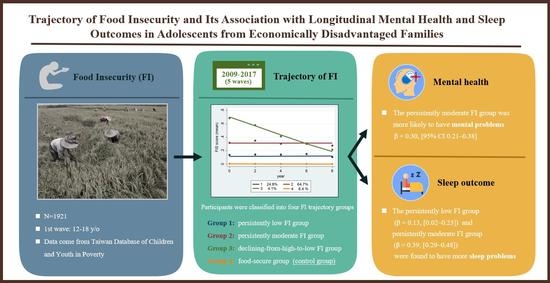
Trajectory of Food Insecurity and Its Association with Longitudinal Mental Health and Sleep Outcomes in Adolescents from Economically Disadvantaged Families
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Measures
2.2.1. Predictor Variable
2.2.2. Outcome Variables
2.3. Covariates
2.4. Analytic Strategy
3. Results
3.1. Demographic Characteristics
3.2. Food Insecurity Trajectories
3.3. Mental Health and Food Insecurity Trajectory
3.4. Sleep Outcomes and Food Insecurity Trajectory Membership
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schroeder, K.; Smaldone, A. Food Insecurity: A concept analysis. Nurs. Forum 2015, 50, 274–284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- More Must Be Done to Improve Food Security for Taiwan’s Poor: Council of Agriculture. Available online: https://www.taiwannews.com.tw/en/news/3528151 (accessed on 10 May 2021).
- Alaimo, K.; Olson, C.M.; Frongillo, E.A., Jr.; Briefel, R.R. Food insufficiency, family income, and health in US preschool and school-aged children. Am. J. Public Health 2001, 91, 781–786. [Google Scholar] [PubMed] [Green Version]
- Shankar, P.; Chung, R.; Frank, D.A. Association of food Insecurity with children’s behavioral, emotional, and academic outcomes: A systematic review. J. Dev. Behav. Pediatrics JDBP 2017, 38, 135–150. [Google Scholar] [CrossRef] [PubMed]
- Alaimo, K.; Olson, C.M.; Frongillo, E.A., Jr. Food insufficiency and American school-aged children’s cognitive, academic, and psychosocial development. Pediatrics 2001, 108, 44–53. [Google Scholar]
- Venci, B.J.; Lee, S.Y. Functional limitation and chronic diseases are associated with food insecurity among U.S. adults. Ann. Epidemiol. 2018, 28, 182–188. [Google Scholar] [CrossRef]
- Arenas, D.J.; Thomas, A.; Wang, J.; DeLisser, H.M. A systematic review and meta-analysis of depression, anxiety, and sleep disorders in US adults with food insecurity. J. Gen. Intern. Med. 2019, 34, 2874–2882. [Google Scholar] [CrossRef]
- Hamelin, A.-M.; Beaudry, M.; Habicht, J.-P. Characterization of household food insecurity in Quebec: Food and feelings. Soc. Sci. Med. 2002, 54, 119–132. [Google Scholar] [CrossRef]
- Nackers, L.M.; Appelhans, B.M. Food insecurity is linked to a food environment promoting obesity in households with children. J. Nutr. Educ. Behav. 2013, 45, 780–784. [Google Scholar] [CrossRef]
- McLaughlin, K.A.; Green, J.G.; Alegría, M.; Costello, E.J.; Gruber, M.J.; Sampson, N.A.; Kessler, R.C. Food insecurity and mental disorders in a national sample of US adolescents. J. Am. Acad. Child Adolesc. Psychiatry 2012, 51, 1293–1303. [Google Scholar] [CrossRef] [Green Version]
- Alaimo, K.; Olson, C.M.; Frongillo, E.A. Family food insufficiency, but not low family income, is positively associated with dysthymia and suicide symptoms in adolescents. J. Nutr. 2002, 132, 719–725. [Google Scholar] [CrossRef] [Green Version]
- Poole-Di Salvo, E.; Silver, E.J.; Stein, R.E. Household food insecurity and mental health problems among adolescents: What do parents report? Acad. Pediatrics 2016, 16, 90–96. [Google Scholar] [CrossRef]
- Burke, M.P.; Martini, L.H.; Çayır, E.; Hartline-Grafton, H.L.; Meade, R.L. Severity of household food insecurity is positively associated with mental disorders among children and adolescents in the United States. J. Nutr. 2016, 146, 2019–2026. [Google Scholar] [CrossRef] [Green Version]
- Nagata, J.M.; Palar, K.; Gooding, H.C.; Garber, A.K.; Whittle, H.J.; Bibbins-Domingo, K.; Weiser, S.D. Food insecurity is associated with poorer mental health and sleep outcomes in young adults. J. Adolesc. Health 2019, 65, 805–811. [Google Scholar] [CrossRef]
- Liang, Y.L.; Tsai, M.C.; Lin, Y.C.; Strong, C.; Lin, C.Y. Poverty and the prediction of health status in adolescents from low-income families in Taiwan. J. Public Health 2019, 42, 44–52. [Google Scholar] [CrossRef]
- Chen, C.-Y.; Hsiao, Y.-C. Dual trajectories of breakfast eating and fruit and vegetable intake over a 5-year follow-up period among economically disadvantaged children: Gender differences. Appetite 2018, 121, 41–49. [Google Scholar] [CrossRef]
- Wang, K.Y.-T.; Lyu, L.-C. An examination of food insecurity among economically disadvantaged youths in Taiwan. J. Asian Public Policy 2017, 10, 183–197. [Google Scholar] [CrossRef]
- Nord, M.; Hopwood, H. Recent advances provide improved tools for measuring children’s food security. J. Nutr. 2007, 137, 533–536. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.H.; Lin, C.Y.; Hsieh, Y.P.; Strong, C.; Meshki, C.; Lin, Y.C.; Tsai, M.-C. Dietary behaviors mediate the association between food insecurity and obesity among socioeconomically disadvantaged youth. Appetite 2019, 132, 275–281. [Google Scholar] [CrossRef]
- Nagin, D.S.; Odgers, C.L. Group-based trajectory modeling in clinical research. Annu. Rev. Clin. Psychol. 2010, 6, 109–138. [Google Scholar] [CrossRef] [Green Version]
- Ding, M.; Keiley, M.K.; Garza, K.B.; Duffy, P.A.; Zizza, C.A. Food insecurity is associated with poor sleep outcomes among US adults. J. Nutr. 2015, 145, 615–621. [Google Scholar] [CrossRef]
- Coplan, J.D.; Gupta, N.K.; Karim, A.; Rozenboym, A.; Smith, E.L.P.; Kral, J.G.; Rosenblum, L.A. Maternal hypothalamic-pituitary-adrenal axis response to foraging uncertainty: A model of individual vs. social allostasis and the “Superorganism Hypothesis”. PLoS ONE 2017, 12, e0184340. [Google Scholar] [CrossRef]
- Tarullo, A.R.; Tuladhar, C.T.; Kao, K.; Drury, E.B.; Meyer, J. Cortisol and socioeconomic status in early childhood: A multidimensional assessment. Dev. Psychopathol. 2020, 32, 1876–1887. [Google Scholar] [CrossRef]
- Bruening, M.; Dinour, L.M.; Chavez, J.B.R. Food insecurity and emotional health in the USA: A systematic narrative review of longitudinal research. Public Health Nutr. 2017, 20, 3200–3208. [Google Scholar] [CrossRef] [Green Version]
- Lachaud, J.; Mejia-Lancheros, C.; Wang, R.; Wiens, K.; Nisenbaum, R.; Stergiopoulos, V.; Hwang, S.W.; O’Camop, P. Mental and substance use disorders and food insecurity among homeless adults participating in the At Home/Chez Soi study. PLoS ONE 2020, 15, e0232001. [Google Scholar] [CrossRef]

| Characteristic | n | % |
|---|---|---|
| Food insecurity group | ||
| Declining from high to low FI group | 79 | 4.1% |
| Persistently moderate FI group | 1242 | 64.7% |
| Persistently low FI group | 477 | 24.8% |
| Food-secure group | 123 | 6.4% |
| Age, years, mean (SD) | 14.4 | (± 1.9) |
| Gender | ||
| Female | 1081 | 56.3% |
| Male | 840 | 43.7% |
| Family structure | ||
| Parents of foreign nationalities | 104 | 5.4% |
| Living with two parents | 403 | 21% |
| Household incomes per person-month * (NTD) | ||
| ≤3000 | 770 | 40.1% |
| 3001–6000 | 792 | 41.2% |
| ≥6001 | 359 | 18.7% |
| Variables | β | 95% CI | p Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Food insecurity group | ||||
| Declining from high to low | 0.187 | −0.023 | 0.398 | 0.081 |
| Persistently moderate | 0.297 | 0.212 | 0.382 | <0.001 |
| Persistently low | 0.091 | −0.001 | 0.182 | 0.052 |
| Gender | ||||
| Female | 0.113 | 0.063 | 0.163 | <0.001 |
| Household incomes (per person-10,000 NTD) | 0.013 | −0.085 | 0.110 | 0.798 |
| Family structure | ||||
| Parents of foreign nationality | −0.099 | −0.201 | 0.004 | 0.059 |
| Living with two parents | 0.041 | −0.019 | 0.101 | 0.182 |
| Variables | β | 95% CI | p Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Food insecurity group | ||||
| Declining from high to low | 0.223 | −0.012 | 0.458 | 0.063 |
| Persistently moderate | 0.387 | 0.290 | 0.484 | <0.001 |
| Persistently low | 0.128 | 0.023 | 0.234 | 0.017 |
| Gender | ||||
| Female | 0.127 | 0.065 | 0.188 | <0.001 |
| Household incomes (per person-10,000 NTD) | 0.050 | −0.117 | 0.126 | 0.936 |
| Family structure | ||||
| Parents of foreign nationality | −0.124 | −0.253 | 0.005 | 0.059 |
| Living with two parents | 0.013 | −0.064 | 0.089 | 0.747 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, T.-H.; Kuo, J.-H.; Liu, C.-Y.; Yu, Y.-F.; Strong, C.; Lin, C.-Y.; Lee, C.-T.; Tsai, M.-C. Trajectory of Food Insecurity and Its Association with Longitudinal Mental Health and Sleep Outcomes in Adolescents from Economically Disadvantaged Families. Nutrients 2021, 13, 1696. https://doi.org/10.3390/nu13051696
Lee T-H, Kuo J-H, Liu C-Y, Yu Y-F, Strong C, Lin C-Y, Lee C-T, Tsai M-C. Trajectory of Food Insecurity and Its Association with Longitudinal Mental Health and Sleep Outcomes in Adolescents from Economically Disadvantaged Families. Nutrients. 2021; 13(5):1696. https://doi.org/10.3390/nu13051696
Chicago/Turabian StyleLee, Ting-Hsuan, Jen-Hao Kuo, Chia-Yi Liu, Yi-Fang Yu, Carol Strong, Chung-Ying Lin, Chih-Ting Lee, and Meng-Che Tsai. 2021. "Trajectory of Food Insecurity and Its Association with Longitudinal Mental Health and Sleep Outcomes in Adolescents from Economically Disadvantaged Families" Nutrients 13, no. 5: 1696. https://doi.org/10.3390/nu13051696