Validating Healthy Eating Index, Glycemic Index, and Glycemic Load with Modern Diets for E-Health Era
Abstract
:1. Introduction
2. Materials and Methods
2.1. Dietary Parameters and Indexes
2.2. Data Analysis
3. Results
3.1. Healthy Eating Parameters
3.2. Predictive Modeling for Healthy Eating Parameters
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Agher, D.; Sedki, K.; Despres, S.; Albinet, J.P.; Jaulent, M.C.; Tsopra, R. Encouraging Behavior Changes and Preventing Cardiovascular Diseases Using the Prevent Connect Mobile Health App: Conception and Evaluation of App Quality. J. Med. Internet Res. 2022, 24, e25384. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.L.; Yang, H.L.; Kusuma, J.D.; Shiao, S.P.K. Validating Accuracy of an Internet-Based Application against USDA Computerized Nutrition Data System for Research on Essential Nutrients among Social-Ethnic Diets for the E-Health Era. Nutrients 2022, 14, 3168. [Google Scholar] [CrossRef] [PubMed]
- Shiao, S.P.K.; Grayson, J.; Lie, A.; Yu, C.H. Predictors of the Healthy Eating Index and Glycemic Index in multi-ethnic colorectal cancer families. Nutrients 2018, 10, 674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shiao, S.P.K.; Grayson, J.; Lie, A.; Yu, C.H. Personalized nutrition—Genes, diet, and related interactive parameters as predictors of cancer in multiethnic colorectal cancer families. Nutrients 2018, 10, 795. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shiao, S.P.K.; Grayson, J.; Yu, C.H.; Wasek, B.; Bottiglieri, T. Gene Environment Interactions and Predictors of Colorectal Cancer in Family-Based, Multi-Ethnic Groups. J. Personal. Med. 2018, 8, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tucker, K.L. Dietary patterns, approaches, and multicultural perspective. Appl. Physiol. Nutr. Metab. 2010, 35, 211–218. [Google Scholar] [CrossRef]
- Turati, F.; Bravi, F.; DiMaso, M.; Bosetti, C.; Polesel, J.; Serraino, D.; Dalmartello, M.; Giacosa, A.; Montella, M.; Tavani, A.; et al. Adherence to the World Cancer Research Fund/American Institute for Cancer Research recommendations and colorectal cancer risk. Eur. J. Cancer 2017, 85, 86–94. [Google Scholar] [CrossRef]
- Vieira, A.R.; Abar, L.; Chan, D.S.M.; Vingeliene, S.; Polemiti, E.; Stevens, C.; Greenwood, D.; Norat, T. Foods and beverages and colorectal cancer risk: A systematic review and meta-analysis of cohort studies, an update of the evidence of the WCRF-AICR Continuous Update Project. Ann. Oncol. 2017, 28, 1788–1802. [Google Scholar] [CrossRef]
- Magalhães, B.; Peleteiro, B.; Lunet, N. Dietary patterns and colorectal cancer: Systematic review and meta-analysis. Eur. J. Cancer Prev. 2012, 21, 15–23. [Google Scholar] [CrossRef]
- Powell, L.; Nguyen, B. Fast-Food and Full-service Restaurant Consumption among Children and Adolescents: Impact on Energy, Beverage and Nutrient Intake. JAMA Pediatr. 2013, 167, 14–20. [Google Scholar] [CrossRef] [Green Version]
- Ocké, M.C. Evaluation of methodologies for assessing the overall diet: Dietary quality scores and dietary pattern analysis. Proc. Nutr. Soc. 2013, 72, 191–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hiza, H.A.; Casavale, K.O.; Guenther, P.M.; Davis, C.A. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J. Acad Nutr. Diet 2013, 113, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Van Horn, L. Healthy eating: What’s your number. J. Am. Diet Assoc. 2008, 108, 1817. [Google Scholar] [CrossRef] [PubMed]
- Guenther, P.M.; Reedy, J.; Krebs-Smith, S.M. Development of the Healthy Eating Index-2005. J. Am. Diet Assoc. 2008, 108, 1896–1901. [Google Scholar] [CrossRef] [PubMed]
- Millar, S.R.; Navarro, P.; Harrington, J.M.; Perry, I.J.; Phillips, C.M. Dietary Quality Determined by the Healthy Eating Index-2015 and Biomarkers of Chronic Low-Grade Inflammation: A Cross-Sectional Analysis in Middle-to-Older Aged Adults. Nutrients 2021, 13, 222. [Google Scholar] [CrossRef]
- Navarro, S.L.; Tarkhan, A.; Shojaie, A.; Randolph, T.W.; Gu, H.; Djukovic, D.; Osterbauer, K.J.; Hullar, M.A.; Kratz, M.; Neuhouser, M.L.; et al. Plasma metabolomics profiles suggest beneficial effects of a low-glycemic load dietary pattern on inflammation and energy metabolism. Am. J. Clin. Nutr. 2019, 110, 984–992. [Google Scholar] [CrossRef]
- Neuhouser, M.L.; Schwarz, Y.; Wang, C.; Breymeyer, K.; Coronado, G.; Wang, C.Y.; Noar, K.; Song, X.; Lampe, J.W. A low-glycemic load diet reduces serum C-reactive protein and modestly increases adiponectin in overweight and obese adults. J. Nutr. 2012, 142, 369–374. [Google Scholar] [CrossRef] [Green Version]
- Fan, Y.; Jin, X.; Man, C.; Gao, Z.; Wang, X. Meta-analysis of the association between the inflammatory potential of diet and colorectal cancer risk. Oncotarget 2017, 8, 59592–59600. [Google Scholar] [CrossRef] [Green Version]
- American Diabetes Association. Carb Counting and Diabetes. Available online: https://diabetes.org/healthy-living/recipes-nutrition/understanding-carbs/carb-counting-and-diabetes (accessed on 15 January 2023).
- WebMD. How to Count Carbs. Available online: https://www.webmd.com/diabetes/diabetes-how-count-carbs (accessed on 15 January 2023).
- The LIVESTRONG Foundation. How Many Grams of Carbs Should You Eat Per Meal? Available online: https://www.livestrong.com/article/427735-number-of-carbohydrates-needed-per-meal (accessed on 15 January 2023).
- Marsh, K.; Barclay, A.; Colagiuri, S.; Brand-Miller, J. Glycemic index and glycemic load of carbohydrates in the diabetes diet. Curr. Diab. Rep. 2011, 11, 120–127. [Google Scholar] [CrossRef]
- Ojo, O.; Ojo, O.O.; Adebowale, F.; Wang, X.H. The Effect of Dietary Glycaemic Index on Glycaemia in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2018, 10, 373. [Google Scholar] [CrossRef] [Green Version]
- Alfonsi, J.E.; Choi, E.E.Y.; Arshad, T.; Sammott, S.S.; Pais, V.; Nguyen, C.; Maguire, B.R.; Stinson, J.N.; Palmert, M.R. Carbohydrate Counting App Using Image Recognition for Youth with Type 1 Diabetes: Pilot Randomized Control Trial. JMIR mHealth uHealth 2020, 8, e22074. [Google Scholar] [CrossRef] [PubMed]
- Kusuma, J.D.; Yang, H.L.; Yang, Y.L.; Chen, Z.F.; Shiao, S.P.K. Validating Accuracy of a Mobile Application against Food Frequency Questionnaire on Key Nutrients with Modern Diets for mHealth Era. Nutrients 2022, 14, 537. [Google Scholar] [CrossRef] [PubMed]
- Nutrition Coordinating Center (NCC). Nutrition Data System for Research. Available online: http://www.ncc.umn.edu/food-and-nutrient-database/ (accessed on 16 January 2023).
- Schakel, S.F.; Sievert, Y.A.; Buzzard, I.M. Sources of data for developing and maintaining a nutrient database. J. Am. Diet Assoc. 1988, 88, 1268–1271. [Google Scholar] [CrossRef]
- Harnack, L.; Lee, S.; Schakel, S.F.; Duval, S.; Luepker, R.V.; Arnett, D.K. Trends in the trans-fatty acid composition of the diet in a metropolitan area: The Minnesota Heart Survey. J. Am. Diet Assoc. 2003, 103, 1160–1166. [Google Scholar] [CrossRef]
- United States Department of Agriculture (USDA). Healthy Eating Index (HEI). Available online: https://www.fns.usda.gov/healthy-eating-index-hei (accessed on 16 January 2023).
- Panizza, C.E.; Shvetsov, Y.B.; Harmon, B.E.; Wilkens, L.R.; Le Marchand, L.; Haiman, C.; Reedy, J.; Boushey, C.J. Testing the Predictive Validity of the Healthy Eating Index-2015 in the Multiethnic Cohort: Is the Score Associated with a Reduced Risk of All-Cause and Cause-Specific Mortality? Nutrients 2018, 5, 452. [Google Scholar] [CrossRef] [Green Version]
- The University of Sydney. About Glycemic Index. Available online: http://www.glycemicindex.com/about.php (accessed on 15 January 2023).
- Harvard Health Publishing. Glycemic Index for 60+ Foods. Available online: https://www.health.harvard.edu/diseases-and-conditions/glycemic-index-and-glycemic-load-for-100-foods (accessed on 15 January 2023).
- Bowman, S.A.; Lino, M.; Gerrior, S.A.; Basiotis, P.P. The Healthy Eating Index: 1994–1996. U.S. Department of Agriculture, Center for Nutrition Policy and Promotion. CNPP-5. Available online: https://www.researchgate.net/publication/242508135_The_Healthy_Eating_Index_1994-96#read (accessed on 15 January 2023).
- Atkinson, F.S.; Foster-Powell, K.; Brand-Miller, J.C. International Tables of Glycemic Index and Glycemic Load Values: 2008. Diabetes Care 2008, 31, 2281–2283. [Google Scholar] [CrossRef] [Green Version]
- Higdon, J. Glycemic Index and Glycemic Load. Available online: http://lpi.oregonstate.edu/mic/food-beverages/glycemic-index-glycemic-load (accessed on 15 January 2023).
- Mendosa, D. Revised International Table of Glycemic Index (GI) and Glycemic Load (GL) Values—2008. Available online: http://www.mendosa.com/gilists.htm (accessed on 15 January 2023).
- Grayson, J.; Gardner, S.; Stephens, M. Building Better Models with JMP® Pro. 2015; SAS Press: Cary, NC, USA, 2015. [Google Scholar]
- Klimberg, R.; McCullough, B.D. Fundamentals of Predictive Analytics with JMP, 2nd ed.; SAS Press: Cary, NC, USA, 2016. [Google Scholar]
- SAS Institute Inc. JMP 13 One-Way ANOVA, 2nd ed.; SAS Institute Inc.: Cary, NC, USA, 2016. [Google Scholar]
- Wu, Y. Elastic Net for Cox’s proportional hazards model with a solution path algorithm. Stat. Sin. 2012, 22, 27–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- SAS Institute Inc. JMP 13 Fitting Linear Models, 2nd ed.; SAS Institute Inc.: Cary, NC, USA, 2016. [Google Scholar]
- Cheng, H.; Garrick, D.J.; Fernando, R.L. Efficient strategies for leave-one-out cross validation for genomic best linear unbiased predictors. J. Anim. Sci. Biotechnol. 2017, 8, 38. [Google Scholar] [CrossRef] [Green Version]
- Vega-Lopez, S.; Venn, B.J.; Slavin, J.L. Relevance of the Glycemic Index and Glycemic Load for Body Weight, Diabetes, and Cardiovascular Disease. Nutrients 2018, 10, 1361. [Google Scholar] [CrossRef] [Green Version]
- Augustin, L.S.; Kendall, C.W.; Jenkins, D.J.; Willett, W.C.; Astrup, A.; Barclay, A.W.; Björck, I.; Brand-Miller, J.C.; Brighenti, F.; Buyken, A.E.; et al. Glycemic index, glycemic load and glycemic response: An International Scientific Consensus Summit from the International Carbohydrate Quality Consortium (ICQC). Nutr. Metab. Cardiovasc. Dis. 2015, 25, 795–815. [Google Scholar] [CrossRef] [Green Version]
- Bhupathiraju, S.N.; Tobias, D.K.; Malik, V.S.; Pan, A.; Hruby, A.; Manson, J.E.; Willett, W.C.; Hu, F.B. Glycemic index, glycemic load, and risk of type 2 diabetes: Results from 3 large US cohorts and an updated meta-analysis. Am. J. Clin. Nutr. 2014, 100, 218–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pauwels, S.; Doperé, I.; Huybrechts, I.; Godderis, L.; Koppen, G.; Vansant, G. Reproducibility and validity of an FFQ to assess usual intake of methyl-group donors. Public Health Nutr. 2015, 18, 2530–2539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xie, B.; Gilliland, F.D.; Li, Y.F.; Rockett, H.R. Effects of ethnicity, family income, and education on dietary intake among adolescents. Prev. Med. 2003, 36, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Rehm, C.D.; Monsivais, P.; Drewnowski, A. The quality and monetary value of diets consumed by adults in the United States. Am. J. Clin. Nutr. 2011, 94, 1333–1339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larson, N.; Eisenberg, M.E.; Berge, J.M.; Arcan, C.; Neumark-Sztainer, D. Ethnic/racial disparities in adolescents’ home food environments and linkages to dietary intake and weight status. Eat Behav. 2015, 16, 43–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Parameters, Units (Units, Max Score) | M ± SD M ± SD | Liquid N = 8 | Convenient N = 30 | Ethnic N = 71 | Smoothie N = 22 | p (F) |
|---|---|---|---|---|---|---|
| Total Fruits, cup | Intake | 2.27 ± 1.70 | 0.39 ± 0.40 | 0.86 ± 0.94 | 5.88 ± 1.60 | <0.0001 |
| (>0.8 cup, 5) | Score | 5 ± 0 | 2.09 ± 1.53 | 3.13 ± 1.29 | 5 ± 0 | S > L E C; L > E C |
| Whole Fruits, cup | Intake | 1.49 ± 2.17 | 0.11± 0.12 | 0.69 ± 0.89 | 5.53 ± 1.52 | <0.0001 |
| (>0.4 cup, 5) | Score | 2.50 ± 2.67 | 1.33 ± 1.49 | 3.87 ± 1.03 | 5 ± 0 | S > L E C; L > C |
| Vegetables, cup | Intake | 1.71 ± 3.17 | 0.89 ± 0.50 | 1.07 ± 0.80 | 7.40 ± 2.09 | <0.0001 |
| (>1.1 cup, 5) | Score | 1.25 ± 2.31 | 3.47 ± 1.10 | 4.00 ± 1.02 | 5 ± 0 | S > L E C |
| Dark greens, cup | Intake | 0.86 ±1.62 | 0.12 ± 0.29 | 0.41 ± 0.44 | 3.73 ± 1.01 | <0.0001 |
| (>0.4 cup, 5) | Score | 1.25 ± 2.31 | 1.04 ± 1.18 | 3.69 ± 1.17 | 5 ± 0 | S > L E C; L > C |
| Total Grains, oz | Intake | 0.00 ± 0.00 | 2.28 ± 1.46 | 2.65 ± 1.72 | 4.27 ± 2.79 | <0.0001 |
| (>3 oz., 5) | Score | 0.00 ± 0.00 | 3.24 ± 1.43 | 3.86 ± 1.00 | 4.33 ± 1.20 | S > E C L; E C > L |
| Whole Grains, oz | Intake | 0.00 ± 0.00 | 0.27 ± 0.16 | 0.51 ± 0.46 | 0.92 ± 0.61 | <0.0001 |
| (>1.5 oz., 5) | Score | 0.00 ± 0.00 | 0.88 ± 0.52 | 1.58 ± 1.02 | 2.80 ± 1.61 | S > E C L; E > C L |
| Dairy, cup | Intake | 0.88 ± 0.40 | 0.60 ± 0.19 | 0.52 ± 0.21 | 0.82 ± 0.71 | 0.0014 |
| (>1.3 cup, 10) | Score | 6.72 ± 3.08 | 4.61 ± 1.48 | 4.02 ± 1.60 | 5.29 ± 3.50 | L S > E |
| Proteins, oz | Intake | 0.00 ± 0.00 | 4.77 ± 2.95 | 3.87 ± 1.45 | 9.15 ± 6.16 | <0.0001 |
| (>2.5 oz., 10) | Score | 0.00 ± 0.00 | 9.36 ± 1.07 | 9.16 ± 1.46 | 9.49 ± 1.47 | S > C E L; C E > L |
| Oils and Nuts, g | Intake | 0.06 ± 0.08 | 12.77 ± 10.25 | 4.47 ± 3.12 | 21.80 ± 28.97 | <0.0001 |
| (>12 g, 10) | Score | 0.05 ± 0.07 | 7.35 ± 3.81 | 3.51 ± 2.24 | 7.33 ± 3.44 | S > E L; C > E |
| Saturated Fats, % calorie | Intake | 1.57± 1.78 | 17.12 ± 6.13 | 10.27 ± 5.79 | 23.07 ± 17.37 | <0.0001 |
| (<8% calorie, 10) | Score | 8.91 ± 2.08 | 5.42 ± 2.10 | 6.63 ± 2.67 | 9.12 ± 1.81 | S > E L; C > E L; E > L |
| Sodium, g | Intake | 2.45 ± 1.82 | 2.25 ± 0.84 | 2.62 ± 1.80 | 5.81 ± 2.45 | <0.0001 |
| (<1.1 g, 10) | Score | 3.75 ± 5.18 | 1.39 ± 1.67 | 1.31 ± 2.13 | 0 ± 0 | S > E L |
| Empty Calories, calorie | Intake | 203.50 ± 0.00 | 283.6 ± 169.5 | 61.89 ± 39.19 | 171.50 ± 179.2 | <0.0001 |
| (<19% calorie, 20) | Score | 19.34 ± 1.86 | 17.14 ± 4.08 | 20.00 ± 0.00 | 20 ± 0 | C > S E; L S > E |
| Healthy Eating Index Score | 48.78 ± 6.37 | 57.86 ± 4.90 | 65.28 ± 5.17 | 78.61 ± 7.43 | <0.0001 | |
| >80 (good) | 0 (0%) | 0 (0%) | 1 (1.4%) | 11 (50%) | S > E C L; E > C L; C > L | |
| ≥64.4 (median distribution) | 0 (0%) | 3 (10%) | 38 (53.5%) | 21 (95.5%) | ||
| Glycemic Index Score | 56.38 ± 4.96 | 59.86 ± 3.06 | 58.88 ± 4.82 | 54.52 ± 3.72 | <0.0001 | |
| ≤55 (low and good) | 2 (25.0%) | 1 (3.33%) | 9 (12.9%) | 14 (63.6%) | C E > S | |
| ≤59 (median distribution) | 3 (27.3%) | 12 (40%) | 20 (28.2%) | 21 (95.5%) | ||
| Glycemic Load (GI x Carbohydrate/100) | 74.30 ± 39.47 | 89.20 ± 24.87 | 68.69 ± 31.71 | 240.8 ± 75.77 | <0.0001 | |
| ≤71.8 (median distribution) | 4 (50%) | 9 (30%) | 53 (74.6%) | 0 (0%) | S > E L C | |
| ≥20 (high) | 8 (100%) | 30 (100%) | 71 (100%) | 22 (100%) | ||
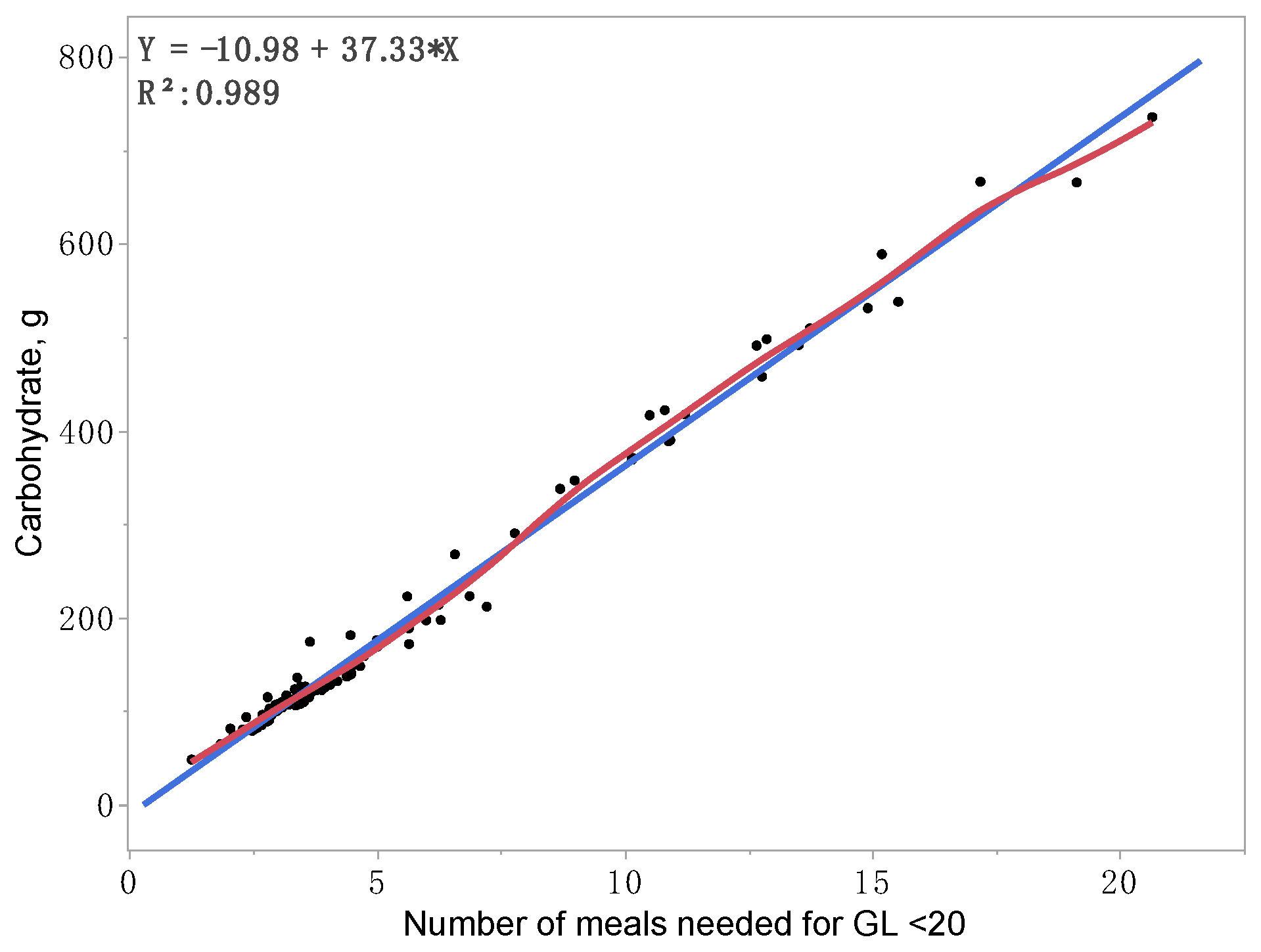
| Number of Meals Needed for GL < 20 | 3.71 ± 1.97 | 4.46 ± 1.24 | 3.43 ± 1.59 | 12.04 ± 3.79 | <0.0001 | |
| ≤3.59 (median distribution) | 4 (50%) | 9 (30%) | 53 (74.6%) | 0 (0%) | S > E L C | |
| Carbohydrates, g | 135.6 ± 81.01 | 148.7 ± 40.40 | 117.4 ± 55.73 | 444.2 ± 140.3 | <0.0001 | |
| ≤123.4 g (median distribution) | 4 (50%) | 10 (33.3%) | 52 (73.2%) | 0 (0%) | S > E L C | |
| Carbohydrates/Meals (GL < 20), g | 35.73 ± 3.30 | 33.50 ± 1.71 | 34.23 ± 3.31 | 36.83 ± 2.23 | 0.0003 | |
| ≤33.95 g (median distribution) | 5 (62.5%) | 17 (56.7%) | 43 (60.6%) | 1 (4.5%) | S > C E | |
| Parameters, Median Units | Logistic Regression Original Model | Generalized Regression Elastic Net Validation | ||
|---|---|---|---|---|
| Estimate (95% CI) | p (χ2) | Estimate (95% CI) | p (χ2) | |
| (Intercept) | −12.46 (−289.1–264.2) | 0.9296 | −9.35 (−9.90–−8.81) | <0.0001 |
| Whole Fruits, ≥0.33 cup | −14.56 (−301.0–271.9) | 0.9206 | −11.40 (−13.54–−9.26) | <0.0001 |
| Whole Grains, ≥0.41 oz | 14.10 (−292.0–263.7) | 0.9208 | −11.02 (−13.21–−8.83) | <0.0001 |
| Empty Calories, ≤88.87 calorie | −14.86 (−261.8–291.5) | 0.9161 | 11.75 (9.64–13.86) | <0.0001 |
| MR | 0.00 | 0.00 | ||
| AICc | 9.77 | 9.78 | ||
| AUC | 1.00 | 1.00 | ||
| Parameters, Median Units | Logistic Regression Original Model | Generalized Regression Elastic Net Validation | ||
|---|---|---|---|---|
| Estimate (95% CI) | p (χ2) | Estimate (95% CI) | p (χ2) | |
| GI≤ 55 | ||||
| (Intercept) | 11.89 (−131.97–155.74) | 0.8713 | 9.68 (7.30–12.05) | <0.0001 |
| Total Fruits, ≥0.43 cup | −11.74 (−155.58–−132.11) | 0.8729 | −9.53 (−10.27–−8.78) | <0.0001 |
| Carbohydrates, ≥123.4 g | −2.06 (−3.44–−0.67) | 0.0037 | −2.06 (−3.42–−0.69) | 0.0032 |
| Mexican Diets | −11.83 (−155.69–132.02) | 0.8719 | −9.63 (−11.91–−7.35) | <0.0001 |
| MR | 0.23 | 0.23 | ||
| AICc | 33.63 | 33.63 | ||
| AUC | 0.84 | 0.84 | ||
| GI ≤ 59 (median) | ||||
| (Intercept) | 1.97 (−155.9–159.8) | 0.9805 | 1.84 (0.14–3.54) | 0.0336 |
| Total Fruits, ≥0.43 cup | −1.47 (−2.38–−0.56) | 0.0016 | −1.47 (−2.38–−0.56) | 0.0016 |
| Mexican Diets | −10.83 (−127.6–106.0) | 0.8558 | −9.92 (−10.99–−8.86) | <0.0001 |
| Chinese Diets | 9.46 (−96.73–115.7) | 0.8614 | 8.69 (7.63–9.74) | <0.0001 |
| MR | 0.13 | 0.13 | ||
| AICc | 33.66 | 33.66 | ||
| AUC | 0.89 | 0.89 | ||
| Parameters, Median Units | Logistic Regression with Validation | Generalized Regression Elastic Net Validation | ||
|---|---|---|---|---|
| Estimate (95% CI) | p (χ2) | Estimate (95% CI) | p (χ2) | |
| (Intercept) | −2.48 (−3.50–−1.46) | <0.0001 | −1.96 (−2.63–−1.28) | <0.0001 |
| Carbohydrates, ≥123.4 g | 4.66 (3.28–6.04) | <0.0001 | 3.67 (2.72–4.62) | <0.0001 |
| MR | 0.13 | 0.13 | ||
| AICc | 29.33 | 28.53 | ||
| AUC | 0.8733 | 0.8733 | ||
| Parameters, Median Units | Logistic Regression with Validation | Generalized Regression Elastic Net Validation | ||
|---|---|---|---|---|
| Estimate (95% CI) | p (χ2) | Estimate (95% CI) | p (χ2) | |
| 3 Diet Factors (Final Model) | ||||
| (Intercept) | −17.38 (−183.4–148.6) | 0.8374 | −15.81 (−19.00–−12.61) | <0.0001 |
| Canned Food Diets | 1.41 (0.45–2.36) | 0.0082 | 2.91 (0.75–5.07) | 0.0082 |
| Mexican Diets | 2.91 (0.75–5.07) | 0.8907 | 10.06 (9.10–11.02) | <0.0001 |
| Smoothie Diets | 3.80 (1.72–5.89) | 0.0004 | 3.80 (1.72–5.88) | 0.0004 |
| MR | 0.20 | 0.20 | ||
| AICc | 35.09 | 35.09 | ||
| AUC | 0.8125 | 0.8125 | ||
| 2 HEI and 1 Diet Factors | ||||
| (Intercept) | −12.26 (−178.2–153.8) | 0.8849 | −10.85 (−12.09–−9.61) | <0.0001 |
| Total Fruits, ≥0.43 cup | 1.59 (0.65–2.53) | 0.0009 | 1.59 (0.65–2.54) | 0.0009 |
| Whole Grains, ≥0.41 oz | 1.41 (0.45–2.36) | 0.0039 | 1.41 (0.46–2.36) | 0.0037 |
| Mexican Diets | 10.89 (−115.1–176.9) | 0.8977 | 9.48 (8.29–10.66) | <0.0001 |
| MR | 0.30 | 0.30 | ||
| AICc | 36.33 | 36.33 | ||
| AUC | 0.88 | 0.88 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Z.-F.; Kusuma, J.D.; Shiao, S.-Y.P.K. Validating Healthy Eating Index, Glycemic Index, and Glycemic Load with Modern Diets for E-Health Era. Nutrients 2023, 15, 1263. https://doi.org/10.3390/nu15051263
Chen Z-F, Kusuma JD, Shiao S-YPK. Validating Healthy Eating Index, Glycemic Index, and Glycemic Load with Modern Diets for E-Health Era. Nutrients. 2023; 15(5):1263. https://doi.org/10.3390/nu15051263
Chicago/Turabian StyleChen, Zhao-Feng, Joyce D. Kusuma, and Shyang-Yun Pamela K. Shiao. 2023. "Validating Healthy Eating Index, Glycemic Index, and Glycemic Load with Modern Diets for E-Health Era" Nutrients 15, no. 5: 1263. https://doi.org/10.3390/nu15051263
APA StyleChen, Z.-F., Kusuma, J. D., & Shiao, S.-Y. P. K. (2023). Validating Healthy Eating Index, Glycemic Index, and Glycemic Load with Modern Diets for E-Health Era. Nutrients, 15(5), 1263. https://doi.org/10.3390/nu15051263






