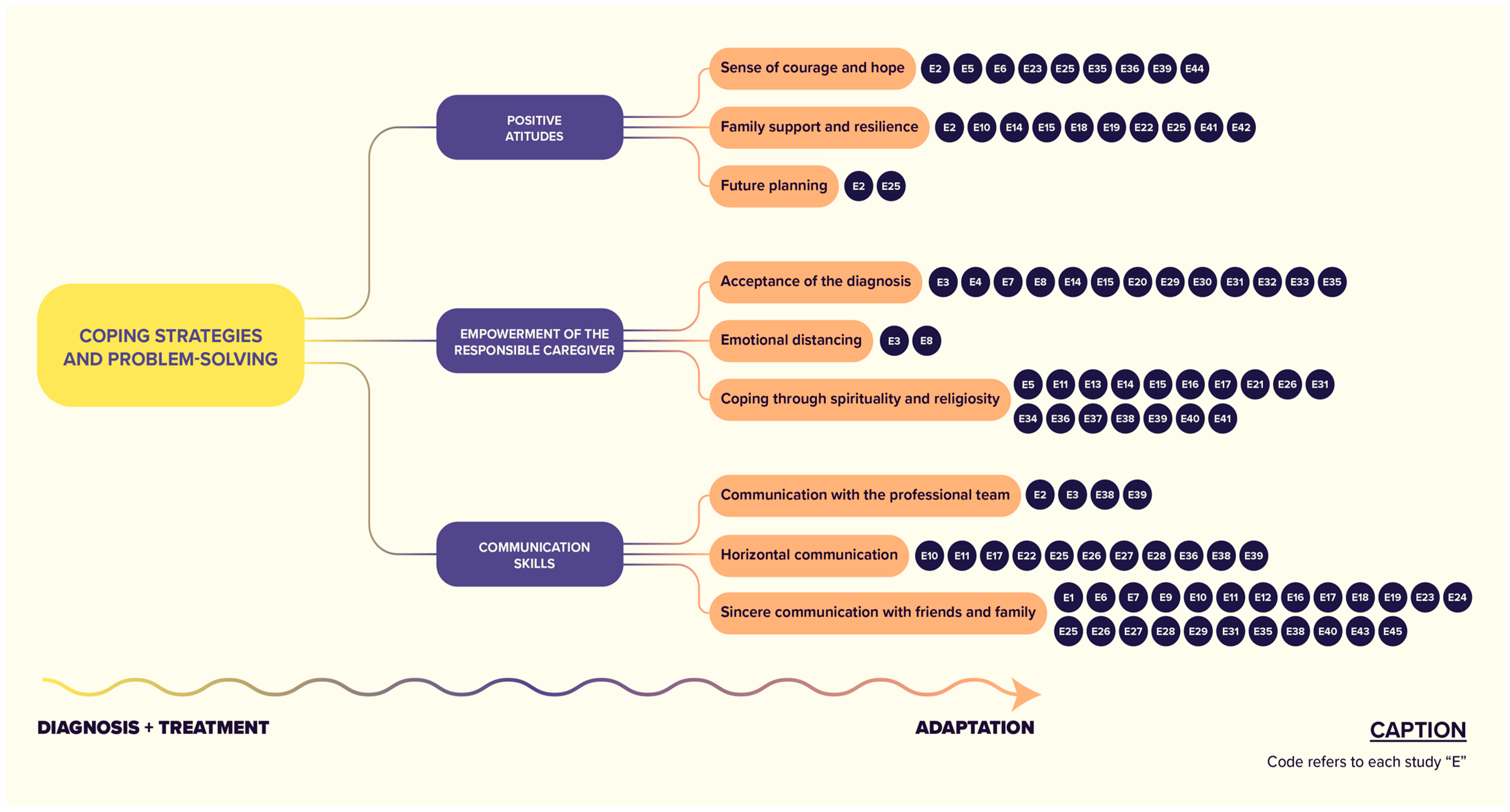
Furthermore, based on the findings of each study, it is emphasized that coping strategies were grouped into categories and subcategories as follows: (1) positive attitudes (including a sense of courage and hope, family support to enhance resilience, and future planning), (2) caregiver empowerment (involving acceptance of diagnosis, emotional distancing, and coping through religiosity), and (3) communication skills (encompassing professional communication, horizontal dialogue with healthcare teams, and sincere communication with friends and family) (Figure 2).
Figure 2.
Coping strategies and problem-solving approaches employed by parents and/or caregivers and those responsible for children and adolescents with cancer, from diagnosis to treatment. Explanatory Note: The acronyms E1, E2, etc., refer to visual elements of self-identification of study codes, that is, the acronym E1 refers to Study 1, and so on.
3.3. Categories and Subcategories of Coping Strategies and Problem-Solving
3.3.1. Positive Attitudes
Positive attitudes in cancer coping refer to the mindset and approaches that patients, caregivers, and family members adopt to deal with the emotional, physical, and psychological challenges associated with the disease. These attitudes involve an optimistic outlook, emotional resilience, acceptance of changes, and a willingness to confront obstacles with courage and hope. Positive attitudes, within the context of coping strategies employed by parents and caregivers of children undergoing cancer treatment, emerge as fundamental components in navigating the multifaceted challenges inherent in the oncological journey. Research demonstrates that these attitudes have a significant impact on psychological well-being, family dynamics, and adaptive skills in the face of adversity. Parents and caregivers with a positive outlook demonstrate greater resilience, fostering an environment of hope, optimism, and proactive problem-solving. Such attitudes not only protect against psychological distress but also empower caregivers to deal with childhood cancer with a sense of efficacy and agency. Additionally, they promote effective communication within the family, strengthening emotional support and facilitating shared decision-making processes. Therefore, cultivating positive attitudes is not just a psychological construct but a dynamic force driving adaptive strategies and family resilience in the face of pediatric cancer diagnosis and treatment [21,31,32,35,36,37,45,53,69,71].
Sense of Courage and Hope
Throughout the journey faced by parents and caregivers of children with cancer, a profound sense of courage and hope emerges as a fundamental psychological resource. This challenging context urges them to adopt a stance of resilience, sustained by an unwavering belief in the possibility of overcoming and healing. Courage is manifested in the ability to face difficult moments, from diagnosis to treatment, with determination and bravery, often surpassing their own limits for the well-being of their child or ward. This courage is sustained by hope, a driving force that propels parents and caregivers to persevere even in the face of the uncertainties and challenges inherent in childhood cancer. It is hope that keeps them focused on moments of despair, guiding them through difficulties and providing a beacon of light amidst the darkness. Thus, the sense of courage and hope not only strengthens parents and caregivers but also empowers them to face each stage of the oncological journey with dignity, determination, and a firm commitment to ensuring the best possible care for the child [32,35,40,55,65,66,67,72].
Family Support and Resilience
Family support and resilience emerge as essential pillars in coping with and resolving problems during the journey of childhood cancer. The presence of a solid family support network provides an environment of emotional and practical security, where parents and caregivers find emotional support, guidance, and assistance in daily tasks related to the child’s care. This support network not only reduces the impact of emotional stress but also strengthens the ability to cope with the challenges inherent in the child’s oncological condition. Additionally, family resilience, characterized by the ability to adapt and recover from adversity, plays a crucial role in overcoming obstacles. Resilient families can adjust to the changes imposed by the illness, find creative solutions to problems, and maintain a sense of hope and optimism, even in the most difficult circumstances. By cultivating both family support and resilience, parents and caregivers become more equipped to face the challenges of childhood cancer, promoting an environment of loving and sustainable care for the child throughout the treatment and recovery process [32,41,44,45,48,49,52,53,55].
Future Planning
In the context of childhood cancer, future planning is essential to provide parents and caregivers with a sense of control and direction. This involves understanding the child’s treatment, considering financial aspects such as medical costs, and cultivating self-care strategies. It also includes establishing social support networks to ensure emotional and practical support. In summary, future planning empowers parents and caregivers to address current challenges while maintaining a hopeful outlook for the future [60].
3.3.2. Empowerment of the Responsible Caregiver
Empowering caregivers of a child with cancer involves providing them with information and resources so they can make informed decisions about treatment. At the same time, it is their responsibility to ensure the best possible care for the child by coordinating family and community support and following medical guidance. This combination of empowerment and responsibility is essential for addressing the challenges of childhood cancer treatment [31,70].
Acceptance of the Diagnosis
Acceptance of the diagnosis by parents and caregivers emerges as a vital coping strategy in the context of childhood cancer. Recognizing and accepting the reality of the diagnosis is the first step in dealing with the emotional and practical challenges that accompany the treatment journey. This acceptance allows parents and caregivers to focus their energies on finding solutions and providing the best possible care for the child. Additionally, acceptance of the diagnosis can facilitate the search for emotional and practical support, both within and outside the family, helping parents and caregivers to feel less isolated and more empowered to face the challenges of childhood cancer. In summary, acceptance of the diagnosis is a powerful tool that enables parents and caregivers to confront the reality of the illness and concentrate their efforts on ensuring the well-being of the child [33,44,45,59].
Emotional Distancing
Emotional detachment, adopted by some parents and caregivers as a coping mechanism, arises as a strategy for psychological protection in the face of the overwhelming impact of childhood cancer. For some, confronting the emotionally intense reality of diagnosis and treatment can be too overwhelming. Thus, emotional detachment allows for a temporary separation from the painful emotions associated with the situation, helping them to maintain a sense of control and functionality. Although it may seem like detachment, this emotional distancing is often an attempt to preserve one’s own mental health in order to continue caring for the child as effectively as possible. However, it is important to recognize that emotional detachment can also have adverse effects, such as difficulties in emotional communication and in building emotional bonds with the child. Therefore, it is essential for parents and caregivers to have access to emotional support and resources to deal with their own feelings while continuing to support the child during cancer treatment [33,38,43,59,69,71].
Coping through Spirituality and Religiosity
Coping through religiosity and spirituality is common among parents and caregivers of children with cancer. Belief in a higher power provides comfort, hope, and purpose, helping to deal with stress and uncertainty. Prayer, meditation, and participation in religious rituals offer a source of inner strength, while the religious community provides support and solidarity. It is important to respect the diverse coping mechanisms of each individual and ensure access to the emotional and spiritual support needed during this challenging journey [35,41,43,44,45,46,47,51,56,64,66,67,68,69].
3.3.3. Communication Skills
Communication emerges as a powerful coping and problem-solving tool for parents and caregivers of children with cancer. Opening frank and open channels of dialogue with the medical team, family, friends, and the child themself is essential for sharing concerns, obtaining information about treatment, and receiving emotional support. Effective communication promotes a deeper understanding of the situation, reducing anxiety and fostering a sense of control over the situation. Additionally, it allows parents and caregivers to express their needs and concerns, facilitating the obtaining of practical and emotional help when necessary. Through communication, parents and caregivers can collaborate with the medical team in decision-making, ensuring that the treatment plan is personalized and tailored to the specific needs of the child [21,31,50,53,68].
Communication with the Professional Team
Communication with the multidisciplinary team plays a crucial role in coping with and resolving problems for parents and caregivers of children with cancer. Establishing an open and transparent channel of communication with doctors, nurses, psychologists, and other healthcare professionals allows parents to better understand the diagnosis, treatment plan, and any concerns related to the child’s health. This effective communication also facilitates the exchange of information, enabling parents to express their needs and concerns, while the team provides appropriate guidance and support. Additionally, communication with the multidisciplinary team helps parents feel more empowered and engaged in the child’s care, fostering a sense of partnership in the treatment process. By working together, parents and the multidisciplinary team can develop effective coping strategies and ensure the best possible care for the child during their journey against cancer [32,33,47,52,55,66,68,71].
Horizontal Communication
Horizontal communication is an approach in which parents and caregivers establish an equal and collaborative dialogue with healthcare professionals, as opposed to the traditionally hierarchical vertical communication. In this context, parents are encouraged to share their experiences, concerns, and knowledge about the child, while healthcare professionals listen attentively, respecting their perspectives and contributions. This approach fosters an environment of trust, mutual respect, and partnership in decision-making related to the child’s cancer treatment. By enabling a more open and horizontal communication, parents feel more empowered and engaged in the child’s care, while healthcare professionals gain valuable insights that can inform and enhance the treatment plan [34,36,39,40,41,48,56,57].
Sincere Communication with Friends and Family
Open and sincere communication with friends and family plays a fundamental role in coping with and resolving problems for parents and caregivers of children with cancer. By openly sharing information about the child’s diagnosis and treatment, parents can receive emotional support, understanding, and solidarity from their loved ones. This frank dialogue also allows friends and family to offer practical help, such as caring for the child’s siblings, preparing meals, or providing transportation to medical appointments. Furthermore, honest communication creates a safe space where parents can express their emotions, fears, and concerns without judgment. This promotes the strengthening of family bonds and the formation of a robust support network, which plays a crucial role in coping with and adapting to the journey of childhood cancer [34,36,37,39,41,42,47,49,53,54,55,56,57,58,61,62,63,65,72,73].
3.4. Coping and Problem-Solving
Coping and problem-solving are fundamental processes in adapting to stressful and challenging situations, such as childhood cancer. Coping refers to the cognitive and behavioral strategies used to deal with stress, while problem-solving involves identifying and implementing practical solutions to the challenges faced. There are different types of coping strategies, including active coping, which involves actively seeking solutions, and emotional coping, which focuses on regulating emotions associated with stress. Additionally, social support plays an important role in coping, providing emotional, instrumental, and informational support during difficult times. As for problem-solving, a proactive and solution-focused approach is essential. This may include clearly identifying problems, generating alternative solutions, and implementing effective action plans. Resilience is also a key aspect, allowing individuals to adapt to changes, learn from challenging experiences, and continue moving forward, even in the face of adversity [74,75,76].
4. Discussion
The diagnosis of childhood cancer is a highly challenging moment for families, demanding adaptive strategies that not only support the sick child but also strengthen the family unit as a whole. The body of evidence from the scoping review, which encompassed 45 studies, revealed a wide range of strategies employed by parents and caregivers, highlighting the crucial importance of family support, religiosity, effective communication, and caregiver empowerment to facilitate positive adaptation during treatment [40,62].
Consistent with previous studies, the presence of positive attitudes such as courage and hope emerge as a fundamental pillar in coping with childhood cancer. Smith et al. (2024) and Luo et al. (2021) emphasize that these attitudes not only strengthen caregivers’ emotional resilience but also directly influence the children’s psychological well-being, creating a positive support environment around them [72,77].
The family support network proves to be a determining factor for better emotional and adaptive outcomes during treatment. Schoors et al. (2019) and Melguizo-Garín et al. (2023) indicate that families with strong social support tend to more effectively handle the stress and uncertainty associated with childhood cancer, highlighting the importance of policies and practices that strengthen this support network. Additionally, Nukpezah et al. (2021) found that in Ghana, parents often turn to community support and religion, underscoring the universality of the importance of social and spiritual support [52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79].
Beyond family support, strategies such as caregiver empowerment have been identified as essential for psychological adaptation and practical support provided to the sick child. Lin et al. (2019) and Mardhyah et al. (2022) discuss how the acceptance of the diagnosis, the use of emotional distancing strategies, and engagement in religious practices help caregivers face the emotional and practical challenges associated with childhood cancer. This finding is reinforced by the study of Deribe et al. (2023), which identified that acceptance of the child’s condition and effective communication with healthcare professionals are essential coping strategies among parents in Ethiopia [68,80,81].
Communication skills, both with the healthcare team and with friends and family, emerge as a fundamental competence to facilitate mutual understanding and continuous support. Smith et al. (2024) and Lin et al. (2019) stress that open and horizontal communication not only promotes personalized care but also strengthens the emotional support needed to face the ups and downs of pediatric oncology treatment [72,80].
Spirituality also plays a crucial role in coping, providing hope and emotional support to parents during their child’s treatment, as found by Chong et al. (2023) among Malay Muslim caregivers of children with acute lymphoblastic leukemia. This spiritual dimension, along with religiosity, is a significant coping strategy that can provide a solid emotional and practical foundation during pediatric oncology treatment [67].
The findings significantly contribute to the field by offering an in-depth and systematic analysis of the coping strategies utilized by parents and caregivers. By categorizing and integrating these strategies, we provide a holistic view of adaptive practices that can be implemented to improve the emotional and practical support offered to these families. Furthermore, the importance of targeted interventions that strengthen positive attitudes, empower caregivers, and promote effective communication is highlighted as essential components in comprehensive care during pediatric oncology treatment [39,40,41,42,46,49].
The three broad themes synthesized from the studies that comprised the final sample of this scoping review highlighted the significant impact of oncological disease on the lives of parents and/or caregivers of children and adolescents, as well as on family dynamics, greatly affecting these caregivers’ ability to cope with situations from diagnosis to treatment continuity. Thus, it is noted that the findings were similar to reviews that focused on pediatric oncological themes [31,32,33,34,35,36,37,38] or included cancer as part of a variety of chronic diseases, as well as life-threatening conditions [39,40,41,42,46,49].
In terms of impact on family functioning, studies (E24 to E32) also reported that parents and caregivers experienced significant disruption in routine and family relationships [54,55,56,57,58,59,60,61,62]. Regarding coping and psychological well-being, qualitative research, evidenced by studies (E35, E43, E45), indicated that parents and caregivers of children and adolescents affected by neoplasms experienced intense feelings with unmet needs, leading to emotional struggles and the adoption of inadequate coping mechanisms (acting out at home) [65,72,73].
In terms of caregivers, much of their social well-being is related to the coping mechanisms they employ, such as the following: (1) positive attitudes, including a sense of courage and hope, family support to enhance resilience, and future planning; (2) caregiver empowerment, involving acceptance of the diagnosis, emotional distancing, and coping through religiosity; and (3) communication skills, encompassing professional communication, horizontal dialogue with healthcare teams, and sincere communication with friends and family [40,43,72]. These caregivers often report difficulties within the family environment, frequently resorting to emotional distancing as a means to strengthen their ability to continue providing care [59]. Additionally, they face overwhelming uncertainties related to the child’s health condition and experience anxiety within the context of family caregiving [38,70]. These findings underscore the pressing need for further research in this area to identify the causes of caregivers’ distress and develop effective support strategies.
Furthermore, it is noteworthy that the burden of care in cancer-related conditions can extend over many years, placing immense strain on the physical, financial, and emotional resources of families and may involve the use of technology (such as feeding tubes and ventilators) [69,72]. Future research should encompass parents and caregivers responsible for children and adolescents with cancer from a variety of life-threatening conditions, particularly those with diagnoses related to pediatric oncology, and with sample sizes large enough to allow for sub-analyses based on different aspects of the child’s illness [51,61,64].
The utilization of theoretical frameworks to guide family or illness-related research assists researchers in contextualizing observed problems. Thus, it is emphasized that studies (E22, E32, E36) strengthen their methodology, results, and discussions by grounding themselves in theoretical frameworks, as they enrich the interpretation of findings and influence clinical practice and future research [52,62,66]. Additionally, studies (E38, E40) have also noted that the absence of a theoretical framework diminishes the quality of research on the proposed topic [21,68]. In this regard, the significance of family relationships in shaping the experience of these parents and caregivers provides a family-focused perspective on familial dynamics [67]. Furthermore, the adoption of a specific model should be a priority to advance knowledge in this field [16,63].
4.1. Study Limitations
The present scoping review delineates some noteworthy limitations. Firstly, it is imperative to acknowledge that while the search strategy was meticulously devised to encompass all relevant studies, it is plausible that some may have inadvertently been omitted. For instance, studies involving parents and/or caregivers of children with cancer, focusing on broader aspects of family well-being, may have eluded detection during the established review process.
4.2. Implications for Nursing Practice
The evidence presented in this study represents a significant contribution to nursing in formulating a care protocol aimed at family caregivers. The ability to provide care, still an emerging theme in studies, provides an understanding of individuals’ conditions to take on caregiving responsibilities. From this perspective, it is possible to provide essential support for nursing practice in developing attributes of knowledge, courage, and patience. Implementing support and guidance actions to strengthen family caregivers in the context of home care can reduce burden and stress, and promote the development of effective coping strategies, thus mitigating the negative impact of these adversities on caregiving ability.
In this context, nurses play a crucial role in identifying the emerging needs of this population. Through collaboration with other healthcare professionals and different levels of care, they can develop strategies to support caregivers, including health education actions and psychological support, with the aim of ensuring adequate care and promoting quality of life for caregivers facing the challenge of home care.
Furthermore, the exploration of coping strategies used by parents and caregivers should be conducted on an individualized basis. Coping support can be facilitated by helping children and their families identify distressing symptoms and exploring strategies that may be helpful in mitigating negative impacts on quality of life.
4.3. Future Research Direction
Families play a crucial role in the development, overall well-being, and coping abilities when there is a child with cancer in the family. Future research could consider exploring the roles of extended family members (such as grandparents), neighbors, and the broader community (including youth clubs and religious or cultural communities) in providing additional support to parents and caregivers. These extended support networks may facilitate better support for these caregivers. Additionally, future work may consider the influence of cultural beliefs or traditions on family adaptation. Researchers should consider designing longitudinal studies on the psychosocial outcomes or coping strategies of parents and caregivers, as well as engaging in more in-depth qualitative approaches. These results may help parents, clinicians, and researchers recognize patterns of change in family dynamics over time and serve as a basis for the development of interventions specific to the unique needs of these caregivers. Furthermore, it is noteworthy that longitudinal studies can also clarify the resilience of parents and caregivers and how support can be directed to strengthen their coping skills.
5. Conclusions
Initially, it is imperative to highlight that coping strategies and problem-solving play a significant role in the process of acceptance and reframing of ideas and feelings related to childhood and adolescent cancer by families. In this context, it becomes crucial that nursing interventions and those of related professionals, both during diagnosis and after treatment, be geared towards empowering families to adopt a range of resources. These include seeking information and understanding about pediatric neoplasms and their future implications, fostering effective intrafamily communication, providing support in delivering specific care to this population, as well as adopting planning and preparation strategies for the inevitable changes that will occur in the family dynamic. Additionally, it is crucial to establish links with support groups composed of families of children with cancer.
As time progresses, such resources bring about changes in family functioning patterns and their interactions with the external environment. During this period, coordinated professional practices become essential to support families in making relevant decisions regarding the child’s development and growth, as well as to assist them in managing the tensions that arise along the way. These practices include encouraging communication and decision-sharing within the family, recognizing and promoting family strengths and beliefs, as well as valuing the unique qualities inherent in a child with cancer.
It is imperative to emphasize, however, that the mere existence of coping strategies and problem-solving does not guarantee adequate adaptation. However, identifying such strategies allows for the presentation of resources that can make the process more manageable for the family unit. In this context, nurses and other healthcare professionals can utilize the findings outlined here as indicators to encourage families to deal more effectively with the situations involving the diagnosis and treatment of cancer in children and adolescents.
Based on the analysis addressed in this scoping review, we can conclude that the care of children and adolescents during and after oncological treatment poses significant challenges for parents and caregivers. The reviewed studies highlighted the substantial impact of the disease on the lives of these caregivers, demonstrating disruptions in family routines and intense emotional relationships. Coping strategies, such as positive attitudes, caregiver empowerment, and communication skills, were identified as crucial for dealing with the demands of care. However, the lack of consistency in the measures used and the absence of control for variables such as the patients’ age and sex represent significant methodological challenges. Furthermore, the lack of information on the time from diagnosis to the start of oncological treatment complicates the understanding of the disease’s impact over time. To advance in this area, longitudinal studies are needed that consider these aspects and employ theoretical frameworks to guide research. By doing so, we can develop more effective interventions to support parents and caregivers throughout the course of their children’s oncological treatment.
Author Contributions
Conceptualization: P.E.G.P. and A.J.S.C.-J.; Validation: P.E.G.P., A.J.S.C.-J., T.M.d.S.R., C.M.S.P.-H., A.A.d.S.T. and H.M.S.; Writing—initial draft preparation: P.E.G.P. and A.J.S.C.-J.; Writing—review and editing: P.E.G.P., A.J.S.C.-J., T.M.d.S.R., C.M.S.P.-H., A.A.d.S.T. and H.M.S. All authors have read and agreed to the published version of the manuscript.
Funding
National Council for Scientific and Technological Development, CNPq Process 443021/2019-8 (CNPq Notice Nº. 27/2029).
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Public Involvement Statement
Not applicable.
Guidelines and Standards Statement
This manuscript was drafted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement.
Use of Artificial Intelligence
Not applicable.
Acknowledgments
The authors wish to acknowledge the School of Nursing of Ribeirao Preto (EERP), University of São Paulo (USP), Collaborating Center of the Development of Nursing Research (PAHO-WHO).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Erdmann, F.; Frederiksen, L.E.; Bonaventure, A.; Mader, L.; Halse, H.; Robison, L.L.; Winther, J.F. Childhood cancer: Survival, treatment modalities, late effects, and improvements over time. Cancer Epidemiol. 2021, 71, 101733. [Google Scholar] [CrossRef] [PubMed]
- Prates, P.E.G.; Alonso, J.B.; Carvalho, E.C.; Arcêncio, R.A.; Zamarioli, C.M. Analysis of Survival of Pediatric Patients with Leukemias and Lymphomas in the Oncological Context: Epidemiological Study in the State of São Paulo, Brazil, 2000–2022. Rev. Bras. Cancerol. 2024, 70, 1–10. [Google Scholar] [CrossRef]
- National Cancer Institute. Estimate for 2023: Incidence of Cancer in Brazil; National Cancer Institute: Rio de Janeiro, Brazil, 2024. Available online: https://www.inca.gov.br/sites/ufu.sti.inca.local/files//media/document//estimativa-2023.pdf (accessed on 20 April 2024).
- Brazilian Society of Pediatrics. Child Health: Growth and Development; Brazilian Society of Pediatrics: São Paulo, Brazil, 2012. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/saude_crianca_crescimento_desenvolvimento.pdf (accessed on 20 April 2024).
- Steliarova-Foucher, E.; Colombet, M.; Ries, L.A.G.; Moreno, F.; Dolya, A.; Bray, F.; Hesseling, P.; Shin, H.Y.; Stiller, C.A.; IICC-3 Contributors. International incidence of childhood cancer, 2001–2010: A population-based registry study. Lancet Oncol. 2017, 18, 719–731. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization. Child and Adolescent Cancer; Pan American Health Organization: Washington, DC, USA, 2022; Available online: https://www.paho.org/es/temas/cancer-ninez-adolescencia (accessed on 20 April 2024).
- Andrade, S.F.O.; Alves, R.F.; Melo, M.O.; Rodrigues, M.J. Quality of Life and Burden of Caregivers of Children with Cancer. Psicol. Cienc. Prof. 2014, 34. [Google Scholar] [CrossRef]
- Amador, D.D.; Gomes, I.P.; Reichert, A.P.S.; Collet, N. Repercussions of childhood cancer for family caregivers: Integrative review. Rev. Bras. Enferm. 2013, 66, 267–270. [Google Scholar] [CrossRef] [PubMed]
- Fetsch, C.F.M.; Portella, M.P.; Kirchner, R.M.; Gomes, J.S.; Benetti, E.R.R.; Stumm, E.M.F. Coping Strategies among Family Members of Cancer Patients. Rev. Bras. Cancerol. 2016, 62, 17–25. Available online: https://rbc.inca.gov.br/index.php/revista/article/view/175/100 (accessed on 20 April 2024).
- Johansen, S.; Cvancarova, M.; Ruland, C. The Effect of Cancer Patients‘ and Their Family Caregivers‘ Physical and Emotional Symptoms on Caregiver Burden. Cancer Nurs. 2018, 41, 91–99. [Google Scholar] [CrossRef]
- Lins, A.L.R.; de Mendonça, E.T.; Moreira, T.R.; Andrade, J.V.; Ramos, D.H.S.; Pedretti, P.A.H. Assessing the burden of family caregivers of cancer patients: A cross-sectional study. Rev. Med. 2022, 55. [Google Scholar] [CrossRef]
- Cardoso, A.C.; Noguez, P.T.; Oliveira, S.G.; Porto, A.R.; Perboni, J.S.; Farias, T.A. Support and Support Network for Family Caregivers of Patients in Palliative Care at Home. Enferm. Foco 2019, 10, 34–39. [Google Scholar] [CrossRef]
- Coppetti, L.C.; Girardon-Perlini, N.M.O.; Andolhe, R.; da Silva, L.M.C.; Dapper, S.N.; Noro, E. Care ability, overload, stress and coping of family caregivers of people undergoing cancer treatment. Rev. Bras. Enferm. 2019, 72. [Google Scholar] [CrossRef]
- Borges, E.L.; Franceschini, J.; Costa, L.H.D.; Fernandes, A.L.G.; Jamnik, S.; Santoro, I.L. Family caregiver burden: The burden of caring for lung cancer patients according to the cancer stage and patient quality of life. J. Bras. Pneumol. 2017, 43, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Mccubbin, M.; Mccubbin, H. Families Coping with Ilness: The Resiliency Model Family Stresse, Adjustment, and Adaptation; Mosby-Year Book: St. Louis, MO, USA, 1993; pp. 21–63. [Google Scholar]
- Koutelekos, I.; Polikandrioti, M.; Krokou, P.; Dousis, E.; Ntafogianni, C.; Evagelou, E.; Vlachou, E.; Ntre, V.; Geronikolou, S.; Koukoularis, D.; et al. Coping Strategies in Greek Parents of Children with Cancer. Adv. Exp. Med. Biol. 2023, 1425, 69–77. [Google Scholar] [CrossRef]
- Makhoul-Khoury, S.; Ben-Zur, H. The Effects of Coping Strategies on Distress and Quality of Life among Jewish and Arab Mothers with a child diagnosed with cancer. Eur. J. Oncol. Nurs. 2022, 58, 102140. [Google Scholar] [CrossRef] [PubMed]
- Belpame, N.; Kars, M.; Deslypere, E.; Rober, R.; Van Hecke, A.; Verhaeghe, S. Coping Strategies of Adolescent and Young Adult Survivors of Childhood Cancer: A Qualitative Study. Cancer Nurs. 2021, 44, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Zimmer-Gembeck, M.J.; Skinner, E.A. The Development of Coping: Implications for Psychopathology and Resilience. Developmental Psychopathology; John Wiley & Sons: Hoboken, NJ, USA, 2016; pp. 1–61. [Google Scholar]
- Houtzager, B.A.; Oort, F.J.; Hoekstra-Weebers, J.E.H.M.; Caron, H.N.; Grootenhuis, M.A.; Last, B.F. Coping and family functioning predict longitudinal psychological adaptation of siblings of childhood cancer patients. J. Pediatr. Psychol. 2004, 29, 591–605. [Google Scholar] [CrossRef] [PubMed]
- Mensah, A.B.B.; Nunoo, H.; Mensah, K.B.; Okyere, J.; Dzomeku, V.M.; Apiribu, F.; Asoogo, C.; Clegg-Lamptey, J.-N. Impact of childhood and adolescence cancer on family caregivers: A qualitative analysis of strains, resources, and coping behaviours. BMC Psychol. 2023, 11, 361. [Google Scholar] [CrossRef] [PubMed]
- Fisher, R.S.; Sharp, K.M.H.; Prussien, K.V.; Himelhoch, A.C.; Murphy, L.K.; Rodriguez, E.M.; Young-Saleme, T.K.; Vannatta, K.; E Compas, B.; A Gerhardt, C. Coping Trajectories and the Health-Related Quality of Life of Childhood Cancer Survivors. J. Pediatr. Psychol. 2021, 46, 960–969. [Google Scholar] [CrossRef] [PubMed]
- National Health Council. Resolution nº 510, of April 7, 2016. Provides for the Standards Applicable to Research in Human and Social Sciences Whose Methodological Procedures Involve the Use of Data Directly Obtained from Participants or Identifiable Information or That May Result in Risks Greater than Those Existing in Everyday Life, as Defined in this Resolution. Official Gazette of the Union, Brasília. 2016, Seção I:44. Available online: https://bvsms.saude.gov.br/bvs/saudelegis/cns/2016/res0510_07_04_2016.html (accessed on 20 April 2024).
- Page, M.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Chapter LL: Scoping reviews (2020 version). In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; Joanna Briggs Institute, 2020; Available online: https://jbi-global-wiki.refined.site/space/MANUAL/4687342 (accessed on 20 April 2024).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Prates, P.E.G.; Correa-Júnior, A.J.S.; Russo, T.M.S.; Paraizo-Horvath, C.M.S.; Teles, A.P.S.; Sonobe, H.M. Familial Coping and Problem-solving in the Care of Children and Adolescents Undergoing Oncological Treatment: A Scoping Review. OSF 2024. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web, and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Centre for Evidence-Based Medicine. Levels of Evidence. 2019. Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009 (accessed on 20 April 2024).
- Wózniak, L.; Izycki, D. Cancer: A family at risk. Prz. Menopauzalny. 2014, 13, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Mu, P.F.; Lee, M.Y.; Sheng, C.C.; Tung, P.C.; Huang, L.Y.; Chen, Y.W. The experiences of family members in the year following the diagnosis of a child or adolescent with cancer: A qualitative systematic review. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 293–329. [Google Scholar] [CrossRef]
- Popp, J.M.; Conway, M.; Pantaleao, A. Parents’ Experience with Their Child’s Cancer Diagnosis: Do Hopefulness, Family Functioning, and Perceptions of Care Matter? J. Pediatr. Oncol. Nurs. 2015, 32, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Nóia, T.C.; Sant’Ana, R.S.E.; Santos, A.D.S.; Oliveira, S.C.; Veras, S.M.C.B.; Lopes-Júnior, L.C. Coping with the diagnosis and hospitalization of a child with childhood cancer. Investig. Educ. Enferm. 2015, 33, 465–472. [Google Scholar] [CrossRef]
- van de Geest, I.M.M.; van den Heuvel-Eibrink, M.M.; Nette-Falkenburg, M.A.; Michiels, E.M.C.; van Vliet, L.; Pieters, R.; Darlington, A.-S.E. Parents’ Faith and Hope during the Pediatric Palliative Phase and the Association with Long-Term Parental Adjustment. J. Palliat. Med. 2015, 18, 402–407. [Google Scholar] [CrossRef] [PubMed]
- He-Shan, M.S.N.; Li-Ming, Y.; Zheng, J.; Bi, Y.L. Uncertainty and Personal Growth Through Positive Coping Strategies Among Chinese Parents of Children with Acute Leukemia. Cancer Nurs. 2016, 39, 202–212. [Google Scholar] [CrossRef]
- Lakkis, N.A.; Khoury, J.M.; Mahmassani, D.M.; Ramia, M.S.; Hamadeh, G.N. Psychological distress and coping strategies in parents of children with cancer in Lebanon. Psycho-Oncology 2016, 25, 428–434. [Google Scholar] [CrossRef]
- Penner, L.A.; Guevarra, D.A.; Harper, F.W.; Taub, J.; Phipps, S.; Albrecht, T.L.; Kross, E. Self-distancing Buffers High Trait Anxious Pediatric Cancer Caregivers against Short- and Longer-term Distress. Clin. Psychol. Sci. 2016, 4, 629–640. [Google Scholar] [CrossRef]
- Cox, T. Caregivers reflecting on the early days of childhood cancer. Eur. J. Cancer Care 2016, 27, e12499. [Google Scholar] [CrossRef]
- Hendricks-Ferguson, V.L.; Pradhan, K.; Shih, C.S.; Gauvain, K.M.; Kane, J.R.; Liu, J.; Haase, J.E. Pilot Evaluation of a Palliative and Endof-Life Communication Intervention for Parents of Children with a Brain Tumor. J. Pediatr. Oncol. Nurs. 2017, 34, 203–213. [Google Scholar] [CrossRef]
- Doumit, M.A.A.; Khoury, M.N. Facilitating and hindering factors for coping with the experience of having a child with cancer: A Lebanese perspective. J. Psychosoc. Oncol. 2017, 35, 346–361. [Google Scholar] [CrossRef]
- Wiener, L.; Battles, H.; Zadeh, S.; Pelletier, W.; Arruda-Coll, M.N.F.; Muriel, A. The perceived influence of childhood cancer on the parents’ relationship. Psycho-Oncology 2017, 26, 2109–2117. [Google Scholar] [CrossRef] [PubMed]
- Abdoljabbari, M.; Sheikhzakaryaee, N.; Atashzadeh- Shoorideh, F. Taking Refuge in Spirituality, a Main Strategy of Parents of Children with Cancer: A Qualitative Study. Asian Pac. J. Cancer Prev. 2018, 19, 2575–2580. [Google Scholar] [CrossRef]
- Chivukula, U.; Kota, S.; Nandinee, D. Burden Experience of Caregivers of Acute Lymphoblastic Leukemia: Impact of Coping and Spirituality. Indian J. Palliat. Care 2018, 24, 189–195. [Google Scholar] [CrossRef]
- Cutillo, A.; Zimmerman, K.; Davies, S.; Madan-Swain, A.; Landier, W.; Arynchyna, A.; Rocque, B.G. Coping strategies used by caregivers of children with newly diagnosed brain tumors. J. Neurosurg. Pediatr. 2018, 23, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Nikfarid, L.; Rassouli, M.; Borimnejad, L.; Alavimajd, H. Religious Coping in Iranian Mothers of Children with Cancer: A Qualitative Content Analysis. J. Pediatr. Oncol. Nurs. 2018, 35, 188–198. [Google Scholar] [CrossRef] [PubMed]
- Doumit, M.A.A.; Rahi, A.C.; Saab, R.; Majdalani, M. Spirituality among parents of children with cancer in a Middle Eastern country. Eur. J. Oncol. Nurs. 2019, 39, 21–27. [Google Scholar] [CrossRef]
- Clever, K.; Schepper, F.; Maier, S.; Christiansen, H.; Martini, J. Individual and Dyadic Coping and Fear of Progression in Mothers and Fathers of Children with Hematologic Cancer. Fam. Process. 2019, 59, 1225–1242. [Google Scholar] [CrossRef]
- Lyu, Q.Y.; Wong, F.K.Y.; You, L.M.; Li, X.W. Perceived Family Impact During Children’s Hospitalization for Treatment of Acute Lymphoblastic Leukemia: A Cross-sectional Study. Cancer Nurs. 2019, 43, 489–497. [Google Scholar] [CrossRef] [PubMed]
- de Paula, D.P.S.; da Silva, G.R.C.; Andrade, J.M.O.; Paraiso, A.F. Cancer in children and adolescents in the family settings: Perceptions and experiences with respect to their diagnosis. Rev. Cuid. 2019, 10, 1–12. [Google Scholar] [CrossRef]
- Díaz-Morales, K.; Reyes-Arvizu, J.; Morgado-Nájera, K.; Everardo-Domínguez, D.M. Symptoms of cancer in children and family care strategies. Rev. Cuid. 2019, 10, 1–12. [Google Scholar] [CrossRef]
- Schoors, M.V.; de Paepe, A.L.; Lemiere, J.; Morez, A.; Norga, K.; Lambrecht, K.; Goubert, L.; Verhofstadt, L.L. Family Adjustment When Facing Pediatric Cancer: The Role of Parental Psychological Flexibility, Dyadic Coping, and Network Support. Front. Psychol. 2019, 10, 2740. [Google Scholar] [CrossRef] [PubMed]
- Lyu, Q.Y.; Zhang, M.F.; Bu, X.Q.; Zhou, X.Z.; Zhao, X. A Qualitative Study Exploring Coping Strategies in Chinese Families During Children’s Hospitalization for Cancer Treatment. J. Pediatr. Nurs. 2019, 48, 27–34. [Google Scholar] [CrossRef]
- Salvador, A.; Crespo, C.; Barros, L. Parents’ psychological well-being when a child has cancer: Contribution of individual and family factors. Psycho-Oncology 2019, 28, 1080–1087. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Petrini, M.A.; Luo, D.; Yang, B.X.; Yang, J.; Haase, J.E. Parents’ Experiences of Having a Young Child with Acute Lymphoblastic Leukemia in China. J. Pediatr. Oncol. Nurs. 2020, 38, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Padeniya, R.N.; Thushari, G.; Nissanka, D.H.; Shashika, C.; Munasinghe, D.H.; Aberathne, D.M.; Weerawardena, P.L.; Galgamuwa, L.S.; Kumarasinghe, N.; Liyanage, L. Maternal coping strategies in response to child’s oncological diseases in Sri Lanka. Acta Oncol. 2020, 59, 866–871. [Google Scholar] [CrossRef] [PubMed]
- Tan, R.; Koh, S.; Wong, M.E.; Rui, M.; Shorey, S. Caregiver Stress, Coping Strategies, and Support Needs of Mothers Caring for their Children Who Are Undergoing Active Cancer Treatments. Clin. Nurs. Res. 2020, 29, 460–468. [Google Scholar] [CrossRef]
- Omari, O.A.; Roach, E.J.; Shakman, L.; Hashmi, A.A.; Sunderraj, S.J.; Francis, F.; Joseph, M.A. The Lived Experiences of Mothers Who Are Parenting Children with Leukemia. Cancer Nurs. 2021, 44, 374–381. [Google Scholar] [CrossRef]
- López, J.; Velasco, C.; Noriega, C. The role of acceptance in parents whose child suffers from cancer. Eur. J. Cancer Care 2021, 30, e13406. [Google Scholar] [CrossRef] [PubMed]
- Koumarianou, A.; Symeonidi, A.E.; Kattamis, A.; Linardatou, K.; Chrousos, G.P.; Darviri, C. A review of psychosocial interventions targeting families of children with cancer. Palliat. Support. Care 2021, 19, 103–118. [Google Scholar] [CrossRef] [PubMed]
- Yeung, N.C.Y.; Cheung, K.C.; Chau, H.C.; Leung, A.W.K.; Li, C.K.; Lam, T.T.N.; Cheng, H.Y.; Cheung, Y.T. Transition from Acute Treatment to Survivorship: Exploring the Psychosocial Adjustments of Chinese Parents of Children with Cancer or Hematological Disorders. Int. J. Environ. Res. Public Health 2021, 18, 7815. [Google Scholar] [CrossRef] [PubMed]
- Basile, N.L.; Chardon, M.L.; Peugh, J.; Edwards, C.S.; Szulczewski, L.; Morrison, C.F. Relationship Between Caregiver Uncertainty, Problem-Solving, and Psychological Adjustment in Pediatric Cancer. J. Pediatr. Psychol. 2021, 46, 1258–1266. [Google Scholar] [CrossRef] [PubMed]
- Miller, T.T.; Maurer, S.H.; Felker, J.T. Searching for a cure on Facebook: Patterns of social media use amongst caregivers of children with brain tumors. Cancer Med. 2022, 11, 3323–3331. [Google Scholar] [CrossRef] [PubMed]
- Farinha, F.T.; Araújo, C.M.F.; Mucherone, P.V.V.; Batista, N.T.; Trettene, A.S. Influence of religiosity/spirituality on informal caregivers of children with leukemia. Rev. Bioét. 2023, 30, 892–899. [Google Scholar] [CrossRef]
- Wang, M.J.; Chang, M.Y.; Cheng, M.Y.; Zhang, R.X. The Psychological Adaptation Process in Chinese Parent Caregivers of Pediatric Leukemia Patients: A Qualitative Analysis. Cancer Nurs. 2022, 45, 835–842. [Google Scholar] [CrossRef]
- Eche, I.J.; Eche, I.M.; Pires, C.; Isibor, C.; Achibiri, A.; Aronowitz, T. A Systematic Mixed-Studies Review of Hope Experiences in Parents of Children with Cancer. Cancer Nurs. 2022, 45, 43–58. [Google Scholar] [CrossRef]
- Chong, A.S.S.; Ahmad, M.B.; Alias, H.; Hussain, R.B.I.; Lateh, A.B.; Chan, C.M.H. Spiritual Coping Among Families of Children with Cancer: A Qualitative Study. Asia Pac. J. Public Health 2023, 35, 408–412. [Google Scholar] [CrossRef]
- Deribe, L.; Addissie, A.; Girma, E.; Abraha, A.; Adam, H.; Lindström, N.B. Stress and coping strategies among parents of children with cancer at Tikur Anbessa Specialized Hospital paediatric oncology unit, Ethiopia: A phenomenological study. BMJ Open 2023, 13, e065090. [Google Scholar] [CrossRef]
- Ochoa-Dominguez, C.Y.; Miller, K.A.; Banegas, M.P.; Sabater-Minarim, D.; Chan, R.Y. Psychological Impact and Coping Strategies of Hispanic Parents of Children with Cancer: A Qualitative Study. Int. J. Environ. Res. Public Health 2023, 20, 5928. [Google Scholar] [CrossRef] [PubMed]
- Phiri, L.; Cheung, W.H.; Cheung, A.T.; Phiri, P.G.M.C. Effectiveness of psychoeducation interventions in reducing negative psychological outcomes and improving coping skills in caregivers of children with cancer: A systematic review and meta-analysis. Psycho-Oncology 2023, 32, 1514–1527. [Google Scholar] [CrossRef] [PubMed]
- Bates, C.R.; Pallotto, I.K.; Moore, R.M.; Covitz, L.M.; Gillette, M.L.D. Barriers and facilitators of family rules and routines during pediatric cancer treatment. J. Pediatr. Nurs. 2023, 72, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Smith, N.D.W.; Bonne, D.M.; Schimmel-Bristow, A.; Rawlins, J.; Ellingham, L.; Sobalvarro, S.; Faith, M.A. The mediating role of caregiver hope in relations among caregivers’ coping and emotional socialization beliefs in pediatric oncology. J. Psychosoc. Oncol. 2024, 42, 271–285. [Google Scholar] [CrossRef] [PubMed]
- Bates, C.R.; Staggs, V.; Dean, K.M.; August, K.J.; Befort, C.A.; Covitz, L.M.; Gillette, M.L.D. Family Rules and Routines During the Early Phases of Pediatric Cancer Treatment: Associations with Child Emotional and Behavioral Health. J. Pediatr. Psychol. 2024, 49, 66–76. [Google Scholar] [CrossRef] [PubMed]
- Folkman, S.; Moskowitz, J.T. Coping: Pitfalls and promise. Annu. Rev. Psychol. 2004, 55, 745–774. [Google Scholar] [CrossRef] [PubMed]
- Skinner, E.A.; Edge, K.; Altman, J.; Sherwood, H. Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychol. Bull. 2003, 129, 216–269. [Google Scholar] [CrossRef]
- Compas, B.E.; Connor-Smith, J.K.; Saltzman, H.; Thomsen, A.H.; Wadsworth, M.E. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychol. Bull. 2001, 127, 87–127. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.H.; Xia, W.; He, X.L.; Zhang, J.P.; Li, H.C.W. Psychological interventions for enhancing resilience in parents of children with cancer: A systematic review and meta-analysis. Support. Care Cancer 2021, 29, 7101–7110. [Google Scholar] [CrossRef]
- Melguizo-Garín, A.; Benítez-Márquez, M.; Hombrados-Mendieta, I.; Martos-Méndez, M.J. Importance of Social Support of Parents of Children with Cancer: A Multicomponent Model Using Partial Least Squares-Path Modelling. Int. J. Environ. Res. Public Health 2023, 20, 1757. [Google Scholar] [CrossRef]
- Nukpezah, R.N.; Fomani, F.K.; Hasanpour, M.; Nasrabadi, A.N. A qualitative study of Ghanaian pediatric oncology nurses’ care practice challenges. BMC Nurs. 2021, 20, 17. [Google Scholar] [CrossRef]
- Lin, B.; Gutman, T.; Hanson, C.S.; Ju, A.; Manera, K.; Butow, P.; Cohn, R.J.; Dalla-Pozza, L.; Greenzang, K.A.; Mack, J.; et al. Communication during childhood cancer: Systematic review of patient perspectives. Cancer 2019, 26, 701–716. [Google Scholar] [CrossRef]
- Mardhiyah, A.; Panduragan, S.L.; Mediani, H.S. Reducing Psychological Impacts on Children with Chronic Disease via Family Empowerment: A Scoping Review. Healthcare 2022, 10, 2034. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).