Feasibility of a Community Healthy Eating and Cooking Intervention Featuring Traditional African Caribbean Foods from Participant and Staff Perspectives
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics
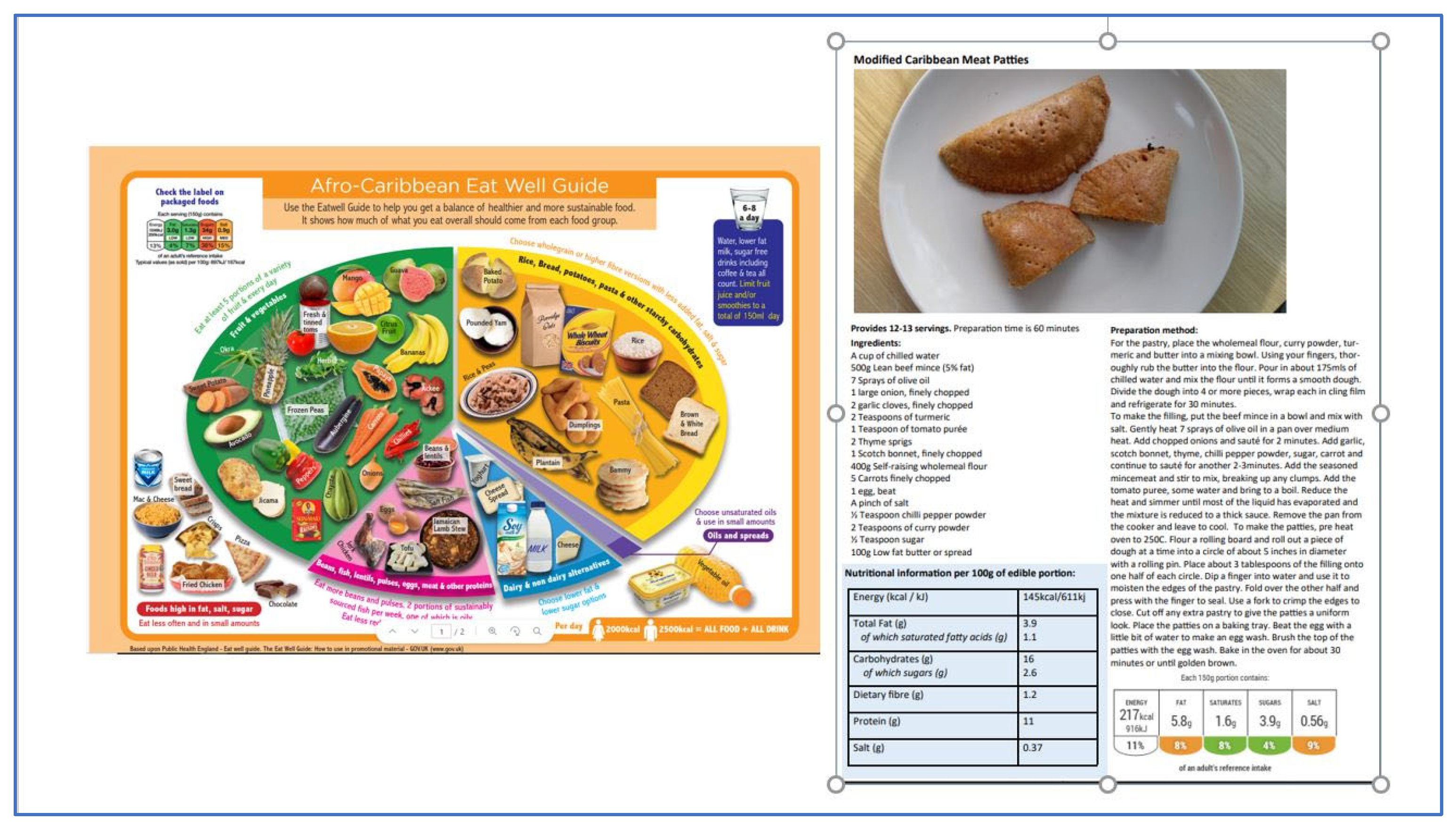
2.2. Intervention Development and Delivery
2.3. Recruitment of Community Service Users and Staff
2.4. Evaluation of Participant Perceptions of the Intervention, Including Acceptability and Relevance to Real Life
2.5. Participants Reported Compliance with Eat Well Guide Dietary Recommendations
2.6. Staff Perceptions of the Intervention and Evaluation of the Potential to Impact on Practice
2.7. Data Analysis
2.7.1. Evaluation of the Feasibility of the Intervention
2.7.2. Evaluation of the Potential for the Intervention to Impact Participants’ Healthy Eating-Related Skills, Knowledge and Behaviours
3. Results
3.1. Sample Characteristics
3.2. Participant Perceptions of the Intervention
3.3. Potential Impact of the Intervention on Participants’ Healthy Eating Awareness, Knowledge, Skills and Behaviours
Participants Perceived Compliance with Eat Well Guide Recommendations
3.4. Staff Views
4. Discussion
4.1. Key Findings
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- NHS Digital. Health Survey for England—2004, Health of Ethnic Minorities, Main Report. Official Statistics, National Statistics. 2006. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/health-survey-for-england-2004-health-of-ethnic-minorities-main-report (accessed on 1 June 2023).
- Harland, I.; Butriss, J.; Gibson, S. Achieving eatwell plate recommendations: Is this a route to improving both sustainability and healthy eating? Nutr. Bull. 2012, 37, 324–343. [Google Scholar] [CrossRef]
- Senior, L.; Maynard, M.; Apekey, T. Nutrient intake of African and Caribbean adults in the United Kingdom. A cross- sectional study. Proc. Nutr. Soc. 2022, 81, E225. [Google Scholar] [CrossRef]
- Apekey, T.A.; Copeman, J.; Kime, N.H.; Tashani, O.A.; Kittaneh, M.; Walsh, D. Nutrient Composition of Popularly Consumed African and Caribbean Foods in the UK. Foods 2019, 8, 500. [Google Scholar] [CrossRef]
- Goff, L.M.; Timbers, L.; Style, H.; Knight, A. Dietary intake in Black British adults; an observational assessment of nutritional composition and the role of traditional foods in UK Caribbean and West African diets. Public Health Nutr. 2015, 18, 2191–2201. [Google Scholar] [CrossRef]
- Food Foundation. Food Insecurity Tracker Update. 2023. Available online: https://foodfoundation.org.uk/publication/food-insecurity-tracker-update-families-continue-face-high-levels-food-insecurity (accessed on 1 July 2023).
- Office for Health Improvement and Disparities. All our Health Personalised Care and Population Health Collection. 2023. Available online: https://www.gov.uk/government/collections/all-our-health-personalised-care-and-population-health#:~:text=All%20Our%20Health%20is%20a,promotion%20of%20wellbeing%20and%20resilience (accessed on 1 July 2023).
- NHS Better Health Healthier Families, Healthier Recipes. 2020. Available online: https://www.nhs.uk/healthier-families/recipes/ (accessed on 1 July 2023).
- Moore, S.; Butler, T. UK government delays restriction of promotions on less-healthy foods: Serious implications for tackling obesity. Obesity 2022, 30, 1722–1723. [Google Scholar] [CrossRef]
- Poti, J.M.; Braga, B.; Qin, B. Ultra-processed food intake and obesity: What really matters for health—Processing or nutrient content? Curr. Obes. Rep. 2017, 6, 420–431. [Google Scholar] [CrossRef] [PubMed]
- British Dietetic Association (BDA). The Importance of Diversifying Healthy Eating Advice. Available online: https://www.bda.uk.com/resource/the-importance-of-diversifying-healthy-eating-advice.html (accessed on 29 September 2022).
- Kreuter, M.W.; Lukwago, S.N.; Bucholtz, D.C.; Clark, E.M.; Sanders-Thompson, V. Achieving Cultural Appropriateness in Health Promotion Programs: Targeted and Tailored Approaches. Health Educ. Behav. 2003, 30, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Leeds City Council. African Caribbean Eat Well Guide for Healthier Eating. 2022. Available online: https://www.leeds.gov.uk/phrc/resources/leaflets-and-posters (accessed on 1 July 2023).
- Moore, S.G.; Apekey, T.A.; Maynard, M.J. Co-developing multicultural recipe resources: An academic—Third sector partnership approach. Proc. Nutr. Soc. 2022, 81, E172. [Google Scholar]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How we design feasibility studies? Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef]
- Garcia, A.L.; Reardon, R.; McDonald, M.; Vargas-Garcia, E.J. Community Interventions to Improve Cooking Skills and Their Effects on Confidence and Eating Behaviour. Curr. Nutr. Rep. 2016, 5, 315–322. [Google Scholar] [CrossRef]
- Liu, J.; Davidson, E.; Bhopal, R.; White, M.; Johnson, M. Adapting health promotion interventions to meet the needs of ethnic minority groups: Mixed-methods evidence synthesis. Health Technol. Assess. 2012, 16, 1–469. [Google Scholar] [CrossRef]
- Public Health England. The Eat Well Guide. 2016. Available online: https://www.nhs.uk/live-well/eat-well/food-guidelines-and-food-labels/the-eatwell-guide/ (accessed on 1 July 2023).
- Croker, H.; Lucas, R.; Wardle, J. Cluster-randomised trial to evaluate the ‘Change for Life’ mass media/ social marketing campaign in the UK. BMC Public Health 2012, 12, 404. [Google Scholar] [CrossRef]
- Grunert, K.G.; Wills, J.M.; Fernández-Celemín, L. Nutrition knowledge, and use and understanding of nutrition information on food labels among consumers in the UK. Appetite 2010, 55, 177–189. [Google Scholar] [CrossRef]
- Garcia, A.L.; Reardon, R.; Hammond, E.; Parrett, A.; Gebbie-Diben, A. Evaluation of the “Eat Better Feel Better” Cooking Programme to Tackle Barriers to Healthy Eating. Int. J. Environ. Res. Public Health 2017, 14, 380. [Google Scholar] [CrossRef] [PubMed]
- Barton, K.L.; Wrieden, W.L.; Anderson, A.S. Validity and reliability of a short questionnaire for assessing the impact of cooking skills interventions. J. Hum. Nutr. Diet. 2011, 24, 588–595. [Google Scholar] [CrossRef]
- Ho, P.; Yeardley, E. Consumer Healthy Eating and Wellbeing 2020, Dataset. University of Leeds. Available online: https://archive.researchdata.leeds.ac.uk/857/ (accessed on 1 December 2022).
- Center for Substance Abuse Treatment (US). Improving Cultural Competence. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); (Treatment Improvement Protocol (TIP) Series, No. 59.) Appendix C, Tools for Assessing Cultural Competence. 2014. Available online: https://www.ncbi.nlm.nih.gov/books/NBK248429/ (accessed on 1 December 2022).
- Fade, S.A.; Swift, J.A. Qualitative research in nutrition and dietetics: Data analysis issues. J. Hum. Nutr. Diet. 2011, 24, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Green, J.; Thorogood, N. Qualitative Methods for Health Research, 4th ed.; SAGE: Los Angeles, CA, USA, 2018. [Google Scholar]
- Posit Team RStudio: Integrated Development Environment for R. Posit Software, PBC, Boston, MA, USA. 2023. Available online: http://www.posit.co/ (accessed on 1 May 2022).
- Linacre, J.M. Winsteps® Rasch Measurement Computer Program (Version 5.4.0). Portland, Oregon. 2023. Available online: https://winsteps.com (accessed on 1 December 2022).
- Ho, P. A new approach to measuring Overall Liking with the Many-Facet Rasch model. Food Qual. Prefer. 2019, 74, 100–111. [Google Scholar] [CrossRef]
- Resnicow, K.; Baranowski, T.; Ahluwalia, J.S.; Braithwaite, R.L. Cultural sensitivity in public health: Defined and demystified. Ethn. Dis. 1999, 9, 10–21. [Google Scholar]
- Wadi, N.M.; Asantewa-Ampaduh, S.; Rivas, C.; Goff, L.M. Culturally tailored lifestyle interventions for the prevention and management of type 2 diabetes in adults of Black African ancestry: A systematic review of tailoring methods and their effectiveness. Public Health Nutr. 2022, 25, 422–436. [Google Scholar] [CrossRef] [PubMed]
- Goff, L.M.; Rivas, C.; Moore, A.; Beckley-Hoelscher, N.; Reid, F.; Harding, S. Healthy Eating and Active Lifestyles for Diabetes (HEAL-D), a culturally tailored self-management education and support program for type 2 diabetes in black-British adults: A randomized controlled feasibility trial. BMJ Open Diabetes Res. Care 2021, 9, e002438. [Google Scholar] [CrossRef] [PubMed]
- Attridge, M.; Creamer, J.; Ramsden, M.; Cannings-John, R.; Hawthorne, K. Culturally appropriate health education for people in ethnic minority groups with type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2014, 4, CD006424. [Google Scholar] [CrossRef]
- Appleton, K.M.; Krumplevska, K.; Smith, E.; Rooney, C.; McKinley, M.C.; Woodside, J.V. Low fruit and vegetable consumption is associated with low knowledge of the details of the 5-a-day fruit and vegetable message in the UK: Findings from two cross-sectional questionnaire studies. J. Hum. Nutr. Diet. 2018, 31, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.G.; Donnelly, J.K.; Jones, S.; Cade, J.E. Effect of Educational Interventions on Understanding and Use of Nutrition Labels: A Systematic Review. Nutrients 2018, 10, 1432. [Google Scholar] [CrossRef]
- Whybrow, S.; Macdiarmid, J.I.; Craig, L.C.; Clark, H.; McNeill, G. Using food intake records to estimate compliance with the Eatwell Plate dietary guidelines. J. Hum. Nutr. Diet. 2016, 29, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Leslie, W.S.; Comrie, F.; Lean, M.E.; Hankey, C.R. Designing the eatwell week: The application of eatwell plate advice to weekly food intake. Public Health Nutr. 2013, 16, 795–802. [Google Scholar] [CrossRef] [PubMed]
- Hollis, J.L.; Whybrow, S.; Craig, L.C.A.; Clark, H.; Garden, L.; McNeill, G. Estimating plate-based model food proportions in adults living in Scotland using short dietary assessment questionnaires. Nutr. Diet. 2019, 76, 521–531. [Google Scholar] [CrossRef]
- BBC Food. Where Are You on the UK Healthy Eating Scale? Available online: https://www.bbc.co.uk/food/articles/uk_healthy_eating_scale (accessed on 1 July 2023).
- Goff, L.M.; Moore, A.; Harding, S. Providing culturally sensitive diabetes self-management education and support for black African and Caribbean communities: A qualitative exploration of the challenges experienced by healthcare practitioners in inner London. BMJ Open Diabetes Res. Care 2020, 8, e001818. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Siad, F.M.; Manalili, K.; Lorenzetti, D.L.; Barbosa, T.; Lantion, V.; Lu, M.; Quan, H.; Santana, M.J. How to measure cultural competence when evaluating patient-centred care: A scoping review. BMJ Open 2018, 17, e021525. [Google Scholar] [CrossRef]
- Wrieden, W.L.; Anderson, A.S.; Longbottom, P.J.; Valentine, K.; Stead, M.; Caraher, M.; Lang, T.; Gray, B.; Dowler, E. The impact of a community-based food skills intervention on cooking confidence, food preparation methods and dietary choices—An exploratory trial. Public Health Nutr. 2007, 10, 203–211. [Google Scholar] [CrossRef]
- Talumaa, B.; Brown, A.; Batterham, R.L.; Kalea, A.Z. Effective strategies in ending weight stigma in healthcare. Obes. Rev. 2022, 23, e13494. [Google Scholar] [CrossRef]




| Characteristic | Participants Who Consented and Completed Pre-Intervention Questionnaires n = 28 (%) | Participants Included in Analysis Who Completed All Three Questionnaires n = 22 (%) |
|---|---|---|
| Gender | ||
| Female | 23 (82%) | 17 (73%) |
| Male | 4 (14%) | 4 (18%) |
| Other | 1 (4%) | 1 (4%) |
| Age (years) | ||
| 18–55 | 9 (32%) | 5 (23%) |
| 55–65 | 10 (36%) | 9 (41%) |
| >65 | 9 (32%) | 8 (36%) |
| Ethnicity 1 | ||
| African Caribbean ethnicities | 14 (50%) | 10 (45%) |
| Other, including White British | 14 (50%) | 12 (55%) |
| Education 2 | ||
| Higher Education | 10 (36%) | 9 (41%) |
| Secondary | 9 (32%) | 6 (27%) |
| None | 9 (32%) | 7 (32%) |
| Body weight 3 | ||
| Happy with it | 4 (14%) | 3 (14%) |
| Lose weight | 18 (65%) | 15 (68%) |
| Gain weight | 4 (14%) | 3 (14%) |
| Prefer not to say | 2 (7%) | 1 (4%) |
| Following any dietary advice, 4 | ||
| Yes | 5 (18%) | 3 (14%) |
| No | 23 (82%) | 19 (86%) |
| Weekly food spend | ||
| £10–20 | 3 (11%) | 3 (14%) |
| £20–40 | 9 (32%) | 8 (36%) |
| £40–60 | 3 (11%) | 0 |
| £60–80 | 4 (14%) | 4 (18%) |
| £80–100 | 5 (18%) | 5 (23%) |
| £100 and above | 0 | 0 |
| Prefer not to say | 4 (14%) | 2 (9%) |
| Measure | Questionnaire Item | Pre- | Post- | Follow-up | p $ |
|---|---|---|---|---|---|
| Median (P25, P75) 3 | Median (P25, P75) | Median (P25, P75) | |||
| Recipe-related skills 1 | Being able to cook from raw/simple ingredients | 5 (4, 5) | 5(4, 5) | 5(4, 5) | 0.862 |
| Following a simple recipe | 5 (4, 5) | 5(4, 5) | 5(4, 5) | 0.983 | |
| Planning meals before shopping | 4 (3, 5) | 4 (4, 5) | 4 (4, 5) | 0.762 | |
| Shopping for food on a budget | 4 (4, 5) | 4 (4, 5) | 5(4, 5) | 0.384 | |
| Perceived importance of 2 | Healthy and nutritious recipe | 4 (3, 5) | 4 (3.25, 5) | 4 (2.35, 5) | 0.456 |
| Recipe to suit myself and whom I cook for | 4 (3, 5) | 4 (4, 5) | 4 (4, 5) | 0.875 | |
| Recipes to suit particular dietary requirements | 3 (3, 4) | 4 (3, 5) | 4 (3.25, 5) | 0.108 | |
| Recipe that incorporates traditional AC foods | 3 (2, 4) | 4 (2.25, 5) | 4 (3, 4) | 0.301 | |
| A recipe recommended to me | 3 (2, 4) | 3 (3, 4) | 3 (3, 4) | 0.035 | |
| Confidence using the AC recipes 3 | In day-to-day cooking | NT | 4 (3, 5) | 4 (3,4. 75) | NT |
| Healthier ingredients | NT | 4 (3, 5) | 4 (3, 5) | NT | |
| Within personal budgets | NT | 4 (2.25, 5) | 4 (3, 5) | NT | |
| % Aware | % Aware | % Aware | |||
| Awareness of | Healthy eating (EWG) incorporating AC foods | 8 (36%) | 14 (63%) | 18 (81%) | 0.0017 |
| Healthier recipes featuring AC traditional foods | 8 (36%) | 14 (63%) | 17 (77%) | 0.006 | |
| Daily allowance of salt, sugars, and fruit and veg | 5 (23%) | 14 (63%) | 18 (81%) | 0.0003 | |
| % correct | % correct | ||||
| Knowledge Quiz | Recommended portions of fruit and vegetables | 20 (95%) | 20 (95%) | NT | 0.625 |
| Daily allowance—salt | 7 (33%) | 5 (24%) | NT | 0.237 | |
| Daily allowance—sugar | 3 (14%) | 5 (24%) | NT | 0.578 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moore, S.G.; Kundra, A.; Ho, P.; Bissell, E.; Apekey, T. Feasibility of a Community Healthy Eating and Cooking Intervention Featuring Traditional African Caribbean Foods from Participant and Staff Perspectives. Nutrients 2023, 15, 3758. https://doi.org/10.3390/nu15173758
Moore SG, Kundra A, Ho P, Bissell E, Apekey T. Feasibility of a Community Healthy Eating and Cooking Intervention Featuring Traditional African Caribbean Foods from Participant and Staff Perspectives. Nutrients. 2023; 15(17):3758. https://doi.org/10.3390/nu15173758
Chicago/Turabian StyleMoore, Sally G., Aashna Kundra, Peter Ho, Esther Bissell, and Tanefa Apekey. 2023. "Feasibility of a Community Healthy Eating and Cooking Intervention Featuring Traditional African Caribbean Foods from Participant and Staff Perspectives" Nutrients 15, no. 17: 3758. https://doi.org/10.3390/nu15173758
APA StyleMoore, S. G., Kundra, A., Ho, P., Bissell, E., & Apekey, T. (2023). Feasibility of a Community Healthy Eating and Cooking Intervention Featuring Traditional African Caribbean Foods from Participant and Staff Perspectives. Nutrients, 15(17), 3758. https://doi.org/10.3390/nu15173758






