Abstract
Childhood obesity and overweight rates are increasing in an exponential way. This type of diet-related health problem has consequences, not only at present but also for children’s future lives. For these reasons, it is very important to find a solution, which could be nutrition intervention programs. The main objective of this article is to investigate the effectiveness of nutrition intervention programs in children aged 3–12 around the world. We used SCOPUS, Web of Science, and PubMed databases to carry out this systematic review and we followed the PRISMA statement. Two authors conducted literature searches independently, finding a total of 138 articles. Finally, after a thorough screening, a total of 19 articles were selected for detailed analysis. The results show that, in general, nutrition intervention programs are effective in improving knowledge and behaviors about healthy habits, and, consequently, that the body mass index value is reduced. However, it is true that we found differences between the incomes of families and geographical areas. In conclusion, we encourage school centers to consider including these types of programs in their educational program and bring awareness of the importance of families too.
1. Introduction
One of the main educational objectives is to promote people healthy lifestyle habits among young related to the Mediterranean diet and the regular practice of physical activity. However, diet-related health problems have a high incidence in children and adults [1,2]. Diet is an important risk factor that can be modified, having a significant impact on people’s health [3]. In fact, eating behavior (such as food choices, and eating events and habits) establishes the health status of people [4]. The most common of these problems are overweight and obesity, which have increased in children in the last few years. This has occurred not only in the richest countries but also in poorer countries [5,6], and the incidence continues to grow. Since 1975, universal obesity has almost tripled [1]. In 2020, 340 million children aged 5–19 and 38.9 million children aged under 5 were obese or overweight [1].
An imbalance between energy intake and expenditure causes overweight and obesity. Energy expenditure cannot be exceeded by energy intake. In consequence, diet quality is essential to maintaining body mass index (BMI) [7].
Nevertheless, there are other diet-related health problems, such as stunting or wasting. A child is stunted when they are too short for their age; a child is wasted when they are too thin for their height (underweight). Even though the prevalence of stunting in children aged under 5 has decreased from 33.1% in 2000 to 22% in 2020, 149.2 million children suffered it in 2020 and 45.4 million suffered from wasting [8].
1.1. Influence of the Socialization
The responsibility for these data is with the eating habits, including food and physical activity [9]. However, they are influenced by the food industry, which advertises unhealthy food and beverage [10] through the media. The nutritional transition process, which is determined by social changes like industrialization, has changed. Years ago, diets were based on fruit, vegetables, legumes, and grains; nowadays, ultra-processed foods are eaten by everyone.
At the present, the food preferences of children are changing, influenced by the exponential development of information and communication technologies (ICT). Advertisements in any media (TV, social media, mobile phones…) and food delivery online platforms promote junk food that contains high salt, sugar, and fat contents [11]. In fact, the most consumed beverages and foods by children have high sugar content. The problem is that diet-related health problems are associated with excessive sugar, salt, and fat consumption [12]. In addition, children spend their time using electronic devices instead of doing physical activities [13]. These data ratify that level of physical activity practice is below the World Health Organization’s (WHO) recommendation [14]. Thus, it is evident that ICT does not help to maintain a healthy diet.
Nevertheless, there are other influences such as friends, teachers, and parents’ attitudes toward food [15]. Independently of the setting, it is very important for children to have good health habits to promote good health habits in adulthood [16].
1.2. Consequences of Diet-Related Health Problems
Eating healthy foods and practicing physical activity reduce the risk of diet-related health problems [17]. Additionally, they could decrease anxiety and depression, and improve academic performance, socialization, or self-esteem [18,19]. The benefits of good nutrition are numerous, but the disadvantages of eating an unhealthy diet are also important to know. Obesity during childhood has consequences, both immediately and in the long-term. It can provoke hypertension, diabetes, and cardiovascular diseases later in life [20], and contributes to later adulthood obesity too [21].
Annually, 17.9 million people die because of cardiovascular diseases [22] which could be provoked by poor diet, over-nutrition, high blood sugar and lipids, low physical activity, or smoking, among other activities [23]. A reduction of these risk factors in daily life could avoid premature deaths [24].
These are the main problems that society faces, and that is why a feasible solution is necessary. Health intervention programs at schools could be a good answer. Childhood is the best period to teach good nutrition because of rapid mental and physical growth.
1.3. Healthy Nutrition Intervention Programs at Schools
Since youngsters spend most of their time at school and their behaviors are influenced by the school environments, educational centers are the best setting in which to carry out this type of intervention [25,26].
School food programs should contribute to child health and well-being [27] and to the promotion of healthy eating patterns [28]. They empower students with the knowledge and attitudes necessary to maintain healthy nutrition in their lives [29]. Although it is true that some countries do not include nutrition in their curriculum (such as Indonesia), these programs could take place in every single school.
These programs should be carried out as early as possible because adult eating habits are developed from an early age [30,31]. The World Health Organization has affirmed that they are efficient in changing eating habits [32] in 1997, but we want to verify if they continue to be effective.
1.4. Objetive
In spite of the educational programs related to balanced nutrition, it is important to analyze the impact it is having on young people between the ages of 3 and 12. During this period, habits take place that will have a significant impact on adolescence. Therefore, the main objective of this systematic review is to investigate the effectiveness of nutrition intervention programs in children aged 3–12 years worldwide.
2. Materials and Methods
The statement of the Preferred Reporting Items for Systematic Review and Meta-Analyses 2020 (PRISMA statement) [33] was considered in the process of searching and writing this article.
2.1. Literature Search
After the agreement about the string search, two authors started the literature search independently. The databases SCOPUS, Web of Science, and PubMed were screened from September to December 2022 to compile the most complete list of studies possible. We looked for relevant articles about nutrition education programs in pre-primary and primary schools published from January 2013 to now. We use two clear and careful descriptors strings, one for each educational stage:
- (“PRE” AND “POST” OR “intervention program”) AND (“dietary behaviour” OR “healthy food” OR “healthy eating” OR “healthy diet” OR “healthy nutrition” OR “healthy habits”) AND (“children” “education” OR “early childhood education” OR “childhood education” OR “childhood school” OR “pre-primary education” OR “infant education” OR “infant school” OR “kindergarten education” OR “nursery education” OR “preschool education” OR “early education”);
- (“PRE” AND “POST”) AND (“dietary behavior” OR “healthy food” OR “healthy eating” OR “healthy diet” OR “healthy nutrition” OR “healthy habits”) AND (“primary school” OR “elementary school” OR “primary education” OR “elementary education” OR “primary students” OR “elementary students”).
In the primary string search, we found 2 articles about pre-primary education.
2.2. Inclusion and Exclusion Criteria
The main criteria for this review were nutrition intervention programs in pre-primary and primary schools over the world. During the selection process the following criteria has been considered:
- Articles from scientific journals were accepted, whereas other types of studies such as gray literature were refused;
- Participants sample had to be made up of preschool of school children, and studies with post-primary, teachers or families as samples were refused;
- Experimental or quasi-experimental articles were accepted, while articles without an intervention program, a pre- and post-intervention, or experimental group were refused;
- Nutrition intervention programs in pre-primary or primary schools were included, whereas we refused articles whose variables were different from eating diet, for instance, physical activity, food wasted, smart devices, hand washing, academic achievement, or teachers’ attitudes, among others;
- Articles with open access and the Spanish or English language were included. We refused articles to which we did not have full access or which were written in other languages.
2.3. Article Selection and Data Extraction
Firstly, we found 17 articles for pre-primary education and 121 for primary education. Removing articles published before 2013, studies repeated in two or more databases, and gray literature, we screened 74 articles in total. Later, we applied the inclusion criteria mentioned before and 42 studies were selected for a full reading. Finally, 19 articles published in scientific journals were included in our systematic review. This process is summarized in Figure 1.
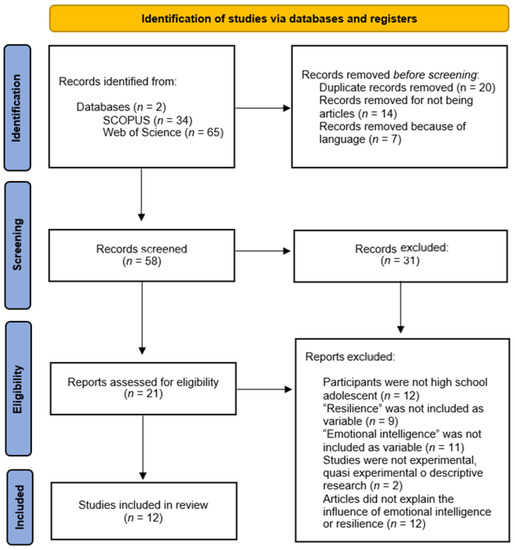
Figure 1.
Flow diagram of the articles during the selection process.
The same two authors extracted the following data from the 19 articles selected: authors’ names, year of publication, instruments used, variables measured, sample, country, and main findings. Then, a third author validated the information.
2.4. Study Quality Assessment
The literature search and article selection were carried out by two authors independently. Some disagreements were found, but they were solved by the consensus of the two authors. We divided the number of agreements by the total number of agreements plus disagreements, then we multiplied the answer by 100 to obtain the inter-rater reliability percent, which resulted in 95%.
3. Results
3.1. Study Characteristics
From the 19 articles that were selected for our systematic review, some data were extracted to know the characteristics of the studies (Table 1). In this sense, we can say that there is a great variety across geographic location. A total of 5 articles were from the United States [34,35,36,37,38], 2 from Malaysia [39,40], 2 from China [41,42], while the rest of countries did not appear in more than one study. The most studied continents were North America and Asia, with 6 out of 19 each continent, closely followed by Europe (5 articles). Most of the American articles selected were developed in the United States (5 out of 6).

Table 1.
Characteristics of the studies selected.
The age range was from 4 to 14 years old. However, most of the studies had a population aged from 6 to 12 years old, as they focused on primary education. Focusing on this stage, children aged 9 years old were the most represented group of the studies analyzed (in 73.68% of the articles). Regarding the instrument, children’s and parents’ questionnaires and surveys were the most used instruments [34,36,37,38,39,40,42,43,44,45,46,47,48,49,50].
3.2. Outcomes
The effectiveness of a nutrition program depends on its aims, activities, methods, and program content, among other factors [53]. That is why we found a great variety of intervention programs. According to the articles selected, we can group nutritional programs into three categories: (1) education component programs (e.g., classroom-based learning, educational modules, and supportive educational materials), (2) practical component programs (e.g., the availability of fruit and vegetable, participation in nutritional campaigns and games), and (3) educational and practical component programs (e.g., theoretical lessons through video lessons or video laboratories, implementation of contents through meaningful activities such as gamified challenges or cooking workshops). This review included 19 intervention studies that reported a significant increase in children’s consumption of a healthy diet, mainly consisting of fruit and vegetables. Overall, 6 studies of these articles included only educational components [35,36,40,41,47,51], 6 studies used practical approaches [37,38,42,44,48,50], and 7 included both approaches [34,39,43,45,46,49,52]. The intervention programs and their duration can be seen in Table 2.

Table 2.
Characteristics of the intervention programs.
3.2.1. Nutritional Knowledge
In Table 3, we observe that nutrition intervention programs increase children’s nutritional knowledge [40,49], especially about the appropriate daily frequency of fruit and vegetable consumption [46], and the sugar content of certain foods [35]. In addition, this knowledge about healthy habits increases, especially among children living in low-income neighborhoods [47]. On the contrary, Sharma et al. found that the EG decreased their nutrition and physical activity knowledge [37]. Finally, these school nutrition practices increase students’ knowledge of active lifestyles and healthy diets [50]. This knowledge increases due to the theoretical lessons and practical activities on the subject of nutrition that take place in class [40,42].

Table 3.
Results about nutritional knowledge.
3.2.2. Body Weight and Body Mass Index (BMI)
In Table 4, we find that children’s participation in nutrition intervention programs causes significant changes in anthropometric variables such as weight, in some cases, over time [40]. The prevalence of normal weight increased, while the prevalence of overweight, obesity, or thinness decreased after the implementation of these programs [40,50].

Table 4.
Results related to body weight and BMI.
In addition, overweight children who participated in these programs reduced their BMI score [39,46]. Additionally, children who were in schools that followed a free fruit and vegetable policy had a better BMI [44]. On the other hand, boys of parents with no higher education had an elevated BMI and a higher chance of being overweight or obese, while girls of parents with no higher education had a lower BMI and a lower chance of being overweight or obese [44]. In turn, Nickel et al. affirmed that boys that lived in rural areas experienced a greater reduction in waist circumference (WC) [47].
Finally, these programs make children do physical activity more frequently, so they can prevent and/or treat overweight and obesity in this population [37,39,46]. However, Sharma et al. did not find significant effects of a video game-based nutritional program on physical activity [37].
3.2.3. Eating Behaviors
In Table 5, we observe that the nutritional quotient (NQ) score increased significantly after participating in these nutrition intervention programs, in relation to diet quality, dietary attitudes, and healthy eating behaviors [42,42,51]. Moreover, we find behavioral improvement with respect to the daily frequency of fruit and vegetable consumption [45,46,51] in both children [38] and parents [34], moderation in the intake of hypercaloric foods [51], changes in the regularity of meals away from home [51] and the frequency of eating five meals per day [39], and adherence to the Mediterranean diet [43]. Verdonschot et al. disagreed, and they did not find significant differences in fruit and vegetable consumption between EG and CG [49].

Table 5.
Results related to eating behaviors.
On the other hand, participation in these programs increased self-confidence in cooking, enjoyment of food and cooking, frequency of cooking at home, availability of fruits and vegetables at home, use of nutrition labels when shopping, and knowledge of bedtime routines [34,35]. Moreover, food waste [45], total fat intake [34], and the percentage of daily calories from morning and afternoon snacks [52], such as cookies, cakes, chocolates [37,48], and sugary drinks [34], were reduced.
Finally, both children living in urban areas and those living in higher-income neighborhoods improved dietary intake self-efficacy [38,47], which may improve children’s cognitive performance [39]. However, Siew et al. and Lin et al. did not find significant changes in children’s nutritional attitudes [40,50].
4. Discussion
This systematic review has given an analysis of the effects of nutrition education programs on children’s nutrition knowledge and eating behaviors. Through this research, we found several types of programs about nutrition at schools which the latter used to obtain different dietary outcomes. Regarding the literature, nutrition education programs increase knowledge and food attitudes [54], practical activities during the programs encourage an increase in physical activities [55] or healthy eating behaviors. However, the most effective programs are those that join both education and practice [56]. These findings are in line with most of the articles selected [34,35,38,39,43,44,45,46,47,48,49]. However, we also found some educational programs which improved the practice scores [40] or eating behaviors [41,51] and practical programs that fostered knowledge [37,42,50].
It is very important that FV policies are promoted in educational environments. In fact, exposure to FV has been shown to contribute to effective nutrition education programs [57]. We found that children which were exposed to FV provision [44,49] or FV education [38,45,49] improved their BMI, FV intake, nutrition knowledge, and behaviors. Previous studies of free fruit and vegetables (FFV) showed a reduction in BMI mean score, a reduction in school-level obesity [58], and an increase in FV intake [59,60,61]. The interventions selected are heterogeneous among the results of prior meta-analyses and systematic reviews [62,63]; however, all of them have adequate alignment among intervention, objectives, and findings, which is an important aspect to be effective [57].
In this sense, the combination of FV provision and education [49] seems to be more effective in eating habits, indeed earlier studies affirmed that education improves nutrition knowledge [64,65]. On their part, Franceschi et al. used an app to prevent overweight and obesity, resulting in an increase in nutritional knowledge [46]. The use of technology for these intervention programs showed that they are beneficial in short-term weight loss [66,67]. However, other non-technological programs also had good results. We found that children’s knowledge improved and consequently they reduced food waste [45]. The knowledge improvement could be seen in nutrition [35,37,40,42,46,49,50], bedtime routine knowledge [35], physical activity knowledge [37], and healthy living in general [47,50]. This is consistent with previous research which focused on the knowledge about healthy eating habits [68,69]. Nutrition knowledge is very important in all stages of our lives because it fosters the awareness of eating and, therefore, inspires people to practice healthy eating [70,71].
Regarding eating behaviors and physical activity, we find some articles that reported changes in behavior [34,37,38,39,41,42,43,45,46,47,48,51], as Weber et al. [72] affirmed in Germany. Regular meal intake, especially at breakfast time, is associated with better overall food consumption [73,74], and it is essential to improving eating behavior [75,76] and physical activity [77]. This regular meal intake was significantly greater in EG [51], so we can affirm that intervention programs help to improve food intake. In this sense, the results of Teo et al. show that, after an intervention program, the frequency of healthy breakfasts, lunches, and dinners increases, improving physical activity frequency and decreasing BMI scores [39]. Moreover, the consumption of cookies, cakes, and chocolates decreased significantly [48]. In general, unhealthy snacks were less consumed after nutrition intervention programs [34,37,48,51] as was confirmed previously [78].
It was believed that nutritional knowledge fosters healthy behaviors [79]. However, in Siew et al. [40] and Lin et al. [50], we do not find significant differences in attitudes while knowledge improves [40]. On the contrary, we found significant behavior, attitudes, and knowledge changes in other articles [42,51].
Nevertheless, depending on the socio-economic groups and geographical regions there are differences in eating behaviors and, consequently in obesity rates [80]. Our results are in line with that statement. Indeed, Nickel et al. affirmed that children in low-income neighborhoods only showed improved nutrition knowledge, while children in higher-income neighborhoods improved their consumption [47]; Øvrebø et al. found differences between parents’ education, resulting in different BMI [44]; and Qian et al. confirmed differences between provinces, whereby there was a better improvement in eating behaviors in higher-income families [41].
All the variables mentioned influence the body mass index (BMI), which allows us to know if a person is underweight or overweight. Through the articles selected, we find changes in BMI depending on different programs [36,40,44,46,51]. Consistent with the other two intervention programs, the BMI is lower in EG than in CG after a nutrition intervention [81,82]. In a literature search, we found contrary opinions about this topic, with some articles emphasizing the effectiveness of these types of programs [83,84] while others affirmed that these interventions were not effective [85,86]. In this sense, our results show that in two intervention programs, there were no significant differences [36,40] while three of them had significant changes and differences. This is corroborated by a previous study, which showed that a 5-2-1-0 intervention program [87] decreases the BMI percentile. A higher BMI is associated with obesity and overweight, and this is the main reason to consider implementing nutrition intervention programs at schools [88].
In short, nutrition intervention programs at schools have a strong impact on children’s eating. The main objective of this study was to check the effectiveness of these programs in impacting children’s nutrition knowledge and behaviors. As we verified, they improve students’ knowledge about healthy diets and foster healthy attitudes and behaviors in their lives. School environments and families are essential in promoting healthy habits and modifying dietary behaviors [89,90]. However, it is more important to include fun and interactive activity-based nutrition sessions [91] because attitude, which is influenced by motivation [92], mediated eating behaviors [93].
5. Conclusions
Despite the results achieved in our systematic review, the impact is rather limited. In this sense, we included articles from all continents except Antarctica, but they are not representative of global nutrition education programs because there is only one article from Oceania and one from Africa. On the contrary, we found a wide variety of articles from countries in Europe and Asia, but not in America.
This is due to the limitations of year of publication and type of publication that reduce the number of possible studies, but the aim was to make the selected articles as relevant and current as possible. In fact, this was the usual reason for eliminating articles not published in peer-reviewed journals and articles published before 2013. On the other hand, we followed the PRISMA methodology, which is a great method in social science research because of its transparency and openness to suggestions and comments.
This systematic review could have important educational implications. In this sense, the promotion of healthy lifestyle habits related to healthy and balanced eating is an educational objective. Therefore, future work could analyze the influence of different types of methodologies that help to reinforce behaviors related to the consumption of healthy food.
Author Contributions
J.M.A.-P. and R.T. conceived the idea; F.L.T. and N.N. wrote the introduction; R.C.-S. and M.A.-P. did the literature search, R.C.-S. and F.L.T. revised the search and wrote the methodology; M.A.-P. and R.C.-S. outlined the results, M.A.-P. and N.N. wrote de results; R.T. and M.A-.P. wrote the discussion; R.C.-S. and R.T. revised the article and approved the article. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We would like to extend our gratitude to the Ministry of University because of the University Teacher Training Program (FPU2021/00004).
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 25 November 2022).
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Willett, W.C. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Australian Dietary Guidelines: Eat for Health; National Health and Medical Research Council: Canberra, Australia, 2013; pp. 1–226.
- LaCaille, L. Eating Behavior. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 641–642. [Google Scholar]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Family Med. Prim. Care 2015, 4, 187–192. [Google Scholar] [PubMed]
- Jaacks, L.M.; Kavle, J.; Perry, A.; Nyaku, A. Programming maternal and child overweight and obesity in the context of undernutrition: Current evidence and key considerations for low- and middle-income countries. Public Health Nutr. 2017, 20, 1286–1296. [Google Scholar] [CrossRef] [PubMed]
- Romieu, I.; Dossus, L.; Barquera, S.; Blottière, H.M.; Franks, P.W.; Gunter, M.; Hwala, N.; Hursting, S.D.; Leitzmann, M.; Margetts, B.; et al. Energy balance and obesity: What are the main drivers? Cancer Causes Control 2017, 28, 247–258. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Levels and Trends in child Malnutrition: UNICEF/WHO/The World Bank Group Joint Child Malnutrition Estimates: Key Findings of the 2021 Edition. Available online: https://www.who.int/publications/i/item/9789240025257 (accessed on 25 November 2022).
- Guevara, R.M.; Urchaga, J.D.; Cabaco, A.S.; Moral-García, J.E. The quality of breakfast and healthy diet in school-aged adolescents and their association with bmi, weight loss diets and the practice of physical activity. Nutrients 2020, 12, 2294. [Google Scholar] [CrossRef]
- Popkin, B.M. Nutrition transition and the global diabetes epidemic. Curr. Diab. Rep. 2015, 15, 64–78. [Google Scholar] [CrossRef]
- Indrayana, S.; Palupi, N.S. Strategi implementasi pencantuman informasi kandungan gula, garam, dan lemak untuk pencegahan risiko penyakit Tidak Menular. Mutu Pangan 2014, 1, 156–164. [Google Scholar]
- Pervin, R.; Hossain, M.A.; Debnath, D.; Nath, B.D. Epidemiological perspectives of dietary sugars, salts and fats. Diet Sugar Salt Fat. Hum. Health 2020, 3, 3–23. [Google Scholar]
- Bentley, G.F.; Turner, K.M.; Jago, R. Mothers’ views of their preschool child’s screen-viewing behaviour: A qualitative study. BMC Public Health 2016, 16, 718. [Google Scholar] [CrossRef]
- Gomes, T.N.; Katzmarzyk, P.T.; Hedeker, D.; Fogelholm, M.; Standage, M.; Onywera, V.; Lambert, E.; Tremblay, M.S.; Chaput, J.-P.; Tudor-Locke, C.; et al. Correlates of compliance with recommended levels of physical activity in children. Sci. Rep. 2017, 7, 16507. [Google Scholar] [CrossRef]
- Kilanowski, J.F. Influences on healthy-eating decision making in latino adolescent children of migrant and seasonal agricultural workers. J. Pediatr. Health Care 2016, 30, 224–230. [Google Scholar] [CrossRef]
- Baker, S.; Morawska, A.; Mitchell, A. Promoting children’s healthy habits through self-regulation via parenting. Clin. Child Fam. Psychol. Rev. 2019, 22, 52–62. [Google Scholar] [CrossRef]
- Saraiva, J.F.K.; Slonczewski, T.; Clisnei, I.M.M. Estratégias interdisciplinares na abordagem do risco cardiovascular para combate à obesidade infantil. Rev. Soc. Bras. Clin. Med. 2017, 15, 214–220. [Google Scholar]
- Muftuoglu, S.; Bayram, S. Determination of the relationship between nutrition habits, social physique anxiety, and physical activity levels of adolescent students. World Nutr. 2020, 11, 62–74. [Google Scholar] [CrossRef]
- López, L.M.J. Condición física y rendimiento académico. J. Sport Health Res. 2018, 10, 349–360. [Google Scholar]
- UNICEF Indonesia. Indonesia: Obesity Rates among Adults Double over Past Two Decades. Indonesia: UNICEF Indonesia-Press Release. Available online: https://www.unicef.org/indonesia/press-releases/indonesia-obesity-rates-among-adults-double-over-past-two-decades (accessed on 26 November 2022).
- World Health Organization WHO. Report of the Comission on Ending Childhood Obesity. Available online: https://www.who.int/publications/i/item/9789241510066 (accessed on 26 November 2022).
- World Health Organization. Cardiovascular Diseases. Available online: https://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1 (accessed on 26 November 2022).
- American Heart Association. Coronary Heart Disease. Available online: https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/coronary-artery-disease (accessed on 26 November 2022).
- de Ferranti, S.D.; Steinberger, J.; Ameduri, R.; Baker, A.; Gooding, H.; Kelly, A.S.; Mietus-Snyder, M.; Mitsnefes, M.M.; Peterson, A.L.; St-Pierre, J.; et al. Cardiovascular risk reduction in high-risk pediatric patients: A scientific statement from the American Heart Association. Circulation 2019, 139, e603–e634. [Google Scholar] [CrossRef]
- Delgado-Noguera, M.; Tort, S.; Martinez-Zapata, M.J.; Bonfill, X. Primary school interventions to promote fruit and vegetable consumption: A systematic review and meta-analysis. Prev. Med. 2011, 53, 3–9. [Google Scholar] [CrossRef]
- Nathan, N.; Wolfenden, L.; Butler, M.; Bell, A.C.; Wyse, R.; Campbell, E.; Milat, A.J.; Wiggers, J. Vegetable and fruit breaks in Australian primary schools: Prevalence, attitudes, barriers and implementation strategies. Health Educ. Res. 2011, 26, 722–731. [Google Scholar] [CrossRef]
- Oostindjer, M.; Aschemann-Witzel, J.; Wang, Q.; Skuland, S.E.; Egelandsdal, B.; Amdam, G.V.; Schjøll, A.; Pachucki, M.C.; Rozin, P.; Stein, J.; et al. Are school meals a viable and sustainable tool to improve the healthiness and sustainability of children´s diet and food consumption? A cross-national comparative perspective. Crit. Rev. Food Sci. Nutr. 2017, 57, 3942–3958. [Google Scholar] [CrossRef]
- Ismail, M.R.; Seabrook, J.A.; Gilliland, J.A. Outcome evaluation of fruits and vegetables distribution interventions in schools: A systematic review and meta-analysis. Public Health Nutr. 2021, 19, 1–13. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Nutrition Education in US Schools. Available online: https://www.cdc.gov/healthyschools/nutrition/school_nutrition_education.htm (accessed on 28 November 2022).
- Craigie, A.M.; Lake, A.A.; Kelly, S.A.; Adamson, A.J.; Mathers, J.C. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas 2011, 70, 266–284. [Google Scholar] [CrossRef] [PubMed]
- Langford, R.; Bonell, C.; Jones, H.; Pouliou, T.; Murphy, S.; Waters, E.; Komro, K.; Gibbs, L.; Magnus, D.; Campbell, R. The World Health Organization’s Health Promoting Schools framework: A Cochrane systematic review and meta-analysis. BMC Public Health 2015, 15, 130. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Expert Committee on Comprehensive School Health Education and Promotion. In Promoting Health through Schools: Report of a WHO Expert Committee on Comprehensive School Health Education and Promotion; World Health Organization: Geneva, Switzerland, 1997; Available online: https://apps.who.int/iris/handle/10665/41987 (accessed on 15 December 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Marshall, A.N.; Markham, C.; Ranjit, N.; Bounds, G.; Chow, J.; Sharma, S.V. Long-term impact of a school-based nutrition intervention on home nutrition environment and family fruit and vegetable intake: A two year follow-up study. PRM 2020, 20, 101247. [Google Scholar] [CrossRef] [PubMed]
- Fisher, M.C.; Villegas, E.; Sutter, C.; Musaad, S.M.; Koester, B.; Fiese, B.H. Sprouts Growing Healthy Habits: Curriculum Development and Pilot Study. Front. Public Health 2019, 7, 65. [Google Scholar] [CrossRef]
- Lynch, B.A.; Gentile, N.; Maxson, J.; Quigg, S.; Swenson, L.; Kaufman, T. Elementary School-Based Obesity Intervention Using an Educational Curriculum. J. Prim. Care Community Health 2016, 7, 265–271. [Google Scholar] [CrossRef]
- Sharma, S.V.; Shegog, R.; Chow, J.; Finley, C.; Pomeroy, M.; Smith, C.; Hoelscher, D.M. Effects of the Quest to Lava Mountain Computer Game on Dietary and Physical Activity Behaviors of Elementary School Children: A Pilot Group-Randomized Controlled Trial. J. Acad. Nutr. Diet. 2015, 115, 1260–1271. [Google Scholar] [CrossRef]
- Song, H.-J.; Grutzmacher, S.; Munger, A.L. Project ReFresh: Testing the Efficacy of a School-Based Classroom and Cafeteria Intervention in Elementary School Children. J. School Health 2016, 86, 543–551. [Google Scholar] [CrossRef]
- Teo, C.H.; Chin, Y.S.; Lim, P.Y.; Masrom, S.A.H.; Shariff, Z.M. Impacts of a School-Based Intervention That Incorporates Nutrition Education and a Supportive Healthy School Canteen Environment among Primary School Children in Malaysia. Nutrients 2021, 13, 1712. [Google Scholar] [CrossRef]
- Siew, C.Y.; Siong, T.E.; Hashim, Z.; Raqi, R.A.; Karim, N.A. Effectiveness of a Nutrition Education Intervention for Primary School Children: The Healthy Kids Programme, Malaysia. Mal. J. Med. Health Sci. 2020, 16, 1–10. [Google Scholar]
- Qian, L.; Newman, I.M.; Yuen, L.W.; Du, W.; Shell, D. Effects of a comprehensive nutrition education programme to change grade 4 primary-school students’ eating behaviours in China. Public Health Nutr. 2019, 22, 903–911. [Google Scholar] [CrossRef]
- Zhou, J. Results form a Quasi-experimental Study of a Training Intervention for Healthy Eating Behaviors of Students. NeuroQuantology 2018, 16, 19–24. [Google Scholar] [CrossRef]
- García, E.; Fernández, G. Educational intervention through a gamification proposal to improve the adherence to the Mediterranean diet in Galician primary schools students. Reto 2022, 44, 128–135. [Google Scholar] [CrossRef]
- Øvrebø, B.; Stea, T.H.; Bergh, I.H.; Bere, E.; Surén, P.; Magnus, P.; Juliusson, P.B.; Wills, A.K. A nationwide school fruit and vegetable policy and childhood and adolescent overweight: A quasi-natural experimental study. PLoS Med. 2022, 19, e1003881. [Google Scholar] [CrossRef]
- Karpouzis, F.; Lindberg, R.; Walsh, A.; Shah, S.; Abbott, G.; Lai, J.; Berner, A.; Ball, K. Evaluating OzHarvest’s primary-school Food Education and Sustainability Training (FEAST) program in 10-12-year-old children in Australia: Protocol for a pragmatic cluster non-randomized controlled trial. BMC Public Health 2021, 21, 967. [Google Scholar] [CrossRef]
- Franceschi, R.; Fornari, E.; Ghezzi, M.; Buzzi, E.; Toschi, M.; Longhi, S.; Maimone, R.; Forti, S.; Carneri, S.; Pirous, F.M.; et al. Educational Intervention of Healthy Life Promotion for Children with a Migrant Background or at Socioeconomic Disadvantage in the Nort of Italy: Efficacy of Telematic Tools in Improving Nutritional and Physical Activity Knowledge. Nutrients 2021, 13, 3634. [Google Scholar] [CrossRef]
- Nickel, N.C.; Doupe, M.; Enns, J.E.; Brownell, M.; Sarkar, J.; Chateau, D.; Burland, E.; Chartier, M.; Katz, A.; Crockett, L.; et al. Differential effects of a school-based obesity prevention program: A cluster randomized trial. Matern. Child Nutr. 2021, 17, e13009. [Google Scholar] [CrossRef]
- Ben Cheikh, A.; Maatoug, J.; Ghammam, R.; Chouikha, F.; Mallat, A.; Ghannem, H. Effect of a school-based intervention in eating habits among school children: Quasi experimental study, Tunisia. Adoles. Med. Health 2020, 33, 157–164. [Google Scholar] [CrossRef]
- Verdonschot, A.; de Vet, E.; van Rossum, J.; Mesch, A.; Collins, C.E.; Bucher, T.; Haveman-Nies, A. Education or Provision? A Comparison of Two School-Based Fruit and Vegetable Nutrition Education Programs in the Netherlands. Nutrients 2020, 12, 3280. [Google Scholar] [CrossRef]
- Lin, Y.-C.; Chen, H.-J.; Wang, Y.; Min, J.; Wu, H.-C.; Carvajal, N.A.; Yang, H.-Y. NASA Mission X program for healthy eating and active living among Taiwanese elementary school students. J. Pediatr. Nurs. 2019, 49, E8–E14. [Google Scholar] [CrossRef]
- Kim, J.; Kim, G.; Park, J.; Wang, Y.; Lim, H. Effectiveness of Teacher-Led Nutritional Status in Preschool Children: Adoption of a NASA Mission X-Based Program. Nutrients 2019, 11, 1590. [Google Scholar] [CrossRef] [PubMed]
- Brown, E.C.; Buchan, D.S.; Drignei, D.; Wyatt, F.B.; Kilgore, L.; Cavana, J.; Baker, J.S. Primary School Children’s Health Behaviors, Attitudes, and Body Mass Index After a 10-Week Lifestyle Intervention with Follow-up. Front. Pediatr. 2018, 6, 178–181. [Google Scholar] [CrossRef] [PubMed]
- Dudley, D.A.; Cotton, W.G.; Peralta, L.R. Teaching approaches and strategies that promote healthy eating in primary school children: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Antwi, J. Nutrition education impact on nutrition knowledge, attitude and practice of schoolchildren: A pilot study in Ghana. Curr. Dev. Nutr. 2020, 4, 1287. [Google Scholar] [CrossRef]
- Morano, M.; Robazza, C.; Bortoli, L.; Rutigliano, I.; Ruiz, M.C.; Campanozzi, A. Physical activity and physical competence in overweight and obese children: An intervention study. Int. J. Environ. Res. Public Health 2020, 17, 6370. [Google Scholar] [CrossRef]
- Habib-Mourad, C.; Ghandour, L.A.; Maliha, C.; Dagher, M.; Kharroubi, S.; Hwalla, N. Impact of a three-year obesity prevention study on healthy behaviors and BMI among Lebanese schoolchildren: Findings from ajyal salima program. Nutrients 2020, 12, 2687. [Google Scholar] [CrossRef]
- Murimi, M.W.; Moyeda-Carabaza, A.F.; Nguyen, B.; Saha, S.; Amin, R.; Njike, V. Factors that contribute to effective nutrition education interventions in children: A systematic review. Nutr. Rev. 2018, 76, 553–580. [Google Scholar] [CrossRef]
- Qian, Y.; Nayga, R.M.; Thomsen, J.M.R.; Rouse, H.L. The effect of the Fresh Fruit and Vegetable Program on childhood obesity. Appl. Econ. Perspect. Policy 2016, 38, 260–275. [Google Scholar] [CrossRef]
- Fogarty, A.W.; Antoniak, M.; Venn, A.J.; Davies, L.; Goodwin, A.; Salfield, N.; Stocks, J.; Britton, J.; Lewis, S.A. Does participation in a population- based dietary intervention scheme have a lasting impact on fruit intake in young children? Int. J. Epidemiol. 2007, 36, 1080–1085. [Google Scholar] [CrossRef]
- Bere, E.; Hilsen, M.; Klepp, K.I. Effect of the nationwide free school fruit scheme in Norway. Br. J. Nutr. 2010, 104, 589–594. [Google Scholar] [CrossRef]
- Evans, C.E.; Christian, M.S.; Cleghorn, C.L.; Greenwood, D.C.; Cade, J.E. Systematic review and meta-analysis of school-based interventions to improve daily fruit and vegetable intake in children aged 5 to 12 y. Am. J. Clin. Nutr. 2012, 96, 889–901. [Google Scholar] [CrossRef]
- Arnotti, K.; Bamber, M. Fruit and vegetable consumption in overweight or obese individuals: A meta-analysis. West J. Nurs. Res. 2020, 42, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Guyenet, S.J. Impact of whole, fresh fruit consumption on energy intake and adiposity: A systematic review. Front. Nutr. 2019, 6, 66. [Google Scholar] [CrossRef]
- Fries, M.; van Dongen, E.; Haveman-Nies, A. Evaluatie van Smaaklessen: Heeft Smaaklessen Eect op Determinanten van Gezond en Bewust Eetgedrag? Leerstoelgroep Humane Voeding: Wageningen, The Netherlands, 2013. [Google Scholar]
- De Villiers, A.; Steyn, N.P.; Draper, C.E.; Hill, J.; Gwebushe, N.; Lambert, E.V.; Lombard, C. Primary school children’s nutrition knowledge, self-ecacy, and behavior, after a three-year healthy lifestyle intervention (HealthKick). Ethn. Dis. 2016, 26, 171. [Google Scholar] [CrossRef]
- Godino, J.G.; Merchant, G.; Norman, G.; Donohue, M.C.; Marshall, S.J.; Fowler, J.H.; Calfas, K.J.; Huang, J.; Rock, C.L.; Griswold, W.G.; et al. Using social and mobile tools for weight loss in overweight and obese young adults (Project SMART): A 2 year, parallel-group, randomised, controlled trial. Lancet Diabetes Endocrinol. 2016, 4, 747–755. [Google Scholar] [CrossRef]
- Raaijmakers, L.C.; Pouwels, S.; Berghuis, K.A.; Nienhuijs, S.W. Technology-based interventions in the treatment of overweight and obesity: A systematic review. Appetite 2015, 95, 138–151. [Google Scholar] [CrossRef]
- David, T.; Julien, A.; Laurie, I.; Nordine, L.; Sébastien, R.; Eric, D.; Martine, M.; Pascale, D. Are eating habits associated with physical fitness in primary school children? Eat. Behav. 2013, 14, 83–86. [Google Scholar] [CrossRef]
- Meyer, P.A.; Yoon, P.W.; Kaufmann, R.B. Introduction: CDC Health Disparities and Inequalities Report-United States. In CDC Health Disparities and Inequalities Report–US, 2013; Moolenaar, R.L., Ed.; MMWR: NJ, USA, 2013; Volume 62, pp. 3–5. [Google Scholar]
- Jones, M.; Pitt, H.; Oxford, L.; Bray, I.; Kimberlee, R.; Orme, J. Association between Food for Life, a whole setting healthy and sustainable food programme, and primary school children’s consumption of fruit and vegetables: A cross-sectional study in England. Int. J. Environ. Res. Public Health 2017, 14, 639. [Google Scholar] [CrossRef]
- Aarestrup, A.K.; Jørgensen, T.S.; Jørgensen, S.E.; Hoelscher, D. Implementation of strategies to increase adolescents’ access to fruit and vegetables at school: Process evaluation findings from the Boost study. BMC Public Health 2015, 15, 86. [Google Scholar] [CrossRef]
- Weber, K.S.; Eitner, J.; Dauben, L.; Spörkel, O.; Strassburger, K.; Sommer, J.; Kaiser, B.; Buyken, A.E.; Kronsbein, P.; Müssig, K. Positive Effects of Practical Nutrition Lessons in a Primary School Setting with a High Proportion of Migrant School Children. Exp. Clin. Endocrinol. Diabetes 2020, 128, 111–118. [Google Scholar] [CrossRef]
- Sharif Ishak, S.; Chin, Y.S.; Mohd Taib, M.N.; Chan, Y.M.; Shariff, Z.M. Effectiveness of a school-based intervention on knowledge, attitude and practice on healthy lifestyle and body composition in Malaysian adolescents. BMC Pediatr. 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Asakura, K.; Todoriki, H.; Sasaki, S. Relationship between nutrition knowledge and dietary intake among primary school children in Japan: Combined effect of children’s and their guardians’ knowledge. J. Epidemiol. 2017, 27, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Mistretta, A.; Turconi, G.; Cena, H.; Roggi, C.; Galvano, F. Nutrition knowledge and other determinants of food intake and lifestyle habits in children and young adolescents living in a rural area of Sicily, South Italy. Public Health Nutr. 2013, 16, 1827–1836. [Google Scholar] [CrossRef] [PubMed]
- Durlak, J.A.; Weissberg, R.P.; Dymnicki, A.B.; Taylor, R.D.; Schellinger, K.B. The impact of enhancing students’ social and emotional learning: A meta-analysis of school-based universal interventions. Child. Dev. 2011, 82, 405–432. [Google Scholar] [CrossRef] [PubMed]
- Reilly, K.L.; Nathan, N.; Wiggers, J.; Yoong, S.L.; Wolfenden, L. Scale up of a multi-strategic intervention to increase implementation of a school healthy canteen policy: Findings of an intervention trial. BMC Public Health 2018, 18, 860. [Google Scholar] [CrossRef]
- Øverby, N.C.; Klepp, K.-I.; Bere, E. Introduction of a school fruit program is associated with reduced frequency of consumption of unhealthy snacks. Am. J. Clin. Nutr. 2012, 96, 1100–1103. [Google Scholar] [CrossRef]
- Makeeva, A. What can be changed by nutrition education? Evaluation of the educational influence on children’s behaviour and nutritional knowledge. Educ. Health 2015, 33, 14–19. [Google Scholar]
- Roberts, K.C.; Shields, M.; de Groh, M.; Aziz, A.; Gilbert, J.-A. Overweight and obesity in children and adolescents: Results from the 2009 to 2011 Canadian Health Measures Survey. Health Rep. 2012, 23, 37–41. [Google Scholar]
- Aday, L.A.; Cornelius, L.J. Designing and Conducting Health Surveys: A Comprehensive Guide; John Wiley & Sons: Hoboken, NJ, USA, 2006. [Google Scholar]
- Sutherland, R.; Campbell, E.; Lubans, D.R.; Morgan, P.J.; Okely, A.D.; Nathan, N.; Wolfenden, L.; Wiese, J.; Gillham, K.; Hollis, J.; et al. ‘Physical Activity 4 Everyone’ school-based intervention to prevent decline in adolescent physical activity levels: 12 month (mid-intervention) report on a cluster randomised trial. Br. J. Sports Med. 2015, 50, 488–495. [Google Scholar] [CrossRef]
- Kothandan, S.K. School based interventions versus family based interventions in the treatment of childhood obesity—A systematic review. Arch. Public Health 2014, 72, 3. [Google Scholar] [CrossRef]
- Sobol-Goldberg, S.; Rabinowitz, J.; Gross, R. School-based obesity prevention programs: A meta-analysis of randomized controlled trials. Obesity 2013, 21, 2422–2428. [Google Scholar] [CrossRef]
- Dobbins, M.; Husson, H.; DeCorby, K.; LaRocca, R.L. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2013, 2, CD007651. [Google Scholar] [CrossRef]
- Williams, A.J.; Henley, W.E.; Williams, C.A.; Hurst, A.J.; Logan, S.; Wyatt, K.M. Systematic review and meta-analysis of the association between childhood overweight and obesity and primary school diet and physical activity policies. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 101. [Google Scholar] [CrossRef]
- Tucker, S.; Lanningham-Foster, L.; Murphy, J.; Olsen, G.; Orth, K.; Voss, J.; Aleman, M.; Lohse, C. A school-based community partnership for promoting healthy habits for life. J. Community Health 2011, 36, 414–422. [Google Scholar] [CrossRef]
- Waters, E.; De Silva-Sanigorski, A.; Burford, B.J.; Brown, T.; Campbell, K.J.; Gao, Y.; Armstrong, R.; Prosser, L.; Summerbell, C.D. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2011, 12, CD001871. [Google Scholar] [CrossRef]
- Wind, M.; Bjelland, M.; Pérez-Rodrigo, C.; Te Velde, S.J.; Hildonen, C.; Bere, E.; Klepp, K.I.; Brug, J. Appreciation and implementation of a school-based intervention are associated with changes in fruit and vegetable intake in 10- to 13-year old schoolchildren–the Pro Children study. Health Educ. Res. 2008, 23, 997–1007. [Google Scholar] [CrossRef]
- Schlechter, C.R.; Rosenkranz, R.R.; Guagliano, J.M.; Dzewaltowski, D.A. A systematic review of children’s dietary interventions with parents as change agents: Application of the RE-AIM framework. Prev. Med. 2016, 91, 233–243. [Google Scholar] [CrossRef]
- Sharifah, S.I.; Chin, Y.S.; Mohd, M.T.; Zalilah, M.S. School-based intervention to prevent overweight and disordered eating in secondary school Malaysian adolescents: A study protocol. BMC Public Health 2016, 16, 1101. [Google Scholar]
- Sabramani, V.; Idayu, I.; Rosnah, S.; Zaleha, M.I.; Saidatul, N.B.; Hasanain, F.G. Managing obesity in Malaysian schools: Are we doing the right strategies? Mal. J. Public Health Med. 2015, 15, 75–83. [Google Scholar]
- Van Stralen, M.M.; Yildirim, M.; te Velde, S.J.; Brug, J.; van Mechelen, W.; Chinapaw, M.J. What works in school-based energy balance behaviour interventions and what does not: A systematic review of mediating mechanisms. Int. J. Obes. 2011, 35, 1251–1265. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).