Adherence to Mediterranean Diet and Selected Lifestyle Elements among Young Women with Type 1 Diabetes Mellitus from Northeast Poland: A Case-Control COVID-19 Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Questionnaire
2.3. Statistical Analysis
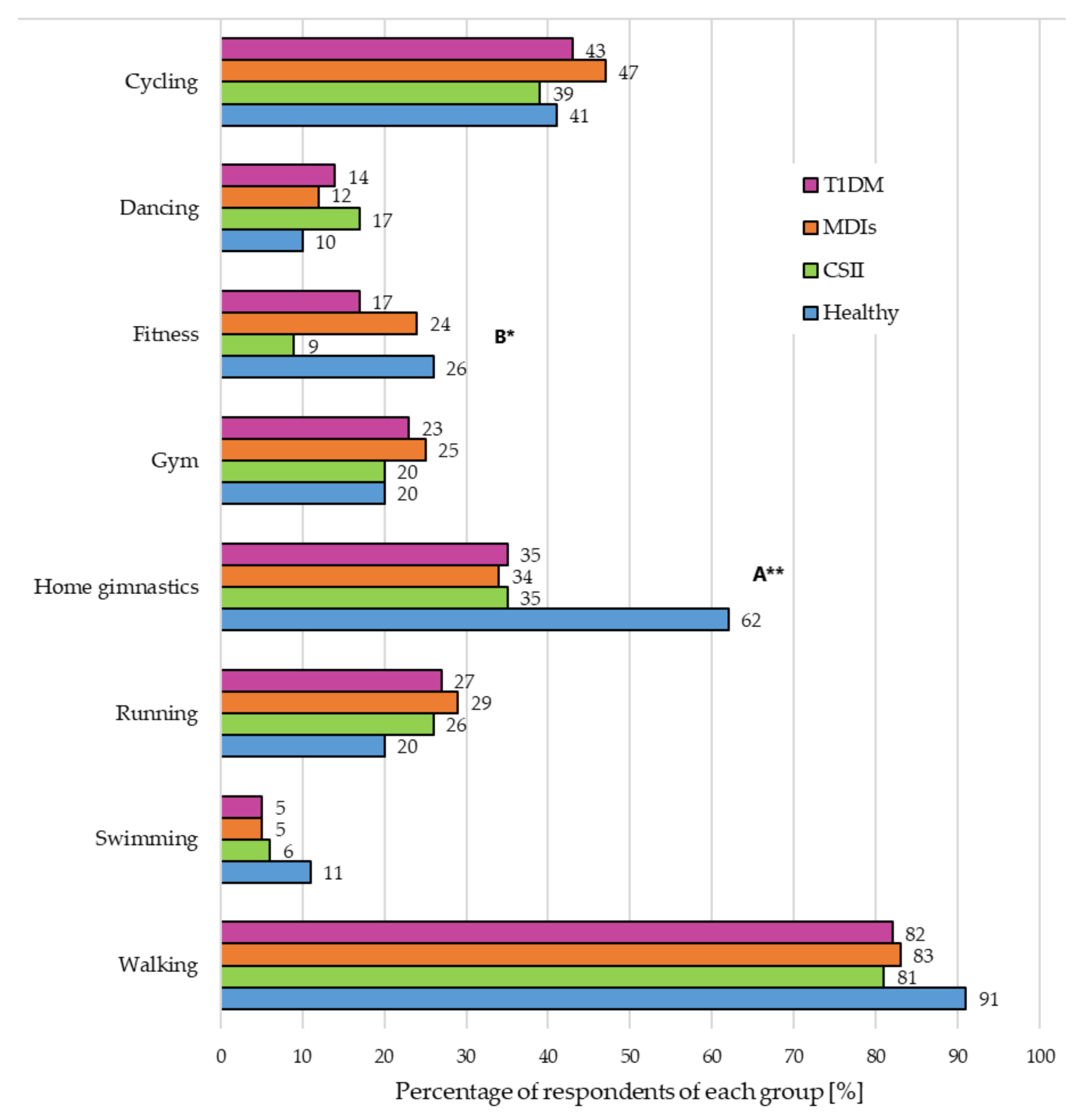
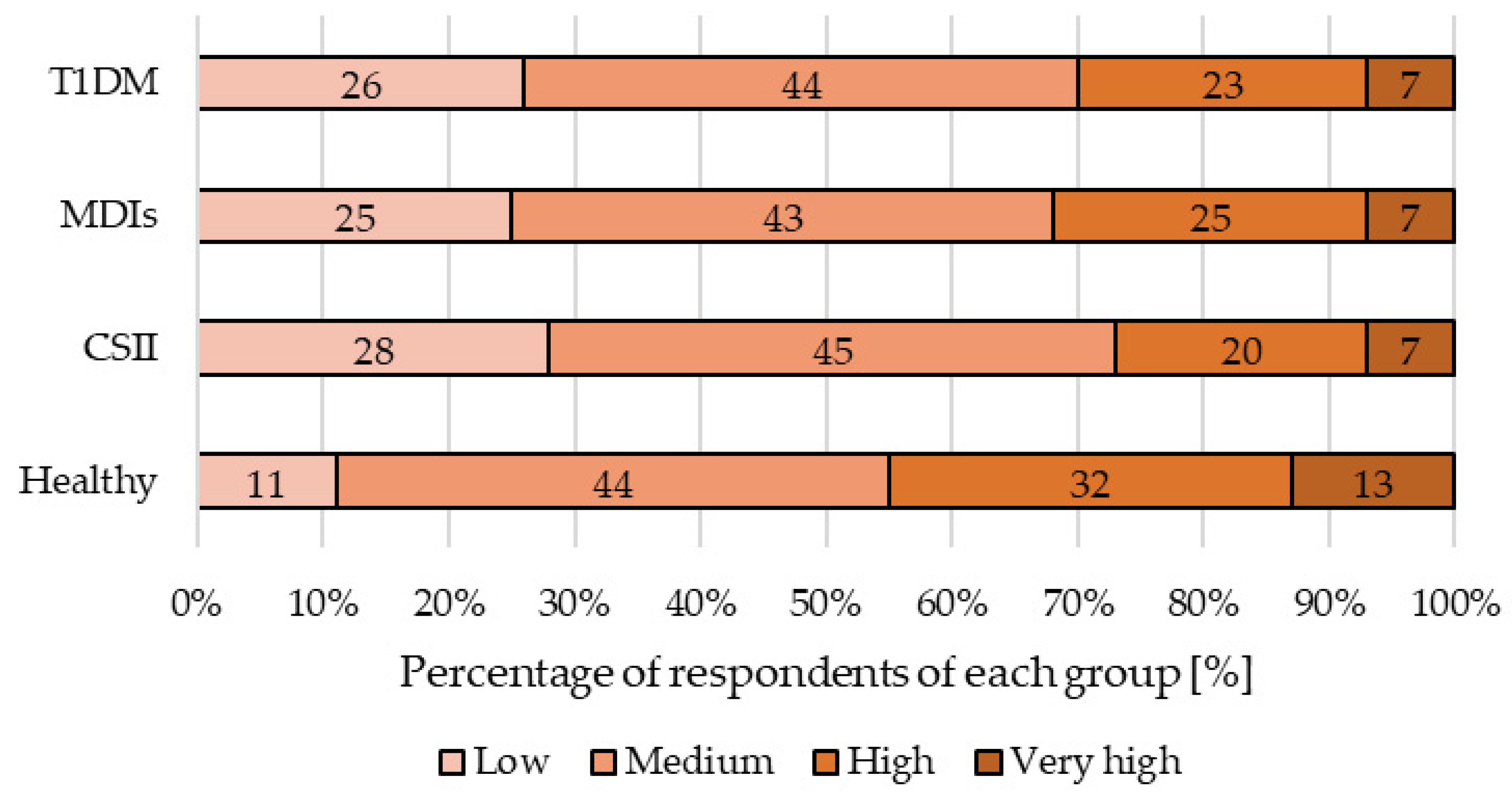
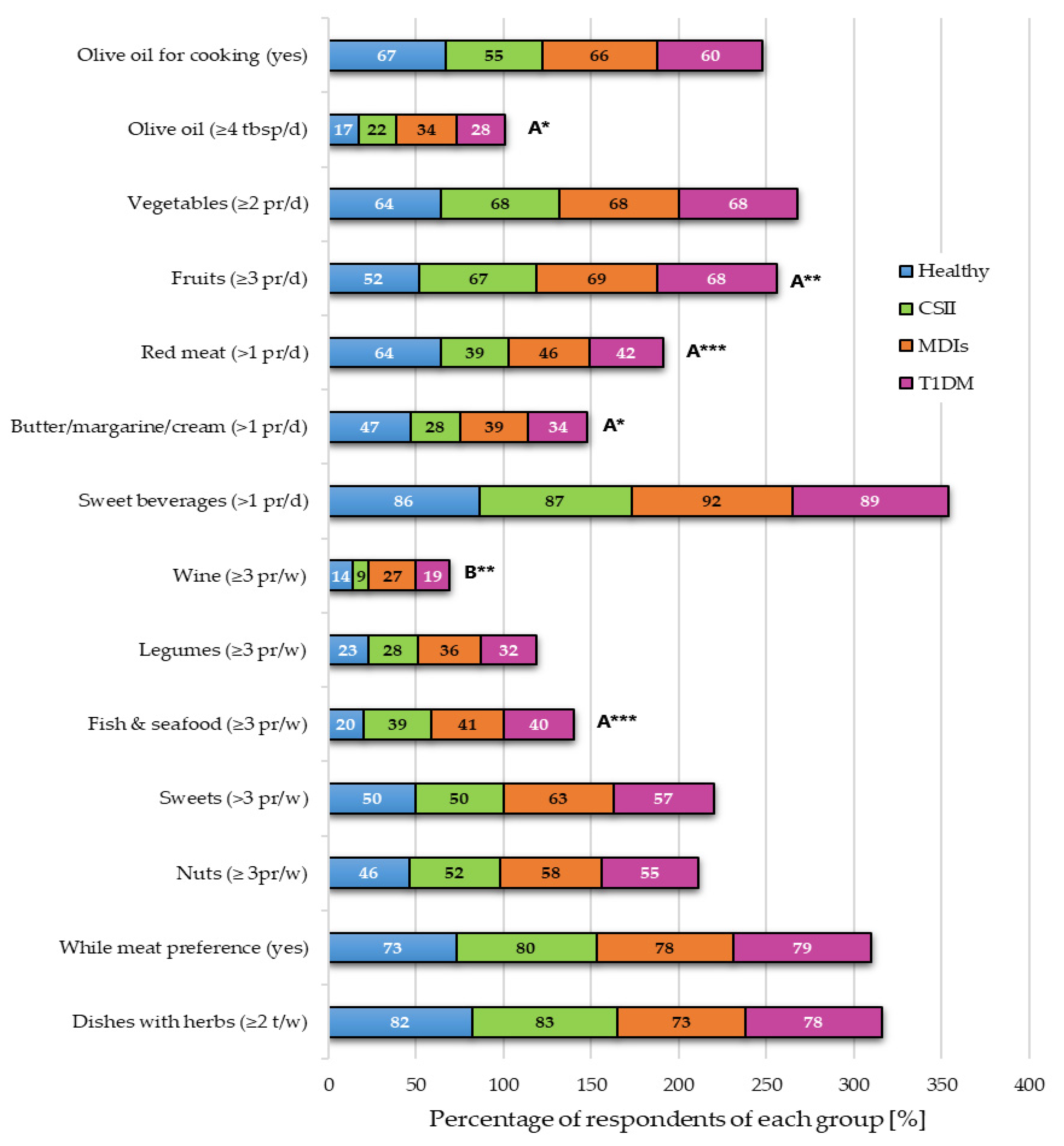
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alberti, K.G.; Zimmet, P.Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet. Med. 1998, 15, 539–553. [Google Scholar] [CrossRef]
- Khan, M.; Adil, S.F.; Alkhathlan, H.Z.; Tahir, M.N.; Saif, S.; Khan, M.; Khan, S.T. COVID-19: A Global Challenge with Old History, Epidemiology and Progress So Far. Molecules 2021, 26, 39. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.L.; Raheem, D.; Ramos, F.; Carrascosa, C.; Saraiva, A.; Raposo, A. Highlights of Current Dietary Guidelines in Five Continents. Int. J. Environ. Res. Public Health 2021, 18, 2814. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Tomaino, L.; Dernini, S.; Berry, E.M.; Lairon, D.; de la Cruz, J.N.; Bach-Faig, A.; Donini, L.M.; Medina, F.-X.; Belahsen, R.; et al. Updating the Mediterranean Diet Pyramid towards Sustainability: Focus on Environmental Concerns. Int. J. Environ. Res. Public Health 2020, 17, 8758. [Google Scholar] [CrossRef]
- Valls-Pedret, C.; Sala-Vila, A.; Serra-Mir, M.; Corella, D.; de la Torre, R.; Martínez-González, M.; Martínez-Lapiscina, E.H.; Fitó, M.; Pérez-Heras, A.; Salas-Salvadó, J.; et al. Mediterranean Diet and Age-Related Cognitive Decline: A Randomized Clinical Trial. JAMA Intern. Med. 2015, 175, 1094–1103. [Google Scholar] [CrossRef]
- Franquesa, M.; Pujol-Busquets, G.; García-Fernández, E.; Rico, L.; Shamirian-Pulido, L.; Aguilar-Martínez, A.; Medina, F.X.; Serra-Majem, L.; Bach-Faig, A. Mediterranean Diet and Cardiodiabesity: A Systematic Review through Evidence-Based Answers to Key Clinical Questions. Nutrients 2019, 11, 655. [Google Scholar] [CrossRef]
- Pérez-Martínez, P.; Mikhailidis, D.P.; Athyros, V.G.; Bullo, M.; Couture, P.; Covas, M.I.; de Koning, L.; Delgado-Lista, J.; Díaz-López, A.; Drevon, C.A.; et al. Lifestyle recommendations for the prevention and management of metabolic syndrome: An international panel recommendation. Nutr. Rev. 2017, 75, 307–326. [Google Scholar] [CrossRef]
- Gaforio, J.J.; Visioli, F.; Alarcón-de-la-Lastra, C.; Castañer, O.; Delgado-Rodríguez, M.; Fitó, M.; Hernández, A.F.; Huertas, J.R.; Martínez-González, M.A.; Menendez, J.A.; et al. Virgin Olive Oil and Health: Summary of the III International Conference on Virgin Olive Oil and Health Consensus Report, JAEN (Spain) 2018. Nutrients 2019, 11, 2039. [Google Scholar] [CrossRef]
- Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021, 44, S40–S52. [CrossRef]
- Kulaga, Z.; Litwin, M.; Tkaczyk, M.; Różdżyńska, A.; Barwicka, K.; Grajda, A.; Świąder, A.; Gurzkowska, B.; Napieralska, E.; Pan, H. The height-, weight-, and BMI-for-age of Polish school-aged children and adolescents relative to international and local growth references. BMC Public Health 2010, 10, 109. [Google Scholar] [CrossRef]
- World Health Organisation. The problem of overweight and obesity. In Obesity: Preventing and Managing the Global Epidemic; World Health Organisation: Geneva, Switzerland, 2000; Volume 894, pp. 5–13. [Google Scholar]
- Grabia, M.; Markiewicz-Żukowska, R.; Puścion-Jakubik, A.; Bielecka, J.; Nowakowski, P.; Gromkowska-Kępka, K.; Mielcarek, K.; Socha, K. The Nutritional and Health Effects of the COVID-19 Pandemic on Patients with Diabetes Mellitus. Nutrients 2020, 12, 3013. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Polish Ministry of Health. Available online: https://www.gov.pl/web/koronawirus/wykaz-zarazen-koronawirusem-sars-cov-2 (accessed on 14 March 2021).
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef] [PubMed]
- Błaszczyk-Bębenek, E.; Jagielski, P.; Bolesławska, I.; Jagielska, A.; Nitsch-Osuch, A.; Kawalec, P. Nutrition Behaviors in Polish Adults before and during COVID-19 Lockdown. Nutrients 2020, 12, 3084. [Google Scholar] [CrossRef] [PubMed]
- Price, S.A.; Gorelik, A.; Fourlanos, S.; Colman, P.G.; Wentworth, J.M. Obesity is associated with retinopathy and macrovascular disease in type 1 diabetes. Obes. Res. Clin. Pract. 2014, 8, e178–e182. [Google Scholar] [CrossRef]
- Islam, S.T.; Abraham, A.; Donaghue, K.C.; Chan, A.K.; Lloyd, M.; Srinivasan, S.; Craig, M.E. Plateau of adiposity in Australian children diagnosed with Type 1 diabetes: A 20-year study. Diabet. Med. 2014, 31, 686–690. [Google Scholar] [CrossRef]
- Vestberg, D.; Rosengren, A.; Olsson, M.; Gudbjörnsdottir, S.; Svensson, A.M.; Lind, M. Relationship between overweight and obesity with hospitalization for heart failure in 20,985 patients with type 1 diabetes: A population-based study from the Swedish National Diabetes Registry. Diabetes Care 2013, 36, 2857–2861. [Google Scholar] [CrossRef]
- Arora, T.; Grey, I. Health behaviour changes during COVID-19 and the potential consequences: A mini-review. J. Health Psychol. 2020, 25, 1155–1163. [Google Scholar] [CrossRef]
- Matias, T.; Dominski, F.H.; Marks, D.F. Human needs in COVID-19 isolation. J. Health Psychol. 2020, 25, 871–882. [Google Scholar] [CrossRef]
- Von Ruesten, A.; Weikert, C.; Fietze, I.; Boeing, H. Association of sleep duration with chronic diseases in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam study. PLoS ONE 2012, 7, e30972. [Google Scholar] [CrossRef]
- Spiegel, K.; Knutson, K.; Leproult, R.; Tasali, E.; Van Cauter, E. Sleep loss: A novel risk factor for insulin resistance and Type 2 diabetes. J. Appl. Physiol. 2005, 99, 2008–2019. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, K.; Tasali, E.; Penev, P.; Van Cauter, E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann. Intern. Med. 2004, 141, 846–850. [Google Scholar] [CrossRef] [PubMed]
- Mayer-Davis, E.J.; Ma, B.; Lawson, A.; D’Agostino, R.B.; Liese, A.D.; Bell, R.A.; Dabelea, D.; Dolan, L.; Pettitt, D.J.; Rodriguez, B.L.; et al. Cardiovascular disease risk factors in youth with type 1 and type 2 diabetes: Implications of a factor analysis of clustering. Metab. Syndr. Relat. Disord. 2009, 7, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Vidal-Peracho, C.; Tricás-Moreno, J.M.; Lucha-López, A.C.; Lucha-López, M.O.; Camuñas-Pescador, A.C.; Caverni-Muñoz, A.; Fanlo-Mazas, P. Adherence to Mediterranean Diet Pattern among Spanish Adults Attending a Medical Centre: Nondiabetic Subjects and Type 1 and 2 Diabetic Patients. J. Diabetes Res. 2017, 2017, 5957821. [Google Scholar] [CrossRef]
- Granado-Casas, M.; Alcubierre, N.; Martín, M.; Real, J.; Ramírez-Morros, A.M.; Cuadrado, M.; Alonso, N.; Falguera, M.; Hernández, M.; Aguilera, E.; et al. Improved adherence to Mediterranean Diet in adults with type 1 diabetes mellitus. Eur. J. Nutr. 2019, 58, 2271–2279. [Google Scholar] [CrossRef]
- Yang, B.; Shi, L.; Wang, A.M.; Shi, M.Q.; Li, Z.H.; Zhao, F.; Guo, X.J.; Li, D. Lowering Effects of n-3 Fatty Acid Supplements on Blood Pressure by Reducing Plasma Angiotensin II in Inner Mongolia Hypertensive Patients: A Double-Blind Randomized Controlled Trial. J. Agric. Food Chem. 2019, 67, 184–192. [Google Scholar] [CrossRef]
- Calabrese, C.M.; Valentini, A.; Calabrese, G. Gut Microbiota and Type 1 Diabetes Mellitus: The Effect of Mediterranean Diet. Front. Nutr. 2021, 7. [Google Scholar] [CrossRef]
- Fraga, C.G.; Croft, K.D.; Kennedy, D.O.; Tomás-Barberán, F.A. The effects of polyphenols and other bioactives on human health. Food Funct. 2019, 10, 514–528. [Google Scholar] [CrossRef]
- Kim, Y.; Keogh, J.B.; Clifton, P.M. Polyphenols and Glycemic Control. Nutrients 2016, 8, 17. [Google Scholar] [CrossRef]
- Momtaz, S.; Salek-Maghsoudi, A.; Abdolghaffari, A.H.; Jasemi, E.; Rezazadeh, S.; Hassani, S.; Ziaee, M.; Abdollahi, M.; Behzad, S.; Nabavi, S.M. Polyphenols targeting diabetes via the AMP-activated protein kinase pathway; future approach to drug discovery. Crit. Rev. Clin. Lab. Sci. 2019, 56, 472–492. [Google Scholar] [CrossRef] [PubMed]
- Polsky, S.; Ellis, S.L. Obesity, insulin resistance, and type 1 diabetes mellitus. Curr. Opin. Endocrinol. Diabetes Obes. 2015, 22, 277–282. [Google Scholar] [CrossRef]
- Wilkin, T.J. The accelerator hypothesis: Weight gain as the missing link between Type I and Type II diabetes. Diabetologia 2001, 44, 914–922. [Google Scholar] [CrossRef]
- Islam, S.T.; Srinivasan, S.; Craig, M.E. Environmental determinants of type 1 diabetes: A role for overweight and insulin resistance. J. Paediatr. Child Health 2014, 50, 874–879. [Google Scholar] [CrossRef] [PubMed]
- Dahlquist, G. Can we slow the rising incidence of childhood-onset autoimmune diabetes? The overload hypothesis. Diabetologia 2006, 49, 20–24. [Google Scholar] [CrossRef]
- Kaštelan, S.; Salopek Rabatić, J.; Tomić, M.; Gverović Antunica, A.; Ljubić, S.; Kaštelan, H.; Novak, B.; Orešković, D. Body Mass Index and Retinopathy in Type 1 Diabetic Patients. Int. J. Endocrinol. 2014, 2014, 387919. [Google Scholar] [CrossRef] [PubMed]
- Pinhas-Hamiel, O.; Levek-Motola, N.; Kaidar, K.; Boyko, V.; Tisch, E.; Mazor-Aronovitch, K.; Graf-Barel, C.; Landau, Z.; Lerner-Geva, L.; Frumkin Ben-David, R. Prevalence of overweight, obesity and metabolic syndrome components in children, adolescents and young adults with type 1 diabetes mellitus. Diabetes Metab. Res. Rev. 2015, 31, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Valerio, G.; Mozzillo, E.; Zito, E.; Nitto, E.D.; Maltoni, G.; Marigliano, M.; Zucchini, S.; Maffeis, C.; Franzese, A. Alcohol consumption or cigarette smoking and cardiovascular disease risk in youth with type 1 diabetes. Acta Diabetol. 2019, 56, 1315–1321. [Google Scholar] [CrossRef]
- Fortin, A.; Rabasa-Lhoret, R.; Lemieux, S.; Labonté, M.E.; Gingras, V. Comparison of a Mediterranean to a low-fat diet intervention in adults with type 1 diabetes and metabolic syndrome: A 6-month randomized trial. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 1275–1284. [Google Scholar] [CrossRef] [PubMed]
- Zhong, V.W.; Lamichhane, A.P.; Crandell, J.L.; Couch, S.C.; Liese, A.D.; The, N.S.; Tzeel, B.A.; Dabelea, D.; Lawrence, J.M.; Marcovina, S.M.; et al. Association of adherence to a Mediterranean diet with glycemic control and cardiovascular risk factors in youth with type I diabetes: The SEARCH Nutrition Ancillary Study. Eur. J. Clin. Nutr. 2016, 70, 802–807. [Google Scholar] [CrossRef]
- Kössler, T.; Weber, K.S.; Wölwer, W.; Hoyer, A.; Strassburger, K.; Burkart, V.; Szendroedi, J.; Roden, M.; Müssig, K.; Roden, M.; et al. Associations between cognitive performance and Mediterranean dietary pattern in patients with type 1 or type 2 diabetes mellitus. Nutr. Diabetes 2020, 10, 10. [Google Scholar] [CrossRef]
- Narodowy Fundusz Zdrowia. NFZ o Zdrowiu: Cukrzyca. Centrala Narodowego Funduszu Zdrowia. Available online: https://www.nfz.gov.pl/ (accessed on 5 October 2020).

| Question | Answer: Yes [Points] | Answer: No [Points] |
|---|---|---|
| 1. Is olive oil the major dietary fat in your diet? | 1 | 0 |
| 2. Do you consume at least 4 tablespoons of vegetable oil every day? | 1 | 0 |
| 3. Do you eat at least 2 servings (about 400 g) of vegetables every day? | 1 | 0 |
| 4. Do you eat at least 3 servings (about 240 g) of fruit every day? | 1 | 0 |
| 5. Do you eat less than 1 serving of red meat/other meat products every day? | 1 | 0 |
| 6. Do you eat less than 1 serving of butter, margarine or cream every day? | 1 | 0 |
| 7. Do you consume less than 1 serving of sweet or sugar-sweetened fizzy drinks every day? | 1 | 0 |
| 8. Do you consume more than 3 glasses (approx. 400 mL) of wine per week per week? | 1 | 0 |
| 9. Do you eat at least 3 servings (approx. 450 g) of legume seeds (peas, beans, broad beans, lentils, chickpeas) per week? | 1 | 0 |
| 10. Do you eat at least 3 servings (approx. 300 g) of fish or seafood weekly? | 1 | 0 |
| 11. Do you consume less than 3 servings of sweets (bought, homemade) weekly? | 1 | 0 |
| 12. Do you eat at least 30 g of nuts per week? | ||
| 13. Do you choose chicken, turkey or rabbit instead of veal, pork or sausage? | 1 | 0 |
| 14. Do you eat pasta, vegetable or rice dishes with garlic, tomatoes, leeks or onions more than twice a week? | 1 | 0 |
| TOTAL | 14 | 0 |
| Studied Parameters | T1DM | Healthy (n = 106) | ||
|---|---|---|---|---|
| Total (n = 113) | CSII (n = 54) | MDIs (n = 59) | ||
| Age (years) | 25 (20–29) | 21 (18–25) | 28 (23–32) | 22 (21–23) |
| Body weight (kg) A**, B*, C** | 71 (61–79) | 68 (61–78) | 72 (62–80) | 60 (56–68) |
| Height (cm) | 170 (165–174) | 170 (165–175) | 169 (163–174) | 168.5 (163–173) |
| Body mass index (kg/m2) A**, C** | 24.4 (21.6–27.7) | 23.6 (21.7–27.0) | 25.4 (22.4–28.4) | 21.9 (19.6–24.1) |
| HbA1c (%) F | 7.1 (6.5–8.0) | 7.0 (6.6–7.8) | 7.3 (6.4–8.2) | - |
| Place of residence | ||||
| Village | 15% | 15% | 15% | 24% |
| City (≤150 k inhabitants) | 29% | 24% | 32% | 27% |
| City (150–250 k inhabitants) | 27% | 30% | 25% | 8% |
| City (≥250 k inhabitants) | 29% | 31% | 27% | 42% |
| Duration of disease E** | ||||
| Up to 5 years | 18% | 28% | 8% | - |
| 5–10 years | 26% | 35% | 17% | - |
| More than 10 years | 56% | 37% | 75% | - |
| Body Mass Index D** | ||||
| Underweight | 5% | 7% | 3% | 8% |
| Normal | 50% | 56% | 45% | 72% |
| Overweight | 32% | 32% | 32% | 17% |
| Obesity | 13% | 5% | 20% | 3% |
| Studied Parameters | T1DM | Healthy (n = 106) | ||
|---|---|---|---|---|
| Total (n = 113) | CSII (n = 54) | MDIs (n = 59) | ||
| Sleep length A** | ||||
| <5 h | 8% | 8% | 8% | 4% |
| 5–8 h | 46% | 46% | 46% | 73% |
| >8 h | 46% | 46% | 46% | 23% |
| Screen time B* | ||||
| <2 h | 10% | 3% | 17% | 5% |
| 2–4 h | 26% | 26% | 27% | 28% |
| 5–7 h | 40% | 54% | 27% | 48% |
| ≥8 h | 24% | 17% | 29% | 18% |
| Number of meals A** | ||||
| 1–2 times/day | 5% | 8% | 3% | 14% |
| 3–4 times/day | 54% | 46% | 61% | 66% |
| ≥5 times/day | 41% | 46% | 36% | 20% |
| Low Medas (n = 41) | Medium Medas (n = 144) | High Medas (n = 34) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Studied Parameters | T1DM | Healthy (n = 26) | T1DM | Healthy (n = 64) | T1DM | Healthy (n = 16) | ||||||
| Total (n = 15) | CSII (n = 11) | MDIs (n = 4) | Total (n = 80) | CSII (n = 37) | MDIs (n = 43) | Total (n = 18) | CSII (n = 6) | MDIs (n = 12) | ||||
| Weekly activity | ||||||||||||
| No activity | 40% | 46% | 25% | 35% | 25% | 24% | 26% | 9% | 50% | 50% | 50% | 6% |
| 1–2 times/week | 33% | 27% | 50% | 31% | 40% | 46% | 35% | 41% | 42% | 17% | 42% | 31% |
| 3–4 times/week | 27% | 27% | 25% | 27% | 26% | 20% | 32% | 36% | 8% | 33% | 8% | 44% |
| ≥5 times/week | - | - | 46% | 7% | 9% | 10% | 7% | 14% | - | - | - | 19% |
| Sleep length | ||||||||||||
| <5 h | 60% | 64% | 50% | 12% | 8% | 8% | 7% | 2% | 17% | 17% | 17% | 81% |
| 5–8 h | - | - | - | 81% | 45% | 41% | 49% | 67% | 33% | 50% | 33% | - |
| >8 h | 40% | 36% | 50% | 7% | 47% | 51% | 44% | 31% | 50% | 33% | 50% | 19% |
| Screen time | ||||||||||||
| <2 h | - | - | - | 12% | 10% | 2% | 17% | 2% | 22% | 17% | 25% | 12.5% |
| 2–4 h | 13% | 9% | 25% | 15% | 26% | 22% | 30% | 34% | 39% | 83% | 17% | 25% |
| 5–7 h | 47% | 55% | 25% | 58% | 45% | 62% | 30% | 44% | 11% | - | 17% | 50% |
| ≥8 h | 40% | 36% | 50% | 15% | 19% | 14% | 23% | 20% | 28% | - | 41% | 12.5% |
| Stress level | ||||||||||||
| Low | 47% | 37% | 75% | 12% | 25% | 30% | 21% | 10% | 39% | 37% | 75% | 13% |
| Medium | 20% | 27% | - | 42% | 44% | 49% | 4% | 45% | 17% | 27% | - | 42% |
| High | 13% | 18% | - | 19% | 25% | 16% | 32% | 34% | 27% | 18% | - | 18% |
| Very high | 20% | 18% | 25% | 27% | 6% | 5% | 7% | 11% | 17% | 18% | 25% | 27% |
| Number of meals | ||||||||||||
| 1–2 times/day | 20% | 18% | 25% | 19% | 39% | 5% | 67% | 14% | 28% | 67% | 8% | 6% |
| 3–4 times/day | 53% | 55% | 50% | 54% | 19% | 41% | - | 69% | 28% | - | 42% | 75% |
| ≥5 times/day | 27% | 27% | 25% | 27% | 42% | 54% | 33% | 17% | 44% | 33% | 50% | 19% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grabia, M.; Puścion-Jakubik, A.; Markiewicz-Żukowska, R.; Bielecka, J.; Mielech, A.; Nowakowski, P.; Socha, K. Adherence to Mediterranean Diet and Selected Lifestyle Elements among Young Women with Type 1 Diabetes Mellitus from Northeast Poland: A Case-Control COVID-19 Survey. Nutrients 2021, 13, 1173. https://doi.org/10.3390/nu13041173
Grabia M, Puścion-Jakubik A, Markiewicz-Żukowska R, Bielecka J, Mielech A, Nowakowski P, Socha K. Adherence to Mediterranean Diet and Selected Lifestyle Elements among Young Women with Type 1 Diabetes Mellitus from Northeast Poland: A Case-Control COVID-19 Survey. Nutrients. 2021; 13(4):1173. https://doi.org/10.3390/nu13041173
Chicago/Turabian StyleGrabia, Monika, Anna Puścion-Jakubik, Renata Markiewicz-Żukowska, Joanna Bielecka, Anita Mielech, Patryk Nowakowski, and Katarzyna Socha. 2021. "Adherence to Mediterranean Diet and Selected Lifestyle Elements among Young Women with Type 1 Diabetes Mellitus from Northeast Poland: A Case-Control COVID-19 Survey" Nutrients 13, no. 4: 1173. https://doi.org/10.3390/nu13041173
APA StyleGrabia, M., Puścion-Jakubik, A., Markiewicz-Żukowska, R., Bielecka, J., Mielech, A., Nowakowski, P., & Socha, K. (2021). Adherence to Mediterranean Diet and Selected Lifestyle Elements among Young Women with Type 1 Diabetes Mellitus from Northeast Poland: A Case-Control COVID-19 Survey. Nutrients, 13(4), 1173. https://doi.org/10.3390/nu13041173











